Abstract
Background
Remote consulting has become part of the medical student clinical experience in primary care, but little research exists regarding the impact on learning.
Aim
To describe the experiences of General Practitioner (GP) educators and medical students in using student-led remote consultations as an educational tool.
Method
A qualitative, explorative study conducted at four UK medical schools. GP educators and medical students were purposively sampled and interviewed.
Results
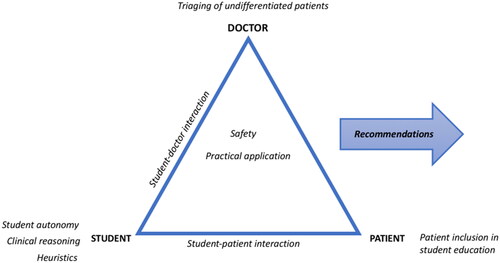
Nine themes arose: practical application, autonomy, heuristics, safety, triage of undifferentiated patients, clinical reasoning, patient inclusion in student education, student–patient interaction, and student–doctor interaction.
Discussion
Remote consulting has become part of the clinical placement experience. This has been found to expose students to a wider variety of clinical presentations. Verbal communication, history-taking, triage, and clinical reasoning skills were practised through remote consulting, but examination skills development was lacking. Students found building rapport more challenging, although this was mitigated by having more time with patients. Greater clinical risk was perceived in remote consulting, which had potential to negatively impact students’ psychological safety. Frequent debriefs could ameliorate this risk and positively impact student–doctor relationships. Student autonomy and independence increased due to greater participation and responsibility. Pre-selection of patients could be helpful but had potential to expose students to lower complexity patients.
Practice points
Remote consulting confers unique educational benefits.
Remote consulting can help develop history-taking and communication skills, as well as clinical reasoning skills.
The psychological safety of the student and the supervisory risk of the tutor can be impacted by remote consulting, but frequent debriefs between the student and tutor can help mitigate this risk.
Learning how to conduct remote, and face-to-face consultations is important in medical education.
Introduction
Face-to-face consultations were the main consultation modality in primary care until the COVID-19 pandemic necessitated a sudden transition to remote consulting i.e. the use of telephone or video (Turner et al. Citation2021). This shift to remote consulting impacted medical student education. Although justified at the time, we lack pedagogical evidence on the limitations and opportunities of remote consulting in medical education. It is now time to pause and re-assess.
Research exploring doctor-led remote consultations has found remote consultations provide an efficient alternative to face-to-face consultations but may not be appropriate for complex cases with multimorbidity (Donaghy et al. Citation2019; Misselbrook Citation2021). Remote consulting can improve access to care, but raises concerns about safety; although, familiarity between patients and clinicians reduces this risk (McKinstry et al. Citation2009). However, none of these papers on remote consulting consider the added dimension encountered within medical education: the student–patient and student–doctor relationships. A recent report predicted that remote consulting is likely to remain (RCGP Citation2021) so should be embedded in the medical student learning experience.
Darnton et al. (Citation2021) evaluated how a population of GP practices reorganised their medical students’ exposure to patients in response to the pandemic, concluding that student contact with patients reduced, but that triaging systems increased the educational value of individual contact. Remote consulting conferred specific educational benefits, but this was dependent upon how students were supervised. The potential to decrease their level of participation was also highlighted (Park et al. Citation2015 cited in Darnton et al. Citation2021).
Al-bedaery et al. (Citation2021) analysed teaching utilising remote consultations, demonstrating that a sequential style of supervision positively impacted student engagement and confidence. Improved frequency and quality of tutor feedback was also observed. In agreement with Darnton et al. (Citation2021), students found passive observation of remote patient encounters disengaging. Both papers discussed barriers to good learning from remote consulting, including GP tutors’ reluctance to allow student autonomy, difficulties in cultivating a team ethos, lack of examination skills practise and reduced clinical variety.
By interviewing students and GP educators across a wider geographical area, we aim to better understand experiences of remote consultations in primary care teaching. We deconstruct what influences the level of student participation when remote consulting is used as an educational tool. We also examine how remote consulting affects the triadic relationship between student, doctor, and patient, identified as crucial to medical education by Park et al. (Citation2015), and how these interactions can be made meaningful, even when conducted remotely. Finally, we consider what promotes effective learning when remote consulting is used as an educational tool, identifying barriers and opportunities and devising recommendations for educators.
Methodology
This qualitative, explorative study was conducted at four UK medical schools (University of Glasgow, Newcastle University, Queen Mary University of London [QMUL] and University College London [UCL]). Participant recruitment was by purposive sampling. Inclusion criteria were: undergraduate medical students in the clinical years (years 3–6) with experience of general practice and GP tutors with experience of student-led remote consultations. Participants were recruited via student forums and direct emails.
Remote consultations were defined as any doctor–patient interaction performed via telephone or video.
Qualitative, semi-structured interviews were conducted using one of two interview schedules (Supplementary Appendices 1 and 2). These interview schedules were adapted slightly in recognition of the differing experience of GPs and students. Our social constructionist epistemology (Bunniss and Kelly Citation2010) invites an iterative approach, identifying themes and better understanding the participants’ experiences (Braun and Clarke Citation2006).
Interviews were undertaken via video conferencing software. These were recorded and transcribed verbatim either by our research team, video conferencing software’s auto-transcriptions or by an external transcription organisation. The interview transcripts were analysed thematically and coded using NVIVO (released March 2020), by members of our research team (QSR International Pty Ltd. Citation2020). Taking an iterative approach to grouping codes and defining the key themes permitted the capturing of new ideas. Undertaking frequent team discussions achieved consistency, as did ‘double-coding’ some transcripts (two researchers coding the same transcript). This allowed a mechanism for highlighting disagreement, which was then resolved through dialogue. A mutually devised codebook was developed, which was used to code subsequent transcripts.
A Patient and Public Involvement representative was involved throughout, helping design the interview schedule, reviewing the codebook, and writing up results. Two medical students also contributed to the project. Ethical approval was granted for this study from all four institutions.
Results
Nineteen GP tutor interviews and eighteen student interviews were performed across the four institutions (). The ‘Timeline of Interviews by Medical School’ shows the interview schedule across the four organisations ().
Table 1. Interviewee demographics and course information.
Analysis arising from the interviews was refined into nine themes: practical application of remote consulting, student autonomy, heuristics, safety, triage of undifferentiated patients, clinical reasoning, patient inclusion in student education, student–patient interaction, and student–doctor interaction ().
Practical application of student-led remote consulting
Experiences of students undertaking remote consultations were mixed, and supervisory practices of GP tutors varied. Most GPs allocated patients from their own list, some used remote consulting themselves to triage patients, inviting those who required a face-to-face appointment into surgery for the students to see. A small number used an e-consult system (patient submitted data regarding their presenting complaint) to identify patients that would be good for students. Students experiencing the e-consult system found it beneficial to prepare for speaking with the patient, but noted the potential for de-skilling as much of the history had already been taken.
Regarding the location of consultations; most students were onsite. Students and tutors overwhelmingly preferred this. However, some were involved in remote consultations offsite (from home) via three-way video links. Problems encountered when students were offsite included: supervisory concerns (harder to give or receive supervision), confidentiality concerns, problems accessing computer systems, reduced team integration, reduced student well-being, and inability to set personal/professional boundaries. A small minority of students preferred offsite because it reduced commuting time.
There’s the whole work/life balance …… I like the journey to and from the GP practice.
(Glasgow Student 3)
I think you definitely act more professionally in a professional environment.
(Newcastle Student 5)
Remote consulting often raised challenges such as issues with connectivity, malfunctioning technology, and the need for users to rapidly upskill. Key enablers to student-led remote consulting included provision of a phone and a space to consult.
Frequently, students had undertaken previous placements where remote consulting was used as a teaching tool. If the GP was inexperienced, students often had to guide GPs on how to proceed. Participants interviewed at the beginning of the study period were more likely to report this than those interviewed later.
So, a lot of it was saying ‘oh the previous doctor I was with did this, so maybe we could try and do that’.
(UCL Student 4)
Most interviewees reported using video consulting less frequently than telephone, as it was more time consuming, and there was a perception that some patients either found it difficult, or lacked a ‘smart’ phone. However, two GPs reported using video consultations often, because they were useful for both consulting and teaching.
We have done one or two videos ….I think the students actually liked it … at least they got to see them on screen I think they prefer this more than just telephone.
(QMUL GP 3)
Autonomy of student
Students took histories and gave simple management advice when consulting remotely and found this ‘useful’ for their learning. Remote consulting usually offered increased student independence compared with face-to-face. Reasons included less time observing, more patient encounters, calling patients independently, holding more responsibility, being better at displaying confidence and having greater autonomy over learning. However, this independence was dependent on the methodology employed by the GP.
Some tutors remained in the room whilst the students consulted, others did not. Some less-experienced students consulted in pairs. A few students described passively observing remote consultations, which they found not conducive to learning, and worse than observing face-to-face consultations.
When I’m watching them [remote consultations]… it’s very easy to disengage…. Whereas if you have a patient in front of you, you show them respect and courtesy and of course you listen.
(Glasgow Student 4)
Students saw being permitted to partake, rather than observe, as essential to effectively learn from remote consulting.
There have been a lot of independent consultations this year…. you can develop your own style.
(Newcastle Student 2)
The exception to this commonly held opinion was when observation gradually built up to independent consulting. In this situation, it was deemed useful.
What was really helpful at the beginning of my placement was letting me… sit in and listen and ask any questions…. Then… giving me time after I’ve called the patient to discuss things and debrief and ask any questions.
(UCL Student 3)
Where there was reduced student autonomy in the remote setting, reasons included the perception of increased risk, and supervisory difficulties.
Heuristics
There was an acknowledgement from most students and some GPs that remote consulting improved verbal communication and history-taking skills, due to a reliance on verbal communication, alongside taking a greater number of histories, resulting in more practice. E-consultations were felt by some to particularly improve focused history-taking skills, but tended to be used less.
The most useful part of remote consulting was the sheer volume of patients that you can actually end up talking to.
(UCL Student 6)
Students also liked remote consulting because it allowed them to research the presenting complaint whilst consulting with patients. This both aided their consultation, and reinforced learning.
The patient can’t see you, so you can be looking things up.
(UCL Student 4)
Despite the accepted educational benefits of remote consulting, the overarching belief amongst the majority of GPs and some students was that the overall face-to-face consulting was better for learning. Reasons for this included being able to examine patients, use all five senses, establish a human connection, understand the patient experience, access patients who struggled with technology, concentrate on the patient rather than the technology, and better ‘link’ the history with the examination.
Both students and GPs frequently raised concerns about the inability to perform clinical examinations during remote consultations. These concerns related to a perceived increase in diagnostic uncertainty and an impact on learning examination skills. There were also reports that the history and examination became disjointed.
It very much condenses the entire thing into a history, basically, and in terms of practising that is probably quite limiting. It’s kind of like learning to drive an automatic…
(UCL Student 5)
Clinical reasoning
‘Clinical reasoning’ is the thought process preceding the formulation of differential diagnosis’ and a management plan. Approximately half of students interviewed thought clinical reasoning could be learned just as effectively, if not more so, from remote consulting, compared with face-to-face. A number of GPs agreed, although one GP felt that it made no difference.
To be able to pick up on key points in history that would lead you to a diagnosis, without being able to see a patient, has been really useful.
(Newcastle Student 2)
At the end of the remote consultation, students had to decide whether to bring the patient into surgery. All students conferred with the GP prior to making this decision.
The decision whether the patient should be examined or not is not one that we would make as medical students. It….requires a lot of experience from the GP…
(UCL Student 4)
However, remote consulting was perceived by some students to present challenges to clinical reasoning, due to the focus on history rather than examination. Several GPs concurred, discussing that remote consulting normalised ‘risk-taking consulting.’
Safety
The theme of ‘safety’ arose, encapsulating; the clinical safety of the patient, the psychological safety of the student and the supervisory risk to the GP tutor. In terms of clinical safety of the patient, there was a consensus amongst both students and GP tutors that challenges in gauging patient understanding, missing non-verbal cues and the lack of examination made it harder to gain clinical information, thus increasing the risk incurred when consulting remotely. GPs acknowledged this added risk for their own remote practice, but felt that students, who often did not know the patients’ background, and were clinically less experienced, undertook an even greater risk.
Giving people drugs and treatments and not seeing them really makes me anxious.
(Glasgow Student 2)
I think if you’re lacking experience, the risk of making mistakes, if you don’t have the full range of inputs and senses is greater.
(Newcastle GP 2)
The second ‘safety’ theme was the psychological safety of the student. Student-led remote consulting was generally felt to be more pressurised for students than face-to-face, due to the uncertainty of diagnosis, concerns about missing something, and the possibility that the student would be the only person that the patient consulted with. Having regular ‘debriefs’ with the GP was felt by many students and most GPs to partially ameliorate the risk taken by students.
I suppose there was more thorough presenting of the case than for the face-to-face consults.
(UCL Student 6)
In contrast, a small number of students reported that remote consulting felt less pressurised, with the telephone providing a barrier, and the option of ‘calling back’ if necessary. One GP agreed with this sentiment.
The final aspect of safety involved the supervisory risk to GP tutors. Most GPs had apprehensions about supervising students who were consulting remotely, including: not witnessing all conversations between patient and student, not reviewing all patients, and having to juggle clinical work with teaching.
I was also juggling my own clinical work …which is like a massive learning curve for me because I've never done any online work before.
(UCL GP 1)
It was harder…I didn’t really have a good feel for the patient…what I find with students is they present everything… part of it is sort of being able to unpick what’s relevant and what’s not.
(UCL GP 4)
Triage of undifferentiated patients
Undifferentiated patients are those with multiple or unclear symptoms, or who do not have a diagnosis. It was interesting to explore how the care of such patients was organised by practices when utilising student-led remote consulting.
Almost always, patients were pre-selected for a student-led consultation, either by the reception staff or the GP. Selection criteria typically included: low complexity, varied pathology and patients who ultimately might require examination. One GP tutor first selected low complexity patients (e.g. sore throats) then gradually increased the level of complexity (e.g. patients with both medical and social problems).
In the first couple of weeks…. I keep it really simple so UTIs, sore throats, eczema. As they approach the last week I ….make it a little bit more complex.
(QMUL GP 3)
Pre-selection of patients for student consultations was generally endorsed by students. One commented that it was ‘a waste of time’ for him to start a case, then defer it to the GP because of its complexity. Another student said she felt less confident when the symptoms were not clear, or when the patient had not been ‘properly triaged.’ Student-reported advantages of pre-selection included: less complex cases offering more autonomy, and more complex cases as being less manageable over the phone. Overall, there was a student preference for consulting with lower complexity patients. This seemed to relate to a feeling that managing more complex patients was beyond their skill-set.
The majority of GPs also supported pre-selection, citing the importance of being able to select patients who required examination, were interesting, relevant to the subject being studied, varied, not overly complex, not ‘follow-up consultations’ and willing to speak to students. One GP reported that by pre-selecting patients, he could discuss the patient with the student first, which aided learning.
Only one GP tutor questioned the value of pre-selection of patients, highlighting the potential negative implications for learning if complex patients were ‘selected out’:
I think that’s the…disadvantage of….telephone calls consultations….not being able to appreciate…the actual complexity of a patient’s health problem.
(QMUL Student 1)
Patient inclusion in student education
Patient participation was reported as unchanged, if not improved, through inclusion of remote interaction, a sentiment expressed by GPs and students alike. Participants reported that only a minority of patients did not wish to speak to students and wanted to speak to the GP directly. Students discussed that having time in consultations enhanced the student–patient connection. They also felt that undertaking more consultations positively impacted upon the quality of those consultations due to improved history-taking skills.
Concerns were raised by both GPs, as well as a small number of students, that remote consulting disadvantages certain groups of patients, such as those with hearing impairments, mental health conditions, learning difficulties, complex co-morbidities, non-English speakers, and those with poor computer literacy. Parker’s (Citation2021) exploration of inequalities in remote consultations corroborates these concerns. This exclusion of certain patient groups was felt to be an ethical issue, but also restrictive in terms of student learning.
However, remote interactions were also reported to create opportunities for patient consultations, which might not have been possible face-to-face e.g. patients with physical disabilities or poor mobility, or working adults. Several GPs and a minority of students highlighted the potential for the inclusion of a wider variety of patients remotely.
Note that the potential for both greater inclusion of some patients, and increased exclusion of others, was often acknowledged by the same participant.
I guess just that you can involve…, patients that work or perhaps couldn’t come in but might be able to do something on the phone.
(Newcastle GP 4)
Student–patient interaction
Building rapport was a reported challenge to remote consulting (and strategies to support this additional learning need are made in the discussion section). GPs and students alike both discussed this, identifying the lack of human connection and loss of subtle non-verbal cues as the main contributory factors. One GP feared that this challenge was greater for students, who often did not know the patients.
Furthermore, this loss of human connection had an impact on students’ perceptions of general practice as a career, with many stating that it made general practice a less desirable choice. One student spoke about the ‘relationships’ being what makes GP special and that being lost remotely. Another referred to general practice as a ‘glorified NHS 111.’ Given that primary care is often the environment in which cultivating doctor–patient relationships and providing patient-centred care is learned, this perception must be reflected on.
I think it’s sad ….they’ve lost that luxury of chatting to patients and making the connections and learning about their lives.
(Newcastle GP 2)
Student–doctor interaction
There were many positive references to a ‘debrief’ between student and doctor. Students found debriefs useful, and nearly all students and GPs reported that these occurred more frequently when remote consulting was used. Remote consulting appeared to require greater trust and better communication between GPs and students.
GP availability to the student was seen as essential by both GPs and students, and all GPs acknowledged the importance of being available to students. Several students believed that remote consulting increased GP availability to them. However, ‘offsite’ students were much more likely to report problems with GP accessibility. Some GPs, in turn, discussed the difficulties that they had experienced when supervising offsite students.
There were frequent student references to the importance of ‘being useful to the GP’. Some GPs affirmed that their students had been helpful, working almost as ‘GP assistants.’ There appeared to be a correlation between the seniority of the student, and their usefulness to the GP.
Discussion
Our study revealed nine themes related to student-led remote consultations in primary care. It is apparent that remote consulting offers unique educational benefits, allowing more student participation, developing history-taking and clinical reasoning skills.
There was a wide variation in how teaching sessions utilising remote consulting were conducted, aligning with the findings of Darnton et al. (Citation2021). We would celebrate this variation in practice and teaching methodologies as being reflective of a speciality in which every patient’s consulting needs are different.
Concern was raised in the literature about whether students consulted with enough patients during the Covid-19 pandemic. Yet, we found that students undertook more consultations. In addition, students were exposed to a wider variety of presentations; although there were concerns about the potential exclusion of some patient groups, validated by Parker et al. (Citation2021).
It was harder to build rapport with patients remotely. However, the fact that the students had longer consultations positively impacted the student–patient relationship. Manninen et al. (Citation2014) examined the role of patients in medical student education, concluding that good relationships between students and patients resulted in better learning experiences. It is essential to invest in the student–patient relationship, in recognition of (a) how fundamental this is to learning and (b) the challenges in building rapport remotely.
Remote consulting positively impacted upon the student–doctor relationship. Debriefs between doctor and student occurred frequently, aligning with Al-Bedaery et al. (Citation2021) findings.
The theme of safety emerged: a novel finding in this study. It was felt by students and GPs that more clinical risk was present when consulting remotely, and that this risk was higher for students. Edmondson’s (Citation2016) work concluded that psychological safety, a shared belief held by members of a team that the team is safe for risk taking, was a prerequisite for learning. The additional clinical risk posed by remote consulting may negatively impact the psychological safety of students. Our work showed that frequent contact between student and GP reduced the perceived risk.
Most participants felt that remote consulting allowed more student autonomy, but in accordance with Darnton (Citation2021) and Al-Bedaery (Citation2021), this depended on how the sessions were run. Observing GPs undertaking remote consults had little educational value unless part of a programme of increasing participation. Lave and Wegners' (Citation1991) ‘Community of Practice Theory’ postulates that students are peripheral members of a community of practice, assuming progressively greater responsibility for patient care. Our findings align with this theory, and the work of Park et al. (Citation2015), who identified participation as crucial to primary care medical education.
Pre-selection of (often lower complexity) patients for student consultations was commonplace. Darnton et al. (Citation2021) discussed that pre-selection of patients was necessary for deriving maximal educational benefit. However, we argue that the advantages of pre-selecting lower-complexity patients need to be balanced against nurturing students’ ability to manage complex, undifferentiated patients. It is exposure to complexity that allows the development of ‘expert generalism’ – the ability to understand the needs of patients with complex, multifactorial bio-psycho-social problems.
Clinical reasoning was felt to be as effectively learned, if not more so, from remote consulting, as students were learning to recognise when a face-to-face consult is necessary. By verbally assessing a patient, and selecting next steps, GPs employ higher order reasoning skills in Bloom’s taxonomy (Bloom 1956, in Anderson and Krathwohl Citation2001). GPs should verbalise their thought-process when remotely assessing patients, to make their reasoning apparent to students, and help students develop these skills. This requires dedicated teaching as it is more challenging than undertaking face-to-face consultations alone. The building up of this ‘judgement knowledge’ will become increasingly important in future with hybrid working.
To achieve this, we must legitimise remote consulting as a teaching modality. This may require reform of the curriculum and assessments, to reflect the hybrid nature of clinical practice. Assessment drives learning (Wormald Citation2009), so it is vital that assessments align to real-life practice.
Participants recognised the importance of learning how to consult using both modalities, as remote consulting was likely to remain. Both students and GPs wanted more training, including: guidance on remote consulting practicalities, direction on the university’s expectations for students consulting remotely, and advice about the balance of face-to-face versus remote consulting. Students also wanted more teaching on: telephone etiquette, differences between in-person and telephone consults, emerging technology, and telephone triage. Pit et al. (Citation2021) concluded that ‘embedding telehealth skills training into the medical training. is essential to prepare the future workforce’ (p. 2)
Recommendations
We have developed a list of practical recommendations for educators to consider when incorporating remote consulting into undergraduate primary care education ().
Table 2. Recommendations for clinician tutors and medical schools.
Our research has highlighted areas that need further exploration to improve the use of remote consulting in general practice education. These include whether the use of remote consults influences career choice and why, and exploration of patient perspective of student-led remote consultations.
Limitations
Responder bias may have been introduced into this study, as participants who consented to being interviewed were more likely to hold polarised views (Adams Citation2015). This study was commenced in 2021 and data collection was undertaken over a 12-month period. Hence, the views and experiences of the interviewees were likely to have evolved throughout the course of the study.
Conclusion
GP tutors and students felt that both remote and face-to-face consulting were important. Remote consulting was viewed as a distinctive skill and earlier exposure to it was seen as beneficial. Remote consulting confers specific educational benefits, especially increased student autonomy, and improved history-taking skills, and communication. However, there are factors which need to be supported in order to achieve meaningful remote learning and patient interactions.
Supplemental Material
Download MS Word (17.1 KB)Acknowledgements
The authors thank all participating GP tutors and medical students from all institutions for their contribution. This paper and the research behind it would not have been possible without them. The authors are grateful to Madiha Sajid, who provided advice and guidance from her perspective as a Public Contributor.
Disclosure statement
No potential conflict of interest was reported by the author(s). The authors alone are responsible for the content and writing of the article.
Additional information
Funding
Notes on contributors
Sarah Armstrong
Dr Sarah Armstrong, MRCGP, Primary Care Population Health Department, University College London. She has expertise in remote primary care medical education, PPI in primary care education, alongside experience as a GP.
Hugh Alberti
Professor Hugh Alberti, Masters in Clinical Education, Sub dean for primary and community care, School of Medical Education, Newcastle University. He has expertise in the areas of patient involvement in undergraduate teaching and influences on GP career choice of students. Other multicentre work includes projects on GP motivations to teach and GP trainees barriers to teaching. Experience as a GP.
Abhishek Bhattacharya
Dr Abhishek Bhattacharya, MRCGP, Primary Care Population Health Department, University College London. Salaried portfolio innovation scheme GP. His interests include medical education and experience as a GP.
Bhavit Dhokia
Bhavit Dhokia, medical student at Queen Mary University of London.
Lauren Hall
Dr Lauren Hall, MBBS, School of Medical Education, Newcastle University. Academic Foundation Doctor. Her research interests include undergraduate primary care medical education.
Sadie Lawes-Wickwar
Dr Sadie Lawes-Wickwar, PhD, Health Psychologist, Lecturer in Medical Education and Deputy Director Medical Education, Primary Care Population Health Department, University College London. She has expertise in investigating the impact and management of long-term conditions, person-centred health care, and evaluating community-based public health interventions.
Eitan Lovat
Dr Eitan Lovat, MBBS, Academic Foundation Doctor, Primary Care Population Health Department, University College London. He is interested in undergraduate medical education.
Shraya Pandya
Shraya Pandya, medical student at Queen Mary University of London.
Sophie Park
Professor Sophie Park, Doctor of Education, Professor of Primary Care Medical Education, Primary Care Population Health Department, University College London. She has expertise in primary care medical education, patient and public involvement (PPI) in primary care education, alongside experience as a GP.
Lindsey Pope
Professor Lindsey Pope, Doctorate in Health Professions Education, GP and Director of Community Based Medical Education, School of Medicine, Dentistry and Nursing. University of Glasgow. She is Co-Director of the Scottish School of Primary Care and the Specialty Adviser for General Practice to the CMO for Scotland. Research interests include: Utilisation of Activity Theory to understand teaching and learning in general practice, GP careers, Doctors’ well-being and Assessment of professionalism.
Madiha Sajid
Madiha Sajid, Masters Education and International Development, Public Contributor, experience as a PPI contributor for research projects, including a project on remote primary care education, personal experience as a patient and carer of a relative, and experience working in student learning and support, including on working groups for equality, diversity, and inclusion in academia. ORCHID: 0000-0001-6294-2595
Penny Wilson
Dr Penny Wilson, Masters in Medical Education, GP Research Fellow, School of Medical Education, Newcastle University. Her research interests include primary care medical education, widening participation.
Louise Younie
Dr Louise Younie, Doctor of Education, Institute of Health Sciences Education, Queen Mary University of London (QMUL). She has expertise in person-centred medical education, qualitative enquiry in medical education, and experience as a GP.
References
- Adams WC. 2015. Conducting semi-structured interviews. In: Newcomer K, Hatry H, Wholey J, editors. Handbook of practical program evaluation. 4th ed. John Wiley and Sons; p. 492–505. DOI:10.1002/9781119171386.
- Al-Bedaery R, Chaudhry U, Ahmed R, Jones M, Noble L, Ibison J. 2021. Undergraduate medical teaching with remote consultations in general practice: realist evaluation. BJGP Open. DOI:10.3399/BJGPO.2021.0185.
- Anderson LW ,Krathwohl DR. 2001. A taxonomy for learning, teaching, and assessing: a revision of Bloom’s taxonomy of educational objectives. New York, NY: Longman.
- Braun V, Clarke V. 2006. Using thematic analysis in psychology. Qual Res Psychol. 3(2):77–101.
- Bunniss S, Kelly D. 2010. Research paradigms in medical education. Med Educ. 44(4):358–366.
- Darnton R, Khan M, Tan X, Jenkins M 2021. Primary care placements in the post-COVID era: a qualitative evaluation of a final year undergraduate clerkship. Med Teach. 44(3):319–327.
- Darnton R, Lopez T, Anil M, Ferdinand J, Jenkins M. 2021. Medical students consulting from home: a qualitative evaluation of a tool for maintaining student exposure to patients during lockdown. Med Teach. 43(2):160–167.
- Donaghy E, Atherton H, Hammersley V, McNeilly H, Bikker A, Robbins L, Campbell J, McKinstry B. 2019. Acceptability, benefits, and challenges of video consulting: a qualitative study in primary care. Br J Gen Pract. 69(686):586–594.
- Edmondson A, Higgins M, Singer S, Weiner J. 2016. Understanding psychological safety in health care and education organizations: a comparative perspective. Res Hum Dev. 13(1):65–83.
- Lave J, Wenger E. 1991. Situated learning: legitimate peripheral participation. Cambridge: Cambridge University Press.
- Manninen K, Welin Henriksson E, Scheja M, Silen C. 2014. Patients’ approaches to students’ learning at a clinical education ward-an ethnographic study. BMC Med Educ. 14(131):131.
- McKinstry B, Watson P, Pinnock H, Heaney D, Sheikh A. 2009. Telephone consulting in primary care: a triangulated qualitative study of patients and providers. Br J Gen Pract. 59(563):209–218.
- Misselbrook D. 2021. General practice after COVID-19: an introduction to our special series. Br J Gen Pract. 71(707):265.
- Park S, Khan N, Hampshire M, Knox R, Malpass A, Thomas J, Anagnostelis B, Newman M, Bower P, Rosenthal J, et al. 2015. A BEME systematic review of UK undergraduate medical education in the general practice setting: BEME Guide No. 32. Med Teach. 37(7):611–630.
- Parker R, Figures E, Paddison C, Matheson J, Blane D, Ford J. 2021. Inequalities in general practice remote consultations: a systematic review. BJGP Open. DOI:10.3399/BJGPO.2021.0040.
- Pit S, Velovski S, Cockrell K, Bailey J. 2021. A qualitative exploration of medical students’ placement experiences with telehealth during COVID-19 and recommendations to prepare our future medical workforce. BMC Med Educ. 21(1):431.
- QSR International Pty Ltd. 2020. NVivo software. https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- RCGP. 2021. The future role of remote consultations & patient ‘triage’. General practice COVID-19 recovery. https://www.rcgp.org.uk/getmedia/72f052b6-3227-48b4-87c9-b05ff90517c4/future-role-of-remote-consultations-patient-triage.pdf
- Turner A, Scott A, Horwood J, Salisbury C, Denholm R, Scott L, Iyer G, Macleod J, Murphy M. 2021. Maintaining face-to-face contact during the COVID-19 pandemic: a longitudinal qualitative investigation in UK primary care. BJGP Open. DOI:10.3399/BJGPO.2021.0036.
- Wormald B, Schoeman S, Somasunderam A, Penn M. 2009. Assessment drives learning: an unavoidable truth? Anat Sci Educ. 2(5):199–204.