ABSTACT
Purpose
This report presents two cases of successful telerehabilitation delivery for patients quarantined due to COVID-19. One of the patients did not speak the therapists’ language, whereas the other presented complete deafness.
Materials and Methods
We assembled a telerehabilitation system using commercial applications, including a remote-control application that minimizes the need for patient’s input. The telerehabilitation comprised a combination of video calls with a physical therapist and a 20-minute exercise video. The first case was of a 72-year-old man who could only speak Cantonese, a language that none of the service providers could speak, making communication difficult. Therefore, telerehabilitation was provided using Google Translate to simultaneously translate the therapist’s instructions in Japanese to Cantonese. The second case involved a 49-year-old man with neurofibromatosis and complete deafness. In this case, communication during the exercise programme was achieved using 25 cue cards that were prepared in advance and used to convey instructions. The patients’ satisfaction was assessed using either of a simple three-item questionnaire (Case 1) or the Telemedicine Satisfaction Questionnaire with five additional items (Case 2).
Results
In both cases, the exercise programme was successfully conducted, and the patients reported being highly satisfied with the programme.
Conclusions
Communication barriers can impede telerehabilitation therapy; this problem is aggravated when the recipients cannot receive on-site education for device operation and exercise performance in advance due to COVID-19 restrictions. However, the use of supplementary methodologies may contribute to solving these issues, further expanding the coverage and applicability of telerehabilitation.
We provided telerehabilitation for two patients with communication difficulties who were quarantined due to COVID-19.
Telerehabilitation was carried out using a system with a remote-control mechanism to minimise patient input and avoid problems caused by their unfamiliarity in operating the devices.
In addition, an online translation mechanism was used to overcome language differences, while cue cards were used for a patient with a hearing impairment.
Telerehabilitation was performed without any technical issues. Both patients reported being highly satisfied with the intervention.
This experience of providing telerehabilitation and overcoming communication difficulties may help develop a strategy to expand the coverage of telerehabilitation in the treatment of patients in isolation due to highly transmissible diseases, such as COVID-19.
IMPLICATIONS FOR REHABILITATION
Introduction
Since its discovery in China in late 2019, the coronavirus disease 2019 (COVID-19), caused by a new coronavirus (SARS-CoV-2), has become a global pandemic [Citation1]. Due to the strong infectivity of COVID-19, strict social distancing measures have been put into effect, especially for individuals who have become infected with the virus, the elderly, and disabled individuals at high risk of developing severe pneumonia. However, concerns have been raised regarding the negative impact of these measures on people’s activity levels and mental and physical health, particularly among the elderly [Citation2].
Under these circumstances, the importance and method of rehabilitation (not only during the acute phase of COVID-19 but also in chronic care) are being reviewed in real time [Citation3,Citation4]. However, rehabilitation delivery often involves being in close proximity with patients over prolonged periods, which increases the risk of infection among the rehabilitation staff [Citation5,Citation6].
To address this issue, telerehabilitation has been proposed as a solution to deliver rehabilitation to quarantined individuals [Citation7]. Telerehabilitation can be conducted through an internet-based remote-communication system to provide patients with exercise instructions and medical information [Citation8]. Several previous reports have proposed telerehabilitation as an effective method of delivering rehabilitation to COVID-19 patients [Citation9,Citation10].
However, telerehabilitation presents various challenges for communication, particularly when there is a language barrier or when treating patients with hearing problems [Citation11,Citation12]. Additionally, because of their isolation, patients with COVID-19 cannot be adequately educated face-to-face on how to operate devices and perform certain exercises before starting the rehabilitation session. Therefore, telerehabilitation is especially difficult for patients with low digital literacy [Citation13]. There is a need for practical strategies to facilitate communication across language barriers without increasing the burden on the patient. This report presents two cases (one in which the patient was hearing-impaired and one in which there was a language barrier) of successful delivery of telerehabilitation within communication difficulties.
Materials and methods
Telerehabilitation system
The telerehabilitation system was developed using existing resources, as reported previously [Citation10,Citation14]. The hardware consisted of a laptop for the service provider, a tablet computer for patients, and a pulse oximeter (RingO2, Neuroceuticals Inc., Tokyo, Japan) to monitor patients’ vital signs. The remote-control software TeamViewer (TeamViewer GmbH, Göppingen, Germany), the conferencing software Zoom (Zoom Video Communications Inc., San Jose, USA), Skype (Microsoft Corp., Microsoft, Redmond, USA), and a viewer application for the pulse oximeter were installed on the tablet used by patients. The accounts for the installed applications were created by the telerehabilitation provider. In addition, the privacy policy of each application was explained to the patients and their consent was obtained to make video calls via third-party applications. It was also confirmed that no individual’s name could be seen on the video during the session, and the connection was anonymized so that no information other than video and audio would be provided on the application. The video call was connected only during the exercise session. The pulse oximeter is a commercial product that can be connected to other devices via Bluetooth. To reduce online traffic, several video files of the exercise programme used in the telerehabilitation session were preinstalled on the tablet.
Procedure of the telerehabilitation programme
Two patients (one with difficulties communicating due to a language barrier and one with hearing loss) who received in-hospital treatment for COVID-19 in private rooms participated in the telerehabilitation programme. With the telerehabilitation system described above, the exercise programme was delivered to patients during one-on-one sessions with a physical therapist who had 12 years of professional experience. Using TeamViewer software, the patient’s tablet was remotely controlled by the therapist. Before starting the session, the therapist set up the apps remotely and prepared them for use during telerehabilitation. After checking the patient’s vital signs (heart rate [HR] and percutaneous oxygen saturation [SpO2]) and basic motor skills, the video exercise programme was implemented under the therapist’s supervision via video call.
The 10-min rehabilitation programme consisted of a video with computer-generated graphics (Speed Inc., Seto, Japan) depicting the following exercises: deep breathing, neck rotation, shoulder rotation, trunk lateral flexion, trunk rotation, hand grip/release, hip flexion, squatting, calf raise, raising both upper limbs forward and raising one leg, three side-steps, and slow/fast walking in place. For patients who lacked stability while standing, the therapist instructed them to perform exercises that could be performed while sitting, such as knee extensions instead of squatting. The patients performed the exercises while watching the video, but when they were unable to understand the movements, the therapist provided them with instructions on how to move. In addition, the therapist provided patients with encouragement and feedback to improve their motivation during the programme. After the programme was completed, patients’ vital signs changes in physical condition were rechecked. The entire programme was planned to be completed within 20 min, including the set-up and cooldown periods.
Assessment
Any malfunctions in the system (such as disconnecting from the internet, failure in launching the apps, and trouble in the video conference application or the remote-control application) were recorded. Patients’ satisfaction with the telerehabilitation session was evaluated.
To evaluate the patient’s satisfaction in the first case, a simple questionnaire was developed, consisting of three questions evaluating the patient’s trust in the program and their loyalty to the service, which are major predictors of patients’ intention to continue using the service [Citation15]. The patient was asked to score the aforementioned items on a scale ranging from 0 (strongly disagree) to 10 (strongly agree). The scale’s questions were as follows: Q1, “Are you satisfied with your decision to participate in this programme?”; Q2, “Do you think this exercise is important for isolated individuals to maintain their health?”; Q3, “Would you recommend this programme to other isolated individuals?”
In the second case, a more detailed assessment of satisfaction was conducted. The patient’s overall satisfaction with the telerehabilitation programme was evaluated using the Telemedicine Satisfaction Questionnaire (TSQ) [Citation16], which consists of 14 items scored on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The 14 items were divided into three subscales: quality of care provided (Factor 1), similarity to face-to-face encounter (Factor 2), and perception of the interaction (Factor 3). In addition, the following items were added to assess patient’s satisfaction with the video exercise program and environment provided by this system: Q1, “I can easily understand how to perform the movements”; Q2, “I feel safe performing the exercises”; Q3, “The room environment is appropriate for performing the exercises in the programme”; Q4, “The devices used are appropriate for performing the exercises”; and Q5, “Telecommunication with medical experts during exercise is helpful.”
Ethics statement
This study’s design was reviewed and approved by the Ethics Review Committee, Fujita Health University (registration no. HM20-047). The patients gave their written informed consent to participate in the study. Prior to consenting, the patients were informed of the use of video calls via third party applications, and explained the privacy policy of each application.
Case description
Case 1: Telerehabilitation for a patient speaking a different language
The patient was a 72-year-old man who had been quarantined after becoming infected with COVID-19 after an outbreak of the disease on the Diamond Princess cruise ship. He began telerehabilitation 23 days after onset of the disease. While participating in the telerehabilitation sessions, he exhibited no signs of pneumonia, even though he tested positive for the polymerase chain reaction test (PCR) after receiving treatment for pneumonia. Although he exhibited no neurological impairment and was independent in his activities of daily living, he was concerned about a decline in motor function due to inactivity during the quarantine; therefore, he requested guidance regarding which exercises he could perform on his own. The patient could only speak Cantonese and was unable to communicate in Japanese and in English, and there were no medical professionals available who could speak Cantonese. Therefore, routine communication with the medical staff was conducted through an interpreter or by using a portable translation device.
To accommodate the patient’s request, a telerehabilitation session was scheduled. As the patient was completely incapable of understanding English or Japanese, and since we had limited access to the translator, we translated the patients’ requests in real-time by using Google Translate (https://translate.google.co.jp/) during the telerehabilitation session. Google Translate provides automated online translation; it also supports voice-recognition and vocalisation functions. The telerehabilitation session was conducted with the combined use of the telerehabilitation system (described in the Materials and Methods section) and Google Translate.
Communication with the patient was conducted with the help of an assistant (who is an engineer) as follows: First, the therapist spoke into the microphone and the spoken content was converted into text via Google Translate. The assistant corrected any text errors resulting from the voice recognition software. After translation, the voice function was used to deliver the message to the patient (). The translation was performed by the therapist using Zoom’s voice sharing function. It was difficult to activate the translation function on the therapist’s side and on the patient’s side simultaneously; hence, telerehabilitation sessions were somewhat one-sided, as the therapist instructed the patient, while the patient’s subjective physical status and requests were registered using Yes/No questions.
Figure 1. Case 1: The therapist’s side during a telerehabilitation session. The physical therapist provided instructions and feedback to the patient using Google Translate. The assistant corrected the dictated text and provided the translated instructions and feedback to the patient using the read-out function on the patient's tablet.

The total session time (from the start of the call until the post-exercise vital-signs check) was 24 m 57 s. There were no technical problems with the internet connection, launching the system on the patient’s tablet, with the video conferencing application, or with the remote-control application. During the session, all the therapist’s instructions were successfully conveyed to the patient. The therapist asked Yes/No questions regarding the patient’s physical status, who reported no signs of dyspnoea or fatigue during the session. Before treatment, the patient’s vital signs were a heart rate of 85 bpm and an SpO2 of 98%; post-treatment, his heart rate was 87 bpm and he had an SpO2 of 98%. After the session, the patient was asked to rate his overall satisfaction with the program. The answers to Q1, Q2, and Q3 regarding satisfaction were scored 7 points, 8 points, and 8 points, respectively. The patient continued performing an exercise regimen on his own during his hospital stay, as instructed, and was discharged 29 days after onset.
Case 2: Telerehabilitation for a patient with hearing impairment
The patient was a 49-year-old man with neurofibromatosis who was infected with COVID-19. He had bilateral deafness and left facial nerve palsy after undergoing bilateral auditory nerve tumour removal surgery. He had a cervical cord tumour at the C2–C5 vertebrae and underwent tumour removal surgery a month before the onset of COVID-19. There was diffuse and mild muscle weakness in both sides of the upper-limb and lower-limb muscles, including the following (right/left): deltoids 4/4, biceps brachii 4/4, triceps brachii 4/4, wrist extensors 4/4, wrist flexors 4/4, iliopsoas 4/4, quadriceps 5/4, tibialis anterior 4/4, and gastrocnemius 4/4. Mild sensory impairment below the C4 level was also observed. He was able to walk with mild assistance using a walker and was independent in self-care, including dressing, eating, and toileting. He started telerehabilitation four days after the onset of COVID-19. There were no signs of pneumonia during the telerehabilitation period. He had no problem reading and used writing for daily communication. Despite complete bilateral hearing loss, his speech was clear.
As the patient was completely deaf, written conversations were chosen as a means of communicating the therapist’s instructions (). In advance, 25 written instructions that might be needed for the exercise were prepared in the form of cue cards. These cue cards were used to provide the patient with instructions at the start of the session to set up the used software, as well as during and after the session to give the patient feedback regarding his movement and to ask him about his physical condition (). Further, to smoothly transfer remote control to the therapist, several steps were visually explained to the patient using cue cards at the start of the session. The therapist also used cue cards to ask the patient about his physical condition to encourage him to report any subjective symptoms. The therapist monitored the patient’s vital signs with a pulse oximeter to ensure the safe execution of the exercise programme. Whenever it was necessary to add instructions or questions during the session, the therapist prepared the instant cue board during the session. The patient had no problems understanding the written text.
Figure 2. Case 2: Telerehabilitation session using cue cards. The therapist gave instructions to the patient by presenting him with cue cards during the video call.
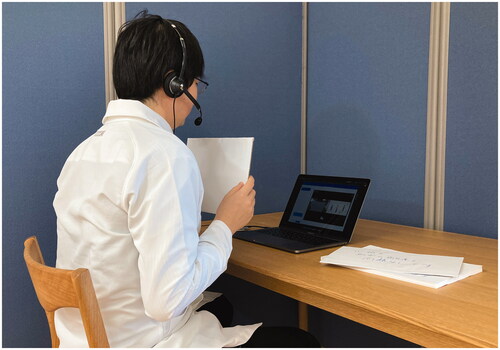
Table 1. List of cue cards’ contents.
Consequently, the patient understood how to operate the equipment and perform the exercises; there were no technical issues during the telerehabilitation sessions. The initial session’s total time (from the start of the call until the post-exercise vital signs check) was 20 m 16 s. As the patient was unable to stand without a handrail for support, the exercise was conducted in a sitting position. The patient’s HR and SpO2 before the exercises were 75 bpm and 98%, respectively, which remained stable at 79 bpm and 98% after the exercise. After the session, the patient scored the TSQ and the questions added specifically for this study (). An item regarding the sound quality of the system (item 2 in Factor 2) was excluded from this case. After the initial session, the patient participated in four more telerehabilitation sessions over two weeks of quarantine. The average time of the telerehabilitation sessions was 18 m 41 s. No technical problems were reported during the sessions.
Table 2. Results of the Telemedicine Satisfaction Questionnaire and additional questions in Case 2.
After the PCR test returned negative results, the patient’s quarantine was lifted and he was transferred to a face-to-face rehabilitation programme. After a 41-day hospital stay, he became independent in his activities of daily living, including walking and bathing, and was discharged to his home without any complications related to COVID-19.
Discussion
In this case report, we introduced two cases of telerehabilitation delivery that required adjustment to account for communication difficulties. This report may provide valuable insights for expanding the coverage of telerehabilitation programmes within the context of COVID-19 and other infectious diseases.
Telerehabilitation is defined by Brennan, Mawson, and Brownsell as “the delivery of rehabilitation services using information and communication technologies” [Citation17]. Further, it has been explored as a way to reduce hospitalisation times and to deliver rehabilitation to patients with poor access to face-to-face services. The importance of telerehabilitation has been emphasized by the circumstances imposed by the COVID-19 pandemic [Citation18], as it limits physical contact and reduces the likelihood of infection [Citation19]. It is interesting to note that in this pandemic, telerehabilitation technologies were not only used to rehabilitate patients literally at a distance, but also in the hospital, where they had direct access to medical services [Citation9,Citation20]. This may not have been conventionally considered within the scope of telerehabilitation; however, we chose to use the term “telerehabilitation” here, as we believe that the most important purpose of the telerehabilitation is to access isolated patients–whether or not they are physically “distant”. The rehabilitation services entail contact or instruction by the clinical expert with the patients for a certain period of time; therefore, sufficient service provision to the patients is hindered under the situation which requires strict isolation. Even though COVID-19 patients were physically close to the service providers, they were still “distant” due to their isolation–this was especially the case in the early stages of the pandemic. In this sense, the pandemic has provided an opportunity to demonstrate the broad potential of telerehabilitation, which is not merely an extension of telemedicine.
The circumstances imposed by the COVID-19 pandemic present various methodological difficulties for telerehabilitation. For example, several previous studies posit that the process of telerehabilitation consists of two stages, namely, the prior practice of exercise and set-up of operating devices, and the subsequent tele-sessions [Citation21–23]. However, when practice is initiated in isolation from the beginning, the user is in charge of handling the device and applications, and must perform the exercises without any on-site assistance. Therefore, communication difficulties often represent significant obstacles for telerehabilitation [Citation24,Citation25].
In this study, the delivery of telerehabilitation required the simplification of device operation through the use of remote-control software and the development of two specific strategies to solve the communication problems presented by each case. The use of remote-control software contributed to simplifying the operation of the system and improving feasibility, as shown in a previous report [Citation14].
To overcome the language difference in the first case, the use of online translation software was effective, demonstrating that it can be a valuable tool for solving communication problems due to language differences. Recent advances in simultaneous translation artificial intelligence will also provide solutions for language differences [Citation26]. Although there remains room for improvement regarding translation accuracy, speed, and dialect and accent detection [Citation27], simultaneous translation applications are being developed for use in the medical field and in other contexts [Citation28]. The combined use of such technologies may enable cross-border interventions. Furthermore, the use of online simultaneous translation technology may allow for even smoother communication compared to on-site interventions with translators and translation devices. In this study, communication using the tablet and online translation proceeded without the need for an intervening translator or additional devices, which prevented the patient’s attention from being diverted from the therapist during telerehabilitation sessions. Participants’ responses were generally positive, however, there may be some arguments whether the scores (seven in Q1 and eight in Q2 and Q3) are high enough to regard high satisfaction to the service. For example, a score of eight in Q3 asking if the patient recommend the service to the others that is similar to the Net Promoter Score used for assessment of commercial service [Citation29], where a score of eight is classified as “passives”, indicating the population that is broadly happy but would not take actions such as repeat and/or promote the service. Further detailed assessment on positives and negatives of the service would be helpful in implementing the service into the rehabilitation clinics.
In contrast to the web-based solution in Case 1, communicating with the hearing-impaired patient was achieved using an analogue solution; the cue board approach is a simple but effective means of communication. Although, at first glance, the presence of severe hearing impairment may seem a significant obstacle for telerehabilitation, the combination of remote-control technology and the analogue cue board constituted a viable solution. In fact, the items in which the patient scored best included “I do not need assistance while using the system” (item 1 in Factor 1) and “I can talk with my health care provider easily” (item 1 in Factor 2), which support the usability of this combination. These results provide clues regarding possible further investigation on the provision of telerehabilitation to patients with hearing loss.
Isolation due to severe infectious diseases, such as COVID-19, can lead to severe declines in motor and cognitive function, which are key elements in quality of life, especially for vulnerable individuals, including the elderly and disabled persons [Citation3,Citation4,Citation30,Citation31]. The existence of a communication barrier may create further difficulties for the affected individuals, including psychological problems. The use of telerehabilitation and the development of new ways to overcome communication barriers could facilitate the delivery of health services and serve as a support for vulnerable individuals by improving their level of functioning during the pandemic.
A limitation of the current report is that the method for assessing patients’ satisfaction with the intervention was different between two cases. In Case 1, an original questionnaire was created in Japanese and then translated into Cantonese. This simple questionnaire was used in this case because of the language barrier and very limited contact with the patient during the early stage of pandemic that made it difficult to obtain detailed feedback from the patient. Further investigation regarding patients’ experience with the use of the telerehabilitation service should be conducted with more detailed and validated questionnaires. For Case 2, the TSQ was used for satisfaction assessment. However, there were several limitations with this. Firstly, the application of the TSQ has not been validated for individuals with disability and there were therefore some issues in applying it to them; for example, there is an item asking about the sound quality of the system, and it was impossible for the patient of Case 2, who was deaf, to evaluate it. Therefore, this item was eliminated from our survey. Since this can happen with a variety of disabilities, including motor and visual impairments, methods for assessing the quality of telerehabilitation systems by people with disabilities need to be further explored. In addition, the TSQ used in this study was a preliminary Japanese version translated by researchers without a standardized procedure. The translation and cross-cultural adaptations of self-reported measures should be done using a standardized procedure [Citation32], and to date, the only existing different-language version of the TSQ is in Turkish [Citation33]. Therefore, a standardized and Japanese-translated version of the TSQ or another appropriate questionnaire for system evaluation should be developed for future studies. In addition, the satisfaction survey might be insufficient in terms of frequency; it was only conducted immediately after the initial intervention. Further, the results of the survey may have been influenced by patients’ social relationship with the service provider. Future research to further clarify patient-friendliness of the services should include more detailed, standardized, and frequent assessments of patient satisfaction over a longer period of time.
Conclusion
In this case report, we described two cases of successful telerehabilitation delivery for two individuals with COVID-19 who presented communication difficulties. The isolation resulting from COVID-19-related social distancing measures can lead individuals to become inactive, which may lead to functional decline. Although there are several practical difficulties in delivering telerehabilitation to patients facing communication barriers, the use of complementary methodologies, such as the ones reported in this case study, may help solve these difficulties and contribute to further expanding the scope and applicability of telerehabilitation.
Acknowledgements
We would like to express our sincere gratitude to all the patients who participated in this study, as well as to the staff of the coronavirus treatment ward who actively suggested the project.
Disclosure statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- World Health Organization. Novel Coronavirus situation report 52. 2020; [cited 2020 Dec 9]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200312-sitrep-52-covid-19.pdf?sfvrsn=e2bfc9c0_4.
- Sepulveda-Loyola W, Rodriguez-Sanchez I, Perez-Rodriguez P, et al. Impact of social isolation due to COVID-19 on health in older people: mental and physical effects and recommendations. J Nutr Health Aging. 2020;24:938–947.
- Ceravolo MG, Arienti C, de Sire A, et al. Rehabilitation and COVID-19: the cochrane rehabilitation 2020 rapid living systematic review. Eur J Phys Rehabil Med. 2020;56(5):642–651.
- De Biase S, Cook L, Skelton DA, et al. The COVID-19 rehabilitation pandemic. Age Ageing. 2020;49(5):696–700.
- Jaffri A, Jaffri UA. Post-Intensive care syndrome and COVID-19: crisis after a crisis? Heart Lung. 2020;49(6):883–884.
- Beeching NJ, Fletcher TE, Beadsworth MBJ. Covid-19: testing times. BMJ. 2020;369:m1403.
- Chang MC, Boudier-Reveret M. Usefulness of telerehabilitation for stroke patients during the COVID-19 pandemic. Am J Phys Med Rehabil. 2020;99(7):582.
- Peretti A, Amenta F, Tayebati SK, et al. Telerehabilitation: review of the state-of-the-art and areas of application. JMIR Rehabil Assist Technol. 2017;4(2):e7.
- Sakai T, Hoshino C, Yamaguchi R, et al. Remote rehabilitation for patients with COVID-19. J Rehabil Med. 2020;52(9):jrm00095.
- Mukaino M, Tatemoto T, Kumazawa N, et al. Staying active in isolation: telerehabilitation for individuals with the SARS-CoV-2 infection. Am J Phys Med Rehabil. 2020;99(6):478–479.
- Lopez AM, Lam K, Thota R. Barriers and facilitators to telemedicine: can you hear me now? Am Soc Clin Oncol Educ Book. 2021;41:25–36.
- Annaswamy TM, Verduzco-Gutierrez M, Frieden L. Telemedicine barriers and challenges for persons with disabilities: COVID-19 and beyond. Disabil Health J. 2020;13(4):100973.
- Seifert A, Batsis JA, Smith AC. Telemedicine in long-term care facilities during and beyond COVID-19: challenges caused by the digital divide. Front Public Health. 2020;8:601595.
- Mukaino M, Tatemoto T, Kumazawa N, et al. An affordable, user-friendly telerehabilitation system assembled using existing technologies for individuals isolated with COVID-19: development and feasibility study. JMIR Rehabil Assist Technol. 2020;7(2):e24960.
- Platonova EA, Kennedy KN, Shewchuk RM. Understanding patient satisfaction, trust, and loyalty to primary care physicians. Med Care Res Rev. 2008;65(6):696–712.
- Yip MP, Chang AM, Chan J, et al. Development of the telemedicine satisfaction questionnaire to evaluate patient satisfaction with telemedicine: a preliminary study. J Telemed Telecare. 2003;9(1):46–50.
- Brennan DM, Mawson S, Brownsell S. Telerehabilitation: enabling the remote delivery of healthcare, rehabilitation, and self management. Stud Health Technol Inform. 2009;145:231–248.
- Turolla A, Rossettini G, Viceconti A, et al. Musculoskeletal physical therapy during the COVID-19 pandemic: is telerehabilitation the answer? Phys Ther. 2020;100(8):1260–1264.
- Assenza C, Catania H, Antenore C, et al. Continuity of care during COVID-19 lockdown: a survey on stakeholders’ experience with telerehabilitation. Front Neurol. 2020;11:617276.
- Turcinovic M, Singson R, Harrigan M, et al. Physical therapy for hospitalized patients with COVID-19 in isolation: feasibility and pilot implementation of telehealth for delivering individualized therapy. Arch Rehabil Res Clin Transl. 2021;3(2):100113.
- Piqueras M, Marco E, Coll M, et al. Effectiveness of an interactive virtual telerehabilitation system in patients after total knee arthoplasty: a randomized controlled trial. J Rehabil Med. 2013;45(4):392–396.
- Moffet H, Tousignant M, Nadeau S, et al. In-home telerehabilitation compared with face-to-face rehabilitation after total knee arthroplasty: a noninferiority randomized controlled trial. J Bone Joint Surg Am. 2015;97(14):1129–1141.
- Hwang R, Bruning J, Morris NR, et al. Home-based telerehabilitation is not inferior to a Centre-based program in patients with chronic heart failure: a randomised trial. J Physiother. 2017;63(2):101–107.
- Hill AJ, Theodoros D, Russell T, et al. Using telerehabilitation to assess apraxia of speech in adults. Int J Lang Commun Disord. 2009;44(5):731–747.
- Lam K, Lu AD, Shi Y, et al. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern Med. 2020;180(10):1389–1391.
- Martins AFT, Graca J, Dimas P, et al. editors. Project MAIA: Multilingual AI agent assistant. Proceedings of the 22nd annual conference of the European association for machine translation. Lisboa, Portugal: European Association for Machine Translation; 2020. p. 495–496.
- Das AK. Translation and artificial intelligence: where are we heading? Int J Transl. 2018;30:72–101.
- Liebling DJ, Lahav M, Evans A, et al. Unmet needs and opportunities for mobile translation AI. Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems 2020. p. 1–13.
- Reichheld FF. The one number you need to grow. Harv Bus Rev. 2003;81(12):46–54. 124.
- Kirwan R, McCullough D, Butler T, et al. Sarcopenia during COVID-19 lockdown restrictions: long-term health effects of short-term muscle loss. Geroscience. 2020;42(6):1547–1578.
- Kemp HI, Corner E, Colvin LA. Chronic pain after COVID-19: implications for rehabilitation. Br J Anaesth. 2020;125(4):436–440.
- Beaton DE, Bombardier C, Guillemin F, et al. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25:3186–3191.
- Özkeskin M, Özden F, Ekmekçi Ö, et al. The reliability and validity of the turkish version of the Telemedicine Satisfaction and Usefulness Questionnaire (TSUQ) and telemedicine patient questionnaire (TPQ) in individuals with multiple sclerosis. Neurol Sci. 2021;2021:1–7.
