ABSTRACT
Complementary and alternative system of medicine has been at the center of drug discovery for different CNS disorders. Medicinal plants have been in use in healthcare settings and have interestingly fostered the leads for drug development aimed at treating various diseases such as CND disorders, malaria, mycetoma, and inflammation. Electroacupuncture (EA) has the ability to protect prolonged restraint stress, attenuate depressions, and manage few CNS disorders. Bacopa monnieri, Rhodiola rosea, Centella asiatica, Cannabis sativa, Curcuma longa, Cyperus rotundus, Morinda citrifolia, and Withania somnifera are among the most common plants used for treating CNS disorder. Bioactive compounds such as valtrate, curcumin, cannabinoids, apomorphine, pergolide, benzatropine, β-asarone, α-Asarone have been used to treat various CNS disorders, such as addiction, insomnia, depression, Alzheimer’s disease, epilepsy, vitiligo, Parkinson’s disease. These complementary and alternative system of medicines have promising lead in the quest to develop more drugs for CNS disorders.
Introduction
Complementary and alternative medicine (CAM) has been known as practices which intend to accomplish the healing effect of medicines; however, it may lack biological credibility, as it is usually not scientifically tested, cannot be tested, or has not been proven to be effective. Complementary medicine (CM), CAM, holistic medicine, and integrative medicine or integrated medicine (IM) are among several rebranding which describe same phenomenon[Citation1]. A typical traditional medical practice can become CAM when it is used in a way that is not in accordance with its original settings with no suitable scientific evidence and explanation. One of the most important goals of medical research is to translate the findings of basic research into beneficial medical developments. In neuropharmacology, it needs understanding the mechanism of disease and the effect of drugs and other compounds on neuronal functions.[Citation2]
The central nervous system (CNS) is part of the nervous system (NS) made up of mostly the spinal cord and brain. The central nervous system incorporates received information, then influences and coordinates the activities of all body parts. The central nervous system also includes the optic nerve, the retina, as well as olfactory epithelium and the olfactory nerves as part of the central nervous system, directly synapsing on the tissues of brain with no intermediate ganglia.[Citation3–5]
The discovery of drugs for the treatment of CNS disorders has faced some setbacks. Nervous system (NS) is vital to human body. In spite of the remarkable progress in knowledge of the CNS functions and structure, discovery of novel drugs along with their development for several central nervous system disorders have been challenging.[Citation2,Citation6,Citation7] Consequently, drug discoveries for CNS treatment and related development program have been experienced eliminations and cutbacks for decades. Complementary and alternative medicine has played a significant role in filling these gaps. CAM has guided the development of some drugs for the treatment of central nervous system (CNS) disorders. This often results in novel or enhanced treatment for CNS disease. In general, it has been noted that CNS drugs record higher rates of failure than their counterparts, clinically and preclinically; in certain areas like neurodegenerative diseases, there has been 100% rate of clinical failures for disease-modifying treatment.[Citation2] Alternative medicine has played a major role to fill this gap in many parts of the world.
Complementary and alternative medicine makes use of theories, practices, and products perceived or believed by people who make use of them to have healing effects; however, their efficacy has not been fully established using scientifically based approaches, or their practices and theories have no recognized part in biomedicine, or their practices and theories are contradicted directly with scientific evidence or biomedical principles.[Citation1,Citation8,Citation9] Medicine (biomedicine), as a part of medical sciences, makes use of principles of biophysics, biology, molecular theory, physiology, clinical practice, as well as other natural sciences, with scientific methodology to establish drug effectiveness. In contrast, alternative practices/products do not originate from making use of established scientific methods/principles, but often based on tradition, hearsay, pseudoscience, etc.[Citation8,Citation9]
Complementary and alternative medicines include various health-care therapies, products, and practices. One of the most notable CAM is the use of medicinal plants (herbs) and their bioactive components. Medicinal plants have been used as complementary and alternative therapies for the treatment of various diseases, including CNS disorders.[Citation10–12] Medicinal plants have been in use in health-care settings and have interestingly fostered the leads for drug development aimed at treating various diseases such as CND disorders, malaria, mycetoma, inflammation, etc. Bacopa monnieri, Centella asiatica, Curcuma longa, Cyperus rotundus, Morinda citrifolia, and Withania somnifera are among the most common plants used for treating CNS disorder.[Citation12] Many medicinal plants have been studied and found to contain important compounds and substances, which may be further explored to assess their beneficial use in the management of disorders such as CNS disorders.[Citation13–15]
This study intends to stimulate interest in studies and applications of various complementary and alternative system of medicine, such as plants, bioactive compounds, acupuncture, etc., as leading potentials for functional and structural novel development of active drugs for treatment of CNS disorders. summarizes major medicinal plants commonly used for treating specific CNS disorders. The central nervous system is a sophisticated and very complex, and its disorders are characteristically treated aiming at critical multiple or single targets. Traditional healers, who make use of CAM such as herbs, focus on distinct types of disease appropriate with their experiences and knowledge, instead of using a specified single biomarker targeted therapeutic measure as commonly used in medicine. Complementary and alternative medicine has been used along with functional medicinal treatments in a way that enhances the treatment effects.[Citation62] Acupuncture which usually involves body piercing using needles to affect the flow of energy may has been thought to complement or increase the effectiveness of science-based medicines when jointly used.[Citation63,Citation64] This alternative therapy has been noted in cancer therapy[Citation65–68] Complementary and alternative medicine has been widely recognized.[Citation69–72]
Table 1. Herbs effective against CNS Disorder.
Action mechanisms of some complementary and alternative medicine in treating disorders of central nervous system
The disorders of CNS are complicated, difficult, and usually require high cost for basic research and clinical therapies because of the mechanisms which are puzzling and most times unknown. Treating central nervous system disorders requires systematic targeted drugs which can pass via brain barriers to targeted precise receptors. Thus far, such systematic targeted drugs usually exhibit severe side effects. Recently, CAM has been vastly recommended and recognized as therapeutic by notable world health bodies, including FAO and WHO. Basic research, medicinal exploration, drug development, and clinical trials of complementary and alternative medicine have significantly increased due to increasing knowledge, awareness, and gradual development.[Citation7,Citation73]
Complementary and alternative medicine has been at the center of drug discovery for different disorders of CNS. Addiction to cocaine is one of the major health, social, and economic challenges in developed nations which influence many people. The development of novel drugs for the treatment of cocaine dependence is urgently required, although a few trials are already in their early stages. Cocaine is known to mostly bind to re-uptake transporters of dopamine, leading to pleasurable addiction. The species Rhodiola rosea L. is among the popular CAM that have anti-stress, anti-depressive, anxiolytic, and adaptogenic properties. Rhodiola rosea can decrease the withdrawal symptoms of morphine and nicotine. Rhodiola rosea has the capacity to potentiate cocaine-induced hyperactivities.[Citation7] It also reduced the expression and acquisition of conditioned place preference induced by cocaine. It is conclusive to state that R. rosea is effective in reducing cocaine rewarding properties, however, not in reinstatement associated with cocaine. Epileptic rats have been used to study the antiepileptic effects of and rhynchophylline and Uncaria rhynchophylla,[Citation7,Citation73] by injecting kainic acid (KA) in rats induced with Sprague-Dawley seizures. Pretreatment with rhynchophylline and Uncaria rhynchophylla can reliably ameliorate seizures occurring simultaneously with reduced mitogen-activated protein kinase (MAPK) c-Jun amino-terminal kinase phosphorylation (JNKp) signal pathways in hippocampus and cerebral cortex.[Citation7] TNF-α, IL-6, and IL-1β were reported not to be altered, meaning that rhynchophylline and Uncaria rhynchophylla therapeutic effects depend on activation of c-Jun amino-terminal kinase phosphorylation during seizure processes induced by kainic acid.
Guo et al.[Citation74] and Guo et al.[Citation75] showed that electroacupuncture (EA) has the ability to protect rat from prolonged restraint stress. Additionally, TGF-β, IL-6, andIL-1β were potentiated in rats with chronic restraint stress; it can be ameliorated by electroacupuncture pre-treatment. It was reported that electroacupuncture can ameliorate depressions accompanied by the alteration of TGF-β, IL-6, and IL-1β in hippocampal CA3 regions. Valtrate, a bioactive compound from Valeriana jatamansi Jones, has been used for treating several mood disorders and can simultaneously reduce depression and corticosterone levels in the serum of rats.[Citation7] Valtrate has shown anxiolytic effects in behavioral model via hypothalamus-pituitary-adrenal axis (HPA axis). The mechanisms discussed here implied that electroacupuncture and herbal medicine could activate similar mechanisms for the treatment of CNS disorders, including epilepsy and depression.
Lee et al.[Citation76] analyzed concurrent use of hypnotic drugs and Chinese herbal medicine therapies among Taiwanese adults with insomnia symptoms in a population-based study. They reported that 83.6% of the insomnia sufferers made use of hypnotic drugs. Suan-Zao-Ren-Tang and Jia-Wei-Xiao-Yao-San were continuously used and co-administered along with hypnotic drugs.[Citation76] They showed that the hip fracture hazard ratio for users of hypnotic drugs who also made use of herbal medicine was below that of those who used only hypnotic drugs. Their result is vital for clinical practices for reducing hip fractures. Additionally, their results are useful for quality of life and health of those with symptoms of insomnia. Complementary and alternative system of medicine has broad categories and mechanisms for treating several CNS disorders, symptoms, and diseases such as addiction, insomnia, depression, epilepsy, vitiligo, etc., with evidence-based medicines from the rudiments which often start with initial observation and basic research up to the expected outcomes which are usually clinical results and patients recovery.
Types of complementary and alternative medicine in use
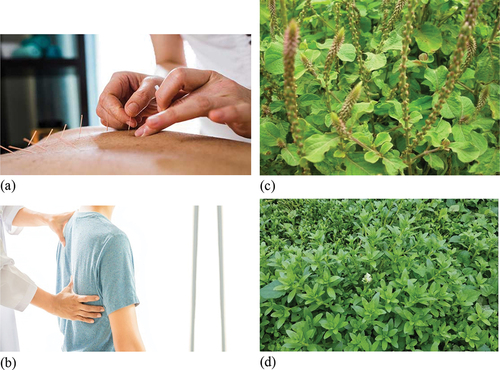
Complementary and alternative medicines include different health-care therapies, products, and practices, which are diverse in methodologies, applications, and foundations. CAM practices are usually classified based on the types of beliefs they are founded or based on their cultural origins.[Citation8] The methodologies may integrate or rely on traditional medicines and practices of a folk knowledge, culture, new concepts of disease and health, pseudoscience, belief in supernatural energies, etc.[Citation8] Each culture usually has its own unique belief or traditional-based health practices developed recently or hundreds, thousands, or even millions of years. shows some of the common CAM used in the management of CNS-related complications.
Figure 1. Complementary and alternative system of medicine in CNS disorders; (a) Acupuncture (b) Chiropractic (c) Achyranthes aspera (d) Enhydra fluctuans Lour.
Belief systems with no scientific base
Complementary and alternative medicines, including the use of homeopathy or naturopathy instead of conventional medicine (see ), are usually based on belief systems which are not often backed by scientific evidence.
Table 2. Use of homeopathy and naturopathy in complementary and alternative medicine.
Traditional systems and supernatural energies
Complementary and alternative system of medicine could rely on practices of traditional medicine, e.g. traditional medicine in Africa, Ayurveda in India, traditional Chinese medicine, etc., to treat some diseases such as CNS disorders, infections, etc. Few beneficial uses of traditional medicine have been studied and recommended in the context of ordinary medicine, although the basic belief is rarely backed by scientific evidence. Traditional medicines are regarded as alternatives when used in other places beyond their home regions; or when rationally expected that the practitioner or patient knows they may not work; or when used in place of or along with recognized functional treatment. In many parts of the world, there are beliefs in supernatural energy existence which are not detected by physical science or beliefs in activities of physics energies. shows the traditional system in CAM against CNS disorders. Plants such as Verbena officinalis, sweetgrass, cedar, sage, tobacco, etc., have been used in supernatural energies in many parts of the world for the healing of one CNS disorder or the other. These medicinal plants are used for the treatment of several disorders and are also used in many ceremonies.
Table 3. Traditional systems and supernatural energy used in complementary and alternative medicine for treatment of diseases like CNS disorders.
Use of herbs and other substances
Natural materials such as plants and plant-based compounds have been used for functional, therapeutic, medicinal, and prophylactic applications against various illnesses.[Citation97–99] Complementary and alternative medicine (CAM) practices make use of natural substances such as foods, herbs, minerals, fungal and animal products, megavitamins, and non-vitamin supplements, including using them in the practices of traditional medicine which may integrate other CAM or non-CAM methods[Citation96,Citation100,Citation101] for the treatment of diseases, including CNS disorders (see for herbs commonly used in treating CNS disorders). Typical examples include the therapeutic claims for ginseng, flaxseed oil, echinacea, Moringa oliefera extracts, glucosamine, Omega-3 fatty acid, fish oil, and nonvitamin supplements. Herbal medicines, also known as phytotherapy, comprise not only usage of plants and their products but could also include using mineral and animal products often in combination with plants. Herbal medicine is part of the major branches of CAM with commercial success, and includes elixirs, powders, and tablets, which are usually available in the form of nutritional supplements. Some herbal medicines have demonstrated to have efficacy in the treatment of diseases such as CNS disorders (see ), which often rely on the bioactive compounds present in them. Bioactive compounds have been described and studied in many natural products for various reasons and can be tapped for exploration against CNS-related diseases.[Citation102–105] Little regulation exists regarding the safety and standards of herbal medicines. Caution should be taken, as many natural products also contain toxic substances and even allergens.[Citation106]
Efficacy of complementary and alternative medicine
Some scientists maintain a firm opinion that CAM therapies do not have the sufficient requisite scientific-based validations, and as a result, their efficacy could not be ascertained.[Citation107] Additionally, most claims about the efficacies of CAM have either been controversial or exist with little or no established scientific evidence, as studies on them are often methodologically flawed and of low quality. Differences in standardization and product quality, selective publication bias, and certain companies that make unproven claims question the efficacies of isolated instances where CAM therapeutic evidence exists,[Citation108] including the treatment of health complications such as malaria, CNS disorders, viral diseases, etc. Someone not diagnosed using medicine with scientific basis may not have in the first instance had true disease identified as a category of alternative disease.[Citation109] Just like conventional drugs, medicines, interventions, and therapies, it may be hard to assess CAM efficacy using clinical trials. This often require high degree of expertise, awareness, and knowledge of CAM and its components. When an effectively established treatment for any health condition is available already, the Helsinki Declaration proclaims that suppressing the treatment is not ethical. Using treatment of standard-of-care along with CAM technique under testing could give difficult-to-interpret or confounded results.[Citation65,Citation110–113] Overall, establishing the efficacy of some CAM used in the treatment of CNS disorders has been challenging, with few recorded successes. However, the use of CAM in the treatment of illnesses such as CNS disorders has been known to be effective in traditional and modern medicines. Several experiments have validated most of these claims (see and 5.3).
Novel approaches in treatment of central nervous system disorders using complementary and alternative medicines
The NS touches every parts of the body, including the skin. Earliest charts of Chinese acupuncture are among the CAM approaches that indicate all the nerves are linked and jointly work to promote health and healthy living.[Citation73] The connection takes place via the brain, spine, and brain stems. Acupuncture is clearly analgesic through inhibiting potential cation channels of transient receptor in the skin.[Citation114] The chemokines role in pain has gradually been understood. Chemokines promote pains in skins and also activate ascending neural pathways which regulate the production of chemokines in nerves all over the body.[Citation115] Chronic pains are body experience which can influence the whole body.
Herbal medicine usage has been in place for thousands of years. Our forefathers partly survived using herbal medicines in treatment of diseases, including CNS disorders. The effectiveness of the herbal medicines largely lies on their constituent bioactive compounds and nutrients. In traditional settings, community and family supports are critical to health-care, such as health care for depression, anxiety, and mood.[Citation116] Religious practices have also been known to play significant roles in health management. Medical marijuana came into the limelight partly because of ganja use in religious rituals in India. The cautious choice of Cannabis sativa CNS active strains by ancient practitioners led to the use of marijuana in medicine today. Cannabis has received wide approval as psychoactive drug for medical and recreational purposes. The main psychoactive, bioactive compound in cannabis is tetrahydrocannabinol, one of the at least 483 known compounds in cannabis, including over 65 cannabinoids. Cannabidiol is also inclusive. Cannabidiol lotion are smoothly rubbed on cheeks for quick relieving of anxiety.[Citation117]
Herbs (sometimes called medicinal plants) are composite mixtures of bioactive plant materials that jointly work to promote health. Over the past 20,000 decades, the evolution of our bodies has stretched to make use of these herbal mixtures, usually as CAM and alternative therapy, or as medicines. Medicinal plants play a significant role in drug discovery for the treatment of various diseases, including CNS disorders, cardiovascular diseases, infection, etc. Some bioactive materials may enhance the other materials bioavailability.[Citation73] Some bioactive compounds could synergize or potentiate the actions of other bioactive constituents.[Citation118,Citation119] The search for single bioactive compounds in herbal medicine has resulted in the production of several drugs currently in use for the treatment of CNS disorders. Using complex herbal medicines could be significant for CNS complications which single bioactive compounds and modern medicines cannot treat effectively, including chronic pain and headaches.
Our body system is the most powerful medicine naturally available to us. In one way or the other, the human body has its unique way of recovering from illness, especially when there are sufficient nutrients, healthy lifestyle, and normal functioning of the body system (Awuchi et al., 2020a,b[Citation120]; b). Drugs just assist the body to heal by itself. This explains the reason why so-called miraculous healings have been largely believed, as our bodies heal themselves.[Citation121] The body heals itself when it is in balance, including balanced nutrition with little or no toxins, as well as healthy lifestyle and regular exercise.[Citation122] Regular exercise on daily basis is critical in achieving this balance. Balance involves ensuring our body is always in shape and strong, without being underweight, overweight, or obese. The heart, most important body part, requires moderate endurance exercise. Myokines produced by muscles during exercise help maintain healthy body.
Currently, standard health-care practices have not recorded huge rapid progress as was the case in the past. For most individuals, health quality has significantly reduced due to cardiovascular diseases, type 2 diabetes mellitus, obesity, depression, and similar diseases.[Citation123–126] Health-care providers have been giving several reasons for their patients’ lifestyle diseases.[Citation125,Citation126] It is high time we learned from traditional healers who maintain that a healthy lifestyle involving living and eating natural foods is vital to having good health.
Traditional medicines and medicinal plants as novel drugs for treatment of CNS disorders
Around one in every nine human deaths has been associated with CNS disorder globally, and at least 28% live with one form of disability or the other at some stage of their lives, as a result of nervous system disorder.[Citation127] Depression has been considered as one of the most causes of disability, which are more frequent globally than other CNS disorders. Top 20 leading causes of disabilities also include illicit drug use, Asperger syndrome, autism, schizophrenia, anxiety disorders, and dementias including Alzheimer’s disease.[Citation128] In traditional medicine, medicinal plants are used in treating several disorders such as CNS disorders for decades, as they are affordable and almost readily available. Recent traditional and complementary medicine (T&CM) global survey indicates that substantial progress has been made in the past decade.[Citation129]
In both developed and developing nations, traditional and complementary medicines are currently used by a significant percentage of the populations. In Europe, at least 100 million people currently make use of traditional and complementary medicines. Consequently, in Europe one in every five people make regular use of traditional and complementary medicines, and also prefer health care that includes traditional and complementary medicine.[Citation130] There is clear evidence of several more users of T&CM in Africa, North America, Australia, and Asia.[Citation131]
Traditional medicines have been one of the vehicles for drug discovery and could serve as sources of new supplements, phytomedicines, and bioactive compounds for the treatment of CNS disorders. Valproic acid, lisdexamfetamine, galanthamine, and apomorphine are currently used first-line drugs for treatment of epilepsy, attention-deficit/hyperactivity disorder, Alzheimer’s disease, and Parkinson’s disease, respectively. The bioactive compounds are originally obtained from Valeriana officinalis L., Ephedra sinica Stapf., Galanthus nivalis L., and Papaver somniferum L, respectively. For long, may regulatory authorities such as the FDA have approved some plant-based drugs, including apomorphine (obtained from morphine in plants such as P. somniferum), melevodopa (obtained from levodopa in plants such as Mucuna pruriens), pergolide (obtained from ergot alkaloids in plants such as Claviceps purpurea), carbidopa (obtained from levodopa in plants such as M. pruriens), and benzatropine (from atropine in plants such as Atropa belladonna) for the treatment of Parkinson’s disease. By 2013, reports indicated that the FDA approved at least 307 natural products and their derivatives from plants, marine organisms, fungi, and bacteria, making up to 21% of new chemical substances with approval.[Citation132]
The most common medicinal plants used in treating CNS disorders include Withania somnifera, Bacopa monnieri, Scoparia dulcis, Tabernaemontana divaricate, Coccinia grandis, Aegle marmelos, Stephania japonica, Centella asiatica, and Asparagus racemosus. Cyperus rotundus, Moringa oleifera, Morinda citrifolia, Curcuma longa, Achyranthes aspera, and Abroma augusta are also widely used in the management of CNS disorders.[Citation12,Citation133] All these plant species have shown notable therapeutic properties against CNS disorders in various studies (see ). The available scientific-based study evidence for Musa sapientum, Hemidesmus indicus, Euphorbia neriifolia, Datura metel, Curcuma longa, Curcuma aromatica, Convolvulus pluricaulis, Coccinia grandis, Clitoria ternatea, Centella asiatica, Bryophyllum pinnatum, Bacopa monnieri, Aegle marmelos, Achyranthes aspera, and Asparagus racemosus support CAM and T&CM claims. Additionally, pharmacological studies or trials are yet to be done for some medicinal plants used traditionally in treatment of various CNS disorders, including Bauhinia acuminata, Lygodium altum, Plumbago rosea, Solena amplexicaulis, and Typhonium trilobatum.[Citation12,Citation134] To cure nervous debility, mental disorder and insanity, epilepsy, paralysis, vitiligo, etc., are among regularly mentioned indications of CNS disorders. Most scientific-based study evidence has been made available for activities against some CNS disorders such as memory loss, mental disorder and insanity, and Alzheimer’s disease. Many other plants have been characterized, and this study recommends them for further study to explore their efficacies against disorders related to the central nervous system.[Citation135–141]
EVIDENCE-BASED MEDICINAL PLANTS and THEIR BIOACTIVE COMPOUNDS EFFECTIVE AGAINST CNS DISORDERS
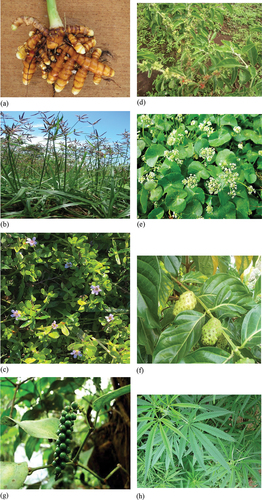
Several plant-based natural substances have been claimed to be effective against almost all CNS disorders. shows plant-derived bioactive compounds, which have already been studied and shown as effective candidates for drug development against CNS disorders. Some of the plants, including Withania somnifera, Morinda citrifolia, Cyperus rotundus, Curcuma longa, Bacopa monnieri, Centella asiatica, etc., are discussed in this section of the study, with more focus on their efficacies against CNS disorders. The major reason for giving detailed discussion on these plant species and their bioactive compounds is to draw attention to the large potentials of CAM in the form of traditional and complementary medicinal as leading candidates in for treating CNS disorders, from commercial and medicinal perspectives.
Table 4. Bioactive compounds effective against CNS disorders.
Curcuma longa, a perennial rhizomatous medicinal plant, belongs to the family of Zingiberaceae; it is used as herb and spice in many parts of the world. Curcuma longa and its bioactive constituents have been linked to cure for various illnesses, including CNS disorders. In addition to protecting memory loss, Curcuma longa contributes to several potential medicinal uses due to its bioactive constituents such as curcuminoids, which are suitable for drug development. Curcumin, a bright yellow natural bioactive compound isolated from Curcuma longa, especially its rhizome, has shown in vivo and in vitro neuropharmacological properties against memory impairment, neuro-inflammation, and various biomarkers of Parkinson’s disease and Alzheimer’s disease.[Citation157,Citation158] Curcumin has undergone clinical evaluation against few CNS disorders. Rainey-Smith et al.[Citation167] initially stated curcumin has a low efficiency against symptoms of dementia. But, recently developed novel formulations of curcumin (Theracurmin and Longvida) guarantee higher bioavailability, in combination with adequate chronic and acute activities for the two curcumin formulations, at all doses, including low doses (80 to 180 mg per day).[Citation168] Burns et al.[Citation169] carried out a study and reported a remarkable improvement in Déjérine-Sottas disease patient trials, where administration of curcumin was done in two escalating doses (2500 and 1500 mg per day) for 12 months. In another study, curcumin was found to reduce levels of salivary cortisol, TNFα, IL-1β, and increase plasma Brain-Derived Neurotropic factor (BDNF), in group treated with curcumin.[Citation170] Lopresti et al.[Citation171] found substantial rise in urinary molecular markers leptin, baseline plasma endothelin-1, substance P, and thromboxane B2, all of which can be associated with curcumin antidepressant action mechanism. In a systematic review, Costa et al.[Citation172] concluded that shared supplementation using curcuma longa reverses behavioral and neurotoxic damage in Alzheimer’s Disease. In another study, Reddy et al.[Citation173] evaluated the protective effects of curcumin against amyloid β induced synaptic and mitochondrial toxicities in Alzheimer’s disease, and reported that curcumin can protect against Alzheimer’s disease. Subedi and Gaire[Citation174] also reported the cellular and molecular mechanisms of curcumin’s neuroprotective effects in cerebral Ischemia.
Cyperus rotundus is an obnoxious weed and a perennial herb commonly found in some parts of the world, mostly in tropics and subtropics. Cyperus rotundus is traditionally used for treating epilepsy and paralysis some countries such as India and Bangladesh.[Citation175] Study has shown potentials of C. rotundus in enhancing cognition and memory. Cyperus rotundus rhizomes have anticonvulsant activities, anti-AChE activities, prevents pyramidal cell loss, and prevents memory loss.[Citation176,Citation177] In electrophysiological and behavioral studies, Nóbrega et al.[Citation147] reported that terpinen-4-ol in Cyperus rotundus essential oil has high effectiveness against convulsion. Additionally, Azimi et al.[Citation146] found that α-cyperone in C. rotundus has the ability to interact with tubulin and is also microtubule polymerization destabilizing agent. The interactions result in inflammation reduction that can benefit inflammatory disease treatment, including Alzheimer’s disease.
Bacopa monnieri is a small medicinal plant from the family of Plantaginaceae. Bacopa monnieri is used for sharpening cognitive functions and has been recognized as a constituent in several Ayurvedic preparations. Bacopa monnieri is consumed traditionally as leafy vegetable because of its known health benefits.[Citation178,Citation179] Scientific-based studies have shown B. monnieri potent activities on regulating reactive oxygen species, monoamine modulation and potentiation, increased cerebral blood flows, reduction of β-amyloid, activation of choline acetyltransferase, inhibition of acetylcholinesterase (AChE), and neuroprotection.[Citation180] Bacopa monnieri has triterpenoid saponins known as bacosides. Out of 12 bacosides analogs, bacoside A has been considered the most potent and most studied Bacopa monnieri component, which in addition includes bacopasaponin C, bacopaside II, bacoside A3, and bacopaside X (a bacosaponin C jujubogenin isomer).[Citation181] Bacoside A has been shown to have significant inhibitory effects against the toxicity of β-amyloid, reduced receptors of GABA associated with epilepsy, enhanced cognitive and memory functions, and fibrillation.[Citation182,Citation183] Bacoside A was also shown to increase activities of glutathione reductase, glutathione peroxidase, catalase, and superoxide dismutase.[Citation155,Citation183] Neale et al.[Citation184] conducted human trials review which made comparison of the nootropic effects of Panax ginseng and Bacopa monnieri nutraceuticals with a synthetic eugeroic drug called modafinil; in their comparative review, Bacopa monnieri showed largest effects and most consistent of all the three preparations tested.
Withania somnifera, also known as gooseberry, winter cherry, Indian ginseng, or ashwagandha, is a plant in the nightshade or Solanaceae family used in CAM for treatment of diseases, including CNS disorders. Of at least 23 Withania species, Withania somnifera is mostly valuable in traditional and complementary medicine. Different uses of Withania somnifera such as treating CNS disorders (e.g., memory loss, nervous tension, senile debility, and tonic) indicate its ethnopharmacological significance. Studies have shown its several activities against CNS disorders, especially anti-convulsant effects, anti-Alzheimer’s activities, nootropic activities, anti-Parkinson’s activities, anti-depression activities, anti-anxiety activities, neuroprotective activities, and neuritic regeneration activities.[Citation159,Citation185–188] The root is most commonly used part, and the bioactive compounds obtained from the root have shown effectiveness against CNS disorders. Withanoside IV and Withanolide A, which are steroidal lactones, diminished β-amyloid protein which enables the treatment of Alzheimer’s disease.[Citation189,Citation190] An in vivo study reported that the glyco-withanolides improved the levels of activities of several enzymes with antioxidant activities in the striatum and frontal cortex of rats, which could be significant for the treatment of Alzheimer’s disease.[Citation191]
Centella asiatica, also called Asiatic pennywort or Indian pennywort, is a herbaceous perennial plant which belongs to the flowering plants of Apiaceae family. It has kidney-shaped leaves, which are used in many traditional and complementary medicine such as Ayurvedic medicine for several centuries. Centella asiatica is applied as revitalizing medicinal plant to strengthen memory and function of nerves. In vivo, Centella asiatica leaves aqueous extracts contribute to enhanced memory and learning processes by the modulation of noradrenaline, 5-hydroxytryptamine, and dopamine systems in the brains of rats,[Citation192] suggesting that polar compounds, such as asiatic acid in the leaves of Centella asiatica, could improve cognitive functions through the influence on systems of neurotransmitter in the central nervous system. Further studies showed that the triterpenoid (asiatic acid) from Centella asiatica upregulates ADAM10 and downregulates β-secretase (BACE1) in primary cortical neurons of rat,[Citation193] prevents induced neurotoxicities in aged rats,[Citation194] diminishes cognitive deficiencies in mice induced by glutamate, and protects cells of SH-SY5Y against apoptosis induced by glutamate, all of which relate to possible routes in treatment of Alzheimer’s disease.[Citation195] Centella asiatica asiatic acid provided effective neuroprotection in chronic Parkinson’s disease through dopaminergic neuron activation.[Citation161] Orhan et al.[Citation196] demonstrated that butyryl cholinesterase inhibitory properties of Chinese Centella asiatica is less strong compared to that of South Asian Centella asiatica.
Morinda citrifolia is a tree in the coffee family, Rubiaceae, that bears fruit; it is commonly found in South Asia[Citation197] and Australia, as well as some other parts of the world where it is sparingly distributed. Every part of Morinda citrifolia have been reported to have several pharmacological activities, especially the fruit, which has long been used as a diet in tropical regions.[Citation198] In the European Union, fruit juice of Morinda citrifolia has been recommended as a novel food since 2002.[Citation199] Studies indicated that fruit juice of Morinda citrifolia has preventive properties against cerebral ischemic neuronal impairment on mice.[Citation200] Muto et al.[Citation201] showed that the fruit juice has protective effects on mice brains from cognitive dysfunction induced by stress, mostly decreasing the density of blood vessel resulting from stress. Administering ethyl acetate extracts of fruit juice of Morinda citrifolia increased antioxidant-enzyme, dopamine, and serotonin levels in serum in mice with cognitive dysfunction induced by beta-amyloid.[Citation202] The fruit ethanol extracts enhanced brain blood flow and memory and reduced acetylcholinesterase activities, oxidative stress, in mice.[Citation203] These factors have been implicated in many CNS disorders.[Citation203,Citation204] Behavioral studies showed that administering the fruits methanolic extract reduced the negative impacts of alcohol and heroin dependence.[Citation205] provides images of some of the commonly used medicinal plants in the treatment of CNS disorders.
Figure 2. Common medicinal plants effective against CNS disorders; (a) Curcuma longa (b) Cyperus rotundus (c) Bacopa monnieri (d) Withania somnifera (e) Centella asiatica (f) Morinda citrifolia (g) Piper cubeba (h) Cannabis sativa.
Many other natural materials, including flavonoids, nobiletin, cocoa, and fisetin, have been shown to exert important therapeutic actions against several altered states of the nervous system.[Citation206–208] Terpenoids and carotenoids, including astragaulus, are other important natural compounds shown to be effective for the treatment of neuronal disorders, astragaulus obtained from the Astragalus membranaceus, and other similar important compounds present many neuroprotective properties.[Citation209,Citation210] Nayak et al.[Citation211] reported the effects of Mucuna pruriens extract on histopathological and biochemical features in ischemia using rat model. Similarly, Neta et al.[Citation212] also reported the effects of Mucuna pruriens (L.) against Parkinson’s Disease.
Methods of application of complementary and alternative medicine
There are many methods used in the application of complementary and alternative medicine in many countries across the globe. Some of these include practices such as acupuncture, massage, drinking tea (e.g., green tea), tai chi, consumption of prepared plant extracts, etc.[Citation213,Citation214] Naturopathy, Homeopathy, Oriental/Chinese medicine, topical application, functional herbal therapy, etc., are used in many countries in Africa, Asia, Europe, and the Americas. Fjær et al.[Citation215] conducted a study on the use of CAM in Europe and reported that most commonly used methods of application of CAM include mind-body medicine (such as relaxation, spiritual, and meditative techniques); whole medical systems (such as acupuncture); body-based and manipulative practices (such as osteopathy, chiropractics, and massage); biologically based systems (such as vitamins, plants, phytochemical/plant extracts, and other natural products), and energy medicine.
Future prospects
There is a need for more studies focused on further exploring more complementary and alternative system of medicines for the treatment of CNS disorders, including anxiety, addiction, insomnia, depression, Alzheimer’s disease, epilepsy, vitiligo, Parkinson’s disease, among others. Most of the CAM therapies such as acupuncture, medicinal plants, bioactive compounds, chiropractic, bioelectromagnetic therapy, etc., need more scientific-based studies to firmly establish their use in developing drugs for CNS disorders. In addition, most of the medicinal plants used in treating CNS disorders have not received sufficient scientific attention. More studies need to be done to discover the phytoconstituents, including bioactive compounds, responsible for their healing effects for potential application in drug discoveries, scientific recognition, and clinical application.
Conclusion
Complementary and alternative system of medicine could rely on practices of traditional medicine, e.g. traditional medicine in Africa, Ayurveda in India, traditional Chinese medicine, etc., to treat some diseases such as CNS disorders, infections, etc. Complementary and alternative system of medicine has been at the center of drug discovery for different CNS disorders. Medicinal plants have been in use in health-care settings and have interestingly fostered the leads for drug development aimed at treating various diseases such CND disorders, malaria, mycetoma, inflammation, etc. Electroacupuncture (EA) has the ability to protect prolonged restraint stress, attenuate depressions, and manage few CNS disorders. Bacopa monnieri, Centella asiatica, Rhodiola rosea, Cannabis sativa, Curcuma longa, Cyperus rotundus, Morinda citrifolia, Withania somnifera, etc., are among the most common plants used for treating CNS disorder. Bioactive compounds such as Valtrate, curcumin, cannabinoids, apomorphine, pergolide, benzatropine, β-asarone, α-Asarone, etc., have been used to treat various CNS disorders, such as addiction, insomnia, depression, Alzheimer’s disease, epilepsy, vitiligo, Parkinson’s disease, etc. Complementary and alternative system of medicines have promising lead in the quest to develop more drugs for CNS disorders.
Acknowledgments
The Author is thankful to Kampala International University, Kampala, for providing the facilities used for this study.
Disclosure statement
No potential conflict of interest was reported by the author.
Data availability statement
Additional data will be made available on request
References
- Phutrakool, P.; Pongpirul, K. Acceptance and Use of Complementary and Alternative Medicine Among Medical Specialists: A 15-Year Systematic Review and Data Synthesis. Syst. rev. 2022, 11(1), 10. DOI: 10.1186/s13643-021-01882-4.
- Gribkoff, V. K.; Kaczmarek, L. K. The Need for New Approaches in CNS Drug Discovery: Why Drugs Have Failed, and What Can Be Done to Improve Outcomes. Neuropharmacology. 2016, 120, 11–19. DOI: 10.1016/j.neuropharm.2016.03.021.
- Estomih Mtui, M. J. T. F.; Gruener, G.2012.Clinical Neuroanatomy and Neuroscience.6thEdinburgh.Saundersp. 38.
- Gizurarson, S. Anatomical and Histologica Factors Affecting Intranasal Drug and Vaccine Delivery. Curr. Drug Delivery. 2012, 9(6), 566–582. DOI: 10.2174/156720112803529828.
- Purves, D.2000.NeuroscienceSecondSunderland, MA.Sinauer Associates.
- Awuchi, C. G.; Aja, M. P.; Mitaki, N. B.; Morya, S.; Amagwula, I. O.; Echeta, C. K.; Igwe, V. I.; Fernandez-Sanchez, J. F. New Psychoactive Substances: Major Groups, Laboratory Testing Challenges, Public Health Concerns, and Community-Based Solutions. J. Chem. 2023, 2023, 1–36. Volume 2023. Article ID 5852315 DOI: 10.1155/2023/5852315.
- Hsieh, C.L.; Lao, L.; Lin, Y.W.; Litscher, G. Complementary and Alternative Medicine for the Treatment of Central Nervous System Disorders. Evidence-Based Complementary and Alternative Medicine. Volume 2014, Article ID 175152. 2014, 2014, 1–2. DOI: 10.1155/2014/175152.
- Beyerstein, B. L. Alternative Medicine and Common Errors of Reasoning. Academic. Medicine. 2001, 76(3), 230–237. DOI: 10.1097/00001888-200103000-00009.
- Hines, T.2003.Pseudoscience and the Paranormal2ndAmerst, New York.Prometheue Books.
- Afzaal, M.; Saeed, F.; Ateeq, H.; Imran, A.; Yasmin, I.; Shahid, A.; Javed, A.; Shah, Y. A.; Islam, F.; Ofoedu, C. E., et al. Survivability of Probiotics Under Hostile Conditions as Affected by Prebiotic-Based Encapsulating Materials. Int. J. Food Prop. 2022, 25(1), 2044–2054. DOI: 10.1080/10942912.2022.2121836.
- Nyarko, R. O.; Awuchi, C. G.; Kumar, R.; Boateng, E.; Kahwa, I.; Boateng, P. O.; Asum, C.; Saha, P. Effect of Calotropis Procera Extract on Appetitte, Body Weight & Lipid Profile in Cafeteria Diet Induced Obesity in Experimental Animal. J. Res Appl Sci Biotechnol. 2022, 1(3), 107–113. DOI: 10.55544/jrasb.1.3.14.
- Uddin, J.; Zidorn, C. Traditional Herbal Medicines Against CNS Disorders from Bangladesh. Natural. Products and Bioprospecting. 2020, 10(2020), 377–410. DOI: 10.1007/s13659-020-00269-7.
- Kavitha, A.; Shanmugan, S.; Awuchi, C. G.; Kanagaraj, C.; Ravichandran, S. Synthesis and Enhanced Antibacterial Using Plant Extracts with Silver Nanoparticles: Therapeutic Application. Inorg. Chem. Commun. 2021, 134, 109045. DOI: 10.1016/j.inoche.2021.109045.
- Khan, A.; Nadeem, M.; Imran, M.; Gulzar, N.; Ahmad, M. H.; Tayyab, M.; Rahim, M. A.; Awuchi, C. G. Impact of Safflower Oil Derived Conjugated Linoleic Acid Supplementation on Fatty Acids Profile, Lipolysis and Sensory Properties of Cheddar Cheese. Int. J. Food Prop. 2022, 25(1), 2223–2236. DOI: 10.1080/10942912.2022.2130356.
- Zahnit, W.; Smara, O.; Bechki, L.; Souici, C. B.; Messaoudi, M.; Benchikha, N.; Larkem, I.; Awuchi, C. G.; Sawicka, B.; Simal-Gandara, J. Phytochemical Profiling, Mineral Elements, and Biological Activities of Artemisia Campestris L. Grown in Algeria. Horticulturae. 2022, 8(10), 914. DOI: 10.3390/horticulturae8100914.
- Dulla, O.; Jahan, F. I. Ethnopharmacological Survey on Traditional Medicinal Plants at Kalaroa Upazila, Satkhira District, Khulna Division, Bangladesh. J. Intercult. Ethnopharmacol. 2017, 6(3), 316–325. DOI: 10.5455/jice.20170719010256.
- Viswanatha, G. L.; Venkataranganna, M. V.; Prasad, N. B. L.; Godavarthi, A. Achyranthes Aspera Attenuates Epilepsy in Experimental Animals: Possible Involvement of GABAergic Mechanism. Brain. Dis. 2017, 32(3), 867–879. DOI: 10.1007/s11011-017-9981-8.
- Reddy, S.; Rao, G.; Shetty, B.; Hn, G. Turk. Neurosurg. 2015, 25(2015), 425–431.
- Yusuf, M.; Wahab, M. A.; Chowdhury, J. U.; Begum, J. Ethno-Medico-Botanical Knowledge from Kaukhali Proper and Betbunia of Rangamati District. J. Begum, Bangladesh J. Plant Taxon. 2006, 13(1), 55–61. DOI: 10.3329/bjpt.v13i1.594.
- Rahman, A. H. M. M. Medico-botanical study of commonly used angiosperm weeds of Rajshahi district, Bangladesh. Wudpecker J. Med. Plants. 2013, 2(3), 44–52.
- Uddin, M. Z.; Kibria, M. G.; Hassan, M. A. Study of Ethnomedicinal Plants Used by the Local People of Feni District, Bangladesh. J. Asiat. Soc. Bangladesh Sci. 2015, 41(2), 203–223. DOI: 10.3329/jasbs.v41i2.46205.
- Jash, R.; Chowdary, K. A. Ethanolic Extracts of Alstonia Scholaris and Bacopa Monniera Possess Neuroleptic Activity Due to Anti-Dopaminergic Effect. Res. 2014, 6(1), 46–51. DOI: 10.4103/0974-8490.122917.
- Walid, R.; Suvro, K. F. A.; Harun-Or-Rashid, M.; Mukti, M.; Rahman, S.; Rahmatullah, M. Ethnomedicinal plants of folk medicinal practitioners of two villages in Bagerhat district of Bangladesh. Am. Eur. J. Sustain. Agric. 2013, 7(2013), 61–74.
- Bhowmik, R.; Saha, M. R.; Rahman, M. A.; Islam, M. A. U. Ethnomedicinal Survey of Plants in the Southern District Noakhali, Bangladesh. Bangladesh Pharm. J. 2015, 17(2), 205–214. DOI: 10.3329/bpj.v17i2.22342.
- Thakur, A. K.; Rai, G.; Chatterjee, S. S.; Kumar, V. Beneficial Effects of an Andrographis Paniculata Extract and Andrographolide on Cognitive Functions in Streptozotocin-Induced Diabetic Rats. Pharm. Biol. 2016, 54(9), 1528–1538. DOI: 10.3109/13880209.2015.1107107.
- Chu, C. N.; Kim, J. W.; Chung, S. Y.; Park, J. H.; Seong, T. -Y.; An, B. H.; Kim, Y. K.; Park, J. H.; Do, Y. R.; Kim, W. Fabrication of Monolithic Polymer Nanofluidic Channels Using Nanowires as Sacrificial Templates. J. Oriental Neu- Ropsychiatry. 2010, 21(42), 43–57. DOI: 10.1088/0957-4484/21/42/425302.
- Rahmatullah, M.; Mollik, A. H.; Rahman, S.; Hasan, N.; Agarwal, B.; Jahan, R. Alter. Complement. Med. 2010, 16(2010), 419–425.
- Joshi, H.; Parle, M., 2012. Cognition Improving and Antioxidant Effects of Asparagus Racemosus Willd in Mice. Paper presented at 28th CINP world congress of neuropsychopharmacology, Stockholm, Sweden, 3–7 June 2012
- Ojha, R.; Sahu, A. N.; Muruganandam, A. V.; Singh, G. K.; Krishnamurthy, S. Asparagus Recemosus Enhances Memory and Protects Against Amnesia in Rodent Models. Brain. Cogn. 2010, 74(1), 1–9. DOI: 10.1016/j.bandc.2010.05.009.
- Uddin, S. N. Traditional Uses of Ethnomedicinal Plants of the Chittagong Hill Tracts. Bangladesh National Herbarium: Dhaka, 2006; 992.
- Kabir, M. H.; Hasan, N.; Rahman, M. M.; Rahman, M. A.; Khan, J. A.; Hoque, N. T.; Bhuiyan, M. R. Q.; Mou, S. M.; Jahan, R.; Rahma- Tullah, M. A Survey of Medicinal Plants Used by the Deb Barma Clan of the Tripura Tribe of Moulvibazar District, Bangladesh. J. Ethnobiol. Ethnomed. 2014, 10(1), 19. DOI: 10.1186/1746-4269-10-19.
- Yoneyama, T.; Arai, M. A.; Akamine, R.; Koryudzu, K.; Tsuchiya, A.; Sadhu, S. K.; Ahmed, F.; Itoh, M.; Okamoto, R.; Ishibashi, M.Notch Inhibitors from Calotropis giganteaThat Induce Neuronal Differentiation of Neural Stem Cells. J. Nat. Prod. 2017, 80(9), 2453–2461. DOI: 10.1021/acs.jnatprod.7b00282.
- Holgado, M. A.; Martín-Banderas, L.; Álvarez-Fuentes, J.; Fernández-Arévalo, M. Neuroprotective Effect of Cannabinoids Nanoplatforms in Neurodegenerative Diseases. J. Drug Delivery Sci. Technol. 2017, 42, 84–93. DOI: 10.1016/j.jddst.2017.04.023.
- Vallée, A.; Lecarpentier, Y.; Guillevin, R.; Vallée, J. N. Effects of Cannabidiol Interactions with Wnt/β-Catenin Pathway and Pparγ on Oxidative Stress and Neuroinflammation in Alzheimer’s Disease. Acta Biochim. Biophys. Sin. 2017, 49(10), 853–866. DOI: 10.1093/abbs/gmx073.
- Hegde, K.; Thakker, S. P.; Joshi, A. B.; Shastry, C. S.; Chandrashekhar, K. S. Anticonvulsant Activity of Carissa Carandas Linn. Root Extract in Experimental Mice. J. Pharm. Res. 2009, 8(2), 117–125. DOI: 10.4314/tjpr.v8i2.44519.
- Rahmatullah, M.; Noman, A.; Hossan, M. S.; Rashid, M. H.; Rahman, T.; Chowdhury, M. H.; Jahan, R. A survey of medicinal plants in two areas of Dinajpur district, Bangladesh including plants which can be used as functional foods. Am. Eur. J. Sustain. Agric. 2009, 3, 862–876.
- Ahmad, M. R.; Justin, A. T.; Manivasagam, T.; Nataraj, J.; Mohamed, M. E.; Chidambaram, S. B. Asiatic Acid Nullified Aluminium Toxicity in in vitro Model of Alzheimer Rsquo S Disease. Biosci. Elite Ed. 2018, 10(1), 287–299. DOI: 10.2741/e823.
- Azam, F. M. S.; Biswas, A.; Mannan, A.; Afsana, N. A.; Jahan, R.; Rahmatullah, M. Are Famine Food Plants Also Ethnomedicinal Plants? An Ethnomedicinal Appraisal of Famine Food Plants of Two Districts of Bangladesh. J. Evid. Based Complement. Altern. Med. 2014, 2014, 1–28. DOI: 10.1155/2014/741712.
- Prajapati, R.; Kalariya, M.; Umbarkar, R.; Parmar, S.; Sheth, N. Colocasia Esculenta: A Potent Indigenous Plant. Int. J. Nutr. Pharmacol. Neurol. Dis. 2011, 1(2), 90–96. DOI: 10.4103/2231-0738.84188.
- Bhatnagar, M.; Shukla, S. D.; Bhatnagar, R. Experimental Neurodegeneration in Hippocampus and Its Phytoremidation. J. Herb. Pharmacother. 2005, 5(2), 21–30. DOI: 10.1080/J157v05n02_03.
- Jabbar, S.; Khan, M. T.; Choudhuri, M. S. The Effects of Aqueous Extracts of Desmodium Gangeticum DC. (Leguminosae) on the Central Nervous System. Die. Pharmazie. 2001, 56(6), 506–508.
- Ibrahim, B.; Sowemimo, A.; van Rooyen, A.; Van de Venter, M. Antiinflammatory, Analgesic and Antioxidant Activities of Cyathula Prostrata (Linn.) Blume (Amaranthaceae). J. Ethnopharmacol. 2012, 141(1), 282–289. DOI: 10.1016/j.jep.2012.02.032.
- Motaleb, M. A.; Hossain, M. K.; Alam, M. K.; Mamun, M. M. A. A.; Sultana, M. Commonly Used Medicinal Herbs and Shrubs by Traditional Herbal Practitioners: Glimpses from Thanchi Upazila of Bandarban. International Union for Conservation of Nature and Natural Resources, Bolipara Nari Kalyan Somity, and Keidanren Nature. Conservation Fund. 2013, (2013), 294.
- Roy, S.; Dutta, S.; Chaudhuri, T. K. In vitro Assessment of Anticholinesterase and NADH Oxidase Inhibitory Activities of an Edible Fern, Diplazium Esculentum. J. Basic Clin. Physiol. 2015, 26(4), 395–401. DOI: 10.1515/jbcpp-2014-0100.
- Paul, A. K.; Al Arif, H.; Seraj, S.; Nahar, A.; Nasrin, D.; Chowdhury, M. H.; Islam, F.; Jahan, R.; Bashar, A. A.; Freedma, R., et al., A survey of plant items eaten by the low income groups of the rural population of Talbunia village in Bagerhat district, Bangladesh with an account of their folk medicinal applications. Am. Eur. J. Sustain. Agric. 2011, 5(1), 132–145.
- Roy, S. K.; Mazumder, U. K.; Islam, A. Pharmacological Evaluation Of Enhydra Fluctuans Aerial Parts For Central Nervous System Depressant Activity. Pharmacologyonline, 2011, 1(2011), 632–643.
- Awuchi, C. G.; Saha, P.; Amle, V. S.; Nyarko, R. O.; Kumar, R.; Boateng, E. A.; Kahwa, I.; Boateng, P. O.; Asum, C. A Study of Various Medicinal Plants used in Ulcer Treatment: A Review. J. Res. in Appl. Sci. Biotechnol. 2023, 2(1),234–246. DOI: 10.55544/jrasb.2.1.34.
- Mollik, A. H.; Hassan, A. I.; Paul, T. K.; Sintaha, M.; Khaleque, H. N.; Noor, F. A.; Nahar, A.; Seraj, S.; Jahan, R.; Chowdhury, M. H., et al. Am. Eur. J. Sustain. Agric. 2010, 1(2010), 349–357.
- Kundu, A.; Mitra, A. Flavoring Extracts of Hemidesmus Indicus Roots and Vanilla Planifolia Pods Exhibit in vitro Acetylcholinesterase Inhibitory Activities. Nutr. 2013, 68(3), 247–253. DOI: 10.1007/s11130-013-0363-z.
- Rudra, S.; Islam, K. N.; Rahman, M. M.; Uddin, S. B.2021.J. Herbs. Spices Med. Plants,2021.
- Shajib, M. S.; Akter, S.; Ahmed, T.; Imam, M. Z. Antinociceptive and Neuropharmacological Activities of Methanol Extract of Phoenix Sylvestris Fruit Pulp. Front. Pharmacol. 2015, 6(2015), 212. DOI: 10.3389/fphar.2015.00212.
- Mathew, M.; Subramanian, S.; Forloni, G. In vitro Screening for Anti-Cholinesterase and Antioxidant Activity of Methanolic Extracts of Ayurvedic Medicinal Plants Used for Cognitive Disorders. PLoS. One. 2014, 9(1), e86804. DOI: 10.1371/journal.pone.0086804.
- Rahman, M. A.; Uddin, S. B.; Wilcock, C. C., Indian J. Tradit. Knowl. 6(2007), 508–517 (2007).
- Amoateng, P.; Adjei, S.; Osei-Safo, D.; Kukuia, K. K.; Bekoe, E. O.; Karikari, T. K.; Kombian, S. B. Extract of Synedrella Nodiflora (L) Gaertn Exhibits Antipsychotic Properties in Murine Models of Psychosis. Med. 2017, 17(1), 389. DOI: 10.1186/s12906-017-1901-2.
- Ghani, A. Medicinal Plants of Bangladesh: Chemical Constituents and Uses, 2nd edn ed, Asiatic Society of Bangladesh: Dhaka, 2003; p. 603.
- Kadir, M. F.; Sayeed, M. S. B.; Setu, N. I.; Mostafa, A.; Mia, M. M. K. Ethnopharmacological Survey of Medicinal Plants Used by Traditional Health Practitioners in Thanchi, Bandarban Hill Tracts, Bangladesh. J. Ethnopharmacol. 2014, 155(1), 495–508. DOI: 10.1016/j.jep.2014.05.043.
- Nakdook, W.; Khongsombat, O.; Taepavarapruk, P.; Taepavarapruk, N.; Ingkaninan, K. The Effects of Tabernaemontana Divaricata Root Extract on Amyloid β-Peptide 25–35 Peptides Induced Cognitive Deficits in Mice. J. Ethnopharmacol. 2010, 130(1), 122–126. DOI: 10.1016/j.jep.2010.04.027.
- Singh, D.; Singh, A. The Toxicity of Four Native Indian Plants: Effect on AChE and Acid/Alkaline Phosphatase Level in Fish Channa Marulius. Chemosphere. 2005, 60(1), 135–140. DOI: 10.1016/j.chemosphere.2004.12.078.
- Faisal, M.; Hossain, A. I.; Rahman, S.; Jahan, R.; Rahmatullah, M. A Preliminary Report on Oral Glucose Tolerance and Antinociceptive Activity Tests Conducted with Methanol Extract of Xanthosoma Violaceum Aerial Parts. Med. 2014, 14(1), 335. DOI: 10.1186/1472-6882-14-335.
- Yeasmin, M.; Karmaker, S.; Hossain, M. S.; Ahmed, S.; Tabassum, A.; Malek, I. A case study of an urban garo tribal medicinal practitioner in Mymensingh district, Bangladesh. World J. Pharm. Pharmaceut. Sci. 2015, 4(12), 70–78.
- Roy, S.; Uddin, M. Z.; Hassan, M. A.; Rahman, M. M. Medico-Botanical Report on the Chakma Community of Bangladesh. Bangladesh J. Plant Taxon. 2008, 15(1), 67–72. DOI: 10.3329/bjpt.v15i1.929.
- May, J. What is Integrative Health? BMJ. 2011, 343(jul12 3), d4372. DOI: 10.1136/bmj.d4372.
- Borkan, J. Complementary Alternative Health Care in Israel and the Western World. Israel J. Health Policy Research. 2012, 1(1), 8. DOI: 10.1186/2045-4015-1-8.
- Awuchi CG. Important Medicinal and Aromatic Plants – Africa. Encyclopedia of Life Support Systems (EOLSS), Developed under the Auspices of UNESCO, ELOSS Publishers: Paris, France. 2023. 1–129.
- Zeller, T.; Muenstedt, K.; Stoll, C.; Schweder, J.; Senf, B.; Ruckhaeberle, E.; Becker, S.; Serve, H.; Huebner, J. Potential Interactions of Complementary and Alternative Medicine with Cancer Therapy in Outpatients with Gynecological Cancer in a Comprehensive Cancer Center. J. Cancer Res. Clin. Oncol. 2013, 139(3), 357–365. DOI: 10.1007/s00432-012-1336-6.
- Ben-Arye, E.; Polliack, A.; Schiff, E.; Tadmor, T.; Samuels, N.2013.Advising Patients on the Use of Non-Herbal Nutritional Supplements During Cancer Therapy: A Need for Doctor-Patient Communication.Journal of Pain and Symptom. Management,466:887–896.10.1016/j.jpainsymman.2013.02.010.
- Jeffery, N.2015.There is No Such Thing as Alternative Medicine.J.Small Animal Practice,5612:687–688.10.1111/jsap.12427.
- Li, B.; Forbes, T. L.; Byrne, J. Integrative Medicine or Infiltrative Pseudoscience? Surgeon. 2018, 16(5), 271–277. DOI: 10.1016/j.surge.2017.12.002.
- Zhang H. M; Luo D.; Chen R.; Wang S. H.; Zhao Y.J.; Li J.X.; Zhou M. F.; Yu Z. M.; Zhang J. L.; Liang F. X.; Research progress on acupuncture treatment in central nervous system diseases based on NLRP3 inflammasome in animal models. Front Neurosci. 2023 Feb 28,17,1118508. PMID: 36925735; PMCID: PMC10011106. Doi: 10.3389/fnins.2023.1118508.
- Ventola C. L. Current Issues Regarding Complementary and Alternative Medicine (CAM) in the United States: Part 2: Regulatory and Safety Concerns and Proposed Governmental Policy Changes with Respect to Dietary Supplements. P & T : a peer-reviewed journal for formulary management. 2010, 35(9), 514–522.
- Garrett, B.; Caulfield, T.; Murdoch, B.; Brignall, M.; Kapur, A. K.; Murphy, S.; Nelson, E.; Reardon, J.; Harrison, M.; Hislop, J.; Wilson-Keates; B. J.; Anthony, J.; Loewen, P. S.; Musoke, R. M.; & Braun, J. A taxonomy of risk-associated alternative health practices: A Delphi study. Health Soc. Care Community. 2022, 30 3, 1163–1181. DOI:10.1111/hsc.13386
- Tyreman, S. Values in Complementary and Alternative Medicine. PMIDMedicine, Health. Care and Philosophy. 2011, 14(2), 209–217. DOI: 10.1007/s11019-010-9297-5.
- Adams, J. D. Highlights of Complementary and Alternative Medicine in Nervous System Conditions: An Interview with Dr. James David Adams, Jr. OBM Complement. Integr. Med. 2019, 4(2), 1-1. DOI: 10.21926/obm.icm.1901014.
- Guo, Z.; Tu, Y.; Guo, T. W.; Wu, Y. C.; Yang, W.; Sun, L.; Yang, X. J.; Zhang, W.; Wang, Y.; Zhang, X. Electroacupuncture Pretreatment Exhibits Anti-Depressive Effects by Regulating Hippocampal Proteomics in Rats with Chronic Restraint Stress. Neuro. Regeneration Research. 2015, 10(8), 1298–1304. DOI: 10.4103/1673-5374.162764.
- Guo, T. W.; Guo, Z.; Zhang, W.; Ma, W.; Yang, X.; Yang, X.; Hwang, J.; He, X.; Chen, X.; Ya, T. Electroacupuncture and Cognitive Behavioural Therapy for Sub-Syndromal Depression Among Undergraduates: A Controlled Clinical Trial. Acupuncture. in Med. 2016, 34(5), 356–363. DOI: 10.1136/acupmed-2015-010981.
- Lee, K. H.; Tsai, Y. T.; Lai, J. N.; Lin, S. K. Concurrent Use of Hypnotic Drugs and Chinese Herbal Medicine Therapies Among Taiwanese Adults with Insomnia Symptoms: A Population-Based Study. Evid. Based Complement. Altern. Med. 2013, 2013, 987862. DOI: 10.1155/2013/987862.
- Ernst, E. A Systematic Review of Systematic Reviews of Homeopathy. Br. J. Clin. Pharmacol. 2002, 54(6), 577–582. DOI: 10.1046/j.1365-2125.2002.01699.x.
- Shang, A.; Huwiler-Müntener, K.; Nartey, L.; Jüni, P.; Dörig, S.; Sterne, J. A.; Pewsner, D.; Egger, M. Are the Clinical Effects of Homoeopathy Placebo Effects? Comparative Study of Placebo-Controlled Trials of Homoeopathy and Allopathy. Lancet. 2005, 366(9487), 726–732. DOI:10.1016/S0140-6736(05)67177-2. PMID 16125589, S2CID 17939264.
- Ernst, E. Rise in Popularity of Complementary and Alternative Medicine: Reasons and Consequences for Vaccination. Vaccine. 2001, 20(Suppl 1), S89–93. DOI: 10.1016/S0264-410X(01)00290-0.
- Jagtenberg, T.; Evans, S.; Grant, A.; Howden, I.; Lewis, M.; Singer, J. Evidence-Based Medicine and Naturopathy. J. Altern. Complement. Med. 2006, 12(3), 323–328. DOI: 10.1089/acm.2006.12.323.
- Sarris, J; Wardle, J. Clinical Naturopathy: An evidence-based guide to practice articulates evidence-based clinical practice, 3rd ed.; Jerome Sarris; Jon Wardle; September 1, 2019 ISBN: 9780729543026 1–944. Elsevier: Netherlands, 2019; p. 1.
- Breeher, L.; Mikulski, M. A.; Czeczok, T.; Leinenkugel, K.; Fuortes, L. J. A Cluster of Lead Poisoning Among Consumers of Ayurvedic Medicine. Int. J. Occup. Environ. Health. 2015, 21(4), 303–307. DOI: 10.1179/2049396715Y.0000000009.
- Centers for Disease Control Prevention. Lead Poisoning Associated with Ayurvedic Medications--Five States, 2000-2003. Morbidity. and Mortality Weekly Report 2004, 53(26), 582–584.
- Dasgupta, A.; Hammett-Stabler, C. A.2011.Herbal Supplements: Efficacy, Toxicity, Interactions with Western Drugs, and Effects on Clinical Laboratory Tests.Hoboken NJ,John Wiley and Sonspp. 202–205.
- Hall, H. “Ayurveda: Ancient Superstition, Not Ancient Wisdom”. Amherst, New York: Skeptical Inquirer, 2017.
- Saper, R. B., et al. Lead, Mercury, and Arsenic in US- and Indian-Manufactured Ayurvedic Medicines Sold via the Internet. JAMA. 2008, 300(8), 915–923.
- Valiathan, M. S. Ayurveda: Putting the House in Order. Guest Editorial. Current Science. 2006, 90(1), 5–6.
- Beyerstein, B. L.; Sampson, W. Traditional Medicine and Pseudoscience in China: A Report of the Second CSICOP Delegation (Part 1). Skeptical. Inquirer. 1996, 20, 4. Archived from the original on 2009-10-04
- Matuk, C. Seeing the Body: The Divergence of Ancient Chinese and Western Medical Illustration. (PDF). Journal of Biocommunication. 2006, 32(1), 1–8.
- Mwaka, A. D.; Abbo, C.; Kinengyere, A. A. Traditional and Complementary Medicine Use Among Adult Cancer Patients Undergoing Conventional Treatment in Sub-Saharan Africa: A Scoping Review on the Use, Safety and Risks. 2020, Volume 12(12), 3699–3712. DOI: 10.2147/CMAR.S251975.
- Bai James, P.; Wardle, J.; Steel, A.; Adams, J. Traditional, Complementary and Alternative Medicine Use in Sub-Saharan Africa: A Systematic Review. BMJ. Glob Health. 2018, 3(5), e000895. DOI: 10.1136/bmjgh-2018-000895.
- Rosa, L.; Rosa, E.; Sarner, L.; Barrett, S. A Close Look at Therapeutic Touch. JAMA. 1998, 279(13), 1005–1010. DOI: 10.1001/jama.279.13.1005.
- Hall, H. Applied Kinesiology and Other Chiropractic Delusions. Skeptical. Inquirer. 2020, 44(3), 21–23.
- Hansson, S. O. Science Denial as a Form of Pseudoscience. Studies in History and Philosophy of Sci. Part A. 2017, 63, 39–47. DOI: 10.1016/j.shpsa.2017.05.002.
- Strahinjevich, B.; Simpson, J. K.; The schism in chiropractic through the eyes of a 1st year chiropractic student. Chiropr. Man. Ther. 2018, 26, 2. DOI:10.1186/s12998-017-0171-x
- Frenkel, M.; David, A.; Sapire, K.; Hausner, D. Complementary and Integrative Medicine in Pancreatic Cancer. Curr. Oncol. Rep. 2023, 25(3),231–242. DOI:10.1007/s11912-023-01370-z
- Awuchi, C. G.; Twinomuhwezi, H.2021.The Medical, Pharmaceutical, and Nutritional Biochemistry and Uses of Some Common Medicinal Plants.Medicinal and Aromatic Plants of the WorldAmeenah G.F.B., in Encyclopedia of Life Support Systems (EOLSS), Developed under the Auspices of UNESCO,Ed.In Ozturk, M.ELOSS Publishers.Paris, France,Available athttps://www.eolss.net/Sample-Chapters/C03/E6-79a-14.pdf.
- Egbuna, C.; Awuchi, C. G.; Kushwaha, G.; Rudrapal, M.; Patrick-Iwuanyanwu, K. C.; Singh, O.; Odoh, U. E.; Khan, J.; Jeevanandam, J.; Kumarasamy, S., et al. Bioactive Compounds Effective Against Type 2 Diabetes Mellitus: A Systematic Review. Olisah and Chukwudi J. ChikwenduCurrent Topics in Medicinal Chemistry. 2021, 21(12), 1. DOI: 10.2174/1568026621666210509161059.
- Palai, S.; Kesh, S. S.; Awuchi, C. G.; Surajudeen, A. A.; Egbuna, C. Role of Phytochemicals in the Treatment of Ectoparasitic Infections: Scabies and Myiasis. In Neglected Tropical Diseases and Phytochemicals in Drug Discovery; Egbuna, C., Akram, M. Ifemeje, J., Eds.; Wiley: New Jersey, 2021; pp. 477–498. DOI:10.1002/9781119617143.ch20.
- De Smet, P. A. G. M. The Role of Plant-Derived Drugs and Herbal Medicines in Healthcare. Drugs. 1997, 54(6), 801–840. DOI: 10.2165/00003495-199754060-00003.
- Morya, S.; Awuchi, C. G.; Menaa, F. (2022a). Advanced Functional Approaches of Nanotechnology in Food and Nutrition. In: Kumar, V.& Hare, V. 2022a.Advanced Functional Approaches of Nanotechnology in Food and NutritionEnvironmental Management Technologies: Challenges and Opportunities,Chowdhary, P.pp. 257–272,New York.CRC Press. Taylor & Francis10.1201/9781003239956-16.
- Amagwula, I. O.; Osuji, C. M.; Omeire, G. C.; Awuchi, C. G.; Okpala, C. O. R. Combined Impact of Freezing and Soaking Times on Different Cowpea varieties’ Flour Functionality and Resultant Gel Strength, Sensory and Product Yield of Moi-Moi. AIMS Agric. Food. 2022, 7(4), 762–776. DOI: 10.3934/agrfood.2022047.
- Islam, F.; Noman, M.; Afzaal, M.; Saeed, F.; Ahmad, S.; Zubair, M. W.; Zahra, S. M.; Hussain, M.; Ateeq, H.; Awuchi, C. G., et al. Synthesis and Food Applications of Resistant Starch-Based Nanoparticles. J. Nanomater. 2022, 2022, 8729258. DOI: https://doi.org/10.1155/2022/8729258.
- Natumanya, P.; Twinomuhwezi, H.; Igwe, V. S.; Maryam, S.; Awuchi, C. G. Effects of Drying Techniques on Nutrient Retention and Phytochemicals in Selected Vegetables. European J. Agriculture Food Sci. 2021, 3(2), 5–14. DOI: 10.24018/ejfood.2021.3.2.247.
- Rafiq, S.; Sofi, S. A.; Kumar, H.; Kaul, R. K.; Mehra, R.; Awuchi, C. G.; Okpala, C. O. R.; Korzeniowska, M. Physicochemical, Antioxidant, and Polyphenolic Attributes of Microencapsulated Freeze-Dried Kinnow Peel Extract Powder Using Maltodextrin as Wall Material. J. Food Process. Preserv. 2022, 46(1), e16177. DOI: 10.1111/jfpp.16177.
- Morya, S.; Singh, N.; Awuchi, C. G. (2022b). Health Hazards of Food Allergens and Related Safety Measures. In: Kumar, V. & Hare, V. 2022b.Environmental Management Technologies: Challenges and Opportunities,Chowdhary, P.pp. 99–114,New York.CRC Press. Taylor & Francis10.1201/9781003239956-7.
- Goldrosen, M. H.; Straus, S. E. Complementary and Alternative Medicine: Assessing the Evidence for Immunological Benefits. Perspective. Nature Reviews Immunology. 2004, 4(11), 912–921. PMID 15516970. S2CID 11708302. DOI: 10.1038/nri1486.
- Sarris, J. “Current Challenges in Appraising Complementary Medicine evidence”(PDF). Medical J. Australia. 2012, 196(5), 310–311. DOI: 10.5694/mja11.10751.
- Alcock, J. Alternative Medicine and the Psychology of Belief. Sci. Rev. Altern. Med. 1999, 3(2).
- Bodeker, G., et al. A Public Health Agenda for Traditional, Complementary, and Alternative Medicine. Am. J. Public Health. 2002, 92(10), 1582–1591. DOI: 10.2105/AJPH.92.10.1582.
- Ernst, E. How Much of CAM is Based on Research Evidence? Evid. Based Complement. Altern. Med. 2011, 2011, 676490. DOI: 10.1093/ecam/nep044.
- Ernst, E.2008.“Placebo and Other Non-Specific Effects”Healing, Hype, or Harm? A Critical Analysis of Complementary or Alternative Medicine.Ernst, E.ed.Imprint Academic,Societas.
- Katz, D. L., et al. The Evidence Base for Complementary and Alternative Medicine: Methods of Evidence Mapping with Application to CAM. Alternative Therapies. in Health Med. 2003, 9(4), 22–30.
- Adams, J. D. The Effects of Yin, Yang and Qi in the Skin on Pain. Medicines. 2016, 3(1), 5. DOI: 10.3390/medicines3010005.
- Adams, J. D.; Guhr, S.; Villasenor, E. Salvia Mellifera—How Does It Alleviate Chronic Pain? Medicines. 2019, 6(1), 18. DOI: 10.3390/medicines6010018.
- Garcia, C.; Adams, J. D. Healing with Medicinal Plants of the West – Cultural and Scientific Basis for Their Use, third edition revis ed.; Abedus Press: La Crescenta, 2016.
- Mandolini, G.; Lazzaretti, M.; Pigoni, A.; Oldani, L.; Delvecchio, G.; Brambilla, P. Pharmacological Properties of Cannabidiol in the Treatment of Psychiatric Disorders: A Critical Overview. Epidemiol. Psychiat Sci. 2018, 27(4), 327–335. DOI: 10.1017/S2045796018000239.
- Awuchi, C. G.; Okpala, C. O. R. Natural Nutraceuticals, Especially Functional Foods, Their Major Bioactive Components, Formulation, and Health Benefits for Disease Prevention - an Overview. J. Food Bioactives. 2022, 19. DOI: 10.31665/JFB.2022.18317.
- Boubekeur, S.; Messaoudi, M.; Awuchi, C. G.; Otekunrin, O.; Sawicka, B.; Idjeri-Mecherara, S.; Bouchareb, S.; Hassani, A.; Sharifi-Rad, M.; Begaa, S., et al. Biological Properties and Polyphenols Content of Algerian Cistus Salviifolius L. Aerial Parts. European J. Biological Research. 2022, 12(2), 163–180. DOI: 10.5281/zenodo.6561505.
- Chinaza, G. A.; Echeta, C. K.; Igwe, V. S. Diabetes and the Nutrition and Diets for Its Prevention and Treatment: A Systematic Review and Dietetic Perspective. Health Sci.Res. 2020, 6(1), 5–19.
- Adams, J. D. Preventive Medicine and the Traditional Concept of Living in Balance. World J. Pharmacol. 2013, 2(3), 73–77. DOI: 10.5497/wjp.v2.i3.73.
- Awuchi, C. G.; Igwe, V. S.; Amagwula, I. O.; Nelson, K.; Madumere, C.; Obunaonye, C.; Nwobodo, F.; Orji, C. ASSESSMENT of TRACE METALS CONTAMINATION on SOIL from ABANDONED ARTISANAL TIN MINING PADDOCK in BARKIN-LADI AREA of PLATEAU STATE. Int. J. Adv. Acad. Res. 2020c, 6(1), 1–46. DOI: 10.46654/ij.24889849.e61112.
- Adams, J. D. Risk Factors for ObesityCardiovascular and metabolic disease scientific discoveries and new therapies; editors, Peplow P, Young T and Adams JD. Royal Society of Chemistry: London, 2015 pp. 59–65.
- Chinaza, G. A.; Igwe, V. S.; Amagwula, I. O. Ready-To-Use Therapeutic Foods (RUTFs) for Remedying Malnutrition and Preventable Nutritional Diseases. Int. J. Adv. Acad. Res. 2020b, 6(1), 47–81.
- Tufail, T.; Ijaz, A.; Noreen, S.; Arshad, M. U.; Gilani, S. A.; Bashir, S.; Din, A.; Shahid, M. Z.; Khan, A. A.; Khalil, A. A., et al. Pathophysiology of Obesity and Diabetes. In Dietary Phytochemicals; Egbuna, C. Hassan, S., Eds.; Springer: Cham, 2021; pp. 29–42. DOI:10.1007/978-3-030-72999-8_2.
- Yasmin, I.; Khan, W. A.; Naz, S.; Iqbal, M. W.; Awuchi, C. G.; Egbuna, C.; Hassan, S.; Patrick-Iwuanyanwu, K. C.; Uche, C. Z. Etiology of Obesity, Cancer, and Diabetes. In Dietary Phytochemicals; Egbuna, C. Hassan, S., Eds.; Springer: Cham, 2021; pp. 1–27. DOI:10.1007/978-3-030-72999-8_1.
- Bergen, D. C.; Silberberg, D. Nervous System Disorders. Neurol. 2002, 59(7), 1194–1196. DOI: 10.1001/archneur.59.7.1194.
- World Health Organization, 2020. Bangladesh. https://www.searo.who.int/bangladesh/mental-health/en. Accessed December 1 2020.
- WHO, 2013. WHO Traditional Medicine Strategy: 2014–2023. https://apps.who.int/iris/bitstream/10665/92455/1/9789241506090_eng.pdf. Accessed December 2 2020
- Zhang, Q. Global Situation and WHO Strategy on Traditional Medicine. Med. Mod. Med. 2018, 1(01), 11–13. DOI: 10.1142/S257590001820001X.
- Barnes, P. M.; Bloom, B.; Nahin, R. L. Complementary and alternative medicine use among adults and children: United States. Natl. Health Stat. Report. 2007, 12, 1–23.
- Patridge, E.; Gareiss, P.; Kinch, M. S.; Hoyer, D. An Analysis of FDA-Approved Drugs: Natural Products and Their Derivatives. Today. 2015, 21(2), 204–207. DOI: 10.1016/j.drudis.2015.01.009.
- Awuchi, C. G. Medicinal Plants: The Medical, Food, and Nutritional Biochemistry and Uses. Int. J. Adv. Acad. Res. 2019, 5(11), 220–241.
- Akram, M.; Adetunji, C. O.; Mohiuddin, E.; Oladosun, T. O.; Ozolua, P.; Olisaka, F. N.; Egbuna, C.; Olugbenga, S. M.; Adetunji, J. B.; Hameed, L., et al. Prospects of Phytochemicals for the Treatment of Helminthiasis. In Neglected Tropical Diseases and Phytochemicals in Drug Discovery; Egbuna, C., Akram, M. Ifemeje, J., Eds.; Wiley: New Jersey, 2021; pp. 199–223. DOI:10.1002/9781119617143.ch7.
- Awuchi, C. G.; Akram, M.; CG, A. Roles of Medicinal Plants in the Diagnosis and Treatment of Eumycetoma. In Neglected Tropical Diseases and Phytochemicals in Drug Discovery; Egbuna, C., Akram, M. Ifemeje, J., Eds.; Wiley: New Jersey, 2021; pp. 453–476. DOI:10.1002/9781119617143.ch19.
- Awuchi, C. G.; Igwe, V. S.; Amagwula, I. O.; Echeta, C. K. Health Benefits of Micronutrients (Vitamins and Minerals) and Their Associated Deficiency Diseases: A Systematic Review. International Journal of Food Sciences [S.L.]. Jan 2020, 3(1), 1–32. DOI: 10.47604/ijf.1024.
- Awuchi, C. G.; Twinomuhwezi, H.; Igwe, V. S.; Amagwula, I. O. Food Additives and Food Preservatives for Domestic and Industrial Food Applications. Journal of Animal Health, [S.L.]. apr2020, 2(1): 1–16.
- Costa, I. M.; Lima, F. O. V.; Fernandes, L. C. B.; Norrara, B.; Neta, F. I.; Alves, R. D.; Cavalcanti, J. R. L. P.; Lucena, E. E. S.; Cavalcante, J. S.; Rego, A. C. M., et al. Astragaloside IV Supplementation Promotes a Neuroprotective Effect in Experimental Models of Neurological Disorders: A Systematic Review. Curr. Neuropharmacol. 2019, 17, 648–665.
- Lastres-Becker, I.; Molina-Holgado, F.; Ramos, J. A.; Mechoulam, R.; Fernández-Ruiz, J. Cannabinoids Provide Neuroprotection Against 6-Hydroxydopamine Toxicity in vivo and in Vitro: Relevance to Parkinson’s Disease. Dis. 2005, 19(1–2), 96–107. DOI: 10.1016/j.nbd.2004.11.009.
- Messaoudi, M.; Rebiai, A.; Sawicka, B.; Atanassova, M.; Ouakouak, H.; Larkem, I.; Egbuna, C.; Awuchi, C. G.; Boubekeur, S.; Ferhat, M. A., et al. Effect of Extraction Methods on Polyphenols, Flavonoids, Mineral Elements, and Biological Activities of Essential Oil and Extracts of Mentha Pulegium L. Molecules. 2022, 27(1), 11. DOI: 10.3390/molecules27010011.
- Sarvarian, M.; Jafarpour, A.; Awuchi, C. G.; Adeleye, A. O.; Okpala, C. O. R. Changes in Physicochemical, Free Radical Activity, Total Phenolic and Sensory Properties of Orange (Citrus sinensis L.) Juice Fortified with Different Oleaster (Elaeagnus Angustifolia L.) Extracts. Molecules. 2022, 27(5), 1530. DOI: 10.3390/molecules27051530.
- Mukherjee, P. K.; Kumar, V.; Mac, M.; Houghton, P. J. vitroAcetylcholinesterase Inhibitory Activity of the Essential Oil from Acorus Calamu and Its Main Constituents. Planta. med. 2007, 733), 283–285. DOI: 10.1055/s-2007-967114.
- Somani, G. S.; Nahire, M. S.; Parikh, A. D.; Mulik, M. B.; Ghumatkar, P. J.; Laddha, K. S.; Sathaye, S. Neuroprotective Effect of Cubebin: A Dibenzylbutyrolactone Lignan on Scopolamine-Induced Amnesia in Mice. Indian J. Med. Res. 2017, 146(2), 255–159. DOI: 10.4103/ijmr.IJMR_156_14.
- Pandey, A.; Bani, S. Hydroxychavicol Inhibits Immune Responses to Mitigate Cognitive Dysfunction in Rats. J. Neuroimmunol. 2010, 226(1–2), 48–58. DOI: 10.1016/j.jneuroim.2010.05.031.
- Blázquez, C.; Chiarlone, A.; Sagredo, O.; Aguado, T.; Pazos, M. R.; Resel, E.; Palazuelos, J.; Julien, B.; Salazar, M.; Börner, C., et al. Loss of Striatal Type 1 Cannabinoid Receptors is a Key Pathogenic Factor in Huntington’s Disease. Brain. 2011, 134(1), 119–136. DOI: 10.1093/brain/awq278.
- Azimi, A.; Ghaffi, S. M.; Riazi, G. H.; Arab, S. S.; Tavakol, M. M.; Pooyan, S. α-Cyperone of Cyperus Rotundus is an Effective Candidate for Reduction of Inflammation by Destabilization of Microtubule Fibers in Brain. J. Ethnopharmacol. 2016, 194, 219–227. DOI: 10.1016/j.jep.2016.06.058.
- Nóbrega, F. F.; Salvadori, M. G.; Masson, C. J.; Mello, C. F.; Nascimento, T. S.; Leal-Cardoso, J. H.; de Sousa, D. P.; Almeida, R. N. Monoterpenoid Terpinen-4-Ol Exhibits Anticonvulsant Activity in Behavioural and Electrophysiological Studies. Med. Cell. Longev. 2014, 2014(2014), 1–9. DOI: 10.1155/2014/703848.
- Furukawa, Y.; Okuyama, S.; Amakura, Y.; Watanabe, S.; Fukata, T.; Nakajima, M.; Yoshimura, M.; Yoshida, T. Isolation and Characterization of Activators of ERK/MAPK from Citrus Plants. Int. J. Mol. Sci. 2012, 13(2), 1832–1845. DOI: 10.3390/ijms13021832.
- Fuentes, R. G.; Arai, M. A.; Sadhu, S. K.; Ahmed, F.; Ishibashi, M. Phenolic Compounds from the Bark of Oroxylum Indicum Activate the Ngn2 Promoter. J. Nat. Med. 2015, 69(4), 589–594. DOI: 10.1007/s11418-015-0919-3.
- Rayan, N. A.; Baby, N.; Pitchai, D.; Indraswari, F.; Ling, E. A.; Lu, J.; Dheen, T. Front. Biosci. Elite Ed. 2011, 3(2011), 1079–1091. DOI: 10.2741/e312.
- Ma, J.; Ren, Q.; Dong, B.; Shi, Z.; Zhang, J.; Jin, D. Q.; Xu, J.; Ohizumi, Y.; Lee, D.; Guo, Y. NO Inhibitory Constituents as Potential Anti-Neuroinflammatory Agents for AD from Blumea Balsamifera. Bioorg. Chem. 2018, 76(2018), 449–457. DOI: 10.1016/j.bioorg.2017.12.008.
- Eubanks, L. M.; Rogers, C. J.; Beuscher, A. E.; Koob, G. F.; Olson, A. J.; Dickerson, T. J.; Janda, K. D. A Molecular Link Between the Active Component of Marijuana and Alzheimer’s Disease Pathology. Pharm. 2006, 3(6), 773–777. DOI: 10.1021/mp060066m.
- Shiao, Y. J.; Su, M. H.; Lin, H. C.; Wu, C. R. Acteoside and Isoacteoside Protect Amyloid β Peptide Induced Cytotoxicity, Cognitive Deficit and Neurochemical Disturbances in vitro and in vivo. Int. J. Mol. Sci. 2017, 18(4), 895. DOI: 10.3390/ijms18040895.
- Alhebshi, A.; Gotoh, M.; Suzuki, I. Thymoquinone Protects Cultured Rat Primary Neurons Against Amyloid β-Induced Neurotoxicity. Biochem. Biophys. Res. Commun. 2013, 433(4), 362–367. DOI: 10.1016/j.bbrc.2012.11.139.
- Malishev, R.; Shaham-Niv, S.; Nandi, S.; Kolusheva, S.; Gazit, E.; Jelinek, R. Bacoside-A, an Indian Traditional-Medicine Substance, Inhibits β-Amyloid Cytotoxicity, Fibrillation, and Membrane Interactions. Chem. NeuroscEvaluation of Constituents of Piper Retrofractum Fruits on Neurotrophic Activityience. 2017, 8(4), 884–891. DOI: 10.1021/acschemneuro.6b00438.
- Kubo, M.; Ishii, R.; Ishino, Y.; Harada, K.; Matsui, N.; Akagi, M.; Kato, E.; Hosoda, S.; Fukuyama, Y. Evaluation of Constituents of Piper Retrofractum Fruits on Neurotrophic Activity. J. Nat. Prod. 2013, 76(4), 769–773. DOI: 10.1021/np300911b.
- Sorrenti, V.; Contarini, G.; Sut, S.; DallAcqua, S.; Confortin, F.; Pagetta, A.; Giusti, P.; Zusso, M. Curcumin Prevents Acute Neuroinflammation and Long-Term Memory Impairment Induced by Systemic Lipopolysaccharide in Mice. Pharmacol. 2018, 9(2018), 183. DOI: 10.3389/fphar.2018.00183.
- Van der Merwe, C.; van Dyk, H. C.; Engelbrecht, L.; van der Westhuizen, F. H.; Kinnear, C.; Loos, B.; Bardien, S. Curcumin Rescues a PINK1 Knock Down SH-SY5Y Cellular Model of Parkinson’s Disease from Mitochondrial Dysfunction and Cell Death. Neurobiol. 2017, 54(4), 2752–2762. DOI: 10.1007/s12035-016-9843-0.
- Konar, A.; Shah, N.; Singh, R.; Saxena, N.; Kaul, S. C.; Wadhwa, R.; Thakur, M. K. Protective Role of Ashwagandha Leaf Extract and Its Component Withanone on Scopolamine-Induced Changes in the Brain and Brain-Derived Cells. PLoS. One. 2011, 6(11), e27265. DOI: 10.1371/journal.pone.0027265.
- Zhang, Y.; Wang, L.; Song, M.; Qiao, L.; Song, M.; Wang, L. Hplc-ESI-MS/ms Analysis of the Water-Soluble Extract from Ziziphi Spinosae Semen and Its Ameliorating Effect of Learning and Memory Performance in Mice. Mag. 2014, 10(40), 509–516. DOI: 10.4103/0973-1296.141777.
- Nataraj, J.; Manivasagam, T.; Thenmozhi, A. J.; Essa, M. M. Neurotrophic Effect of Asiatic Acid, a Triterpene of Centella Asiatica Against Chronic 1-Methyl 4-Phenyl 1, 2, 3, 6-Tetrahydropyridine Hydrochloride/Probenecid Mouse Model of Parkinson’s Disease: The Role of MAPK, Pi3K-Akt-GSK3β and mTOR Signalling Pathways. Neurochem. Res. 2017, 42(5), 1354–1365. DOI: 10.1007/s11064-017-2183-2.
- VanGilder, R. L.; Kelly, K. A.; Chua, M. D.; Ptachcinski, R. L.; Huber, J. D. Administration of Sesamol Improved Blood–Brain Barrier Function in Streptozotocin-Induced Diabetic Rats. Brain. Res. 2009, 197(1), 23–34. DOI: 10.1007/s00221-009-1866-6.
- Esposito, G.; Scuderi, C.; Savan, C.; Steardo, L.; De Filippis, D.; Cottone, P.; Iuvone, T.; Cuomo, V.; Steardo, L.Cannabidiol in vivo Blunts β-Amyloid Induced Neuroinflammation by Suppressing IL-1β and iNOS Expression Br. J. Pharmacol. 2007, 151(8), 1272–1279. DOI: 10.1038/sj.bjp.0707337.
- Radad, K.; Moldzio, R.; Taha, M.; Rausch, W. D. Thymoquinone Protects Dopaminergic Neurons Against Mpp+and Rotenone. Res. 2009, 23(5), 696–700. DOI: 10.1002/ptr.2708.
- Okugawa, H.; Ueda, R.; Matsumoto, K.; Kawanishi, K.; Kato, A. Effect of α-Santalol and β-Santalol from Sandalwood on the Central Nervous System in Mice. Phytomedicine. 1995, 2(2), 119–126. DOI: 10.1016/S0944-7113(11)80056-5.
- Kazmi, I.; Afzal, M.; Ali, B.; Damanhouri, Z. A.; Ahmaol, A.; Anwar, F. Anxiolytic Potential of Ursolic Acid Derivative-A Stearoyl Glucoside Isolated from Lantana Camara L. (Verbanaceae). J. Trop. Med. 2013, 6(6), 433–437. DOI: 10.1016/S1995-7645(13)60069-3.
- Rainey-Smith, S. R.; Brown, B. M.; Sohrabi, H. R.; Shah, T.; Goozee, K. G.; Gupta, V. B.; Martins, R. N. Curcumin and Cognition: A Randomised, Placebo-Controlled, Double-Blind Study of Community-Dwelling Older Adults. J. Nutr. 2016, 115(12), 2106–2113. DOI: 10.1017/S0007114516001203.
- Small, G. W.; Siddarth, P.; Li, Z.; Miller, K. J.; Ercoli, L.; Emerson, N. D.; Martinez, J.; Wong, K. P.; Liu, J.; Merrill, D. A., et al. Memory and Brain Amyloid and Tau Effects of a Bioavailable Form of Curcumin in Non-Demented Adults: A Double-Blind, Placebo-Controlled 18-Month Trial. Am. J. Geriatr. Psychiatry. 2018, 26(3), 266–277. DOI: 10.1016/j.jagp.2017.10.010.
- Burns, J.; Joseph, P. D.; Rose, K. J.; Ryan, M. M.; Ouvrier, R. A. Effect of Oral Curcumin on Déjérine-Sottas Disease. Neurol. 2009, 41(4), 305–308. DOI: 10.1016/j.pediatrneurol.2009.04.030.
- Yu; Pei, L. B.; Zhang, Y.; Wen, Z. Y.; Yang, J. L. J. Clin. Psychopharmacol. 2015, 35(4), 406–410. DOI: 10.1097/JCP.0000000000000352.
- Lopresti, A. L.; Maes, M.; Meddens, M. J.; Maker, G. L.; Arnoldussen, E.; Drummond, P. D. Curcumin and Major Depression: A Randomised, Double-Blind, Placebo-Controlled Trial Investigating the Potential of Peripheral Biomarkers to Predict Treatment Response and Antidepressant Mechanisms of Change. Neuropsychopharmacol. 2015, 25(1), 38–50. DOI: 10.1016/j.euroneuro.2014.11.015.
- Costa, I. M.; Lima, F. O. V.; Fernandes, L. C. B.; Norrara, B.; Neta, F. I.; Alves, R. D.; JRLP, C.; Lucena, E. E. S.; Cavalcante, J. S.; Rego, A. C. M., et al. Astragaloside IV Supplementation Promotes a Neuroprotective Effect in Experimental Models of Neurological Disorders: A Systematic Review. Curr. Neuropharmacol. 2019, 17(7), 648–665. DOI: 10.2174/1570159X16666180911123341.
- Reddy, P. H.; Manczak, M.; Yin, X.; Grady, M. C.; Mitchell, A.; Kandimalla, R.; Kuruva, C. S. Protective Effects of a Natural Product, Curcumin, Against Amyloid β Induced Mitochondrial and Synaptic Toxicities in Alzheimer’s Disease. J. Investig. Med. 2016, 64(8), 1220–1234. DOI: 10.1136/jim-2016-000240.
- Subedi, L.; Gaire, B. P. Neuroprotective Effects of Curcumin in Cerebral Ischemia: Cellular and Molecular Mechanisms. ACS Chem. Neurosci. 2021, 12(14), 2562–2572. DOI: 10.1021/acschemneuro.1c00153.
- Panda, D.; Pradhan, S.; Palita, S. K.; Nayak, J. K. Ecol. Environ. Conserv. 2014, 20(2014), 35–38.
- Rabbani, M.; Ghannadi, A.; Malekian, N. Evaluation of the Effect of Cyperus Rotundus L. in Scopolamine-Induced Learning Deficit in Mice. Adv. Biomed. Res. 2014, 3(2014), 217–221. DOI: 10.4103/2277-9175.143293.
- Sharma, R.; Gupta, R. Cyperus Rotundus Extract Inhibits Acetylcholinesterase Activity from Animal and Plants as Well as Inhibits Germination and Seedling Growth in Wheat and Tomato. 2007, 80(24–25), 2389–2392. DOI: 10.1016/j.lfs.2007.01.060.
- Braun, L.; Cohen, M. Herbs and Natural Supplements: An Evidence-Based Guide; Churchill Livingstone Australia: London, 2014Vol. 2. p. 1384
- Islam, A. T. M. R.; Hasan, M.; Islam, T.; Rahman, A.; Mitra, S.; Das, S. K. Ethnobotany of Medicinal Plants Used by Rakhine Indigenous Communities in Patuakhali and Barguna District of Southern Bangladesh. J. Evid.-Based Integr. Med. 2020, 25, 2515690X20971586. DOI:10.1177/2515690X20971586.
- Sukumaran, N. P.; Amalraj, A.; Gopi, S. Neuropharmacological and Cognitive Effects of Bacopa Monnieri (L.) Wettst – a Review on Its Mechanistic Aspects. Ther. Med. 2019, 44(2019), 68–82. DOI: 10.1016/j.ctim.2019.03.016.
- Deepak, M.; Sangli, G. K.; Arun, P. C.; Amit, A. Quantitative Determination of the Major Saponin Mixture Bacoside a inBacopa Monnieri by HPLC. Phytochem. Anal. 2005, 16(1), 24–29. DOI: 10.1002/pca.805.
- Malishev, R.; Shaham-Niv, S.; Nandi, S.; Kolusheva, S.; Gazit, E.; Jelinek, R. Bacoside-A, an Indian Traditional-Medicine Substance, Inhibits β-Amyloid Cytotoxicity, Fibrillation, and Membrane Interactions. A.C.S. Chem, Neuroscience. 2017, 8(4), 884–891. DOI: 10.1021/acschemneuro.6b00438.
- Mathew, J.; Soman, S.; Sadanandan, J.; Paulose, C. S. Decreased GABA Receptor in the Striatum and Spatial Recognition Memory Deficit in Epileptic Rats: Effect of Bacopa Monnieri and Bacoside-A. J. Ethnopharmacol. 2010, 130(2), 255–261. DOI: 10.1016/j.jep.2010.04.043.
- Neale, C.; Camfi J, D.; Reay, C.; Stough, A.; Scholey, B. Cognitive Effects of Two Nutraceuticals Ginseng and Bacopa Benchmarked Against Modafinil: A Review and Comparison of Effect Sizes. J. Clin. Pharmacol. 2013, 75(3), 728–737. DOI: 10.1111/bcp.12002.
- Bhattacharya, S. K.; Bhattacharya, A.; Sairam, K.; Ghosal, S. Anxiolytic-Antidepressant Activity of Withania Somnifera Glycowithanolides: An Experimental Study. Phytomedicine. 2000, 7(6), 463–469. DOI: 10.1016/S0944-7113(00)80030-6.
- Jayaprakasam, B.; Nair, M. G. Cyclooxygenase-2 Enzyme Inhibitory Withanolides from Withania Somnifera Leaves. Tetrahedron. 2003, 59(6), 841–849. DOI: 10.1016/S0040-4020(02)01601-0.
- Kulkarni, S. K.; Akula, K. K.; Dhir, A. Ind. J. Experim. Biol. 2008, 46(2008), 465–469.
- RajaSankar, S.; Manivasagam, T.; Surendran, S. Neurosci. Lett. 2009, 454(2009), 11–15.
- Kuboyama, T.; Tohda, C.; Komatsu, K. Withanoside IV and Its Active Metabolite, Sominone, Attenuate Aβ(25-35)-Induced Neurodegeneration. Eur. J. Neurosci. 2006, 23(6), 1417–1426. DOI: 10.1111/j.1460-9568.2006.04664.x.
- Sehgal, N.; Gupta, A.; Valli, R. K.; Joshi, S. D.; Mills, J. T.; Hamel, E.; Khanna, P.; Jain, S. C.; Thakur, S. S.; Ravindranath, V. Withania Somnifera Reverses Alzheimer’s Disease Pathology by Enhancing Low-Density Lipoprotein Receptor-Related Protein in Liver. Natl. Acad. Sci. 2012, 109(9), 3510–3515. DOI: 10.1073/pnas.1112209109.
- Bhattacharya, S. K.; Satyan, K. S.; Ghosal, S. Antioxidant Activity of Glycowithanolides from Withania Somnifera. Indian J. Exp. Biol. 1997, 35(3), 236–239.
- Nalini, K.; Aroor, A. R.; Rao, A.; Karanth, K. S. Effect of Centella asiatica fresh leaf aqueous extract on learning and memory and biogenic amine turnover in albino rats. Fitoterapia. 1992, 63(1992), 231–238.
- Patil, S. P.; Maki, S.; Khedkar, S. A.; Rigby, A. C.; Chan, C. Withanolide a and Asiatic Acid Modulate Multiple Targets Associated with Amyloid-β Precursor Protein Processing and Amyloid-β Protein Clearance. J. Nat. Prod. 2010, 73(7), 1196–1202. DOI: 10.1021/np900633j.
- Haleagrahara, N.; Ponnusamy, K. Neuroprotective Effect of Centella Asiatica Extract (CAE) on Experimentally Induced Parkinsonism in Aged Sprague-Dawley Rats. J. Toxicol. Sci. 2010, 35(1), 41–47. DOI: 10.2131/jts.35.41.
- Xu, M. F.; Xiong, Y. Y.; Liu, J. K.; Qian, J. J.; Zhu, L.; Gao, J. Asiatic Acid, a Pentacyclic Triterpene in Centella Asiatica, Attenuates Glutamate-Induced Cognitive Deficits in Mice and Apoptosis in SH-SY5Y Cells. Sin. 2012, 33(5), 578–587. DOI: 10.1038/aps.2012.3.
- Orhan, I. E.; Atasu, E.; Senol, F. S.; Ozturk, N.; Demirci, B.; Das, K.; Sekeroglu, N. Comparative Studies on Turkish and Indian Centella Asiatica (L.) Urban (Gotu Kola) Samples for Their Enzyme Inhibitory and Antioxidant Effects and Phytochemical Characterization. Crops. Prod. 2013, 47(2013), 316–322. DOI: 10.1016/j.indcrop.2013.03.022.
- Das, S. C.; Rahman, M. A. Taxonomic Revision of the Genus Morinda L. (Rubiaceae) in Bangladesh. Bangladesh J. Bot. 2011, 40(2), 113–120. DOI: 10.3329/bjb.v40i2.9766.
- Wang, M. Y.; West, B. J.; Jensen, C. J.; Nowicki, D.; Su, C.; Palu, A. K.; Anderson, G. Acta Pharmacol. Sin. 2002, 23(2002), 1127–1141.
- Dussossoy, E.; Brat, P.; Bony, E.; Boudard, F.; Poucheret, P.; Mertz, C.; Giaimis, J.; Michel, A. Characterization, Anti-Oxidative and Anti-Inflammatory Effects of Costa Rican Noni Juice (Morinda Citrifolia L.). J. Ethnopharmacol. 2011, 133(1), 108–115. DOI: 10.1016/j.jep.2010.08.063.
- Harada, S.; Hamabe, W.; Kamiya, K.; Satake, T.; Tokuyama, S. Protective effect of Morinda citrifolia on the ischemic neuronal damage. Yakugaku Zasshi: J. Pharm. Soc. Jpn. 2009, 129(2), 203–207. DOI:10.1248/yakushi.129.203.
- Muto, J.; Hosung, L.; Uwaya, A.; Isami, F.; Ohno, M.; Mikami, T. Morinda Citrifolia Fruit Reduces Stress-Induced Impairment of Cognitive Function Accompanied by Vasculature Improvement in Mice. Behav. 2010, 101(2), 211–217. DOI: 10.1016/j.physbeh.2010.04.014.
- Muralidharan, P.; Kumar, V. R.; Balamurugan, G. Protective Effect of Morinda Citrifolia Fruits on β-Amyloid (25-35) Induced Cognitive Dysfunction in Mice: An Experimental and Biochemical Study. Res. 2010, 24(2), 252–258. DOI: 10.1002/ptr.2922.
- Pachauri, S. D.; Tota, S.; Khandelwal, K.; Verma, P. R. P.; Nath, C.; Hanif, K.; Shukla, R.; Saxena, J. K.; Dwivedi, A. K. Protective Effect of Fruits of Morinda Citrifolia L. on Scopolamine Induced Memory Impairment in Mice: A Behavioral, Biochemical and Cerebral Blood Flow Study. J. Ethnopharmacol. 2012, 139(1), 34–41. DOI: 10.1016/j.jep.2011.09.057.
- Butterfield, D. A.; Perry, G.; Avila, J.; Moreira, P. I.; Sorensen, A. A.; Tabaton, M. Perspectives on Oxidative Stress in Alzheimer’s Disease and Predictions of Future Research Emphases. J. Alzheimers Dis. 2018, 64(s1), S469–479. DOI: 10.3233/JAD-179912.
- Narasingam, M.; Pandy, V.; Mohamed, Z. Noni (Morinda Citrifolia L.) Fruit Extract Attenuates the Rewarding Effect of Heroin in Conditioned Place Preference but Not Withdrawal in Rodents. Anim. 2016, 65(2), 157–164. DOI: 10.1538/expanim.15-0088.
- Ludovici, V.; Barthelmes, J.; Nägele, M. P.; Enseleit, F.; Ferri, C.; Flammer, A. J.; Ruschitzka, F.; Sudano, I. Cocoa, Blood Pressure, and Vascular Function. Front. Nutr. 2017, 4, 36. DOI: 10.3389/fnut.2017.00036.
- Maher, P. Protective Effects of Fisetin and Other Berry Flavonoids in Parkinson’s Disease. Food. Funct. 2017, 8(9), 3033–3042. DOI: 10.1039/c7fo00809k.
- Nakajima, A.; Ohizumi, Y. Potential Benefits of Nobiletin, a Citrus Flavonoid, Against Alzheimer’s Disease and Parkinson’s Disease. Int. J. Mol. Sci. 2019, 20(14), 3380. DOI: 10.3390/ijms20143380.
- Costa, I. M.; Freire, M. A. M.; de Paiva Cavalcanti JRL; de Araújo DP; Norrara, B.; Moreira Rosa, I. M. M.; de Azevedo EP; Do Rego ACM; Filho, I. A.; Guzen, I. M. M., et al. Share Supplementation with Curcuma Longa Reverses Neurotoxic and Behavioral Damage in Models of Alzheimer’s Disease: A Systematic Review. Curr. Neuropharmacol. 2019, 17(5), 406–421. DOI: 10.2174/0929867325666180117112610.
- Yang, J.; Li, J.; Lu, J.; Zhang, Y.; Zhu, Z.; Wan, H. Synergistic Protective Effect of Astragaloside IV–Tetramethylpyrazine Against Cerebral Ischemic-Reperfusion Injury Induced by Transient Focal Ischemia. J. Ethnopharmacol. 2012, 140(1), 64–72. DOI: 10.1016/j.jep.2011.12.023.
- Nayak, V. S.; Kumar, N.; D’Souza, A. S.; Nayak, S. S.; Cheruku, S. P.; Pai, K. S. R. The Effects of Mucuna Pruriens Extract on Histopathological and Biochemical Features in the Rat Model of Ischemia. Neuroreport. 2017, 28(18), 1195–1201. DOI: 10.1097/WNR.0000000000000888.
- Neta, F. I.; Costa, I. M.; Lima, F. O. V.; Fernandes, L. C. B.; JRLP, C.; Freire, M. A. M.; Lucena, E. E. S.; Rego, A. C. M.; Araújo-Filho, I.; Azevedo, E. P., et al. Effects of Mucuna Pruriens (L.) Supplementation on Experimental Models of Parkinson’s Disease: A Systematic Review. Pharmacognosy. Rev. 2018, 12(23), 78–84. DOI: 10.4103/phrev.phrev_46_17.
- Khalid-Khan, S.; Khalid-Khan, F.; Gratzer, D.2015.Practical Applications of Complementary and Alternative Therapies in Adults and Youth with Anxiety Disorders.Ed.A Fresh Look at Anxiety Disorders.IntechOpen,10.5772/61046.
- Martin, J. H.; Patel, J. Complementary and Alternative Therapies in the Palliative Setting. Intern Med. J. 2022, 52(10), 1677–1684. DOI: 10.1111/imj.15922.
- Fjær, E. L.; Landet, E. R.; McNamara, C. L.; Eikemo, T. A. The Use of Complementary and Alternative Medicine (CAM) in Europe. BMC. Complement Med Ther. 2020, 20(1), 108. DOI: 10.1186/s12906-020-02903-w.
