 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Dominant narratives of prescription opioid misuse (POM) in the U.S. have portrayed it as an issue primarily affecting White communities. In this study we explore POM as reported in data from the 2015 National Survey on Drug Use and Health, using an intersectional multilevel analysis of individual heterogeneity and discriminatory accuracy (MAIHDA). We map the risk of POM through a series of multilevel models with individuals (N = 43,409) nested within strata formed by the intersections of gender, race/ethnicity, income, and age. We find meaningful heterogeneity between and within strata. The ten strata with the greatest risk for POM were comprised of individuals identifying as White, African American, and non-White Hispanic, and included individuals of low, medium, and high income. We uncover intersections of social position with high risk for POM that are often excluded from dominant narratives, including young high-income African American women. Intersectional approaches are essential for advancing our understanding of health inequalities and unfolding epidemics such as that of POM in the U.S.
Background
The ongoing opioid epidemic in the U.S. has drawn considerable attention nationally and internationally, and was declared a ‘public health emergency’ in March 2017 (Davis, Citation2017). The impact of opioid misuse remains a cause for alarm in the U.S., and though prescribing rates have declined since 2010 (Schuchat et al., Citation2017), current rates remain three times higher than in 1999, and opioid-involved deaths are still on the rise (Guy Jr. et al., Citation2017). In 2017, 67.8% of drug overdose deaths involved an opioid (Scholl et al., Citation2019), and more than 35% of opioid-related mortality involved prescription opioids (CDC, Citation2018). Opioid misuse accounts for substantial health, social, and economic costs in the U.S. (Bonnie et al., Citation2017; Manchikanti et al., Citation2012; Schuchat et al., Citation2017).
Since the early 2000s, much of the rhetoric in the media surrounding the epidemic has framed opioid misuse as a problem affecting primarily middle-class, rural and suburban White individuals (Netherland & Hansen, Citation2016). This coding of the epidemic as ‘White’ corresponds with marked differences in the perception and handling of POM compared to heroin use, which is historically coded as Black. POM has been met with reduced stigma, a greater willingness to provide resources for treatment and support, and a reduced desire to pursue punitive measures (Hansen & Netherland, Citation2016; Laguna, Citation2018; Netherland & Hansen, Citation2017). While less punitive responses are to be celebrated, their apparent race- and class-based motivations are deeply troubling, particularly given the historic and contemporary criminalization of related substance use under the guise of the ‘War on Drugs’ (Bechteler & Kane-Willis, Citation2017; Netherland & Hansen, Citation2016; Provine, Citation2007).
While in absolute terms the dominant narratives surrounding the ‘whiteness’ of the opioid epidemic appear warranted – according to a recent CDC Morbidity and Mortality Weekly Report (Seth et al., Citation2018) 79% of all opioid-related deaths (33,450 of 42,249 deaths in 2016) were among non-Hispanic White people – this obscures two important points. First, the rate of opioid misuse and deaths among non-White individuals is also high; in 2016 there were 17.5 deaths among non-Hispanic White people, 10.3 deaths among non-Hispanic Black people, and 6.1 deaths among Hispanic people per 100,000 in the population. The impact of the epidemic on racial/ethnic minorities has, however, been largely overlooked. Second, findings about the distribution of the epidemic across the population tend to be reported in purely additive terms, with comparisons made only by race/ethnicity, or by gender, or by age (Alexander et al., Citation2018; Nicholson & Ford, Citation2018; Seth et al., Citation2018). This framing obscures the intersectional nature of the epidemic – with perhaps numerous, heavily affected social strata being rendered invisible. As a consequence, the needs of heavily affected populations may be under-recognized and unmet, while the social processes that generate these needs and disparities go unchallenged.
Meanwhile, recent critiques highlight that the dominant narrative of POM in the U.S. as a problem of the White middle-class does not reflect the reality of the phenomenon (Bechteler & Kane-Willis, Citation2017; Nicholson & Ford, Citation2018). This is particularly important to investigate as racialized narratives about substance misuse and racial bias in healthcare have implications in terms of access to pain management as well as treatment for substance use disorders (Monnat, Citation2017; Nicholson & Ford, Citation2018).
Netherland and Hansen (Citation2017) suggest that public health could be an ‘alternate ideology to a medical or punitive frame – one that may be able to encompass important structural issues, such as race, geography, and class’ (p. 19). Our present analysis seeks to encompass several of these structures. By grouping individuals within strata comprised of intersections of gender, race/ethnicity, income, and age, and assessing the variation within and between those strata, we attempt to reframe substance misuse from an individual medical or punitive problem and conceptualize it within structural contexts. Although the included social categorizations are not the only structural factors that could be associated with POM, they do represent major axes of marginalization and inequality in U.S. society and are frequently evaluated in social epidemiology and intersectional scholarship (Berkman & Kawachi, Citation2000; Collins & Bilge, Citation2016; Crenshaw, Citation1989; Krieger, Citation2011; Schultz & Mullings, Citation2006). While these axes are often measured individually, in line with critical theories of population health such as ecosocial theory (Krieger, Citation2011), social production, and political economy of health (Conrad & Kern, Citation1981; Doyal, Citation1979), we regard these as proxies for social positions within complex, interlocking systems of inequality and the social experiences that these positions likely entail. Observed inequalities in POM across strata are therefore understood to be an end result of intersectional social processes operating at several ecological levels.
We argue that the question of POM in the U.S. is highly suitable for an intersectional approach, which enables us to explore the heterogeneous distribution of the epidemic, to interrogate dominant narratives, and to illuminate intersections of social position that may have been overlooked so far.
Intersectionality in population health
Intersectionality theory posits that individuals are positioned within interlocking structures of privilege and marginalization based on power dynamics surrounding social categorizations such as gender, race, and class. This framework was originally articulated in order to account for the ways in which women of colour were discriminated against within a legal system that failed to address the intersection of both womanhood and blackness (Crenshaw, Citation1989). In more recent years, intersectionality has been applied as a theoretical framework within social epidemiology (Axelsson Fisk et al., Citation2018; Bauer, Citation2014; Evans, Citation2015; Evans et al., Citation2018; Green et al., Citation2017; Merlo, Citation2018; Wemrell et al., Citation2017a). In this study, we apply an intersectional framework to position individuals within intersecting social systems that shape lived experiences with implications for population health.
McCall (Citation2005) has famously identified three major approaches within the intersectionality literature: the anti-categorical, which critiques the use of social categorizations on the grounds that they fail to recognize the inherent fluidity of such labels and that using (or reproducing) them may serve to reify structural inequity; the intercategorical, which provisionally accepts social categorizations in order to identify and act on existing inequities; and the intracategorical, which provides a nuanced focus on particular intersections of marginalization. To date, the intercategorical approach has been the one most frequently used in social epidemiological research, with the focus of such studies being the health effects of social strata membership (Sen et al., Citation2009; Veenstra, Citation2013). Anti-categorical research has been used more rarely in population health research because studies of this type, typically qualitative in orientation, tend to focus on the meaning of the social categorizations or identity labels themselves, or on the nature of lived experiences of individuals at particular social locations, rather than their effects on health outcomes.
Recently, however, an expanded view of the anti-categorical approach has been proposed, suggesting an anti-categorical interpretation of health effects (Merlo, Citation2018; Wemrell et al., Citation2017b) and using anti-categorical interpretations in conjunction with intercategorical ones to examine population health (Mulinari et al., Citation2018). These studies propose operationalizing intercategorical complexity through measures of differences between-group average risk, such as odds ratios (ORs) or risk ratios (RRs), and anti-categorical complexity through measures of discriminatory accuracy (DA) which gauges the ability of a certain category to correctly discriminate between people with or without the outcome of interest, which we have done (Merlo, Citation2018; Mulinari et al., Citation2018; Wemrell et al., Citation2017b). In this study, we apply both intercategorical and anti-categorical approaches, enabling improved discernment of the extent to which the intersectional strata shape the distribution of POM.
Descriptive intersectional scholarship has rightly been critiqued on the grounds that merely describing intersectional patterns in dependent variables without calling attention to the social processes that give rise to inequalities runs the risk of blunting intersectionality’s ‘critical edge and transformative aims’ (May, Citation2015, p. 141). We argue that our approach maintains such a critical edge for two reasons. First, as argued by Evans (Citation2019), the main issue with descriptive intersectional studies is not their descriptive nature per se, but that they tend to be atheoretical in framing and interpretation, and therefore fail to draw attention to (and critique) the social processes that generate observed intersectional patterns. By drawing on critical theories of population health (Conrad & Kern, Citation1981; Doyal, Citation1979; Krieger, Citation2011) and interpreting observed inequalities accordingly, we aim to highlight the underlying social processes driving the POM epidemic. Second, as noted, the dominant narratives about the opioid epidemic affect a form of erasure through which the experiences and needs of minority populations are left under-recognized and unaddressed. Our purpose is to challenge and complicate this simplistic and exclusionary narrative.
Social processes and inequalities in the opioid epidemic
Both pain management and substance use are complex, related phenomena influenced by a variety of social processes. In the case of POM, it is necessary to consider a variety of factors, including: (1) the likelihood of individuals becoming patients requiring pain management, (2) factors influencing physician assessment of pain in their patients (which can affect prescribing rates and dosages), (3) contextual influences in the lives of individuals relying on opioids for pain management that may determine, through stress and coping pathways (Crutchfield & Gove, Citation1984), their likelihood of developing POM, (4) individuals’ agency and ability to negotiate with their physicians for adequate pain management, (5) micro-contextual factors such as group norms, perceptions of drug-related risks, effects and behaviours and local drug availability (Stanistreet, Citation2005; Yedinak et al., Citation2016) and (6) macro-environmental factors such as state drug policy (Yedinak et al., Citation2016) and interests and practices of pharmaceutical companies. Importantly, social processes such as these will operate differently across intersectional social strata. We would expect, as a consequence, that this would result in substantial inequalities in POM across the population. In this study, we aim to establish the extent of such inequalities, while identifying intersectional social locations which are particularly exposed to social processes needing to be further elucidated and addressed.
Following the work of Jones et al., (Citation2016) and as recently described in explicitly intersectional terms by Evans (Citation2015), Evans et al. (Citation2018), Axelsson Fisk et al. (Citation2018) and Hernández-Yumar et al. (Citation2018), we carry out an intersectional multilevel analysis of individual heterogeneity and discriminatory accuracy (MAIHDA) (Merlo, Citation2018). This methodological approach enables an improved mapping of the possible heterogeneity of the opioid epidemic in the U.S. population, with regards to the social categorizations of gender, race/ethnicity, income, and age. This multilevel approach conceptualizes individuals (at level-1) as nested within intersections of social position (level-2) and therefore treats social strata labels as analogous to other social contexts (such as schools or neighbourhoods) (Evans et al., Citation2018). Treating strata labels as contexts rather than as individual-level characteristics addresses the critiqued tendency in quantitative intersectional scholarship (Choo & Ferree, Citation2010; Ferree & Hall, Citation1996), as well as in social epidemiology at large (Krieger, Citation2011; O’Campo & Dunn, Citation2012; Wemrell et al., Citation2016), to locate the cause(s) of interest within individuals rather than at a structural and processual level. We believe that examining the opioid epidemic in explicitly intersectional terms through a multilevel model will enable us to more suitably capture the complexity of POM in the U.S.
Aims
Using a large, nationally representative data set and applying an intersectional MAIHDA approach we examine the intersections of gender, race/ethnicity, income, and age in order to provide a nuanced mapping of POM in the adult U.S. population. In doing so, we challenge the dominant narrative that characterizes POM as a White, middle-class rural/suburban problem.
Methods
Data
This study was based on the public use dataset from the 2015 National Survey on Drug Use and Health (NSDUH-2015), a cross-sectional interview survey conducted annually by the Substance Abuse and Mental Health Services Administration. The public use file containing 57,146 individuals, representative of the U.S. non-institutionalized civilian population, was subsampled using the statistical disclosure limitation method Micro Agglomeration, optimal probabilistic Substitution, optimal probabilistic Subsampling, and optimal sampling weight Calibration (MASSC) from the full survey sample of 68,073 individuals, aged 12 and above at the time of the survey (Center for Behavioral Health Statistics and Quality, Citation2016). The survey was based on an independent multistage area probability sample from all 50 states and the District of Colombia, and included household populations as well as residents of non-institutional group quarters and individuals without permanent residence, accounting for approximately 97% of the total U.S. population (Center for Behavioral Health Statistics and Quality, Citation2016). The characteristics of the survey are explained in detail elsewhere (Center for Behavioral Health Statistics and Quality, Citation2016). After excluding those with a missing outcome (N = 342) and those under age 18 (N = 13,395), the study sample includes 43,409 individuals.
Ethical considerations
NSDUH-2015 data have been de-identified and are publicly available. The NSDUH-2015 was approved by the Research Triangle Institute’s Institutional Review Board.
Prescription opioid misuse
The binary outcome prescription opioid misuse (yes vs. no) was based on the respondent’s answer to a survey question asking them to indicate which, if any, prescription opioid was used most recently in a way not directed by a physician in the past year. Respondents who did not indicate misuse of any of the prescription opioids listed were coded as ‘no’. Indication of misusing any of the listed opioids was coded as ‘yes.’ Heroin and other non-prescription opioids and opiates were not included in the outcome variable.
Intersectional social strata
Sociodemographic proxies of social identity and social process were used to construct intersectional strata. These were gender, race/ethnicity, income and age.
Gender was categorized as male or female. While the absence of a non-binary or other gender category is a limitation, male and female were the only categories included in the survey.
Race/ethnicity was self-identified according to the following NSDUH categories: Non-Hispanic White, Non-Hispanic Black/African American, Hispanic, and those with other identities (‘Other racial/ethnic minorities’), which included Non-Hispanic Native American or Alaska Native, Native Hawaiian or Pacific Islander, Asian, or more than one race/ethnicity. Further stratification of this final category would have yielded strata with an insufficient number of individuals for analysis.
Income was divided into three categories: high, medium and low. These were defined using the federal poverty thresholds for 2015 (U.S. Bureau of the Census, Citation2015) for different household compositions and defined as high income (400% and greater of poverty threshold), medium income (200–399% of poverty threshold) and low income (less than 200% of poverty threshold).
Age was recoded from the survey categories into three groups: 18–29, 30–49 and 50+ years. These capture three distinct life phases: early adulthood, mid-adulthood, and older adulthood.
The study includes 72 intersectional social strata constructed through the matrix of all combinations of the above defined categories of each social identity/process variable: gender (2 categories), race/ethnicity (4 categories), income (3 categories) and age (3 categories).
Analysis
Multilevel logistic regression models
As described in detail previously (Axelsson Fisk et al., Citation2018; Evans et al., Citation2018; Hernández-Yumar et al., Citation2018), an intersectional MAIHDA analysis models two-level hierarchical data with individuals at level 1 nested within intersectional strata at level 2. We modelled the risk of POM using three two-level random-intercept logistic regression models, described below. We estimated each model using Markov chain Monte Carlo (MCMC) methods. For a complete summary of the statistical methods, see the online Supplement.
Model 1: simple intersectional
Model 1 included a random intercept for the intersectional strata, but no covariates, which can be written as
where denotes the probability of opioid misuse for individuals in stratum
(
),
denotes the intercept, and
denotes the stratum-specific random effect. We then calculated the absolute risk (AR) of POM for each stratum by transforming the predicted logit or log-odds of POM into the corresponding predicted probability.
The AR values allow us to ascertain the risk of POM for each stratum, in absolute terms. We used the MCMC chains for and
to construct 95% credible intervals (CI) for these probabilities to summarize the statistical uncertainty surrounding these predictions.
As this is a logistic model, we used a latent response approach to calculate the Variance Partition Coefficient (VPC) (Goldstein et al., Citation2002).
In the context of our study, the VPC is defined as the proportion of variation in the probability of POM that can be attributed to differences between strata, and is a measure of DA. A low VPC indicates that little of the observed variation in POM can be attributed to the strata level, meaning that the DA of the intersectional strata is low, while a high VPC indicates that the DA of the intersectional strata is high. We further plotted a receiver operating characteristic curve (ROC) and report the area under the curve (AUC) as a complementary assessment of DA (see Supplement).
Model 2: partially-adjusted intersectional
In a series of intermediate models, we made separate adjustments for each of the four identity/process variables used to construct the strata. We calculated the Proportional Change in Variance (PCV) between each of the versions of model 2 and model 1. The PCV indicates the share of the overall variation in POM across strata that can be accounted for by the given variable included in the model.
A low PCV value indicates that the identity/process variable in question does not have a substantial impact on the variation in POM across the strata, and thus that the incremental DA is small.
Model 3: intersectional interaction
The final model serves two purposes. First, it provides us with an assessment of interaction effects beyond the additive effects of the four identity/process variables included in the strata, thus allowing us to identify strata with higher or lower risk than would be expected based on the additive effects of the variables. Second, the inclusion of each of the variables as covariates allows us to obtain mutually adjusted ORs for the main effects of gender, race/ethnicity, income, and age.
This model simultaneously included all four identity/process variables as covariates with fixed-effect regression coefficients but with no interaction variables between them. Following the methods outlined by Axelsson Fisk et al. (Citation2018), we decomposed the probability of POM for each stratum into the part due to main effects of the covariates, and that due to interactions between the covariates. If there were no interactions between the four variables, the inclusion of the covariates as main effects would explain all between-stratum variance; the stratum-level random effects would be 0. If this were not the case, the residual stratum-level random effects could be interpreted as the result of two- and higher-way interaction effects between the variables of the intersectional strata, assuming no relevant variables were omitted from the model.
By subtracting the main effects probability from the total probability for each stratum, we obtained the probability of POM accounted for by two-way and higher interactions between the variables. We interpret this value as the absolute risk due to interaction (ARI). A positive ARI means that individuals in that stratum have a higher risk than expected based on the simple addition of the risks conveyed by the variables that define the stratum (i.e., hazardous or synergistic interaction), while a negative ARI means a lower risk than expected (i.e., protective or antagonistic interaction). We also calculated 95% CIs for all model 3 ARs as well as ARIs (see Supplementary Table S1).
Software
All models were run in MLwiN 3.02 (Charlton et al., Citation2017; Rasbash et al., Citation2017) called from Stata 14.1 using the runmlwin command (Leckie & Charlton, Citation2013). Estimation was performed using MCMC methods (Browne, Citation2017), with diffuse prior distributions for all parameters. Quasilikelihood methods were used to provide starting values for all parameters. For each model, the burn-in length was 10,000 iterations and the monitoring chain length was 50,000 iterations, with thinning every 10 iterations. The code used for the models is provided in the Supplement.
Results
Summaries of models 1 (Simple Intersectional), 2 (Partially-adjusted Intersectional), and 3 (Intersectional Interaction) are presented in , including the VPC (expressed as a %), the PCV (expressed as a %), and the regression coefficients (expressed as ORs).
Table 1. Summaries for each of the models. Model 1, the unadjusted random intercept model; each version of model 2, adjusted independently for gender, race/ethnicity (the category ‘Other racial/ethnic minorities’ has been abbreviated to ‘Other REM’), income, and age; model 3, the main effects model which adjusts simultaneously for all four dimensions. Regression coefficients are exponentiated and presented as odds ratios (ORs) with 95% credible intervals (CIs). Variance, variance partitioning coefficient (VPC), and proportional change in variance (PCV) are reported as percentages.
maps the ARs and 95% CIs for all intersectional strata in model 1. presents these predicted percentages side-by-side with the observed percentages of POM. We found that the three strata with the highest predicted absolute risk (AR) for POM were White men with low income aged 18–29 (stratum 7: AR 13.04%, 95% CI 11.59–14.53%); African American women with high income aged 18–29 (stratum 46: AR 10.24%, 95% CI 5.04–17.56%); and White men with medium income, aged 30–49 (stratum 8: AR 9.56, 95% CI 7.77–11.50). The highest observed percentage of opioid misuse pertained to stratum 46 (16%). This stratum included a small number of individuals (N = 50) compared to most other strata, thus its predicted probability is shrunk towards the population average (Steele, Citation2008) to a greater extent than that of larger strata.
Table 2. Model 1 predictions of absolute risk (AR) for all intersectional strata, with 95% credible intervals (CIs). Results are sorted by the four dimensions which form the intersectional strata: gender, race/ethnicity, income, and age.
Figure 1. Model 1 predictions for opioid misuse with 95% credible intervals for all intersectional strata ranked from least to greatest absolute risk (AR), reported as predicted probability (%).
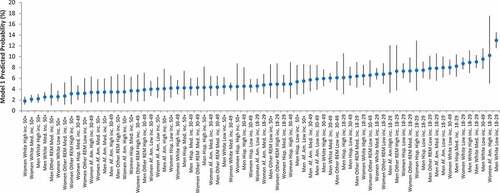
We found that the lowest predicted ARs for POM pertained to White women with high income, aged 50 and above (stratum 39: AR 1.81%, 95% CI 1.17–2.63%); White women with medium income, aged 50 and above (stratum 42: AR 2.16%, 95% CI 1.50–2.94%); and White men with high income, aged 50 and above (stratum 3: AR 2.23%, 95% CI 1.48–3.12%).
Model 1 had a VPC of 7.54% (), with an AUC value of 0.64 (), suggesting moderate clustering of individual risk by stratum and thus a low DA of these strata. While the moderate VPC indicates meaningful variation (i.e. inequalities) between strata with respect to POM, the low AUC indicates that the intersectional categorizations are not sufficient to discriminate with particularly strong accuracy between those who misuse prescription opioids and those who do not. Together, these measures indicate that while substantial within-strata heterogeneities exist, the intersectional strata meaningfully capture variation in POM, which calls for a theoretical exploration of the possible social processes underlying the observed distribution.
Figure 2. Receiver operator characteristic curve (ROC) constructed from predicted probabilities of model 1. The area under the curve (AUC) is an indicator of the discriminatory accuracy of the strata for predicting risk of misusing prescription opioids.
Among the strata with the ten highest predicted AR values, six included White race/ethnicity, three included African American race/ethnicity, and one included non-White Hispanic race/ethnicity. Seven strata included men. Five strata included low income, three included medium income, and two included high income. Eight included ages 18–29, and two included ages 30–49. This is indicative of a complexity that was not evident through the presentation of ORs for each of the intersectional variables alone ().
In the four different versions of model 2, we adjusted for each of the four variables separately. While the PCV values indicate the proportion of the between-stratum variance that is explained by each of the respective sets of covariates, only one model yielded a PCV value greater than 10%: the age-adjusted model (2D), which explained 69.8% of the between-stratum variance (). Thus, among the four variables, age has by far the strongest DA with regards to the outcome. Indeed, we see that in the unadjusted model (model 1) eight out of the ten strata with the highest ARs included those aged 18–29, while among the ten strata with the lowest ARs, none included those aged 18–29, and nine of ten included those aged 50 and above ().
In the other three versions of model 2 (), when adjusted for gender, race/ethnicity, and income, the VPC values changed minimally from that of model 1 (7.54%), to 7.04%, 8.02%, and 7.04%, respectively. This is consistent with the stratum-specific findings in which we observed greater variation among categories of gender, race/ethnicity, and income than in that of age among the ten strata with the highest AR and similarly in the ten strata with the lowest AR.
Model 3 showed a VPC of 0.48%, indicating very small residual interaction effects, with a PCV of 94% indicating that nearly all between-strata variation was explained by adjusting for the main effects of the four identity/process variables (). This suggests that 94% of the variation between the ARs of different strata was due to additive effects of gender, race/ethnicity, income and age and that only 6% was due to two-way or higher-order interaction effects between these variables. The main effects of each variable are presented as ORs (), and indicate lower risk for women, higher risk for White individuals, and higher risk for low income individuals and those aged 18–24. However, as discussed above, greater complexity was evident among the intersectional, stratum-specific results.
By decomposing the model 3 predicted probabilities, we were able to isolate interaction effects of the identity/process variables. The CIs of all 72 stratum-specific interaction effects included 0, so none of the predicted probabilities deviated significantly from what one would expect based only on the main effects of the four variables. The three most positive and most negative interaction effects with 95% CIs are presented in .
Table 3. The three strata with the most positive and most negative interaction effects. These were obtained by subtracting the model 3 main effects predicted percentage (PP) from the total effects PP. A positive interaction effect indicates a higher PP than that predicted by additive effects alone, thus a more hazardous interaction, while a negative interaction PP effect indicates a protective interaction. (the category ‘Other racial/ethnic minorities’ has been abbreviated to ‘Other REM’).
Of the three strata with the most positive (hazardous) interaction effects, all were low income and White. Of the three strata with the most negative (protective) interaction effects, all were low income, aged 18–29, and non-White. The complete results of model 3 are presented in the supplementary (Table S1).
Discussion
Applying an intersectional MAIHDA approach enabled us to provide a more nuanced description of the distribution of POM in the adult U.S. population. Our findings add complexity to the narrative of the opioid epidemic as primarily White and male by illuminating other intersections of social identity and position where POM is common.
By carrying out a descriptive analysis of POM within an explicitly contextual, intersectional framework, we seek to counter the trend in epidemiology to focus on individual risk factors rather than underlying mechanisms (Lofters & O’Campo, Citation2012) or fundamental causes of particular health outcomes (Krieger, Citation2011; Link & Phelan, Citation1995). We have operationalized this by nesting individuals within intersectional strata, allowing for an assessment of the risk attributable to variation between and within strata. By recognizing the high degree of heterogeneity of risk within social strata we seek to counteract the potential stigmatization or stereotyping (Olofsson et al., Citation2014) conveyed by current intercategorical approaches.
Complicating current narratives
Previous studies have found White race/ethnicity (Han et al., Citation2017; Seth et al., Citation2018) and younger age (Kolodny et al., Citation2015) to be associated with higher risk of opioid misuse, though there is substantial heterogeneity of risk factors (King et al., Citation2014) and overlap between categorizations (Han et al., Citation2017). We found that White men and women had both the highest and the lowest AR for POM, while the differentiating factor was age (with those aged 18–29 having higher AR). Meanwhile, of the ten social strata with highest risk, four included non-White identities.
Other recent studies have found that rates of prescription opioid use (Harrison et al., Citation2018) and misuse (Nicholson & Ford, Citation2018) have become more similar between Black and White individuals. Our intersectional approach deepens our understanding of the demographic patterning of POM and reveals intersections of social position with high AR of that would otherwise have been concealed. For example, among the strata with the ten highest ARs for POM were high-income African American women, aged 18–29, and as well as Hispanic and African American men with low and medium income, aged 18–29. Thus, simple racial and economic categorizations erase the complexity of the distribution of POM in the U.S., and could potentially contribute to mistargeted interventions, unequal distribution of resources, and unjust racialized narratives surrounding substance use.
While the variable to which the greatest between-strata variation can be attributed was age (as indicated by the PCV in model 2), we found significant heterogeneity within the strata (as demonstrated by the moderate VPC of model 1). This further indicates a need for caution when making categorical statements about the nature of POM. Thus, the intersectional MAIHDA approach allows us to highlight interlocking dimensions of social position that have an increased risk for POM, while subverting dominant narratives about the face of the epidemic.
Embodiment of social conditions
The ecosocial theory of disease distribution posits that we come to embody, biologically, our societal and ecological circumstances, and that this explains observed distributions of health outcomes at the population level (Krieger, Citation2011). With regards to POM, we have observed high AR within social strata comprised by different intersections of gender, race/ethnicity, income, and age, though age accounted for the largest share of between-stratum variation.
Young, high-income, African American women were found to have the second highest AR, yet individuals within this stratum have not been included in the mainstream narrative surrounding the opioid epidemic. This leads us to consider what mechanisms may be driving this pattern. As outlined previously, such factors may include physician assessment of pain and micro- and macro-contextual factors. For instance, racism has been identified as a fundamental cause of health inequity (Phelan & Link, Citation2015), and Feagin and Bennefield (Citation2014) articulate the ways in which systemic racism can shape the relationship between physicians and patients of colour, leading to unjust differences in health. Studies have shown that there is under-treatment of pain in people of colour (Green et al., Citation2003), and racial disparities in opioid prescriptions (Singhal et al., Citation2016). One potential explanation for why young, high-income African American women have high POM rates is that as physicians become more aware of their own racial biases and seek to reduce this under-management of pain in minority populations, they will be more likely to select young and high SES minority women as the recipients of this increase in pain management. Alternatively, the under-treatment of pain and under-prescribing of opioids to minority populations could provide motivation for some individuals to self-medicate for pain, which would be categorized as misuse of a prescription opioid even if it is not problematic use in the conventional sense. Young, high-income African American women, therefore, may be more comfortable disregarding directives for use that will be insufficient for management of pain. These are merely possible explanations for the observed patterns. Results from these descriptive analyses invite deeper, qualitative investigations of the uncovered patterns in order to improve our understanding of the lived experiences of individuals occupying particular social positions.
Race/ethnicity and class – narratives of substance use
Historically, substance use has been met by either criminalization/vilification or empathy/therapeutic support, depending on the narrative surrounding the identity of those using the substance. From opium in the late 1800s to crack cocaine in the 1970s, dominant narratives have often framed a particular social group as the scapegoat for social decay associated with drug use (Laguna, Citation2018; Murakawa, Citation2011; Provine, Citation2007). However, when a substance has been associated with the White middle class, it is deemed more acceptable, and individuals with substance use disorders are seen as deserving of empathy and treatment rather than criminalization (Laguna, Citation2018; Provine, Citation2007; Reinarman, Citation1994). POM follows this trend, with the current framing of a public health crisis differing markedly from the rhetoric of criminality that surrounded heroin use in communities of colour (Bechteler & Kane-Willis, Citation2017; Netherland & Hansen, Citation2016). The differential treatment of substance use when a particular substance is associated with a privileged position can be used to uphold systems of power, and in the case of opioids, to preserve whiteness (Netherland & Hansen, Citation2017). The heterogeneity we have observed in the risk for POM complicates this narrative of whiteness. While unidimensional analysis is not only insufficient to fully map patterns of disease distribution, in cases such as that of POM, it may also serve to uphold systems of inequity.
Intercategorical and anti-categorical approaches
Inherent tensions arise when attempting to identify health inequities based on social position while preventing stigmatization and stereotyping of population groups. As many scholars have noted, simplistic categorizations in public health, and racial categorizations in particular (Gravlee, Citation2009; Kaufman & Cooper, Citation2010; Krieger, Citation2003; Valles, Citation2012) may be ethically problematic and are insufficient to account for social complexity. Additionally, measures of difference between group averages typically used in epidemiology do not account for the variance within and overlaps between categorizations (Merlo et al., Citation2017; Mulinari et al., Citation2018). We believe that by using an intercategorical intersectional approach alongside an anti-categorical one, operationalized through measurement of differences in average between strata as well as of the DA of those strata, epidemiological inquiry can resolve some of the existing tensions between needing to uncover health inequity and to avoid perpetuating stigma and stereotypes about presumably risky identities (Olofsson et al., Citation2014). Thus, measures of DA combined with assessments of group averages can provide insight into how an intercategorical approach should be weighed against an anti-categorical one, in relation to the given outcome (Merlo, Citation2018; Wemrell et al., Citation2017b). In this case, we found evidence supporting an intercategorical approach based on the intersections of gender, race/ethnicity, income, and age, to insufficiently capture POM in the adult U.S. population. Evoking Marmot’s concept of proportionate universalism (Carey et al., Citation2015; Marmot & Bell, Citation2012), and the related argument that health actions should be universal rather than targeted, but be of a scale and intensity that is proportionate to the level of disadvantage, our results suggest that while a population level approach appears appropriate to curb opioid misuse, the scale and intensity of efforts should be balanced with attention toward of the cross-sections of the population with the greatest risk.
Limitations
This study has several limitations. Although the survey data were nationally representative, we do not account for geographical regional variation in POM patterns, as further stratification would have made the sample too small, though there have been noted differences in the distribution of opioid risk in different regions and cities (Bechteler & Kane-Willis, Citation2017) and between urban and rural environments (Rigg & Monnat, Citation2015). Another significant limitation is that due to our sample size, we were not able to stratify the ‘other racial/ethnic minorities’ category further. Native American and Alaska Native communities have been heavily impacted by the opioid epidemic (Seth et al., Citation2018). Categorizations of race/ethnicity are problematic in and of themselves, as some respondents may have trouble identifying which category they belong to, definitions are not historically constant, and some racial/ethnic categories may not be mutually exclusive (Kaplan, Citation2014). Additionally, the data do not capture high-risk groups such as incarcerated individuals and homeless individuals. Due to the racial disparity in the U.S. prison population, and the fact that racialized health disparities have been identified in those populations, risk for POM may not be represented by these data (Nowotny et al., Citation2017). Furthermore, estimates used for income level are based on a single poverty scale for all individuals, which may have overestimated the effective income class for some states, as we did not have access to data about which state each respondent was from. Finally, the NSDUH-2015 survey relies on self-reported drug use, and thus self-reporting bias could lead to under- or over-reporting.
Conclusions
Addressing the opioid epidemic necessarily involves careful consideration of complex social issues. For instance, reporters (Cronrath, Citation2018; Peterson & Armour, Citation2018) and researchers (Netherland & Hansen, Citation2016) alike have noted the differential framings of the opioid epidemic (coded as White) and the heroin epidemic (coded as Black/minority), and consequently the inequitable treatment of those affected (the former being treated as a health issue deserving of treatment and compassion, the latter as a form of social deviance deserving of criminalization). Similarly, the relationship between equitable pain management and opioid over-prescription – one of the main drivers of the current epidemic – takes on thorny racial overtones. There is a substantial and persistent treatment gap between White individuals and non-White minorities, with Black individuals being significantly less likely to receive prescriptions for pain management even after adjustment for severity of pain (Ezenwa et al., Citation2006; Monnat, Citation2017; Mossey, Citation2011; Pletcher et al., Citation2008; Singhal et al., Citation2016). In tension with calls for equitable treatment and the framing of pain management as a health justice issue are the high rates of POM and death that result from opioid over-prescription.
By taking an intersectional perspective on the opioid epidemic we highlight gaps in the dominant narrative and identify both social strata whose experience with the epidemic have thus far been rendered invisible, and the extent to which this epidemic is patterned complexly across society according to fundamental social determinants. It is our hope that as solutions are sought, these will continue to be framed in terms of addiction treatment, and that marginalized populations will not be overlooked when it comes to the allocation of treatment resources. Similarly, we hope that these solutions will be mindful of the roles of race/ethnicity, gender, class and age in shaping provision of pain management care in health care settings.
Supplemental Material
Download PDF (464.3 KB)Supplemental Material
Download PDF (246.6 KB)Acknowledgements
We would like to express our gratitude to Region Skåne for providing the research facilities that enabled this research.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Alexander, M. J., Kiang, M. V., & Barbieri, M. (2018). Trends in black and white opioid mortality in the United States, 1979–2015. Epidemiology, 29(5), 707–715.
- Axelsson Fisk, S., Mulinari, S., Wemrell, M., Leckie, G., Perez-Vicente, R., & Merlo, J. (2018). Chronic obstructive pulmonary disease in Sweden: An intersectional multilevel analysis of individual heterogeneity and discriminatory accuracy. Social Science & Medicine (Population Health), 4, 334–346.
- Bauer, G. R. (2014). Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Social Science & Medicine, 110, 10–17.
- Bechteler, S. S., & Kane-Willis, K. (2017). Whitewashed: The African American opioid epidemic. https://www.thechicagourbanleague.org/cms/lib/IL07000264/Centricity/Domain/1/Whitewashed%20AA%20Opioid%20Crisis%2011-15-17_EMBARGOED_%20FINAL.pdf
- Berkman, L. F., & Kawachi, I. (Eds.). (2000). Social epidemiology. Oxford: Oxford University Press.
- Bonnie, R. J., Kesselheim, A. S., & Clark, D. J. (2017). Both urgency and balance needed in addressing opioid epidemic: A report from the national academies of sciences, engineering, and medicine. Jama, 318(5), 423–424.
- Browne, W. J. (2017). MCMC estimation in MLwiN v3.00.
- Carey, G., Crammond, B., & De Leeuw, E. (2015). Towards health equity: A framework for the application of proportionate universalism. International Jounal for Equity in Health, 14(81). doi:10.1186/s12939-015-0207-6
- CDC. (2018). Overdose deaths involving prescription opioids. Date Accessed, February 15, 2019 Retrieved from https://www.cdc.gov/drugoverdose/data/prescribing.html.
- Center for Behavioral Health Statistics and Quality. (2016). 2015 national survey on drug use and health public use file codebook. Rockville, MD: Substance Abuse and Mental Health Services Administration. Retrieved from https://www.datafiles.samhsa.gov/study-dataset/national-survey-drug-use-and-health-2015-nsduh-2015-ds0001-nid16894
- Charlton, C., Rashbash, J., Browne, W. J., Healy, M., & Cameron, B. (2017). MLwiN Version 3.00.
- Choo, H. Y., & Ferree, M. M. (2010). Practicing intersectionality in sociological research: A critical analysis of inclusions, interactions, and institutions in the study of inequalities. Sociological Theory, 28(2), 129–149.
- Collins, P. H., & Bilge, S. (2016). Intersectionality. Cambridge: Polity.
- Conrad, P., & Kern, R. (1981). The social production of disease and illness. In P. Conrad & R. Kern (Eds.), The sociology of health and illness: Critical perspectives (pp. 9–11). New York: St. Martin’s Press.
- Crenshaw, K. (1989). Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum, 8(1), 139–167.
- Cronrath, D. S. (May 9, 2018). Race and the opioid epidemic. Folio Weekly Retrieved from http://folioweekly.com/stories/race-and-the-opioid-epidemic,19717
- Crutchfield, R. D., & Gove, W. R. (1984). Determinants of drug use: A test of the coping hypothesis. Social Science & Medicine, 18(6), 503–509.
- Davis, J. H. (2017). Trump declares opioid crisis a ‘Health Emergency’ but Requests No Funds. New York Times. Retrieved from https://www.nytimes.com/2017/10/26/us/politics/trump-opioid-crisis.html
- Doyal, L. (1979). The policitcal economy of health. London: Pluto Press.
- Evans, C. R. (2015). Innovative approaches to investigating social determinants of health - social networks, environmental effects and intersectionality. ( Doctoral Dissertation). Harvard University, Boston, MA.
- Evans, C. R. (2019). Modeling the intersectionality of processes in the social production of health inequalities. Social Science & Medicine. doi:10.1016/j.socscimed.2019.01.017
- Evans, C. R., Williams, D. R., Onnela, J. P., & Subramanian, S. V. (2018). A multilevel approach to modeling health inequalities at the intersection of multiple social identities. Social Science & Medicine, 203, 64–73.
- Ezenwa, M. O., Ameringer, S., Ward, S. E., & Serlin, R. C. (2006). Racial and ethnic disparities in pain management in the United States. Journal of Nursing Scholarship, 38(3), 225–233.
- Feagin, J., & Bennefield, Z. (2014). Systemic racism and U.S. health care. Social Science & Medicine, 103, 7–14.
- Ferree, M. M., & Hall, E. J. (1996). Rethinking stratification from a feminist perspective: Gender, race, and class in mainstream textbooks. American Sociological Review, 61(6), 929–950.
- Goldstein, H., Browne, W. J., & Rashbash, J. (2002). Partitioning variation in multilevel models. Understanding Statistics: Statistical Issues in Psychology, Education, and the Social Sciences, 1(4), 223–231.
- Gravlee, C. C. (2009). How race becomes biology: Embodiment of social inequality. American Journal of Physical Anthropology, 139(1), 47–57.
- Green, C. R., Anderson, K. O., Baker, T. A., Campbell, L. C., Decker, S., Fillingim, R. B., … Vallerand, A. H. (2003). The unequal burden of pain: Confronting racial and ethnic disparities in pain. Pain Medicine, 4(3), 277–294.
- Green, M. A., Evans, C. R., & Subramanian, S. V. (2017). Can intersectionality theory enrich population health research? Social Science & Medicine, 178, 214–216.
- Guy, G. P., Jr., Zhang, K., Bohm, M. K., Losby, J., Lewis, B., Young, R., … Dowell, D. (2017). Vital signs: Changes in opioid prescribing in the United States, 2006–2015. Morbidiity and Mortality Weekly Report, 66(26), 697–704.
- Han, B., Compton, W. M., Blanco, C., Crane, E., Lee, J., & Jones, C. M. (2017). Prescription opioid use, misuse, and use disorders in US adults. Annals of Internal Medicine, 167(5), I24–I24.
- Hansen, H., & Netherland, J. (2016). Is the prescription opioid epidemic a white problem? American Journal of Public Health, 106(12), 2127–2129.
- Harrison, J. M., Lagisetty, P., Sites, B. D., Guo, C., & Davis, M. A. (2018). Trends in prescription pain medication use by race/ethnicity among US adults with noncancer pain, 2000–2015. American Journal of Public Health, 108(6), 788–790.
- Hernández-Yumar, A., Wemrell, M., Abásolo Alessón, I., González López-Valcárce, B., Leckie, G., & Merlo, J. (2018). Socioeconomic differences in body mass index in Spain: An intersectional multilevel analysis of individual heterogeneity and discriminatory accuracy. PLoS One, 13(12), e0208624.
- Jones, K., Johnston, R., & Manley, D. (2016). Uncovering interactions in multivariate contingency tables: A multi-level modelling exploratory approach. Methodological Innovations, 9. doi: 10.1177/2059799116672874
- Kaplan, J. (2014). The quality of data on “Race” and “Ethnicity”: Implications for health researchers, policy makers, and practitioners. Race and Social Problems, 6(3), 214–236.
- Kaufman, J. S., & Cooper, R. S. (2010). The use of racial/ethnic categories in medical diangosis and treatment. In I. Whitmarsh & D. S. Jones (Eds.), What’s the use of race? Modern governance and the biology of difference (pp. 187–206). Cambridge, MA: The MIT Press.
- King, N. B., Fraser, V., Boikos, C., Richardson, R., & Harper, S. (2014). Determinants of increased opioid-related mortality in the United States and Canada, 1990–2013: A systematic review. American Journal of Public Health, 104(8), E32–E42.
- Kolodny, A., Courtwright, D. T., Hwang, C. S., Kreiner, P., Eadie, J. L., Clark, T. W., & Alexander, G. C. (2015). The prescription opioid and heroin crisis: A public health approach to an epidemic of addiction. Annu Rev Public Health, 36, 559–574.
- Krieger, N. (2003). Does racism harm health? Did child abuse exist before 1962? On explicit questions, critical science, an current controversies: An ecosocial perspective. American Journal of Public Health, 93, 194–199.
- Krieger, N. (2011). Epidemiology and the people’s health – Theory and context. New York, NY: Oxford University Press Inc.
- Laguna, S. (2018). Constructing drug using victims: Raceand class in policy debates on ecstasy use in the U.S. Contemporary Drug Problems, 45(1), 67–81.
- Leckie, G., & Charlton, C. (2013). runmlwin – A program to run the MLwiN multilevel modelling software from within Stata. Journal of Statistical Software, 52(11), 1–40.
- Link, B. G., & Phelan, J. (1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, 80–94. doi:10.2307/2626958
- Lofters, A., & O’Campo, P. (2012). Differences that matter. In P. O’Campo & J. Dunn (Eds.), Rethinking social epidemiology: Towards a science of change (pp. 93–109). Dordrecht: Springer.
- Manchikanti, L., Helm, S., 2nd, Fellows, B., Janata, J. W., Pampati, V., Grider, J. S., & Boswell, M. V. (2012). Opioid epidemic in the United States. Pain Physician, 15(3 Suppl), ES9–38.
- Marmot, M., & Bell, R. (2012). Fair society, healthy lives. Public Health, 126(Supplement 1), S4–S10.
- May, V. M. (2015). Pursuing intersectionality, unsettling dominant imaginaries. New York: Routledge.
- McCall, L. (2005). The complexity of intersectionality. Signs, 30(3), 1771–1800.
- Merlo, J. (2018). Multilevel analysis of individual heterogeneity and discriminatory accuracy (MAIHDA) within an intersectional framework. Social Science & Medicine. doi:10.1016/j.socscimed.2017.12.026
- Merlo, J., Mulinari, S., Wemrell, M., Subramanian, S. V., & Hedblad, B. (2017). The tyranny of the averages and the indiscriminate use of risk factors in public health: The case of coronary heart disease. Social Science & Medicine (Population Health), 3, 684–698.
- Monnat, S. M. (2017). Drugs, alcohol, and suicide represent growing share of U.S. mortality. In The Carsey school of public policy at the scholars’ repository (pp. 1–6). Durham, NH: Carsey School of Public Policy, University of New Hampshire. Retrieved from: https://scholars.unh.edu/carsey/292
- Mossey, J. M. (2011). Defining racial and ethnic disparities in pain management. Clinical Orthopaedics and Related Research, 469(7), 1859–1870.
- Mulinari, S., Wemrell, M., Rönnerstrand, B., Subramanian, S. V., & Merlo, J. (2018). Categorical and anti-categorical approaches to US racial/ethnic groupings: Revisiting the National 2009 H1N1 Flu Survey (NHFS). Critical Public Health, 28(2), 177–189.
- Murakawa, N. (2011). TOOTHLESS the methamphetamine “Epidemic,” “Meth Mouth,” and the racial construction of drug scares. Du Bois Review-Social Science Research on Race, 8(1), 219–228.
- Netherland, J., & Hansen, H. (2016). The war on drugs that wasn’t: Wasted whiteness, “Dirty Doctors,” and race in media coverage of prescription opioid misuse. Culture, Medicine and Psychiatry, 40(4), 664–686.
- Netherland, J., & Hansen, H. (2017). White opioids: Pharmaceutical race and the war on drugs that wasn’t. Biosocieties, 12(2), 217–238.
- Nicholson, H. L., & Ford, J. A. (2018). Correlates of prescription opioid misuse among black adults: Findings from the 2015 national survey on drug use and health. Drug and Alcohol Dependence, 186, 264–267.
- Nowotny, K. M., Rogers, R. G., & Boardman, J. D. (2017). Racial disparities in health conditions among prisoners compared with the general population. Social Science & Medicine (Population Health), 3, 487–496.
- O’Campo, P., & Dunn, J. R. (2012). Rethinking social epidemiology: Towards a science of change. Dordrecht and New York: Springer.
- Olofsson, A., Zinn, J. O., Griffin, G., Nygren, K. G., Cebulla, A., & Hannah-Moffat, K. (2014). The mutual constitution of risk and inequalities: Intersectional risk theory. Health, Risk & Society, 16(5), 417–430.
- Peterson, K., & Armour, S. (2018). Opioid Vs. crack: Congress reconsiders its approach to drug epidemic. The Wall Street Journal, Retrieved from https://www.wsj.com/articles/opioid-v-crack-congress-reconsiders-its-approach-to-drug-epidemic-1525518000
- Phelan, J. C., & Link, B. G. (2015). Is racism a fundamental cause of inequalities in health? Annual Review of Sociology, 41, 311–330.
- Pletcher, M. J., Kertesz, S. G., Kohn, M. A., & Gonzales, R. (2008). Trends in opioid prescribing by race/ethnicity for patients seeking care in us emergency departments. Jama, 299(1), 70–78.
- Provine, D. M. (2007). Unequal under law: Race in the war on drugs. Chicago: The University of Chicago Press.
- Rasbash, J., Steele, F., Browne, W. J., & Goldstein, H. (2017). A user’s guide to MLwiN v3.00. Bristol, UK: Centre for Multilevel Modelling, University of Bristol.
- Reinarman, C. (1994). The social construction of drug scares. In P. A. Adler & P. Adler (Eds.), Constructions of deviance: Social power, context, and interaction (pp. 92–105). Belmont, CA: Wadsworth Publishing Co.
- Rigg, K. K., & Monnat, S. M. (2015). Urban vs. rural differences in prescription opioid misuse among adults in the United States: Informing region specific drug policies and interventions. International Journal of Drug Policy, 26(5), 484–491.
- Scholl, L., Seth, P., Kariisa, M., Wilson, N., & Baldwin, G. (2019). Drug and opioid-involved overdose deaths — United States, 2013–2017. Morbidiity and Mortality Weekly Report, 67(5152), 1419–1427.
- Schuchat, A., Houry, D., & Guy, G. P., Jr. (2017). New data on opioid use and prescribing in the united states. Jama, 318(5), 425–426.
- Schultz, A. J., & Mullings, L. (Eds.). (2006). Gender, race, class, and health: Intersectional approaches. San Francisco, CA: Jossey-Bass.
- Sen, G., Iyer, A., & Mukherjee, C. (2009). A methodology to analyse the intersections of social inequalities in health. Journal of Human Development and Capabilities, 10(3), 397–415.
- Seth, P., Scholl, L., Rudd, R. A., & Bacon, S. (2018). Overdose deaths involving opioids, cocaine, and psychostimulants – United States, 2015–2016. Morbidity and Mortality Weekly Report, 67(12), 349–358.
- Singhal, A., Tien, -Y.-Y., & Hsia, R. Y. (2016). Racial-ethnic disparities in opioid prescriptions at emergency department visits for conditions commonly associated with prescription drug abuse. PLoS One, 11(8), e0159224.
- Stanistreet, D. (2005). Constructions of marginalised masculinities among young men who die through opiate use. International Journal of Men’s Health, 4(3), 243–265.
- Steele, F. (2008). Introduction to multilevel modelling concepts. Module 5. Bristol, UK: Centre for Multilevel Modelling, University of Bristol.
- U.S. Bureau of the Census. (2015). Poverty threshold by size of famiy and number of children. Retrieved from https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html
- Valles, S. A. (2012). Heterogeneity of risk within racial groups, a challenge for public health programs. Preventive Medicine, 55(5), 405–408.
- Veenstra, G. (2013). Race, gender, class, sexuality (RGCS) and hypertension. Social Science & Medicine, 89, 16–24.
- Wemrell, M., Merlo, J., Mulinari, S., & Hornborg, A. C. (2016). Contemporary epidemiology: A review of critical discussions within the discipline and a call for further dialogue with social theory. Sociological Compass, 10(2), 153–171.
- Wemrell, M., Mulinari, S., & Merlo, J. (2017a). An intersectional approach to multilevel analysis of individual heterogeneity (MAIH) and discriminatory accuracy. Social Science & Medicine, 178, 217–219.
- Wemrell, M., Mulinari, S., & Merlo, J. (2017b). Intersectionality and risk for ischemic heart disease in Sweden: Categorical and anti-categorical approaches. Social Science & Medicine, 177, 213–222.
- Yedinak, J., Kinnard, E., Hadland, S., Green, T., Clark, M., & Marshall, B. (2016). Social context and perspectives of non-medical prescription opioid use among young adults in Rhode Island: A qualitative study. The American Journal on Addictions, 25, 659–665.
