ABSTRACT
Background
In the context of aphasia rehabilitation, there is a perceived need for interventions with a reduced linguistic demand targeting well-being. Mind-body and creative arts approaches are holistic and person-centred approaches, primarily relying on means other than verbal exchanges and promoting self-regulation strategies.
Aims
This mixed-method systematic review aimed to evaluate the availability, feasibility and effectiveness of mind-body and creative arts therapies in promoting well-being for people with aphasia. Eight databases were searched using subject headings and keywords. Full-text screening, critical appraisal and data extraction were conducted independently by two reviewers. A segregated synthesis approach was used (i.e., Revised Effect Direction Plot technique and Thematic Synthesis approach). Findings are presented in a narrative and visual form.
Main Contribution
Twenty-two studies were included (Mind-body: n = 11; Creative arts: n = 11). Heterogeneity of study design and quality, intervention type, procedures and dosage, outcomes, and level of offered communication support were identified. Improvements were noted across a wide range of well-being outcomes with more consistent positive results for anxiety and communication. One hundred and twenty-eight findings were extracted and synthesised in three broad themes: positive impact on self, empowering multifaceted experience, and relevance of needs-centred adjustments.
Conclusion
Provisional findings about the benefits of mind-body and creative arts interventions on aspects of well-being for some individuals with aphasia were identified. However, findings are complex and need to be interpreted cautiously. Facilitators and barriers to these therapies are highlighted with related recommendations for practice. This review poses a demand for further research in the field, implementing rigorous methodology and aphasia-specific support to facilitate inclusion and engagement.
Introduction
At least 250,000 people in the UK live with aphasia. Aphasia frequently has a severe impact on the everyday life of the individuals affected and their families. People with aphasia (pwa) often become reliant on others to communicate, with related changes in interpersonal relationships, social roles and participation to work and leisure activities (Manning et al., Citation2019). The loss of autonomy and the increased cognitive demand on everyday tasks can lead pwa to develop negative feelings, such as low mood, irritation, distress, alienation, low self-esteem and vulnerability (Shiggins et al., Citation2020). Aphasia appears to be a significant risk factor for both post-stroke depression, reported for 70% of pwa in the first three months post-stroke, and anxiety, observed in 20–25% of people with a left hemisphere stroke after the first six months (De Wit et al., Citation2008; Barker-Collo et al., 2007). Post-stroke depression has been associated with poor rehabilitation and quality of life (QoL) outcomes with correlated difficulties in clinical recovery, therapy engagement and return to life (Robinson, Citation2006). Depression and anxiety might also affect both cognitive processing (Eysenck et al., Citation2007) with negative consequences on the already impaired language output (Knapp et al., Citation2017) and social relationships (Code et al., Citation1999) with an exacerbation of social isolation and negative feelings. This enhances the importance of therapy programmes for pwa addressing emotional difficulties (Cruice et al., Citation2011).
Contemporary psychotherapy largely relies on verbal exchanges (*Yeates, Citation2019). Aphasia might prevent the affected individuals from expressing their emotions, receiving accurate diagnoses of mood disorders (*Dickinson et al., Citation2017), and being offered accessible mental health services (Simmons‐Mackie & Damico, Citation2007) with negative effects on the amount and quality of psychological support pwa can access. There is, therefore, an urgent demand for person-centred approaches that rely less on communication and can promote well-being (*Yeates, Citation2019). Well-being therapies are by nature less reliant on communication as these usually implement a holistic approach targeting not a specific need or skill but the individual as a whole (Simmons‐Mackie & Damico, Citation2007). As highlighted by the Living with Aphasia: Framework for Outcome Measurement, A-FROM (Kagan et al., Citation2008), an individual’s QoL is indeed not determined by a single factor (e.g., aphasia severity) but by the continuous interaction of several life domains (i.e., aphasia severity, life participation, linguistic environment, and personal factors). Holistic approaches encompass self-regulation strategies and value person-centred care and might represent a tool to empower pwa to become independent in dealing with their emotional conditions in everyday life (De Silva, Citation2011).
In regard to this, mind-body and creational arts approaches can be considered holistic and person-centred approaches, primarily relying on other means than the verbal medium and focusing on behavioural exercises or on art-based activities to promote mind-body connection and well-being. These usually group-based approaches impart self-regulation strategies and might empower individuals to play an active role in managing their mental health (Kapitan, Citation2012). They are potentially cost-effective, non-invasive, and straightforward to implement in clinical practice and in the home setting therapies (Wahbeh et al., Citation2008) and have been shown to have some positive effects in promoting social participation and alleviating mood disorders amongst stroke patients (Ali et al., Citation2014). However, for results to be considered reliable and applicable, single study findings need to be replicated across several participants and contexts (Petticrew & Roberts, Citation2008). To explore the evidence and improve understanding of mind-body and creative arts therapies in promoting well-being for pwa, a comprehensive, rigorous, and transparent investigation of the literature was conducted.
Aim
Grounded in the FAME (Feasibility, Appropriateness, Meaningfulness, and Effectiveness) framework (Pearson et al., Citation2015), this systematic review aims to evaluate the availability, feasibility, and effectiveness of mind-body and creative arts therapies to promote well-being for pwa. The objectives are
To identify interventions that use mind-body and/or creative arts;
To explore feasibility, in terms of accessibility, appropriateness, and meaningfulness of the identified interventions for pwa;
To determine effectiveness of the identified interventions in improving global well-being and/or aspects of well-being for pwa.
Methods
The review was conducted as described in a protocol registered in PROSPERO (International prospective register of systematic reviews; CRD42020197876), and it is reported according to PRISMA guidelines (Page et al., Citation2021b). The review was conducted in five stages: literature search, study selection, data extraction, quality assessment, and data analysis.
Design
To address the review objectives, a mixed-method systematic review methodology was implemented. Mixed-methods promoted the collection of a broad data set, a comprehensive understanding of the intervention effects from different perspectives, and the validation of findings by comparing and contrasting quantitative and qualitative data through triangulation techniques (Creswell & Creswell, Citation2017; Hong et al., Citation2017).
Selection criteria
The SPIO (Study design, Population, Interventions, and Outcomes) framework, targeting the key components of the research study, was used to determine the selection criteria ().
Table 1. SPIO inclusion/exclusion criteria
SPIO is an adaptation of the Population, Interventions, Comparison, and Outcomes framework (Bettany-Saltikov, Citation2012) that has already been applied to define systematic review selection criteria in stroke research (e.g., Lawrence et al., Citation2013).
Population: adults (≥18 years old) with acquired aphasia or mixed populations where the aphasia-only data can be extracted. Interventions: a mind-body or a creative arts intervention. In the context of this review, “mind-body therapies” were intended as approaches implementing different types of behavioural exercises to promote the connection between mind and body with the aim of enhancing health and well-being (Love et al., Citation2019). Creative arts interventions were defined as therapeutic approaches using art-based activities and the creative process to facilitate self-expression (Puig et al., Citation2006). Any intervention procedures, duration, and intensity were included, as far as data about the review-relevant intervention could be extracted.
This review excluded the following: interventions not developed as holistic mind-body and/or creative arts therapies and interventions with review with different primary target outcomes such as interventions including selected elements derived from mind-body and/or creative arts therapies used to target outcomes that deviate from the primary scope of this review. To take an example, Melodic Intonation Therapy interventions use musical elements specifically to improve speech function and therefore do not align with the review purpose. Study design: all study designs have been included (quantitative, qualitative, and mixed-method). Outcomes: any outcome measuring global well-being and/or aspects of well-being (e.g., well-being, mood, confidence, social participation, Quality of Life (QoL), communication, cognition, and fatigue).
Search methods
Scoping searches were conducted in a systematic review repository (i.e., PROSPERO) to identify systematic reviews in the field and in two bibliographic databases to refine the search terms (i.e., MEDLINE and PsycInfo). Search strings were developed combining subject headings and keywords targeting the Population and Intervention parameters of the SPIO framework through Booleans operators (Box 1). The pool of keywords was expanded by identifying concepts and synonyms through a mind map process. A filter (i.e., tTitle and abstract only) was applied to the search in databases where an excessive number of irrelevant sources were retrieved (e.g., PsycArticles).
No delimiters were applied to the search. Selecting a starting date for the search could have led to the exclusion of relevant studies as mind-body therapies derived from traditions originated from oriental healing practices. Language restriction was not applied for this search as the main reviewer had access to speakers of a wide range of languages who could assist with translation.
In April 2020, the finalised search was run in seven databases, i.e., Allied and Complementary Medicine Database, Cumulative Index to Nursing and Allied Health Literature, MEDLINE, PsycInfo, PsycArticles, Linguistics and Language Behavior abstract, and PubMed Central. To identify any additional published and/or unpublished studies, ProQuest Dissertations & Theses Database, Science Citation Index, International Clinical Trials Registry Platform, Applied Social Sciences Index, and Abstracts were searched; aphasia and mind-body/creative arts research studies were contacted through professional organisation websites, and reference lists of relevant systematic reviews and identified papers were screened. The authors were contacted if the full paper could not be fully accessed online and/or when additional information was necessary to determine eligibility (e.g., extracted data).
Study selection
Titles and abstracts of all identified studies were screened by two reviewers (MP and HF). Studies were coded as follows: “included”, “excluded”, and “undecided”. Where inclusion was uncertain, the reviewer erred on the side of inclusion. Full text of “included” and “undecided” papers was independently reviewed by two of the authors (MP and HF) to identify eligible studies. Any potential disagreement was resolved through discussion with a third reviewer (ML), when necessary. As part of the selection process, it was decided to exclude observational studies as they often did not apply scientifically rigorous procedures, as well as unpublished studies, which did not report information systematically.
Data extraction
To ensure rigour and systematicity, data in terms of population, study design and methods, interventions, and outcomes were extracted using a bespoke tool based on the domains of the Template for Intervention Description and Replication (TIDieR) checklist (Hoffmann et al., Citation2014). The second reviewer (HF) independently extracted data for 50% of the included studies.
Quality appraisal
Standardised design-specific quality appraisal checklists were used to categorise each study and assess its quality. The following tools were used: the Single-Case Experimental Design-SCED Scale (Tate et al., Citation2008) for studies up to 10 participants (Graham et al., Citation2012), the Joanna Briggs Institute Critical Appraisal Checklist for Quasi-Experimental Studies (Tufanaru et al., Citation2017), the Critical Appraisal Skills Programme (CASP) Randomised Controlled Trial Checklist, and the CASP Qualitative Checklist (CASP Checklists, Citation2020). Single-case studies using qualitative methods were appraised using the CASP Qualitative Checklist as questions seemed more appropriate than those of the SCED Scale. The reviewer then classified the studies as follows: “poor” studies with a score <5; “medium” studies with a score between 5 and 8, and “high” studies with scores ≥8. The second reviewer independently assessed the quality of 50% of the included studies.
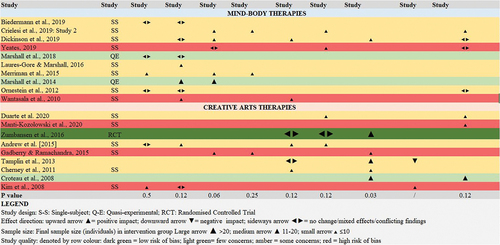
Synthesis of results
A segregated synthesis was conducted where quantitative and qualitative studies were analysed in two distinct syntheses (Sandelowski et al., Citation2006). To analyse quantitative studies, a revised Effect Direction Plot was used. This technique enables exploring the effectiveness of interventions based on evidence about outcome improvement, deterioration, or no change (Boon & Thomson, Citation2021). Effect Direction Plots have been shown to be appropriate to synthesise effect measures for systematic reviews including non-randomized studies and several sources of evidence, where meta-analysis cannot be performed and effect sizes are not available for all the studies (Boon & Thomson, Citation2021, please refer to this paper for the full procedure). Data were visually represented in a table (). The non-parametric sign test was used to provide statistical evidence for the effect direction synthesis.
Qualitative findings from the included studies were synthesised using thematic synthesis. Specifically, a three-stage process was used to analyse and combine secondary qualitative data: line-by-line coding of findings of primary studies, the organisation of codes into “descriptive themes”, and the development of “analytical themes”. This approach enables reviewers to preserve the findings from the primary studies and integrate these by transparently generating novel constructs within a specific research context (Thomas & Harden, Citation2008).
Results
Search outcomes
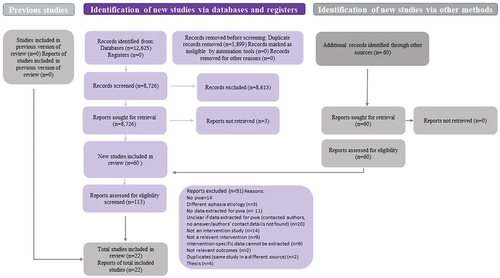
Out of 8,726 unique bibliographic records, 113 studies were selected for full-text screening, and of these, 22 studies were found to be eligible for the review (). Reasons for the remaining 91 records are reported in the chart. Two records were irretrievable as these were only available as paper copies at the British Library, which was closed due to Covid-19 restrictions at the time of full-text screening (July 2020).
Figure 1. Flowchart showing the review data selection process adapted from the PRISMA 2020 flow diagram template for systematic reviews (adapted from Page et al., Citation2021a).
Study characteristics
Publication years of the included studies range from 2008 to 2020. Seven studies were conducted in the USA, five studies in the UK, three in Australia, two in Canada, one in Brazil, one in Italy, one in Korea, and one in New Zealand. The study location for one study is not specified ().
Study designs
In relation to the methods used, thirteen studies used mixed methods (*Duarte et al., Citation2020; *Mantie-Kozlowski et al., Citation2020; *Biedermann et al., Citation2019; *Crielesi et al., Citation2019: Study 2; *Dickinson et al., Citation2017; *Yeates, Citation2019; *Andrew (Citation2015); *Gadberry and Ramachandra (Citation2015); *Merriman et al. (Citation2015); *Tamplin et al. (Citation2013); *Orenstein et al. (Citation2012); *Cherney et al. (Citation2011); *Croteau et al. (Citation2008)), six quantitative (*Kim et al., Citation2008; *Laures-Gore & Marshall, Citation2016; *Marshall et al., Citation2014, Citation2018; *Wantsala et al., Citation2010; *Zumbansen et al., Citation2017), and three qualitative studies (*Castka et al., Citation2009; *Mantie-Kozlowski et al., Citation2018; *Panda et al., Citation2020).
Participant characteristics
Across the twenty-two studies, 134 participants were included: 119 people with aphasia, 9 stroke survivors with no aphasia, and 17 significant others. Participants with aphasia presented with a range of aphasia types and severities, where the information was specified, type of aphasia included fluent (n = 36), to nonfluent (n = 30) and mixed (n = 30). Based on the information provided, stroke was the most common cause of aphasia (n = 17), followed by unspecified left-hemisphere brain damage (n = 3), gunshot (n = 1), brain tumour (n = 1), surgical removal of neoplasm (n = 1), and Primary Progressive Aphasia (PPA) (n = 1). The age of participants with aphasia ranged between 19 years and 82 years. Sixty-four participants were male (47.7%), and 39 were female (29.1%); gender of 31 was not reported (23.1%). Poor reporting of some population characteristics (i.e., ethnicity, educational level, marital status, living status, and aphasia severity) was found across several studies.
Intervention characteristics
Eleven studies were classified as mind-body interventions, and eleven studies were classified as creative arts interventions (). All the interventions were delivered face-to-face: Fifteen were delivered in groups and seven in one-to-one sessions. Regarding session duration and frequency, a high degree of variation was found across the studies ().
Table 2. Characteristics of included interventions.
Outcomes
Twenty outcomes related to well-being were identified. Attention, language, and mood were the most common outcomes measured in relation to mind-body interventions for pwa, whereas the most common outcomes measured in relation to creative arts therapies for pwa were QoL, mood, language, communication, social participation, and cognition. Participants were tested before and immediately after the intervention; however, most studies (n = 18) did not report any long-term follow-up measures. Sixty-two different outcome measures related to well-being aspects were used across the studies (); researchers’ observations were also used.
Table 3. Summary of measures used for each well-being-related outcome identified.
Feasibility
Although originally healthcare evidence-based practice sought to investigate findings in relation to intervention effectiveness, there is now a growing attention on simultaneously exploring end users’ needs and perceptions (Pearson et al., Citation2015). Complex interventions embody multiple interrelated components (Craig et al., Citation2008), and it is, therefore, of paramount importance not to focus solely on effectiveness but to take these aspects into account while evaluating an intervention.
Specifically, one feasibility study was identified (*Mantie-Kozlowski et al., Citation2018); six mind-body interventions and three creative-arts interventions explored some components of intervention feasibility. Nineteen out of twenty-two mind-body interventions implemented strategies to support pwa’s engagement with the interventions. In *Marshall et al. (Citation2018), an SLT developed an aphasic-specific mindfulness programme. Seven studies applied some modifications to the course programme and/or materials, e.g., reduced duration and content (*Panda et al., Citation2020; *Crielesi et al., Citation2019: Study 2; *Marshall et al., Citation2018; *Laures-Gore & Marshall, Citation2016); same structure pattern for each session (*Panda et al., Citation2020); aphasia-specific changes to musical score and choreography (*Castka et al., Citation2009); modifications to song writing technique (*Mantie-Kozlowski et al., Citation2020), adjustments to warm-up exercises, lyrics, and music (*Tamplin et al., Citation2013); enlarged font size; and single-page materials (*Mantie-Kozlowski et al., Citation2018). Eight studies reported using simplified language and communication strategies to facilitate pwa’s communication (*Mantie-Kozlowski et al., Citation2020; *Yeates, Citation2019; *Crielesi et al., Citation2019: Study 2; *Dickinson et al., Citation2017; *Marshall et al., Citation2018; *Laures-Gore & Marshall, Citation2016; *Gadberry & Ramachandra, Citation2015; *Cherney et al., Citation2011). Four studies provided aphasia-friendly visual support (*Panda et al., Citation2020; *Marshall et al., Citation2018; *Andrew (Citation2015); *Castka et al., Citation2009) or visual and kinaesthetic teaching (*Yeates, Citation2019) to facilitate engagement with practices. In seven studies, a speech therapist or aphasiologist facilitated the session (*Andrew (Citation2015); *Cherney et al. (Citation2011, Citation2020, Citation2020, Citation2020); *Castka et al. (Citation2009); *Croteau et al. (Citation2008)) or provided training to the practitioner who delivered the session (*Dickinson et al., Citation2017). For the remaining six studies, aphasia-specific support was not reported (*Kim et al., Citation2008; *Marshall et al., Citation2014; *Orenstein et al., Citation2012; *Wantsala et al., Citation2010; *Yeates, Citation2019; *Zumbansen et al., Citation2017). Poor reporting of adjustments and strategies to promote inclusion of individuals with communication difficulties has been highlighted (Lawrence et al., Citation2016) and represents an issue for subsequent research and practice, as it prevents understanding of how meaningfully pwa were involved. Concerning meaningfulness, several participants described these therapies as a positive and enjoyable experience bringing enjoyment and satisfaction (e.g., *Biedermann et al., Citation2019; *Duarte et al., Citation2020). In terms of practicality, all interventions were community-based and activities were conducted in locations external to the home. Positive feedback was expressed regarding location accessibility and duration of one intervention (*Mantie-Kozlowski et al., Citation2018). Cost was not explored in any of the included studies.
Quality
Methodological quality was mixed, but most commonly of medium quality. Specifically, n = 3 studies were rated as being of high quality, n = 3 studies were rated as medium-high quality, n = 10 studies were of medium quality, and n = 6 studies were classified of being of poor quality. Common methodological weaknesses included small sample size, lack of control groups, lack or limited use of inter-rater reliability measures, and lack of follow-up. Nevertheless, as this review was exploratory in nature, no studies were excluded for having methodological limitations.
Effectiveness
A narrative summary of studies demonstrating the positive effect direction is reported, and results from the Revised Effect Direction Plot used to explore effectiveness are presented in .
As shown in , regarding mind-body therapies, a positive effect direction was found for language and anxiety outcomes in a study involving pwa in Unilateral Nostril Breathing sessions (*Marshall et al., Citation2014). However, no differences were found with the control group of stroke survivors with no aphasia, who also achieved higher scores on language tasks.
Regarding medium-quality studies, the single-subject study from *Crielesi et al. (Citation2019) showed a positive effect direction for anxiety, depression, QoL, and some well-being aspects (e.g., social participation, interpersonal relationships, and emotion management) for a small group of pwa involved in a Mindfulness-based course. A significantly reduced anxiety (p < .001) maintained at a 3-weeks follow-up was also observed along with positive changes in emotional state and improved communication for a person with aphasia engaging with a Mindfulness-based intervention (*Dickinson et al., Citation2017). Similarly, a reduction of anxiety and depression and some attention gains were found for a person with aphasia involved in a group Mindfulness-based programme (*Merriman et al., Citation2015) and small language output improvements recorded for an individual with aphasia engaging with a Mindfulness-based training (*Laures-Gore & Marshall, Citation2016). Improvements in language and mood were also reported for a person with aphasia involved in a Mindfulness-based programme (*Wantsala et al., Citation2010), and a positive effect direction for QoL was found for an individual with aphasia involved in Taiji classes (*Yeates, Citation2019), although these last two studies were found to have methodological weaknesses.
Regarding creative arts therapies, *Zumbansen et al.’s (Citation2016) RCT showed positive effect directions for communication for pwa involved in choir sessions and compared to groups of pwa either engaging with a drama course or receiving no intervention. Although statistically significant functional communication improvements (p = 0.04) were found for pwa engaging with a choral singing intervention, no difference was shown compared to the control group involved in drama classes. Significant gains in communication (p = 0.01) and significant others’ perceptions of pwa’s improved ability to engage in group conversations (p = 0.04) were also observed for pwa involved in a theatre intervention in comparison to the control group (*Croteau et al., Citation2008). Positive effect directions were also found in relation to some well-being aspects (e.g., social participation, interpersonal relationships, and personality). In the quasi-experimental study from *Tamplin et al. (Citation2013), increased confidence and small gains in communication were reported for pwa involved in a community choir. An increase in communication confidence was also observed for pwa involved in drama classes (*Cherney et al., Citation2011) with medium effect sizes found for some mood measures (i.e., mood-positive outcomes, d = 0.61). Positive effect directions for QoL and well-being aspects (i.e., improved confidence) were found for a single-subject study involving a person with aphasia in a clowning group (*Duarte et al., Citation2020). Gains in QoL, mood, and semantic information gathering were observed for pwa involved in an observational drawing course (*Andrew, Citation2015).
Although the following studies were rated of being of poor quality and might be subjected to bias, positive effect directions for anxiety and depression and communication were noticed for pwa after engagement with music therapy (*Gadberry & Ramachandra, Citation2015). Increased confidence was observed in a person with aphasia involved in a song writing activity (*Mantie-Kozlowski et al., Citation2020). Gains in attention and other cognitive skills (e.g., memory and drawing) were reported for one person with aphasia involved in an art therapy intervention (*Kim et al., Citation2008).
Themes
This section illustrates the qualitative data extracted from the included studies.
As shown in , 128 findings were extracted from the seventeen primary mixed-method and qualitative studies; findings were initially coded into four codes. Initial codes were reviewed for similarities and differences; novel codes were developed. The final set of codes were aggregated into 12 initial descriptive themes, which were then aggregated into 3 main themes in line with the key points of the review questions, i.e., effectiveness, relevance, and feasibility (; ). Each synthesised theme is illustrated below with verbatim quotes from the primary studies. There is a high incidence of citations from *Panda et al. (Citation2020) and *Tamplin et al. (Citation2013) as these studies reported several participants’ quotes covering a wide range of topics that allow an accurate representation of the qualitative findings from the included studies.
Figure 2. Revised effect direction plot for quantitative studies including sign test p-values for well-being outcomes, study design, and quality (adapted from Boon & Thomson, Citation2021) .
Positive impact on self
Engaging with mind-body or creative arts therapies was frequently described by participants as a beneficial experience that had a positive impact on self (e.g., *Crielesi et al., Citation2019: Study 2). Participants reported enjoying the course (e.g., *Mantie-Kozlowski et al., Citation2018), feeling relaxed, being calmer, and having fun (*Duarte et al., Citation2020).
When the meditation was introduced, I found that it did give me a calmness … Definitely very calm, yeah, yeah. It sets me up for the day (*Panda et al., Citation2020, p. 19)
I felt more at ease. Calmer, more at ease, I felt at ease (*Duarte et al., Citation2020, p. 10)
I had a lot of fun, I really liked it! (*Duarte et al., Citation2020, p. 10)
[Singing] makes me feel good. But more importantly it makes me feel good on behalf of the guys who can’t speak properly. I get more enjoyment seeing them succeed more than anything, but I do enjoy singing with them (*Tamplin et al., Citation2013, p. 937)
These activities were also reported as needed and useful.
I like to do this, I feel good. When I don’t come, I miss it (*Duarte et al., Citation2020, p. 9)
Boredom basically, erm, brilliant (gestures thumbs up). Going to this Tai Ji group. I like yoga, very similar, both I think great (*Yeates, Citation2019, p. 19)
[…] this is helping me bring the best out of me … I was in my own little shell. That shell has broken open now. It’s made me more confident, and I must admit I’m freer to talk to people (*Tamplin et al., Citation2013, p. 936)
Some authors stated that participants also reported the feeling of having learnt something new and useful (*Biedermann et al., Citation2019) and described these activities as meaningful and rewarding (*Duarte et al., Citation2020; *Mantie-Kozlowski et al., Citation2020). In addition to this, as previously reported, participants perceived improvements across several areas from communication, to mood, motivation, confidence, self-acceptance, sense of self, self-control, emotion management, and resilience.
Because I know I feel different now. Before I started this whole thing now I
used to be angry, now it’s all ssssssss [nullified] (*Panda et al., Citation2020, p. 18)
Well [the choir] has given me more courage to step out, its building my self esteem back … I tackle things better in that respect (*Tamplin et al., Citation2013, p. 936)
For me, it was quite definite. For me, when I had the stroke, my greatest fear was
having another stroke and I’m on my own. So I didn’t know if I had stroke what I
would do. But the meditation made me definitely, I know that, get over my fear. It was amazing. I just don’t think of it anymore (*Panda et al., Citation2020, p. 19)
I’m sure I’ve got bad thoughts somewhere, but they ain’t there now. It really is good.
The whole day is new, it’s different, I know I’m not getting a lot from the day because
of what’s going on, but for me it’s giving that grounding and then you can go off
through the day (*Panda et al., Citation2020, p. 19)
I feel like someone else (*Duarte et al., Citation2020, p. 10)
Empowering multifaceted experience
Participants recognised multiple meanings to these therapies. Of great importance, participants appreciated being involved in an activity that is not impairment-focused or related to stroke and/or aphasia, but that promotes a strength-based skill (*Biedermann et al., Citation2019). Taking part in a meditation group session was viewed by participants as not determined by their linguistic competence and not requiring verbal output (*Panda et al., Citation2020; *Yeates, Citation2019).
Moreover, by engaging with a non-stroke-related activity, a shift from stroke symptoms is promoted.
Well the thing is that each day I’m- I know I’m going like that [moves hands
upwards], I’m constantly going up. So you’re doing stroke and you’re only looking at
stroke not the other things (*Panda et al., Citation2020, p. 18)
Some individuals perceived that they were facilitated to acknowledge the progresses they were making in their recovery journey.
… I did some meditation last night … it’s great. And you know, that meant a lot to me, here’s somebody that’s sane- well- better and taking meditation and it’s working and I feel great (*Panda et al., Citation2020, p. 12).
Pwa also recognised these activities as an opportunity to learn a new skill and discover a talent (*Biedermann et al., Citation2019). Some individuals involved in meditation also reported starting to develop acceptance and resilience.
By accepting a situation, it gives you, I feel, the step up to “well here I am, where do I
go from here”, that’s what meditation, I feel, can do for a person (*Panda et al., Citation2020, p. 18).
At the same time, as will be presented in more detail below, the group environment created an opportunity for social engagement (*Panda et al., Citation2020; *Yeates, Citation2019).
Engaging in these activities also offered individuals a break from everyday life and from negative thoughts.
I think it’s important, instead of racing around – I tend to be racing around because
there’s a few things I need to know- to study- um that you get caught up in the hurlyburly. So it’s really nice just to be there and relax, yeah (*Panda et al., Citation2020, p. 13)
It makes me forget many things … many things … (*Duarte et al., Citation2020, p. 10)
[this activity is] giving yourself some breathing room (*Panda et al., Citation2020, p. 13)
For some participants, this protected time represented a time to establish a connection with nature or an act of spirituality similar to a prayer (*Panda et al., Citation2020).
The relevance of needs-centred adjustments
This theme encompasses the perceived facilitators and barriers participants experienced in relation to accessibility, an essential intervention component representing the first step for inclusion (Pearl & Cruice, Citation2017).
The group presence was reported as a very valuable component to the experience. Participants recognised the importance and benefits of sharing similar journey with other attenders and therefore a shared understanding of their experiences and interest in exploring copying strategies for negative feelings (*Crielesi et al., Citation2019: Study 2; *Merriman et al., Citation2015).
With helping each other, well- we’re all in the same- had strokes, um some
more fortunate or blessed than others, but we understand each other (*Panda et al., Citation2020, p. 16)
The group was a useful source of sense of belonging, mutual support, and boosted motivation (*Castka et al., Citation2009; *Tamplin et al., Citation2013)
I’m quite a social person, I enjoy that aspect of doing it as a group. And also, hearing
about the experiences of how the others were relating to the meditation (*Panda et al., Citation2020, p. 16)
We have a laugh […] you know the whole row is laughing because they’ve picked up on it and that’s the beauty of the choir … they’re close knit and understand one another and accept one another (*Tamplin et al., Citation2013, p. 936)
Some of the guys there with aphasia that I’m very close to, I feel that I need to help them get through it, you know … and it’s helping myself at the same time … it’s helping me share with the guys in the choir who have aphasia to help them lift their voices up too (*Tamplin et al., Citation2013, p. 936)
Initially he wasn’t all that keen to participate, he was doing a lot of listening but now he is really joining in and his voice is a lot stronger too. And I guess he is projecting a little more and feeling more comfortable about it, and he looks forward to going (*Tamplin et al., Citation2013, p. 937).
The group also represented an opportunity for social engagement and bonding, particularly important for people with aphasia who frequently experience isolation after their stroke (Nyström, Citation2006).
I feel really pleased when I see them and that’s the only thing, I’ve got these other
projects- I miss not seeing them you know. I always think of them (*Panda et al., Citation2020, p. 15)
They socialize out of choir as well. They get together at each other’s houses maybe once a month and call it “blokes with strokes” … They just have a few drinks and chat and bbq (*Tamplin et al., Citation2013, p. 936)
The group was also identified as a reason for continuing attendance.
Cause we get going because it’s the group and everybody … then we can sit down and experience. It’s really the group that keeps me here, you know (*Panda et al., Citation2020, p. 16)
Importance was also given to the meditation facilitator who can offer support and guidance promoting learning and active involvement.
I use the breath and I’m always thinking about you [referring to meditation
facilitator] at home - it’s a purpose. So, either she’s here or she’s not, but she’s putting me in the zone (*Panda et al., Citation2020, p. 11)
Some stroke survivors reported that including a partner might improve the experience and boost motivation for home practice (*Merriman et al., Citation2015); a slight preference for caregiver involvement was also found in *Mantie-Kozlowski et al.’s (Citation2018) but the authors hypothesised that this was related to desire to be in a larger group.
Two main aspects of successful learning of a new activity were identified: practice and time. Another important identified factor was that individuals have unique preferences for type and length of practices, and therefore, it would be important to consider this while planning the intervention in order to give participants flexibility to pick their favourite activity as this might have an influence on continued attendance and practice.
Concerning the barriers, some difficulties were reported in relation to some language tasks. The activity of filling in a diary to record positive activities proved to be challenging for four stroke survivors, who expressed a preference for audio-recording their thoughts or sharing these with the group (*Merriman et al., Citation2015). Another reported challenge was in relation to the activity of generating a lyric, and the participant expressed frustration due to her word-finding difficulties (*Mantie-Kozlowski et al., Citation2020). Moreover, three stroke survivors with hemiplegic arms reported finding engaging with a body scan exercise difficult as the practice was guided, referring to both arms simultaneously, and participants experienced different sensations in each arm (*Merriman et al., Citation2015). Moreover, long Mindfulness practices proved to be challenging for some participants due to attentional difficulties and fatigue. One participant also reported reduced motivation to practice at home (*Merriman et al., Citation2015). In addition to this, it was reported that starting a new activity can cause some distress (*Yeates, Citation2019) and that learning a new skill can be challenging.
I was very, very nervous. People I don’t know. It’s helped me, it’s a lot … I liked it and I still like it now (*Yeates, Citation2019, p. 19)
Specifically, the process of learning meditation was described by some participants as initially challenging (*Panda et al., Citation2020).
Really it was hard because early on, I did a lot of- I went to bed [makes snoring sound] (*Panda et al., Citation2020, p. 10)
[my mind] keeps wandering off, with football or cricket or anything, anything except what I’m supposed to be doing’ (*Panda et al., Citation2020, p. 10)
As previously mentioned, time and practice were considered essential to develop meditation skills (*Panda et al., Citation2020).
It took me easily six months (*Panda et al., Citation2020, p. 10) I mean now it’s good, but it’s taken two years (*Panda et al., Citation2020, p. 10)
For me? Oh it was gradual (*Panda et al., Citation2020, p. 11)
The thing is the repetition going in and eventually it just clicks (*Panda et al., Citation2020, p. 11)
Interestingly, some participants showed some resistance to the Mindfulness notions of “acceptance” and “non-striving”. They perceived these concepts as contrasting to the attitude they had to adopt through their recovery journey; not accepting their post-stroke abilities led them to develop the necessary motivation to progress in their rehabilitation process (*Merriman et al., Citation2015).
Discussion
This mixed-methods review aimed to identify interventions delivering mind-body or creative arts therapies for pwa and to explore their effectiveness in improving aspects of well-being, as well as their feasibility and meaningfulness. As a result, a wide range of intervention types, procedures, outcomes measured, as well as an inconsistent pattern of findings have been found. Specifically, twenty-two mind-body and creative arts therapies have been identified, delivering different types of intervention (Mindfulness-based (n = 8), meditation (n = 1), Taiji (n = 1), Unilateral Nostril Breathing (n = 1), art therapy (n = 1), drawing (n = 1), clowning (n = 1), drama (n = 1), theatre workshop (n = 1), musical (n = 1), music therapy (n = 1), choir-based groups (n = 3), and therapeutic song writing (n = 1)).
Improvements were noted across a wide range of well-being outcomes; anxiety and communication were the outcomes with more consistently positive results. These positive findings are consistent with the benefits in a wide range of well-being-related outcomes (e.g., stress, anxiety, depression, and QoL) identified in systematic reviews exploring the impact of Mindfulness-based interventions for stroke survivors (Lawrence et al., Citation2013), people with multiple sclerosis (Simpson et al., Citation2021), and individuals affected by long-term conditions and their caregivers (Parkinson et al., Citation2019).
However, similar to what has been reported in the previously mentioned reviews, improvements reported in this review were generally small, rarely statistically significant, and not always experienced by every participant. In the context of this review, the variability of participants’ responses within and across studies might be related to the inclusion of pwa with a heterogeneous language profile. Although this is often the case for studies involving pwa (Otal et al., Citation2015), people with different language abilities might experience a different level of engagement with the interventions that might consequently affect therapy response. Moreover, most of the included studies presented with methodological limitations. A majority of studies did not implement any control to mitigate bias or treatment fidelity measures to assess the reliability and replicability of the interventions. Most studies lacked long-term data collection, which impacts ability to assess intervention effects in the long term.
The heterogeneity of the methods used and the lack of methodological rigour and long-term data collection affect the insight into the reliability of findings.
Although no evidence of significant harm was found, some adverse effects were reported such as distress to being involved in a new activity and learning new skills (*Yeates, Citation2019), frustration with impairment-focused tasks (e.g., keeping a diary and body scan; *Merriman et al., Citation2015), and attentional difficulties and fatigue following the high cognitive demand of some lengthy activities (*Merriman et al., Citation2015; Lo et al., Citation2019). As highlighted by Baer et al. (Citation2019) in a review exploring mindfulness-based programmes, in these types of therapies, participants engage with several exercises entailing a complex interaction of cognition functions, emotions, and sensations and therefore, they might experience some challenges and discomfort. Although evidence of harm is usually low for these therapies, the occurrence of silent harm is not excluded, and this might be actually exacerbated for pwa as they might experience difficulties in expressing their distress or masking their issues.
This review shows that language, cognitive, and physical impairments can raise a barrier to participation in some activities and cause some distress. Acknowledging participants’ difficulties and/or concerns is essential to offer person-centred support and prevent negative experiences. Baer et al. (Citation2019) state that facilitators need to be aware of the intervention theoretical and empirical backgrounds, as well as of the potential challenges and related strategies to tackle these; participants’ suitability for a specific intervention needs to be carefully assessed; the key programme elements and related techniques and rationale have to be shared with the participants to promote the learning of new skills; participants need to be systematically monitored and any adverse event reported. This also highlights the importance of adjusting the interventions to the needs and preferences of the involved individuals (e.g., reduced session length) to promote their active engagement and prevent distress.
With regard to feasibility, this review shows that mind-body and creative arts interventions are easily implemented on a daily basis. Required resources were a safe, accessible, and quiet venue, an activity facilitator offering communication support and aphasia-friendly resources. However, it has to be acknowledged that time needs to be dedicated to plan in advanced session structure and devise aphasia-specific adjustments. These therapies appeared to be well-accepted by pwa who described the activities they were involved in as meaningful, valuable, rewarding, stimulating and empowering (e.g., *Mantie-Kozlowski et al., Citation2020).
Importantly, participants appreciated that these interventions were not impairment-focused but linked to social and leisure activities they might normally have engaged with prior to their stroke. Although stroke survivors stress the importance of having their needs recognised, they also express the desire to be involved in pre-stroke life activities (e.g., O’Sullivan & Chard, Citation2010). In the study by Lawrence et al. (Citation2013), family members of young stroke survivors reported stroke survivors’ goal to return to a certain level of pre-stroke life normality.
Additionally, these therapies were perceived as having multiple meanings and applications. These interventions offered an opportunity to learn something new (e.g., *Biedermann et al., Citation2019) and to acquire a self-management tool (*Panda et al., Citation2020). This confirms findings from a previous review showing that yoga and Mindfulness might be valuable post-stroke self-management practices (Lazaridou et al., Citation2013). Research shows that Mindfulness-based interventions are beneficial to facilitate self-management of anxiety and depression for individuals affected by different clinical disorders such as stroke, diabetes, epilepsy, cancer, multiple sclerosis, and other conditions (e.g., Lawrence et al., Citation2020; Simpson et al., Citation2021; Zimmermann et al., Citation2018). Research from Kapitan (Citation2012) also shows that individuals involved in art therapy can play an active role in managing their mental health.
These therapies were also viewed as a social engagement opportunity (e.g., *Panda et al., Citation2020). A qualitative systematic review showed that creative arts therapies promote social engagement for stroke survivors (Lo et al., Citation2019), and this was also found in the feasibility study of a stroke-adapted Mindfulness course (Lawrence et al., Citation2020). Furthermore, these therapies were seen as offering a protected time where to rest from daily life and negative thoughts (*Duarte et al., Citation2020). Some participants associated a spiritual meaning with Mindfulness-based practice (*Panda et al., Citation2020), and this spiritual experience connotation was also identified in a systematic review of stroke survivors involved in art activities (Lo et al., Citation2019).
Regarding accessibility, all interventions were community-based; this can be a cause of accessibility issues, as reported in a systematic review, which showed that stroke survivors and family members with mobility and transport issues were excluded a priori from stroke secondary prevention interventions (Lawrence et al., Citation2016). However, research shows that mind-body interventions can be implemented and practiced in a home environment (e.g., *Orenstein et al., Citation2012) and online (Lawrence et al., Citation2021; Simpson et al., Citation2021), which is increasingly relevant in light of COVID-19 restrictions. Additionally, from other studies, we acknowledge that the expected cost to deliver these therapies is minimal (Sobel, Citation2000; Wolsko et al., Citation2004).
Regarding activity engagement, a key element in promoting pwa’s engagement with therapy and the group was the facilitator presence. The behaviour of facilitators has a direct influence on attenders’ participation (Lee & Azios, Citation2020); facilitators can support participants by providing adjusted exercises and tailored resources and promoting the use of multimodal communication techniques and conversational turns. Another essential component was the group and the fact that this was formed by people sharing a similar experience and goals, which is in line with previous research into mindfulness for stroke survivors (Jani et al., Citation2018; Lawrence et al., Citation2020). The importance of the group presence is also highlighted by the review by Lawrence et al. (Citation2016) where it is highlighted that stroke survivors associate the group experience with improved mood and self-esteem. The review by Lo et al. (Citation2019) also showed that peer support and social interaction were key aspects of group involvement for participants with stroke taking part in creative arts interventions.
To either receive an additional motivation boost especially for home practice or to feel part of a big group, pwa were generally willing for partners to be included in the intervention (e.g., *Merriman et al., Citation2015). Lawrence et al. (Citation2016) also highlighted that family members motivated and supported stroke survivors to make positive changes to lifestyle behaviours. This was also found by Jani et al. (Citation2018) where stroke survivors reported that engagement of some stroke survivors might have depended on the support offered by their carers. The systematic review by Parkinson et al. (Citation2019) also showed that a person affected by a long-term condition attending a Mindfulness-based intervention in a partnership with their caregiver might be facilitated, in terms of engagement, practice, and copying, by their partner. With all this considered, the inclusion of family members in these therapies might be a beneficial factor further enhancing the quality of the experience. Key aspects of a successful experience were also reported as time and practice (*Panda et al., Citation2020). Gaining familiarity with the facilitator and group through an introduction session and structured course was also considered an important component that facilitates engagement with a new activity (Jani et al., Citation2018).
In relation to study participants, the frequently found lack of data for some population characteristics (e.g., ethnicity, education, living status, and aphasia severity) prevents us from understanding the extent of the representative nature of the aphasic population. A variety of aphasia types and severities have been found. Although the majority of pwa involved had mild-moderate aphasia, people with severe communication impairments were included in some studies. This raises the importance of ensuring communication inclusion. Surprisingly, this review shows that strategies and adjustments to accommodate pwa’s needs were not always implemented or reported preventing evaluation of the effective engagement of pwa with the interventions. Three studies did not report any strategy or facilitation, and other studies merely implemented a limited amount of support. Although communication guidelines are available (e.g., Stroke Association, Citation2012), the types of supportive communication strategies varied across studies; when implemented, these were always determined by the research team without taking into account the needs and views of pwa. It is widely recognised that pwa have complex communication needs. There is, therefore, an urgent demand for studies involving pwa to effectively implement supportive conversation strategies, aphasia-friendly documentation, and materials and apply other aphasia-specific modifications that can promote active participation for pwa.
Strengths and limitations
Every stage of the review was meticulously planned and presented in a written protocol registered on PROSPERO to ensure implementation of rigorous, transparent, and reproducible procedures (Petticrew & Roberts, Citation2008). One main change was applied. The originally planned aggregative synthesis (Pearson et al., Citation2015) did not appear to be appropriate in the context of the review findings, and hence, a segregated synthesis was conducted (Sandelowski et al., Citation2006).
This study adopted an inclusive approach incorporating quantitative, qualitative, and mixed-methods studies. The reviewer has combined subject searching with keyword searching to run an extensive search. However, in some databases, subject headings were not always available, and the reviewer frequently relied on extensive keyword searching. Synonyms and descriptors of the search parameters were used (e.g., “word finding difficulties” in relation to aphasia). This might have led to retrieval of less specific, broader, and sometimes irrelevant results. Moreover, the high number of duplicates might be related to the fact that the truncation technique was not implemented. All these factors might have affected the time-effectiveness of the search process.
To ensure rigour and systematicity, a second reviewer (HF) was involved in the process of screening (100%), and data extraction and quality appraisal (50%). A broad and comprehensive search strategy was implemented and extended to the grey literature to identify all the relevant studies. Synthesising findings from quantitative, qualitative, and mixed-methods studies was found to be challenging due to the disparate nature of the quantitative and qualitative data sets in terms of heterogeneity of study design and quality, intervention type and dosage, and measured outcomes. Following this consideration, a separate synthesis was conducted to respect the methodological identity and intrinsic value of all types of primary-level studies (Heyvaert et al., Citation2013).
The Revised Effect Direction Plot technique used to identify intervention effectiveness has some intrinsic limitations; Boon and Thomson (Citation2021) acknowledge that when the number of studies is small, the utility of the sign test might be limited, resulting in unrepresentative synthesis if studies with an unclear direction of effect are not included. This might be the case for this review, where many outcomes had conflicting results and could not be included in the effect-direction plot calculation. Regarding narrative syntheses, a challenge was represented by some findings, which could be included in more than one category. It was decided to include in the first theme all the reported positive effects of the therapies and in the second theme all the “meanings”/’functions’ that study participants associated with these therapies. This choice is justified by the interpretive nature of qualitative research that encourages reviewers to apply their unique perspective to interpret rigorously extracted and reported data (Galdas, Citation2017). Furthermore, poor reporting of some population characteristics, collection of follow-up data, and strategies to support pwa’s engagement and methodological weaknesses resulted in a reduction of the review understanding of the mode and context of intervention delivery and thoroughness.
Conclusions
This is the first review exploring the effectiveness, feasibility, and inclusiveness of mind-body and creative arts interventions targeted at pwa. Due to the heterogeneity of design, interventions, and outcomes, it is challenging to state the effectiveness of these interventions in improving global well-being of pwa. Gains were observed in some outcomes (e.g., communication, anxiety, mood, communication confidence, and perception of self). However, findings are provisional and characterised by heterogeneity across participants and studies. Further studies implementing rigorous design, methods, and reporting are needed. Nevertheless, pwa perceive mind-body and creative arts interventions as positive, meaningful, and accessible recreational activities, promoting empowerment, confidence, peer support, and well-being (e.g., *Tamplin et al., Citation2013). These therapies were found to be easy to implement, and other studies showed that these interventions have usually minimal cost and could be effectively delivered online (Lawrence et al., Citation2021; Simpson et al., Citation2021). By highlighting pwa’s perceptions on engagement facilitators and barriers, this review also aims to provide information about the essential features and needed adjustments to promote therapy accessibility for pwa. This study provides emerging evidence on the benefits of mind-body and creative arts interventions for pwa. By offering self-management strategies and opportunities to learn a strength-based skill, socialise, and have a break from negative thoughts, these holistic, person-centred, and highly acceptable programmes might empower pwa to take an active role in their well-being management.
Box 1. Example of search string using boolean operators
Acknowledgments
We acknowledge The UK Stroke Association for funding the HEADS: UP study (SA PPA 18\100011) of which this funded PhD review is part.
We thank Dr Ben Parkinson for advice during data synthesis.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- *Andrew, C. [2015]. Drawing for people with aphasia: An Investigation into the Possible Benefits of Learning Observational Drawing for People with Aphasia. [ Masters dissertation, City University London
- *Biedermann, B., Croasdale, R., Whitworth, A., Neville, H., & Sedlmeier, P. (2019). Effects of meditation on attention and spoken word finding in people with aphasia. Poster presented at academy of aphasia 57th annual meeting - Macau, Macao, Frontiers in Human Neuroscience, October 9 https://doi.org/10.3389/conf.fnhum.2019.01.00112
- *Castka, K., Abbanat, G., Holland, A., & Szabo, G. (2009). Potential benefits of participating in an aphasia theater program. http://aphasiology.pitt.edu/id/eprint/1972
- *Cherney, L. R., Oehring, A. K., Whipple, K., & Rubenstein, T. (2011). “Waiting on the words”: Procedures and outcomes of a drama class for individuals with aphasia. Seminars in Speech and Language, 32(3), 229–42. https://doi.org/10.1055/s-0031-1286177
- *Crielesi, M., Roche, L., Monopoli, G., Yeates, G. N., & Monte, S. (2019). Mindfulness interventions for people with aphasia–case evidence from individual and group therapy formats Meredith, K.H., and Yeates, G. N. eds . Scholar. In Psychotherapy and Aphasia: Interventions for Emotional Wellbeing and Relationships. (pp. 107–135). Routledge.
- *Croteau, C., Le Dorze, G., Marchoux-Fortier, M., & Getty, M. (2008). What effects does the participation in a theatre workshop have on individuals affected by aphasia. In Poster session presented at the 13th International aphasia rehabilitation conference, Ljubljana, Slovenia.
- *Dickinson, J., Friary, P., & McCann, C. M. (2017). The influence of mindfulness meditation on communication and anxiety: A case study of a person with aphasia. Aphasiology, 31(9), 1044–1058. https://doi.org/10.1080/02687038.2016.1234582
- *Duarte, J. D. S., Rocha, J. D. S., & Brandão, L. (2020). The practice of the art of clowning by a person with aphasia: A case report. Revista CEFAC, 22(4), 1–10. https://doi.org/10.1590/1982-0216/20202245520
- *Gadberry, A. L., & Ramachandra, V. (2015). The effectiveness of a music therapy protocol for a person with nonfluent aphasia: A preliminary case report. Music and Medicine, 7(1), 46–8. https://doi.org/10.47513/mmd.v7i1.297
- *Kim, S. H., Kim, M. Y., Lee, J. H., & Chun, S. I. (2008). Art therapy outcomes in the rehabilitation treatment of a stroke patient: A case report. Art Therapy, 25(3), 129–133. https://doi.org/10.1080/07421656.2008.10129593
- *Laures-Gore, J., & Marshall, R. S. (2016). Mindfulness meditation in aphasia: A case report. NeuroRehabilitation, 38(4), 321–329. https://doi.org/10.3233/NRE-161323
- *Mantie-Kozlowski, A., Mantie, R., & Keller, C. H. (2018). Enjoyment in a recreational sing-along group for people with aphasia and their caregivers. Aphasiology, 32(5), 518–537. https://doi.org/10.1080/02687038.2018.1427208
- *Mantie-Kozlowski, A., Mantie, R. A., & Keller, C. H. (2020). Therapeutic songwriting as a meaningful, relationship-oriented activity to establish authentic communicative opportunities during therapy for an individual with PPA. Aphasiology, 35(11), 1432–1447. https://doi.org/10.1080/02687038.2020.1812248
- *Marshall, R. S., Basilakos, A., Williams, T., & Love-Myers, K. (2014). Exploring the benefits of unilateral nostril breathing practice post-stroke: Attention, language, spatial abilities, depression, and anxiety. The Journal of Alternative and Complementary Medicine, 20(3), 185–194. https://doi.org/10.1089/acm.2013.0019
- *Marshall, R. S., Laures‐Gore, J., & Love, K. (2018). Brief mindfulness meditation group training in aphasia: Exploring attention, language and psychophysiological outcomes. International Journal of Language & Communication Disorders, 53(1), 40–54. https://doi.org/10.1111/1460-6984.12325
- *Merriman, J., Walker-Bircham, S., Easton, S. A., & Maddicks, R. (2015). The development of a mindfulness group for stroke patients: A pilot study. Clinical Psychology Forum, 267, 26–30 https://pure.port.ac.uk/ws/portalfiles/portal/3447470/The_Development_of_a_Mindfulness_Group_for_Stroke_Patients.pdf.
- *Orenstein, E., Basilakos, A., & Marshall, R. S. (2012). Effects of mindfulness meditation on three individuals with aphasia. International Journal of Language & Communication Disorders, 47(6), 673–684. https://doi.org/10.1111/j.1460-6984.2012.00173.x
- *Panda, S., Whitworth, A., Hersh, D., & Biedermann, B. (2020). “Giving yourself some breathing room … ”: An exploration of group meditation for people with aphasia. Aphasiology, 35(12), 1544–1572. https://doi.org/10.1080/02687038.2020.1819956
- *Tamplin, J., Baker, F. A., Jones, B., Way, A., & Lee, S. (2013). ‘Stroke a Chord’: The effect of singing in a community choir on mood and social engagement for people living with aphasia following a stroke. NeuroRehabilitation, 32(4), 929–941. https://doi.org/10.3233/NRE-130916
- *Wantsala, J., Shirley, J., & Lundgren, K. (2010). The use of mindfulness-based stress reduction in treating aphasia. [no details].
- *Yeates, G. N. (2019 The potential contribution of mind-body interventions within psychological support following aphasia Meredith, K. H., and Yeates, G.N. eds Psychotherapy and Aphasia: Interventions for Emotional Wellbeing and Relationships. (Routledge). Psychotherapy and Aphasia. 136–164 https://www.researchgate.net/profile/Giles-Yeates/publication/338580919_The_potential_contribution_of_mind-body_interventions_within_psychological_support_following_aphasia_A_conceptual_review.
- *Zumbansen, A., Peretz, I., Anglade, C., Bilodeau, J., Généreux, S., Hubert, M., & Hébert, S. (2017). Effect of choir activity in the rehabilitation of aphasia: A blind, randomised, controlled pilot study. Aphasiology, 31(8), 879–900. https://doi.org/10.1080/02687038.2016.1227424
- Albuquerque, A. S., & Tróccoli, B. T. (2004). Desenvolvimento de uma escala de bem-estar subjetivo. Psicologia: Teoria E Pesquisa, 20(2), 153–164. https://doi.org/10.1590/S0102-37722004000200008
- Ali, K., Gammidge, T., & Waller, D. (2014). Fight like a ferret: A novel approach of using art therapy to reduce anxiety in stroke patients undergoing hospital rehabilitation. Medical Humanities, 40(1), 56–60. https://doi.org/10.1136/medhum-2013-010448
- Babbitt, E. M., & Cherney, L. R. (2010). Communication confidence in persons with aphasia. Topics in Stroke Rehabilitation, 17(3), 214–223. https://doi.org/10.1310/tsr1703-214
- Baer, R., Crane, C., Miller, E., & Kuyken, W. (2019). Doing no harm in mindfulness-based programs: Conceptual issues and empirical findings. Clinical Psychology Review, 71(July 2019), 101–114. https://doi.org/10.1016/j.cpr.2019.01.001
- Beck, A. T., Epstein, N., Brown, G., & Steer, R. A. (1988). An inventory for measuring clinical anxiety: The beck anxiety inventory. Journal of Consulting and Clinical Psychology, 56(6), 893–897. https://doi.org/10.1016/0272-7358(88)90050-5
- Beck, A. T., & Steer, R. A. (1993). Beck anxiety inventory: BAI. Psychological Corporation. https://doi.org/10.1007/978-0-387-79948-3_197
- Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the beck depression inventory-II (Pearson). https://doi.org/10.1007/978-1-4419-1005-9_441
- Bénaim, C., Pélissier, J., Petiot, S., Bareil, M., Ferrat, E., Royer, E., … Hérisson, C. (2003). Un outil francophone de mesure de la qualité de vie de l’aphasique: Le SIP-65. Annales de Réadaptation Et de Médecine Physique, 46(1), 2–11. https://doi.org/10.1016/S0168-6054(02)00306-9
- Benton A. (1967). Problems of Test Construction in the Field of Aphasia. Cortex, 3(1), 32–58. 10.1016/S0010-9452(67)80005-4
- Bettany-Saltikov, J. (2012). How to do a systematic literature review in nursing: A step-by-step guide. Open University Press [Scholar].
- Biedermann, B, Beyersmann, L., Mason, C., Hameau, S., and Nickels, L. 2014 The Battery for Assessment of Plural Processing in Aphasia (Frequency) test (BAPPA-F) (Macquarie Online Test Interface (MOTIf))https://www.motif.org.au/home/test/bappaf
- Biedermann , B., Beyersmann, L., Mason, C., Hameau, S., and Nickels, L. 2014b The Battery for Assessment of Plural Processing in Aphasia (Regularity) test (BAPPA-R) (Macquarie Online Test Interface (MOTIf))https://www.motif.org.au/
- Boon, M. H., & Thomson, H. (2021). The effect direction plot revisited: Application of the 2019 cochrane handbook guidance on alternative synthesis methods. Research Synthesis Methods, 12(1), 29–33. https://doi.org/10.1002/jrsm.1458
- CASP Checklists (2020). CASP Qualitative Checklist. CASP-Critical Appraisal Skills Programme https://casp-uk.net/casp-tools-checklists/
- Code, C., Hemsley, G., & Herrmann, M. (1999). The emotional impact of aphasia. Seminars in Speech and Language, 20(1), 19–31. https://doi.org/10.1055/s-2008-1064006
- Conners, K. (2004). Conners continuous performance test (CPT-II): Version 5 for windows, technical guide and software manual. Multi-Health Systems. https://doi.org/10.1007/978-0-387-79948-3_1535
- Craig, P., Dieppe, P., Macintyre, S., Michie, S., Nazareth, I., & Petticrew, M. (2008). Developing and evaluating complex interventions: The new medical research council guidance. BMJ 2008, 337(a1655), 979–983. https://doi.org/10.1136/bmj.a1655
- Creswell, J. W., & Creswell, J. D. (2017). Research design: Qualitative, quantitative, and mixed methods approaches. Scholar. Sage publications.
- Cruice, M., Worrall, L., & Hickson, L. (2011). Reporting on psychological well-being of older adults with chronic aphasia in the context of unaffected peers. Disability and Rehabilitation, 33(3), 219–228. https://doi.org/10.3109/09638288.2010.503835
- De Silva, D. (2011). Evidence: Helping people help themselves. A review of the evidence considering whether it is worthwhile to support self-management. The Health Foundation [Scholar].
- De Wit, L., Putman, K., Baert, I., Lincoln, N. B., Angst, F., Beyens, H., … Feys, H. (2008). Anxiety and depression in the first six months after stroke. A longitudinal multicentre study. Disability and Rehabilitation, 30(24), 1858–1866. https://doi.org/10.1080/09638280701708736
- Doyle, P., McNeil, M., Hula, W., & Mikolic, J. (2003). The burden of stroke scale (BOSS): Validating patient-reported communication difficulty and associated psychological distress in stroke survivors. Aphasiology, 17(3), 291–304. https://doi.org/10.1080/729255459
- Druks, J., and Masterson, J. 2000 An object and action naming battery (East Sussex: Psychology Press.)
- Duncan, P. W., Wallace, D., Lai, S. M., Johnson, D., Embretson, S., & Laster, L. J. (1999). The stroke impact scale version 2.0: Evaluation of reliability, validity, and sensitivity to change. Stroke, 30(10), 2131–2140. https://doi.org/10.1161/01.STR.30.10.2131
- Erickson R J, Goldinger S D and LaPointe L L. (1996). Auditory Vigilance in Aphasic Individuals: Detecting Nonlinguistic Stimuli with Full or Divided Attention. Brain and Cognition, 30(2), 244–253. 10.1006/brcg.1996.0016
- Eysenck, M. W., Derakshan, N., Santos, R., & Calvo, M. G. (2007). Anxiety and cognitive performance: Attentional control theory. Emotion, 7(2), 336–353. https://doi.org/10.1037/1528-3542.7.2.336
- Fougeyrollas, P., & Noreau, L. (1998). Assessment of life habits, general short form (life-H 3.0). International Network on the Disability Creation Process; Canadian Society for the International Classification of Impairments, Disabilities and Handicaps.
- Galdas, P. (2017). Revisiting bias in qualitative research: Reflections on its relationship with funding and impact. International Journal of Qualitative Methods, 16(1), 1–2. https://doi.org/10.1177/1609406917748992
- Goodglass , H., Kaplan, N., and Barresi, B 2001 Boston Diagnostic Aphasia Examination 3rd (Baltimore: Lippincott: Williamson & Wilkins)
- Gough, H.G., and Heilbrun, A.B. 1983 The Adjective Check List Manual. (Palo Alto, CA: Consulting Psychologist Press.)
- Graham, J. E., Karmarkar, A. M., & Ottenbacher, K. J. (2012). Small sample research designs for evidence-based rehabilitation: Issues and methods. Archives of Physical Medicine and Rehabilitation, 93(8), S111–S116. https://doi.org/10.1016/j.apmr.2011.12.017
- Helm-Estabrooks , N. 1992ADP: Aphasia diagnostic profiles (Pro Ed)
- Helm-Estabrooks, N.(2001).Cognitive linguistic quick test-plus:CLQT. Scholar.Psychological Corporation.
- Helm-estabrooks, N., and Nicholas, M. 2003 Narrative Story Cards (PRO-ED Incorporated)
- Heyvaert, M., Maes,B., & Onghena, P.(2013). Mixed methods research synthesis: Definition, framework, and potential. Quality & Quantity, 47(2),659–676. https://doi.org/10.1007/s11135-011-9538-6
- Hilari, K., Byng, S., Lamping, D. L., & Smith, S. C. (2003). Stroke and aphasia quality of life scale-39(SAQOL-39) evaluation of acceptability, reliability, and validity. Stroke, 34(8), 1944–1950. https://doi.org/10.1161/01.STR.0000081987.46660.ED
- Hoffmann, T. C., Glasziou, P. P., Boutron, I., Milne, R., Perera, R., Moher, D., andMichie, S. (2014). Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348(g1687), 1–12. https://doi.org/10.1136/bmj.g1687
- Hong, Q. N., Pluye, P., Bujold, M., & Wassef, M. (2017). Convergent and sequential synthesis designs: Implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Systematic Reviews, 6(1), 1–14. https://doi.org/10.1186/s13643-017-0454-2
- Jani, B. D., Simpson, R., Lawrence, M., Simpson, S., & Mercer, S. W. (2018). Acceptability of mindfulness from the perspective of stroke survivors and caregivers: A qualitative study. Pilot and Feasibility Studies, 4(1), 1–9. https://doi.org/10.1186/s40814-018-0244-1
- Kabat-Zinn J. (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry, 4(1), 33–47. 10.1016/0163-8343(82)90026-3
- Kagan, A., Simmons‐Mackie, N., Rowland, A., Huijbregts, M., Shumway, E., McEwen, S., … Sharp, S. (2008). Counting what counts: A framework for capturing real‐life outcomes of aphasia intervention. Aphasiology, 22(3), 258–280. https://doi.org/10.1080/02687030701282595
- Kapitan, L. (2012). Does art therapy work? Identifying the active ingredients of art therapy efficacy. Art Therapy, 29(2), 48–49. https://doi.org/10.1080/07421656.2012.684292
- Kaplan, E., Goodglass, H., and Weintraub, S. 2001 The Boston Naming Test 3rd (Philadelphia, PA: Lea and Febiger)
- Kay, J., Lesser, R., & Coltheart, M. (1996). Psycholinguistic assessments of language processing in aphasia (PALPA): An introduction. Aphasiology, 10(2), 159–180. https://doi.org/10.1080/02687039608248403
- Kertesz, A. 2006 The Western Aphasia Battery (San Antonio, TX : PsychCorp)
- Kim S, Kim M, Lee J and Chun S. (2008). Art Therapy Outcomes in the Rehabilitation Treatment of a Stroke Patient: A Case Report. Art Therapy, 25(3), 129–133. 10.1080/07421656.2008.10129593
- Kim H and Na D L. (2004). Normative Data on the Korean Version of the Western Aphasia Battery. Journal of Clinical and Experimental Neuropsychology, 26(8), 1011–1020. 10.1080/13803390490515397
- Knapp, P., Burton, C. A. C., Holmes, J., Murray, J., Gillespie, D., Lightbody, C. E., … Lewis, S. R. (2017). Interventions for treating anxiety after stroke. Cochrane Database of Systematic Reviews, 2017(5), 1–33. https://doi.org/10.1002/14651858.CD008860.pub3
- Lawrence, et al., (2020). HEADS: UP (helping ease anxiety and depression following stroke) psychological self-management intervention non-randomised feasibility study: Report [unpublished].
- Lawrence, Davis B, Clark C., (2021). HEADS: UP online (helping ease anxiety and depression following stroke) psychological self-management intervention non-randomised feasibility study: Report [unpublished].
- Lawrence, M., Booth, J., Mercer, S., & Crawford, E. (2013). A systematic review of the benefits of mindfulness-based interventions following transient ischemic attack and stroke. International Journal of Stroke, 8(6), 465–474. https://doi.org/10.1111/ijs.12135
- Lawrence, M., Pringle, J., Kerr, S., & Booth, J. (2016). Stroke survivors’ and family members’ perspectives of multimodal lifestyle interventions for secondary prevention of stroke and transient ischemic attack: A qualitative review and meta-aggregation. Disability and Rehabilitation, 38(1), 11–21. https://doi.org/10.3109/09638288.2015.1031831
- Lazaridou, A., Philbrook, P., & Tzika, A. A. (2013). Yoga and mindfulness as therapeutic interventions for stroke rehabilitation: A systematic review. Evidence-Based Complementary and Alternative Medicine, 2013 Article ID 357108 , 1–9. https://doi.org/10.1155/2013/357108
- Lee, J. B., & Azios, J. H. (2020). Facilitator behaviors leading to engagement and disengagement in aphasia conversation groups. American Journal of Speech-language Pathology, 29(1S), 393–411. https://doi.org/10.1044/2019_AJSLP-CAC48-18-0220
- Lo, T. L. T., Lee, J. L. C., & Ho, R. T. H. (2019). Creative arts-based therapies for stroke survivors: A qualitative systematic review. Frontiers in Psychology, 2018(9), 1–12. https://doi.org/10.3389/fpsyg.2018.01646
- Lomas, J., Pickard, L., Bester, S., Elbard, H., Finlayson, A., & Zoghaib, C. (1989). The communicative effectiveness index: Development and psychometric evaluation of a functional communication measure for adult aphasia. Journal of Speech and Hearing Disorders, 54(1), 113–124. https://doi.org/10.1044/jshd.5401.113
- Love, M. F., Sharrief, A., Chaoul, A., Savitz, S., & Beauchamp, J. E. S. (2019). Mind-body interventions, psychological stressors, and quality of life in stroke survivors: A systematic review. Stroke, 50(2), 434–440. https://doi.org/10.1161/STROKEAHA.118.021150
- Manning, M., MacFarlane, A., Hickey, A., & Franklin, S. (2019). Perspectives of people with aphasia post-stroke towards personal recovery and living successfully: A systematic review and thematic synthesis. PloS One, 14(3), 1–22. https://doi.org/10.1371/journal.pone.0214200
- McNair, D. M., Lorr, M., & Droppleman, L. F. (1971). Manual for the profile of mood states (POMS). San Diego: Educational and Industrial Testing Service. Scholar.
- Nespoulous, J. L., Lecours, A. R., Lafond, D., Lemay, A., Puel , M., Cot, F., . . . , and Giroux, F. 1992 Protocole Montréal-Toulouse d’examen linguistique de l’aphasie MT-86 M1béta Module standard initial 2nd (Isbergues: Ortho-Edition)
- Nyström M. (2006). Aphasia – an existential loneliness: A study on the loss of the world of symbols. International Journal of Qualitative Studies on Health and Well-being, 1(1), 38–49. 10.1080/17482620500501883
- O’Sullivan, C., & Chard, G. (2010). An exploration of participation in leisure activities post‐stroke. Australian Occupational Therapy Journal, 57(3), 159–166. https://doi.org/10.1111/j.1440-1630.2009.00833.x
- Otal, B., Olma, M. C., Flöel, A., & Wellwood, I. (2015). Inhibitory non-invasive brain stimulation to homologous language regions as an adjunct to speech and language therapy in post-stroke aphasia: A meta-analysis. Frontiers in Human Neuroscience, 9(236), 1–7. https://doi.org/10.3389/fnhum.2015.00236
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., and Moher, D. (2021a). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372(n71) , 1–9. https://doi.org/10.1136/bmj.n71
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., and Moher, D. (2021b). Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. Journal of Clinical Epidemiology, 134 June 01 , 103–112. https://doi.org/10.1016/j.jclinepi.2021.02.003
- Parkinson, B., Lawrence, M., McElhinney, E., Booth, J., & Parkinson, B. (2019). Mindfulness for people with long-term conditions and their family caregivers: A systematic review. Complementary Therapies in Clinical Practice, 34(2019), 76–86. https://doi.org/10.1016/j.ctcp.2018.10.019
- Paul, D. R., Frattali, C., Holland, A. L., Thompson, C. K., Caperton, C. J., & Slater, S. C.(2004). Quality of communication life scale: Manual. American Speech-Language Hearing Association. https://doi.org/10.1007/978-3-319-56782-2_9143-2
- Pearl, G., & Cruice, M. (2017). Facilitating the involvement of people with aphasia in stroke research by developing communicatively accessible research resources. Topics in Language Disorders, 37(1), 67–84. https://doi.org/10.1097/TLD.0000000000000112
- Pearson, A., White, H., Bath-Hextall, F., Salmond, S., Apostolo, J., & Kirkpatrick, P. (2015). Amixed-methods approach to systematic reviews. International Journal of Evidence-based Healthcare, 13(3), 121–131. https://doi.org/10.1097/XEB.0000000000000052
- Petticrew, M., & Roberts, H. (2008). Systematic reviews in the social sciences: A practical guide. John Wiley & Sons.
- Ponsford, J., & Kinsella, G. (1991). The use of a rating scale of attentionalbehaviour. Neuropsychological Rehabilitation, 1(4), 241–257. https://doi.org/10.1080/09602019108402257
- , M.R., and PRESCOTT, T.E. 1978 Revised Token Test (Austin, TX.: Pro-ed)
- Puig, A., Lee, S. M., Goodwin, L., & Sherrard, P. A. (2006). The efficacy of creative arts therapies to enhance emotional expression, spirituality, and psychological well-being of newly diagnosed stage I and stage II breast cancer patients: A preliminary study. The Arts in Psychotherapy, 33(3), 218–228. https://doi.org/10.1016/j.aip.2006.02.004
- Robertson, I. H., Ward, T., Ridgeway, V., & Nimmo-smith, I. J. S. A. (1994). The test of everyday attention (TEA). Thames Valley Test Company. 197–221. Scholar.
- Robinson , R. G. 2006 II The clinical neuropsychiatry of stroke: Cognitive, behavioral and emotional disorders following vascular brain injury. (Cambridge University Press.)
- Rousseaux, M., Delacourt, A., Wyrzykowski, N., & Lefeuvre, M. (2001). TLC: Test lillois de communication. Ortho Édition. Scholar.
- Sandelowski, M., Voils, C. I., & Barroso, J. (2006). Defining and designing mixed research synthesis studies. Research in the Schools: A Nationally Refereed Journal Sponsored by the Mid-South Educational Research Association and the University of Alabama, 13 (1), 29 1–15. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2809982/. Scholar
- Shiggins, C., Soskolne, V., Olenik, D., Pearl, G., Haaland-Johansen, L., Isaksen, J., … Horton, S. (2020). Towards an asset-based approach to promoting and sustaining well-being for people with aphasia and their families: An international exploratory study. Aphasiology, 34(1), 70–101. https://doi.org/10.1080/02687038.2018.1548690
- Simmons‐Mackie, N. N., & Damico, J. S. (2007). Access and social inclusion in aphasia: Interactional principles and applications. Aphasiology, 21(1), 81–97. https://doi.org/10.1080/02687030600798311
- Simpson, R., Simpson, S., Wasilewski, M., Mercer, S., & Lawrence, M. (2021). Mindfulness-based interventions for people with multiple sclerosis: A systematic review and meta-aggregation of qualitative research studies. Disability and Rehabilitation 2021 Aug 23 , 1–15. https://doi.org/10.1080/09638288.2021.1964622
- Sobel, D. S. (2000). The cost-effectiveness of mind-body medicine interventions. Progress in Brain Research, 122 2000 ( Scholar), 393–412 https://www.researchgate.net/profile/David-Sobel-2/publication/12579327_The_cost-effectiveness_of_mind-body_medicine_interventions/links/615886964a82eb7cb5e70214/The-cost-effectiveness-of-mind-body-medicine-interventions.pdf.
- Spielberger, C. (1983). State-trait anxiety inventory (form y) manual. palo alto. CA: Mind Garden. Scholar.
- Spinnler, H., & Tognoni, G. (1987). Standardizzazione e taratura italiana si test neuropsicologici. The Italian Journal of Neurological Sciences, 6(8), 47–50.
- Stern, R. A. (1997). Visual analog mood scales, VAMS. Psychological Assessment Resources.
- Stern, R. A. (1999). Assessment of mood states in aphasia. In Seminars in speech and language (Vol. 20, © 1999 by, pp. 33–50). Thieme Medical Publishers, Inc. https://doi.org/10.1055/s-2008-1064007
- Stroke Association, 2012. Accessible information guidelines, making information accessible for people with aphasia. stroke association. [onine] [viewed 24/04/2019]. Available from: https://www.stroke.org.uk/sites/default/files/accessible_information_guidelines.pdf1_.pdf
- Sutcliffe, L. M., & Lincoln, N. B. (1998). The assessment of depression in aphasic stroke patients: The development of the stroke aphasic depression questionnaire. Clinical Rehabilitation, 12(6), 506–513.Suškevičs. https://doi.org/10.1191/026921598672167702
- Swinburn , K., Porter, G., and Howard, D. 2004 Comprehensive aphasia test (New York, NY: Psychology Press)
- Tate, R., McDonald, S., Perdices, M., Togher, L., Schultz, R., & Savage, S. (2008). Rating the methodological quality of single-subject designs and n-of-1 trials: Introducing the single-case experimental design (sced) scale. Neuropsychological Rehabilitation, 18(4), 385–401. https://doi.org/10.1080/09602010802009201
- Thomas, J., & Harden, A. (2008). Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Medical Research Methodology, 8(1), 1–10. https://doi.org/10.1186/1471-2288-8-45
- Tufanaru, C., Munn, Z., Aromataris, E., Campbell, J., & Hopp, L. (2017). Systematic reviews of effectiveness. Joanna Briggs Institute Reviewer’s Manual. The Joanna Briggs Institute. https://reviewersmanual.joannabriggs.org/
- Von Steinbüchel, N., Wilson, L., Gibbons, H., Hawthorne, G., Höfer, S., Schmidt, S., … Truelle, J. L. (2010). Quality of life after brain injury (QOLIBRI): Scale development and metric properties. Journal of Neurotrauma, 27(7), 1167–1185. https://doi.org/10.1089/neu.2009.1076
- Wahbeh, H., Elsas, S. M., & Oken, B. S. (2008). Mind–body interventions: Applications in neurology. Neurology, 70(24), 2321–2328. https://doi.org/10.1212/01.wnl.0000314667.16386.5e
- Weaver, B., Bédard, M., & McAuliffe, J. (2013). Evaluation of a 10-minute version of the attention network test. The Clinical Neuropsychologist, 27(8), 1281–1299. https://doi.org/10.1080/13854046.2013.851741
- Wenk-Sormaz , H. 2005 Meditation can reduce habitual responding Alternative therapies in health and medicine 11 2 42–58 https://www.proquest.com/docview/204832654/fulltextPDF/6135362A82C24033PQ/1?accountid=15977
- The Whoqol Group. (1998). Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological Medicine, 28(3), 551–558. https://doi.org/10.1017/S0033291798006667
- Wolsko, P. M., Eisenberg, D. M., Davis, R. B., & Phillips, R. S. (2004). Use of mind-body medical therapies. Journal of General Internal Medicine, 19(1), 43–50. https://doi.org/10.1111/j.1525-1497.2004.21019.x
- Zeidan F, Johnson S K, Diamond B J, David Z and Goolkasian P. (2010). Mindfulness meditation improves cognition: Evidence of brief mental training. Consciousness and Cognition, 19(2), 597–605. 10.1016/j.concog.2010.03.014
- Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
- Zimmermann, F. F., Burrell, B., & Jordan, J. (2018). The acceptability and potential benefits of mindfulness-based interventions in improving psychological well-being for adults with advanced cancer: A systematic review. Complementary Therapies in Clinical Practice, 30(February 2018), 68–78. https://doi.org/10.1016/j.ctcp.2017.12.014
Appendices
Appendix 1.
Table 4. Theoretical framework: pwa’s perspective on mind-body and creative arts interventions
Appendix 2.
Table 5. Summary of findings for included studies