Abstract
Safety communication relates to the sharing of safety information within organizations in order to mitigate hazards and improve risk management. Although risk researchers have predominantly investigated employee safety communication behaviors (e.g. voice), a growing body of work (e.g. in healthcare, transport) indicates that public stakeholders also communicate safety information to organizations. To investigate the nature of stakeholder safety communication behaviors, and their possible contribution to organizational risk management, accounts from patients and families – recorded in a government public inquiry – about trying to report safety risks in an unsafe hospital were examined. Within the inquiry, 410 narrative accounts of patients and families engaging in safety communication behaviors (voicing concerns, writing complaints, and whistleblowing) were identified and analyzed. Typically, the aim of safety communication was to ensure hospital staff addressed safety risks that were apparent and impactful to patients and families (e.g. medication errors, clinical neglect), yet unnoticed or uncorrected by clinicians and administrators. However, the success of patient and family safety communication in ameliorating risk was variable, and problems in hospital safety culture (e.g. high workloads, downplaying safety problems) meant that information provided by patients and families was frequently not acted upon. Due to their distinct role as independent service-users, public stakeholders can potentially support organizational risk management through communicating on safety risks missed or not addressed by employees and managers. However, for this to happen, there must be capacity and openness within organizations for responding to safety communication from stakeholders.
1. Introduction
Research on safety communication investigates how organizational risk management can be supported through employees engaging in behaviors to ‘raise and openly discuss safety issues’ (Hofmann and Stetzer Citation1998, p. 646). Studies have identified the antecedents of employee safety communication (e.g. safety culture, skills and knowledge), the different behaviors used to raise safety concerns (e.g. voice, incident reporting), and the importance of these behaviors for the sharing of information on hazards and safety improvements in organizations (Beus, McCord, and Zohar Citation2016; Macrae Citation2009; Noort, Reader, and Gillespie Citation2019; Tucker and Turner Citation2015).
Although safety communication research has predominantly focused on employees, studies in domains such as transport, heavy industry, and healthcare indicate that public stakeholders (e.g. hospital patients, service-users) also engage in safety communication behaviors (e.g. raising safety concerns) (Gillespie and Reader Citation2018; Turner Citation1976). Whilst risk scholars have long investigated public perceptions of risk associated with organizations (Johnson Citation1999), less research has investigated the nature and significance of public stakeholder safety communication behaviors. The current study addresses this through analyzing patient and family accounts – recorded in a government public inquiry into unsafe healthcare – of raising concerns about the safety of treatments in a UK hospital (Francis Citation2013). Through establishing the type, content, and causes of patient and family safety communication behaviors in hospitals, the aim is to examine how stakeholder safety communication can contribute to risk management in organizations.
1.1. Safety communication
Research on safety communication arises from the observation that problems in information sharing (e.g. on hazards) are a common contributory factor in accidents (Hald, Gillespie, and Reader Citation2021; Turner and Pidgeon Citation1997). Consequently, effective and open safety communication is considered essential for employees and managers to develop a collective and dynamic awareness of organizational safety risks, to share information on how safety management can be improved (e.g. learning from error, new procedures), and ensure a shared understanding of safety roles and responsibilities (Cigularov, Chen, and Rosecrance Citation2010; Griffin, Cordery, and Soo Citation2016; Weick and Sutcliffe Citation2007). Where safety communication is not open or effective (e.g. due to employees being discouraged from voicing concerns), information on risk is less likely to be shared, which increases the likelihood of an accident due to decision-makers (e.g. supervisors, senior managers) being unaware of emerging hazards (Turner and Pidgeon Citation1997; Westrum Citation2014). Examples include the Columbia Space Shuttle disaster, where junior engineers remained silent about their concerns regarding damage on the aircraft prior to shuttle launch, or the Tenerife aircraft collision, where opportunities for a co-pilot to raise concerns to the pilot about the unsafe take-off were not taken (Edmondson Citation2018). Furthermore, problems in safety communication can also lead to opportunities for improving safety not being discussed and realized: for instance, training requirements, technical innovations, or new procedures.
Safety communication research has identified three core behaviors. First, safety voice, which relates to employees inter-personally communicating safety information (e.g. verbally, by email) to individuals or groups (e.g. teams, safety units) (Noort, Reader, and Gillespie Citation2019). Safety voice is shown to be a multi-dimensional construct, with behaviors attempting to prevent hazards, promote safety improvements, prohibit unsafe activity, and express general dissatisfaction (Bazzoli and Curcuruto Citation2020; Bienefeld and Grote Citation2014; Curcuruto et al. Citation2020). Second, incident reporting, which focuses on employees submitting reports about accidents, near-misses, or safety concerns to their organization (Macrae Citation2014a). Incident reports are distinct from safety voice due to their formality (i.e. using an institutional procedure), and data are conceptualized as essential for monitoring risk, capturing errors, and supporting organizational learning (e.g. from past incidents). Third, whistleblowing, which refers to employees raising safety concerns with an independent part of an organization or an external body (e.g. regulator). Employees engage in whistleblowing behaviors to bring external scrutiny to risks they believe are being intentionally ignored internally (Antonsen Citation2009; Miceli, Near, and Dworkin Citation2008).
The willingness and ability of employees to engage in safety communication behaviors is a function of organizational safety climate and safety culture. Safety climate broadly relates to perceptions about the prioritization of safety within an organization (e.g. management commitment to safety), and safety culture to shared norms and values on safety (e.g. incident reporting) (Bisbey et al. Citation2020; Griffin and Neal Citation2000; Westrum Citation2004). Organizational members are more likely to engage in safety communication behaviors when open communication is encouraged and normalized, psychological safety is high, institutions focus on learning rather than blame, effective systems exist for gathering safety data, managers are committed to safety, and people have good communication skills (Curcuruto and Griffin Citation2018; Griffin and Neal Citation2000; Nembhard and Edmondson Citation2006; Noort, Reader, and Gillespie Citation2019; Waring Citation2005). Leadership is also crucial for generating safety communication, with safety voice and incident reporting being more likely when leaders are transformational (e.g. creating a vision for safety management), inclusive, and concerned with following safety rules (Bazzoli et al. Citation2020; Conchie, Taylor, and Donald Citation2012; Tucker and Turner Citation2015).
Thus, safety communication research focuses on the sharing of information amongst organizational members to identify hazards and opportunities for improving safety. Traditionally, safety communication research has focused on employees behavior, however a growing body of work has recognized that members of the public (herein: ‘stakeholders’) also engage in safety communication.
1.2. Stakeholder safety communication
Within the organizational literature, members of the public are often considered ‘stakeholders’ who can affect or be affected by the objectives of an institution (Freeman Citation1984). Risk scholars have long been interested in stakeholder perceptions of risk in domains where wider society is affected by organizational safety activities, and can potentially impact the success of institutional policies (e.g. on energy) (Chilton et al. Citation2002; He et al. Citation2014). Additionally, researchers have suggested that in settings where stakeholders experience problems in managing safety (e.g. patients in healthcare, passengers on public transport), they can contribute to organizational risk management through sharing information on observations of safety risks (Reader and Gillespie Citation2021). Drawing on stakeholder theory, it is theorized that the independence (e.g. from organizational culture and hierarchies) and external positionality (e.g. as service users) of stakeholders can enable them to perceive and report on safety problems that may be unrecognized or unaddressed within organizations (e.g. unsafe practices that have been normalized, poor coordination between units). By engaging in safety communication behaviors, stakeholders can contribute to organizational risk management though reporting such issues. However, due to their lack of official role within organizations, absence of safety expertise, reliance on service-providers (e.g. in healthcare), and minimal influence for enacting change, the pathways through which stakeholders communicate to organizations on safety is unclear (e.g. compared to employees), and the validity and influence of information largely untested.
Nonetheless, studies have indicated that stakeholder communication about safety concerns may be valuable for organizational risk management. For example, in Turner’s (Citation1976) seminal analysis of the etiology of organization disasters, he noted that a recurring feature of accidents (e.g. the Aberfan colliery disaster, or the Hixon rail accident) was the dismissal (e.g. by management) of communication from the public on concerns about the safety of operations in the organizations involved. More recently, accidents such as the Grenfell Tower fire in London (which led to over 70 deaths) have shown how public communication about concerns over building safety (flammable cladding and a lack of fire escapes) were well-founded, but tragically dismissed by organizations responsible for managing risk (MacLeod Citation2018). Additionally, in domains such as policing, it is recognized that complaints from the public are a valuable source of data for detecting unsafe conduct by officers (Dugan and Breda Citation1991).
Most notably, a substantial body of research in healthcare reports patients and families to often engage in safety communication behaviors whilst in hospital (Lawton et al. Citation2017). Patient safety research addresses the concern that approximately 10% of hospital patients experience an adverse event (e.g. medication error), and whilst most studies explore how the behaviors of clinical staff contribute to safe treatments, they also show patients and families to have a role in improving safety (Levtzion-Korach et al. Citation2010; O’Hara et al. Citation2018; Vincent Citation2011). Investigations find that patients and families often voice concerns during care (e.g. identifying medication errors), regularly write complaints to report safety incidents, and in-extremis, whistleblow on unsafe hospitals (Armitage et al. Citation2018; Entwistle et al. Citation2010; Francis Citation2013; Gillespie and Reader Citation2018). Whilst this work in healthcare has not been conceptualized using the safety communication literature, it is significant because it can provide insight on the nature and contribution of stakeholder safety communication behaviors to risk management in organizations.
1.3. Current study
An investigation of patient and family safety communication behaviors was undertaken in order to examine the nature and potential contribution of stakeholder safety communication to risk management in organizations. The study analyzed accounts of patient and family safety communication reported in a public inquiry into unsafe care at the Mid-Staffordshire Hospital Trust in England, where safety failures are estimated to have contributed to between 400 and 1,200 avoidable patient deaths over three years (2005–2008).
A government inquiry in 2009 investigating the causes of unsafe care at Mid-Staffordshire collected statements from hundreds of patients and staff about their attempts to report observations of safety risks at the hospital. The inquiry found failures in hospital risk management (e.g. error reporting, learning from incidents) to underlie unsafe care, and a key conclusion from the inquiry was that ‘the truth (of unsafe care) was uncovered… mainly because of the persistent complaints made by a very determined group of patients and those close to them’ (Francis Citation2013, p. 65; Macrae Citation2014b). Given the gravity of the inquiry, its detailed and verbatim reporting of patients and families engaging in safety communication, the validation of the content being communicated, and the contextualization of patient and family safety communication behaviors, the report represents a valuable data source on stakeholder safety communication. Furthermore, through reporting on stakeholder communication behaviors in different institutional contexts (e.g. whilst receiving care, after an accident), and capturing organizational responses to these, the inquiry can provide insight on the types of communication behavior used by stakeholders, and the factors which prompt them and determine outcomes. The study had two research objectives.
Research objective 1 (RO1) aimed to describe the nature, content, and factors leading to patient and family safety communication behaviors recorded in the Mid-Staffordshire public inquiry (‘inquiry’). A content analysis was first undertaken, with reports of patients and families communicating concerns about safety being systematically identified and codified in terms of the main forms of safety communication behavior described in the literature (voice, safety reporting, whistleblowing), and the types of risks reported to hospital staff (i.e. perceived or experienced threats to patient safety). A thematic analysis then identified the factors that prompted patients and families to engage in safety communication behaviors.
Research objective 2 (RO2) aimed to identify and explain organizational responses to patient and family safety communication reported within the inquiry. Consistent with the broader literature on communication in organizations (Macnamara Citation2018), patient and family safety communication behaviors can only contribute to hospital risk management if they are acknowledged and actioned by staff and managers. Utilizing a content analysis, the responses of hospital employees and managers to patient and family reporting safety risks (accepting, ignoring, denying, inaction) were systematically identified and codified in terms of response strategies identified within the communication literature (Gillespie Citation2020; Morrison Citation2014; Noort, Reader, and Gillespie Citation2021). A thematic analysis then focused on the commonly identified factors determining staff and managerial responses to safety communication.
Based on RO1 and RO2, a process model outlining the triggers, steps, and outcomes of patient and family safety communication was developed. The study aimed to contribute to the literature through (i) analyzing how and why public stakeholders communicate observations of safety risks to organizations, (ii) describing and explaining institutional responses to stakeholder safety communication, and (iii) conceptualizing the potential contribution of stakeholders to organizational risk management.
2. Method
2.1. Data
This study analyzed the UK government’s public inquiry into the Mid Staffordshire NHS Foundation Trust (from herein: ‘the Trust’), which was an organization responsible for managing two hospitals: Stafford (350 in-patient beds) and Cannock Chase (115 in-patient beds). The Trust, which was dissolved in 2014, served approximately 300,000 people in England, with around 17,000 admissions annually, and 3,000 staff.
The inquiry focused primarily on Stafford Hospital, and was published over five volumes (Francis Citation2010, Citation2013). Safety problems became evident at the Trust in 2009 due to patient complaints about unsafe care, pressure from whistleblowers, and high mortality rates. A public inquiry was undertaken in 2009 to investigate claims of unsafe care, account for them, and ensure organizational learning. The inquiry, commissioned by the UK government, cost over £20 million and was undertaken by a team of lawyers led by Sir Robert Francis QC (a barrister in medical law). Witness statements were invited from those (e.g. patients, staff) who experienced or delivered care at the hospital from 2005.
In total, 966 patients and relatives provided information to the inquiry (65 orally), with 72% reporting negative experiences. The inquiry also heard from 82 current and former members of staff (33% nurses, 27% doctors). Over five volumes, the inquiry synthesized these submissions and reported verbatim or summarized accounts of witness experiences in order to generate an explanatory account of events. Severe and frequent lapses in managing patient care were identified, including avoidable medical errors, not reporting injuries, not correcting errors, leaving patients in unhygienic conditions, not responding to emergencies, and ignoring safety data. Variable levels of patient harm, ranging from emotional distress to death, were caused by lapses. The inquiry concluded that key factors leading to the unsafe care were the acceptance of low safety standards, poor training, staff burnout, not reporting or learning from clinical accidents, penalizing mistakes, and managerial underplaying of risk data (e.g. dismissing safety concerns). The inquiry generated over 290 recommendations for improving patient safety in the NHS, and had a profound effect on UK health policy.
2.2. Analysis
The public inquiry documents were uploaded into Nvivo 12. Two distinct analyses were undertaken, and these used content analysis (to codify instances of safety communication) and thematic analysis (to identify and interpret recurring types of safety communication events) (Attride-Stirling Citation2001; Corbin and Strauss Citation2014).
2.2.1. The nature, content, and factors underlying patient and family safety communication behaviors (RO1)
Narrative accounts of safety communication behaviors were first identified. The author systemically read the inquiry and identified excerpts of text containing accounts (either verbatim or summarized by the inquiry) of patients and families communicating to the hospital (e.g. to staff, managers) about perceived risks to patient safety during treatment or after care had occurred. A trained MSc-level research assistant then evaluated these excerpts to confirm that they were accounts of safety communication. The research assistant also systematically read the inquiry to identify any overlooked reports. A content analysis was undertaken (Corbin and Strauss Citation2014), and reports the codes used. First, the behaviors used by patients and families to communicate safety risks were coded using an adapted taxonomy of the key safety communication behaviors (safety voice, incident reporting, whistleblowing) (Macrae Citation2009; Mannion and Davies Citation2015; Noort, Reader, and Gillespie Citation2019). Second, the content of patient and family safety communication was coded according to the widely used UK NHS National and Reporting Learning System’s (NRLS) safety event taxonomy (Donaldson, Panesar, and Darzi Citation2014; Howell et al. Citation2015). The aim was to establish the types of safety risks perceived and reported by patients and families (which could be multiple).
Table 1. Coding categories used to analyze patient and family safety communication.
In terms of procedure, a corroboration approach was used to optimize the accuracy of coding (Crabtree and Miller Citation1999). This involves a two-step process of coding, whereby a framework is applied to textual data by one coder, and then checked for accuracy by a second coder. Initially, the two coders independently codified a subset of textual excerpts from the public inquiry (approximately 50), and then calibrated their understanding of the coding framework in (e.g. by reviewing the coding categories, comparing sections of coding, discussing borderline cases). The first coder then applied the coding framework to the remaining textual excerpts, and the second coder (an expert in the field) reviewed each coded segment to ensure accuracy. Divergences in coding were discussed, and considered against the context of notes, to finalize how textual excerpts were codified. Descriptive data on the prevalence and types of safety communication behaviors and reported risks were generated. Finally, voice behaviors were examined to determine whether patients and families reported engaging in the four types of voice identified in the literature: preventing direct hazards, promoting safety improvements, prohibiting unsafe behavior, or generally expressing dissatisfaction with safety (Bazzoli and Curcuruto Citation2020).
An interpretative thematic analysis was then undertaken to identify the reasons for patient and family safety communication. Following procedures for thematic analysis (Braun and Clarke Citation2006), and previous case study research (Eisenhardt Citation1989), recurring themes about factors that led to patients and families raising safety concerns were identified. The analysis was undertaken by a single researcher, with it being grounded in the textual excerpts identified through the content analysis, and the broader context within which text was framed (Nowell et al. Citation2017). Concretely, this involved systematically reading and re-reading textual excerpts coded through the content analysis to identify recurring patterns of communication behavior within the data. Cross-cutting themes (e.g. safety problems not being recognized by staff) that could describe and help interpret the excerpts were identified and interpreted using key theories and topics within the broader patient safety and safety communication literature (e.g. safety culture, risk perception, error management, HRO theory). Lightly edited excerpts (for comprehension) were extracted to illustrate the analysis.
2.2.2. Organizational responses to patient and family safety communication (RO2)
Instances of safety communication identified in the inquiry (see 2.2.1) were analyzed by the author to identify accounts of how hospital staff responded to patients and families. Following the procedure for content analysis outlined in 2.2.1, textual excerpts were codified in terms of strategies (accepting, ignoring, denying, inaction) identified within the organizational communication literature for responding to voice and whistleblowing behaviors (see ) (Gillespie Citation2020; Morrison Citation2014; Noort, Reader, and Gillespie Citation2021).
Emulating the qualitative analysis described for RO1, a thematic analysis was undertaken to analyze the factors shaping hospital responses to patient and family safety communication behaviors. Excerpts within the inquiry describing factors shaping responses of staff and managers to patient safety communication were identified, and then interpreted using the safety literature (see 2.2.1). Lightly edited excerpts (for comprehension) were extracted to illustrate the analysis. A process model outlining the triggers, steps, and outcomes of patient and family safety communication was then developed.
3. Results
3.1. The nature, content, and factors underlying patient and family safety communication behaviors (RO1)
In total, 410 excerpts describing verbatim or summarized accounts of patient and family safety communication were identified.
3.1.1. Patient and family safety communication behaviors
The majority of excerpts (n = 292, 71%) referred to safety voice behaviors, with patients and families attempting to raise concerns about safety risks directly to hospital staff (e.g. nurses, doctors, administrators). See for examples. These were consistent with ‘safety voice’, with speaking up on emerging (e.g. wrong drugs, heart attacks), ongoing (e.g. diagnostic problems, neglect), or prospective (e.g. care planning) safety problems.
Table 2. Illustrative examples of patient and family safety voice.
A further 27% (n = 111) of safety communication events related to submitting formal complaints, and these were somewhat analogous to incident reports. Complaints attempted to report safety problems experienced during care, and to obtain an explanation and reassurance that future patients would not experience similar risks (see ). Complaints were often written to escalate problems that voice behaviors had not been successful in resolving safety risks: for instance, addressing concerns of misdiagnosis of cancer. Additionally, 2% (n = 7) of safety communication events related to whistleblowing, where concerns were raised with external parties, such as the media, an advocacy service, or a Member of Parliament (MP). Finally, all four types safety voice behavior outlined in the literature were identified (Bazzoli and Curcuruto Citation2020). Safety communication focused on preventing direct hazards (e.g. wrong medications), promoting safety improvements (e.g. communication between patients and staff), prohibiting unsafe behavior (e.g. challenging hygiene failures), and expressing general dissatisfaction (e.g. on staff attitudes).
Table 3. Illustrative examples of patient and family complaints.
3.1.2. Content of patient and family safety communication
The analysis found patients and families to report on 581 observations of safety risks (see for a summary and examples). Two thirds of observations referred to four safety risks (out of a possible 15). These were: patient neglect (e.g. nutrition tubes left unchecked; patients left in unhygienic conditions); availability of staff and services (e.g. waiting days for a diagnosis of heart failure); communication and consent (e.g. staff not taking consent for operations); and clinical assessments (e.g. misdiagnosing a brain tumor). These were notable due to staff often being unaware of them (mis-communication), and for focusing on problems that staff were aware of but had not resolved (e.g. not cleaning wounds, medication errors).
Table 4. Safety risks featured in patient and family safety communication.
3.1.3. Factors underlying patient and family safety communication
The thematic analysis found patients and families to engage in safety voice when they perceived risks to safety during treatment provision that were not recognized, or taken seriously, by hospital staff. Often, the poor safety culture at the Trust (e.g. normalization of unsafe care; absence of staff capabilities to address errors; poor safety monitoring) spilled over to impact patients by manifesting in visible and harmful safety lapses, which precipitated safety communication to spur staff into action.
Illustrative excerpt 1, a family recalling trying to raise concerns about their father’s care: ‘I kept asking them and asking them about the swelling and I never got any answers. I think that in the end, that the water actually hit his lungs and then his heart, and that killed him.’
Illustrative excerpt 2, a relative discussing trying to get help for her father: ‘Again, my father’s drip had run out. I went down and asked them to replace it. We will come in a minute, we will come in a minute… I think I went down four times for that.
Illustrative excerpt 3, the inquiry on families reporting failing equipment: ‘[The family] raised concerns about equipment not working, particularly the heart rate monitor, and… recall that the nurse stated that the machine “never functions properly”.’
Patients and families not only observed risks to patient safety: they also picked up on more systemic problems in risk management (e.g. hygiene control, not responding to alarms), and voiced their concerns.
Illustrative excerpt 4, a wife recalling trying to improve infection control standards: ‘I brought in … soap, to wash him with and [the ward sister]… she came and told me off for bringing it and she said:… why are you bringing in soap and a towel; we don’t need that, we have got alcohol gel. And I said: because C. difficile doesn’t respond to alcohol gel.’
Illustrative excerpt 5, a family member trying to ensure staff respond to patient alarms: ‘My brother just said: excuse me, what happens when a patient rings a bell? They said that bell – that light up there lights up. He said: you mean that one that must have been lit for at least 20 minutes? They said, oh.’
Thus, safety voice behaviors were attempts to get staff to correct safety problems that patients and families thought had been missed or ignored. Written complaints, alternatively, were submitted to ensure that failures to manage safety risks were learnt from by hospitals. These were often not captured by staff incident monitoring systems, meaning that patients and families were trying to report supplementary information on safety problems in healthcare delivery.
Illustrative excerpt 6, a daughter trying to address concerns about her mother’s death: ‘The post mortem revealed that the patient had suffered peritonitis from a punctured bowel. Her daughter believes that her mother ‘was not treated properly because she was elderly’ and…complained to the hospital…’
Illustrative excerpt 7, the inquiry on a complaint about an investigation: ‘The hospital conceded that the incident forms were inaccurate, sought to explain the errors and provided further copies of the incident forms. Still dissatisfied, Mrs Y’s son raised the issue a further time with the hospital which ultimately conceded that the three incident forms contained misleading and inaccurate information.’
As a last resort, and where patients and families felt they were not listened to, they whistleblew to external parties: for instance, to their local MP, the media, or the healthcare regulator. The aim was to publicly reveal unsafe care, and circumvent unresponsive hospital management.
Illustrative excerpt 8, the inquiry on patient and family whistleblowing: ‘There was an increasing public outcry led by a group of patients and patients’ relatives who had had experiences of poor care at the hands of the Trust… The group mounted a campaign for a public inquiry into the failings…’
3.2. Organizational responses to patient and family safety communication (RO2)
In total, the analysis identified descriptions of 409 responses by hospital staff or managers to patient and family safety communication. Examples are included in .
Table 5. Examples of staff responses to patient and family safety communication.
3.2.1. Organizational response strategies to patient and family safety communication
The most common employee managerial response to patient and family safety communication was inaction (58.4%). For safety voice, inaction often meant acknowledging a concern, but not correcting it (e.g. acknowledging a blood transfusion error, but not resolving it); for complaints, inaction involved accepting patient safety failures, but making no concrete plans to address them. Denial (19.3%) of safety voice typically involved refutation of a clear safety risk or request for help (e.g. where a CT for a head injury was denied, but later scans revealed internal bleeding); for complaints, it involved disputing patient accounts. Ignoring (9.3%) safety voice involved staff disregarding concerns or requests; for complaints, letters (e.g. about poor nursing care) were not responded to. Only 13% of the responses involved accepting a safety risk raised by patients and families (e.g. bringing in extra staff). Whistleblowing involved communication with external parties, and therefore institutional responses were not coded.
In conclusion, the majority of safety communication behaviors identified were not responded to. This is unsurprising given the nature of the inquiry: yet, also reveals how potential opportunities generated by patients and families for mitigating risk were missed.
3.2.2. Factors underlying organizational responses to patient and family safety communication
The safety culture problems at the trust which underlay failures to provide safe care (e.g. normalization of poor safety standards, low safety motivation) also led to voice acts being frequently ignored or not addressed.
Illustrative excerpt 9, the inquiry on a nurse dismissing an observation of a treatment error: ‘His daughter was concerned that…he was receiving nutrition in error. She requested to see a doctor, however she was told by a senior nurse that it was not necessary… A junior nurse observed the patient and immediately noted that… he should not have been receiving the nutrition. A doctor was eventually called, but his daughter believes it was already too late.’
Illustrative excerpt 10, the inquiry on a doctor not taking a wife’s concerns about her husband seriously: ‘He returned to the hospital where the consultant made light of his face which was contorted with pain and of his enlarged stomach saying ‘Is he having twins?’…. The following day the patient again returned to the hospital and was diagnosed with a twisted bowel.’
Hospital staff reported how problems in safety culture, for instance high workloads and acceptance of poor safety standards, prevented them from responding appropriately to safety communication by patients. Also, when they did try to engage with the concerns raised, their efforts were often stymied by organizational processes and management.
Illustrative excerpt 11, a doctor describing failures in safety management: ‘I was more than surprised at the level of care that we regarded as being acceptable.… The way in which we structured our care and in particular the battle-fatigued attitude of the staff did not lead to – it wasn’t conducive for good quality care. It was a case of getting through the day rather than how good can we be today.’
Illustrative excerpt 12, a senior nurse on raising safety concerns: ‘Patient care was not up to acceptable standards… I filled out incident forms quite liberally to try to bring to someone’s attention what was actually happening, to highlight poor care issues. We got the impression that nothing was changing.’
Furthermore, the problems in safety culture that inhibited effective responses to patient and family safety voice also prevented effective learning from complaints. Complaints were often not investigated properly, data trends were not analyzed, and opportunities for learning missed.
Illustrative excerpt 13, the inquiry on a poor investigation into a complaint: ‘[The] daughter was informed that her father would improve… Two days later the patient died. His daughter complained to the hospital; however the response simply stated that the hospital was improving its standards.’
Illustrative excerpt 14, the inquiry on an ineffective complaint investigation: ‘A complaint was made to PALS, who after investigation were still unable to say how the injury had happened and lost the formal complaint and incident report.’
Illustrative excerpt 15, the inquiry on how trends and observations in complaints were not recognized or learnt from: ‘The Trust had a high rate of complaints compared to other Trusts…. Managers did not appear to be aware of these signs of systemic problems. The investigation and the handling of complaints was poor and when action plans were produced, action often did not follow.’
Yet, when patients and families were successful in catalyzing staff or management to engage with their concerns, this could avert harm or lead to improvements.
Illustrative excerpt 16, a successful safety voice act: ‘[The patient collapsed and her daughter] ran to the ward and called out for help. A doctor appeared and Patient A was helped with her breathing.’
Illustrative excerpt 17, the inquiry on learning from a complaint about patient fall: ‘[an action plan was developed] saying that all staff in the EAU would be instructed to maintain effective communication after a patient had fallen’
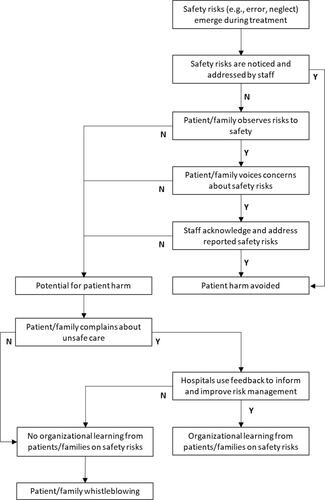
3.3 A Process model for patient and family safety communication behaviors
models the triggers, steps, and outcomes of patient and family safety communication. This conceptualizes patients and families to engage in safety voice when they perceive risks to patient safety that they believe hospital staff are unaware of or not correcting. Where risks go unaddressed, or unexpected harm occurs, patients and families write complaints in order to trigger an investigation and organizational learning. Where safety communication is acknowledged, and due to patients and families raising unrecognized or unsolved safety risks, hospitals can potentially avert harm and ensure organizational learning on safety. Conversely, not responding to patient and family safety communication behaviors potentially leads to safety risks not being addressed for current and future patients.
4. Discussion
The analysis of the Mid Staffordshire public inquiry found patients and families to engage in safety communication behaviors when they perceived risks to healthcare safety that they believed were not recognized by hospital staff and managers. The safety communication behaviors used – safety voice, complaints, and whistleblowing – were broadly aligned with those used by organizational employees (Curcuruto et al. Citation2020; Macrae Citation2009; Mannion and Davies Citation2015). Through highlighting unnoticed or unsolved safety risks, patients and families created opportunities for improving risk management within the Trust: however, a lack of listening by staff and management resulted in chances for organizational learning not being taken.
4.1. Theoretical and practical implications
The study demonstrates how safety communication behaviors from public stakeholders can support safety management in organizations. Patients and families were found to engage in similar forms of safety communication behaviors to employees (voice, reporting, whistleblowing), with these also appearing multi-dimensional in nature (Bazzoli and Curcuruto Citation2020; Macrae Citation2014b; Noort, Reader, and Gillespie Citation2019). In-line with concepts such as high reliability organization (HRO) theory (Martínez-Córcoles and Vogus Citation2020; Weick and Sutcliffe Citation2007), and through their independence and different vantage point to employees, stakeholders can ensure that organizational members are aware of risks and opportunities for improving safety management that would otherwise be missed. However, the potential learning that can arise from stakeholder safety communication behavior largely rests on the openness of staff and managers for listening to the concerns and insights of those who are external, potentially inexpert, and sometimes easy to dismiss.
In terms of enabling and utilizing stakeholder safety communication for supporting safety management, questions emerge. Employee safety communication is known to be influenced by leadership and safety climate, and it should be established to what extent stakeholder safety communication is also a function of these factors. For example, in healthcare, patients are more likely to communicate safety concerns when they perceive clinicians and managers to solicit and welcome their contribution (Entwistle et al. Citation2010; Schiffinger, Latzke, and Steyrer Citation2016; Schwappach Citation2010), and this is potentially a distinct dimension of safety climate that requires examination (i.e. openness to stakeholder communication on safety). Given the established role of organizational leadership in determining safety climate and employee safety communication, its indirect influence (e.g. through safety climate) upon stakeholder safety communication behavior also merits investigation. For instance, similar to employees (Conchie, Taylor, and Donald Citation2012), are patients and families more likely to engage in safety communication behaviors in organizations where leaders are considered transformational (e.g. with this shaping staff and stakeholder attitudes)? A further question relates to the degree to which safety communication behaviors are a product of stakeholder values towards safety, their communication skills, and willingness to step beyond the role of service user (e.g. moving from the role of a patient receiving care to that of someone trying to improve safety management in a hospital). Interpersonal dynamics, and the framing of a service-user’s role (e.g. as an extension of the team delivering a service) might also shaping willingness to communicate, and the type of behavior engaged in (e.g. voice to an organizational member, or a complaint to an institutional department).
Somewhat paradoxically, and distinct to employees, stakeholder safety communication behavior may be most likely to occur and be valuable in organizations when there is a poor safety climate and culture. This is because problems in safety (especially severe ones) will likely only become apparent to stakeholders when there is a poor safety culture for identifying and addressing safety issues (i.e. leading to problems not being fixed, and thus spilling over to affect stakeholders). Building on concepts such as double-loop learning (Argyris Citation1976), this indicates that the significance of stakeholders raising concerns about safety in an organization may go beyond the specific issues being raised. Rather, stakeholder safety communication, in aggregate, may reveal deeper problems in safety management within an organization (i.e. in terms of institutional capabilities for recognizing and capturing safety problems), with this being underscored when staff and managers do not listen to stakeholder concerns. To examine this, future research might consider overlaps and disjunctions between relationship between external stakeholder safety communication on safety and internal organizational safety data.
In terms of developing pathways through which organizations (e.g. senior managers) and regulators can solicit and analyze stakeholder safety communication, various guiding principles emerge. Most obviously, stakeholder safety communication, which might appear to be disruptive, negative, and sometimes easy to ignore or fudge (e.g. complaints), must be welcomed and recognized as valuable within organizations. Second, explicit processes for stakeholders to communicate safety concerns should be instituted, with these being evaluated in an independent, transparent, and systematic manner in order to ensure that the issues raised are listened to. Third, following the double-loop learning perspective (Argyris Citation1976), stakeholder safety communication might be considered a form of data source for evaluating safety culture, whereby instances of communication, and responses to them, are documented and analyzed. As recognized within the inquiry, the unsafe care at Mid-Staffordshire was not revealed by a single voice act or complaint, but, rather, a cumulation of observations and reports on safety management failures within the Trust.
More broadly, the idea of stakeholders engaging in safety communication behaviors to support organizational risk management requires consideration. Ethically, questions arise about the appropriateness of engaging service users who will often only interact with organizations in a transient and informal fashion, and lack expertise or training on safety. Accountability for safety management clearly lies upon organizational employees and managers, and using stakeholder safety communication to identify safety problems and potential improvements could risk shifting responsibility for safety away from organizations, and place an unreasonable burden upon public stakeholders.
4.2. Limitations
The analyzed public inquiry was highly specific to healthcare, and produced in a political context (to understand an institutional failure). Whilst data was collected from over 1,000 witnesses, participants were self-selected, and accounts of safety communication cannot be verified. The analysis was focussed on patient and family perspectives on unsafe care, and staff accounts of whether and how they responded to specific instances of patient voice were mostly not collected or available. Nonetheless, the safety problems in the Trust are incontrovertible, and patient and family accounts of safety communication were highly consistent and made independently. The source submissions of patients and families were not accessible, and the analysis relied on a mixture of summary and verbatim patient accounts. No insight was available on the group or individual factors that shaped safety communication behavior. Qualitative coding used content analysis, which constrains the range of codes that can be used to analyze data, and thematic analysis, which is interpretative and subjective.
The extent to which the findings can be generalized to other healthcare settings or non-healthcare domains is unclear, and future research might examine stakeholder safety communication in other settings (e.g. building safety, security, transport), and attempt to determine the prevalence of stakeholder safety communication in organizations (e.g. hospitals). Also, the current analysis focused on stakeholder safety communication in an organization with a poor safety culture, and little is known about stakeholder safety communication in institutions that manage risk effectively (e.g. in aviation). To investigate stakeholder safety communication, new methodologies are required: for example using interviews or survey-style measurements, or alternatively, others forms of naturally occurring data (e.g. online forums).
4.3. Conclusions
The analysis of safety failures at Mid-Staffordshire shows that when stakeholders observe risks that impact upon their safety, they engage in safety communication behaviors (voicing concerns, complaining, whistleblowing) to bring their concerns to the attention of staff and managers. Due to their alternative positionality (e.g. as independent service-users), stakeholders can potentially support risk management through reporting on safety issues missed or not addressed in organizations, and these behaviors may be especially valuable where cultural factors inihibit employee safety communication. However, stakeholder communication on safety can only improve organizational risk management if there is capacity and openness within organizations and regulators for responding to concerns.
Acknowledgement
The author would like to express gratitude to Jess Joseph for study support.
Disclosure statement
There are no current or potential conflicts of interest (i.e. financial interests) arising from this work.
References
- Antonsen, S. 2009. “Safety Culture and the Issue of Power.” Safety Science 47 (2): 183–191. doi:https://doi.org/10.1016/j.ssci.2008.02.004.
- Argyris, C. 1976. “Single-Loop and Double-Loop Models in Research on Decision Making.” Administrative Science Quarterly 21 (3): 363–375. doi:https://doi.org/10.2307/2391848.
- Armitage, G., S. Moore, C. Reynolds, P.-A. Laloë, C. Coulson, R. McEachan, R. Lawton, I. Watt, J. Wright, and J. O’Hara. 2018. “Patient-Reported Safety Incidents as a New Source of Patient Safety Data: An Exploratory Comparative Study in an Acute Hospital in England.” Journal of Health Services Research & Policy 23 (1): 36–43. doi:https://doi.org/10.1177/1355819617727563.
- Attride-Stirling, J. 2001. “Thematic Networks: An Analytic Tool for Qualitative Research.” Qualitative Research 1 (3): 385–405. doi:https://doi.org/10.1177/146879410100100307.
- Bazzoli, A, and M. Curcuruto. 2020. “Safety Leadership and Safety Voices: Exploring the Mediation Role of Proactive Motivations.” Journal of Risk Research 24: 1–20.
- Bazzoli, A., M. Curcuruto, J. I. Morgan, M. Brondino, and M. Pasini. 2020. “Speaking up about Workplace Safety: An Experimental Study on Safety Leadership.” Sustainability 12 (18): 7458. doi:https://doi.org/10.3390/su12187458.
- Beus, J. M., M. A. McCord, and D. Zohar. 2016. “Workplace Safety: A Review and Research Synthesis.” Organizational Psychology Review 6 (4): 352–381. doi:https://doi.org/10.1177/2041386615626243.
- Bienefeld, N, and G. Grote. 2014. “Speaking up in Ad Hoc Multiteam Systems: Individual-Level Effects of Psychological Safety, Status, and Leadership within and across Teams.” European Journal of Work and Organizational Psychology 23 (6): 930–945. doi:https://doi.org/10.1080/1359432X.2013.808398.
- Bisbey, T. M., M. P. Kilcullen, E. J. Thomas, M. J. Ottosen, K. Tsao, and E. Salas. 2020. “Safety Culture: An Integration of Existing Models and a Framework for Understanding Its Development.” Human Factors 63: 88–110.
- Braun, V, and V. Clarke. 2006. “Using
- Chilton, S., J. Covey, L. Hopkins, M. Jones-Lee, G. Loomes, N. Pidgeon, and A. Spencer. 2002. “Public Perceptions of Risk and Preference-Based Values of Safety.” Journal of Risk and Uncertainty 25 (3): 211–232. doi:https://doi.org/10.1023/A:1020962104810.
- Cigularov, K. P., P. Y. Chen, and J. Rosecrance. 2010. “The Effects of Error Management Climate and Safety Communication on Safety: A Multi-Level Study.” Accident; Analysis and Prevention 42 (5): 1498–1506. doi:https://doi.org/10.1016/j.aap.2010.01.003.
- Conchie, S. M., P. J. Taylor, and I. J. Donald. 2012. “Promoting Safety Voice with Safety-Specific Transformational Leadership: The Mediating Role of Two Dimensions of Trust.” Journal of Occupational Health Psychology 17 (1): 105–115.
- Corbin, J, and A. Strauss. 2014. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA: Sage publications.
- Crabtree, B, and W. Miller. 1999. Doing Qualitative Research. Thousand Oaks, CA: Sage Publications.
- Curcuruto, M, and M. A. Griffin. 2018. “Prosocial and Proactive “Safety Citizenship Behaviour” (SCB): The Mediating Role of Affective Commitment and Psychological Ownership.” Safety Science 104: 29–38. doi:https://doi.org/10.1016/j.ssci.2017.12.010.
- Curcuruto, M., K. Strauss, C. Axtell, and M. A. Griffin. 2020. “Voicing for Safety in the Workplace: A Proactive Goal-Regulation Perspective.” Safety Science 131: 104902. doi:https://doi.org/10.1016/j.ssci.2020.104902.
- Donaldson, L. J., S. S. Panesar, and A. Darzi. 2014. “Patient-safety-related hospital deaths in England: Thematic analysis of incidents reported to a national database, 2010–2012.” PLoS Medicine 11 (6): e1001667. doi:https://doi.org/10.1371/journal.pmed.1001667.
- Dugan, J. R., and D. R. Breda. 1991. “Complaints about Police Officers: A Comparison among Types and Agencies.” Journal of Criminal Justice 19 (2): 165–171. doi:https://doi.org/10.1016/0047-2352(91)90050-6.
- Edmondson, A. C. 2018. The Fearless Organization: Creating Psychological Safety in the Workplace for Learning, Innovation, and Growth. New Jersey: John Wiley & Sons.
- Eisenhardt, K. M. 1989. “Building Theories from Case Study Research.” The Academy of Management Review 14 (4): 532–550. doi:https://doi.org/10.2307/258557.
- Entwistle, V. A., D. McCaughan, I. S. Watt, Y. Birks, J. Hall, M. Peat, B. Williams, and J. Wright. 2010. “Speaking up about Safety Concerns: Multi-Setting Qualitative Study of Patients’ Views and Experiences.” Quality and Safety in Health Care 19 (6): e33–e33.
- Francis, R. 2010. Independent Inquiry into Care Provided by Mid Staffordshire NHS Foundation Trust January 2005–March 2009 (Vol. 375). London: The Stationery Office. https://www.gov.uk/government/publications/independent-inquiry-into-care-provided-by-mid-staffordshire-nhs-foundation-trust-january-2001-to-march-2009.
- Francis, R. 2013. Report of the mid-Staffordshire NHS Foundation Trust Public Inquiry. https://www.gov.uk/government/publications/report-of-the-mid-staffordshire-nhs-foundation-trust-public-inquiry
- Freeman, R. E. 1984. Strategic Management: A Stakeholder Approach. Boston: Pitman.
- Gillespie, A. 2020. “Disruption, Self-Presentation, and Defensive Tactics at the Threshold of Learning.” Review of General Psychology 24 (4): 382–396. doi:https://doi.org/10.1177/1089268020914258.
- Gillespie, A, and T. Reader. 2018. “Patient-Centered Insights: Using Healthcare Complaints to Reveal Hotspots and Blindspots in Quality and Safety.” The Milbank Quarterly 96 (3): 530–567. doi:https://doi.org/10.1111/1468-0009.12338.
- Griffin, M. A., J. Cordery, and C. Soo. 2016. “Dynamic Safety Capability: How Organizations Proactively Change Core Safety Systems.” Organizational Psychology Review 6 (3): 248–272. doi:https://doi.org/10.1177/2041386615590679.
- Griffin, M. A., and A. Neal. 2000. “Perceptions of Safety at Work: A Framework for Linking Safety Climate to Safety Performance, Knowledge, and Motivation.” Journal of Occupational Health Psychology 5 (3): 347–358.
- Hald, E. J., A. Gillespie, and T. W. Reader. 2021. “Causal and Corrective Organisational Culture: A Systematic Review of Case Studies of Institutional Failure.” Journal of Business Ethics 174: 457–483.
- He, G., A. P. Mol, L. Zhang, and Y. Lu. 2014. “Nuclear Power in China after Fukushima: Understanding Public Knowledge, Attitudes, and Trust.” Journal of Risk Research 17 (4): 435–451. doi:https://doi.org/10.1080/13669877.2012.726251.
- Hofmann, D. A., and A. Stetzer. 1998. “The Role of Safety Climate and Communication in Accident Interpretation: Implications for Learning from Negative Events.” Academy of Management Journal 41 (6): 644–657.
- Howell, A.-M., E. M. Burns, G. Bouras, L. J. Donaldson, T. Athanasiou, and A. Darzi. 2015. “Can Patient Safety Incident Reports Be Used to Compare Hospital Safety? Results from a Quantitative Analysis of the English National Reporting and Learning System Data.” Plos ONE 10 (12): e0144107. doi:https://doi.org/10.1371/journal.pone.0144107.
- Johnson, B. B. 1999. “Exploring Dimensionality in the Origins of Hazard-Related Trust.” Journal of Risk Research 2 (4): 325–354. doi:https://doi.org/10.1080/136698799376763.
- Lawton, Rebecca., Jane Kathryn. O’Hara, Laura. Sheard, Gerry. Armitage, Kim. Cocks, Hannah. Buckley, Belen. Corbacho, et al. 2017. “Can Patient Involvement Improve Patient Safety? A Cluster Randomised Control Trial of the Patient Reporting and Action for a Safe Environment (PRASE) Intervention.” BMJ Quality & Safety 26 (8): 622–631. doi:https://doi.org/10.1136/bmjqs-2016-005570.
- Levtzion-Korach, Osnat., Allan. Frankel, Hanna. Alcalai, Carol. Keohane, John. Orav, Erin. Graydon-Baker, Janet. Barnes, et al. 2010. “Integrating Incident Data from Five Reporting Systems to Assess Patient Safety: Making Sense of the Elephant.” Joint Commission Journal on Quality and Patient Safety 36 (9): 402–410.
- MacLeod, G. 2018. “The Grenfell Tower Atrocity: Exposing Urban Worlds of Inequality, Injustice, and an Impaired Democracy.” City 22 (4): 460–489. doi:https://doi.org/10.1080/13604813.2018.1507099.
- Macnamara, J. 2018. “Toward a Theory and Practice of Organizational Listening.” International Journal of Listening 32 (1): 1–23. doi:https://doi.org/10.1080/10904018.2017.1375076.
- Macrae, C. 2009. “Making Risks Visible: Identifying and Interpreting Threats to Airline Flight Safety.” Journal of Occupational and Organizational Psychology 82 (2): 273–293. doi:https://doi.org/10.1348/096317908X314045.
- Macrae, C. 2014a. Close Calls: Managing Risk and Resilience in Airline Flight Safety. London: Palgrave.
- Macrae, C. 2014b. “Early Warnings, Weak Signals and Learning from Healthcare Disasters.” BMJ Quality & Safety 23 (6): 440–445. doi:https://doi.org/10.1136/bmjqs-2013-002685.
- Mannion, R, and H. T. Davies. 2015. “Cultures of Silence and Cultures of Voice: The Role of Whistleblowing in Healthcare Organisations.” International Journal of Health Policy and Management 4 (8): 503–505.
- Martínez-Córcoles, M, and T. J. Vogus. 2020. “Mindful Organizing for Safety.” Safety Science 124: e104614–e104614. doi:https://doi.org/10.1016/j.ssci.2020.104614.
- Miceli, M. P. J. P. Near, and T. M. Dworkin. 2008. Whistle-Blowing in Organizations. New York: Lexington.
- Morrison, E. W. 2014. “Employee Voice and Silence.” Annual Review of Organizational Psychology and Organizational Behavior 1 (1): 173–197. doi:https://doi.org/10.1146/annurev-orgpsych-031413-091328.
- Nembhard, I, and A. C. Edmondson. 2006. “Making It Safe: The Effects of Leader Inclusiveness and Professional Status on Psychological Safety and Improvement Efforts in Health Care Teams.” Journal of Organizational Behavior 27 (7): 941–966. doi:https://doi.org/10.1002/job.413.
- Noort, M. C., T. W. Reader, and A. Gillespie. 2019. “Speaking up to Prevent Harm: A Systematic Review of the Safety Voice Literature.” Safety Science 117: 375–387. doi:https://doi.org/10.1016/j.ssci.2019.04.039.
- Noort, M. C., T. W. Reader, and A. Gillespie. 2021. “Safety Voice and Safety Listening during Aviation Accidents: Cockpit Voice Recordings Reveal That Speaking-up to Power is Not Enough.” Safety Science 139: 105260. doi:https://doi.org/10.1016/j.ssci.2021.105260.
- Nowell, L. S., J. M. Norris, D. E. White, and N. J. Moules. 2017. “Thematic Analysis: Striving to Meet the Trustworthiness Criteria.” International Journal of Qualitative Methods 16 (1): 160940691773384–160940691773313. doi:https://doi.org/10.1177/1609406917733847.
- O’Hara, Jane K., Caroline. Reynolds, Sally. Moore, Gerry. Armitage, Laura. Sheard, Claire. Marsh, Ian. Watt, John. Wright, and Rebecca. Lawton. 2018. “What Can Patients Tell us about the Quality and Safety of Hospital Care? Findings from a UK Multicentre Survey Study.” BMJ Quality & Safety 27 (9): 673–682.
- Reader, T. W., and A. Gillespie. 2021. “Stakeholders in Safety: Patient Reports on Unsafe Clinical Behaviors Distinguish Hospital Mortality Rates.” The Journal of Applied Psychology 106 (3): 439–451.
- Research in Psychology 3 (2): 77–101. [Database] doi:https://doi.org/10.1191/1478088706qp063oa.
- Schiffinger, M., M. Latzke, and J. Steyrer. 2016. “Two Sides of the Safety Coin?: How Patient Engagement and Safety Climate Jointly Affect Error Occurrence in Hospital Units.” Health Care Management Review 41 (4): 356–367.
- Schwappach, D. L. 2010. “Review: Engaging Patients as Vigilant Partners in Safety: A Systematic Review.” Medical Care Research and Review: MCRR 67 (2): 119–148. doi:https://doi.org/10.1177/1077558709342254.
- Tucker, S, and N. Turner. 2015. “Sometimes It Hurts When Supervisors Don’t Listen: The Antecedents and Consequences of Safety Voice among Young Workers.” Journal of Occupational Health Psychology 20 (1): 72–81.
- Turner, B. A. 1976. “The Organizational and Interorganizational Development of Disasters.” Administrative Science Quarterly 21 (3): 378–397. doi:https://doi.org/10.2307/2391850.
- Turner, B. A., and N. F. Pidgeon. 1997. Man-Made Disasters. London: Butterworth-Heinemann.
- Vincent, C. 2011. Patient Safety. London: John Wiley & Sons.
- Waring, J. J. 2005. “Beyond Blame: Cultural Barriers to Medical Incident Reporting.” Social Science & Medicine (1982) 60 (9): 1927–1935. doi:https://doi.org/10.1016/j.socscimed.2004.08.055.
- Weick, K. E., and K. M. Sutcliffe. 2007. Managing the Unexpected: Resilient Performance in an Age of Uncertainty. San Francisco, CA: Jossey-Bass.
- Westrum, R. 2004. “A Typology of Organisational Cultures.” Quality and Safety in Health Care 13 (suppl_2): ii22–ii27. doi:https://doi.org/10.1136/qshc.2003.009522.
- Westrum, R. 2014. “The Study of Information Flow: A Personal Journey.” Safety Science 67: 58–63. doi:https://doi.org/10.1016/j.ssci.2014.01.009.