ABSTRACT
Purpose
This study investigates whether Acquired Brain Injury (ABI) is associated with changes in sexual function and satisfaction and how such changes are experienced, focusing on invisible impairments after ABI.
Materials and Methods
A study-specific questionnaire was distributed in 2018–2019. The sample included individuals aged 20–90 years diagnosed with ABI due to subarachnoid hemorrhage (SAH), trauma, infection, or anoxia (ischemic stroke and intracerebral hemorrhage excluded), who participated in brain injury rehabilitation in Sweden, 2014–2016. Chi-square and Logistic regression analyses were used.
Results
The study consists of 250 participants (response rate was 40%). Among participants 78% (194/250) had resumed sexual life. Participants reporting sexual changes also experienced more consequences related to ABI. Those with decreased sexual desire (63%, 148/234) reported more ABI consequences, including decreased memory (86% vs 65%, p = 0.000), decreased concentration ability (82% vs 65%, p = 0.003), and increased tiredness (91% vs 70%, p = 0.000) compared to those with intact desire. Such consequences can be invisible to others.
Conclusion
Visible impairments are known to impact sexual functions and satisfaction after ABI. Our results show how invisible impairments also have a great impact. From a biopsychosocial perspective, these results imply that individuals should receive sexual rehabilitation, irrespective of ABI impairment.
Introduction
Globally many individuals live with the consequences of Acquired Brain Injury (ABI), an umbrella term (Citation1) including, among others, Subarachnoid Hemorrhage (SAH) (incidence 6/100 000) (Citation2), Stroke (220/100 000) (Citation3), and Traumatic Brain Injuries (TBI) (900–1300/100 000) (Citation4). Some consequences after ABI are physical and visible, such as impaired walking ability, while consequences including impaired memory, inability to focus, fatigue, bladder/bowel symptoms, and difficulties managing activities of daily living (ADL) may be invisible to others (Citation5). Even if invisible, however, these consequences can have an impact on life after ABI, including on sexuality. The dysexecutive syndrome, which also can be invisible to others, includes for example difficulties in initiation, inhibition, flexibility, and planning. In a study investigating whether dysexecutive problems were related to risky sexual behavior, Moreno et al. (Citation6) found that individuals with more dysexecutive symptoms also engaged in more risky sexual behavior.
Neurosexuality has been defined as “a framework for the scientific study of the relationships between sexuality and the brain” (Citation7). Hence, neurosexuality includes how specific brain structures contribute to sexual functions, emotions, and behavior in all individuals, not just those with ABI. Moreno et al. (Citation7) acknowledge that neurosexuality needs to have a transdisciplinary approach since “it transcends traditional boundaries and integrates the perspectives of natural, social, and health sciences in a humanities context to build a comprehensive understanding of the neural correlates of sexual behavior” (Citation7).
Rehabilitation after ABI has partly neglected sexuality issues, even though several studies reveal that sexuality can be affected (Citation8–15), and should therefore be integrated into brain injury rehabilitation (Citation16). Previous studies have approached sexuality and ABI from different perspectives (those of individuals with ABI, partners, or professionals), while this study will focus on individuals with ABI. Time since injury, ABI severity, diagnoses, and methodology vary in earlier studies. Some were conducted only a few weeks after ABI, others several years later (Citation16). Studies have often been directed toward specific diagnoses such as TBI (Citation8–10,Citation16,Citation17) or Stroke (Citation12–15,Citation18–20), but rarely SAH (Citation21), while studies on anoxic, post-infectious, or post-inflammatory ABI are lacking. Research methods cover both qualitative (Citation22) and quantitative studies (Citation10), including a variety of instruments, sampling methods, and analyses (Citation21). This variety complicates comparisons of studies, and none of the instruments covers all aspects of sexuality and ABI. Irrespective of definition, time since injury, and study method, research has shown that ABI can affect sexuality and emphasized the prevalence of sexual dysfunction in individuals with ABI and the need for further studies (Citation13,Citation22–25). Invisible aspects and their impact on sexuality is one area which needs further investigation to gain in-depth knowledge concerning sexuality after ABI.
Invisible consequences and sexuality after ABI
After recovering from ABI, individuals might not have visible impairments, but could still suffer from consequences invisible to others (i.e., fatigue or memory impairment) (Citation15,Citation23,Citation25,Citation26). Invisible impairments can affect health and social interactions, such as limiting social participation due to fatigue and/or bladder/bowel symptoms, but they could also influence sexual interactions. Lingsom (Citation27) stressed that individuals with invisible disabilities might want to “pass” as without a disability. Lingsom (Citation27) discussed neither sexuality nor ABI, but these views on invisible impairments and social interactions in general can be of importance in research on sexuality after ABI. To our knowledge, there are a few studies including aspects of invisible disabilities and sexuality after ABI (Citation23,Citation25,Citation28–30), but the invisibility and its consequences for sexuality has not yet been thoroughly examined. Goldin et al. (Citation29) argued that fatigue is associated with lower frequency of sexual activity among individuals with TBI than the comparison group without TBI. Communication aspects surrounding sexuality after ABI have been even less described. In one pilot study, however, Lemieux et al. (Citation31) argued that lack of communication skills among aphasic individuals with stroke and spouses resulted in decreased initiation of sexual activities.
Sexual changes after ABI
Earlier research (Citation8,Citation9,Citation11,Citation16,Citation18,Citation23,Citation25) has reported sexual changes after ABI for functions such as sexual desire, erectile function, lubrication, and orgasm, but also for sexual satisfaction. In a review of nine studies from 1981 to 2003 regarding experiences of individuals with TBI, Moreno et al. (Citation16) stated that erectile dysfunction (ED) varied between 30% and 58%. Likewise, Grenier-Genest et al. (Citation18) showed ED between 28% and 75% in their review of twenty-one studies from 1981 to 2017 investigating stroke and sexual functions. Grenier-Genest et al. (Citation18) also disclosed that lubrication difficulties were experienced in between half and three quarters (50%–77%) of the females. In one of the studies included in the review by Moreno et al. (Citation16), 14% reported overall sexual dysfunction; but the participants in that study were only six weeks post-injury. In a study concerning sexuality and limb amputation, Verschuren et al. (Citation32) argued that individuals newly injured might still be adapting to their new situation and are therefore likely to change their experiences of sexuality. This might also apply to individuals with ABI.
To compare with the general population in Sweden (not focused on ABI), sexual activity decreases with age, and there are also gender differences. Swedish studies report that about 70–80% total are sexually active (Citation33,Citation34), while in the age group 65–84 about 60% among males and only 40% among females are (Citation33). However, over time (from 1972 to 2000) both sexual activity and satisfaction had increased among individuals aged 70 years (Citation35). Among the oldest (≥90 years) 10% are still sexually active (Citation34). Stentagg et al. (Citation34) found that females were more satisfied with their sexual life than males in all age-groups (about 90% vs 80%). While the study by the Public Health Agency of Sweden (Citation33) showed that almost 60% were satisfied with their sexual life. However, in age group 65–84 years only 48% of females and 33% of males were satisfied (Citation33). Sander et al. (Citation11) reveal, in a study of 223 individuals one year post-TBI that 82% had resumed their sexual life, but about half (55%) reported decreased frequency in sexual activities, one third (34%) decreased sexual desire, while almost one third (29%) experienced dissatisfaction with sexual function. Kreuter et al. (Citation25) presented similar findings in a Swedish study from 1998, in which half of the 92 participants were dissatisfied with the frequency of sexual activity after TBI. In the 1980s, Sjögren and Fugl-Meyer (Citation28,Citation36) studied stroke and sexuality in a Swedish context, and implied that ED for men and fatigue for women were the main causes of decreased sexual enjoyment (Citation28), while dependency in ADL and decreased skin sensibility were associated with decreased frequency of intercourse (Citation36). These invisible consequences are also of interest concerning other ABI diagnoses. In recent years, a few Swedish studies have explored sexuality of individuals with stroke and stressed that sexuality issues need to be assessed but that guidelines are lacking (Citation12,Citation15,Citation26). There is a lack of contemporary studies concerning ABI diagnoses other than stroke with a Swedish perspective. In a Swedish qualitative pilot study from 2010, participants experienced changes in sexual functions after ABI, in terms of fatigue, erection/lubrication, and/or orgasm (Citation23). Participants described coping strategies, but not always with the best results. Hence, further studies need to explore sexuality after ABI.
Holistic approach with a biopsychosocial model
Sexual dysfunction after ABI can occur due to organic dysfunctions (Citation37), but might also arise due to emotional or social changes; and a biopsychosocial model (Citation16,Citation30,Citation38,Citation39) can therefore provide more insight. In a narrative review, Park et al. (Citation13) stressed that even though specific brain lesions can change biological conditions, this is not enough to predict outcome of sexual function. This is in line with the findings of Kreuter et al. (Citation25), as well as Bivona et al.’s (Citation30) biopsychosocial analysis of sexuality after TBI. The latter stated that sexual changes might occur not only due to location of TBI but also psychosocial factors. Interpretations of sexuality after ABI can be deeper when applying a holistic perspective including individuals’ personalities, experiences, and social contexts. Moreno et al. (Citation16) utilize a biopsychosocial model of sexuality developed by Gan in 2005. The model includes Neuropsychological & Psychological effects, Medical & Physical issues, and Relationship changes. They suggest a transdisciplinary team approach to address these aspects. However, changes in sexuality might still be overlooked as a normal variation in the life cycle (Citation22). In a qualitative study, Nilsson et al. (Citation12) revealed that individuals six years after stroke attributed negative sexual experiences to age or circumstances other than stroke. Ek (Citation23) also found that some individuals thought of their sexual problems as age-related rather than due to ABI. This is consistent with the study by Layman et al. (Citation22), where individuals with TBI and partners attributed their changes in sexuality to age. On the other hand, Layman et al. (Citation22) also found that individuals with TBI and partners rated sexual functions lower than the control group without injury. These findings illustrate the striving to be part of a “normal” and accepted social context, where changes due to age are considered a normal part of the life cycle.
There is a shortage of studies with perspectives of individuals with ABI on sexuality, specifically in relation to invisible physical and cognitive consequences after ABI other than stroke (Citation20). Most contemporary studies are from the U.S., Canada, and Australia, and research on sexuality after non-stroke-ABI in (Northern) Europe is lacking. Stroke and sexuality have been covered in research both internationally (Citation18,Citation19) and in Sweden (Citation12,Citation15,Citation26,Citation36), while sexuality in other ABI groups needs further exploration. To our knowledge, this is the first study in Sweden with national coverage and a focus on several invisible disabilities affecting sexuality after ABI. This study examines subjective experiences of changes in sexuality after ABI, covering a population with non-stroke-ABI, and including both visible and invisible impairments. Hence, this study had two major aims: (1) to explore experiences of sexuality after ABI, with a specific focus on invisible consequences after ABI and (2) to determine possible associations with sexual dysfunctions and dissatisfaction.
Methods
Participants and data collection procedure
This is a cross-sectional study and data were collected on one occasion by a postal survey, in 2018–2019. Potential participants were recruited from the national quality register for rehabilitation, Web-Rehab SwedenFootnote1 (Citation40), hereinafter referred to as the Web-Rehab register. The Web-Rehab register collects demographic data and data on physical, psychological, and cognitive domains, and uses a classification for diagnostic groups (Citation41). We included the following diagnostic groups: Subarachnoid hemorrhage (SAH), Traumatic brain injury (TBI), Post infectious and Post- inflammatory brain injury, and Anoxic brain injury. Many countries have national guidelines for stroke care, and the category Stroke deserves to be illuminated in a study concerning sexuality with focus on individuals with stroke only. Hence, we neither included the diagnostic groups Stroke and other cerebrovascular diseases, which include Ischemic stroke and Intracerebral hemorrhage, nor Other brain injuries, which include progressive diseases such as malign tumors and dementia and involve other challenges than those we aim to study. Despite the exclusion of stroke and other brain injuries we will use the concept ABI consistently for better readability.
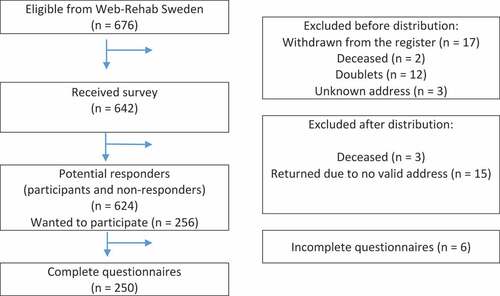
All participants met the following inclusion criteria: completed inpatient brain injury rehabilitation in Sweden between 2014 and 2016; diagnosed with an ABI in the classification groups described above; age ≥18 years at the time of rehabilitation; Swedish speaking without an interpreter; and has ability to answer a questionnaire independently. The latter was ensured by the results from the Functional Independent Measure (FIM) (Citation42) assessed at discharge from rehabilitation, with inclusion for individuals scoring equivalent to Independent at the item for “comprehension.” Participants who interrupted the rehabilitation were excluded, irrespective of cause. All inclusion and exclusion criteria were ensured through the registration in the Web-Rehab register at discharge from rehabilitation. presents the flow chart for inclusion and exclusion in the study. Non-responders received two reminders, three weeks apart. A total of 250 of the 624 potential individuals completed the questionnaire and were included in the study, providing a response rate of 40%. We applied for background data and contact information from the Web-Rehab register for distribution of the questionnaire to all 624 individuals (250 participants and 374 non-responders).
The postal survey consisted of written information about the study, a questionnaire, and a pre-paid envelope for responding. The written information included a short presentation of the study and description of how confidentiality was secured, and emphasized that participation was voluntary. It also provided information about how to get in contact with a nonprofit counselor for sexual issues if needed. There was no financial compensation for participation.
The study-specific questionnaire
A questionnaire was designed, inspired by instruments such as “The Brain Injury Questionnaire of Sexuality” (Citation43), “Sexual Interest and Satisfaction (SIS) Scale” (Citation25), earlier studies (Citation23,Citation24,Citation44), and from clinical practice. Due to the study group’s circumstances, the questions needed to be easy both to understand and to answer. Interview studies including individuals with ABI and partners were utilized to validate the questions (Citation23,Citation24); but a peer group of researchers and PhD students also validated the themes and questions. We edited the questionnaire in an iterative process until the residue of sixty-four questions. From a brain injury rehabilitation unit, five outpatients and six professionals pilot-tested both the questionnaire and the information letter. After receiving feedback, we made some minor changes in layout and wording but did not delete any questions at that point.
The questionnaire consisted of four themes, and this study covers the first three. The first included eight items concerning background information: gender (options: male, female, trans person, and other), place of residence, employment, relationship status, perceived health/diseases, and medications. In the second theme, 12 items included functional ability in physical, cognitive, and social aspects. The theme covered questions on walking capacity, ADL, and bladder/bowel symptoms, followed by other common consequences after ABI, such as memory, tiredness, concentration, speech, and mood. The third theme included 32 items and covered sexuality after ABI. Initially, this part defined sexual intercourse, sexual activity, and sexuality. Subsequently, the questions asked for sexual orientation (options: heterosexual, homosexual, bisexual, asexual, other, and I don’t want to answer). Next came sexual functions, covering sexual desire, initiation of sexual activity with partner, pain, erection, lubrication, ejaculation, and orgasm (). A six-point Likert scale was utilized for the questions on satisfaction. The questions had fixed answers except for questions on gender, disease, health, medication, and bowel/bladder symptoms, where the alternative other could be specified. The fourth theme covered Rehabilitation and will be presented in an upcoming study.
Statistical analysis
Cronbach’s Alpha index was calculated to measure the internal consistency of two constructs: “Cognitive functions” (0.859) and “Sexual functions” (0.818 males, 0.855 females). Variables were dichotomized into positive and negative categories. Variables with a six-point Likert scale were coded as “dissatisfied” for 1 to 3 and “satisfied” for 4 to 6. We also created a new variable by subtracting the six-point Likert scale variable “satisfaction with present sexual life” from the variable “satisfaction with sexual life as it was before ABI”; the new variable had a range of −5 to +3. Thereafter, we dichotomized the variable, where −5 to −1 were coded as 1 while 0 to +3 were coded as 0. The dichotomized variable was named “decreased satisfaction with sexual life” and was used for our analysis. As explained earlier, the variables were dichotomized, but we also re-coded them into 1 = the statement, and 0 = not the statement.
All statistical analyses were calculated in IBM SPSS statistics, version 25. A two-sided p-value < 0.05 was considered to indicate statistical significance. The participants’ characteristics were presented as numbers and percentages (%). The characteristics of participants and non-responders were compared using chi-squared test for nominal variables; meanwhile, means, standard deviation, and student’s t-test were calculated for the variables age, Length of Stay (LOS), and FIM total scores for cognitive items and physical items, separately. From the second theme (functional ability) we used 12 items as independent variables, and from the third theme (sexuality after ABI) 10 items were used as dependent variables for the chi-squared calculations. Finally, we performed a binary logistic regression analysis using the dependent variable “Dissatisfaction with sexual desire.”
Study ethics
Ethical approval was obtained from the Ethical Review Board in Lund, Sweden (Code: EPN:2017 799). Ethical considerations have been taken in the implementation of this study because individuals with ABI are vulnerable, and their personal experiences regarding sexuality after the ABI are sensitive information.
Results
Participant characteristics
presents the characteristics of both participants (n = 250) and non-responders (n = 374), providing data from the Web-Rehab register; and it also presents additional characteristics of the participants, providing data from the questionnaire. There were no significant differences in gender, age, diagnosis, Length of Stay (LOS), or ethnicity, between participants and non-responders, and the mean age was 54 years in both groups with a range of 20–90 years (SD 14) and 20–94 years (SD 16) respectively. The participants were discharged to independent living without personal dependence to a significantly greater degree (69% vs 59%, p = 0.022), and their educational level was significantly higher than that of non-responders (university 29% vs 21%, p = 0.003). Despite statistical significance, the mean differences were generally small in the groups of participants and non-responders concerning FIM cognitive (32.16 vs 31.58, p = 0.032) and FIM physical (85.77 vs 83.56, p = 0.018) items total score. Since 95% of the participants reported heterosexual orientation, and only 2% reported bi- or homosexual orientation, there were no further divided analyses based on sexual orientation.
Table 1. Background characteristics of participants and non-responders (n = 624).
The ABI had affected the participants’ physical, cognitive, and sexual functions, and this paragraph presents data not shown in table. A large proportion reported cognitive impairments after ABI. Decreased memory was reported by 77% (192/248), increased tiredness by 76% (188/248), decreased ability to concentrate by 83% (207/249), mood changes by 58% (144/249), and speaking/talking difficulties by 32% (80/249) of the participants. More than three quarters of the participants (78%, 194/250) had resumed sexual life, alone or with a partner. The majority of those who had (56%, 82/147) reported no or decreased initiation of sexual activities with a partner. Genital pain during sexual activity was reported by one-tenth (9%, 17/186), and general pain during sexual activity by 6% (12/187).
Sexual desire and satisfaction with sexual life
More than half of the participants reported no or decreased sexual desire (63%, 148/234), dissatisfaction with sexual desire (54%, 120/222), and decreased satisfaction with present sexual life (53%, 102/192), see . The table illustrates a clear trend of significant differences between groups. Decreased cognitive functions, as well as the physical aspects, were significantly more commonly reported by individuals who experienced decreased sexual desire than by those who did not (35–92% vs 16–70%, p = 0.000 – p = 0.005). The most significant difference was seen between those experiencing decreased sexual desire and who also reported reduced initiative to sexual activity compared to those with intact sexual desire (86% vs 19%, p = 0.000). Similar patterns of significant differences were revealed in the chi-squared calculations for the dependent variables “Dissatisfaction with sexual desire” and “Decreased satisfaction with sexual life” ().
Table 2. Experience of decreased sexual desire, dissatisfaction with sexual desire, and decreased satisfaction with sexual life in relation to cognitive functions, physical impairment, health/illness, and medication.
Changes in orgasm experiences
Among participants who had resumed sexual life after ABI (n = 194), more than one-third experienced no or decreased orgasm (38%, 59/157), but also dissatisfaction with frequency of orgasm (38%, 63/168), and/or dissatisfaction after sexual activity (38%, 64/167), see . For the group experiencing dissatisfaction with frequency of orgasm the chi-squared calculations showed significantly more cognitive and physical impairments compared to the group who did not experience dissatisfaction (34–92% vs 18–73%, p = 0.000 – p = 0.018). These differences between groups were significant for all variables except for ADL and walking ability. Similarly, a significant proportion of individuals who experienced dissatisfaction after sex also reported having increased cognitive impairments (except for mood changes) compared to those who did not experience dissatisfaction (44–91% vs 23–76%, p = 0.000 – p = 0.033) ().
Table 3. Decreased orgasm, dissatisfaction with orgasm, and dissatisfaction after sex in relation to cognitive functions, physical impairment, health/illness, and medication.
Arousal experiences among females and males
Among participants who had resumed sexual life, almost one-third (31%) of the females reported negative arousal experiences in terms of no or decreased lubrication during vaginal intercourse, while males reported arousal changes to a larger degree (). No or less common nocturnal erection was experienced by 62% (66/106) of males, and 48% (53/111) experienced no or less erection when aroused (data not shown in table), while erectile dysfunction (ED) in sexual activities was experienced by about half (51%, 57/112) of the male participants (). Significant differences appeared between those reporting ED and those who did not, concerning consequences after ABI; and mood changes showed the greatest difference (70% vs 42%, p = 0.002), followed by bowel/bladder symptoms (51% vs 24%, p = 0.003). Among females who reported decreased lubrication during vaginal intercourse, significantly more individuals also reported speaking difficulties (61% vs 28%, p = 0.015) and reduced initiative to sexual activities with a partner (73% vs 42%, p = 0.039), compared to those with intact lubrication ().
Table 4. Erectile dysfunction, early ejaculation, absent ejaculation, and decreased lubrication in relation to cognitive functions, physical impairment, health/illness, and medication1.
Binary logistic regression model for dissatisfaction with sexual desire
shows associations between dissatisfaction with sexual desire and impairments after ABI. Reduced initiative to sexual activity (p = 0.008), decreased orgasm (p = 0.026), and decreased satisfaction with sexual life (p = 0.001), were all associated with dissatisfaction with sexual desire in this model, while the other variables were not.
Table 5. Factors associated with dissatisfaction with sexual desire.
To summarize our results, chi-squared calculations revealed many significant differences between the groups reporting negative experiences regarding sexuality compared to those who did not. In other words, participants who reported more sexual dysfunctions also reported more cognitive and physical impairments.
Discussion
This study shows that many participants experienced changes in sexual life after ABI, such as reduced sexual desire, erectile dysfunction, early ejaculation, vaginal dryness during sexual intercourse, decreased orgasm, and decreased satisfaction with present sexual life. Our results demonstrate that sexuality is affected after ABI, which is consistent with previous studies (Citation8,Citation9,Citation11,Citation16,Citation18,Citation23,Citation25). In the general population in Sweden (not focused on ABI), sexual dysfunctions have been reported, such as ED (17%) which was higher with older age (65–84 years, 28%) (Citation33). In our study consisting of individuals with ABI, males reported ED to a much higher extent (51%). In the general population, 13% of females all ages reported vaginal dryness, while the number was 17% in the age-group 45–64 years (Citation33). Our study showed decreased lubrication at vaginal intercourse in 31%. In the general population physical impairments affecting sexuality were reported by 8% of females (in all age groups), 4% in younger males (30–44 years), and 16% among males aged 65–84 years. In our study, the findings of a generally high FIM physical and cognitive total score (32/35 and 86/91 respectively), as well as the high number reporting independence in ADL (90%) reveals that the participants’ subjective experiences of ADL measured by the questionnaire are comparable to the FIM score assessed at discharge from rehabilitation. This illustrates that the sample is characterized by generally high cognitive and physical functions after ABI, and yet a large proportion of participants reported decreased sexual function and satisfaction. Notably, our results revealed that participants experiencing changes in sexuality also experience more cognitive and physical consequences, which can be invisible to others. In comparison, the population-based study in Sweden (Citation33) showed that satisfaction with sexual life was 60%, and lowest among males in age-groups 16–29 years (32%) and 65–84 years (33%), while about half (53%) in our study reported decreased satisfaction with sexual life.
Sexual desire, cognitive problems, and initiation of sexual activity
Reduced sexual desire was reported almost twice (63%) as often in our study, compared to the number (34%) in Sander et al.’s U.S. study (Citation11), which focused on sexuality one year post-TBI. In the Swedish general population (not focusing on ABI), lack of sexual desire was reported by 20% among females and 8% among males (Citation33). In our study, more than half (54%) were also dissatisfied with their sexual desire and, among those, about 90% also experienced problems with memory, tiredness, concentration, and used any medication, compared to about 70% among those who were satisfied with their sexual desire. It is important to mention that among those in our sample who had resumed sexual life, about half (52%) also initiated less sexual activities with partner. The action of initiating sexual activity is not merely an act of choice but can be decreased due to lowered sexual desire or lowered ability to initiate activities in general due to the dysexecutive syndrome after ABI. Fatigue is also known for minimizing activity in general and can be one of the reasons why the participants did not initiate sexual activity with partners to the same extent. These results reflect those of Goldin et al. (Citation29): that fatigue was affecting sexual frequency, suggesting that fatigue should be further investigated in the context of sexuality rehabilitation after ABI. Moreno et al. (Citation6) also emphasized the importance of including both cognitive and behavioral aspects of the dysexecutive syndrome in sexual rehabilitation during brain injury rehabilitation. Our results show that invisible impairments have an impact on sexuality and thus that individuals should receive sexual rehabilitation irrespective of ABI impairment.
The holistic – Biopsychosocial perspective
In the binary logistic regression analysis, none of the invisible cognitive impairments (aside from reduced initiative to sexual activity – if that is considered a result from ABI cognitive consequences) showed significant associations with being dissatisfied with sexual desire, despite each of them showing significant differences in chi-squared calculations. These results might support the idea that none of the aspects are solely responsible for the dissatisfaction. Therefore, a holistic approach, including common consequences after ABI, needs to be considered in sexual rehabilitation, with a biopsychosocial perspective (Citation16,Citation38,Citation39). Sexual dysfunctions due to physical aspects such as ABI location cannot be totally neglected. Unfortunately, we had no information about ABI location, but results from the FIM at discharge from rehabilitation and the subjective perspectives from the questionnaire reveal that there are existing impairments in physical functions, such as bladder/bowel symptoms, which also could impact sexuality. For example, men with ED reported bladder/bowel symptoms twice as often as those without ED. Some impairments might overlap physical, psychological, and social domains, such as increased fatigue. Hence, sexual rehabilitation after ABI needs to address sexual functions in a biopsychosocial perspective also including neuropsychology and neurosexuality.
Invisible consequences and sexuality
In our study, consequences that can be invisible to others were significantly more often reported by those who also reported sexual dysfunction. For example, about 90% among those experiencing decreased orgasm and dissatisfaction after sex also reported decreased memory, increased tiredness, and decreased concentration, compared to about 70% among those who had intact orgasm experience and were sexually satisfied. Lingsom (Citation27) mentioned neither sexuality issues nor ABI, but the thoughts on invisible impairments and social interactions in general give an interesting and important perspective suitable for applying to sexuality after ABI. Even though our study group was not the one with the greatest persisting disabilities, they still experienced many sexual dysfunctions and dissatisfactions with sexual life, which can influence intimate relations negatively, especially if attempting to cover impairments due to ABI. Lingsom (Citation27) stated that non-disabled individuals might sense invisible impairments but not be able to point them out, while individuals with invisible impairments due to injury or illness might try to cover up the symptoms and give reasonable explanations for why they are, for example, tired (Citation27). Individuals with invisible impairments due to ABI may avoid social interactions, since maintaining a façade is exhausting. Impairments that are invisible to others can be difficult to cope with for anyone, but especially for the group of individuals with ABI – also in relation to sexuality and intimacy. The effort to maintain a façade can create a vicious circle where individuals cover their difficulties and healthcare professionals do not notice that something is challenging for the individual. Lingsom (Citation27) described this as trying to “pass.” The individual living with an invisible impairment might want to control the disclosure, and if it occurs unwillingly, the individual might not be in control (Citation27). This could happen in a new relationship or a new sexual practice. Our results showed that even though some relationships had ended (n = 40), new relationships were also established (n = 24). Ek (Citation23) reports that participants who received positive reactions when talking about their ABI in a new relationship felt more confidence in new interactions. Another reason to disclose the ABI could involve being judged according to their new condition, which in a sexual situation could lower the expectations and stress for the individual with ABI. The results from our study showed that almost one third (32%) experienced speaking difficulties, while almost twice as many (61%) among women with decreased lubrication at intercourse did so. This is an important issue for rehabilitation units to consider in sexual rehabilitation since individuals with ABI could be trained in how to communicate and disclose the ABI. According to Lingsom (Citation27), obstacles for the disclosure might include communication difficulties due to cognitive impairments or because it can be difficult to describe a dysfunction that the individual normally tries to cover. Anyone could experience difficulties expressing individual needs and desires regarding sexuality, and we believe that speaking difficulties among women in our study can make it even more difficult to specify intimate wishes in sexual interactions and thereby make it difficult to maintain arousal and lubrication. Lever and Pryor (Citation19) argued that young women post-stroke feared being disclosed as a person who had stroke, and Lingsom (Citation27) emphasized the importance of timing for disclosure. That is, in a sexual situation, if it occurs too early, a potential partner could withdraw, and if it occurs too late, a person might feel overlooked.
Limitations
Constructing a study-specific questionnaire has limitations. There were difficulties finding a suitable instrument containing all the aspects we wanted to study concerning physical, cognitive, and other invisible consequences of ABI in relation to sexuality. Therefore, we developed a study-specific questionnaire inspired by other instruments (Citation25,Citation43), interview studies, and earlier experiences of developing research questions, as well as clinical experience of the targeted sample. To reduce shortcomings, we validated the questionnaire through interview studies with individuals with ABI and partners (Citation23,Citation24). In addition, we utilized a peer group of researchers and PhD students, and five outpatients and six professionals from a brain injury rehabilitation unit, for validation. One limitation in this study is the lack of control group. However, there are some Swedish population-based studies (Citation33–35) focusing on sexuality in general population, and these brought some insight to aging and sexuality in general. Another question to consider is that individuals with an ABI may struggle to recall their former life situation, so how can any interpretations be concluded considering the risk of what Voormolen et al. refer to as “Good-old-days bias” (Citation45)? Voormolen et al. (Citation45) found inconsistent answers two weeks, three months, six months, and twelve months post-injury. However, in the early phase post-injury, individuals might still not have discovered or accepted remaining consequences, as stated by Verschuren et al. (Citation46). Therefore, our focus was on investigating remaining dysfunctions and satisfaction, and the selection criteria required participants not to be in their acute or sub-acute phase after ABI, but to have lived with the condition for some time. The participants were expected to respond based on their current situation. However, this includes a risk for recall bias due to memory deficits or lack of insight (anosognosia) regarding some consequences after ABI. The reports on sexual changes reflect their present experience of decreased function and satisfaction and might indicate a similar decrease among other individuals with an ABI. Due to the method of a self-administered questionnaire, only individuals sufficiently independent can participate, which implies that we cannot check whether everything is clearly understood and, unfortunately, we could not interview all the participants. However, this has been thoroughly discussed during the project, and both the inclusion criteria and the development of the questionnaire were conducted to facilitate participation. The response rate is still quite low (40%), but that was expected, considering the group studied, the sensitive subject, and the generally low response rates in contemporary questionnaire studies. Our results are specific to Swedish conditions, and generalizability to other cultures need to be cautiously considered. In Sweden, both education and health care, including rehabilitation, are mainly provided by the community, and not based on private actors. However, there is a risk that individuals that did not meet the inclusion criteria, for example, due to linguistic difficulties, also will be neglected in clinical practice. This study was mainly descriptive and cross-sectional, which decreases the possibility to make assumptions for how sexuality might change over time. Hence, a follow-up study using the same questionnaire would be interesting. Many questionnaire studies lack data on non-responders, but a strength of our study is the additional background characteristics of both participants and non-responders, acquired from the Web-Rehab register.
Conclusions
This study discloses that many participants experienced negative sexual changes after ABI, regarding sexual desire, arousal, orgasm, and satisfaction. Those who experience sexual changes also experience more cognitive and physical consequences, which can be invisible to others. Therefore, sexual rehabilitation should be integrated into brain injury rehabilitation, for individuals both with and without visible impairments. The study contributes to knowledge about the simultaneous occurrence of invisible impairments, decreased sexual functions, and decreased sexual satisfaction after ABI. Implications include further studies focusing on relational aspects and sexual rehabilitation. Hence, it is important to have a holistic approach in rehabilitation after ABI – one that includes sexuality issues. If professionals manage to raise this issue at an early-stage misconceptions can be clarified, minor problems can be solved, and avoidance or manifest problems can be prevented. This might lead to greater well-being for the individual. Our clinical recommendation is that sexuality issues need to be raised by professionals, not only when individuals with ABI present a problem. Further research should include follow-up studies and qualitative studies with an interdisciplinary approach focusing on invisible impairments.
Acknowledgments
We would like to thank all the participants, Svenskt register för rehabiliateringsmedicin, the professionals, and patients who participated in the pilot testing of the questionnaire, medical secretary Anette Bladh at Skåne University Hospital (for assistance with distributing questionnaires), and Ola Stjärnhagen (for statistical support).
Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
Notes
1. After material collection the Web-Rehab Sweden register has changed both name and website. The new name of the register is “Svenskt register för Rehabiliteringsmedicin”. However, we will use Web-Rehab register throughout the text.
References
- O’Shea A, Frawley P, Leahy JW, Nguyen HD. A critical appraisal of sexuality and relationships programs for people with acquired brain injury. Sex Disabil. 2020;38(1):57–83.doi:10.1007/s11195-020-09616-5.
- Etminan N, Chang HS, Hackenberg K, de Rooij NK, Vergouwen MDI, Rinkel GJE, Algra A. Worldwide incidence of aneurysmal subarachnoid hemorrhage according to region, time period, blood pressure, and smoking prevalence in the population: a systematic review and meta-analysis. JAMA Neurol. 2019;76(5):588–97.doi:10.1001/jamaneurol.2019.0006.
- Wafa HA, Wolfe CDA, Emmett E, Roth GA, Johnson CO, Wang Y. Burden of stroke in Europe: thirty-Year projections of incidence, prevalence, deaths, and disability-adjusted life years. Stroke. 2020;51(8):2418–27.doi:10.1161/STROKEAHA.120.029606.
- Dewan MC, Rattani A, Gupta S. Estimating the global incidence of traumatic brain injury. J Neurosurg 2019;130:1080–97.
- Dulhanty LH, Hulme S, Vail A, Patel HC, Tyson SF. The self-reported needs of patients following subarachnoid hemorrhage (SAH). Disabil Rehabil. 2020;42(24):3450–56.doi:10.1080/09638288.2019.1595748.
- Moreno JA, McKerral M. Relationships between risky sexual behaviour, dysexecutive problems, and mental health in the years following interdisciplinary TBI rehabilitation. Neuropsychol Rehabil. 2018;28(1):34–56.doi:10.1080/09602011.2015.1136222.
- Moreno A, Gan C, Zasler ND, Moreno A, Gan C, Zasler ND. Neurosexuality: a transdisciplinary approach to sexuality in neurorehabilitation. NeuroRehabilitation. 2017;41(2):255–59.doi:10.3233/NRE-001480.
- Strizzi J, Olabarrieta-Landa L, Olivera S, Valdivia Tangarife R, Andrés Soto Rodríguez I, Fernández Agis I, Arango-Lasprilla JC. Sexual function in men with traumatic brain injury. Sex Disabil. 2017;35(4):461–70.doi:10.1007/s11195-017-9493-9.
- Strizzi J, Olabarrieta Landa L, Pappadis M, Olivera SL, Valdivia Tangarife ER, Fernandez Agis I, Perrin PB, Arango-Lasprilla JC, et al. Sexual functioning, desire, and satisfaction in women with TBI and healthy controls. Behav Neurol. 2015;2015:1–7.
- Ponsford JL, Downing MG, Stolwyk R. Factors associated with sexuality following traumatic brain injury. J Head Trauma Rehabil. 2013;28(3):195–201.doi:10.1097/HTR.0b013e31828b4f7b.
- Sander AM, Maestas KL, Pappadis MR, Sherer M, Hammond FM, Hanks R. Sexual functioning 1 year after traumatic brain injury: findings from a prospective traumatic brain injury model systems collaborative study. Arch Phys Med Rehabil. 2012;93(8):1331–37.doi:10.1016/j.apmr.2012.03.037.
- Nilsson MI, Fugl-Meyer K, von Koch L, Ytterberg C, et al. Experiences of sexuality six years after stroke: a qualitative study. J Sex Med. 2017;14(6):797–803.doi:10.1016/j.jsxm.2017.04.061.
- Park J-H, Ovbiagele B, Feng W. Stroke and sexual dysfunction — a narrative review. J Neurol Sci. 2015;350(1–2):7–13.doi:10.1016/j.jns.2015.02.001.
- Pryor J, Lever S. Insights into the nature of female sexuality from the perspective of female stroke survivors. Disabil Rehabil. 2020;42(1):71–77.doi:10.1080/09638288.2018.1492635.
- Vikan JK, Nilsson MI, Bushnik T, Deng W, Elessi K, Frost-Bareket Y, Kovrigina E, Shahwan J, Snekkevik H, Åkesson E, et al. Sexual health policies in stroke rehabilitation: a multi national study. J Rehabil Med. 2019;51(5):361–68.doi:10.2340/16501977-2552.
- Moreno JA, Arango Lasprilla JC, Gan C, McKerral M. Sexuality after traumatic brain injury: a critical review. NeuroRehabilitation. 2013;32(1):69–85.doi:10.3233/NRE-130824.
- Anto-Ocrah M, Tiffany K, Hasman L, van Wijngaarden E. Mild traumatic brain injury/concussion and female sexuality, a scoping review of the literature. Inj Epi. 2020;7(1):1–13.doi:10.1186/s40621-020-0232-9.
- Grenier-Genest A, Gérard M, Courtois F, Moreno A, Gan C, Zasler ND. Stroke and sexual functioning: a literature review. NeuroRehabilitation. 2017;41(2):293–315.doi:10.3233/NRE-001481.
- Lever S, Pryor J. The impact of stroke on female sexuality. Disabil Rehabil. 2017;39(21):2011–20.doi:10.1080/09638288.2016.1213897.
- Vikan JK, Snekkevik H, Nilsson MI, Stanghelle JK, Geirdal AØ, Fugl-Meyer KS, et al. Sexual satisfaction and associated biopsychosocial factors in stroke patients admitted to specialized cognitive rehabilitation. Sexual Med. 2021;9(5):100424.doi:10.1016/j.esxm.2021.100424.
- Epprecht L, Messerli M, Samuel R, Seule M, Weber J, Fournier J-Y, Surbeck W, et al. Sexual dysfunction after good-grade aneurysmal subarachnoid hemorrhage. World Neurosurg. 2018;111:e449–e453.
- Layman DE, Dijkers MP, Ashman TA. Exploring the impact of traumatic brain injury on the older couple: ‘yes, but how much of it is age, I can’t tell you … ’. Brain Injury. 2005 Oct;19(11):909–23. doi:10.1080/02699050500109928.
- Ek A-S. Individual experiences of sexual life after an acquired brain injury - an interview study [ 1-year master student thesis, in Swedish]. Malmö: Malmö University; 2010.
- Ek A-S. Balancing between individual and relational needs - a qualitative study of partners’ perspectives on sexual life after acquired brain injury [ 2-year master student thesis, in Swedish]. Malmö: Malmö University; 2011.
- Kreuter M, Dahllöf AG, Gudjonsson G, Sullivan M, Siösteen A, et al. Sexual adjustment and its predictors after traumatic brain injury. Brain Injury. 1998;12(5):349–68.doi:10.1080/026990598122494.
- Fugl-Meyer KS, Nilsson MI, Von Koch L, Ytterberg C, et al. Closeness and life satisfaction after six years for persons with stroke and spouses. J Rehabil Med. 2019;51(7):492–98.doi:10.2340/16501977-2566.
- Lingsom S. Invisible Impairments: dilemmas of concealment and disclosure. Scandinavian J Disabil Res. 2008;10(1):2–16.doi:10.1080/15017410701391567.
- Sjögren K, Fugl-Meyer AR. Sexual problems in hemiplegia. Disabil Rehabil. 1981;3(1):26–31.
- Goldin Y, Cantor JB, Tsaousides T, Spielman L, Gordon WA, et al. Sexual functioning and the effect of fatigue in traumatic brain injury. J Head Trauma Rehabil. 2014;29(5):418–26.doi:10.1097/HTR.0b013e31829cf76d.
- Bivona U, Antonucci G, Contrada M, Rizza F, Leoni F, Zasler ND, Formisano R. A biopsychosocial analysis of sexuality in adult males and their partners after severe traumatic brain injury. Brain Injury. 2016;30(9):1082–95.doi:10.3109/02699052.2016.1165867.
- Lemieux L, Cohen-Schneider R, Holzapfel S. Aphasia and sexuality. Sex Disabil. 2001;19(4):253–66.doi:10.1023/A:1017953308761.
- Verschuren JE, Geertzen JH, Enzlin P, Dijkstra PU, Dekker R, et al. People with lower limb amputation and their sexual functioning and sexual well-being. Disabil Rehabil. 2015;37(3):187–93.doi:10.3109/09638288.2014.913704.
- SRHR 2017. Pub Health Agency Sweden. 2019. Available from. https://www.folkhalsomyndigheten.se/publikationer-och-material/publikationsarkiv/s/sexuell-och-reproduktiv-halsa-och-rattigheter-i-sverige-2017/?pub=60999.
- Stentagg M, Skär L, Berglund JS, Lindberg T. Cross-sectional study of sexual activity and satisfaction among older adult’s ≥60 years of age. Sexual Med. 2021 Apr;9(2):100316. doi:10.1016/j.esxm.2020.100316.
- Beckman N, Waern M, Gustafson D, Skoog I. Secular trends in self reported sexual activity and satisfaction in Swedish 70 year olds: cross sectional survey of four populations, 1971-2001. Br Med J. 2008;337(7662):151–54.doi:10.1136/bmj.a279.
- Sjögren K, Fugl-Meyer AR. Adjustment to life after stroke with special reference to sexual intercourse and leisure. J Psychosom Res. 1982;26(4):409–17.doi:10.1016/0022-3999(82)90015-0.
- Latella D, Maggio MG, De Luca R, Maresca G, Piazzitta D, Sciarrone F, Carioti L, Manuli A, Bramanti P, Calabro RS, et al. Changes in sexual functioning following traumatic brain injury: an overview on a neglected issue. J Neurosurgical Soc Australasia. 2018;58:1–6.
- Engel GL. The need for a new medical model: a challenge for biomedicine. J Interprof Care. 1989;4(1):37–53.
- Borrell-Carrio F, Suchman AL, Epstein RM. The biopsychosocial model 25 years later: principles, practice, and scientific inquiry. Annals of Family Medicine. 2004;2(6):576–82.doi:10.1370/afm.245.
- Svenskt register för rehabiliteringsmedicin, in Swedish [cited 2022 24 october]. Available from: https://svereh.registercentrum.se
- Stibrant-Sunnerhagen K, Tölli A, Lannsjö M. Diagnosgrupper för NASS, in Swedish: svenskt register för rehabiliteringsmedicin; 2016 [cited 2022 october 24]. Available from: https://registercentrum.blob.core.windows.net/svereh/r/Diagnosgrupper-for-NASS-BJl4IZZz7Y.pdf
- Stineman MG, Shea JA, Jette A, Tassoni CJ, Ottenbacher KJ, Fiedler R, Granger CV. The functional Independence measure: tests of scaling assumptions, structure, and reliability across 20 diverse impairment categories. Arch Phys Med Rehabil. 1996;77(11):1101–08.doi:10.1016/S0003-9993(96)90130-6.
- Stolwyk RJ, Downing MG, Taffe J, Kreutzer JS, Zasler ND, Ponsford JL. Assessment of sexuality following traumatic brain injury: validation of the brain injury questionnaire of sexuality. J Head Trauma Rehabil. 2013;28(3):164–70.doi:10.1097/HTR.0b013e31828197d1.
- Elmerstig E, Wijma B, Swahnberg K. Prioritizing the partner’s enjoyment: a population-based study on young Swedish women with experience of pain during vaginal intercourse. Journal of Psychosomatic Obstetrics & Gynecology. 2013;34(2):82–89.doi:10.3109/0167482X.2013.793665.
- Voormolen DC, Cnossen MC, Spikman J, Polinder S, Iverson GL, de Koning M, van der Naalt J. Rating of pre-injury symptoms over time in patients with mild traumatic brain injury: the good-old-days bias revisited. Brain Injury. 2020;34(8):1001–09.doi:10.1080/02699052.2020.1761563.
- Verschuren JEA, Enzlin P, Geertzen JHB, Dijkstra PU, Dekker R. Sexuality in people with a lower limb amputation: a topic too hot to handle? Disabil Rehabil. 2013;35(20):1698–704.doi:10.3109/09638288.2012.751134.