Abstract
Individual risk assessment for atherosclerotic cardiovascular disease is important for safe menopausal hormone prescription. Besides the traditional risk factors, female-specific risk variables related to pregnancy and gynecologic conditions importantly contribute to a more tailored risk assessment in women at middle age. Of these, prior pre-eclampsia/HELLP (hemolysis, elevated liver enzymes and low platelets) syndrome and early spontaneous menopause (<40 years) seem to be the strongest adverse risk variables. Concomitant inflammatory disorders should also be taken into account. Adding a coronary artery calcium score with a computed tomography scan to risk assessment has a high predictive value for future cardiovascular events. This should be considered to discriminate between low-risk and high-risk women when uncertainty exists. In women at intermediate risk, menopausal hormone therapy can be easily combined with preventive medication if cardiovascular risk factors are present. In women at higher risk who have severe disabling vasomotor symptoms, a lower dosage of hormone therapy can be considered in good collaboration between the gynecologist and the cardiologist/vascular specialist.
摘要
动脉粥样硬化性心血管疾病的个体风险评估对于安全的绝经后激素处方具有重要意义。除了传统的风险因素, 与妊娠和妇科疾病相关的女性特有的风险变量对中年女性进行更有针对性的风险评估具有重要意义。其中, 先兆子痫/HELLP(溶血、肝酶升高和血小板降低)综合征和早期自发性绝经(<40岁)似乎是最强烈的不良风险变量。伴随的炎症性疾病也应该被考虑在内。将计算机断层扫描冠状动脉钙化积分加入风险评估中, 对未来的心血管事件有很高的预测价值。当存在不确定性时, 应考虑区分低风险和高风险女性。在中等风险的女性中, 如果存在心血管危险因素, 绝经激素治疗可以很容易地与预防性药物相结合。对于有严重血管舒缩症状的高风险女性, 在妇科医生和心血管专家的良好合作下, 可以考虑使用较低剂量的激素治疗。
Introduction
Despite all new and reassuring insights that have been gained since the Women’s Health Initiative (WHI) studies were published more than 20 years ago, the resistance against menopausal hormone therapy (MHT) has not faded away. Although there is renewed interest for menopausal symptoms and work ability, many perimenopausal women and physicians are still hesitant for MHT [Citation1]. Besides the fear for breast cancer with MHT, there is a persistent anxiety for atherosclerotic cardiovascular diseases (ASCVD). A major barrier in this discussion is the lack of collaboration between various medical disciplines to tailor individual risk appropriately. Women around middle age represent a difficult ‘grey zone’ in cardiology, with uncommon symptoms and findings at routine cardiology investigation [Citation2]. Over the last decade our understanding of ischemic heart disease in women has taken huge steps forward [Citation3,Citation4]. It is now well known that women have less obstructive coronary artery disease, with non-obstructive coronary artery disease and coronary vasomotor disorders at least twice as often as men, especially in the age group 40–70 years. Different underlying pathophysiology leads to different symptoms and requires other diagnostic and therapeutic pathways. Cardiovascular risk assessment is nowadays more accurate than it used to be and we are well able to discriminate between low-risk and high-risk women around menopausal age. This makes safe MHT prescription for each individual more feasible.
Cardiovascular risk estimation
Our insight into primary prevention of ASCVD risk factors is quite different from 25 years ago when the WHI study was still ongoing. The thresholds of normal blood pressure and lipid levels are lower with many more options for lifestyle and medical treatment. and show the latest European prevention guidelines depicted with the SCORE2 algorithms, which are derived from large population-based studies as the current leading risk charts [Citation5,Citation6]. The estimated absolute risk for a given age and combination of risk factors differs substantially across global regions, with the UK and Western European countries assigned as low-risk countries. In general, most non-smoking women aged <60 years are at low risk, whereas the majority above 60 years are at intermediate to high risk with more than 5% risk for a cardiovascular event in 10 years’ time. As women experience fewer CVD events at any given age, their absolute risks in all age groups are lower than in men. This does not mean that all perimenopausal women are at low risk. Lipid levels and blood pressure increase importantly in women aged ≥50 years [Citation7]. Of importance is that inherited ASCVD risk is not taken into account in the SCORE2 risk charts, whereas a positive family risk is an even stronger risk factor for women than for men [Citation8]. In addition, in symptomatic women the appropriate cardiac diagnosis is still underestimated as most cardiologists still use the diagnostic work-up that originally was developed for the standard male patient [Citation4]. If perimenopausal women are in the intermediate cardiovascular risk category, the use of MHT is not a strict contraindication if adequate treatment of ASCVD risk factors is provided and controlled. Another limitation of these charts is that only smoking is included as an important lifestyle factor, whereas an unhealthy diet, overweight and lack of exercise are also crucial risk factors for ASCVD.
Figure 1. Overview of atherosclerosis cardiovascular risk (ASCVD) classification in the SCORE2 charts. HDL-C, high-density lipoprotein cholesterol; SBP, systolic blood pressure.
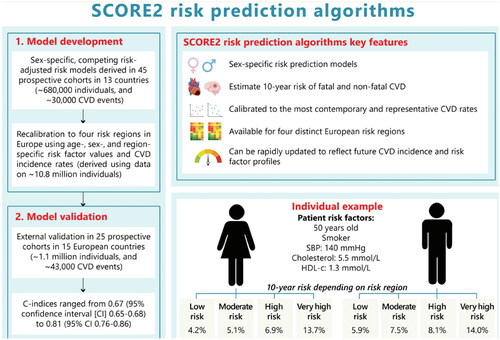
Figure 2. Atherosclerosis cardiovascular risk (ASCVD) score in low-risk European countries (UK and Western Europe) [Citation5]. HDL, high-density lipoprotein.
![Figure 2. Atherosclerosis cardiovascular risk (ASCVD) score in low-risk European countries (UK and Western Europe) [Citation5]. HDL, high-density lipoprotein.](/cms/asset/a0b321dd-1938-461c-8395-5ec372cdc51f/icmt_a_2259799_f0002_c.jpg)
Consider female-specific risk variables during the lifetime
Sex-specific factors related to hormonal and reproductive status are known to relate to ASCVD risk and are not accounted for in daily practice [Citation7]. Especially at younger age (<60 years), evidence is increasing that assessments of female-specific risk factors add to identify women at higher risk. Reproductive and pregnancy-related factors may predispose to earlier signs of endothelial dysfunction, vascular inflammation and atherosclerosis. This is less relevant for the older female population when the traditional cardiovascular risk factors dominate. This age distribution before/after 60 years also accounts for the presence of vasomotor symptoms (VMS). A recent meta-analysis showed that more severe VMS indicate a higher risk in women aged <60 years, but not in the years thereafter [Citation9]. Migraines with aura from puberty onwards are associated with a higher ASCVD risk [Citation10]. Chronic gynecologic conditions such as endometriosis and other chronic inflammatory diseases are also associated with an increased ASCVD risk [Citation11]. These conditions are less often evaluated than hypertensive pregnancies, which have now been recognized as serious ASCVD risk factors in women [Citation7]. However, there are no clear guidelines yet on how to deal with these additional risk variables, but their impact may be larger than the traditional risk factors (). It has been suggested to add 10 years of age risk in women after prior early pre-eclampsia/HELLP (hemolysis, elevated liver enzymes and low platelets) syndrome, but this is not yet indicated in the current prevention guidelines [Citation5]. For all other female-specific risk variables there is no clear guidance at the moment.
Table 1. Relative risk in early and late pre-eclampsia/HELLP in relation to traditional ASCVD risk factors.
Coronary artery calcium score with computed tomography
Adding signs of subclinical atherosclerosis by using the coronary artery calcium (CAC) score to risk factor assessment significantly improves individual ASCVD risk prediction, which is especially important for middle-aged women. The CAC score enables identification of high-risk women who are overlooked in the commonly used SCORE2 charts. It has been demonstrated that women after pre-eclampsia have a two-fold elevated risk for a positive CAC score at the age of 50 years compared to controls, whereas in women with premature ovarian insufficiency the presence of CAC was not elevated [Citation11–13]. The latter is very reassuring for safe prescription of hormone therapy until the average of menopause. In the UK National Institute for Health and Care Excellence (UK-NICE) guidelines, measurement of the CAC score in intermediate-risk patients has been added to the guidelines for patients with symptoms of angina [Citation14]. In the European and North American prevention lipid guidelines, the use of CAC is endorsed in patients at intermediate risk who may be good candidates for preventive medical therapies [Citation15]. This may apply, for instance, to individuals with slightly elevated lipid levels. A higher CAC score than normal for age/gender can be an appropriate argument to initiate lipid-lowering therapy.
There are many patients who will likely benefit from CAC testing who are not presently considered. For example, the use of the CAC scores can be helpful as a decision tool in women at intermediate ASCVD risk, when there is uncertainty about the safety of MHT. This is not yet done in clinical practice, but it is important to know that a CAC score with computed tomography is relatively cheap, takes only 10 min at a radiology department and has low radiation exposure, and its result has a high predictive value in ASCVD risk estimation. A negative (zero) CAC score in women aged <60 years reflects a low ASCVD risk and is often very reassuring for the patient and their doctor. In patients with known ischemic heart disease there is no additional value in assessing the CAC score as they already are at higher risk.
Menopausal hormone therapy in high-risk women
MHT is, in general, not recommended in women at high ASCVD risk and after a prior cardiovascular event [Citation7]. However, in clinical practice individual decisions can be made when secondary cardiovascular prevention measures are adequately taken and women continue to have disabling VMS. Important is that there are no residual cardiac symptoms and that all secondary prevention guidelines are followed according to the guidelines. The duration of MHT should be limited, depending on the relief of symptoms, with a preference for local suppletion. If oral MHT is needed, a low dose is advised, for instance only two or three times per week. In good collaboration between the gynecologist and cardiologist this can be tailored according to the individual symptoms and efficacy of the therapy.
Conclusion
Estimation of ASCVD risk in perimenopausal women needing MHT can be tailored by adding female-specific risk factors and a CAC score with computed tomography if there is doubt about individual risk. A negative CAC score has a high predictive value for a low cardiovascular risk. If necessary for disabling VMS, treatment of risk factors can be combined with temporary low-dose MHT in individuals at intermediate or even higher risk.
Potential conflict of interest
The author reports the following conflicts of interest: consultancy for Organon and Omron. The author alone is responsible for the content and writing of the article.
Source of funding
None.
References
- Riach K, Jack G. HRT in the UK: the culture behind the demand. Maturitas. 2023;175:107744. S0378-5122(23)00034-8. doi: 10.1016/j.maturitas.2023.02.003.
- Regitz-Zagrosek V, Oertelt-Prigione S, Franconi PE, et al. V. Gender in cardiovascular diseases: impact on clinical manifestations, management, and outcomes. Eur Heart J. 2016;37(1):24–34.
- Vogel B, Acevedo M, Appelman Y, et al. The lancet women and cardiovascular disease commission: reducing the global burden by 2030. Lancet. 2021;397(10292):2385–2438. doi: 10.1016/S0140-6736(21)00684-X.
- Kunadian V, Chieffo A, Camici PG, et al. EAPCI expert consensus document on ischaemia with Non-Obstructive coronary arteries in collaboration with european society of cardiology working group on coronary pathophysiology & microcirculation endorsed by coronary vasomotor disorders international study group. Eur Heart J. 2020;41(37):3504–3520. doi: 10.1093/eurheartj/ehaa503.
- Frank LJ, Visseren , et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice: developed by the task force for cardiovascular disease prevention in clinical practice with representatives of the european society of cardiology and 12 medical societies With the special contribution of the european association of preventive cardiology (EAPC). European Heart Journal. 2021;42:3227–3337.
- SCORE2 working group and ESC Cardiovascular risk collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42(25):2439–2454.
- Maas AHEM, Rosano G, Cifkova R, et al. Cardiovascular health after menopause transition, pregnancy disorders, and other gynaecologic conditions: a consensus document from european cardiologists, gynaecologists, and endocrinologists. Eur Heart J. 2021;42(10):967–984. doi: 10.1093/eurheartj/ehaa1044.
- Patel MJ, de Lemos JA, Philips B, et al. Implications of family history of myocardial infarction in young women. Am Heart J. 2007;154(3):454–460. doi: 10.1016/j.ahj.2007.05.016.
- Armeni A, Anagnostis P, Armeni E, et al. Vasomotor symptoms and risk of cardiovascular disease in peri- and postmenopausal women: a systematic review and meta-analysis. Maturitas. 2023;171:13–20. doi: 10.1016/j.maturitas.2023.02.004.
- Kalkman DN, Couturier EGM, El Bouziani A, et al. Migraine and cardiovascular disease: what cardiologists should know. Eur Heart J. 2023;44(30):2815–2828. doi: 10.1093/eurheartj/ehad363.
- Zoet GA, Benschop L, Boersma E, et al. Prevalence of subclinical coronary artery disease assessed by coronary computed tomography angiography in 45- to 55-Year-Old women With a history of preeclampsia. Circulation. 2018;137(8):877–879. doi: 10.1161/CIRCULATIONAHA.117.032695.
- Benschop L, Brouwers L, Zoet GA, et al. Early onset of coronary artery calcification in women With previous preeclampsia. Circ Cardiovasc Imag. 2020;13(11):e010340.
- Gunning MN, Meun C, van Rijn BB, et al. Coronary artery calcification in middle-aged women with premature ovarian insufficiency. Clin Endocrinol. 2019;91(2):314–322. doi: 10.1111/cen.14003.
- Alfakih K, Greenwood JP, Plein S. The 2016 update to NICE CG95 guideline for the -investigation of new onset stable chest pain: more -innovation, but at a cost? Clin Med (Lond). 2017 Jun;17(3):209–211. Available from: calcium-scoring-factsheet-245273149.pdf.
- Dzaye O, Dudum R, Reiter-Brennan C, et al. Coronary artery calcium scoring for individualized cardiovascular risk estimation in important patient subpopulations after the 2019 AHA/ACC primary prevention guidelines. Prog Cardiovasc Dis. 2019;62(5):423–430. doi: 10.1016/j.pcad.2019.10.007.
