 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Studies on aging and migration often note a ‘language barrier’ for older migrants when communicating in a (medical) second language (L2) context. Yet how a limited L2 proficiency impacts the aging process of migrant adults has, so far, not been systematically investigated. This question is important given that having a limited L2 proficiency may pose immediate drawbacks on one's ability to maintain independence. Through a combination of qualitative interviews and quantitative language and cognitive measures, this study investigates if and under which circumstances a ‘language barrier’ may be detrimental for the aging process of a group of older female Turkish migrants in the Netherlands. Findings suggest that a limited L2 proficiency reciprocally fuels feelings of L2 insecurity, which impacts the formation of social relationships in the L2, feelings of belonging and lower wellbeing levels. A firm embedding in an L1 network positively impacts wellbeing levels, yet results in a heavy dependence on others in L2 situations. We conclude that limited L2 skills may steer the aging process in a detrimental direction for those older migrants who lack a social support network in the L1 and cannot communicate effectively in the L2.
1. Introduction
The rapidly aging population in modern societies is becoming more and more ethnically diverse. Increased mobilisation over the last few decades has resulted in large portions of migrants – who settled in western countries for economic, political, personal or other reasons – to age in an environment that differs culturally, socially, but also linguistically from their home environment. In the Netherlands alone, it is estimated that older migrant adults will make up 21% of the aging population by 2060, compared to 11% in 2015 (van Duin and Stoeldraijer Citation2014).
The research on aging and migration in Europe to date spans studies looking into living situations of older migrants, mobility patterns, access to social services and care practices (e.g. Bolzman Citation2012, Citation2013; Forssel and Torres Citation2012; Karl and Torres Citation2015). In addition, there is a substantial body of research on the health status of older ‘first-generation’ migrants in Europe, which reports a generally worse health condition, a higher prevalence of cardiovascular diseases and mental health problems and depression for some migrant groups, in comparison to the native population (Carballo, Divino, and Zeric Citation1998; Uitewaal et al. Citation2004; Sol-Aur and Crimmins Citation2008).
Little research has been conducted on one of the most salient social aspects of aging for older migrant populations: the linguistic environment. So far, there are only a handful of studies noting language barriers in access to healthcare services (see Lai and Chau Citation2007; Asanin and Wilson Citation2008, in Canada and Dias, Severo, and Barros Citation2008,in Portugal), usually as part of larger processes relating to ethnicity (in the Netherlands, see Stronk, Ravelli, and Reijneveld Citation2001) or acculturation (degree of participation in the host culture) (Ince et al. Citation2014). Lack of proficiency in the target language may, as the few studies above indicate, mediate access to and utilisation of services. With linguistic environment being one of the main differences between native and migrant populations, it seems counterintuitive that past studies have not taken this factor into account more.
In a recent research notes article reporting on perceptions of health, wellbeing and linguistic barriers of older Turkish adults by healthcare workers with insights into their local Turkish communities (Pot, Keijzer, and de Bot Citationsubmitted), it was suggested that language is a mediating factor for migrant older adults in gaining access to healthcare services, but also to maintain a degree of wellbeing (also see Priebe et al. Citation2011). Limited L2 proficiency postulates a circle of dependencies that limits interactional opportunities, the construction of social networks and limited abilities to express and communicate healthcare needs, akin to the more robust body of health sciences research that has found health determiners to interact (see below). Language thus plays an intricate role in the aging process, yet because of these interactions with social, cognitive and physical factors it is a methodologically difficult factor to extract from other social aging processes.
This paper builds on the scantly available evidence about the mediating role of language in the aging process of older migrants and specifically elaborates on the earlier research notes article, by expanding the investigation into the linguistic component in the older Turkish migrants' aging trajectories. The central question that guides this investigation is under which circumstances this previously reported language barrier does steer the aging process of older migrants in a detrimental direction and perhaps increases vulnerability. More specifically, we consider how the L2 environment and L2 competence impact wellbeing levels for a specific group of older migrants in the Netherlands: female Turkish migrants.
2. Background
2.1. Migrant aging
Research in the interdisciplinary field of aging (social gerontology) and migration (migration studies) typically distinguishes two ‘core’ groups of migrants: retirement migrants (i.e. older adults settling into another environment post retirement, typically Europe's older population labelled ‘baby boomers’, similar to ‘snow birds’ in the USA) and labour migrants who settled in the destination countries as (young) adults (Warnes et al. Citation2004; Warnes and Williams Citation2006). The first group includes some of the more affluent older adults, whereas the latter group is very heterogeneous in terms of origins, cultural characteristics, and the diversity of social networks. Although the group of older migrants by itself should not be regarded as a group with special/distinct needs from the outset (White Citation2006), the group does include ‘some of the most disadvantaged and socially-excluded of western Europe's older people’ (Warnes and Williams Citation2006, p. 7).
This paper reflects on one particular migrant population in the second ‘core’ migrant group: Turkish ‘first generation’ labour migrants in the Netherlands. The Turkish migrants constitute the largest migrant group in the Netherlands; together with Moroccan, Surinamese, Antilles and Moluccan migrants they make up 6% of the total Dutch elderly (55+) population (Schellingerhout Citation2004). Healthwise, there is considerable variation among the different migrant groups. (Inter)-individual variation aside, older adults from Turkish and Moroccan descend are generally found to be in worse health compared to their native Dutch peers (van der Wurff et al. Citation2004; Parlevliet et al. Citation2016).
This is not to say that ‘being a migrant’ automatically results in detrimental health. Rather, a lower health status is often an accumulation of factors that relate to the migrant experience, including age, sex and level of education (Schellingerhout Citation2004; Verhagen et al. Citation2013). Different indicators of health have furthermore been found to interact: chronical and physical limitations lead to a lower psychological wellbeing and decreased perception of health (Blankevoort et al. Citation2013; Christopher Citation2014). In a similar vein, environmental factors contribute to the (perception of) health status, and the ability to seek help or assistance (Birren and Schaie Citation2001). Moreover, the outlook on aging as a process of decline vs. an accumulation of experiences, see Ramscar et al. (Citation2014), contributes to a positive or negative view on aging and may influence cognitive and social behaviour (see section 2.4).
2.2. The l2 environment
The L2 environment is one such factor that interacts with health outcomes in complex ways. Immediate effects are observed in communicative settings, whereby a limited L2 proficiency restricts communication in especially medical settings. Clients in L2-dominant institutional care are less satisfied with the care they receive and are prone to social isolation (Ramos and Karl Citation2016). Vice-versa, better L2 communication has been directly associated with increased use of health facilities and use of care by Turkish older adults both in the Netherlands and in Germany (Fassaert, Hesselink, and Verhoeff Citation2009; Wengler Citation2011). Below the communicative surface, however, the L2 environment also plays a role in migrant wellbeing. Language is closely tied to identity formation and acculturation.
Among Turkish immigrants in Europe, the Turkish language is the strongest marker of identity (Yagmur and van de Vijver Citation2012). As such, the Turkish immigrant community in the Netherlands is considered a high vitality group within the concept of ethnolinguistic vitality (EVT) (Yagmur Citation2009). The degree of linguistic shift to the host language or home-language maintenance is an indicator of a minority group's EVT. Low vitality groups assimilate to the host language and culture, as they lack distinctiveness as a group, whereas high vitality groups retain much of their language in a multilingual setting. The high L1 language maintenance of the Turkish group is largely because of the well-organised group they form in Dutch society (e.g. high birth rates, densely concentrated living areas) and their extensive ethnic support network.
This high L1 maintenance may come at a cost regarding L2 proficiency. Statistics on Dutch language proficiency in the Netherlands show that, in general, the older Turkish population (age 55+) often report to have significant problems with understanding/speaking Dutch (Huijnk and Andriessen Citation2016). In his review on the health status of older migrants in the Netherlands, Schellingerhout (Citation2004) reports that 61% of Turkish older adults require linguistic assistance at medical appointments. These limited L2 skills are a direct result of the migration policies in the 1950s/60s in the Netherlands, whereby the migrant workers were attracted on a temporary premise; the idea was that after a few years they would return to Turkey (some migrants still hold on to this idea: Liversage and Mirdal (Citation2017) explore the strength of this ‘myth of return’ in a longitudinal study of two Turkish immigrants in Denmark, whose wish to return turns into a myth as time goes by). Therefore, both the Turkish immigrants and the Dutch government did not feel the initial need to invest in the Dutch language. Grouped housing and long working hours at factories with colleagues from the same nationality fostered the establishment of dense ethnic networks (Yagmur Citation2011; Ciobanu, Fokkema, and Nedelcu Citation2017).
For a large majority of the Turkish immigrants, these conditions mark their degree of cultural integration. Integration, or other acculturative strategies (assimilation, separation and marginalisation), in turn, also determine (mental) health status. Acculturation has been defined as the (group and individual) changes that occur when different cultural groups are in continuous contact (Redfield, Linton, and Herskovits Citation1936). Research among Turkish adults in the Netherlands and Germany has noted higher indices of psychological distress and depression for those individuals with a low degree of acculturation. For Turkish first- and second generation migrants, a higher degree of integration is associated with lower rates of depression, whereas the opposite is found for higher degrees of marginalisation and separation (Ince et al. Citation2014; Janssen-Kallenberg et al. Citation2017).
2.3. Social network formation
In social interaction, Wei (Citation1994) observes a reciprocal relationship between L2 proficiency and establishing social network ties with the host community by Chinese immigrants in Britain, whereby a better proficiency enables network formation that, in turn, reinforces language skills. This circular movement also operates in reverse, in that those with limited L2 skills are less able to connect with the host community, thus creating fewer opportunities to practise the language. For Turkish migrants, the frequent absence of L2 social network ties may also be fuelled by the initial idea of ‘temporality’ of their stay in the Netherlands.
Moreover, high L1 maintenance and low L2 skills may invoke linguistic insecurity or (second) language anxiety. For first-generation immigrants (Turks in the Netherlands), Sevinc and Dewaele (Citation2016) and Sevinc and Backus (Citation2017) find that majority language anxiety (MLA) is more prevalent than heritage language anxiety, and add MLA to Wei's (Citation1994) vicious circle linking language proficiency to social network formation. MLA ensues from a (perceived) negative evaluation of L2 use by native speakers and may lead to avoidance of using that language, which leads to reduced proficiency and conflicted identities, in which a sense of belonging is distorted. The sense of belonging and attachment to an identity is vital to involvement in social networks and building social capital (Haslam et al. Citation2009). Rejection on linguistic grounds may fuel insecurity and decreased social interaction, which is a locus for more pressing problems such as loneliness and depression.
In a qualitative study on social embeddedness of older Turkish labour migrants in Vienna, Palmberger (Citation2017) argues that those migrants with access to cultural, political and religious associations are generally socially well-embedded. Despite adverse conditions relating to their socio-economic and migration background, migrants with well-embedded social ties manage within their everyday lives. However, accessibility and social engagement may be limited when older migrants are physically or psychologically compromised, or when these voluntary associations are not present in the direct environment.
Indeed, research on social networks of older adults reveals that adults who are embedded in diverse networks indicate to have higher subjective wellbeing levels (and lower levels of loneliness and anxiety). A wider range of social ties contributes to wellbeing, independent of health status and demographic confounds (Litwin and Shiovitz-Ezra Citation2010).
Clearly, the social environment shapes language development and influences health status and psychological wellbeing at various levels, from the degree of integration to the degree and quality of interaction. Language development is further determined by other, individual factors such as low educational levels, limited literacy abilities and cognitive dispositions, which constrain the ability or willingness of migrants to take up Dutch language courses or, in the case of literacy, limit access to health care facilities (Kristiansen et al. Citation2016).
2.4. Language use and aging
In their book on aging in multilingual contexts, de Bot and Makoni (Citation2005) propose a dynamic model of language use in aging, in which aging is regarded as a system, that develops under the influence of changes within the individual (physical and psychological) and external changes relating to attitudes towards aging in society, and an individual's perception of this. This means that age-related psychological changes may impact language use: changes in cognitive resources, such as declining memory or attention hamper the maintenance or development of language skills. Similarly, fewer language skills may trigger low quality interaction or ‘elderspeak’ (Kemper and Harden Citation1999), as a result of changing perceptions or stereotypes associated with old age.
Although a full treatment of the cognitive processes at work in language development and the impact of aging on this is beyond the scope of this paper, highlighting this issue here is important as it is likely that different cognitive dispositions influence language usage outcomes (Wingfield and Grossman Citation2006; Burke and Shafto Citation2008). This may lead to more or less social engagement or increased susceptibility to loneliness and the development of depressive symptoms, for example. In addition, mindset and (aging) stereotypes influence cognitive behaviour. An individual's perception of her cognitive abilities (whether these are ‘fixed’ or flexible accross the lifespan) has direct repercussions on the ability to learn and adopt a positive mindset (Dweck Citation2000; Dweck and Molden Citation2017). Ramscar et al. (Citation2014) argue that aging as a process of decline is based on false beliefs. They rather consider aging as an accumulation of experience, and as such explain slower performance on psychometric tasks as a reflection of increased knowledge rather than cognitive decline. In line with Dweck's observations, Ramscar et al. (Citation2014, p. 35) note that ‘[…] the [prevailing stereotypical] ideas about “cognitive decline” […] are likely to be exerting a strong, negative influence on the lives of many millions of older adults’.
From a socio-cultural perspective, language and cognition are intertwined: language is an important tool to mediate complex cognitive processes such as attention and memory (Vygotsky Citation1978). The process of mediating higher mental processes using language is called ‘languaging’, and investigated in relation to age-related cognitive decline in the work of Swain and Lapkin (Lapkin, Swain, and Psyllakis Citation2010; Swain and Lapkin Citation2011; Swain, Lapkin, and Deters Citation2013). To study the effect of languaging on cognition, the authors conducted a number of qualitative studies involving mildly cognitively impaired and socially isolated long-term-care residents in Canada. They asserted that engaging in languaging activities, which are effortful and go beyond simple communication (e.g. solving crossword puzzles, discussing an article or writing a poem), improves cognitive functioning. When considering language as a mediating cognitive tool, stereotypical language use such as elderspeak may be harmful to cognition. Swain Swain (Citation2013) remarks that elderspeak inhibits the ability of the recipient ‘to language’, through which self-esteem is lowered and cognitive decline fuelled (Swain Citation2013).
Moreover, in communicative settings, limited L2 proficiency may put up a barrier in accessing institutions or receiving desired care. A study towards doctor-migrant patient (with low L2 skills) communication in a hospital in Ghent, Belgium revealed that those migrants who do not bring along an informal interpreter, often a family or community member, to consults – as their L2 proficiency is just sufficient enough to warrant the absence of an interpreter – are restricted in expressing their emotions and complaints. As a result, they are more vulnerable than those migrants with no L2 proficiency, who can still voice their emotions through the interpreter (De Maesschalck, Deveugele, and Willems Citation2011).
It is thus not simply the presence or absence of language skills that puts older migrants at an advantage or disadvantage with regard to managing their aging process, but the way in which individuals handle communicative situations in the L2 environment. Moreover, cognitive abilities, issues of identity formation and environmental opportunities to interact are pivotal in advancing L2 development and increasing L2 usage. The interaction of all of these factors may lead some individuals to avoid L2 social interaction and invest in their L1 social networks. However, when social opportunities are limited and a social network is lacking, some migrants may indeed be, as Warnes et al. (Citation2004) note in Section 2.1 above, among the most vulnerable older adults in society.
The current study aims to identify whether, and when, older migrants are linguistically compromised and whether limited psychological wellbeing for these older adults may be heightened by the L2 context. The focus here is in particular on female Turkish migrants, as it has been noted that for this group, L2 proficiency is lowest. They often have had fewer opportunities to practise the language and tend to have a lower educational level (Palmberger Citation2017), and may experience risks relating to L2 proficiency, e.g. after becoming widowed.
In studying this issue, we adopt a mixed-methods approach, as we believe that solely studying group processes can only reveal limited information on language usage. As language and aging processes are highly individually distinct, a qualitative approach allows for a more fine-grained insight into the interaction between L2 proficiency, usage and mental, physical and social aging processes. Although a mixed-methods approach increases the risk of wrongly generalising individual results to larger groups, such a methodology is an insightful addition to the usually larger group studies on migrants in the medical and behavioural sciences. Individual experiences are important in highlighting differential (linguistic) experiences and subsequently targeting interventions, which may be broader in nature.
By means of semi-structured interviews and language, literacy and cognitive tasks, we seek to answer the question of whether (and when) language forms a barrier in maintaining independence and a high sense of wellbeing in the aging process of older female Turkish adults in the Netherlands. Our hypothesis is that a low level of proficiency in Dutch constrains individuals in building resources to ward off dependence and increase the risk of social isolation and depression.
3. Method
3.1. Participants
A total of 42 ‘first-generation’ Turkish women were interviewed (of whom 39 complete datasets (interview + tasks) were obtained). Following Sevinc and Backus (Citation2017), we regard ‘first generation’ Turkish immigrants as either migrants who arrived in the Netherlands through labour migration or family reunification in the 1960s/70s, as well as those migrants who migrated after marrying a second-generation Turkish spouse. Informants ranged in age from 52–84 (mean age = 61). provides an overview of informant's age, education, and length of residence in the Netherlands.
Table 1. Demographic information of the informants. Age at testing, Length of residence in years, and education in years.
The informants were recruited through the network of the consultants interviewed in Pot, Keijzer, and de Bot (Citationsubmitted) and through a self-constructed network by a Turkish-speaking assistant (male) based on a snowball effect via family and professional acquaintances. Before the interview, informants received full information about the study (in Turkish) and informal informed consent was obtained. Informants did not receive financial reimbursement, but were offered a small gift at the end of the interview session.
The study did not include a native-Dutch control group. The current informant sample varied on a number of important dimensions such as age, length of residence but also educational level and, very importantly, proficiency levels of Dutch. Through this inter-group variation, and because the migrant experience has unique factors associated with it (see Section 2.1 above), the group is analysed on a continuum; as we deemed this more informative than setting off their data against a group of Dutch native speakers matched in terms of age and education level.
3.2. Materials
A questionnaireFootnote1 served as the basis for a semi-structured interview. Included in the questionnaire were questions on migration history, language usage, belonging, (language) attitudes, social relationships and health and healthcare use. These questions were adapted from the sociolinguistic questionnaire by Keijzer (Citation2007).
A subjective measure of wellbeing (CASP-12, shortened version of CASP-19) spanning the life domains of older adults; ‘control and autonomy’, ‘self-realisation’ and ‘pleasure’, was taken from Wiggins et al. (Citation2007). Questions included one's ability to carry out daily activities, satisfaction with life, feeling that life has meaning and is purposeful, feeling left-out, and experiencing economical or physical constraints. Wellbeing scores were calculated on a scale of one to four with a maximum total score of 48.
In addition, respondents completed a picture-naming task in Dutch, with a descriptive picture of a vegetable stall and an action-driven picture of a man in a tree (Nicholas and Brookshire Citation1993). This served as a rough measure of L2 proficiency. The picture-descriptions were assessed on lexical density and verb usage (cf. Gordon Citation2006). The final score reflects the ratio of verbs relative to the lexical density of the description, which provides a rough but adequate measurement of the complexity (sentence formation abilities) of Dutch language proficiency of individuals.
L2 literacy level was assessed using a measure of functional literacy based on a literacy framework for Dutch as an L2 (‘Raamwerk alfabetisering NT2’) (CITO Citation2008). Informants were asked to indicate whether they were able to read certain short passages of text, medicine prescriptions, opening hours, and could distinguish important mail from junk mail. A three point scale was used: 3 = can do this with ease, 2 = can do this but with difficulty, 1 = cannot do this.
Lastly, a working memory score was obtained from a quick-to-administer, visuo-spatial, non-verbal measurement of working memory: a Corsi Blocks Tapping Task (Corsi Citation1972). A working memory score provided insight into the cognitive abilities of individuals, which could be related to (and partly explain) performance on the language and literacy measures. Due to time restrictions and fatigue of the informants, more fine-grained measures of proficiency, literacy and cognition were not feasible.
3.3. Procedure
Each interview and set of tasks lasted between 90 and 120 min. Informants were interviewed in Turkish by either a female, Dutch-speaking interviewer joined by an informal interpreter who translated into Turkish , or a male, Turkish-speaking interviewer
. All interviews were recorded and, for the interpreted interviews, a Turkish native speaker checked the interviews to account for the accuracy in the translations. Informants were interviewed either in their own homes (n=17, where in three instances a husband actively participated in the interview), at a cultural meeting centre
or the mosque
.
3.4. Analysis
Correlation analyses were applied to note relationships between the language, cognitive, literacy and background measures, using SPSS and R to plot the data and these relationships (using a Loess smoothing curve to quickly view general trends). One-way ANOVAs and a Tukey post-hoc analysis with the CASP measure as the dependent variable were conducted to see whether a subscale of the CASP measure was related to any of the other measures. In other words, whether wellbeing was directly associated with the informants' degree of L2 mastery. Lastly we checked with an ANOVA whether informants' place of residence (urban vs rural) significantly impacted any of the other measures.
All interviews were fully transcribed.Footnote2 The transcriptions were coded following the procedure of a thematic analysis to find repeated patterns of meaning (Braun and Clarke Citation2006). The dataset was thus coded into different categories, relating to language competence, usage and learning, cultural factors, socio-emotional factors, social relationships, day-to-day activities and health and health-care use/communication. The categories were subsequently collapsed into four distinct themes: L2 competence, belonging, social relationships and opportunities/anxiety to interact, and health status. The themes provided insight into the causes for the different scores on the wellbeing questionnaire.
4. Results
To detail the role of L2 competence in this group's aging processes and wellbeing levels, this section first presents a statistical overview of the language, cognitive and background measures that were found to interact. Subsequently, the themes emerging from the interview data give insight into individual strategies and motives for higher and lower wellbeing levels related to L2 competence.
4.1. Statistical analyses
In below, descriptive results are reported for all informants on the different measures (literacy, wellbeing and working memory). The picture-descriptions were analysed using a number of lexical measures, which are reported separately in .
Table 2. Literacy measure (max 39), CASP-12 wellbeing (max 48), Corsi forward and backward span (FWS/BWS, max 8), Corsi total number of trials correctly reproduced (FWC/BWC, max 16).
Table 3. Total number of narrative words, Type/token ratio (TTR), number of sentences produced on the narrative task, proportion of correct inflected verbs, number of verbs relative to the total amount of narrative words (V/Tnarr) and number of verbs and nouns relative to the total amount of narrative words(V+N/Tnarr).
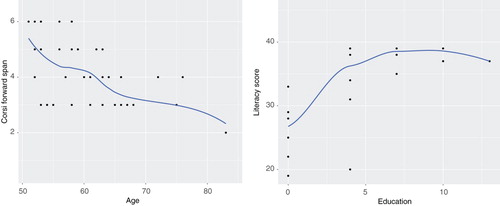
Correlation analyses revealed that age at testing negatively correlated with education in years, working memory scores and literacy (). In other words, ‘oldest old’ individuals are more often low-literate and lower educated than their ‘younger old’ peers. Furthermore, the higher an informant's age, the fewer verbs she uses in her L2, and the fewer sentences she can construct ().
Table 4. Age at testing in relation to education, working memory, literacy and wellbeing.
Table 5. Age at testing in relation to the different language measures.
Literacy level correlated positively with years of education and working memory scores (). Furthermore, those informants with higher literacy skills perform better on the lexical measures related to sentence formation ().
Table 6. Correlations between literacy level and education, language measures and working memory.
Table 7. Correlations between V/Tnarr and education, number of sentences, total narrative words, proportion of inflected verbs, literacy and age.
The correlation plots with Loess smoothing curve for working memory and literacy level and education and literacy level are provided in .
Figure 1. Correlation plots with Loess smoothing curve for working memory and age (1) and literacy level and education (2).
The wellbeing measure (CASP) did not correlate with any of the other measures, suggesting the absence of a relationship between L2 competence and wellbeing. The variation in wellbeing scores in relation to L2 proficiency is plotted in below.
Figure 2. Variation in wellbeing scores in relation to L2 competence, operationalised as total amount of verbs relative to the number of total narrative words.
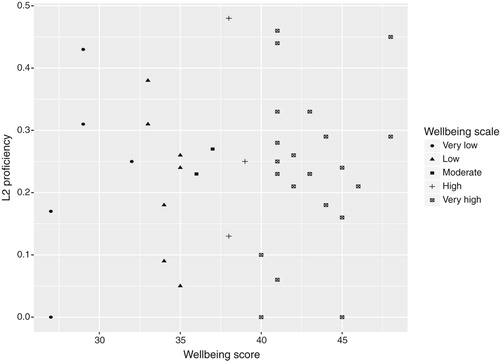
A one-way ANOVA analysis on the different wellbeing levels revealed again no relationship of any of the variables with the CASP measure. A Tukey post-hoc analysis showed a relational trend for V+N/Tnarr where the difference between the very low/low and moderate group in relation to the CASP measure approached significance (standard error = 4.909, p=.038).
As the informants were selected from both urban and rural settings, we checked whether the environment made a difference in the analyses. To this end, we coded the different cities and towns with regard to the density of the Turkish population in that area (taken from the CBS (Citation2013) data), thereby excluding Leeuwarden and Almelo because the data included only one informant from these cities.
An ANOVA on the place of residence revealed a significant difference between the places for years of education only (f=4.935, p=.001). Tukey post-hoc analyses revealed that this difference was significant or near-significant for the towns with a smaller Turkish population, Goor and Rijssen, as compared to the cities of Nijmegen and Groningen.
Power issues due to the small sample size require these analyses to be interpreted with great caution. They serve as an exploratory analysis to view potential trends in the data and the significant interactions are used as indicators for the interpretation of the interview data below.
4.2. Interview data
The quantitative data revealed no direct effect of L2 competence on wellbeing levels. The analyses were unable to detect an indirect relationship. To this end, we analysed the content of the interviews quantitatively. A few patterns in the quantitative data can be detected with regard to stressors for wellbeing levels. Some older adults report low wellbeing levels because of a poor health status, which may hypothetically limit their opportunities to engage in social interaction and makes them prone to feelings of loneliness. Other informants, however, may be content with their lives due to the presence of a strong social support network, even though their health situation is relatively low. Below, in , stressors for wellbeing levels at the lower and higher end of the spectrum are listed (omitting factors that, at the group level, have been shown above to correlate with wellbeing). These may act as resilience resources and below are illustrated with excerpts from the interviews (limited in number for reasons of space).
Table 8. Individual stressors for differential wellbeing levels from the interview data.
4.3. Health status
All informants who show low wellbeing levels note physical constraints as a main influencing factor. These constraints in turn limit individuals to participate in activities and keep up social relationships (1). A limited level of L2 proficiency in combination with a low health status further reduces mobility and interaction opportunities (2).
| (1) | 03RO17 (56): ‘I divorced my husband and things got moving. I started a language course. I found a job. I took driving lessons and went to swimming lessons. But my health problems forced me to stop’. | ||||
| (2) | 05R16 (72): ‘I cannot go anywhere. I do not go anywhere. I just sit here. I sometimes go grocery shopping; that is easy. Then I just take what I need and check out at the register’. | ||||
4.4. L2 anxiety
A low L2 competence may lead in some cases to shame and avoidance of speaking Dutch (3). Strategies for lowering this anxiety relate to group formation (4) or determination/motivation to improve L2 competence (5).
| (3) | 07GR17 (58): ‘I feel inferior when I'm talking to a Dutch person. I avoid communication. The less I speak, the better. That is how I feel’. | ||||
| (4) | 02R16 (62): ‘The people I worked with at the factory were all Turkish as well[…]. Things that I did not know or was unsure about, we could ask each other. What one person did not know, the other knew’. | ||||
| (5) | 01L17 (61): ‘If you don't know the language, you'll look at people's faces and you would not understand anything. I experienced this myself, so I told myself that I'll learn it no matter what’. | ||||
| (6) | 04V16 (translated): ‘In the 1990s, there was a Dutch course at the Turkish society. There I noticed that I did not speak correctly. I use the wrong language forms and sentence constructions. After this, I was ashamed to visit the doctor and to engage in activities. So I quit doing that. I could express myself, but felt ashamed and anxious to speak, still’. | ||||
4.5. Social network
Higher levels of wellbeing are observed when informants note the presence of a social support network. The importance of a social support network in the absence of L2 competence is illustrated in (7), and is especially true for accessing healthcare services (8).
| (7) | 03H17 (61): ‘When there's something important, I would like to have someone with a strong language knowledge with me, because I am afraid of telling the wrong things. Sometimes I take a friend with me in these situations, but not all the time’. | ||||
| (8) | 04GR17 (55): ‘We were going to the doctor with someone else in our first years in the Netherlands, but now we have the courage to go on our own. Now I'm going and if I don't understand I simply ask my doctor for clarification. […] I have to, because my children are working night and day. They cannot follow me around to supermarkets or doctors’. | ||||
A social network is typically formed through family connections, connections in the immediate neighbourhood or work contacts. Yet, as (8) shows, social support cannot always be provided.
4.6. Belonging
Experiencing positive emotions with social relationships makes informants experience a high sense of wellbeing, regardless of proficiency level. The ability to form social connections may relate to a sense of belonging (9). Nonetheless, many informants note living in-between two cultures (10) and some express the wish to return to Turkey (11). In turn, and in line with ethnolinguistic vitality theories, feelings of belonging impact L2 investment (12).
| (9) | 02GR17 (58): ‘I have a Turkish speaking network. What can I talk about with the Dutch anyway? I say ‘moi’ when I see them around the door. There are a lot of differences between our culture and theirs’. | ||||
| (10) | 04N17 (60): ‘We're foreigners here and ‘Almanci’ there. We're not Dutch or Turkish’. | ||||
| (11) | 01GR17 (52): ‘I would like to take my kids on my wings and fly to Turkey. I dream about being a bird sometimes so I could fly to my home, see my neighbours and friends’. | ||||
| (12) | 04GR17(55): ‘I don't watch [television] in Dutch at all these days. I feel like I'm living in Turkey because I always watch Turkish channels’. | ||||
5. Discussion
The present study explored new terrain in migrant and aging research by examining the often reported language barrier in migrant (health-related) aging processes through a set of quantitative language and cognitive measures and qualitative interview data. The quantitative measures revealed the hetereogeneity of the group of female older Turkish informants. Overall, working memory performance declines with advancing age, and the informants at the older end of the spectrum show lower levels of education and literacy skills. In combination with insights from the qualitative interviews, individual differences with regard to the maintenance and (potential) detrimental impact of a limited L2 proficiency on aging and wellbeing are observed.
The quantitative data reveal that the population under scrutiny markedly differs in cognitive, physical and social/life-style factors. Age of individuals correlates with education, working memory score and literacy level, meaning that the ‘oldest old’ adults show lower working memory performance, lower levels of education and generally have underdeveloped literacy skills. These relations are not surprising, as clear links between education and literacy level have been established by studies in the past (Howard, Sentell, and Gazmararian Citation2006; van der Heide et al. Citation2013).
Considering the language measures in this study, there is a visible trend towards less complex sentence constructions by older individuals. Moreover, lower educated and low-literate individuals use fewer (inflected) verbs, which corresponds to findings from other low L2-literate populations (Tarone, Bigelow, and Hansen Citation2009). We know from studies on language learning by low-literate individuals that they typically lack metacognitive and metalinguistic awareness (knowledge about language), which may hamper their language learning in traditional classroom settings (Tarone, Bigelow, and Hansen Citation2009; Kurvers, van de Craats, and van Hout Citation2015). It is necessary to point out, however, that some individuals are low-literate in general, whereas others have literacy skills in their L1, but lack L2 literacy skills.
As becomes apparent in the interview data, often the lower educated and low-literate individuals have had limited opportunities to interact and practice Dutch. Taking care of the household, sometimes in combination with factory work with other Turkish colleagues, prevented the adults from attending language classes and investing time in learning (see quotations (4) and (9)). In addition, the initial living conditions (see Section 2.1) promoted the formation of dense L1 networks, through which the need to learn the L2 was low and, currently, these older adults rely heavily on their family and/or L1 support network for linguistic assistance. If this network/support is absent, as in quotation (8), linguistic insecurities need to be overcome to be able to manage (health) communication in the L2. Otherwise, L2 anxiety may promote isolation (see quotation (2)). Moreover, limited learning skills in general may have contributed to negative experiences with and subsequent avoidance of language learning classes and L2 interaction. Quotation (6) is in this regard of particular interest.
Linguistic insecurities are specifically heightened in medical settings, where communicating important information can make the difference between an adequate or inadequate treatment. Whereas (informal) interpreters at important meetings are preferred (recall the Ghent study by De Maesschalck, Deveugele, and Willems Citation2011), the interview data show that informal interpreters are not always available or may not fully disclose all information (see quotation (7)). There seems to be a linguistic trade-off between either involving an interpreter in healthcare communication and not disclosing or communicating all information (correctly), or communicating without an interpreter through which expressing complaints and emotions is limited, and L2 insecurities may be heightened.
The quantitative data also show marked differences in wellbeing levels within the group of older Turkish adults. Although these are not directly related to L2 proficiency (see ) the interview data, in line with Palmberger's (Citation2017) observations, reveal that stressors that mark a change in wellbeing levels are related to social aspects of aging, attitudes towards the L2 environment and a sense of belonging. In other words, L2 proficiency may modify social behaviour, and, by consequence, indirectly influence wellbeing levels. Although in communicative L2 settings this leads to the language barrier reported in the (health) literature, not in all cases does this barrier increase the likelihood of becoming vulnerable or prevent access to healthcare and -information. Those older adults with a lower level of L2 proficiency are not necessarily worse off healthwise, or feel less well, as long as they are firmly embedded in a social network (see quotation (9)).
L2 interaction through work or neighbourhood contacts fuels the creation of social relationships in the L2 and, in turn, promotes situational belonging (reminiscent of Wei's (Citation1994) vicious circle). Contrastively, the dominantly Turkish-speaking network of most of the informants (see the quotations in Section 4.6) typically supports attachment to Turkish culture and the maintenance of the Turkish language, reinforced by TV input and contact with family members in Turkey. This links back to the high ethnolinguistic vitality of Turkish in the Netherlands (see Section 2.2). A meta-analysis on acculturation and mental health has assessed that being oriented towards both cultures is associated with the lowest (mental) health issues and low risk for depression (Yoon et al. Citation2013).
Nonetheless, a firm embedding in a social L1 network, where dependency on family is high but L2 insecurity low also allows older migrants with a low L2 competence to age ‘well’ in a linguistically familiar environment where they feel at home. Based on the interview data, we have tried to capture this relationship between language, wellbeing and social network in .
Figure 3. Schematic representation of the interaction between language, wellbeing and social network.
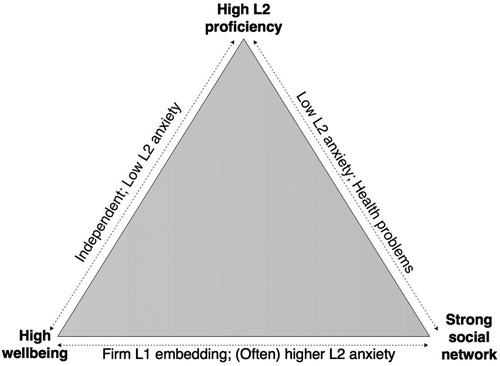
The triangle in illustrates three of four distinguishable scenarios relating to language, social support and wellbeing within this group. On one side of the triangle there are the older adults who have a relatively high L2 proficiency and a high sense of wellbeing, but perhaps a weaker social support network (or have stressed this less in the interviews as for them social support (relating to language) is less necessary). They are often independent and demonstrate low levels of L2 anxiety. On the other side are those individuals who have a strong support network and a high level of L2 proficiency, but low wellbeing levels. These older adults also exhibit low levels of L2 anxiety, but often have physical or mental health problems that markedly lowers their sense of wellbeing. On the third side of the triangle are those older adults with a firm embedding in an L1 support network, who can get by without much L2 knowledge because of a heavy reliance on others. These older adults are dependent, but, when in L2 situations, often show higher levels of L2 anxiety. There is a fourth scenario, that falls outside these boundaries and is thus not pictured in the triangle, whereby individuals have both a low sense of wellbeing, low social support and low L2 proficiency. These older adults, of which there are three in the current dataset, spend most of their time indoors and often report physical or mental health problems. Quotation (2) is an example of this fourth, detrimental scenario.
These four scenarios are not rigid and individuals may move between corners of the triangle depending on changing social, linguistic or health-related circumstances. A small group of individuals in the sample has invested in language courses at a later age (see quote (1) and (5)) or overcome their linguistic insecurities and gained more independence (see quote (8)). Other individuals see their (neighbourhood) network crumbling as result of old age or remigration of neighbours/friends. For this group, an acute loss of social support may result in withdrawal from social interaction and heightened linguistic insecurity. Loss of linguistic resources to maintain independence can be compensated for by the presence of a family support network, but this may also work the other way around.
As such, the triangle also highlights to some extent the dynamic role that language occupies in studying migrant aging. As becomes evident from the interviews, individual migration trajectories, but also notions of acculturation and ethnolinguistic vitality, as well as a deficit or experience-oriented perspective on aging (see Section 2.4) shape language and social experiences that in one individual culminate in high linguistic insecurity and low social interaction, and in others a willingness to master the L2 and strengthen L2 social network ties. In combination with an individual's initial conditions, such as educational level, literacy skills, place of residence, and life-experiences (e.g. heavy factory work, household duties, and the idea of ‘temporality’, which may have culminated in a form of pendular migration whereby individuals divide their time between their country of origin and the host country), the impact of language on aging trajectories is highly individually distinct.
This subsequently makes the ‘language barrier’ difficult to study from a methodological point of view. Here, we have highlighted only the most foregrounded factors in this particular sample of informants relating to the linguistic influence on aging processes, as there are many more (e.g. acculturative stress in acculturation processes, see Jang and Chiriboga Citation2010). Language is a contextually-embedded variable and as such cannot be studied in isolation from other ‘confounding’ factors. Of course, it is important to consider demographic, lifestyle, health and cognitive characteristics when assessing the impact of a social variable such as language on the aging process, yet controlling for all of these factors creates a distorted picture of reality. A combination of both quantitative measures, background measures and interviews to distinguish individual life trajectories, allows to gauge the differential impact of these confounding factors on L2 development and language usage. We stress, therefore, that the outcomes of this study are only to a certain extent generalisable to a wider population of older migrants. Nonetheless, this study is, to our knowledge, the first to systematically investigate the effects of the often-reported ‘language barrier’ on migrant aging. Sometimes, a limited L2 proficiency does result in a language barrier and steer the aging process in a detrimental direction, but this may be circumvented through an older migrant's firm embedding in an L1 support network.
5.1. Limitations
One could ask whether issues of language are related not to competence in the L2 but rather result from overall lower linguistic abilities. The correlation of literacy level and education with L2 competence in this study does suggest that a lower degree of literacy restricts linguistic abilities, something that is also highlighted in the literature on language learning and literacy (lower meta-linguistic awareness, see Kurvers, van de Craats, and van Hout Citation2015). For these older adults, the absence of literacy is also problematic in an L1 environment. To this end, insight into their L1 abilities would have been useful, yet for the understanding of the influence of the L2 environment and L2 competence on the larger picture of aging this added information is not a necessity.
In addition, the study raises some methodological issues. Informants were interviewed in different settings that likely have influenced their ability or willingness to share information. Sevinc and Backus (Citation2017), who used a similar methodological approach (interviews), note that in their responses, majority language anxiety levels were generally higher for self-reports when the interlocutor was a native speaker. It could well be that individuals showed a heightened level of anxiety when confronted with questions in Dutch. The informal interpreter who was present, however, acted as a mediator, also on an emotional level, because he or she had a bond of trust with the informant, which allowed the informants to open up and share their emotions. For those interviews directly administered in Turkish, speaking one's mind may have been easier, yet has similar drawbacks. The male gender of the interviewer, first of all, may have limited the female informants to talk about personal issues and emotions and, secondly, there was no established trust-relationship between the interviewer and informant, which may have made some individuals refrain from extensively discussing certain subjects.
This is connected to the likely biased informant sample. We have tried to obtain a heterogeneous informant sample by recruiting informants from different parts of the Netherlands, smaller towns as well as larger cities, and from a variety of socio-economic backgrounds (most pronounced in the differential level of education). Nonetheless, participation depends on availability and it is likely that we have not reached the most vulnerable individuals in the population. Despite these limitations, however, the group shows a large degree of individual variation.
To be able to tease apart low literacy and L2 proficiency from socio-economic status or ‘the migrant experience’, we have tried to include an equal number of native Dutch low-educated, low-literate adults. We obtained five datasets (interviews + tasks) from L1 native Dutch adults from a variety of backgrounds, which is not enough to contrast with the Turkish informants. The common denominator of these five interviews was the shame that is associated with limited literacy skills and which leads to avoiding certain social situations. This is markedly different from the factors resulting in social avoidance for the Turkish group, for whom low literacy is much more readily accepted by the native Dutch interlocutors. This finding underscores our decision to analyse the Turkish informants on a continuum (see Section 3.1).
6. Implications and conclusion
In a society of which its older population is expanding, health-care policies are geared towards providing efficient care with limited financial and professional means. In the Netherlands, this meant a transition in the organisation of the health-care system towards a more liberal model that was realised in early 2015 (van de Schroot and de Jong Citation2014). Individuals are encouraged to remain (living) independent with the help of their own social network. Encouraging individuals to invest in developing L2 skills may significantly lower L2 anxiety and increase health-related independence.
An interesting avenue for an intervention study to promote L2 use among this older migrant group may be through the concept of languaging addressed in Section2.4. From the interviews it becomes apparent that most older adults with a low proficiency tend to avoid L2 communicative situations, yet can get by with some rudimentary Dutch phrases (at the supermarket, at the doctor) that they acquired during their extensive stay in the Netherlands (see e.g. quote (8)). As it has been proven that meaningful and effortful communication in the L1 can significantly boost an individual's cognition (and self-worth), engaging in communication in the L2, by building on what the participant already possesses of L2 knowledge and extensive scaffolding, L2 anxiety can be lowered and cognition may be enhanced (see Pot, Keijzer, and de Bot Citation2017).
This study has contributed to our understanding of the differential impact of a limited L2 proficiency on the aging process and, moreover, has highlighted the embedded nature of language in (social) aging processes. Some individuals avoid L2 interactions and build a strong L1 support network, which allows them to age relatively well in an L2 environment. When social opportunities are limited, however, older migrants may need to overcome linguistic insecurities to avoid isolation and loneliness, with differential rates of success.
Acknowledgments
We would like to thank all informants for taking part in the study and their informal interpreters who assisted with the interviews. We also thank Egemen Curuk for his helpful assistance in recruiting and interviewing informants. In addition, we would like to thank two anonymous reviewers for their insightful comments on an earlier version of this paper.
Disclosure statement
No potential conflict of interest was reported by the authors.
Notes on contributors
Anna Pot is a PhD candidate at the department of Applied Linguistics at the University of Groningen. Her research project centers on the different cognitive and social aspects of multilingual aging, both in an immigrant context as well as in a native population of older adults in the Netherlands.
Merel Keijzer is Associate Professor of Applied Linguistics at the University of Groningen, where she also holds a Rosalind Franklin Fellowship position. Her research interests span different facets of bilingualism: bilingual education, bilingual processing, first language attrition, and the cognitive consequences of bilingualism. Her main research interest is in bilingualism and cognitive aging.
Kees de Bot got his PhD from the University of Nijmegen in the Netherlands. His interests range from bilingual processing to language attrition and language development over the lifespan. He recently retired from the University of Groningen and is now working at the University of Pannonia in Hungary.
Notes
1 The questionnaire can be obtained by contacting the first author.
2 In Dutch for the interpreted interviews, and in Turkish for the Turkish interviews. The interviewer who interviewed in Turkish did not master Dutch. Therefore, the transcriptions were subsequently translated from Turkish into English.
References
- Asanin, J., and K. Wilson. 2008. “‘I Spent Nine Years Looking for a Doctor’: Exploring Access to Health Care Among Immigrants in Mississauga, ON, Canada.” Social Science & Medicine 66 (6): 1271–1283.
- Birren, J. E., and K. W. Schaie. 2001. Handbook of the Psychology of Aging. San Diego, CA: Academic Press.
- Blankevoort, C. G., E. J. A. Scherder, M. B. Wieling, T. Hortobágyi, W. H. Brouwer, R. H. Geuze, and M. J. G. van Heuvelen. 2013. “Physical Predictors of Cognitive Performance in Healthy Older Adults: A Cross-Sectional Analysis.” PLoS ONE 8 (7): e70799.
- Bolzman, C. 2012. “Democratization of Ageing: Also a Reality for Elderly Immigrants?” European Journal of Social Work 15 (1): 97–113.
- Bolzman, C. 2013. “Ageing Immigrants and the Question of Return: New Answers to an Old Dilemma?”. In Return migration in later life, edited by John Percival, 67–88. Bristol: Policy Press.
- Braun, V., and V. Clarke. 2006. “Using Thematic Analysis in Psychology.” Qualitative Research in Psychology 3 (2): 77–101.
- Burke, Deborah M., and Meredith A. Shafto. 2008. “Language and Aging.” The Handbook of Aging and Cognition 3: 373–443.
- Carballo, M., J. J. Divino, and D. Zeric. 1998. “Migration and Health in the European Union.” Tropical Medicine & International Health 3 (12): 936–944.
- Christopher, G. 2014. The Psychology of Ageing: From Mind to Society. Basingstroke: Palgrave MacMillan.
- Ciobanu, R. O., T. Fokkema, and M Nedelcu. 2017. “Ageing as a Migrant: Vulnerabilities, Agency and Policy Implications.” Journal of Ethnic and Migration Studies 43 (2): 164–181.
- Corsi, P. M. 1972. “Human Memory and the Medial Temporal Region of the Brain.” Dissertation Abstracts International 34: 819B.
- de Bot, K., and S. Makoni. 2005. Language and Aging in Multilingual Contexts. Bilingual Education and Bilingualism 53. Clevedon: Multilingual Matters Ltd.
- De Maesschalck, S., M. Deveugele, and S. Willems. 2011. “Language, Culture and Emotions: Exploring Ethnic Minority Patients' Emotional Expressions in Primary Healthcare Consultations.” Patient Education and Counseling 84: 406–412.
- Dias, S. F., M. Severo, and H. Barros. 2008. “Determinants of Health Care Utilization by Immigrants in Portugal.” BMC Health Services Research 8: 207.
- Dweck, C. 2000. Self-theories: Their Role in Motivation, Personality, and Development. 1st ed. Philadelphia, PA: Psychology Press.
- Dweck, C. S., and D. Molden. 2017. "Mindsets: Their Impact on Competence Motivation and Acquisition." In Handbook of Competence Motivation: Theory and Application, edited by Andrew J. Elliot, Carol S. Dweck, David S. Yeager, 135–154. New York: Guilford Press.
- Fassaert, T., A. E. Hesselink, and A. P. Verhoeff. 2009. “Acculturation and Use of Health Care Services by Turkish and Moroccan Migrants: A Cross-sectional Population-based Study.” BMC Public Health 9: 332.
- Forssel, E., and S. Torres. 2012. “Social Work, Older People and Migration: An Overview of the Situation in Sweden.” European Journal of Social Work 15 (1): 115–130.
- Gordon, J. K. 2006. “A Quantitative Production Analysis of Picture Description.” Aphasiology 20 (2): 188–204.
- Haslam, S. A., J. Jetten, T. Postmes, and C. Haslam. 2009. “Social Identity, Health and Well-being: An Emerging Agenda for Applied Psychology.” Applied Psychology 58 (1): 1–23.
- Howard, D. H., T. Sentell, and J. A. Gazmararian. 2006. “Impact of Health Literacy on Socioeconomic and Racial Differences in Health in an Elderly Population.” Journal of General Internal Medicine 21 (8): 857–861.
- Huijnk, W., and I. Andriessen. 2016. “Integratie in zicht? De integratie van migranten in Nederland op acht terreinen nader bekeken.” Technical Report. Den Haag: Sociaal en Cultureel Planbureau. Accessed August 23, 2017. https://www.scp.nl/Publicaties/Alle_publicaties/Publicaties_2016/Integratie_in_zicht.
- Ince, B. U., T. Fassaert, M. de Wit, P. Cuijpers, J. Smit, J. Ruwaard, and H. Riper. 2014. “The Relationship between Acculturation Strategies and Depressive and Anxiety Disorders in Turkish Migrants in the Netherlands.” BMC Psychiatry 14 (1): 249–267.
- Jang, Y., and D. A. Chiriboga. 2010. “Living in a Different World: Acculturative Stress Among Korean American Elders.” The Journals of Gerontology: Series B 65 (1): 14–21.
- Janssen-Kallenberg, H., H. Schulz, U. Kluge, J. Strehle, H. Wittchen, U. Wolfradt, U. Koch-Gromus, A. Heinz, M. Mösko, and D. Dingoyan. 2017. “Acculturation and Other Risk Factors of Depressive Disorders in Individuals with Turkish Migration Backgrounds.” BMC Psychiatry 17: 264.
- Karl, U., and S. Torres. 2015. Ageing in Contexts of Migration. London; New York: Routledge.
- Keijzer, M. C. J. 2007. “Last in First Out? An Investigation of the Regression Hypothesis in Dutch Emigrants in Anglophone Canada.” PhD diss., Vrije Universiteit, Amsterdam.
- Kemper, S., and T. Harden. 1999. “Experimentally Disentangling What's Beneficial about Elderspeak from What's Not.” Psychology and Aging 14 (4): 656–670.
- Kristiansen, M., O. Razum, H. Tezcan-Güntekin, and A. Krasnik. 2016. “Aging and Health among Migrants in a European Perspective.” Public Health Reviews 37: 20.
- Kurvers, J., I. van de Craats, and R. van Hout. 2015. “Footprints for the Future: Cognition, Literacy and Second Language Learning by Adults.” In Adult Literacy, Second Language, and Cognition, edited by I. van de Craats, J. Kurvers, and R. van Hout, 7–32. Nijmegen: CLS.
- Lai, D. W. L., and S. B. Y. Chau. 2007. “Predictors of Health Service Barriers for Older Chinese Immigrants in Canada.” Health & Social Work 32 (1): 57–65.
- Lapkin, S., M. Swain, and P. Psyllakis. 2010. “The Role of Languaging in Creating Zones of Proximal Development (ZPDs): A Long-Term Care Resident Interacts with a Researcher.” Canadian Journal on Aging/La Revue canadienne du vieillissement 29 (4): 477–490.
- Litwin, H., and S. Shiovitz-Ezra. 2010. “Social Network Type and Subjective Well-being in a National Sample of Older Americans.” The Gerontologist 51 (3): 379–388. doi:10.1093/geront/gnq094.
- Liversage, A., and G. M. Mirdal. 2017. “Growing Old in Exile: A Longitudinal Study of Migrant Women from Turkey.” Journal of Ethnic and Migration Studies 43 (2): 287–302.
- Nicholas, L. E., and R. H. Brookshire. 1993. “A System for Quantifying the Informativeness and Efficiency of the Connected Speech of Adults with Aphasia.” Journal of Speech and Hearing Research 36 (2): 338–350.
- Palmberger, M. 2017. “Social Embeddedness in Old Age: Transnational Aging and Care among Turkish Labour Migrants in Vienna.” Journal of Ethnic and Migration Studies 43 (2): 235–249.
- Parlevliet, J. L., O. Uysal-Bozkir, M. Goudsmit, J. P. van Campen, R. M. Kok, G. ter Riet, B. Schmand, and S. E. de Rooij. 2016. “Prevalence of Mild Cognitive Impairment and Dementia in Older Non-western Immigrants in the Netherlands: A Cross-sectional Study: MCI and Dementia Prevalence in Immigrants.” International Journal of Geriatric Psychiatry 31: 1040–1049.
- Pot, A., M. C. J. Keijzer, and K. de Bot. 2017. “Enhancing Language Awareness in Migrants' Third Age to Promote Wellbeing.” In Third Age Learners of Foreign Languages, edited by Danuta Gabrys-Barker. Bristol: Multilingual Matters.
- Pot, A., M. Keijzer, and K. de Bot. submitted. “Do Low L2 Abilities Impede Healthy Aging for Migrant Older Adults in the Netherlands?” Dutch Journal of Applied Linguistics. Manuscript submitted for publication.
- Priebe, S., S. Sandhu, S. Dias, A. Gaddini, T. Greacen, E. Ioannidis, and U. Kluge, et al. 2011. “Good Practice in Health Care for Migrants: Views and Experiences of Care Professionals in 16 European Countries.” BMC Public Health 11: 187.
- CITO. 2008. “Raamwerk Alfabetisering NT2.”
- Ramos, A. C., and U. Karl. 2016. “Social Relations, Long-term Care, and Well-being of Older Migrants in Luxembourg.” GeroPsych: The Journal of Gerontopsychology and Geriatric Psychiatry 29 (2): 115–123.
- Ramscar, M., P. Hendrix, C. Shaoul, P. Milin, and H. Baayen. 2014. “The Myth of Cognitive Decline: Non-linear Dynamics of Lifelong Learning.” Topics in Cognitive Science 6 (1): 5–42.
- Redfield, R., R. Linton, and M. J. Herskovits. 1936. “Memorandum for the Study of Acculturation.” American Anthropologist 38 (1): 149–152.
- Schellingerhout, R. 2004. “Gezondheid en welzijn van allochtone ouderen.” Technical Report. Sociaal en Cultureel Planbureau.
- Sevinc, Y., and A. Backus. 2017. “Anxiety, Language Use and Linguistic Competence in an Immigrant Context: A Vicious Circle?” International Journal of Bilingual Education and Bilingualism 0 (0): 1–19.
- Sevinc, Y., and J-M. Dewaele. 2016. “Heritage Language Anxiety and Majority Language Anxiety among Turkish Immigrants in the Netherlands.” International Journal of Bilingualism 0 (0): 1–21.
- Sol-Aur, A., and E. M. Crimmins. 2008. “Health of Immigrants in European Countries.” The International migration review 42 (4): 861–876.
- Stronk, K., A. C. J Ravelli, and S. A. Reijneveld. 2001. “Immigrants in the Netherlands: Equal Access for Equal Needs?” Journal of Epidemiology and Community Health 55 (10): 701–707.
- Swain, M. 2013. “Cognitive and Affective Enhancement among Older Adults: The Role of Languaging.” Australian Review of Applied Linguistics 36 (1): 4–19.
- Swain, M., and S. Lapkin. 2011. “Languaging as Agent and Constituent of Cognitive Change in an Older Adult: An Example.” Canadian Journal of Applied Linguistics/Revue canadienne de linguistique appliquée 14 (1): 104–117.
- Swain, M., S. Lapkin, and P. Deters. 2013. “Exploring the Effect of Languaging Activities on Cognitive Functioning: The Case of an Older Adult in a Long-Term Care Facility.” Activities, Adaptation & Aging 37 (1): 1–18.
- Tarone, E., M. Bigelow, and K. Hansen. 2009. Literacy and Second Language Oracy. Oxford: Oxford University Press.
- CBS. 2013. “Turkse Nederlanders per gemeente.” Accessed July 7, 2017. https://www.volksgezondheidenzorg.info/onderwerp/bevolking/regionaal-internationaal/etniciteit/methoden.
- Uitewaal, P. J. M., D. R. Manna, M. A. Bruijnzeels, A. W. Hoes, and S. Thomas. 2004. “Prevalence of Type 2 Diabetes Mellitus, Other Cardiovascular Risk Factors, and Cardiovascular disease in Turkish and Moroccan immigrants in North West Europe: A Systematic Review.” Preventive Medicine 39 (6): 1068–1076.
- van der Heide, I., J. Wang, M. Droomers, P. Spreeuwenberg, J. Rademakers, and E. Uiters. 2013. “The Relationship Between Health, Education, and Health Literacy: Results From the Dutch Adult Literacy and Life Skills Survey.” Journal of Health Communication 18 (sup 1): 172–184.
- van der Wurff, F. B., A. T. F. Beekman, H. Dijkshoorn, J. A. Spijker, C. H. M. Smits, M. L. Stek, and A. Verhoeff. 2004. “Prevalence and Risk-factors for Depression in Elderly Turkish and Moroccan Migrants in the Netherlands.” Journal of Affective Disorders 83 (1): 33–41.
- van de Schroot, R., and F. de Jong. 2014. “Hervorming van zorg en ondersteuning: de vertaling van de transities binnen de gemeente.” Accessed August 24, 2017. http://www.vilans.nl/docs/vilans/publicaties/VILANS_ZORGTRANSITIE_DIGI.pdf.
- van Duin, C., and L. Stoeldraijer. 2014. “Bevolkingsprognose 2014–2060: groei door migratie.” Centraal Bureau voor de Statistiek. Accessed August 24 2017. https://www.cbs.nl/nl-nl/achtergrond/2014/51/bevolkingsprognose-2014-2060-groei-door-migratie.
- Verhagen, I., W. J. G. Ros, B. Steunenberg, and N. J. de Wit. 2013. “Culturally Sensitive Care for Elderly Immigrants through Ethnic Community Health Workers: Design and Development of a Community based Intervention Programme in the Netherlands.” BMC Public Health 13: 227.
- Vygotsky, L. S. 1978. Mind in Society: The Development of Higher Psychological Processes. Cambridge: Harvard University Press.
- Warnes, A. M., K. Friedrich, L. Kellaher, and S. Torres. 2004. “The Diversity and Welfare of Older Migrants in Europe.” Ageing & Society 24 (3): 307–326.
- Warnes, A. M., and A. Williams. 2006. “Older Migrants in Europe: A New Focus for Migration Studies.” Journal of Ethnic and Migration Studies 32 (8): 1257–1281.
- Wei, L. 1994. Three Generations, Two Languages, One Family: Language Choice and Language Shift in a Chinese Community in Britain. Clevedon: Multilingual Matters.
- Wengler, A. 2011. “The Health Status of First- and Second-generation Turkish Immigrants in Germany.” International Journal of Public Health 56 (5): 493–501.
- White, P. 2006. “Migrant Populations Approaching Old Age: Prospects in Europe.” Journal of Ethnic and Migration Studies 32 (8): 1283–1300.
- Wiggins, R. D., G. Netuveli, M. Hyde, P. Higgs, and D. Blane. 2007. “The Evaluation of a Self-enumerated Scale of Quality of Life (CASP-19) in the Context of Research on Ageing: A Combination of Exploratory and Confirmatory Approaches.” Social Indicators Research 89 (1): 61–77.
- Wingfield, A., and M. Grossman. 2006. “Language and the Aging Brain: Patterns of Neural Compensation Revealed by Functional Brain Imaging.” Journal of Neurophysiology 96 (6): 2830–2839.
- Yagmur, K. 2009. “Language Use and Ethnolinguistic Vitality of Turkish Compared with the Dutch in the Netherlands.” Journal of Multilingual and Multicultural Development 30 (3): 219–233.
- Yagmur, K. 2011. “Does Ethnolinguistic Vitality Theory Account for the Actual Vitality of Ethnic Groups? A Critical Evaluation.” Journal of Multilingual and Multicultural Development 32 (2): 111–120.
- Yagmur, K., and F. J. R. van de Vijver. 2012. “Acculturation and Language Orientations of Turkish Immigrants in Australia, France, Germany and the Netherlands.” Journal of Cross-Cultural Psychology 43 (7): 1110–1130.
- Yoon, E., C. Chang, S. Kim, A. Clawson, S. E. Cleary, M. Hansen, J. P. Bruner, T. K. Chan, and A. M. Gomes. 2013. “A Meta-analysis of Acculturation/enculturation and Mental Health.” Journal of Counseling Psychology 60 (1): 15–30.
