Abstract
Background and Methods: This paper reviews the current capacity of personnel in enabling access to assistive technology (AT) as well as the systems and processes within which they work, and was reviewed, discussed, and refined during and following the Global Research, Innovation, and Education in Assistive Technology (GREAT) Summit.
Findings: Key concepts addressed include a person-centred team approach; sustainability indicators to monitor, measure, and respond to needs for service design and delivery; education, research, and training for competent practice, using the six rehab-workforce challenges framework; and credentialing frameworks. We propose development of a competence framework and associated education and training programs, and development and implementation of a certification framework for AT personnel.
Conclusions: There is a resolve to address the challenges faced by People globally to access assistive technology. Context specific needs assessment is required to understand the AT Personnel landscape, to shape and strengthen credentialing frameworks through competencies and certification, acknowledging both general and specific skill mix requirements.
Personnel in assistive technology (AT) provision should be trained using a person-centred team approach, which emphasizes appropriate skill-mix to address multiple needs within the community.
Sustainability indicators should be used which allow personnel to monitor, measure and respond to needs for service design and delivery.
A competence framework with associated education and training program, coupled with the development and implementation of a certification framework for AT personnel needs, will promote quality in AT personnel training globally.
Implications for Rehabilitation
Part A: assistive technology personnel context
Introduction
The United Nations “Convention on the Rights of Persons with Disabilities” (CRPD) requires governments to meet the assistive technology (AT) needs of citizens [Citation1]. To achieve this requirement, Member States need to undertake a needs assessment and progressively work towards enacting legislation, developing policies, procurement and provision systems, building work-force capacity, and promoting AT product availability and advancement, through stakeholder engagement in research, education and training.
Furthermore, Tebbutt et al. illustrate how the achievement of each of the 17 sustainable development goals (SDGs) can be facilitated using assistive products [Citation2]. They argued that “without promoting the availability of assistive products the SDGs cannot be achieved equitably [Citation2]”. Tebbutt et al. highlight how assistive products are considered both a mediator and a moderator of SDG achievement. To this end, the World Health Organization (WHO) recognizes the importance of access to assistive technologies, as evidenced by the recent adoption of Resolution EB142.R6 (improving access to AT) by the World Health Organization Executive Board, [Citation3] the World Health Assembly resolution WHA 58.23, [Citation4] and the WHO Global Disability Action Plan 2014–2021 which called for Member States to improve access to AT [Citation5].
Usage of AT is widely recognized as enabling people to carry out activities of daily living, and enjoy full citizenship through their participation in domains of life including economic, political, social, cultural, spiritual, religious and leisure [Citation6–8]. As an example, a recent systematic review with meta-analysis found AT supported adolescents and adults with learning disabilities achieve better educational outcomes, increased satisfaction with learning, and improved quality of life [Citation9].
Access to AT is challenging internationally, particularly for people in lower resourced environments, where only 5–15% of people who require AT have access to it due to multifactorial reasons including a shortage of skilled professionals [Citation10]. Even in high resource countries, people living in low income households experience significant barriers to accessing AT. Poor planning and commissioning, limited initiatives, leadership and governance in relation to AT services are associated with a lack of information and/or education and training available to persons who require or provide AT [Citation11]. A survey of experts specializing in AT found that respondent countries reported an average 29% of the capacity to implement planned services [Citation12]. It is widely acknowledged that significant workforce shortages exist in many contexts, which is a major barrier in meeting the needs of people requiring AT. In fact, countries with the highest prevalence of disability-related health conditions tend to be those with the lowest supply of health workers skilled in provision of AT (as low as two professionals per 10,000 population) [Citation13].
A multi-disciplinary workforce in a health system is often required to meet AT needs. The recent WHO publication Rehabilitation in Health Systems [Citation14] suggests that multi-disciplinary rehabilitation can be effective in managing chronic, complex or severe conditions. Based on the high level of evidence, they recommend that a multi-disciplinary workforce should be available, “as different rehabilitation disciplines require specific skills” (p.8) [Citation14]. However, multi-disciplinary workforces may be burdened by high barriers such as cost and availability of qualified personnel, or lack of integration resulting in inefficient service delivery. Planning provision and service impact requires exploration of specific contexts, gleaning an understanding of the place, people, pace and policy required to build a sustainable community of practice, utilizing sustainability indicators to monitor, measure and respond to the AT provision process [Citation15,Citation16].
This paper reviews the current capacity of human resources in enabling access to AT as well as the systems and processes within which they function, and was reviewed, discussed, and refined during and following the Global Research, Innovation, and Education in Assistive Technology (GREAT) Summit. We propose a sustainable approach as the way forward for human resources development to meet the AT needs of every citizen.
Part B: challenges in the current personnel approach for at provision
In high resourced environments, there are clearly established professions who act as AT personnel, including, but not limited to, occupational therapy, physiotherapy, speech and language therapy, and physical and rehabilitation medicine. Within each of these professions, AT provision often comprises a part, but not the whole of the profession’s focus. Additional professional groups including prosthetists/orthotists, rehabilitation engineers and AT professionals may focus directly on AT service provision. In these contexts, work within a multidisciplinary team provides opportunities for task shifting, with the appropriate mix of knowledge and skills to achieve AT related outcomes.
Often, AT personnel are trained in a single area of expertise (e.g., visual, hearing, mobility products), and focus on assessing for and providing a specific AT solution. This may contribute to having too many AT specialists and not enough general rehabilitation practitioners, particularly in higher-resourced contexts. In lower-resourced countries, nonspecific rehabilitation professions or other health workers may be responsible for the provision of AT services. It is important to identify the optimal mix of generalists and specialists to achieve identified outcomes in each context, supported by adequate training for skilled personnel, and opportunities for continuing education to allow increased specialization for cases of higher complexity.
Many people require a range of AT products and services from multiple sources to meet their specific needs. As AT is provided across multiple sectors, it becomes increasingly complex and requires collaborative multi-disciplinary approaches [Citation17,Citation18]. Where government agencies are responsible for providing AT, various services are generally planned and procured (commissioned) independently from one another, often by different departments or organizations, with limited collaboration with other sectors and agencies. Given the heterogeneity of populations, a greater understanding by those planning and commissioning services is required. The avoidance of unnecessary overlap among personnel will promote a more integrated approach. There is a need for coordination of services, as well as skill-mix among the human resources charged with the provision system.
AT services are at risk of not being truly person-centred, as individuals’ AT needs are rarely planned for or assessed coherently [Citation19,Citation20]. Current delivery models for most AT services tend to be reactive (i.e., a product or service is put in place after something happens), with relatively little focus on prevention, as it is difficult to provide evidence on whether an outcome has been prevented. It is usually the immediate (often clinical) rather than anticipatory need that is considered. For example, an individual with a complex progressive condition like multiple sclerosis may receive services which address immediate needs for mobility and fatigue management, without consideration for future AT needs for self-care, maintaining employment, and other activities of daily living. AT services often have a focus on assessment and prescription, without robust and consistent systems in place for evaluating if individual goals have been achieved throughout the process, from referral to follow-up and management [Citation21].
Often wider issues are not considered, including the environment where the product is to be used, and the role of care providers. This is complicated by little focus on innovation and continuous improvement in the provision process, as providers are often guided by detailed and prescriptive specifications, imposed by payers who have little incentive to fund cutting edge AT services and products. As a result, duplication in administration, assessment, and procurement results in disjointed provision, and increases service-related costs.
While examples of models and standards of best practice service provision processes exist, e.g., CECOPS Standards, there is a lack of role clarity regarding the personnel involved [Citation22,Citation23]. Two examples demonstrate the importance of priority products and the potential personnel involved.
(1) Visual assistive products – low vision is attributable to “…serious consequences in almost all aspects of human life: moving around, caring for oneself, social interaction, education, employment, leisure. Without vision, the world (the natural world and urban world) suddenly becomes less accessible [Citation23].” The type of priority assistive products (APL) required and skill mix of personnel involved to meet the “obstacles faced by individuals” of all ages will vary, given the graduation of visual acuity from mild visual impairment to total blindness with no light perception [Citation23,Citation24]. Individuals involved in the design, assessment and provision of visual products include a number team members, for example: persons with vision loss, ophthalmologists, orientation and mobility specialists, education and rehabilitation professionals (occupational therapists, psychologists, physical and rehabilitation medicine physicians), computer engineers [Citation23].
(2) Posture and wheeled mobility assistive products – the WHO (2008) “Guidelines on the Provision of Manual Wheelchairs in Less Resourced Settings” acknowledges the importance of providing an appropriate wheelchair as a basic human right, describing an eight step process for service delivery [Citation25]. Wheelchair and seating AT (WSAT) is a primary need, described as “An enabler both extrinsically and intrinsically for people …posture and mobility impairments…to actively participate across their life span in everyday living. The type and complexity of the WSAT provided will depend on the limitations and restrictions caused to individuals” …to personally participate within their desired environment and context [Citation26]. The guidelines include the stakeholders directly involved in the service delivery process [Citation27] for example users, families and carer providers, government authorities, health and rehabilitation services, supporting organizations rehabilitation personnel, wheelchair service personnel [Citation25]. These guidelines have been utilized in research to assess the delivery process within context [Citation28]. Inconsistencies exist in low and lower middle-income countries, for example, with disparities found regarding education and training of personnel involved, with no clear indicators regarding who is responsible for oversight of the provision system [Citation29].
People using AT services should be empowered with the right knowledge, information and safeguards in place, to make informed decisions, with more choice and control to manage their health care, and wellbeing with respect to their AT needs.
It is the shared responsibility of personnel to work in collaboration with people using AT services to improve coordination and communication, remove organizational barriers, and achieve best outcomes. AT systems should be developed with focus on prevention, ensuring the use of evidence-based policies and strategies, to strengthen systems, promote sustainability, and meet the diversity of needs in a timely and appropriate manner.
A skill-mix approach rather than specific staff type within a health workforce can facilitate the delivery of person-centred health care services [Citation13,Citation30–32]. A personnel solution which addresses basic skills for AT provision for all service providers, with specialization for cases of increased complexity, may have the potential to mainstream AT provision in wider health and social care services, reaching a larger part of the population. Formal and non-formal education pathways represent an opportunity to develop capacity among those who are not normally engaged in rehabilitation and AT provision (i.e., physicians, physician’s assistants, nurses, nurse practitioners, AT users, caregivers). In addition, there are opportunities to support, develop and establish local educational programs that are both contextually relevant and culturally sensitive, diversifying the workforce required for successful implementation of AT systems [Citation33].
Part C: context-aware personnel development and training using a skill mix and task-shifting approach
Developing sustainable processes and service delivery models is complex and challenging, given the diversity of people, products and personnel involved globally [Citation2,Citation34]. Appropriate infrastructures are required when planning, providing and evaluating AT service [Citation21]. Focusing specifically on skills necessary to develop sustainable infrastructures requires consideration of country specific dimensions, and the already available professional resources. There is a need to build personnel capacity for individuals and/or teams to provide appropriate AT, with multiple professions involved as prescribers, producers, payers and policy makers [Citation35]. In addition, personnel responsible for oversight, procurement, commissioning, provision and evaluation of AT services, require adequate education and training to enable appropriate AT systems to be realized [Citation36]. It is also important to highlight the need for the community and other related professionals to have a basic understanding of the importance of AT for improving lives, as a non-collaborative environment may reduce the effectiveness of any specific intervention [Citation37]. This capacity building and professional development should foster a lifelong learning perspective to accommodate the rapid pace of change in both technology and society at large [Citation38].
A primary challenge to address, when considering specific personnel needs, is the understanding and use of the term “assistive technology”. For example, in areas of rehabilitation, education, research or policy development the type of AT can vary depending on the context, and assistive product required.
Definitions of AT, assistive products (AP) and priority assistive products (APL) presented by the WHO [Citation39] are in Appendix A. AT products may replace body function and structures or optimize functioning by restoring, augmenting and compensating body function or body structure impairments [Citation40]. Drawing from a number of sources [Citation23,Citation24,Citation41], it is also possible to categorize the WHO APL [Citation39], into four groupings: daily living, communication, sensory, personal mobility and further divide into sub-groupings which may assist with planning for services and personnel required (see sample classification in Appendix B). Using this approach may allow the development of specific competencies and areas of practice, for example around posture and wheeled mobility or daily living products.
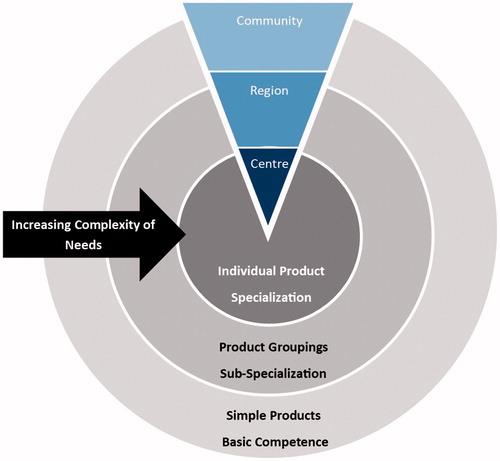
The development of a core set of baseline competencies in each of the priority assistive products, followed by specialization and advanced training in product groupings may help to address the needs of people with increasing complexity, and provide avenues for continuing education of personnel, and the application of best practice provision evidence. A systematic approach to personnel education and training (), which acknowledges the need for basic competence across a range of devices at the community level, followed by specialization of personnel in product groupings, will contribute to a provision system which can be modified and adapted to local contexts. This will ensure meeting the greatest need for basic devices within communities, while allowing individuals with higher levels of need to be seen by personnel with additional specialized education and training. Using this model, all practitioners are responsible for generalist practice, while specialist services are located centrally within the broader context.
A new skillset is also required across planning, procuring and service delivery systems. This skillset must address the challenge of interoperability, where some priority assistive products are compatible and can be integrated; for example, when a person requires the use of apps, communication devices, environmental controls and a wheelchair. Furthermore, it is important to recognize that while the APL represents a range of AT prioritized for global provision, service providers should be prepared to address AT outside the confines of such a list.
The development of appropriate skill mix across a range of potential providers may help to alleviate the lack of service integration and oversight, overcome challenges of overloaded personnel, and avoid rigid systems which cannot meet individual and context specific needs. In each context, a thorough needs assessment, with robust epidemiological data, will allow the development of the appropriate mix of skills and professionals to advance AT practice and provision processes. Furthermore, gathering information regarding the complex and varied needs of people who use AT, will allow for continuous learning systems, aimed to improve accountability, efficiency and quality [Citation42,Citation43]. Understanding an individual’s personal requirements is an important factor for determining needs, and respective resource use across a range of assistive products [Citation43].
To achieve appropriate skill mix requires the development of new staffing models where certain tasks are “shifted” from those with specialist training to those with generalist training [Citation44]. Task shifting aims to increase the workforce to enhance services, while lowering costs. By reducing the amount of education required, it can be considered an effective approach to overcome the issue of shortage and unbalanced skill-mix among health professions [Citation30,Citation44]. Evidence on task shifting in a variety of domains shows this approach may be more cost effective and offer higher quality care than a physician-centred model [Citation45], and can effectively deliver a number of specific interventions. These include preventive interventions for maternal and child health, stroke recovery tasks, and management of chronic conditions such as asthma, hypertension, diabetes, epilepsy, anxiety and depression [Citation46–49]. Rehabilitation assistants, have gained recognition recently in higher resourced settings, demonstrating the potential to alleviate burden within the rehabilitation system, and serve as a good example of how tasks may be shifted to those with shorter or more generalist training [Citation50].
Community-based rehabilitation (CBR) was introduced by the WHO as a strategy to increase access to rehabilitation and was strengthened by the publication of the guidelines for CBR [Citation10]. The guidelines strongly encourage the training of alternative cadres through curricula which targets specific contextual needs [Citation44]. Assistive technologies are acknowledged within the CBR guidelines as an essential component. Specifically, the guidelines suggest community health workers should be knowledgeable about the function and application of assistive devices, including basic fabrication and maintenance, while being aware of community resources, including potential funding [Citation10]. Furthermore, the guidelines state that people who require access to rehabilitation and their families should be included in this learning process [Citation10]. Community health workers have long since been considered the key to address the lack of rehabilitation facilities in underserved areas. CBR personnel may represent an opportunity to address the AT needs of citizens given the widespread presence of CBR programs around the globe [Citation10,Citation51]. In CBR, the extent of the human resources that are needed for adequate health care necessitates new thinking about what sort of personnel and training is most likely to be effective. A systematic review of CBR staff concluded “research is needed on the training, performance and impacts of rehabilitation workers, including their capability of working across sectors and engaging with and making use of health systems research [Citation52]”. A comprehensive job and skills analysis is needed in order to retain clinical effectiveness and patient’s safety [Citation52].
The context often has a determining influence on the outcomes of interventions [Citation53]. In some instances, people may be discouraged from accessing health services due to the prejudicial attitudes they experience from health professionals [Citation54,Citation55]. Alternative personnel may be considered more acceptable at the community level. In one study, community health workers delivering maternal and child health interventions were appreciated for their kindness, availability, accessibility, non-dogmatic approaches and respect [Citation56]. A range of AT personnel with appropriate skillsets who work in community settings can play a role in overcoming such barriers. In order to be effective, task shifting procedures should be framed within health policies and receive recognition by the country’s health system [Citation30]. Moreover, alternative cadres’ role should be clearly described, as well as the tasks they are expected to undertake.
Key considerations
Several key principles are considered here when developing a sustainable strategy for AT provision, which must be understood and put into force by all personnel engaged in the entire AT provision process.
Person-centred team approach
Assistive technology provision requires a team approach with individual people requiring AT at the centre of the process when making decisions regarding assessment, procurement and overall service delivery. This person-centred team approach is critical at all stages of the AT process, beginning with the design of AT to meet the user’s actual needs. It is expected that personnel working across all areas of AT provision will have sufficient knowledge, skills, abilities and attitudes necessary for person-centred design, procurement, delivery, and evaluation of AT products and services, regardless of their level of specialization or generalist backgrounds [Citation57].
Person-centred AT provision hinges on the provision of client-centred service provision, working together in the development of priority assistive products and systems for provision. Six key concepts are considered in client-centred care: individual autonomy, partnership, provider and client responsibility, enablement, contextual understanding, accessibility and respect for diversity [Citation58]. These key concepts must be understood and applied by all personnel involved in provision of AT, maintaining the person and their needs/goals at the centre of the process. A review of models and instruments used in the selection and provision of AT found that, despite a lack of evidence-based procedures for AT provision, most of the available models and instruments client-centred [Citation59].
The principles of user-centred design also suggest a need for user involvement early in the design of both technologies and systems [Citation60]. People using AT are typically aware of their own needs, including environmental limitations, and may participate in co-creation to ensure more beneficial design [Citation61]. The inclusion of AT use experience and ideas in the development and evaluation of medical and assistive technologies can improve design interface, function, and quality of devices [Citation62,Citation63]. Furthermore, this increases the likelihood the end product will be suitable for use by the person within the context, thereby increasing the likelihood of adoption [Citation61].
Sustainability indicators to monitor, measure and respond to needs for service design and delivery
A lack of guiding principles regarding structures and processes relating to organizational responsibilities makes it difficult to both evaluate and improve the overall quality of services provided. The absence of clear guiding principles also leads to ambiguity around roles and responsibilities, causing a lack of clarity around service expectation for the individuals’ using services and those providing services, and confusion among government and private insurance payers.
Having sustainability indicator based quality frameworks (e.g., CECOPS) which include methods of monitoring, measuring outcomes and standards for procurement and provision of services, would provide a common baseline, and a benchmark against which organizations could respond for continuous improvement [Citation16,Citation64]. This in turn could be evaluated by others such as government and private insurance payers, not only based on outcomes but also efficiency of service provision processes. Education and training on any such sustainability indicators would then give individuals, organizations and sectors a clearer understanding of roles, responsibilities and required outcomes for sustainable development.
Education, research, and training for competent practice
To address a person-centred skill mix team approach, allowing for sustainability safeguards in design and service delivery of priority assistive products, education, research and training for competent practice is essential. Adapting the six rehab-workforce challenges [Citation65] provides a structure to identify the central elements required to conduct research, develop competency and practice criteria required for AT personnel (see ).
Table 1. The six rehab-workforce challenges [Citation58] framework.
Local institutions of higher education and training (IHET) are ideally situated to equip current and emerging AT personnel to meet the six rehab-workforce challenges and assist with realizing the CRPD and SDGs in relation to AT personnel. Universities or IHET are primarily responsible for the generation and translation of knowledge and can potentially contribute in four areas namely: (1) conducting research, (2) revision of curricula, (3) equipping current AT personnel and (4) developing accredited training modules for non-profession AT personnel.
Conduct research (addressing challenges 1, 3 and 6): The first workforce challenge “To establish personnel requirements to account for the need and demand of assistive technology” can be addressed by research conducted by faculty and post-graduate students in the different fields of rehabilitation studies. This may focus on generating an overall understanding of the roles of the specific personnel involved in AT assessment and provision, including the potential role of the person requiring AT in the provision process. Furthermore, the impact of training different cadres of AT personnel can be evaluated, while maintaining a focus on local initiatives, or internationally developed solutions which may be adapted to local contexts.
Revision of current education and training curriculum for emerging health professionals (addressing challenges 2, 3, 4 and 5): Inter-professional education (IPE) has become an integral component of most health-professionals’ training. A module or component on AT should be included in the IPE content for all rehabilitation professionals. For example, all rehabilitation professionals should be educated and evaluated in providing training to people requiring AT as well as community volunteers, through methodologies including case studies which highlight the complexity of AT provision. The importance of an interdisciplinary and multidisciplinary approach to AT assessment and practice in resource poor and rural settings should be highlighted in education programs.
Engage with and equip current health professionals working with AT (addressing challenges 3, 4 and 5): Most IHET who educate health professionals work in close contact with local clinicians. If the need is identified, post-graduate education and training workshops for clinicians who work with AT can be conducted with additional resources provided for train the trainer programs provided. This can potentially enhance the required skill mix for effective and appropriate AT provision.
Develop formally recognized/accredited education and training modules/courses for nonprofessional cadres of AT personnel (addressing challenges 1–5): Local IHET can develop formally recognized or accredited education and training modules and courses for non-formal AT personnel, with a clearly defined scope of practice. If the education and training is formally recognized and/or accredited, it is more likely that staff will be retained for a longer period. It will also enable task shifting to reduce personnel workload in areas with severe staff shortages.
Develop contextually relevant credentialing frameworks for professional cadres of AT personnel (addressing challenges 2, 5 and 6): Credentialing frameworks. Credentialing frameworks may address each of three levels: individual personnel, personnel education and training, and service delivery, including planning and commissioning.
At the individual personnel level, AT competency or outcome-based frameworks define the knowledge, skills, attitudes and professional competencies required for different levels of service and levels of responsibility within the AT provision process. Competency based frameworks identify specific skillsets required for the performance of AT personnel, including necessary outcomes to be achieved to demonstrate competency. Outcomes-based frameworks offer flexibility in terms of how something can be achieved, and have a broad application across different settings and environments. They are less prescriptive in terms of absolute requirements, and the specific skills needed, allowing the individual or group to be innovative. Outcomes-based frameworks are safeguarded by being incorporated into wider and comprehensive, auditable quality indicators. The Rehabilitation Engineering and Assistive Technology Society of North America (RESNA; www.resna.org) and International Association of Accessibility Professionals (IAAP; www.accessibilityassociation.org), and CECOPS (www.cecops.org.uk) have developed examples of competency based and outcome-based credentialing frameworks respectively, which may be linked to national qualification systems [Citation66]. Additional frameworks could be developed for specific areas of technology [Citation67]. These frameworks would be coupled with education and training programs to address the specific needs of new and existing AT personnel.
To address the needs for personnel knowledge and training, and to mainstream AT learning in existing education and training systems, similar certification frameworks could be developed to accredit or recognize educational programs for AT personnel. The Council on the Accreditation of Allied Health Education Programs (CAAHEP) recently approved an accreditation standard for AT education programs which addresses the skill mix of instructors, training approaches, and training content to address specific needs of individual personnel [Citation66]. While this specifically addresses AT personnel needs in a high-resourced context, these standards may provide a framework for developing similar accreditation standards which are flexible and allow for context-dependent training programs to take shape. Accreditation or recognition for education programs ensures a standard is met in the knowledge and skill of personnel, which can be monitored and evaluated over time. Furthermore, education standards define outcomes associated with specific competencies, or skillsets which are deemed to be critical to role performance and continual professional education for trained personnel.
In addition, credentialing for service delivery processes must be considered, as individual personnel must work within a service delivery context. These protocols should cover the planning, commissioning, service delivery and clinical and technical aspects of services. For example, CECOPS provides support tools to enable organizations to monitor their compliance with the outcomes and drive continuous improvement. CECOPS also provide training to all groups involved in AT with content driven by the outcome-based framework.
Part D: Way forward
This position paper was reviewed, discussed and refined during and following the GREAT Summit. During this discussion, two specific areas of action emerged as a way forward when addressing personnel needs for AT provision.
Development of a competence framework and associated education and training programs
There is an identified need to establish a set of process and skill-based competencies for AT provision personnel, assuring individual needs are met in specific contexts. It is important to approach the overall provision process from a sustainability perspective, including service planning and commissioning, as well as oversight for services, not simply on building competence with specific technologies.
A focus on building competence in the provision process, from access to services and assessment, to follow up and management, will allow the workforce to continue advancing skills to keep up with the pace of ever changing society and technology.
The development of a matrix of competencies/skills related to various groupings of AT products, at varying degrees of depth would facilitate development of education and training programs which can be locally tailored and include existing programs and professional roles. A scalable competency matrix, with levels of skill proficiency, will best meet the needs of both high and low-resourced countries, in planning and executing education and training programs and certification. This could be developed through the use and evaluation of best practice case studies which address the skill mix required, to meet a range of individual needs, to allow health systems to apply best practice findings in a contextually relevant way.
Where overlaps exist between groupings of AT products, competencies should include skills in referral and collaboration, or use of skill mix in the local context. This set of core AT provision competencies will need to include those competencies required by both clinical and technical staff, as well as any other individuals responsible for planning and executing AT services or related processes, including service oversight and continuous evaluation.
Contributors to this position paper call on the WHO to establish a working group to develop a competency framework which is internationally relevant, yet can be adapted to context-specific needs.
Development and implementation of a certification framework
Although education and training may lead to individual certification, this is a second priority as compared to development of competency-based training programs to address skill mix necessary for AT provision. As countries or regional groups look to develop certification for AT provision, they may look to established schemes which are in place in other jurisdictions.
Furthermore, certification may apply to individuals, provision systems or training programs. With the understanding that certification is necessarily linked to infrastructure in each context, these may serve as a source of inspiration, rather than seen as roadmaps to specific outcomes for each country. The WHO has an opportunity to define a basic level certification threshold which addresses specific and contextual needs for certification, based on those which already exist [Citation25,Citation68], and recognizes the unique and dynamic nature of populations and national contexts. Contributors to this position paper call on the WHO to establish a Certification Working Group to continue this discussion beyond the scope of the GREAT summit.
There is a resolve to address the challenges faced by people globally to access AT. Context specific needs assessment is required to understand the AT personnel landscape, to shape and strengthen credentialing frameworks through competencies and certification, acknowledging both general and specific skill mix requirements. These actions to address and support personnel capacity building, taken in concert with others across the five GATE areas of focus on people, provision, policy and products, will contribute to increased access to appropriate assistive products and services globally, and ensure the realization of rights for all people who require assistive technologies.
Appendix_B08052018.docx
Download MS Word (14.4 KB)Appendix_A.docx
Download MS Word (14.1 KB)Table_1.docx
Download MS Word (28.2 KB)Acknowledgements
We are very grateful to the many participants in the GREAT summit who provided stimulating discussion points, some of which have been included in this paper.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- UN General Assembly. Convention on the rights of persons with disabilities. Treaty Ser. [Internet]. A/RES/61/1:3. Available from: http://www.refworld.org/docid/45f973632.html
- Tebbutt E, Brodmann R, Borg J, et al. Assistive products and the sustainable development goals (SDGs). Global Health. 2016;12:79.
- World Health Organization Executive Board. Resolution EB142.R6 improving access to assistive technology. Geneva, Switzerland: World Health Organization; 2018.
- World Health Assembly. World Health Assembly Resolution WHO 58.23 on disability, including prevention, management and rehabilitation. Geneva: World Health Organization; 2005.
- World Health Organization. Global disability action plan 2014–2021. Geneva: World Health Organization; 2015.
- Lansley PR, McCreadie C, Tinker A. Can adapting the homes of older people and providing assistive technology pay its way? Age Age. 2004;33:571–576.
- Cho HY, MacLachlan M, Clarke M, et al. Accessible home environments for people with functional limitations: a systematic review. Int J Environ Res Public Health. 2016;13:826.
- Garçon L, Khasnabis C, Walker L, et al. Medical and assistive health technology: meeting the needs of aging populations. Gerontologist. 2016;56:S293–S302.
- Perelmutter B, McGregor KK, Gordon KR. Assistive technology interventions for adolescents and adults with learning disabilities: an evidence-based systematic review and meta-analysis. Comput Educ. 2017;114:139–163.
- World Health Organization. Community-based rehabilitation guidelines. Geneva: World Health Organization; 2010.
- Visagie S, Eide AH, Mannan H, et al. A description of assistive technology sources, services and outcomes of use in a number of African settings. Disabil Rehabil Assist Technol. 2016;12:1–8.
- Gould M, Leblois A, Cesa Bianchi F, et al. Convention on the rights of persons with disabilities, assistive technology and information and communication technology requirements: where do we stand on implementation? Disabil Rehabil Assist Technol. 2015;10:295–300.
- Gupta N, Castillo-Laborde C, Landry MD. Health-related rehabilitation services: assessing the global supply of and need for human resources. BMC Health Serv Res. 2011;11:276.
- World Health Organization. Rehabilitation in health systems. Geneva: World Health Organization; 2017.
- Gowran RJ, Kennan A, Marshall S, et al. Adopting a sustainable community of practice model when developing a service to support patients with epidermolysis bullosa (EB): a stakeholder-centered approach. Patient. 2014;8:51–63.
- Gowran RJ, McKay EA, O’Regan B. Sustainable solutions for wheelchair and seating. Assistive technology provision: presenting a cosmopolitan narrative with rich pictures. Technol Disabil. 2014;26(2–3):137–152.
- Muller D. Foreword: global perspectives and emerging themes in assistive technology assessment. In: Federici S, Scherer MJ, editors. Assistive technology assessment handbook. Boca Raton (FL): CRC Press; 2012. p. ix–xii.
- Andrich R, Mathiassen NE, Hoogerwerf EJ, et al. Service delivery systems for assistive technology in Europe: an AAATE/EASTIN position paper. Technol Disabil. 2013;25(3):127–146.
- Bauer S, Elsaesser L-J, Scherer M, et al. Promoting a standard for assistive technology service delivery. Technol Disabil. 2008;20(3):39–48.
- Federici S, Scherer MJ, Borsci S. An ideal model of an assistive technology assessment and delivery process. Technol Disabil. 2014;26(1):27–38.
- Federici S, Scherer MJ. Assistive technology assessment handbook. Rehabilitation science in practice series; 2012. p. xxii, 446 pp.
- Eggers SL, Myaskovsky L, Burkitt KH, et al. A preliminary model of wheelchair service delivery. Arch Phys Med Rehabil. 2009;90:1030–1038.
- Manduchi R, Krniawan S. Assistive technology for blindness & low vision. USA: CRC Press; 2013.
- Cook AM, Polgar JM. Cook and Hussey’s Assistive Technologies: Principles and Practice technologies: principles and practice. New York: Elsevier Health Sciences; 2015. 592 pp.
- World Health O. Guidelines on the provision of manual wheelchairs in less resourced-settings. Geneva: Switzerland; 2008.
- Gowran RJ. Building a sustainable wheelchair and seating provision community – meeting people’s primary needs now and in the future. Limerick: University of Limerick; 2012.
- Rousseau-Harrison K, Rochette A, Routhier F, et al. Perceived impacts of a first wheelchair on social participation. Disabil Rehabil Assist Technol. 2012;7:37.
- Toro ML, Eke C, Pearlman J. The impact of the World Health Organization 8-steps in wheelchair service provision in wheelchair users in a less resourced setting: a cohort study in Indonesia. BMC Health Serv Res. 2015;16:26.
- McSweeney E, Gowran RJ. Wheelchair service provision education and training in low and lower middle income countries: a scoping review. Disabil Rehabil Assist Technol. 2017. Epub ahead.
- Fulton BD, Scheffler RM, Sparkes SP, et al. Health workforce skill mix and task shifting in low income countries: a review of recent evidence. Hum Resour Health. 2011;9.
- Zurn P, Dal Poz MR, Stilwell B, et al. Imbalance in the health workforce. Hum Resour Health. 2002;2:13.
- MacLachlan M, Mannan H, McAuliffe E. Staff skills not staff types for community-based rehabilitation. Lancet. 2011;277:1988–1989.
- Jans LH, Scherer MJ. Assistive technology training: diverse audiences and multidisciplinary content. Disabil Rehabil Assist Technol. 2006;1:69–77.
- Kuo DZ, Houtrow AJ. Recognition and management of medical complexity. Pediatrics. 2016;138:e1–13.
- Batavia M, Batavia AI., Friedman R. Changing chairs: anticipating problems in prescribing wheelchairs. Disabil Rehabil. 2001;23:539–548.
- Marasinghe KM, Lapitan JM, Ross A. Assistive technologies for ageing populations in six low-income and middle-income countries: a systematic review. BMJ Innov. 2015;1:182–195.
- Churchill J, Hoogerwerf E-J. Promoting Assistive Technology Competence among Care Staff in Europe. Assistive Technology: From Research to Practice – Proceedings of AAATE; 2013. p. 458–463.
- Hoogerwerf E-J, Gresswell A. Guidelines for lifelong learning in AT. In: Eizmendi G, Azkoitia J, Craddock G, editors. Challenges for assistive technology. Amsterdam: IOS Press; 2007. p. 623–627.
- Health W. Priority assistive products list: improving access to assistive technology for everyone, everywhere. Geneva: World Health Organization; 2016.
- Bauer SM, Elsaesser L-J, Arthanat S. Assistive technology device classification based upon the World Health Organization’s, International Classification of Functioning, Disability and Health (ICF). Disabil Rehabil Assist Technol. 2011;6:243–259.
- Eide A, Oderud T. Assistive technology in low-income countries. In: Maclachlan M, Schwarts L, editors. Disability and international development: towards inclusive global health. New York (NY): Springer Publishing Company; 2009. p. 149–160.
- Busse R, Geissler A, Aaviksoo A, et al. Diagnosis related groups in Europe: moving towards transparency, efficiency, and quality in hospitals? BMJ. 2013;346:f3179.
- Hopfe M, Stucki G, Marshall R, et al. Capturing patients’ needs in casemix: a systematic literature review on the value of adding functioning information in reimbursement systems. BMC Health Serv Res. 2015;16:40.
- Mannan H, Boostrom C, Maclachlan M, et al. A systematic review of the effectiveness of alternative cadres in community based rehabilitation. Hum Resour Health. 2012;10:20.
- Callaghan M, Ford N, Schneider H. A systematic review of task-shifting for HIV treatment and care in Africa. Hum Resour Health. 2010;8:8.
- Gilmore B, McAuliffe E. Effectiveness of community health workers delivering preventive interventions for maternal and child health in low- and middle-income countries: a systematic review. BMC Public Health. 2013;13:847.
- Akinyemi RO, Owolabi MO, Adebayo PB, et al. Task-shifting training improves stroke knowledge among Nigerian non-neurologist health workers. J Neurol Sci. 2015;359:112–116.
- Joshi R, Alim M, Kengne AP, et al. Task shifting for non-communicable disease management in low and middle income countries – a systematic review. PLoS One. 2014;9:e103754.
- van Ginneken N, Tharyan P, Lewin S, et al. Non-specialist health worker interventions for mental health care in low- and middle-income countries. Cochrane Database Syst Rev. 2013;11:CD009149.
- Lizarondo L, Kumar S, Hyde L, et al. Allied health assistants and what they do: a systematic review of the literature. J Multidisc Healthc. 2010;3:143–153.
- Adya M, Samant D, Scherer MJ, et al. Assistive/rehabilitation technology, disability, and service delivery models. Cogn Process. 2012;13:1.
- Mannan H, Maclachlan M, McAuliffe E. The human resources challenge to community based rehabilitation: the need for a scientific, systematic and coordinated global response. DCID. 2012;23:6–16.
- Gilmore B, MacLachlan M, McVeigh J, et al. A realist synthesis of rehabilitation human resources in resource-poor areas. Hum Resour Heal. 17AD; in press.
- Munthali A, Mannan H, Maclachlan M, et al. Non-use of formal health services in Malawi: perceptions from non-users. Malawi Med J. 2015;26(4):126–132.
- Eide A, Mannan H, Khogali M, et al. Perceived barriers for accessing health services among individuals with disability in four African countries. PLoS One. 2015;10:e0125915.
- Glenton C, Colvin CJ, Carlsen B, et al. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis. Cochrane Database Syst Rev. 2013;10:CD010414.
- Scherer M, Jutai J, Fuhrer M, et al. A framework for modelling the selection of assistive technology devices (ATDs). Disabil Rehabil Assist Technol. 2007;2:1–8.
- Law M, Baptiste S, Mills J. Client-centred practice: what does it mean and does it make a difference? Can J Occup Ther. 1995;62:250–257.
- Scherer MJ, Craddock G. Matching person & technology (MPT) assessment process. Technol Disabil. 2002;14:125–31.
- Gulliksen J, Göransson B, Boivie I, et al. Key principles for user-centred systems design. Behav Inf Technol. 2003;22:397–409.
- Olsson E. What active users and designers contribute in the design process. Interact Comput. 2004;16:377–401.
- Shah SGS, Robinson I. User involvement in healthcare technology development and assessment: structured literature review. Int J Health Care Qual Assur. 2006;19:500–515.
- Kübler A, Holz EM, Riccio A, et al. The user-centered design as novel perspective for evaluating the usability of BCI-controlled applications. PLoS One. 2014;9:e112392.
- Bell S, Morse S. Experiences with sustainability indicators and stakeholder participation: a case study relating to a “Blue Plan” project in Malta. Sust Dev. 2004;12:1–14.
- Jesus TS, Landry MD, Dussault G, et al. Human resources for health (and rehabilitation): six rehab-workforce challenges for the century. Hum Resour Health. 2017;15:8.
- Committee on Accreditation Rehabilitation Engineering and Assistive Technology Education (RESNA-CAAHEP). Standards and guidelines for the accreditation of educational programs in assistive technology [Internet]; 2016. Available from: http://www.caahep.org/CAAHEP/media/CAAHEP-Documents/AssistiveTechnologyStandards.pdf
- Gresswell A, Hoogerwerf EJ, editors. Guidelines for lifelong learning in assistive technology. Bologna, Italy: KPT Consortium; 2007.
- World Health O. Guidelines for training personnel in developing countries for prosthetics and orthotics services. Geneva: World Health Organization; 2005.
Appendix A. Glossary of key terms
Assistive technology (AT) is the application of organized knowledge and skills related to assistive products, including systems and services. Assistive technology is a subset of health technology.
Assistive products (AP): Any external product (including devices, equipment, instruments or software), especially produced or generally available, the primary purpose of which is to maintain or improve an individual’s functioning and independence, and thereby promote their well-being. Assistive products are also used to prevent impairments and secondary health conditions.
Priority assistive products (APL): Those products that are highly needed, an absolute necessity to maintain or improve an individual’s functioning and which need to be available at a price the community/state can afford.