ABSTRACT
The aim of this study was to explore interaction of interprofessional hospital trauma teams. A theory about how team cognition is developed through a dynamical process was established using grounded theory methodology. Video recordings of in-real-life resuscitations performed in the emergency ward of a Scandinavian mid-size urban hospital were collected and eligible for inclusion using theoretical sampling. By analyzing interactions during seven trauma resuscitations, the theory that trauma teams perform patient assessment and resuscitation by alternating between two process modes, the two main categories “team positioning” and “sensitivity to the patient,” was generated. The core category “working with split vision” explicates how the teams interplay between the two modes to coordinate team focus with an emergent mental model of the specific situation. Split vision ensures that deeper aspects of the team, such as culture, knowledge, empathy, and patient needs are absorbed to continuously adapt team positioning and create precision in care for the specific patient.
Introduction
Trauma teams are trained to organize task-work systematically in accordance with protocols for examining and resuscitating trauma patients (Van Olden et al., Citation2004) with team roles outlined in advance (Tiel Groenestege-Kreb et al., Citation2014). As the important coordination of trauma teams relies on communication and other non-technical skills, these aspects have become standard to teach in trauma simulation and teamwork training (Rosen et al., Citation2018). Effective non-technical skills help the teams reach emergent cognitive states, such as “a team mental model,” which in turn is associated with good medical performance (Johnsen et al., Citation2017; Westli et al., Citation2010). Those authors estimate team cognition through the assessment of behaviors associated with team cognition. Another approach is to compare how team members’ individual cognition overlap and thereby constitute an “emergent state of team cognition” (Coolen et al., Citation2019). Interactive team cognition is an approach to team cognition, which posits that team cognition is created through communication and interaction in a dynamic process coupled to task and other contextual conditions (Cooke et al., Citation2013). To examine such a dynamic process, behavior interaction data and verbal communication can be used (Huang et al., Citation2021).
The emergency medical environment is highly unpredictable and rapidly changing, and moderating factors such as cultural homogeneity, temporal dispersion and authority differentiation condition the role of team cognition for performance (Niler et al., Citation2021). This points to a need to understand the role of aspects relating to team cognition in the diversity of contexts appearing in health-care. Although a simulated environment may adequately represent the in-real-life (IRL) trauma environment, it is also possible that such an environment represents “work as imagined,” with less variable and dynamic contingencies that are easier to train for. Xiao et al. (Citation1996) observed in IRL teams that communication collapses may occur in escalating trauma resuscitation. Citation2017) revealed differences in emergency team’s structured interactions between three different situations in the same medical environment: simulation, “imagination of the reality,” and IRL. There is a paucity of research utilizing the IRL operational context that probably forms specific modes of sense-making and collaboration in teams.
This study of trauma teams was conducted primarily in an IRL environment to inductively investigate and formulate a theory about the significance of interaction between team members for the action phase of trauma team resuscitations
Background
The success of trauma resuscitation relies on teams made up of different professionals and disciplines for optimal treatment of patients requiring prompt care (Courtenay et al., Citation2013). Trauma is the leading cause of death among people<5 years in the Western world (Krug et al., Citation2000). Traditionally, emphasis has been put on individual task accomplishments; thus teams act “multiprofessionally.”As the teams are shaped “ad hoc,” team members differ from time to time (Courtenay et al., Citation2013).
The potential success of ad hoc teams presuppose handling problem-solving, coordination and workflow as “interprofessional teams,” imposing a high degree of cognitive complexity on the teams (Cooke et al., Citation2013). Team cognition can also be explained by cognitive states such as “team mental model” or “transactive memory,” which signify a team’s common understanding of how information can be organized or retrieved to anticipate and act accordingly (Kozlowski, Citation2018).
Although different concepts of team cognition have slightly different definitions, they all represent perceptual understanding and knowledge structures residing in the team that are continuously shaped and revised (Cooke et al., Citation2013; Porter-Oʼgrady et al., Citation2006). The acquisition and retention of a common mental model are deemed important for effective team processes of teams in general (DeChurch & Mesmer-Magnus, Citation2010; Marks et al., Citation2001; Mathieu et al., Citation2017; Mesmer-Magnus et al., Citation2017; Niler et al., Citation2021) and trauma teams in particular (Johnsen et al., Citation2017; Westli et al., Citation2010), and may be targeted through simulation training (Fernandez et al., Citation2017).
Health-care literature on team cognition is still “in its infancy” (Fernandez et al., Citation2017), and research that investigates how team dynamics unfold over time rather than describe static cognitive states has been called for (Kolbe & Boos, Citation2019). Depending on compositional and contextual factors, teams can be variably dependent on team cognition. A recent meta-analysis of moderating factors of team cognition used teams across domains to identify conditioning factors of team cognition for performance (Niler et al., Citation2021). Only one health-care team study that simulated two-person anesthesia teams could be included (Burtscher et al., Citation2011).
We found it valuable to expand this field with a study of trauma teams working in the IRL context. Unlike individual cognition, interactive team cognition can be studied by observing the behaviors of and interactions between team members (Porter-Oʼgrady et al., Citation2006), which provides information on how the team responds to internal and external forces to which they are exposed in IRL situations. These team dynamics were explored using a grounded theory approach.
Methods
Study design and setting
This grounded theory study used a constant comparative analysis of video-recorded material collected between June 2017 and February 2018 at the emergency ward of a mid-size Swedish hospital receiving 150–200 trauma patients per year.
Research paradigm and research team reflexivity
We aimed to study behavior in the action phase of trauma resuscitation and how interactions shape teamwork. Interaction, such as communication, is a social act that carries meaning and affects people. The grounded theory stems from post-positivism, which takes an objective stand to data and acknowledges a symbolic meaning to actions. This means that close examination of data collected will present a pattern of how the small parts connect into a bigger picture, or a theory about a social process. This methodology was originally developed by Barney Glaser to explain how social circumstances affect the actions and experiences of people. The Glaserian variant is purely inductive and allows the empirical data studied to guide the whole process, including the formulation of the research question, sampling, and literature review. In this process the researcher is considered relatively unaffected by pre-conception but get deeply immersed in the data during the process, and will be eventually enriched by experience and impressions that aids in theory building (Glaser & Holton, Citation2005).
We found this methodology to suit our project inquiry and that Glaser’s view of an “objective reality out there” fits better with an observational study of interactions than e.g. Charmaz’s constructivist grounded theory, which aims to reconstruct an experienced reality. The primary researcher (LF) is a female anesthesiologist with 12 years’ experience and trauma resuscitation team member on demand. As the present study was her first study on team cognition and interaction, she did not have preconceived ideas about teamwork processes. IM is a female emergency medicine resident, at the time working at the hospital where the study was conducted and is a trauma resuscitation team member on demand. At the time of the study, KL was a female medical student, had no clinical or contextual experience but had a cultural background from another Scandinavian country. A primary researcher with minimal medical experience would have grasped less of the communication but would have had less pre-understanding. However, we wanted the results to be founded on the interactions made, and the researchers naturally did not form a theory regarding the medical situation but coded the interactions for their symbolic meaning concerning teamwork. We find this to be coherent with Glaser’s idea that researcher should not enter the field with preconceived theories and ideas to which they force the data (Glaser & Strauss, Citation1967;Urquhart, Citation2002).
The coding and analysis process were performed by LF, under continuous guidance by CB. CB is a female registered nurse and PhD who is skilled in emergency and critical care, with clinical experience from another hospital. She is a lecturer on qualitative methodology at the university and has profound research experience in qualitative methods, especially grounded theory methodology. The use of a single coder is customary in the grounded theory (Hoare et al., Citation2012;Willumsen & Hallberg, Citation2003). The use of an unexperienced coder is also encouraged if skilled supervision is ensured (Glaser, Citation1978). Interpretation and reporting of results were made in conjunction with the rest of the research group, LN and KB, who are both female PhD-degree anesthesiologists working at a university hospital, with extensive research experience in the fields of anesthesiology and patient safety (LN) and anesthesiology and cellular biology (KB).
Ethical approval and consent
Ethics approval was received from the Ethical Review Board in Linköping, Sweden (No:2017/32–33). Information was given to hospital employees engaging in trauma resuscitation before the study started through group meetings and e-mail. Written consent was obtained in conjunction with the given information or after a data recording. No analysis was undertaken before consent was obtained from all active health-care participants visible in the video. The Ethical Review Board waived patient informed consent. The face of the patient was blurred out and made unrecognizable. The patients’ identities were not familiar to the researchers, and the focus of the study was on team interaction.
Data collection and context
A trauma team pager assembled the emergency trauma team in response to a trauma patient approaching or entering the trauma bay. The trauma teams consisted of 9–13 members representing different professions and medical specialties but unique individuals each time. The roles that were represented in all teams and constituted the core group are displayed in (). All physicians, except interns, were skilled with Advanced Trauma Life Support certification, and all registered nurses with Trauma Nurse Core Course certification.
Table 1. Roles represented in all trauma teams.
The primary survey is the initial assessment of a trauma patient, which is aimed at identifying and treating any life-threatening injuries quickly. The teams evaluated and resuscitated the patients according to resuscitation structure called c (external bleeding)-A (airway)-B (breathing)-C (circulation)-D (disability)-E (exposure).
Recordings from two cameras and one microphone in the emergency room were activated by a nurse not part of the trauma team. The videos were edited (LF) so that only the primary survey process after the handover from the retrieving ambulance or corresponding entry was visible/audible. Nineteen consecutive videos were collected, of which two were erased owing to lack of consent. Four recordings were simulations in the same environment, activated through the regular trauma pager system and recorded and edited similarly to real-life videos.
Theoretical sampling
Theoretical data sampling (Glaser, Citation1978) was performed from the video material collected in advance, that is 17 recorded resuscitations of 10–14 minutes’ duration. LF, IM and KL transcribed five of these eligible videos for studying verbal interaction (Molin et al., Citation2021). The videos (V) consisted of intense communication, sometimes including parallel dialogs between team members, which required around 10 working hours per video and researcher. This data pool (video, untranscribed video and transcripts) was turned and returned to for theoretical sampling. How the video material was going to be approached and used in this grounded theory analysis was not decided beforehand but guided by the process.
Orienting phase
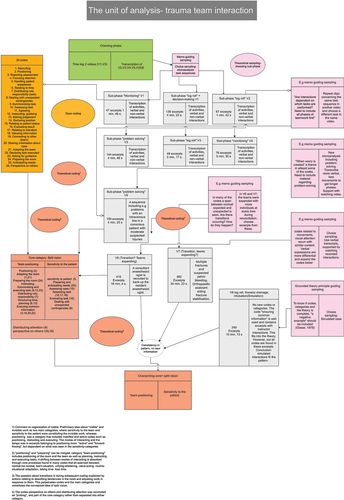
Video materials contain enormous interactional details and needs selection (Derry et al., Citation2010). This study aimed to investigate interactions in teams during the action-phase of a primary survey. LF, IM, and KL watched and transcribed the verbal interactions in five videos (V2, V3, V4, V5, and V8) to apprehend the entirety of the situation. All resuscitations were found to include recurring sub-phases such as patient log-roll, intra-venous line placement, specific task procedures, and problem-solving phases. LF and IM agreed on the sub-phases seen in the videos. LF then watched and took notes from two whole videos (V1 and V3), creating a timeline of team structural re-formation, tasks, and occurrences to reveal a starting point for theoretical sampling. The use of such an orienting phase is serviceable in an inductive study using video material (Derry et al., Citation2010) and has been used in other grounded theory studies (Hoare et al., Citation2012). Memos written during the orienting phase were used to initiate theoretical sampling, which started with choosing two different sub-phases of teamwork, namely opening phase “monitoring” and “patient log-roll.” A sub-phase from a video clip can be selected in order to decompose video material into material that can be micro-analyzed (Derry et al., Citation2010). A chosen sub-phase was transcribed using the Maxqda software (LF) for verbal utterances intertwined with movements in the room, gazes and activities. The grounded theory is founded on observations that seem important on the basis of the actual analysis step, and this often relates to actions – interactions in the chosen setting with a focus on the social process studied (Fathi Najafi et al., Citation2016). Later, coding was performed primarily on verbal interactions, supported by watching interaction sequences ().
Data analysis
Open coding (Glaser, Citation1978;Patton, Citation2015) of the selected material and constant comparison of the incidents/excerpts, codes, and emerging categories was made. A code is a cognitive symbol with an outer behavior and a loaded inner meaning. The classic grounded theory methodology proclaims that three questions are asked to the data to find out the substantial meaning of every incident and code (Glaser, Citation1978): “What is this data a study of?,” “Which category or sub-category does this incident indicate?,” “What happens in the data?” The content of the code was kept in the excerpt belonging to it and followed through the analysis as the codes were grouped into categories. For instance, the code “assessing task” was created from different excerpts of interactions, such as V4: “anesthesiologist: “Are we going to log-roll and all that now? Are you sure that you want to do that? Maybe we should take him to the CT?¨ The rest of the team looks at the anesthesiologist. “What do we get from a log-roll?” From another case V6: Examining physician: “I would be happy if you would just stitch up with some single sutures, and get the plaster cast on.” All the excerpts belonging to this code concerned tasks and some valuing about if, why, how, and when. Every time a code was identified, its content was compared with the content already included in that code and with other codes and excerpts belonging to them. This trajectory of coding enriched a code or category with the excerpt content that thus had both the objective (behavior) and subjective (meaning) contents, that the coder found in the excerpts included in that code/category. In the last example above, the objective meaning of the excerpt could be “expressing how he wants the procedure done,” whereas the underlying meaning could be “pacing up a procedure.” Ultimately, 193 excerpts of interactions from the studied material were included in the code “assessing task.”
Memos are notes taken throughout the process and a memo written in conjunction with excerpts belonging to the code example above was “He (examining physician) asks the orthopedic surgeon about how much time he has left; he seems worried about the patient, wants to hurry?” “Assessing task” relates to “coordinate and plan” (another code). Memos were written to help in theory building and to understand the relationship between codes. Excerpts, codes, and memos were kept in an Excel file, which made it possible to sort and compare codes and coding families as the volume of data increased. A logbook including longer memos that also summarized the content of each code and how codes related to each other were written, and a scheme of codes was also drawn on paper for visualization during the process. Two preliminary categories were formed that were initially thought to represent “the visible” and “the invisible work,” which later in the process was named “team positioning” and “sensitivity to the patient.” The codes “perspective on others,” “distributing attention,” and the code “relating to time” intersected the two categories and were eventually found to constitute a core that spans between the different modes of working. This core was named “split vision.”
The core category “working with split vision” explicates how teams work with the two process modes through this “team sense,” a way of perceiving and acting that ensures appropriate motion between the two process modes ().
Figure 2. The “split vision” theory.

Interactions from seven IRL trauma resuscitations and one in-situ simulation were included in the final analysis ().
Table 2. Videos from which materials used for the study were obtained.
The coding process was undertaken in parallel to the inclusion and comparison of new data until the new data did not alter the pattern, and the theory was deemed tenable () (Glaser, Citation1965). This means that the inclusion of more data did not present a different pattern or alter the theoretical proposition. The literature review was undertaken subsequent to theory formation and accounted for the integration of the theory into the existing literature (Glaser, Citation1978).
Results
The two main categories, “team positioning” and “sensitivity to the patient,” are explained below, followed by the core category, “split vision.” The categories are interpretative in nature and represent a theoretical model based on the iterative comparisons of empirical data. The theory is therefore outlined in the present tense, whereas the observed behavior used to illustrate some of the occurrences in data is written in the past tense.
Team positioning
Team positioning is the “making of work,” including the team’s executive function, accomplishing tasks and managing workflow. In team positioning, seemingly automatic behavior is used and accounts for the speed and effectiveness significant for this process mode. Team positioning represents the team’s self-image as a solid unit able to take action and move forward as such.
Team members’ physical positioning in the room affected their ability to perform and influence the situation through their own activity and role-taking. Moving close to the patient created proximity to the working team center and thereby raised this possibility. The use of reviews, directives, or correction by a formal team leader attributed leadership as expected. When the need for a review was announced by another team member, it hinted that leadership was absent or not keeping pace with the team members or the situation, and such a call thereby forces the formal leader into the expected positioning.
In team positioning, case-related information and status details are made available to the team members. Sharing facts contributes to the fellowship regarding the process of understanding and collective responsibility for future steps.
Results according to expectation moved the teams forward in time, as new parts of the preset structured protocol were accomplished. Meeting the needs of the protocol and staying effective were expressed and valued by the team and thereby appeared central. Task scheduling and use of common effective language perpetuated the teams’ positioning function, enabling the anticipation of preparative work, workload, and competence, which effectuated the plan at hand. Compliance to the agreed positioning, conversation style, and protocol fulfillment could also bring specific satisfaction to a team.
This seemingly productive team process mode needs continuous reestablishment to stay in line with situational needs. Accordingly, the teams interacted in valuing processes where detailed instructions were launched. These formed the category “sensitivity to the patient,” which represents a conceptual idea about another process mode of the team.
Sensitivity to the patient
Team individuals comprehended aspects of the situation and shared them in between, resulting in valuing processes. Such interactions were founded in and creates the category “sensitivity to the patient.” As the examination proceeds and results are verbalized by the positioning team, the ability to make qualified trade-offs in response to the acquired competence increases through switching to “sensitivity to the patient.” This accounts for a team cognitive state, entrained by emotions and reflexive empathy. It seemed that team members were allowed to interact freely in this process mode.
Evaluative discussions were conducted in a disjointed and irregular manner, distinct from the rigid and standardized conversation structure manifested by the positioning team. As this process mode was given time, creativity, and the possibility to extract experience, team introspection could emerge from the interaction between the protocol standards and the input of the patient’s medical history and other values sensed by team members.
The conversation style in this mode seemed founded in a mutual agreement about cooperation. The specific force found in the positioning team’s directive and coordinating communication was absent, slowing the process and broadening the interaction scope. It also allowed the extraction of competence from specific individuals or going deep into reflection, which accounts for a flattening of hierarchy. This makes it a process of knowledge building for the present and future.
Responsive patients communicated with the team and attracted attention to the need for comfort, explanation, and participation. Irregular and hampering responsive communication toward the patient relocated attention from team members, which disabled team unification and disrupted reevaluations. However, constant interaction with the patient seemed to create familiarity and assured the patient’s well-being. Likewise, the unresponsive patient helped the team interpret the situation’s acuteness. Sensing the patient thus helps to adapt the process tempo. Communicating to the patient was found central in this mode, but some of the communications toward the patient were categorized into the positioning mode. Such communications regarded instructions and planning, which involved the patient, but also directed the team. The patient could thus constitute a part of the team in “team positioning,” rather than just the object of attunement and consideration in “sensitivity to the patient.”
Working with “split vision”
The phenomenon of “split vision” is an extraordinary sense defined as “an ability to simultaneously see different possibilities.” “Split vision” is used by teams to monitor team processes and maintain a course between a predefined process mode and a process mode from which emergent situational understanding could be extracted.
A “split vision” requisite is a shared team self-image, including a common presumption about the starting point, objectives, and team possibilities, which form a baseline for alternation. This presumption rests in the category team positioning. Team members perceived others in the team, thereby staying informed about where knowledge and expertise could be obtained and if roles and tasks needed to be reestablished. This included taking notice of task achievements to comprehend other individuals and where they found themselves in the process. For example in V4: emergency nurse: “But then we have to gather us, if we are to … ” when the team is planning to insert one more intra venous cannula and, at the same time remove the trauma transfer stretcher and prepare drugs and equipment for sedation and intubation. This process demands patience and empathy and could be a key behavior that shapes team culture. It is a reflective act contributing to a continuous learning process.
Expectations and presumptions about work were developed through experience and knowledge obtained through team interactions. When teams use “split vision,” they continuously probe performance according to the expectations created by the protocol standard and the group’s experience. The teams had to stay open to new impressions and interpretations about the immediate reality. Absorbing other perspectives contributes to the creation of updated anticipation.
The probing of others enabled the process to flow, as other individuals could help with problem resolution or essential task synchronization, such as in V7, where the emergency nurse asks the airway nurse to give the patient intra-venous Ringer’s acetate but gets the response, “Soon, I can,” and the emergency nurse answers, “But I can do it myself (prepare the fluid), so she can put the ‘IV‘ in.” A problem resolution could be undertaken parallel to other processes. At times, a team member loudly declared the problem and thus requested the team to focus on the problem. This represents a shift to “team positioning,” in which the problem was given attention, required engagement from many parts, altered the present plan, or needed coordination, or a sub-group of the team was “running out of options.” Sometimes, it was also a way of assuring that the team was in agreement and will take mutual responsibility for reaching a solution. “Split vision” allows for gearing up or down in response to situational needs.
Discussion
The findings of this inductive study suggests that trauma teams are equipped with a common cognitive ability, a “split vision.” The core category “split vision” connects the categories of “positioning of the team” and “sensitivity to the patient” and produces a set of theoretical propositions.
Trauma resuscitation has escalation potential (Xiao et al., Citation1996), and “split vision” helps the team set a suitable pace. The protocol standard and training demand efficacy, yet individual deflections might increase accuracy for a particular patient. “Split vision” is an unspoken screening activity that the team members collectively use, which is subtly expressed in their interaction in between. Such screening to meet accuracy and functionality in response to a specific situation seems to be an important component of team adaptability in this context.
Interpretation of findings
Team orientation facilitates team performance through increased involvement, strategizing, and goal sharing (Salas et al., Citation2005). Mutual agreement about expected work and the current situation is probably required in the use of “split vision.” The trauma team is dedicated to the team and tasks and will share objectives and the starting point, and formal leadership is assigned to the team leader. The time frame for the assembling and dissolving team is also defined in hospital standards (Barach & Weinger, Citation2007). This agreement is presumably a preconceived self-image for the trauma team entering the resuscitation room and can be understood as part of a common team mental model. A team that has reformed during operation strives to restore its position by altering to a positioning mode. This might be tacitly understood but can also be negotiated.
In our study, the hierarchy was at times allowed to flatten, as seen in the category “sensitivity to the patient.” The team leader facilitated team processes by synchronizing and combining contributions from all individual team members. It can be proposed that leadership can be altered during trauma resuscitation, depending on situational needs. This requires sensing, to which “split vision” can contribute.
The team might be unaware of balancing ethical and medical values, but how this is performed is unique to the trauma team’s particular culture. As the team is shaped ad hoc, it is logical that pre-set standards and training form the baseline. However, how the patient status screening, explained by the category “sensitivity to the patient,” is allowed to mold the operative style and pace signals that the team has self-confidence regarding clinical judgment when the situation is perceived as complex or goes beyond standards. Furthermore, standards and protocols noticed in the category “team positioning” can be put aside for the patient’s benefit when needed. Regardless of team type, it seems that such adaptation is essential for the fine-tuning of performance to meet needs (Burke et al., Citation2006). Our study illustrates how the team can function rather unaltered in the positioning mode but shifts with increased complexity to the sensitivity mode, where distinct adaptation behavior dominates. Complexity does not, in this regard, necessarily imply that the patient is more severely wounded. It has to do with having to make multiple assumptions when the situation deviates from pre-set standards. The lower pace used in the sensitivity mode is logical, as it requires both assessment and plan formulation.
In our analysis, the teams used probing of others, which resembles “mutual performance monitoring” and “back-up behavior,” as described by Salas et al. (Citation2005) Knowledge is built from continuous monitoring of other team members’ achievements, commentaries, and sharing of their own information and status details. Such behavioral processes are believed to be important for team adaptation, specifically in highly interdependent teams (Burke et al., Citation2006), which means that teams can equalize the burden on their members by recognizing overload and filling gaps in knowledge or task liberation. “Probing of others” emerged as a central feature to effectuate “split vision,” which also illustrated interdependence in the team. “Probing of others” complement the existing knowledge about monitoring other team members in the generation of a perspective on time, without explicit formulation, and this perpetuates “split vision.”
Understanding how team cognition is established and updated is important for the possibility of making environmental changes and for creating adequate needs specification for team training. The team members apply tools that are combined medical and interactive experiences in response to multiple contextual factors that alter otherwise potentially stereotypical care. This study underlines the need to strive for cognitive fidelity simulation, even though the real-world-context is difficult to mimic. Interactions are specified to the actual patient on the basis of feelings, relationships, and presumptions about the future – considerations that are difficult to stimulate in simulation training. What was observed in the positioning mode illustrated the “action,” which resembled what the manuals and simulation training teach; however, sensitivity to the patient mode was entrained by interactions with patients that considered their feelings and experiences. Our findings could be used to implement more training in creative decision-making, evaluation, and plan formulation in team training. Such training could be designed as case discussions and mental simulations, and strategized to encourage the teams to reach solutions to nonstandard situations where ethical problems, ill-structured problem formulation, and technical shortcomings are included.
A relevant conceptualization of interactive team cognition in IRL trauma teams increases the ability to create a system where human interaction is appreciated and allowed to complement standardizations and technical solutions as the component that enables patient precision.
Strengths and limitations
The strength of this study that IRL work performance was examined to explain human factors and interactions created when trauma team members interact in authentic emergency situations. The use of the grounded theory to explore details about human interaction is optimal for conceptualization of social processes. The environment shapes attitudes and knowledge of its habitants. The study addresses a knowledge gap that lies between a retrospective analysis of trauma care and experimental study of human interaction in simulation teams.
A limitation of this study pertains to the use of single-center material and a limited number of teams. However, the resulting theory is based on many interactions. Specific hospital and cultural settings may form distinct behaviors that could potentially widen the understanding of the phenomenon observed in the material used in this study. An even more heterogeneous material in terms of injury level and thus time pressure might also increase understanding. However, it is reasonable to assume that interactions in other settings fit the pattern of our study and share the same basic process of reaching cognitive states. Observation of interactions in the team working with a simulated case did not alter the pattern. This does not mean that team dynamics in real-life and simulated environments cannot differ. However, it reveals that this particular social process is observable also in a simulated environment. The chosen methodology and research question do not allow for a comparison of “how much” or in what way interactions in these environments differ, but future studies could address this issue.
Conclusion
Trauma teams use “split vision” in a dynamic process of trauma teamwork, which seems central for team adaptation. It is used to coordinate team focus with an emergent mental model coupled to the specific situation. At the same time, it is an ability to absorb deeper aspects of the particular team in terms of knowledge, experience, empathy, and culture, which is used to align the team with situational demands and create precision for the patient.
Availability of data and materials
Data sharing is not applicable to this article, as the empirical data are sensitive in nature and a reexamination of data would not either support or overturn the findings.
Ethical approval
Ethical approval was obtained from the Regional Ethical Review Board in Linköping, Sweden (No:
2017/32–33). Written consent from all involved participants was also obtained.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Liselott Fornander
Liselott Fornander is a consultant physician in anesthesiology and intensive care, and a phD-student within the area of team cognition and communication at Linköping university. She is currently a member of the Vrinnevi hospital trauma board, working with advancing team processes, the development and implementation of a CRM-training program and advancing simulation training.
Carina Berterö
Carina Berterö is a registered nurse and a university professor in nursing science with a broad range of experience of caring in a variety of care settings. Her research interests revolve around aspects of nursing care in hospital care, primary care and palliative home care. Additional research focuses on intensive care and family functioning.
Ida Molin
Ida Molin is an internal medicine resident, with a research interest in the emergency medicine field, communication and teamwork.
Kati Laukkanen
Kati Laukkanen is an Intern at Linköping University Hospital with a special focus on patient pedagogy. She is currently working on a project to produce material to assist in preparing paediatric patients and their parents to reduce stress and uncertainty before surgical operations. Her research interests are focused on patient pedagogy and emergency care, particularly in connection to team communication and paediatric patients.
Lena Nilsson
Lena Nilsson is a consultant anesthetist, and associate professor in anesthesiology. Her research interests revolve around aspects on patient safety in prehospital care, hospital care, primary care, and home healthcare. Additional research focuses on perioperative optimisation and postoperative care also after hospital discharge.
Karin Björnström
Karin Björnström Karlsson is a consultant anaesthetist, and PhD within the anesthesiology field with both pharmacological and pedagogical interest, and is a lecturer at the medical and nursing faculty. The interprofessional team in the operating room and their communication is of special interest.
References
- Barach, P., & Weinger, M. B. (2007). Trauma team performance. In W. Wilson, C. Grande, & D. Hoyt (Eds.), Trauma: Emergency resuscitation, perioperative anesthesia, surgical management (pp. 101–114). CRC Press.
- Burke, C. S., Stagl, K. C., Salas, E., Pierce, L., & Kendall, D. (2006). Understanding team adaptation: A conceptual analysis and model. The Journal of Applied Psychology, 91(6), 189–207. https://doi.org/10.1037/0021-9010.91.6.1189
- Burtscher, M. J., Kolbe, M., Wacker, J., & Manser, T. (2011). Interactions of team mental models and monitoring behaviors predict team performance in simulated anesthesia inductions. Journal of Experimental Psychology Applied, 17(3), 257–269. https://doi.org/10.1037/a0025148
- Calder, L., Mastoras, G., Rahimpour, M., Sohmer, B., Weitzman, B., Cwinn, A., Hobin, T., & Parush, A. (2017). Team communication patterns in emergency resuscitation: A mixed methods qualitative analysis. International Journal of Emergency Medicine, 10(1), 24. https://doi.org/10.1186/s12245-017-0149-4
- Cooke, N. J., Gorman, J. C., Myers, C. W., & Duran, J. L. (2013). Interactive team cognition. Cognitive science, 37(2), 255–285. https://doi.org/10.1111/cogs.12009
- Coolen, E., Draaisma, J., & Loeffen, J. Measuring situation awareness and team effectiveness in pediatric acute care by using the situation global assessment technique. (2019). European Journal of Pediatrics, 178(6), 837–850. PMID: 30900075; PMCID: PMC6511358. https://doi.org/10.1007/s00431-019-03358-z
- Courtenay, M., Nancarrow, S., & Dawson, D. (2013). Interprofessional teamwork in the trauma setting: A scoping review. Human Resources for Health, 11(57). https://doi.org/10.1186/1478-4491-11-57
- DeChurch, L., & Mesmer-Magnus, J. (2010). The cognitive underpinnings of effective teamwork: A meta-analysis. The Journal of Applied Psychology, 95(1), 32–53. https://doi.org/10.1037/a0017328
- Derry, S, Pea, R, Barron, B, Engle, R, Erickson, F, Goldman, R, … Sherin, B. (2010). Conducting video research in the learning sciences: guidance on selection, analysis, technology, and ethics. Journal of the Learning Sciences, 19(1), 3–53. https://doi.org/10.1080/10508400903452884
- Fathi Najafi, T., Latifnejad Roudsari, R., Ebrahimipour, H., & Bahri, N. (2016). Observation in grounded theory and ethnography: What are the differences? Iranian Red Crescent Medical Journal, 18(11). https://doi.org/10.5812/ircmj.40786
- Fernandez, R., Shah, S., Rosenman, E. D., Kozlowski, S. W. J., Parker, S. H., & Grand, J. A. (2017). Developing team cognition: A role for simulation. Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare, 12(2), 96–103. PMID: 28704287; PMCID: PMC5510246. https://doi.org/10.1097/SIH.0000000000000200
- Glaser, B. G. (1965). The constant comparative method of qualitative analysis. Social problems, 12(4), 436–445. https://doi.org/10.2307/798843
- Glaser, B. G. (1978). Theoretical Sensitivity: Advances in the Methodology of Grounded Theory (3rd ed.). Sociology Press.
- Glaser, B. G., & Holton, J. (2005). Basic social processes. Grounded Theory Review, 4(3), 1–27.
- Glaser, B. G., & Strauss, A. (1967). The Discovery of Grounded Theory: Strategies for Qualitative Research. Aldine de Gruyter.
- Hoare, K., Mills, J., & Francis, K. (2012). Dancing with data: An example of acquiring theoretical sensitivity in a grounded theory study. International Journal of Nursing Practice, 18(3), 240–245. https://doi.org/10.1111/j.1440-172X.2012.02038.x
- Huang, L., Cooke, N. J., Gutzwiller, R. S., Berman, S., Chiou, E. K., Demir, M., & Zhang, W. (2021). Chapter 13 - distributed dynamic team trust in human, artificial intelligence, and robot teaming. In Chang S., Nam, & Joseph B, Eds. Trust in Human-Robot Interaction. SBN 9780128194720(pp. 301–319). Academic Press: https://doi.org/10.1016/B978-0-12-819472-0.00013-7.
- Johnsen, B. H., Westli, H. K., Espevik, R., Wisborg, T., & Brattebø, G. (2017). High-performing trauma teams: Frequency of behavioral markers of a shared mental model displayed by team leaders and quality of medical performance. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 25(1), 109. https://doi.org/10.1186/s13049-017-0452-3
- Kolbe, M., & Boos, M. (2019). Laborious but elaborate: The benefits of really studying team dynamics. Frontiers in psychology, 10, ISSN=1664-1078. https://doi.org/10.3389/fpsyg.2019.01478
- Kozlowski, S. W. J. (2018). Enhancing the effectiveness of work groups and teams: A reflection. Perspectives on Psychological Science, 13(2), 205–212. https://doi.org/10.1177/1745691617697078
- Krug, E. G., Sharma, G. K., & Lozano, R. (2000). The global burden of injuries. J Public Health, 90, 523–526. https://doi.org/10.2105/ajph.90.4.523
- Marks, M. A., Mathieu, J. E., & Zaccaro, S. J. (2001). A temporally based framework and taxonomy of team processes. Academy of Management Review, 26(3), 356–376. https://doi.org/10.2307/259182
- Mathieu, J. E., Hollenbeck, J. R., van Knippenberg, D., & Ilgen, D. R. (2017). A century of work teams in the journal of applied psychology. The Journal of Applied Psychology, 102(3), 452–467. https://doi.org/10.1037/apl0000128
- Mesmer-Magnus, J., Niler, A. A., Plummer, G., Larson, L. E., & DeChurch, L. A. (2017). The cognitive underpinnings of effective teamwork: A continuation. Career Development International, 22(5), 507–519. https://doi.org/10.1108/CDI-08-2017-0140
- Molin, I., Fornander, L., & Berggren, P. (2021). An analysis of trauma team communication using the verbal response mode taxonomy. Surgery, 170(6), 1849–1854. https://doi.org/10.1016/j.surg.2021.05.043
- Niler, A., Mesmer-Magnus, J., Larson, L., Plummer, G., Dechurch, L., & Contractor, N. (2021). Conditioning team cognition: A meta-analysis. Organizational Psychology Review, 11(2), 204138662097211. https://doi.org/10.1177/2041386620972112.
- Patton, M. Q. (2015). Qualitative Research & Evaluation Methods (4th ed.). SAGE.
- Porter-Oʼgrady, T., Alexander, D. R., Blaylock, J., Minkara, N., & Surel, D. (2006). Constructing a team model. Nursing Administration Quarterly, 30(3), 211–220. https://doi.org/10.1097/00006216-200607000-00005
- Rosen, M. A., DiazGranados, D., Dietz, A. S., Benishek, L. E., Thompson, D., Pronovost, P. J., & Weaver, S. J. (2018). Teamwork in healthcare: Key discoveries enabling safer, high-quality care. The American Psychologist, 73(4), 433–450. https://doi.org/10.1037/amp0000298
- Salas, E., Sims, D. E., & Burke, C. S. (2005). Is there a “big five” in teamwork? Small Group Research, 36(5), 555–599. https://doi.org/10.1177/1046496405277134
- Tiel Groenestege-Kreb, D., Van Maarseveen, O., & Leenen, L. (2014). Trauma team. British Journal of Anaesthesia, 113(2), 258–265. https://doi.org/10.1093/bja/aeu236
- Urquhart, C. (2002). Regrounding grounded theory - or reinforcing old prejudices? A brief reply to bryant. Journal of Information Technology Theory and Application (JITTA), 4(3). Article 5.Available at. https://aisel.aisnet.org/jitta/vol4/iss3/5
- Van Olden, G. D., Meeuwis, J. D., Bolhuis, H. W., Boxma, H., & Goris, R. J. (2004). Advanced trauma life support study: Quality of diagnostic and therapeutic procedures. Journal of Trauma: Injury, Infection, and Critical Care, 57(2), 381–384. https://doi.org/10.1097/01.TA.0000096645.13484.E6
- Westli, H. K., Johnsen, B. H., Eid, J., Rasten, I., & Brattebø, G. (2010). Teamwork skills, shared mental models, and performance in simulated trauma teams: An independent group design. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 18(1), 47. https://doi.org/10.1186/1757-7241-18-47
- Willumsen, E., & Hallberg, L. (2003). Interprofessional collaboration with young people in residential care: Some professional perspectives. Journal of Interprofessional Care, 17(4), 389–400. https://doi.org/10.1080/13561820310001608212
- Xiao, Y., Hunter, W. A., Mackenzie, C. F., Jefferies, N. J., Horst, R. L., & Group, L. (1996). Task complexity in emergency medical care and its implications for team coordination. LOTAS group. level one trauma anesthesia simulation. Human Factors, 38, 636–645. https://doi.org/10.1518/001872096778827206