ABSTRACT
Medical students preparing to undertake general practice (GP) placements need to be equipped with the unique skills required to successfully utilise and adapt to current and emerging remote consultation modalities used in primary care and integrate this into their day-to-day clinical practice. Medical educators needed to flexibly and quickly cater learning to the evolving landscape.
A three-hour teaching session was devised to be delivered to 50 students online via Microsoft Teams™ and facilitated by five general practice tutors in groups of 10, prior to students’ GP placements. In pre-assigned pairs, students undertook two role-play scenarios for the main remote modalities of telephone and video-consultations. E-consultations were explored via discussion of simulated encounters. The authentic technology pertinent to each modality was used; this included a training version of NHS Scotland’s Near Me IT platform for video-consultations, the students’ own mobile phones for telephone consultations and simulated PDFs generated using the e-consultation facility. Teaching was evaluated via a student focus group pre and post placement.
Student feedback was positive. The session prepared them for their placement and increased their confidence. They suggested this teaching be incorporated earlier in the medical school curriculum. They appreciated learning with the same IT platforms used on placement. Some students had no prior experience of remote consultations and subsequently were expected to undertake independent remote consultations almost immediately upon arrival.
Careful design of challenging scenarios mirroring common GP presentations via remote modalities can increase student preparedness and confidence prior to GP placements during the COVID-19 pandemic.
Introduction
Remote consultations or telemedicine are terms used to denote the delivery of medical education and healthcare services from one geographical location to another using technology [Citation1]. Internationally, countries like the U.S.A. [Citation2], Australia [Citation3] and the U.K. [Citation4] have utilised some form of remote consultations for years. In U.K. primary care, the main remote modalities include telephone consultations, video-consultations (VC) and more recently, e-consultations (a digital triage tool in which patients enter information online and can communicate with their general practitioner) [Citation5].
The recent COVID-19 pandemic has served to highlight the need for medical educators to flexibly and quickly cater learning to an evolving clinical landscape. Despite the growing recognition of the role of remote consultations in the delivery of healthcare; medical school teaching in this area appears to lag behind, with little evidence found on reviewing the literature that teaching has caught up with the seismic shift in practice. However, elsewhere in the world, countries like the U.S.A. [Citation6], Australia [Citation7] and France [Citation8] already include such teaching in their undergraduate curriculum(s) to differing degrees. COVID-19 has served as a catalyst for medical schools to develop remote consultation skills teaching as it remains a viable way for students to gain clinical exposure during the pandemic [Citation9].
Benefits of such teaching include the development of medical knowledge, improved ability to deliver patient care [Citation10]. It also serves to provide students with a strong foundation to engage with remote consultations as they become part of mainstream clinical care in future [Citation11]. Boyers et al. [Citation12] showed that trainees gained more from remote consultation skills teaching when taught at an undergraduate level instead of postgraduate level. Sartori et al. [Citation13] confirmed remote consultations required their own unique skill set and those unfamiliar with this medium struggled to utilise it. This is perhaps why the U.K. General Medical Council [Citation14] expects newly qualified doctors to be competent to ‘use methods of communication used by patients and colleagues, such as technology-enabled communication platforms’.
The aim of this study was to develop an innovative and authentic GP-based teaching session to introduce final year undergraduate medical students to the key clinical skills required to carry out remote consultations prior to their assistantship in GP.
Methods
A three-hour small group tutorial session was designed by LL and PC for approximately 50 final year medical students. The session was delivered during students’ core week teaching; a week of dedicated teaching received prior to undertaking a 7-week GP assistantship. The session was delivered using Microsoft Teams™ and was facilitated by five GP tutors. Tutors were prepared by providing them with a robust tutor guide and training before the session. Tutors had the opportunity to give the trainer (LL) informal feedback once the session had finished. The learning outcomes were designed to challenge students with real-life complex cases () that required a holistic approach.
Students were split into five groups of 10 prior to the session. They were advised to access pre-learning and reading resources [Citation15–20] which centred around specific communication and examination skills required to conduct remote consultations successfully and medico-legal and clinical governance processes to support clinicians in undertaking these safely. Half the group was pre-assigned to the role of ‘Student 1’ and the other half as ‘Student 2’. Students were emailed scenario information relevant to their pre-assigned role – alternating being patient/doctor in pairs.
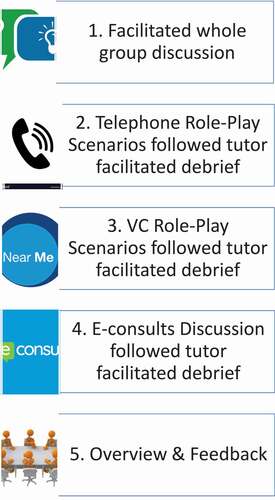
The session itself was conducted in five sections ().
1. Facilitated discussion:
Tutors facilitated a discussion amongst all 10 students based on the pre-learning material.
2. Telephone role-play scenarios:
Using their own mobile phones on audio only to eliminate visual clues, each of the five student pairs worked through two different telephone scenarios in isolation from their tutor. In one scenario, student 1 role played the clinician and student 2 role played the patient, before swapping roles for the second scenario. Tutor facilitated debriefing and discussion with the whole group of 10 students online within MS Teams then followed.
3. VC role-play scenarios:
Using a special training version of NHS Scotland’s VC platform [Citation21], each of the five student pairs role played two different scenarios (). Again, student 1 role played the General Practitioner for one scenario and the patient for the other, and vice versa for student 2. Students were set up with logon details for the VC platform in advance and advised to familiarise themselves with accessing this prior to the session. This simulates the same technology and processes students would use in clinical practice. Tutor facilitated debriefing and discussion with the whole group of 10 students online within MS Teams then followed.
4. E-consults discussion:
E-consult is an online triage platform where patients answer a series of questions that are tailored to their presenting complaint, which the General Practitioner then reviews. Whilst remaining in the same pairs for the previous role-play scenarios, students conferred on how they would approach and manage two e-consult scenarios. These involved students receiving two PDFs, one per scenario, which had been generated using the e-consult software appendix 1) for mock patients and would meet the same format and style that General Practitioners would receive. Tutor facilitated debriefing and discussion with the whole group of 10 students online within MS Teams then followed.
5. Overview and feedback:
Tutors facilitated a discussion amongst all 10 students based on their learning throughout the session, highlighting key areas and take-home points. Final opportunity was given for questions from the students before being asked for their feedback on the session. Students were informed on the ‘real-life’ outcomes of the four role-play scenarios undertaken as these were based on genuine (anonymised) clinical cases from the author (LL).
Student feedback
To evaluate students’ learning and experience from the teaching session, students who participated in the session were invited via email to participate in two focus groups. The first focus group took place after the teaching session but prior to initiation of the students’ placements. It concentrated on the teaching session itself and explored the students’ experience, what they learned and what they would change for future sessions. The second focus group session involved the same students and took place after completion of their placement. It focused on whether students felt the teaching session had adequately prepared them for carrying out remote consultations with real patients. A series of pre-set open questions was used, and open participation encouraged.
Both focus group sessions were carried out using Microsoft Teams™ to allow for social distancing by a peer facilitator (PC) who was not directly involved in the delivery of the teaching session. The sessions were recorded using the record function of Microsoft Teams™ and the audio was transcribed by a member of the educational administrative team. Students were consented before and after the recording. The transcript was then subsequently analysed by two educators (LL and VW) who were not involved in the focus groups.
Results
Informal feedback from GP tutors stated that overall the teaching session went well. Problems had been anticipated logistically as this was a novel session and run online to comply with social distancing requirements. In reality, good administrative preparation and clear communication to students and their innate ability to utilise technology [Citation22] meant that it worked well in practice. Tutors expressed some concerns at the tutor training prior to the session about why the authentic platforms were being used. They had reservations that they would be unable to directly observe students during the scenario role-plays. However, students enjoyed using the authentic platforms and tutors felt after the session that it worked well as students felt less pressure from not being directly observed. Tutors felt debriefing helped reinforce salient learning points.
Main negative feedback from tutors was that they felt there was too much content to be covered in a three-hour session. A further issue was several students experiencing problems accessing some of the IT platforms; however, this may have been a result of students’ inadequate preparation. A few students had not yet returned to the U.K. at the time of the session which could have caused issues with mobile phone charges during telephone consultation role-play; however, this was bypassed by utilising an internet-based mobile carrier, for example, Whatsapp™. Students also had the fall-back option of carrying out the consultations using Teams™ if they experienced any technical video/telephone issues.
In total, five students from four of the five different tutor groups volunteered to participate in the focus groups. Both sessions lasted approximately 50 minutes. The focus groups established students had a broad spectrum of prior experience with remote consultations: some having had extensive exposure to telephone and video from previous primary or secondary care placements or teaching, and others not having any. None had any previous exposure to e-consultations or remote consultation cases of this difficulty. Students strongly appreciated the opportunity to get acquainted with remote consultation platforms used in primary care, ‘I was quite glad I got to do this before going on GP placement next week because it familiarises you with the system and everything’. For some it was reassuring to practise something ‘I have never practised before, get rid of those first-time jitters’. This was echoed in the post-placement focus group, ‘I would say that having the tutorial beforehand made me feel more confident than I would have’. Students found that it was beneficial ‘having that first punch at it with a colleague, does take away your initial apprehension’, and that no direct supervision while doing this was not detrimental. However, they did acknowledge that the post-scenario discussion with the GP facilitator was key at identifying areas for improvement, such as appreciating how best to handle an urgent presentation remotely, admitting ‘I probably didn’t realise the severity of it’. It was noted by students that by not being able to directly see the patient in front of them, they had to be ‘more in tune’ with the clinical need so as not to overlook it.
The post-placement focus group affirmed that the majority of consultations carried out during the students’ placements were done remotely and some students were expected to take lead in these consultations early on, ‘from our second day we were having our own list of remote consultations’. The focus groups were also useful at identifying ways the teaching session could be adapted in future. Students stated that it would be helpful to have guidance on the repercussions for confidentiality when carrying out remote consultations and in particular, what to do if it is not the patient that answers the phone and what type of information can be left on an answering machine. There were other areas that they also suggested to explore, ‘a little preparation within the tutorial you know just to say sometimes there might be intimate examinations’. Students mirrored the tutor feedback that there was a lot to cover in the session, ‘it felt a little bit short or maybe like if you guys introduced another session’. Additionally, they felt that it would be beneficial if the concepts covered by the session could be introduced earlier in the curriculum and built upon in a spiralised fashion, ‘it would be really useful to have it in earlier years’. They also stated that they believed that remote consultation skills could soon be examined ‘in OSCEs from an early stage especially with COVID and stuff’.
Discussion
As the students had a varying amount of prior remote consultation experience and there was little in the way of embedded remote consultation skills teaching in the UK medical school curriculum, there was a real educational need for this session. One unique feature was the efforts made to include the same platforms that students would encounter in primary care to prepare them and make simulations more authentic. While elements of this session are only relevant locally, for example, the use of ‘Near Me’ software to deliver VC, the principles can be extrapolated and applied to any local equivalent platform, which most should already have access to. In fact, given that students responded well to using their local VC software, and how it benefited the simulation by making it more authentic, we would suggest any educators considering adapting this session for own their own purposes should strive to incorporate their own local VC software where possible.
This study was not without its limitations. In view of the immediate need for this education session due to the COVID-19 pandemic, this session was developed rapidly and, as one student fed back, is open to further adaptation. As the focus of evaluation was whether students found the teaching session useful, no focus groups were carried out with the tutors and information was collected anecdotally. It was possible that there was an element of selection bias as participants were asked to volunteer for the focus groups and the self-selecting minority that did may not necessarily reflect the student cohort. The facilitator (PC) as a fellow student knew the students. He had designed but not delivered the programme.
Important lessons emerged from developing and evaluating this teaching session. The fact that the students were immediately placed in the hot seat stressed the importance in adequately preparing them. However, in practice both students and tutors agreed that this resulted in too much content being delivered in one session. One way of overcoming this, which was suggested by the students themselves, was to introduce this teaching earlier in the curriculum and spiral it as students progressed. By doing this the skills of dealing with the lack of face contact in a variety of remote methods used, could enable the learning to be built spirally from earlier years. This will be advantageous as remote consultations will inevitably be part of the post-COVID-19 era, with different bodies advocating modernisation of consultations even before the COVID-19 pandemic [Citation23,Citation24].
Conclusion
While the future has never been more uncertain, remote consultations will undoubtedly remain in some capacity. Careful design of challenging scenarios which not only mirror common GP presentations but also integrate some of the difficulties of consulting remotely can be utilised to prepare students. This helps them develop familiarity with the technology and the necessary skills to successfully utilise them. We believe that this online methodology offers ongoing opportunities for all educators to move this into education in the post-COVID-19 era.
Supplemental Material
Download MS Word (613 KB)Acknowledgments
We would like to take this opportunity to thank all the GP tutors and medical students who were involved in this teaching.
We would also like to thank Dr Christine Kay and the University of Aberdeen for providing PC with funding in the form of the Summer Medical Education Scholarship.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplemental data
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Zanaboni P, Knarvik U, Wootton R, Adoption of routine telemedicine in Norway: the current picture. Glob Health Action. [Online]. 2014;7(1):22801. [cited 2021 March 1]. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3888886/#
- Li H, Telemedicine and Ophthalmology. Surv Ophthalmol. [Online]. 1999;44(1):61–72. [cited 2021 March 1]. Available from https://www.sciencedirect.com/science/article/pii/S0039625799000594?casa_token=lWlop9iOxzgAAAAA:JoOl8QIiozSmAOBh5-y6JhWYdL7IhBOQ0IZKVSvGM-WwxfE55Z0U7KA3b_dBcXrl6kdFmV9rpw
- Crowe B, McDonald I, Telemedicine in Australia. Recent developments. J Telemed Telecare. [Online]. 1997;3(4):188–193. [cited 2021 March 1]. Available from https://pubmed.ncbi.nlm.nih.gov/9614732/
- Audit Scotland. A review of telehealth in Scotland. 2011. [cited 2021 March 1]. Available from: https://www.audit-scotland.gov.uk/docs/health/2011/nr_111013_telehealth.pdf
- eConsult. What is eConsult [Online]. 2021. [cited 2021 March 1]. Available from: https://econsult.net/primary-care
- Jumreornvong O, Yang E, Race J, et al. Telemedicine and medical education in the age of COVID-19. Acad Med. 2020;95(12):1838–1843. [cited 2021 March 1]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7489227/
- Rienits H, Teuss G, Bonney AL. Teaching telehealth consultation skills. Clin Teach. 2015;13(2):119–123. [cited 2021 March 1]. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/tct.12378
- Yagobian S, Ohannessian R, Mathieu- Fritz A, et al. National survey of telemedicine education and training in medical schools in France. J Telemed Telecare. 2019; [cited 2021 March 1]. Available from: https://journals.sagepub.com/doi/10.1177/1357633X18820374?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub++0pubmed&
- Dedeilia A, Sotiropoulos M, Hanrahan J, et al. Medical and surgical education challenges and innovations in the COVID-19 era: a systematic review. In Vivo. 2020. [cited 2021 March 1]. Available from: http://iv.iiarjournals.org/content/34/3_suppl/1603.long
- Pathipati A, Azad T, Jethwani K. Telemedical education: training digital natives in telemedicine. J Med Internet Res. 2016;18(7):e193. [cited 2021 March 1]. Available from: https://www.jmir.org/2016/7/e193/
- Pourmand A, Ghassemi M, Sumon K, et al. Lack of telemedicine training in academic medicine: are we preparing the next generation. Telemed E-Health. 2020;27(1):62–67. [cited 2021 March 1]. Available from: https://pubmed.ncbi.nlm.nih.gov/32294025/
- Boyers L, Schultz A, Baceviciene R, et al. Teledermatology as an educational tool for teaching dermatology to residents and medical students. Telemed J E Health. 2015;21(4):312–314
- Sartori D, Olsen S, Weinshiel S, et al. Preparing trainees for telemedicine: a virtual OSCE pilot. ASME Med Educ. 2019. Available from ; 53: 517–518. [cited 2021 March 1]. https://onlinelibrary.wiley.com/doi/full/10.1111/medu.13851 5
- General Medical Council. Outcomes for graduates. 2018 [Online]. [cited 2021 March 1]. Available from: https://www.gmc-uk.org/-/media/documents/outcomes-for-graduates-a4-6_pdf-78952372.pdf
- Greenhalgh T, Koh G, Car J. Covid-19: a remote assessment in primary care. BMJ. 2020; [cited 2021 March 1]. Available from: https://www.bmj.com/content/368/bmj.m1182
- General Medical Council. Remote prescribing high level principles. 2020 [Online]. [cited 2021 March 1]. Available from: https://www.gmc-uk.org/ethical-guidance/learning-materials/remote-prescribing-high-level-principles?utm_source=media&utm_medium=media&utm_campaign=principles
- General Medical Council. Remote consultations. 2020 [Online]. [cited 2021 March 1]. Available from: https://www.gmc-uk.org/ethical-guidance/ethical-hub/remote-consultations
- Medicspot. Handbook for video consultations. 2020 [Online]. [cited 2021 March 1]. Available from: https://gpexcellencegm.org.uk/wp-content/uploads/Handbook_for_video_consultations_2nd_Edition.pdf
- NHS Scotland National Videoconferencing Service. Better Clinical Sessions. 2020 [Online]. [cited 2021 March 1]. Available from: https://www.vc.scot.nhs.uk/better-vc/better-clinical-sessions/
- Royal College of General Practitioners. Key principles for intimate assessment undertaken remotely in response to COVID-19. 2020 [Online]. [cited 2021 March 1]. Available from: https://elearning.rcgp.org.uk/pluginfile.php/154305/mod_page/content/12/Key%20principles%20for%20intimate%20clinical%20assessments_July%202020.pdf
- NHS Scotland. Attend anywhere. 2020 [Online]. [cited 2021 March 1]. Available from: https://nhs.attendanywhere.com/login
- Azer S, Algrain H, Alkhelaif R, et al. Evaluation of the educational value of Youtube videos about physical examination of the cardiovascular and respiratory systems. J Med Internet Res. 2013;15(11):e241. [cited 2021 March 1]. Available from: https://www.jmir.org/2013/11/e241/?newDesign
- Royal College of Physicians. Outpatients: The future- adding value through sustainability. 2018 [Online]. [cited 2021 March 1]. Available from: https://www.rcplondon.ac.uk/projects/outputs/outpatients-future-adding-value-through-sustainability
- Royal College of General Practitioners. Fit for the Future - A vision for general practice. 2019 [Online]. [cited 2021 March 1]. Available from: rcgp.org.uk/-/media/Files/News/2019/RCGP-fit-for-the-future-report-may-2019.ashx?la=en