Abstract
Phenomenon
In the United Kingdom (UK) the government has increased the number of places at university to study medicine in England to meet workforce demands. In parallel, there have been growing student numbers in other healthcare professions and new professions whose roles overlap with doctors, such as advanced nurse practitioners and physician associates, have been introduced. These increasing numbers of medical students and other healthcare professions training in the same clinical setting have led to questions about the effect on the student experience. We aimed to investigate the impact of student-student encounters on the learning experience during clinical placements before student numbers increase further.
Approach
In this investigation medical student perceptions were collected retrospectively at Norwich Medical School, University of East Anglia in the UK, during the 2018/19 academic year following two clinical placements in secondary care settings. Through mandatory online course evaluations, all medical students were asked if their learning had been positively or negatively affected by other students, and how frequently they had certain student-student experiences.
Findings
Responses from 786 (of 844) medical students (93% response rate) demonstrated that most students felt their learning had been affected in some way by the presence of others while on their secondary care placements. Students experienced both positive and negative impacts of encounters with other students. Final year students tended to report more negative experiences, with first year students reporting more positive. while some students had experienced competition for learning opportunities and lower quality interactions with patients and doctors due to “overcrowding,” more students reported benefits from learning from and with other students. However, it also was found that any negative encounters with other students, even if accompanied by positive experiences, detrimentally affected student satisfaction with the placement.
Insights
This investigation indicates that student-student interactions influence the clinical learning experience of medical students both positively and negatively. Given the overriding influence of negative encounters, the findings suggest a need to maximize the beneficial effects of encountering other students on clinical placements; while protecting against missed or poor-quality learning opportunities due to competition between students, particularly for more senior students. Medical educators need to consider where their clinical attachments are at risk from multiple students being present at the same time and work to alleviate the negative impacts of such student-student encounters, while actively encouraging peer learning experiences between the medical students and collaborative activities between students of different healthcare professions. This is likely to become increasingly important as student numbers in medicine and other healthcare professions continue to grow.
Introduction
As in other countries,Citation1 there are concerns in the United Kingdom (UK) that the number of doctors being educated is insufficient to meet current and future workforce demands.Citation2,Citation3 Consequently, recent UK Government policy has been to increase the number of medical students in England by approximately 25% through the staggered creation of 1500 new places each year.Citation4 From the academic year 2018/19 onwards, additional students have been allocated to the existing UK medical schools as well as five new institutions. This mirrors the situation internationally, where shortages in the total number of doctors needed to meet population demand, insufficient numbers of certain specialists, and regional inequalities has led to increases in the number of medical students at existing medical schools as well as the creation of new medical schools.Citation5,Citation6
Whenever and wherever expansion of medical students numbers are implemented similar obstacles must be addressed, such as financial considerations, securing adequate educational resources, availability of sufficient academic and clinical faculty, and finding expanded or new clinical sites for students.Citation7 Some concerns have been raised regarding how such expansion of medical student places may affect the overall quality of medical education.Citation8 It is recognized that increasing medical student numbers will require an increase in the overall capacity of clinical placements.Citation9,Citation10 Along these lines, a number of challenges must be addressed so as not to affect quality of the clinical educational experience, including workload of clinical educators on placements, space and resources for students in the physical environment, and the clinical culture including patient availability.Citation11 Various nations have recognized that this cannot be accomplished without adapting how clinical placements are coordinated.Citation12,Citation13
Evaluation specifically of the perceived quality of learning after a swift expansion of medical student numbers has led to some reported negative experiences.Citation14 Yet, some institutions have successfully dealt with surges in overlapping student clinical placements through innovative timetabling and adaptation of placement requirements with positive student outcomes, suggesting that solutions can be found.Citation15 Such findings highlight the need for medical schools to proactively consider how to optimally manage increased student numbers while maintaining high quality medical education.
In addition to medical student expansion there are an increasing number of other healthcare students. Several new roles have been developed in recent years to adapt to National Health Service (NHS) workforce and service demands, including advanced nurse practitioners and physician associates, whose clinical capabilities overlap with traditional medical roles.Citation16 In 2018, it was estimated that 600 physician associates were practicing in the UK, with approximately 1600 students in training.Citation17 In the USA there have been rapidly growing numbers of advance practice registered nurses and physician assistants over the last two decades as well.Citation1 Inevitably, these students undertake clinical attachments alongside medical students in hospitals and community placements. Despite concerns from some, physician associates have been found to have no overall detrimental effect on postgraduate medical education, and possibly enhance it.Citation18
The Norwich Medical School (NMS) at the University of East Anglia (UEA) was established in 2002 following the last expansion of medical students in the UK. It offers a five-year degree of Bachelor of Medicine and Bachelor of Surgery (MBBS) in undergraduate medicine; comprising an integrated systems-based course, centered around problem-based learning (PBL), with clinical placements during all five years. Medical students may be placed at sites across the counties of Norfolk, Suffolk, and Essex, UK. Many of these sites also receive students from other medical schools and of other allied healthcare professions, including from UEA’s two-year postgraduate MSc in Physician Associate Studies established in 2016 with a capacity of 30 students per year.
NMS successfully bid for more medical student places in both the 2018/19 and 2019/20 academic years; increasing the cohort size from 167 students in 2017/18, to 183 in 2018/19 and then 208 in 2019/20. Once the full expansion has worked through to all years, the student numbers will have increased from a baseline of 835 to 1100 (25% increase from 2015 to 2023).
As cohort sizes increase, Norwich medical students will learn in larger groups and increasingly overlap with each other in the clinical environment. while medical student training has never been completely solitary, with the well-established norm being that students undertake clinical placements in groups, the extent and nature of the impact other students have in the clinical setting has not been fully explored. There is some evidence that medical students receive considerable benefit from peer relationships formed during learning in the clinical setting.Citation19 However, ad hoc feedback received previously from Norwich medical students about encounters with others on placement has been predominantly negative, including comments about missing out on learning opportunities due to competition with other students. We aimed to investigate the impact that encounters with other students had on the perceived quality of learning during students’ clinical attachments before the numbers grow further. This information may help optimize existing strengths and manage potential problems as future cohorts expand.
Method
Study setting
The NMS five-year MBBS is a fully integrated, systems-based course. At the time of the investigation, the MBBS comprised 15 modules: 12 taught modules, one student assistantship module, and two elective modules. Other medical school curricula often have distinct pre-clinical and clinical phases, where students learn through discipline-focused lectures during the first years of the training, followed by clinical placement in the later years. However, at NMS campus-based learning for each of the 12 taught modules of the MBBS, covering the underpinning biological, social, and clinical sciences of medicine, is integrated with early and ongoing patient contact; such that there are clinical placements in all five years of the MBBS.
The taught modules in years 1 to 4 were composed of (i) blocks of campus-based teaching including PBL sessions, lectures, seminars, consultation skills sessions, anatomy, and medical research, and one day per week in primary care and (ii) a four-week block of secondary care placement. The taught module in year 5 comprised campus-based teaching and clinical placements (both primary and secondary care) running alongside each other throughout the module. Year 5’s student assistantship module is spent wholly in a secondary care clinical placement (see Appendix Box 1 for further details of the MBBS).
Participants
The participants were students on NMS’s five-year MBBS during the 2018/19 academic year. All students who were present on the MBBS during the 12 taught modules and the student assistantship module of years 1-5 were required to complete an evaluation form at the end of the module (up to three evaluation forms per year). Only those students who consented for the feedback they provided in these evaluation forms to be used for purposes beyond course development were included in the study reported here.
Materials
Evaluation forms were developed for each of the 12 taught modules and the student assistantship module. The forms covered all aspects of the students’ experience during the campus-based and secondary care blocks of the module, with the aim of using student feedback to develop the MBBS for future students. In the secondary care clinical placement section of the first two evaluation forms of the year, students were asked to complete questions regarding their experiences with other students while on placements; in addition to the five standard secondary care placement questions asked for every module each year (see Appendix Box 2).
In both evaluation forms the students were asked to rate their satisfaction (on a five-point scale, from 1 = Not at all satisfied to 5 = Completely satisfied) with (i) placement organization and (ii) learning experience overall for their secondary care placement.
Additionally, in the first evaluation form of their year, students were asked if they had had any encounters with other students which had led to (i) an improved (positive) and / or (ii) a reduced (negative) quality experience (the response options were: “No,” “Yes occasionally,” and “Yes often”) during their first block of secondary care placement. To indicate what type of student they had interacted with while on placement, students selected from a list of six types (“Other same module UEA medical student,” “Other same year UEA medical student,” “UEA medical student from a different year,” “Medical student from another university,” “Physician Associate student,” or “Nursing student”); an “Other (please specify)” space was also provided for students to mention any other type of student they had encountered not listed. An open-ended question was also provided for comment.
In the second evaluation form of their year, students were provided with a list of nine positive experiences and ten negative experiences they might have had due to the presence of other students. They were asked to indicate how often they had experienced each, if at all, during their second block of secondary care placement (“I didn’t experience this,” “This happened once,” or “This happened multiple times”). To ensure that these lists were relevant and salient to the medical students, the authors reviewed students’ responses to the first evaluation’s open-ended questions, along with issues that students raised spontaneously in previous course evaluations. There was an open-ended question following each list of experiences, where students could provide details if they had had any other types of experience due to other students. This allowed identification of any further interactions which had not come up previously, ensuring that students were not limited to just the experiences provided in the two lists.
Procedure
The evaluation forms were created in SurveyMonkey by the NMS’s lead for MBBS evaluation (SM), with input on the questions to be asked about each area of the MBBS from the staff involved in developing and providing the learning activities for that area. Data were then collected online, via an individual link to each student’s own copy of the evaluation form hosted in SurveyMonkey sent to their university email address by the MBBS evaluation lead. Students were subsequently sent up to three reminder emails containing their individual link if they had not fully completed the form at the reminder time. The data collection period commenced immediately following the last day of teaching for the module and was generally over two weeks.
Consent
The primary purpose of MBBS evaluations is to gather students’ feedback to contribute to ongoing course development. The faculty’s research ethics committee provided approval for NMS to ask students if they would consent for the medical school to use the anonymous data for additional purposes such as promotional or academic. This consent is obtained at the end of each student’s last evaluation form of the academic year for the feedback provided that year.
Statistical analysis
Data were downloaded from SurveyMonkey into Excel 2016. Number and percentage of type of other students encountered and type of experience were calculated. Responses to the first form’s open-ended questions were reviewed by all three authors to identify any additional types of students and experiences with other students for use in the second form (data not reported here). Statistical analysis was conducted using IBM SPSS Statistics 25 to investigate the impact of negative and positive experiences with other students on satisfaction with (i) organization; and (ii) overall experience for the second placement of the year (two dependent variables). Four between-group types of experience were used in the analysis: (i) no experiences with other students; (ii) only negative experiences with other students; (iii) only positive experiences with other students; or (iv) both positive and negative experiences with other students (one independent variable with four groups). As the two satisfaction questions were rated on an ordinal scale (1 = Not at all satisfied, 2 = Slightly satisfied, 3 = Moderately satisfied, 4 = Very satisfied, 5 = Completely satisfied) the non-parametric Kruskal-Wallis test was used; followed by Dunn’s pairwise tests with the significance level adjusted using a Bonferroni correction for multiple tests.
Results
Eight hundred and forty of 846 students completed the first evaluation form of the year. Eight hundred and thirty-nine of 844 students completed the second evaluation form of the year (NB the number of students present at different times during the academic year can vary slightly due to students intercalating for health or academic reasons). In total, 844 students completed the clinical placement section of one or both evaluation forms. Demographic information was not collected in all evaluation forms; so, no demographic details are available.
Responses from students who had not consented for their anonymous feedback to be used for additional purposes were removed, leaving a sample of 786 of 844 students (93%). The breakdown by year group is as follows: year 1 = 174, year 2 = 158, year 3 = 140, year 4 = 163, year 5 = 151.
Type of other students encountered - Negative experiences
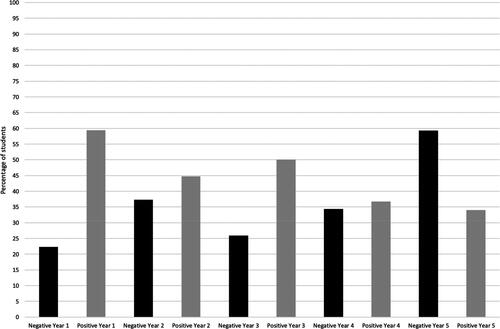
Thirty-six percent of students had “occasionally” or “often” perceived a negative impact on their learning opportunities through encounters with other students while on their first secondary care placement of the year. Instances were lowest in year 1 (22%) and highest in year 5 (59%) ().
Figure 1. Percentage of students who (“Yes occasionally” or “Yes often”) had negative and / or positive encounters with other students.
The type of other student encountered was different according to the year group (see Appendix Table A). Students in years 1 to 4 generally had their negative encounters with students on the same module (and thus also the same year) as themselves. Year 1 students additionally experienced negative encounters with UEA medical students from a different year. This is unsurprising, as the first secondary care placement of year 1 is a general introduction to hospital working and the students are allocated to a variety of different specialties which they will study in later modules where there may be students from other years undertaking their specialty placement. Year 5 students experienced most negative encounters with physician associate students. They also had negative experiences with other year 5 students; both students on the same module as themselves and students studying the other year 5 module who were on placement at the same time. A small number of other types of students were mentioned in response to the “Other, please specify” option including pharmacy, paramedic, and midwifery students as well as Foundation doctors (qualified doctors working on a two-year postgraduate training program).
Type of other students encountered - Positive experiences
Forty-five percent of students had “occasionally” or “often” perceived a positive impact on their learning opportunities through encounters with other students while on their first secondary care placement of the year; with the highest instances in year 1 (59%) and the lowest in year 5 (34%) ().
Sixty-eight of the year 1 students had experienced positive encounters with other UEA students in a different year group. In year 2, UEA students in other year groups were also the most selected type of student for a positive encounter, and it was the second most selected in year 3. The most selected student type in years 3, 4 and 5, and the second most selected in years 1 and 2, was other UEA students studying the same module (see Appendix Table A). As with negative encounters, pharmacy, paramedic and midwifery students, and Foundation doctors were mentioned by a small number of students for positive encounters. Additionally, a few year 1 students mentioned positive experiences with radiology/radiography students.
Type of experiences with other students
When the students were provided with specific examples of types of experiences they may have had with other students it was found that across years 1 to 5 an average of 75% of students had experienced both positive and negative impacts (year 1 = 85%, year 2 = 78%, year 3 = 71%, year 4 = 61%, year 5 = 80%) while on their second secondary care placement; with only 8% or less experiencing neither (year 1 = 5%, year 2 = 3%, year 3 = 4%, year 4 = 8%, year 5 = 2%).
Of those who reported instances where their learning experience had been improved by other students, the most frequently selected positive impact was learning through watching or working with other students (79%) (see Appendix Table B). Seventy percent or more students also indicated that another student had taught them theoretical knowledge, answered their questions or explained things, given them advice or tips on the module, or that they had taught another student and found this to be useful. The least commonly selected experience across all years (40%) was learning about what other healthcare professions do through being with students from these professions, followed by another student watching them with a patient and giving feedback (48%). Also, relatively less frequent in years 4 and 5 was another student teaching them clinical skills.
When asked about instances where the presence of other students was detrimental to their learning (see Appendix Table C), around half of the students (49-58%) had found the room to be too crowded for comfort, there to be too many students around patients and been made to feel unwelcome by staff due to too many students being present. In years 1 (54%) and 2 (49%) a lack of resources to study due to the presence of other students was also an issue for about half of the students. In year 5, 40-52% of the students had experienced problems with missing out on performing tasks or procedures because others took the available opportunities, having nothing to do because other students had taken all of the available learning opportunities, and learning experience being negatively affected by too many students on a ward round. Somewhat reassuringly, only a fifth or less of the students (9-20%) had been confused about what they were expected to learn due to other students who were studying at a different level or a different curriculum.
Experiences with other students and satisfaction with placement
Further analysis was conducted to look at how experiences with other students might affect (i) satisfaction with organization of the placement; and (ii) satisfaction with secondary care learning experience overall.
Analysis focused on data from the second placement because the results indicated that when provided with specific examples of possible positive and negative impacts of encounters, more students reported having such experiences. Given that students were asked for feedback some days or weeks after the experience, the cued recognition required to answer the questions about the second placement block might be more dependable than the open recall required for the first placement block’s questions.
The Kruskal-Wallis test for the dependent variable satisfaction with organization of the placement indicated a difference between the mean ranks of at least one pair of groups (χ2(3) = 21.42, p <.001). Subsequent Dunn’s pairwise tests showed a difference between the only positive experiences group and i) the only negative experiences group (p <.001); and ii) the group who had had both positive and negative experiences (p <.001) ().
Table 1. Summary descriptives for the Kruskal-Wallis test.
Similarly, the Kruskal-Wallis test for the dependent variable satisfaction with learning experience on the placement overall indicated a difference between the mean ranks of at least one pair of groups (χ2(3) = 20.80, p <.001). Dunn’s pairwise tests once again showed a difference between the group who had only positive experiences and i) the group who had only negative experiences (p <.001); and ii) the group who had had both positive and negative experiences (p <.001) ().
Thus, there is evidence that those students who had only positive experiences were more satisfied with the organization of their placement and their overall learning experience on placement than students who had any kind of negative experiences - whether that was just negative experiences or both negative and positive. These findings suggest that negative experiences on placement due to the presence of other students have a detrimental effect on students’ view of the whole placement, even if they also had some positive experiences.
Discussion
This retrospective, survey-based investigation of medical students’ experiences demonstrates that they do perceive other students in the clinical environment to affect their learning, but in diverse ways with both negative and positive impacts. This investigation appears to be the first to formally describe and quantify such perceptions of students in a UK medical school, but our observations should have relevance to any clinical setting accommodating large or increased numbers of learners or adapting the way in which different learners interact on placements.
Our findings suggest a number of key factors that could assist in planning for future clinical placements at NMS, many of which could be considered by other medical training institutions adjusting the format of their own clinical placements. Firstly, we confirmed that the majority of our students did feel their learning was changed due the presence of their colleagues. Reassuringly, although somewhat surprisingly, the prevalence of positive encounters with other students was greater than negative ones. However, negative encounters appeared to be powerful enough to adversely influence student satisfaction with the entire clinical attachment, even when coupled with positive encounters. This highlights the need to take account of the likelihood of encounters with other students (both other medical students and students from other healthcare professions) in placement planning and to actively identify areas where negative experiences may occur so as to optimize the learner experience.
Secondly, our findings indicate that placement planning around encounters with other students needs to take full account of the medical students’ year of study. Students in earlier years of the course appeared to gain more benefit from encounters with other students, compared to more senior students. Year 1 students were most likely to report having questions answered by other students, getting tips, being taught clinical skills, and getting feedback from other students. Furthermore, junior students felt students in higher years of the MBBS most positively influenced their learning. Encouragingly, final year students were most likely to report a benefit from teaching other students; so, they appear to gain from this relationship too.
The notion that students learn from their peers is not new. Formal peer-assisted learning (PAL) is well documented as an effective teaching method with several student-related benefits.Citation20–22 Some challenges have been identified with establishing PAL within the clinical setting specifically.Citation23 However, a review of studies reporting same-level PAL in clinical placements indicated that PAL can be implemented effectively using a tool or framework to create structure to the interactions, with beneficial outcomes similar to our own findings such as learning clinical skills, getting feedback on performance, and feeling supported and understanding the placement environment.Citation21 Additionally, there is evidence that informal peer groups in a clinical setting benefit students with support both socially and academically.Citation19 Our students appear to be taking advantage of shared time on their placements to create their own avenues of learning. With increased student numbers there will be more opportunities for such informal PAL activities and to formalize these interactions both within and across year groups. For example, buddying-up schemes or intentionally overlapping students in different years of the MBBS may be potential platforms to enhance opportunities for PAL on clinical attachments to the benefit of both junior and senior students. Positive signposting for both staff and students about these intentional interactions, as well as suggestions for structuring shared time is likely to further enhance the learning experience.
However, this needs to be balanced with the important observation that students in their final year of the MBBS were most likely to have had negative encounters with other students and reported the highest frequency of the various negative experiences. This could be explained by a few factors. while there is a considerable amount of clinical time in both primary and secondary care throughout all five years of the MBBS, the final year of our course is the most hands-on. The final year students have many procedural skills to get signed off and they rotate through clinical areas geared for practical learning, such as emergency departments (Accident and Emergency) and acute assessment units. Sometimes such learning opportunities may be finite or spontaneous (i.e., only so many procedures to perform with supervision), creating competition between students for access. Also, final year students attached to general acute admission areas and shadowing under a medical or surgical team are likely to overlap with students in other years or physician associate students undertaking their designated specialty-specific placements. Encounters may then occur and be perceived as “intrusions” into the learning area for these senior students. Feedback from senior students indicates that they view the learning opportunities they have during their final year as their “last chance” before graduation and commencing their Foundation training (an internship program; the two-year training program they will be commencing as soon as they successfully complete their undergraduate medical studies), and consequently they feel that their opportunities to practice should take priority over the lower year students. As such, senior medical students may need more lone working time on their clinical attachments. This could be accomplished by timetabling them with a higher proportion of their time spent over evenings and weekends. They may be less likely to overlap with other students, who are spending the bulk of their time undertaking placements during normal working hours, and this more closely mirrors the working patterns they will soon undertake as junior doctors. From this point of view, these learners might have the most to lose from increasing numbers of students and their clinical placements may need to take priority over those of students at the start of the MBBS.
Nonetheless, our findings demonstrate the benefits of collaboration in learning. Forming relationships with each other while on placement, through the mutually beneficial objective of learning, should theoretically encourage a sense of collegiality. This will hopefully translate into future cooperative professional relationships and an appreciation of different perspectives, necessary for successful clinical practice in a team setting.
Limitations and future research
There are a number of limitations to this investigation. Firstly, it is likely that the views expressed have been influenced by the individual personalities of students and their preferred style of learning. However, the good response rate of 93% (786 of 844 students) and large sample size across all five years of the MBBS, including the full range of specialties and placements at different hospitals, should minimize this kind of respondent bias. Furthermore, we used a two-phase structure to develop the questionnaire to ensure that researcher bias was limited; whereby we used instances of encounters with other students reported via open-ended questions to formulate appropriate closed questions to quantify the burden of those experiences. This enabled us to use examples of encounters students had with other students during the first placement to get a count of the number of each type of positive and negative experience across all the MBBS students during the second placement. This revealed that the prevalence of negative encounters, particularly with students from other healthcare professions, was lower than ad hoc comments from students had suggested previously and that there were a variety of positive experiences occurring frequently across all five years of the MBBS that had not been identified previously. We ensured that the students were not limited to the lists of experiences provided to them by accompanying these with open-ended questions where students could describe other types of positive and negative encounters. However, there were no consistently raised additional types of experience; most of the students who did provide a comment merely elaborated on the responses they had selected, for example, by providing examples of when the experience had occurred. An additional advantage of providing lists generated from previous student responses of positive and negative experiences to select from, relates to the evaluation period taking place at the end of the module; which could be several weeks after the secondary care placement component. The lists enabled students to use recognition, rather than free recall, when evaluating their experiences with other students while on placement. This would make retrieval of memories about encounters when asked some weeks later easier, and thus provide a more complete picture of the type and extent of positive and negative experiences with other students while on placement across the whole responding sample.
Secondly, student feedback is only one metric to measure the quality of medical education; positive or negative student perceptions about their experiences in a learning environment do not automatically equate to the caliber of teaching and training provided. It would be useful in further research to consider the impact of encounters with other students on performance on clinical assessments such as OSCEs (Objective Structured Clinical Examination). Related to this, in their final year, NMS medical students are required to complete a clinical competency record in which they are required to perform a set of specific clinical skills on patients they encounter during their clinical placements in the presence of a qualified healthcare professional and get their performance signed off as satisfactory. This record currently comprises 25 tasks that students will be expected to perform as a junior doctor. In institutions where there is not such a requirement, future research may need to examine the impact of increasing student numbers on whether senior students continue to meet essential competencies before graduation. In our own institution we need to consider the impact on opportunities and resources to first practice the clinical skills (on fellow students, models, and patients), and then availability of willing patients on clinical placements with which to perform the clinical skills under observation from a qualified health professional. There is also the burden on these health professionals of having to observe an increasing number of students for signing off clinical skills to consider.
Thirdly, this evaluation focused on the experiences of the medical students only. Considering the viewpoints of other healthcare profession students would create a more well-rounded perspective of the experiences of all clinical learners in the placement setting and should be incorporated into similar future research. The importance of collaborative practice in effective healthcare delivery is well established, as is the role of interprofessional education in enhancing such collaborative practice.Citation24 NMS medical students undertake classroom-based interprofessional learning (IPL) activities in year 1; followed by later clinical IPL sessions (students in years 4 and 5 undertake clinically authentic, simulation-based clinical skill sessions with paramedic, nursing, and pharmacy students) which are very well regarded by the medical students.Citation25 However, our findings suggest that the informal encounters the medical students had with students from other professions while on clinical placements in this study were less positive. In particular, it was found that the final year students were experiencing issues of encounters with the physician associate students. At our institution, where both the medical students and physician associate students are studying within the same medical school and attend some of the same campus-based teaching as well as clinical placements, it is both feasible and desirable to evaluate if the physician associate students are having similar experiences. If they are, then we will need to work with both groups of students and course organizers to develop strategies to promote collegiality and address competition for learning and practice opportunities. A pilot study investigating the feasibility of paired clinical placements with pairs of medical and physician assistant students found good acceptability of the learning experience by the students, with no additional burden reported by the supervisor.Citation26 Thus, in addition to actively developing relationships between medical student peers through experiences in the clinical setting, there is a need to incorporate early and ongoing deliberate experiences with other healthcare students while on placement. This should foster a culture of collaboration across all learners sharing patient encounters, practice opportunities, and learning experiences at the same placement location.
Additionally, the views of the teachers and other clinicians supervising the students while on clinical placements were not considered. Other studies have demonstrated that clinical educators report challenges from their perspective with increased student numbers,Citation11 including impacts on workload, physical limitations in the clinical working space, and the type and number of patients available for students to see. Increases in student numbers have also been perceived by teachers to negatively affect their ability to interact with students and identify those struggling, with subsequent detrimental effects on job satisfaction and burnout.Citation14 In contrast, there is preliminary evidence that the burdens on clinical placement providers are outweighed by the contributions of medical students to the healthcare environment,Citation27 so it is important to ensure that increasing student numbers does not detract from advantages to the healthcare team, patients, and the wider hospital.
Finally, this investigation was conducted at one UK medical school, and the results might not extend to other medical institutions. However, the students surveyed undertook clinical placements over multiple separate secondary healthcare settings, comprising larger university teaching hospitals and smaller district general hospitals and a /wide range of specialties, so the findings are likely to be representative of the “average” medical student experience in the UK and elsewhere in the world.
The changing clinical and educational environment will require an evolution in how we organize clinical teaching. When outlining strategies for expanding clinical capacity, Barnett et al. highlighted the need to “Refine the coordination, planning and administration of placements.”Citation13(p487) Our findings indicate that increasing student numbers may create challenges for those timetabling medical students on clinical placements in the future. They will need to be proactive in identifying where student overlap provides educational benefit and minimizing cross-over at particular crunch points where learning may be impaired. This would require careful coordination between administrative teams from medical, nursing, and physician associate courses, in collaboration with the clinical placement providers and engagement from other universities placing students at that location.
Training an increasing number of students may require sourcing new clinical placement opportunities too.Citation10 In the years since our institution was established in 2002 we have already expanded further into the region, with additional hospitals providing placements to the medical students and increased time in the community. In a nationwide study of the type of placements being used in Canada for training various healthcare professions including medical students, Smith et al.Citation28 identified a wide, diverse range of locations; thus highlighting the array of options available to expand into for clinical experience when combined with innovative learning and supervision strategies. Expanding clinical placements to more rural and community locations can both accommodate increased student numbers and help to address shortages of doctors in areas of lower population densities.Citation12,Citation13,Citation29 From the perspective of our findings, in previously underutilized clinical settings the senior students may have more autonomy and opportunities for lone working, and less competition to undertake the practice they need before graduating.
At NMS we now have a baseline for these student-student interactions and plan to monitor for any change as the format of clinical learning evolves and larger cohorts of medical students run through the MBBS. These observations will help inform course planning to maintain the clinical learning experience for our students as their numbers grow.
Conclusion
Medical students at NMS appear to regard interactions, particularly negative encounters, with their colleagues as a factor in determining satisfaction with clinical placements. There is unlikely to be a perfect optimization to these encounters, as it is probably not possible to have positive experiences without negative ones too. Nonetheless, for our students this balance seems to presently tip in the positive direction. The aim of our investigation was born out of concerns about students clashing on placements, and apprehension over how this may worsen with more students on the way, but our current snapshot would seem reassuring. Acknowledging these student-student interactions, both within and between professions, and introducing structured activities to enhance the benefits students are already gaining from learning alongside each other while on placement will become increasingly important to ensure future students continue to have a good learning experience with an increasing number of medical and other healthcare students training in the clinical setting.
Supplemental Material
Download PDF (668.8 KB)Disclosure statement
The authors report no declarations of interest.
References
- Association of American Medical Colleges. The complexities of physician supply and demand: projections from 2018 to 2033. 2020. https://www.aamc.org/system/files/2020-06/stratcomm-aamc-physician-workforce-projections-june-2020.pdf. Published 2020. Accessed April 25, 2021.
- Moberly T. UK has fewer doctors per person than most other OECD countries. BMJ. 2017;357:j2940. doi:10.1136/bmj.j2940.
- Royal College of Physicians. Underfunded, under-doctored, overstretched: The NHS in 2016. https://www.rcplondon.ac.uk/guidelines-policy/underfunded-underdoctored-overstretched-nhs-2016. Published September 21, 2016. Accessed November 30, 2020.
- Department of Health. 2017. Expansion of undergraduate medical education. Government response to consultation. https://www.gov.uk/government/consultations/expanding-undergraduate-medical-education. Published March 14, 2017. Accessed November 30, 2020.
- Eley DS, Young L, Wilkinson D, Chater AB, Baker P. Coping with increasing numbers of medical students in rural clinical schools: options and opportunities. Med J Aust. 2008;187(3):669–671.
- Dalen JE, Ryan KJ. United States medical school expansion: impact on primary care. Am J Med. 2016;129(12):1241–1243. doi:10.1016/j.amjmed.2016.05.021.
- Mallon WT. Medical school expansion: Déjà Vu all over again?Acad Med. 2007;82(12):1121–1125. doi:10.1097/ACM.0b013e318159cca6.
- Harris PF. Five new medical schools: a decline in standards is inevitable. BMJ. 2018;361. doi:10.1136/bmj.k1868.
- Hays RB, McKinley RK, Sen Gupta TK. Twelve tips for expanding undergraduate clinical teaching capacity. Med Teach. 2019;41(3):271–274. doi:10.1080/0142159X.2018.1429587.
- Smith PM, Corso LN, Cobb N. The perennial struggle to find clinical placement opportunities: a Canadian national survey. Nurse Educ Today. 2010;30(8):798–803. doi:10.1016/j.nedt.2010.02.004.
- Melvin JK, Byerley JS, Steiner MJ, Steiner B, Beck Dallaghan GL. Balancing clinical capacity with learner numbers. Clin Teach. 2020;17(1):13–21. doi:10.1111/tct.13103.
- Mlambo M, Dreyer A, Dube R, Mapukata N, Couper I, Cooke R. Transformation of medical education through decentralised training platforms: a scoping review. Rural Remote Health. 2018;18(1):4337. doi:10.22605/RRH4337.
- Barnett T, Walker LE, Jacob E, Missen K, Cross MD, Shahwan-Akl L. Expanding the clinical placement capacity of rural hospitals in Australia: displacing Peta to place Paul?Nurse Educ Today. 2012;32(5):485–489. doi:10.1016/j.nedt.2011.08.013.
- Mengistu BS, Vins H, Kelly CM, et al. Student and faculty perceptions on the rapid scale-up of medical students in Ethiopia. BMC Med Educ. 2017;17(1):11. doi:10.1186/s12909-016-0849-0.
- Kraakevik JA, Beck Dallaghan GL, Byerley JS, et al. Managing expansions in medical students’ clinical placements caused by curricular transformation: perspectives from four medical schools. Med Educ Online. 2021;26(1):1857322. doi:10.1080/10872981.2020.1857322.
- Imision C, Castle-Clarke S, Watson R. Reshaping the workforce to deliver the care patients need. Research Report. Nuffield Trust. https://www.nuffieldtrust.org.uk/research/reshaping-the-workforce-to-deliver-the-care-patients-need. Published May 17, 2016. Accessed November 30, 2020.
- Ritsema T. Faculty of Physician Associates census results 2018. Royal College of Physicians. https://www.fparcp.co.uk/about-fpa/fpa-census. Published 2018. Accessed November 30, 2020.
- Roberts S, Howarth S, Millott H, Stroud L. Experience of the impact of physician associates on postgraduate medical training: a mixed methods exploratory study. Clin Med (Lond). 2019;19(1):4–10. doi:10.7861/clinmedicine.19-1-4.
- Chou CL, Teherani A, Masters DE, Vener M, Wamsley M, Poncelet A. Workplace learning through peer groups in medical school clerkships. Med Educ Online. 2014;19(1):25809. doi:10.3402/meo.v19.25809.
- Sevenhuysen S, Farlie MK, Keating JL, Haines TP, Molloy E. Physiotherapy students and clinical educators perceive several ways in which incorporating peer-assisted learning could improve clinical placements: a qualitative study. J Physiother. 2015;61(2):87–92. doi:10.1016/j.jphys.2015.02.015.
- Tai J, Molloy E, Haines T, Canny B. Same-level peer-assisted learning in medical clinical placements: a narrative systematic review. Med Educ. 2016;50(4):469–484. doi:10.1111/medu.12898.
- Friel O, Kell D, Higgins M. The evidence base for peer assisted learning in undergraduate medical education: a scoping study. MedEdPublish. 2018;7(1). doi:10.15694/mep.2018.0000044.1.
- Bennett D, O’Flynn S, Kelly M. Peer assisted learning in the clinical setting: an activity systems analysis. Adv Health Sci Educ Theory Pract. 2015;20(3):595–610. doi:10.1007/s10459-014-9557-x.
- World Health Organization. Framework for action on interprofessional education & collaborative practice. https://apps.who.int/iris/handle/10665/70185. Published 2010. Accessed May 2021.
- Webb LA, Miles S, Bassi HK, Lindqvist SM, Bowker LK. Medical students’ views about interprofessional clinical skills sessions for delivering interprofessional education. Under Review.
- Pippit K, Moloney-Johns A, Jalilibahabadi S, Gren LH. Collaboration versus competition: an interprofessional education experience. Fam Med. 2015;47(4):298–301.
- Molloy E, Lew S, Woodward-Kron R, Delany C, Dodds A, Lavercombe M, Hughson J. Medical Student Clinical Placements as Sites of Learning and Contribution. Melbourne: University of Melbourne; 2018.
- Smith PM, Spadoni MM, Proper VM. National survey of clinical placement settings across Canada for nursing and other healthcare professions - who’s using what?Nurse Educ Today. 2013;33(11):1329–1336. doi:10.1016/j.nedt.2013.02.011.
- Tarimo CN, Kapanda GE, Muiruri C, et al. Building clinical clerkships capacity in a resource-limited setting: the case of the Kilimanjaro Christian Medical University College in Tanzania. Ann Glob Health. 2018;84(1):129–138. doi:10.29024/aogh.15.
