ABSTRACT
Test anxiety of 625 medical students was assessed at semester start and two days prior to two oral exams with the PAF questionnaire [Prüfungsangstfragebogen]. Global and subscale scores for the categories emotionality, worry, interference, and lack of confidence were obtained at three time points. The first assessment was used to identify those participants (n = 104) who showed the highest PAF scores. Medical hypnosis against test anxiety was performed with one half ten days before the first exam. The other half served as a matched, untreated control group. The mean global PAF scores and the emotionality and lack of confidence scores showed a statistically significant reduction from assessment to assessment within the hypnosis group, but not in the control group. Interference increased significantly in the control group but not in the hypnosis group. In conclusion, medical hypnosis seems to be beneficial and effective in helping students reduce test anxiety.
Introduction
Test anxiety is a common phenomenon among university students (Chapell et al., Citation2005; Gerwing et al., Citation2015; Hahne, Citation1999; Neuderth et al., Citation2009; Schaefer et al., Citation2007) which may diminish academic performance and thus increase the risk of failure in an evaluative situation (Farooqi et al., Citation2012; Rana & Mahmood, Citation2010). Previous studies suggest that medical students are particularly susceptible to test anxiety (Hahne, Citation1999; Schaefer et al., Citation2007). This might be related to high levels of burnout and stress-associated psychiatric disorders in this group (Dahlin & Runeson, Citation2007; Dyrbye et al., Citation2008, Citation2006, Citation2014). The associated prevalence rates markedly exceed those found among age-matched peers and in the general population (Busch et al., Citation2013; Dyrbye et al., Citation2006, Citation2014; Warnecke et al., Citation2011).
Symptoms of mental disorders manifest early in the course of the medical curriculum and become worse within the first years (Burger et al., Citation2014; Scholz et al., Citation2015). This trend is perpetuated over the semesters (Voltmer et al., Citation2012) resulting in a very high prevalence of psychiatric disorders among postgraduates (Arigoni et al., Citation2010; Bruce et al., Citation2005; Mache et al., Citation2012). Therefore, it seems advisable to address this problem at an early stage as a component of the medical curriculum. Some pioneering attempts to offer courses on stress management and relaxation applying techniques like autogenic training, progressive muscle relaxation, meditation and mindfulness training in the medical curriculum have shown promising data (Prato & Yucha, Citation2013; Scholz et al., Citation2016; Warnecke et al., Citation2011; Wild et al., Citation2014).
The present study investigated the effect of a short hypnotic intervention on test anxiety as an important stressor and possibly relevant risk for mental health in undergraduate medical students. Previous reports already indicated the benefit of hypnotherapy in the treatment of test anxiety (Erickson, Citation1965; Hebert, Citation1984; Mathur & Khan, Citation2011; Sapp, Citation1991, Citation2013; Stanton, Citation1993). However, no detailed and controlled analyses of its impact on the four test anxiety dimensions emotionality, worry, interference and lack of confidence in medical students have been conducted so far. The present study fills this gap by applying a refined and condensed version of the TAI-G questionnaire (Hodapp, Citation1991, Citation1996), the PAF questionnaire (‘Prüfungsangstfragebogen’; German for ‘test anxiety questionnaire’) (Hodapp et al., Citation2011; Hoferichter et al., Citation2016). It was used to assess the effect of a hypnotic intervention on the dimensions of test anxiety in first year medical students at the Friedrich-Alexander-University of Erlangen-Nürnberg, Germany.
First preliminary findings of our pilot study on that topic have already been published as an interim report describing first tendencies already discernible in a small subgroup of study participants (Hammer et al., Citation2020). Having completed the acquisition and analysis of data we provide the full report after evaluation of the entire study collective in the present article.
Materials and methods
Study design
During the three semesters from winter term 2017/18 to winter term 2018/19, a total of 625 first year medical students of the Friedrich-Alexander-University Erlangen-Nürnberg, Germany were enrolled in a study investigating test anxiety. The students were surveyed repeatedly with the PAF-questionnaire (Hodapp et al., Citation2011; Hoferichter et al., Citation2016) over the course of one semester. The participants were recruited from the previously described (Hammer et al., Citation2016) anatomy course ‘functional anatomy of the locomotor system’ at the Department of Functional and Clinical Anatomy, Erlangen, Germany (Friedrich-Alexander-University Erlangen-Nürnberg, Germany). Participation in the anatomy course was obligatory for all medical students at the study site.
The course represented the students’ first curricular contact to the field of macroscopic anatomy. It did not involve cadaver dissection, but rested on tutor-guided small group teaching and the demonstration of anatomic models and prosected specimens. The course included two oral tests of approximately 10 minutes for every course participant. Passing both oral tests was mandatory to complete the course and to participate in the dissection course in the following semester. For the assessment of the students’ test anxiety the PAF questionnaire was applied at the very beginning of the semester and two days prior to each of the two oral tests. Overall and dimension-specific severity of test anxiety were thus monitored for the duration of one semester.
The first assessment was also used to identify those 104 candidates who showed the highest test anxiety scores. This cohort was divided into two groups: one half (n = 52) was assigned to the intervention group (hypnosis group) receiving a one-hour session of medical hypnosis twelve days prior to the first oral test (i.e. ten days prior the second assessment). The second half (n = 52) served as a parallelised control group not receiving any treatment or intervention. The control group closely matched the hypnosis group in terms of age and gender as well as overall and dimension-specific severity of test anxiety. A direct comparison of the hypnosis group with the control group was carried out to estimate the effect of medical hypnosis on test anxiety in our study collective.
PAF questionnaire
The PAF is comprised of 20 items representing statements that describe the participant’s thoughts and perceptions in or regarding a test situation. The participant is asked to choose an appropriate response for each item/statement on a Likert scale from 1 to 4 (1 = ‘hardly ever’, 2 = ‘sometimes’, 3 = ‘often’ and 4 = ‘almost always’). Summation of the values across all 20 items yields a total test anxiety score. The global PAF score ranges between 20 (no signs of test anxiety at all) and 80 (dramatic perception of test anxiety in every test situation). The 20 items of the PAF questionnaire are divided into four subscales comprising five items each. Every subscale represents a different dimension or category of test anxiety investigated by the corresponding five items. The dimensions are: emotionality (emotional and physical tension), worry (thoughts of failure and/or consequences thereof), interference (distraction from task by irrelevant thoughts), lack of confidence (low self-esteem, lack of confidence in one’s own abilities). Summation of the five item scores within every subscale gives a separate test anxiety value for every dimension and allows for a more differentiated analysis of the appearance and effects of test anxiety in the individual. Within every subscale 5 represents the minimum (no signs of this dimension of test anxiety at all), and 20 the maximum value (dramatic perception of this dimension in every test situation).
Medical hypnosis
An individualised hypnosis session was conducted for every participant in the hypnosis group by the same accredited hypnotherapist. The hypnosis sessions were carried out as described in detail previously (Hammer et al., Citation2020). A preliminary talk (briefing) explored the participants’ expectations, attitudes and experiences regarding medical hypnosis and the pending intervention. It was also used to ascertain when (prior to oral and/or written tests) and how (concrete symptoms) test anxiety was perceived and to exclude contraindications for the intervention. The subsequent medical hypnosis part began with an individually chosen induction (e.g., eye fixation). Then, a positive internal resource (e.g., a situation from the past that the student had mastered successfully and that had caused an emotionally and physiologically positive reaction) was evoked in the student’s perception. After that, an emotional exposition to the future anatomy test (in sensu) was imagined. As soon as the participant reported symptoms of test anxiety and/or showed vegetative signs of it (increased heart and breathing rate, signs of unease in the facial expression, etc.), the internal resource was evoked again to experience a reduction in the symptomatic. Ultimately, the continuous reduction of anxiety symptoms culminated in a positive completion of the fictive test situation. The subsequent debriefing was used to ensure the students’ alertness and orientation and to discuss the individual hypnotic experience and effect of the respective phrasings. Instructions were given to re-listen to the audio file that was recorded during the individual hypnosis on the participants´ mobile devices, intended to be performed daily in self-administered sessions at home until the examination. However, post-test surveys of all participants indicated that adherence to this instruction was highly variable.
Statistical analyses
Within the hypnosis group and the control group the mean (± standard deviation [SD]) global and subscale-specific test anxiety scores were calculated for every PAF assessment. Data distribution was tested for normality with a Kolmogorov-Smirnov test within both groups for every assessment. Differences between assessments within each group were either tested for statistical significance with a Bonferroni-corrected univariate analysis of variance for dependent samples (normal distribution) or with a Bonferroni-corrected Friedman test for dependent samples (no normal distribution). Only participants who had taken part in all three assessments were included in longitudinal comparisons within each group (dependent samples; hypnosis group: n = 46; control group: n = 42). Differences between hypnosis and control group within every assessment were tested for statistical significance with a two-tailed t-test for independent samples (normal distribution) or with a Mann-Whitney-U test (no normal distribution). Statistical analyses were performed with SPSS statistics software, version 26. The threshold for statistical significance was set at p < 0.05 for all analyses.
Ethics statement
This study was conducted in accordance with the World Medical Association Declaration of Helsinki and the appropriate guidelines for human studies. Informed and written consent was obtained from every study subject prior to the first survey. The research presented in the present manuscript was approved by the local ethics committee (application number 108_17 B) of the Faculty of Medicine, Friedrich-Alexander-University Erlangen-Nürnberg, Germany.
Results
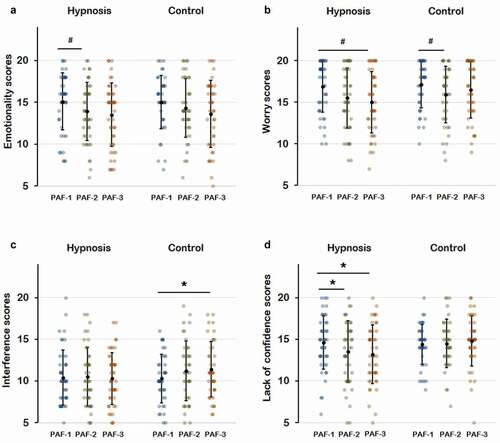
The mean (± SD) global and subscale-specific PAF scores of the hypnosis and the control group are provided in for every assessment. The global scores are also illustrated in (supplemental material), the subscale scores are also shown in (supplemental material). Within the hypnosis group, a statistically significant reduction of the global score as well as the emotionality, worry, and lack of confidence scores was detected. As for the global and the lack of confidence scores the differences between the first and the second assessment (PAF-1 vs. PAF-2) as well as the first and the third assessment (PAF-1 vs. PAF 3) were found statistically significant. Within the emotionality and worry subscales only the differences between the first and the third assessment (PAF-1 vs. PAF 3) reached statistical significance. In the control group, the only significant score reduction was found within the subscale ‘worry’ between the first and the second assessment (PAF-1 vs. PAF-2). The interference scores remained fairly constant from assessment to assessment in the hypnosis group. In the control group, however, the interference scores showed a statistically significant increase from the first to the third assessment (PAF-1 vs. PAF-3). Assessment-specific comparison of the hypnosis group and the control group yielded no statistically significant differences.
Table 1. Demographic data and PAF scores. Values represent mean ± standard deviation unless stated otherwise. PAF-1: first assessment at semester start; PAF-2: second assessment before first test; PAF-3: third assessment before second test. Asterisk: p < 0.05 (Bonferroni-corrected univariate analysis of variance for dependent samples). Hash: p < 0.05 (Bonferroni-corrected Friedman test for dependent samples). Numbers indicate compared pairs.
Figure 1. Mean (±SD) global test anxiety scores as obtained by the three different surveys with the PAF questionnaire. PAF-1: first survey at semester start; PAF-2: second survey two days prior to the first oral test; PAF-3: third survey two days prior to the second oral test. Asterisk: p < 0.05 (Bonferroni-corrected univariate analysis of variance for dependent samples).
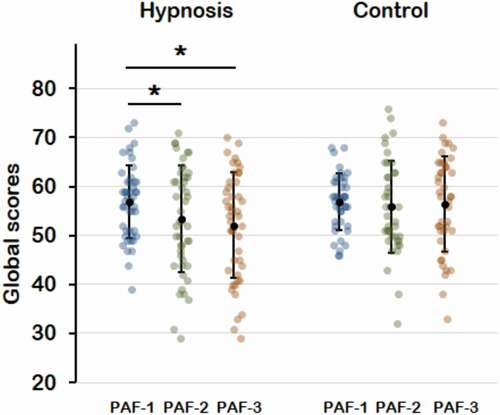
Figure 2. Mean (±SD) Subscale scores as obtained by the three different surveys with the PAF questionnaire. A: emotionality scores; B: worry score; C: interference scores; D: lack of confidence scores; PAF-1: First survey. PAF-2: second survey; PAF-3: third. Asterisk: p < 0.05 (Bonferroni-corrected univariate analysis of variance for dependent samples). Hash: p < 0.05(Bonferroni-corrected friedman test for dependent samples).
Discussion
Estimated effect of medical hypnosis
Due to the controlled design applied in the present study it seems plausible that the one-hour-intervention with medical hypnosis was the main reason for the beneficial effects on test anxiety. This is in line with previous studies demonstrating the efficacy of hypnosis in the treatment of anxiety (Valentine et al., Citation2019). While the global PAF scores remained fairly constant in the control group they showed a statistically significant decline in the hypnosis group. However, a direct intergroup comparison between the hypnosis group and the control group revealed no statistically significant differences, presumably due to the limited sample size. These findings are in line with the preliminary results published previously (Hammer et al., Citation2020).
A similar pattern was found with respect to the emotionality and lack of confidence subscales. Those scores also decreased continuously and significantly in the hypnosis group, but not in the control group. The worry subscale showed a statistically significant decrease from the first to the third assessment in the hypnosis group and from the first to the second assessment in the control group. Maybe, this partially reflects a hypnosis-independent adaptation process presumably elicited by the students’ growing experience as the course and semester progressed. Therefore, the reduction of the worry scores within the hypnosis group has to be interpreted with caution.
While the interference scores remained fairly constant in the hypnosis group, they increased gradually within the control group, but without statistical significance. This tendency had already been vaguely discernible in the preliminary findings preceding this article (Hammer et al., Citation2020). Perhaps, the hypnosis intervention applied in this study has the potential to counteract a naturally occurring deterioration of interference in students exhibiting high levels of test anxiety.
Hypnosis seemed to have had a substantial effect on lack of confidence. The scores decreased significantly from assessment to assessment in the hypnosis group but not in the control group. The differences in the mean lack of confidence scores between the hypnosis group and the control group did not reach statistical significance. Maybe a larger sample size will also prove the intergroup differences statistically significant.
Notably, the effects of hypnosis on test anxiety occurred although only one therapist-guided medical hypnosis session of one hour was carried out with every subject. Several consecutive individualised hypnosis sessions may have the potential to increase the effects on test anxiety even further. Moreover, a combination of hypnosis with other psychological interventions might augment the positive effects (Valentine et al., Citation2019). Apart from this, it has been demonstrated that the efficiency of hypnosis is heavily dependent on the hypnotist and the client and their relationship (Bryant et al., Citation2012; Laurence et al., Citation2008). This has to be taken into account, if hypnosis is to be extended to universities to help test anxious students. Because of this relationship-dependent variability, direct comparisons of hypnosis with other techniques aimed at reducing test anxiety are problematic. Nevertheless, Spies (Citation1979) reported that desensitising hypnosis was as effective in the reduction of test anxiety as relaxing training with biofeedback. However, he also emphasised that hypnosis was superior with regards to the economy of time and effort.
Further limitations
As mentioned in the methods section, the participants were advised to listen regularly (once per day, every day) to the audio-recording of their hypnosis session. However, there was no possibility to ensure the candidates’ adherence. A non-structured assessment of the students revealed that a daily application was rarely the case. Therefore, the individual exposure to hypnosis varied between participants, which represents a confounding factor.
The present study is further limited by the fact that it relies on ‘self-reports’ via questionnaires. Although the PAF represents an officially validated psychological questionnaire (Donati et al., Citation2019; Hodapp et al., Citation2011; Hoferichter et al., Citation2016; Schnell et al., Citation2013), it can only measure test anxiety through the lens of the participants’ own perception and ability to report. A correlation of reduced self-reported test anxiety with an improvement in academic performance would convincingly underscore the positive effects of hypnosis. First preliminary evaluations of the study participants’ oral exam grades showed no statistically significant effect (data not shown), which is in line with previous reports (Melnick & Russell, Citation1976). However, it is difficult to assess oral academic performance in a standardised manner if large cohorts are assessed by several examiners simultaneously. Perhaps, the introduction of standardised oral examinations may solve or mitigate this problem (Shah et al., Citation2013; Shenwai & Patil, K., Citation2013).
Further limitations arise from the control group not having received any intervention or alternative programme. This may have created expectations regarding the benefits of hypnosis (Kirsch, Citation1990) and might bear the risk of an uncontrolled placebo effect due to the attention obtained as a member of the hypnosis group. Therefore, this circumstance may have caused unwanted artificial effects. However, every alternative control intervention would have brought about confounding data distortions of its own. Therefore, a real negative control receiving no intervention was considered the second best solution since it mimics the real situation test-anxious students are confronted with.
Conclusion
The present study demonstrated that medical students can benefit markedly from medical hypnosis used as a tool to mitigate test anxiety. The findings obtained indicate a positive influence on test anxiety in general (global scores) as well as on all dimensions of test anxiety (subscales) investigated. Lack of confidence seems to be particularly rewarding target for the hypnotic intervention applied here. Testing the effect of different hypnotic approaches or relaxation techniques, particularly on the test anxiety subscales, may lead to further valuable insight and should be the subject of future research. Even though the present study has a primary focus on test anxiety, its results may, at least partially, be of relevance for the broader issue of stress management and the control of risky behaviour and experience patterns in medical students and postgraduates. Its comparatively cost-effective nature (Spies, Citation1979) makes medical hypnosis a rewarding target for further studies in this field.
Acknowledgments
The authors gratefully acknowledge the organisational assistance provided by Elke Kretzschmar, Anke Fischer-Gößwein, Andrea Eichhorn and Maike Hemmerlein.
Disclosure statement
The authors reported no conflict of interest.
Additional information
Notes on contributors
Christian M. Hammer
Christian M. Hammer is an adjunct professor of anatomy and Master of Medical Education (MME) at the Institute of Functional and Clinical Anatomy, FAU Erlangen-Nürnberg, Germany. He teaches anatomy to first and second year medical and dental students.
Michael Scholz
Michael Scholz is an associate professor of anatomy at the Institute of Functional and Clinical Anatomy, FAU Erlangen-Nürnberg, Germany. He teaches macroscopic and microscopic anatomy to first and second year medical and dental students. He also holds the degree of Master of Medical Education (MME).
Larissa Bischofsberger
Larissa Bischofsberger is a student of dental medicine at the Friedrich-Alexander University (FAU) of Erlangen-Nürnberg, Germany, and doctoral candidate at the Institute of Functional and Clinical Anatomy in Erlangen, Germany.
Alexander Hammer
Alexander Hammer is a consultant neurosurgeon in the Department of Neurosurgery of the Paracelsus Medical University Nürnberg, Germany. His scientific focus lies on the investigation of risk factors concerning outcome dynamics after aneurysmal subarachnoid hemorrhage. He has also developed a strong interest for student welfare and stress management.
Benedikt Kleinsasser
Benedikt Kleinsasser is a doctoral candidate at the Institute of Functional and Clinical Anatomy, FAU Erlangen-Nürnberg, Germany. He teaches anatomy to first and second year medical and dental students.
Friedrich Paulsen
Friedrich Paulsen is a full professor of anatomy and vice president ‘people’ at the Friedrich-Alexander University (FAU) of Erlangen-Nürnberg. He is also head of the Institute of Functional and Clinical Anatomy in Erlangen, Germany, and Editor-in-Chief of the ‘Annals of Anatomy’.
Pascal H.M. Burger
Pascal H. M. Burger is a senior physician and head of the ADHD ambulatory at the University Hospital of Psychiatry, Zurich, Switzerland. He has graduated as Master of Medical Education (MME). He is an approved hypnotherapist and teaches psychiatric/psychosomatic courses in Erlangen and Zurich.
References
- Arigoni, F., Bovier, P. A., & Sappino, A. P. (2010). Trend of burnout among Swiss doctors. Swiss Medical Weekly, 140, w13070. https://doi.org/10.4414/smw.2010.13070
- Bruce, C. T., Thomas, P. S., & Yates, D. H. Burnout and psychiatric morbidity in new medical graduates. (2005). Medical Journal of Australia, 182(11), 599. author reply 599 https://doi.org/10.5694/j.1326-5377.2005.tb06833.x
- Bryant, R. A., Hung, L., Guastella, A. J., & Mitchell, P. B. (2012). Oxytocin as a moderator of hypnotizability. Psychoneuroendocrinology, 37(1), 162–166. https://doi.org/10.1016/j.psyneuen.2011.05.010
- Burger, P. H., Tektas, O. Y., Paulsen, F., & Scholz, M. (2014). From freshmanship to the first “Staatsexamen” increase of depression and decline in sense of coherence and mental quality of life in advanced medical students. Psychotherapie, Psychosomatik, medizinische Psychologie, 64(8), 322–327. https://doi.org/10.1055/s-0034-1374593
- Busch, M. A., Maske, U. E., Ryl, L., Schlack, R., & Hapke, U. (2013). Prevalence of depressive symptoms and diagnosed depression among adults in Germany: Results of the German Health Interview and Examination Survey for Adults (DEGS1)]. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz, 56(5–6), 733–739. https://doi.org/10.1007/s00103-013-1688-3
- Chapell, M., Blanding, Z., Silverstein, M., Takahashi, M., Newman, B., Gubi, A., & McCann, N. (2005). Test anxiety and academic performance in Undergraduate and Graduate students. Journal of Educational Psychology, 97(2), 268–274. https://doi.org/10.1037/0022-0663.97.2.268
- Dahlin, M. E., & Runeson, B. (2007). Burnout and psychiatric morbidity among medical students entering clinical training: A three year prospective questionnaire and interview-based study. BMC Medical Education, 7(1), 6. https://doi.org/10.1186/1472-6920-7-6
- Donati, M., Izzo, V., Scabia, A., Boncompagni, J., & Primi, C. (2019). Measuring test anxiety with an invariant measure across genders: The case of the German test anxiety inventory. Psychological Reports, 123(4), 003329411984322. https://doi.org/10.1177/0033294119843224
- Dyrbye, L. N., Thomas, M. R., Massie, F. S., Power, D. V., Eacker, A., Harper, W., Durning, S., Moutier, C., Szydlo, D. W., Novotny, P. J., Sloan, J. A., & Shanafelt, T. D. (2008). Burnout and suicidal ideation among U.S. medical students. Annals of Internal Medicine, 149(5), 334–341. https://doi.org/10.7326/0003-4819-149-5-200809020-00008
- Dyrbye, L. N., Thomas, M. R., & Shanafelt, T. D. (2006). Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Academic Medicine, 81(4), 354–373. https://doi.org/10.1097/00001888-200604000-00009
- Dyrbye, L. N., West, C. P., Satele, D., Boone, S., Tan, L., Sloan, J., & Shanafelt, T. D. (2014). Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Academic Medicine, 89(3), 443–451. https://doi.org/10.1097/acm.0000000000000134
- Erickson, M. H. (1965). Hypnosis and examination panics. American Journal of Clinical Hypnosis, 8(4), 356–358. https://doi.org/10.1080/00029157.1965.10402446
- Farooqi, Y., Ghani, R., & Spielberger, C. (2012). Gender differences in test anxiety and academic performance of medical students. International Journal of Psychology & Behavioral Sciences, 2(2), 38–43. https://doi.org/10.5923/j.ijpbs.20120202.06
- Gerwing, T. G., Rash, J. A., Allen Gerwing, A. M., Bramble, B., & Landine, J. (2015). Perceptions and incidence of test anxiety. The Canadian Journal for the Scholarship of Teaching and Learning, 6(3). http://dx.doi.org/10.5206/cjsotl-rcacea.2015.3.3
- Hahne, R. (1999). Studium und Psychische Probleme. Sonderauswertung zur 15. Sozialerhebung des Deutschen Studentenwerks.Deutsches Studentenwerk.
- Hammer, C. M., Paulsen, F., Burger, P. H. M., & Scholz, M. (2016). Integration of the musculature in the course “functional anatomy of the locomotor system” Preparing medical students for the dissection course. Annals of Anatomy, 208, 234–240. https://doi.org/10.1016/j.aanat.2016.08.002
- Hammer, C. M., Scholz, M., Bischofsberger, L., Paulsen, F., & Burger, P. H. (2020). Feasibility of clinical Hypnosis for Test Anxiety in first Year medical Students. International Journal of Clinical and Experimental Hypnosis, 68(4), 511–520. https://doi.org/10.1080/00207144.2020.1799379
- Hebert, S. W. (1984). A simple hypnotic approach to treat test anxiety in medical students and residents. Journal of Medical Education, 59(10), 841–842. https://doi.org/10.1097/00001888-198410000-00013
- Hodapp, V. (1991). Das Prüfungsängstlichkeitsinventar TAI-G: Eine erweiterte und modifizierte Version mit vier Komponenten [The Test Anxiety Inventory TAI-G: An expanded and modified version with four components]. Zeitschrift Für Pädagogische Psychologie/German Journal of Educational Psychology, 5(2), 121–130.
- Hodapp, V. (1996). The TAI-G: A multidimensional approach for the assessment of test anxiety. In C. Schwarzer & M. Zeidner (Eds.), Stress, anxiety, and coping in academic settings (pp. 95–130). Francke.
- Hodapp, V., Rohrmann, S., & Ringeisen, T. (2011). Prüfungsangstfragebogen : PAF; Manual. Hogrefe.
- Hoferichter, F., Raufelder, D., Ringeisen, T., Rohrmann, S., & Burkowski, W. M. (2016). Assessing the multi-faceted nature of test anxiety among secondary school students: An English version of the German test anxiety questionnaire: PAF-E. The Journal of Psychology, 150(4), 450–468. https://doi.org/10.1080/00223980.2015.1087374
- Kirsch, I. (1990). Changing expectations: A key to effective psychotherapy. Thomson Brooks/Cole Publishing Co.
- Laurence, J.-R., Beaulieu-Prévost, D., & Du Chéné, T. (2008). Measuring and understanding individual differences in hypnotizability. In M. Nash & A. J. Barnier (Eds.), The Oxford handbook of hypnosis: Theory, research and practice (pp. 225–253). Oxford University Press.
- Mache, S., Vitzthum, K., Groneberg, D., & Klapp, B. F. (2012). How to stay mentally healthy during medical education. Stress coping and relaxation behaviour of female and male students. Medical Teacher, 34(10), 867. https://doi.org/10.3109/0142159x.2012.716187
- Mathur, S., & Khan, W. (2011). Impact of hypnotherapy on examination anxiety and scholastic performance among school children. Delhi Psychiatry Journal, 14(2), 337–342.
- Melnick, J., & Russell, R. W. (1976). Hypnosis versus systemic desensitization in the treatment of test anxiety. Journal of Counseling Psychology, 23(4), 291–295. https://doi.org/10.1037/0022-0167.23.4.291
- Neuderth, S., Jabs, B., & Schmidtke, A. (2009). Strategies for reducing test anxiety and optimizing exam preparation in German university students: A prevention-oriented pilot project of the University of Wurzburg. Journal of Neural Transmission (Vienna), 116(6), 785–790. https://doi.org/10.1007/s00702-008-0123-7
- Prato, C. A., & Yucha, C. B. (2013). Biofeedback-assisted relaxation training to decrease test anxiety in nursing students. Nursing Education Perspectives, 34(2), 76–81. https://doi.org/10.5480/1536-5026-34.2.76
- Rana, R., & Mahmood, N. (2010). The relationship between test anxiety and academic achievement. Bulletin of Education and Research, 32(2), 63–74.
- Sapp, M. (1991). Hypnotherapy and test anxiety: Two cognitive-behavioral constructs: The effects of hypnosis in reducing test anxiety and improving academic achievement in college students. Australian Journal of Clinical Hypnotherapy and Hypnosis, 12(1), 25–31.
- Sapp, M. (2013). Test Anxiety: Applied research, assessment, and treatment interventions (3rd, ed. ed.). University Press of America, Inc.
- Schaefer, A., Matthess, H., Pfitzer, G., & Kohle, K. (2007). [Mental health and performance of medical students with high and low test anxiety]. Psychotherapie, Psychosomatik, medizinische Psychologie, 57(7), 289–297. https://doi.org/10.1055/s-2006-951974
- Schnell, K., Tibubos, A. N., Rohrmann, S., & Hodapp, V. (2013). Test and math anxiety: A validation of the German test anxiety questionnaire. Polish Psychological Bulletin, 44(2), 193–200. https://doi.org/10.2478/ppb-2013-0022
- Scholz, M., Neumann, C., Steinmann, C., Hammer, C. M., Schroder, A., Essel, N., & Burger, P. H. (2015). Development and correlation of work-related behavior and experience patterns, burnout and quality of life in medical students from their freshmanship to the first state examination. Psychotherapie, Psychosomatik, medizinische Psychologie, 65(3–4), 93–98. https://doi.org/10.1055/s-0034-1375630
- Scholz, M., Neumann, C., Wild, K., Garreis, F., Hammer, C. M., Ropohl, A., … Burger, P. H. (2016). Teaching to Relax: Development of a Program to Potentiate Stress—Results of a Feasibility Study with Medical Undergraduate Students. Applied Psychophysiology and Biofeedback, 208(3), 275–281. https://doi.org/10.1016/j.aanat.2016.08.002
- Shah, H. K., Vaz, F., & Motghare, D. D. (2013). Structured oral examination: From subjectivity to objectivity -An experience in community medicine. Journal of Educational Research and Medical Teacher, 1(1), 26–28.
- Shenwai, M. R., & Patil, K., B. (2013). Introduction of structured oral examination as A novel assessment tool to first year medical students in pysiology. Journal of Clinical and Diagnostic Research : JCDR, 7(11), 2544–2547. https://doi.org/10.7860/JCDR/2013/7350.3606
- Spies, G. (1979). Desensitization of test anxiety: Hypnosis compared with biofeedback. American Journal of Clinical Hypnosis, 22(2), 108–111. https://doi.org/10.1080/00029157.1979.10403207
- Stanton, H. E. (1993). Using hypnotherapy to overcome examination anxiety. American Journal of Clinical Hypnosis, 35(3), 198–204. https://doi.org/10.1080/00029157.1993.10403004
- Valentine, K. E., Milling, L. S., Clark, L. J., & Moriarty, C. L. (2019). The efficacy of hypnosis as a treatment for anxiety: A meta-analysis. International Journal of Clinical and Experimental Hypnosis, 67(3), 336–363. https://doi.org/10.1080/00207144.2019.1613863
- Voltmer, E., Kotter, T., & Spahn, C. (2012). Perceived medical school stress and the development of behavior and experience patterns in German medical students. Medical Teacher, 34(10), 840–847. https://doi.org/10.3109/0142159X.2012.706339
- Warnecke, E., Quinn, S., Ogden, K., Towle, N., & Nelson, M. R. (2011). A randomised controlled trial of the effects of mindfulness practice on medical student stress levels. Medical Education, 45(4), 381–388. https://doi.org/10.1111/j.1365-2923.2010.03877.x
- Wild, K., Scholz, M., Ropohl, A., Brauer, L., Paulsen, F., & Burger, P. H. (2014). Strategies against burnout and anxiety in medical education–implementation and evaluation of a new course on relaxation techniques (Relacs) for medical students. PLoS One, 9(12), e114967. https://doi.org/10.1371/journal.pone.0114967
