?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Introduction
Repeat sport-related concussion (SRC) is anecdotally associated with prolonged recovery. Few studies have examined repeat concussion within the same athlete. We sought to explore differences in symptom burden and recovery outcomes in an individual athlete’s initial and repeat SRC.
Methods
A retrospective within-subject cohort study of athletes aged 12–23 years diagnosed with two separate SRCs from 11/2017–10/2020 was conducted. Primary outcomes were initial symptom severity and time-to-symptom-resolution. Secondary outcomes included return-to-learn (RTL) and return-to-play (RTP) duration.
Results
Of 868 athletes seen, 47 athletes presented with repeat concussions. Median time between concussions was 244 days (IQR 136–395). Comparing initial to repeat concussion, no differences were observed in time-to-clinic (4.3 ± 7.3vs.3.7 ± 4.6 days, p = 0.56) or initial PCSS (26.2 ± 25.3 vs. 30.5 ± 24.1, p = 0.32). While a difference was observed in time-to-symptom resolution between initial/repeat concussion (21.2 ± 16.3 vs. 41.7 ± 86.0 days, p = 0.30), this did not reach statistical significance. No significant differences were observed in time-to-RTL (17.8 ± 60.6 vs. 6.0 ± 8.3 days, p = 0.26) and RTP (33.2 ± 44.1 vs. 29.4 ± 39.1 days, p = 0.75). Repeat concussion was not associated with symptom resolution on univariate (HR 1.64, 95% CI 0.96–2.78, p = 0.07) and multivariable (HR 0.85, 95% CI 0.49–1.46, p = 0.55) Cox regression.
Conclusion
No significant differences in symptom duration and RTP/RTL were seen between initial/repeat concussion.
Introduction
Sport-related concussion (SRC) is a growing public health concern, with approximately 25% of children and adolescents participating in organized sports reporting previous concussion (Citation1,Citation2). Demographics and medical history factors associated with increased concussion incidence and prolonged symptom resolution include female sex (Citation3,Citation4), attention-deficit hyperactivity disorder (ADHD) (Citation5), learning disabilities (Citation6), pre-injury migraines (Citation7), and psychiatric history (Citation8). Furthermore, prior concussion history is among the strongest risk factors for sustaining a repeat concussion and a prolonged recovery (Citation3,Citation9–11). In a 2021 surveillance study, approximately 7% of adolescents reported a history of two or more concussions (Citation1). Prior literature has shown that athletes with previous concussions have increased initial symptom burden compared to those without concussion histories (Citation12). The effect of concussion history on symptom resolution is mixed, with several studies showing athletes with prior concussions take longer to recover from a subsequent concussion, while other studies did not find this effect (Citation13–17).
Although the effects of multiple concussions are well-known, few studies have sought to track recovery from initial and repeat concussion within the same athlete, the ideal way to control for measurable and unmeasurable confounding variables. Investigating clinical differences between an initial and repeat concussion in the same athlete provides an additional level of control and may help elucidate the potential cumulative effects of multiple concussive injuries. A prior within-subject study of nine athletes with repeat SRC reported delayed visual-kinesthetic integration and coherence recovery after an athlete’s second concussion compared to their first injury (Citation18). Furthermore, a within-subject study examining 78 adolescents following their first and second concussion measured neurocognitive performance, persistent post-concussion symptoms, and recovery time (Citation19). The study found worse visual motor speed after the second concussion, but no difference in initial symptom burden, other cognitive test scores, or recovery time (Citation19). Given the limited number of studies using this analytic strategy and the fact that both prior studies only compared athletes after their first and second lifetime concussions, our objectives were to: 1) compare the primary outcomes of initial symptom burden and time to symptom resolution between the initial and repeat concussion, and 2) evaluate secondary outcomes of return-to-learn (RTL) and return-to-play (RTP). Based on prior literature citing the negative predictor of a concussion history (Citation12–16,Citation20,Citation21), we hypothesized that repeat concussion within the same athlete would be associated with more severe symptom burden and prolonged recovery.
Methods
Study design and athlete selection
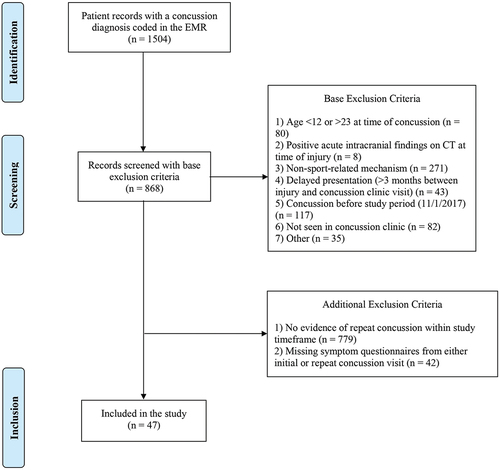
A retrospective, within-subject cohort study was conducted using data from the Vanderbilt Sports Concussion Center (VSCC) registry. Institutional Review Board (IRB 192,033) ethical approval was obtained and the study was deemed to be exempt with consent not required. Athletes diagnosed with a concussion and seen by VSCC providers between 11/2017–10/2020 were screened for eligibility (n = 1,504). Concussion diagnosis was defined in accordance with International Classification of Diseases (ICD)-9 and ICD-10 concussion codes (850.* and S06.0X**, respectively), and post-concussion syndrome (310.2 and F07.81). Inclusion criteria were defined as athletes 12–23 years old presenting to VSCC within 3 months of initial injury with subsequently diagnosed SRC based on the most recent Concussion in Sport Group (CISG) guidelines (n = 868) (Citation22). Athletes without evidence of a second concussion within the timeframe of the study documented in the electronic medical record were furthermore excluded (n = 779), as were those with missing symptom questionnaires from either initial or repeat concussion visits (n = 42). An athlete flow diagram detailing inclusion and exclusion criteria is provided in .
Data collection and definitions
A manual review and extraction of provider notes in the electronic medical record was performed; data were extracted into a secure REDCap database (Citation23,Citation24). Past medical history, including diagnoses of ADHD, learning disabilities, and personal history of migraines and psychiatric illness, was obtained upon review of provider clinic notes at initial presentation and review of any recorded diagnoses in the patient’s electronic medical record. Family history of migraine and psychiatric illness was obtained via self-report on clinic intake questionnaires. Concussion history was based on a self-report intake questionnaire that assessed prior medically-diagnosed concussions. The initial concussion was operationally defined as the first concussion the athlete was treated for in our clinic; it did not have to be their first lifetime concussion. A repeat concussion was defined as additional concussion in the same athlete during the study timeframe. Time between concussion was calculated between the date of initial and repeat concussion. Symptom severity was measured by Post-Concussion Symptom Scale (PCSS), a 22-item self-report measure recording symptom severity on a 7-point Likert scale of severity from 0–6, administered at time of initial presentation and at each subsequent encounter (Citation25). Loss of consciousness and/or amnesia was defined as present if mentioned in the initial concussion visit note or self-reported on an athlete-completed intake questionnaire. Time to clinic was defined as days from injury to clinic presentation.
Outcomes
The primary outcomes included: 1) initial symptom severity, measured via initial PCSS at time of presentation, and 2) time to symptom resolution, defined as declaration in a clinic note by a trained concussion specialist that an athlete had recovered, or when the athlete’s PCSS returned to baseline/zero. Time to symptom resolution was measured as the number of days between date of concussion and symptom resolution. To reach symptom resolution, either the treating physician, neuropsychologist, or certified athletic trainer must have documented in the medical record that all symptoms had resolved or returned to pre-injury baseline status. For athletes lost to follow-up prior to achieving symptom resolution, we measured the length-of-care episodes (i.e., days between initial VSCC visit and last follow-up) and time to dropout (i.e., days between injury and last visit). Secondary outcomes included RTL and RTP. RTL was defined as the number of days between date of concussion and when a athlete returned to any school activities, including half-days. RTP was defined as the number of days between date of concussion and initial graduated return to physical activities.
Statistical analysis
Descriptive statistics were performed on demographics, medical history, injury characteristics, and postinjury outcomes. Categorical variables were presented as percentage frequencies, while all continuous variables except time between concussions were presented as mean ± standard deviation. Time between concussions was presented as median with interquartile range (IQR) given non-normal distribution. Given the novelty of the study design, an a priori power analysis using a small-to-medium effect size of 0.35 was conducted, resulting in a sample size requirement of 67 athletes to achieve 0.8 power at an alpha of 0.05 on a two-tailed paired samples t-test (G*Power Version 3.1.9.6). Within-group comparisons were analyzed via Chi-square statistics and paired t-tests. Pooled Cohen’s d standardized mean differences were obtained to estimate effect size.
A univariable Cox regression model was performed for factors hypothesized to affect symptom resolution, with results reported as hazard ratios and 95% confidence intervals. The event was defined as symptom resolution; data were censored at the last visit to clinic where the athlete was still symptomatic and deemed not recovered. Subsequently, a multivariable Cox regression model to determine the effect of repeat concussion on time to symptom resolution was performed. Covariates added to the model were determined a priori based off prior literature and included sex (Citation4), time to clinic presentation (Citation26), and initial PCSS (Citation27). Subgroup analysis of athletes with no history of previous concussion with first and second concussion within the study timeframe was subsequently conducted to assess any potential effect of previous concussion; for each outcome, only patients with data available from both the initial and repeat concussion were analyzed. Statistical significance was set a priori at p < 0.05.Analyses were performed using SPSS 27 (IBM, Armonk, NY).
Results
Demographics and medical history
The final cohort included 47 athletes with repeat concussions. Of these athletes, 62% (n = 29) were treated for their first and second lifetime concussions in our program, 19% (n = 9) were treated for second and third lifetime concussions, and 19% (n = 9) had at least two prior concussions before presenting to clinic for treatment of additional concussions. Most athletes were White (n = 38, 81%) and the majority were male (n = 29, 62%). Nearly all athletes in the cohort were covered by private insurance (n = 42, 89%) and just over half attended public school (n = 26, 55%). Median time between initial concussion and repeat concussion was 244 days (IQR 136–395). Demographics and medical history are summarized in .
Table 1. Demographics for patients incurring initial and repeat concussion.
Injury characteristics
Mean age at injury for initial injury was 15.8 ± 1.9 years and 16.7 ± 1.7 years for repeat concussion [t(46)=-9.76, p < 0.001]. Athletes initially presented to similar care settings following initial and repeat concussion [(6) = 4.30, p = 0.64] and there was no difference in sport distribution [
(11) = 4.65, p = 0.95]. There were no statistical differences in the rate of amnesia or loss of consciousness (). Moreover, no statistical difference was observed in mean time to clinic for initial and repeat concussion [4.3 ± 7.3 vs. 3.7 ± 4.6 days, t(46) = 0.59, p = 0.56, Cohen’s pooled d=-0.09].
Table 2. Injury characteristics and outcomes.
Outcomes
For the primary outcome of initial symptom severity, while initial concussion exhibited a lower symptom burden at presentation than repeat concussion [26.2 ± 25.3 vs. 30.5 ± 24.1, t(38)=-1.00, p = 0.32, pooled Cohen’s d = 0.15, less than small effect size], this difference did not reach statistical significance. Additionally, although initial concussion was associated with a shorter time to symptom resolution by approximately 20 days [n = 34, 21.2 ± 16.3 days, n = 27, 41.7 ± 86.0 days, t(19)=-1.06, p = 0.30, pooled Cohen’s d = 0.18, less than small effect size], this difference was not statistically significant. Of note, symptom resolution data were not available for 13 (28%) of athletes following their initial concussion and 20 (43%) of athletes following their repeat concussion.
Regarding secondary outcomes of RTL and RTP, there was no statistically significant difference in mean time to RTL [n = 43, 17.8 ± 60.6 days vs. n = 40, 6.0 ± 8.3 days, t(35) = 1.14, p = 0.26, pooled Cohen’s d=-0.13, less than small effect size] or RTP [n = 37, 33.2 ± 44.1 days vs. n = 26, 29.4 ± 39.1 days, t(24) = 0.33, p = 0.75, pooled Cohen’s d=-0.05, negligible effect size] between initial and repeat concussion. Lastly, no statistically significant difference in length-of-care episodes [n = 46, 27.4 ± 46.0 days vs. n = 46, 45.0 ± 125.8 days, t(44)=-0.87, p = 0.20, pooled Cohen’s d = 0.09, negligible effect size] between the initial and repeat concussion was observed. summarizes injury characteristics and general outcomes for the cohort.
Sub-group analysis of first and second concussion
A subgroup analysis of athletes sustaining first and second lifetime concussion within the cohort (n = 29) revealed similar results; outcome data were not available for 7 athletes following their first concussion (24%) and 11 athletes following their second concussion (38%). There was no significant difference in initial symptom burden [23.3 ± 28.0 vs. 28.8 ± 23.6, t(23)=-0.97, p = 0.34, pooled Cohen’s d = 0.18, less than small effect size) – and for those who had outcome data, no differences were observed in time to symptom resolution between initial and repeat concussion [17.5 ± 14.5 vs. 25.0 ± 43.3 days, t(13)=-0.72, p = 0.49, pooled Cohen’s d = 0.18, less than small effect size]. Similarly, our secondary outcome analysis revealed no difference between time to RTL, RTP, or length-of-care episode. Furthermore, no difference in time to clinic presentation was observed. Subgroup analysis of athletes experiencing first and second concussion is presented in Supplementary Table S1.
Cox regression of factors associated with symptom resolution
summarizes univariate Cox regression of factors related to symptom resolution in both the total cohort and subgroup. Compared to initial injury, a repeat concussion was not significantly associated with prolonged symptom resolution [Hazard Ratio (HR) = 1.64, 95% CI = 0.96–2.78, p = 0.07]. Demographical variables such as sex were not found to predict longer symptom duration. Increased time to clinic presentation (HR 0.98, 95% CI 0.94–1.02, p = 0.18) did not significantly predict prolonged time to symptom resolution. Higher PCSS at initial presentation was associated with prolonged symptom resolution (HR 0.98, 95% CI 0.97–0.99, p < 0.001). No differences were observed in subgroup analysis.
A multivariable Cox regression analysis of factors associated with symptom resolution () showed that higher initial PCSS (HR 0.97, 95% CI 0.96–0.99, p < 0.001) and longer time to clinic presentation (HR 0.94, 95% CI 0.90–0.99, p = 0.01) each uniquely predicted greater symptom duration. Repeat concussion status was not significantly associated with predicting symptom resolution (HR 0.85, 95% CI 0.49–1.46, p = 0.55) (). Again, no differences were observed in subgroup analysis of athletes diagnosed with first and second concussion ().
Figure 2. Multivariable Cox regression survival analysis for factors associated with symptom resolution. (A) Initial and repeat concussion. (B) First and second concussion only.
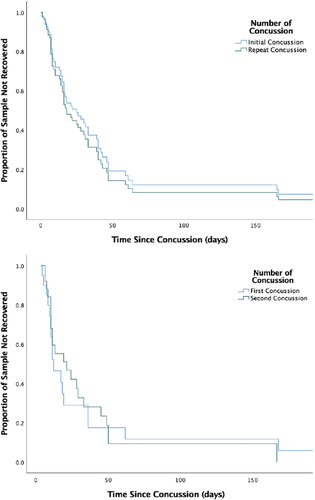
Table 3. Univariate Cox regression of factors related to symptom resolution.
Table 4. Multivariable Cox regression analysis of factors associated with symptom resolution.
Discussion
Our study assessed initial symptom burden and time to symptom resolution between initial and repeat concussion within the same athlete and revealed similar injury characteristics and outcomes between the two concussions. The present study is the first to investigate the concussion recovery outcomes beyond an athlete’s first and second lifetime concussion using a within-subjects design. Initial symptom burden was marginally higher following the repeat concussion compared to initial concussion, although this difference did not reach statistical significance. Furthermore, though time to symptom resolution was longer in the repeat concussion by approximately 20 days, these results, along with the secondary outcomes of RTL and RTP, were not statistically significant due to small sample size. Additionally, all effect size values (which are traditionally less affected by small samples) were less than small (d < 0.20) or negligible, suggesting that our null findings may not be due to limited sample size. In a multivariable Cox regression analysis adjusting for variables related to recovery (gender, time to presentation, initial symptom burden), repeat concussion was not significantly associated with prolonged symptom resolution compared to initial concussion. Furthermore, subgroup analysis of athletes with no prior concussion history revealed similar injury characteristics and outcomes between those with a history of concussions prior to the study’s initiation.
Initial symptom burden and symptom resolution
Our study did not show statistically significant differences in initial symptom burden or time to symptom resolution between initial and repeat concussion. While extensive literature on multiple concussions exists, less is known regarding recovery following repeat concussion in the same individuals. Previous between-group studies in large cohorts of athletes have evaluated the effect of concussion history on symptom burden and recovery with mixed results (Citation10,Citation18,Citation20). These between-group cohort studies may be influenced by confounding variables between groups. A within-group study found that athletes took longer to present to clinic (9.9 vs. 6.9 days, p = 0.02), had worse sleep symptoms, and worse visual motor speed during their initial clinical visit following their first concussion; however, no difference in total initial symptom burden (29.7 vs. 27.3 initial total PCSS, p = 0.48) or recovery time (65.8 vs. 69.1 days, p = 0.68) was observed (Citation19). These findings are largely consistent with our study. In contrast to the previous study, athletes presenting to our clinic did not exhibit a statistically significant difference in time to presentation between initial and repeat concussion (4.3 vs. 3.7 days, p = 0.56), an important confounder in initial PCSS scores. While a decreased time to presentation for repeat injury may be reflective of improved concussion education and awareness following treatment for initial concussion, it is important to note that athletes in our study presented to clinic in about half the time as the previous study (approximately 4 vs. 7–10 days), suggesting that our athletes may have a baseline awareness and urgency to present to clinic early on. The effect sizes evaluating differences in time to clinic and initial symptom burden were less than small/negligible, suggesting little difference between initial and repeat concussion beyond statistical significance.
While the difference in time to symptom recovery in our cohort did not reach statistical significance, the raw data show that mean time to symptom resolution was approximately three weeks longer following the repeat concussion (41.7 ± 86.0 days) than initial concussion (21.2 ± 16.3 days). While the lack of statistical significance could be related to our sample size, it is noteworthy to discuss that the high standard deviation for days to symptom resolution following the repeat concussion may be driven by a few outliers in the data. Further, the effect size difference between the initial and repeat concussions was less than small (d = 0.18), further suggesting that it is important to interpret the three-week difference in the raw data with caution. Finally, it is important to recognize that the Cox regression models used the data for individuals who achieved symptom resolution in our clinic and those who were followed in our clinic while they were symptomatic but eventually dropped out of care before achieving symptom resolution, thus maximizing the sample size. Further inquiry with larger cohorts of within-group subjects is indicated to determine whether this difference in time to symptom resolution can be replicated.
Return-to-learn and return-to-play
Our study showed no statistical difference in time to RTL or RTP between initial and repeat concussion in athletes sustaining multiple concussions. Our study is the first to examine RTL through a within-subjects study of athletes with repeat concussion. Although RTL was slightly longer following initial concussion compared to repeat concussion, no statistically significant difference was noted and the effect size was negligible. While recent literature has expanded on RTL duration and accommodations following concussion (Citation28,Citation29), few studies have examined the effect of repeat concussion on RTL (Citation30). In a study of non-sport acute concussions in children with a median age of 11.5 years, those with repeat concussions more frequently reported lower grades one year after returning to school compared to those without repeat injury (14% vs. 3%, p < 0.001) (Citation30). In addition, the athletes in our study displayed no difference between each concussion in RTP duration. A study of high school athletes sustaining multiple concussions within a single sport season found that those with recurrent concussion experienced prolonged RTP (Citation31). While the results of this study are compelling, median time between initial and recurrent concussion was 21 days in this study; in contrast, median time between initial and repeat concussion among our athletes was 244 days. Several studies have investigated time between concussions as a factor in concussion recovery (Citation20,Citation31–33), with shortened time between concussion associated with prolonged RTP and medical disqualification (Citation20,Citation31). Furthermore, athletes in the previous study endorsed loss of consciousness more frequently following recurrent concussion than initial concussion (6.8% vs. 1.7%, p = 0.04), suggesting that the nature of injuries may have been different. Conversely, a study examining RTP in male ice hockey players with varying concussion histories found that those with 1–2 previous concussions initiated RTP earlier than those with no concussion history (10.7 vs. 11.5 days) (Citation32). Further within-subject studies with a larger sample size are indicated to examine the effect of repeat concussion on RTP.
Limitations
Our study has several important limitations. First, our interpretation of symptom resolution was based on data extracted from provider notes. If the concussion clinic provider did not explicitly state that symptom resolution occurred, a PCSS score of zero or equivalent to the athlete’s baseline with other clinical data (e.g., documentation the athlete started the RTP protocol) was used as a proxy. However, this represents clinic-assessed symptom resolution when the athlete may have truly achieved symptom resolution days before this appointment, thus leading to a potential overestimation of this value. In addition, while our study is the largest of its kind, these data are from a single-institution’s specialty concussion center, which limits the generalizability of the study. Although our sample size was limited and our analyses may have been underpowered to find a true difference between groups; thus, there is a possibility that our interpretation of non-significant p-values were based on false negative results. We employed effect size analyses in addition to traditional significance testing since effect sizes are not influenced by small sample sizes. Regardless of the sample size of our or future studies, the magnitude of the effect sizes in this study may suggest that true effect likely did not exist. Further research with a multi-institutional prospective cohort with a larger sample size achieving adequate power are indicated to validate the preliminary findings of our study. Furthermore, these multi-institutional studies may be important since many adolescents with an SRC do not present to a specialty concussion center. In addition, our sample may include more complex athletes more likely to have delayed recovery. Finally, understanding the variability in recovery times in cases with similar injury characteristics and identical presenting risk factors remains an avenue of active exploration. Further investigation into this variability in recovery using a within-subjects design is warranted.
Conclusions
When comparing symptoms and the course of initial and repeat concussions in the same athlete, no differences in injury characteristics and outcomes were observed. Repeat concussion was not associated with prolonged symptom resolution.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Veliz P, McCabe SE, Eckner JT, Schulenberg JE. Trends in the prevalence of concussion reported by US adolescents, 2016-2020. JAMA. 2021;325(17):1789–1791. doi:10.1001/jama.2021.1538.
- Refakis CA, Turner CD, Cahill PJ. Sports-related concussion in children and adolescents. Clin Spine Surg. 2017;30(5):191–96. doi:10.1097/BSD.0000000000000451.
- Tsushima WT, Siu AM, Ahn HJ, Chang BL, Murata NM. Incidence and risk of concussions in youth athletes: comparisons of age, sex, concussion history, sport, and football position. Arch Clin Neuropsychol. 2018;34(1):60–69. doi:10.1093/arclin/acy019.
- Zuckerman SL, Apple RP, Odom MJ, Lee YM, Solomon GS, Sills AK. Effect of sex on symptoms and return to baseline in sport-related concussion: clinical article. J Neurosurg Pediatr. 2014;13(1):72–81. doi:10.3171/2013.9.PEDS13257.
- Aggarwal SS, Ott SD, Padhye NS, Schulz PE. Sex, race, ADHD, and prior concussions as predictors of concussion recovery in adolescents. Brain Inj. 2020;34(6):811–19. doi:10.1080/02699052.2020.1740942.
- Harmon KG, Drezner JA, Gammons M, Guskiewicz KM, Halstead M, Herring SA, Kutcher JS, Pana A, Putukian M, Roberts WO, et al. American medical society for sports medicine position statement: concussion in sport. Br J Sports Med. 2013;47(1):15–26. doi:10.1136/bjsports-2012-091941.
- Terry DP, Huebschmann NA, Maxwell BA, Cook NE, Mannix R, Zafonte R, Seifert T, Berkner PD, Iverson GL. Preinjury migraine history as a risk factor for prolonged return to school and sports following concussion. J Neurotrauma. Published online August 2, 2018. doi:10.1089/neu.2017.5443.
- Legarreta AD, Brett BL, Solomon GS, Zuckerman SL. The role of family and personal psychiatric history in postconcussion syndrome following sport-related concussion: a story of compounding risk. J Neurosurg Pediatr. 2018;22(3):238–43. doi:10.3171/2018.3.PEDS1850.
- Gerberich SG, Priest JD, Boen JR, Straub CP, Maxwell RE. Concussion incidences and severity in secondary school varsity football players. Am J Public Health. 1983;73(12):1370–1375. doi:10.2105/ajph.73.12.1370.
- Guskiewicz KM, Weaver NL, Padua DA, Garrett WE. Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28(5):643–650. doi:10.1177/03635465000280050401.
- Schulz MR, Marshall SW, Mueller FO, Yang J, Weaver NL, Kalsbeek WD, Bowling JM. Incidence and risk factors for concussion in high school athletes, North Carolina, 1996-1999. Am J Epidemiol. 2004;160(10):937–44. doi:10.1093/aje/kwh304.
- Ellis M, Krisko C, Selci E, Russell K. Effect of concussion history on symptom burden and recovery following pediatric sports-related concussion. J Neurosurg Pediatr. 2018;21(4):401–08. doi:10.3171/2017.9.PEDS17392.
- Corwin DJ, Zonfrillo MR, Master CL, Arbogast KB, Grady MF, Robinson RL, Goodman AM, Wiebe DJ. Characteristics of prolonged concussion recovery in a pediatric subspecialty referral population. J Pediatr. 2014;165(6):1207–15. doi:10.1016/j.jpeds.2014.08.034.
- Eisenberg MA, Andrea J, Meehan W, Mannix R. Time interval between concussions and symptom duration. Pediatrics. 2013;132(1):8–17. doi:10.1542/peds.2013-0432.
- Miller JH, Gill C, Kuhn EN, Rocque BG, Menendez JY, O’Neill JA, Agee BS, Brown ST, Crowther M, Davis RD, et al. Predictors of delayed recovery following pediatric sports-related concussion: a case-control study. J Neurosurg Pediatr. 2016;17(4):491–496. doi:10.3171/2015.8.PEDS14332.
- Guideline for Concussion/Mild Traumatic Brain Injury & Prolonged Symptoms. [accessed 2022 Feb 15]. https://braininjuryguidelines.org/concussion/fileadmin/pdf/Concussion_guideline_3rd_edition_final.pdf.
- Iverson GL, Gardner AJ, Terry DP, Ponsford JL, Sills AK, Broshek DK, Solomon GS. Predictors of clinical recovery from concussion: a systematic review. Br J Sports Med. 2017;51(12):941–48. doi:10.1136/bjsports-2017-097729.
- Slobounov S, Slobounov E, Sebastianelli W, Cao C, Newell K. Differential rate of recovery in athletes after first and second concussion episodes. Neurosurgery. 2007;61(2):338–344. discussion 344 doi:10.1227/01.NEU.0000280001.03578.FF.
- French J, Jennings S, Eagle SR, Collins MW, Kontos AP. A within-subjects comparison of clinical outcomes for patients’ first and second concussions. J Head Trauma Rehabil. 2021;36(2):114–19. doi:10.1097/HTR.0000000000000612.
- Castile L, Collins CL, McIlvain NM, Comstock RD. The epidemiology of new versus recurrent sports concussions among high school athletes, 2005–2010. Br J Sports Med. 2012;46(8):603–10. doi:10.1136/bjsports-2011-090115.
- Morgan CD, Zuckerman SL, King LE, Beaird SE, Sills AK, Solomon GS. Post-concussion syndrome (PCS) in a youth population: defining the diagnostic value and cost-utility of brain imaging. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg. 2015;31(12):2305–2309. doi:10.1007/s00381-015-2916-y.
- McCrory P, Meeuwisse W, Dvořák J, Echemendia RJ, Engebretsen L, Feddermann-Demont N, McCrea M, Makdissi M, Patricios J, Schneider KJ, et al. Consensus statement on concussion in sport-the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838–47. doi:10.1136/bjsports-2017-097699.
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi:10.1016/j.jbi.2008.08.010.
- Kontos AP, Elbin RJ, Schatz P, Covassin T, Henry L, Pardini J, Collins MW. A revised factor structure for the post-concussion symptom scale: baseline and postconcussion factors. Am J Sports Med. 2012;40(10):2375–84. doi:10.1177/0363546512455400.
- Eagle SR, Puligilla A, Fazio-Sumrok V, Kegel N, Collins MW, Kontos AP. Association of time to initial clinic visit with prolonged recovery in pediatric patients with concussion. J Neurosurg Pediatr. 2020;26(2):165–70. doi:10.3171/2020.2.PEDS2025.
- Meehan WP, Mannix R, Monuteaux MC, Stein CJ, Bachur RG. Early symptom burden predicts recovery after sport-related concussion. Neurology. 2014;83(24):2204–2210. doi:10.1212/WNL.0000000000001073.
- Purcell LK, Davis GA, Gioia GA. What factors must be considered in ‘return to school’ following concussion and what strategies or accommodations should be followed? A systematic review. Br J Sports Med. 2019;53(4):250–250. doi:10.1136/bjsports-2017-097853.
- O’Neill JA, Cox MK, Clay OJ, Johnston JM, Novack TA, Schwebel DC, Dreer LE. A review of the literature on pediatric concussions and return-to- learn (RTL): implications for RTL policy, research, and practice. Rehabil Psychol. 2017;62(3):300–23. doi:10.1037/rep0000155.
- van Ierssel J, Ledoux AA, Tang K, Correll R, Yeates KO, Gioia G, Freedman SB, Sangha G, Boutis K, Beer D, et al. Symptom burden, school function, and physical activity one year following pediatric concussion. J Pediatr. 2021;228:190–8.e3.
- Currie DW, Comstock RD, Fields SK, Cantu RC. A paired comparison of initial and recurrent concussions sustained by US high school athletes within a single athletic season. J Head Trauma Rehabil. 2017;32(2):90–97. doi:10.1097/HTR.0000000000000240.
- Echlin PS, Tator CH, Cusimano MD, Cantu RC, Taunton JE, Upshur REG, Czarnota M, Hall CR, Johnson AM, Forwell LA, et al. Return to play after an initial or recurrent concussion in a prospective study of physician-observed junior ice hockey concussions: implications for return to play after a concussion. Neurosurg Focus. 2010;29(5):E5. doi:10.3171/2010.9.FOCUS10210.
- McCrea M, Broglio S, McAllister T, Zhou W, Zhao S, Katz B, Kudela M, Harezlak J, Nelson L, Meier T, et al. Return to play and risk of repeat concussion in collegiate football players: comparative analysis from the NCAA concussion study (1999–2001) and CARE consortium (2014–2017). Br J Sports Med. 2020;54(2):102–109. doi:10.1136/bjsports-2019-100579.