ABSTRACT
There is a growing debate about the involvement of the gut microbiome in COVID-19, although it is not conclusively understood whether the microbiome has an impact on COVID-19, or vice versa, especially as analysis of amplicon data in hospitalized patients requires sophisticated cohort recruitment and integration of clinical parameters. Here, we analyzed fecal and saliva samples from SARS-CoV-2 infected and post COVID-19 patients and controls considering multiple influencing factors during hospitalization. 16S rRNA gene sequencing was performed on fecal and saliva samples from 108 COVID-19 and 22 post COVID-19 patients, 20 pneumonia controls and 26 asymptomatic controls. Patients were recruited over the first and second corona wave in Germany and detailed clinical parameters were considered. Serial samples per individual allowed intra-individual analysis. We found the gut and oral microbiota to be altered depending on number and type of COVID-19-associated complications and disease severity. The occurrence of individual complications was correlated with low-risk (e.g., Faecalibacterium prausznitzii) and high-risk bacteria (e.g., Parabacteroides ssp.). We demonstrated that a stable gut bacterial composition was associated with a favorable disease progression. Based on gut microbial profiles, we identified a model to estimate mortality in COVID-19. Gut microbiota are associated with the occurrence of complications in COVID-19 and may thereby influencing disease severity. A stable gut microbial composition may contribute to a favorable disease progression and using bacterial signatures to estimate mortality could contribute to diagnostic approaches. Importantly, we highlight challenges in the analysis of microbial data in the context of hospitalization.
Introduction
The global pandemic caused by the new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) brought the health systems to its limitations. The disease is characterized by respiratory symptoms although there is increasing evidence of gastrointestinal (GI) tract involvement.Citation1–3 Nausea, vomiting, and diarrhea are relatively common in COVID-19Citation4 and a proportion of patients report only gastrointestinal symptoms.Citation5 The virus itself is not limited to the lungs but replicates in human enterocytesCitation6 and is detectable in the patients’ fecal samples.Citation1,Citation7 GI symptoms in patients with COVID-19 appear to be associated with increased disease severity and complications,Citation8 although the underlying causes are not understood. Recent studies suggest that an altered microbial composition correlates with COVID-19 disease severity and inflammatory response to the disease.Citation9,Citation10
Common complications of COVID-19 include venous thromboembolism,Citation11,Citation12 hemodynamic instability,Citation13 and acute kidney injury.Citation14 Particularly in severe cases, an excessive and prolonged immune response to the virus is thought to be a catalyst of severity.Citation15,Citation16
The composition of the gut microbiota plays a critical role in the immunological homeostasis of the human body.Citation17,Citation18 It is known that the human gut microbiome is sensitive to changes in the hosts’ environment.Citation19 In addition to antibiotic use and diet,Citation20 critically ill patients show a rapid depletion of health-promoting organisms.Citation21
The study examined the impact of gut and oral microbiota on complication rate and outcome and, conversely, how hospitalization affects the gut microbial composition in this cohort.
Material and methods
Study cohorts
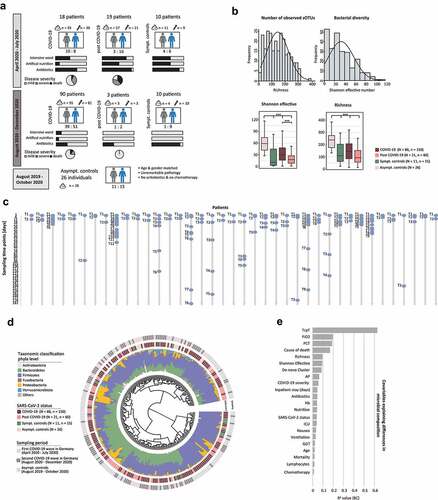
The study population consists of four groups: (1) 108 patients with laboratory confirmed SARS-CoV-2 infection, (2) 22 patients post COVID-19 who had cleared the virus and were tested negative at first sampling, (3) 20 symptomatic pneumonia controls (SC) and (4) 26 age- and gender-matched asymptomatic controls (AC) (, ). Altogether, 251 stool samples and 160 saliva samples were examined. A deteiled overview of sampling time point and frequency is shown in . Serial samples were collected to investigate intra-individual changes over time. A total of 25 and 15 COVID-19 patients, 11 and 5 post COVID-19 patients and 3 and 2 SC provided serial stool and saliva samples, respectively (). The SC patients were admitted with respiratory symptoms of community-acquired-pneumonia (CAP) and were tested negative for SARS-CoV-2. Patients in the AC group were considered SARS-CoV-2 negative as they presented mainly for screening colonoscopy and showed no symptoms of SARS-CoV-2 infection. To minimize potential influencing factors on the microbiota in the AC cohort, patients with active cancer, inflammatory bowel disease (IBD), oncologic therapy, or antibiotic intake at the time of examination or within 6 months prior were excluded. Endoscopic examination and pathology reports from colon biopsies had to be unremarkable.
Table 1. Demographic and Clinical Characteristics of the Study Population
Figure 1. Microbial Composition of the Gut Observed in the Cohort.
Patient recruitment and sampling
Acquisition of patients was conducted at the university hospital Klinikum rechts der Isar, Technical University Munich, Germany. COVID-19 patients, post COVID-19 patients and SC were prospectively recruited between April 2020 to July 2020 (first COVID-19 wave in Germany) and August 2020 to December 2020 (second COVID-19 wave in Germany), whereas the AC group was prospectively recruited between August 2019 and October 2020. Because these were control patients in an intestinal microbiome-only study, saliva was not obtained (). Stool, saliva, and blood samples were collected at least once per week during the inpatient stay. To ensure follow-up and bio-sample collection after discharge, patients were invited to follow-up visits. SARS-CoV-2 infection was confirmed by quantitative reverse transcription PCR (TaqMan™-PCR performed on Roche cobas® 6800, Basel, Switzerland), performed on nasopharyngeal swabs. For the post COVID-19 patients, the first stool sample was collected on average 30 days after the negative PCR. In the AC group, stool samples were collected either before or 6 weeks after bowel preparation for colonoscopy. To characterize the disease activity, laboratory parameters and data regarding fraction of inspired oxygen (FiO2), ventilation mode, diet, intensive or normal ward and antibiotic use were collected at each time point of stool or saliva sampling.
Classifications
Patients with COVID-19 or post COVID-19 were classified into three groups based on the WHO ordinal scale for clinical improvement for hospitalized patients with COVID-19,Citation22 which has been used in other COVID-19 studies:Citation23 (i) mild disease, composed of patients with no oxygen therapy (score 3) or oxygen by mask or nasal prongs (score 4); (ii) severe disease, including patients requiring noninvasive ventilation or high-flow oxygen (score 5), intubation and mechanical ventilation (score 6) or ventilation and additional organ support (score 7), and (iii) fatal disease (death, score 8). Ventilation mode during inpatient stay was divided in two groups: (i) Oxygen via nasal prongs, and (ii) mechanically ventilated either pressure controlled (PC) or pressure assisted (PA) and tracheostomy (TS) after long period of intubation. Considering the varying impact of different antibiotics on the gut microbiota, antibiotic therapy was classified according to their spectrum of activity (Supplementary Table 1). Patients were either fed normally or with formulated food via gastric tube in combination with or without parenteral nutrition (summarized in tube feeding).
Ethical approval
All patients provided written informed consent. The study was conducted in accordance with the declaration of Helsinki and approved by the ethics committee of the Technical University Hospital of Munich (221/20 S-SR).
Sample preparation and 16S rRNA gene sequencing
Fecal and saliva samples were stored in a solution to stabilize DNA (MaGix PBI, Microbiomix GmbH, Regensburg, Germany). Sample preparation and paired-end sequencing was performed on an Illumina MiSeq targeting the V3V4 region of the 16S rRNA gene. No batch effect could be observed for samples sequenced on different sequencing runs (Supplementary Figure 1 A). Detailed description of the methods is published.Citation24 Raw FASTQ files were processed using the NGSToolkit (https://github.com/TUM-Core-Facility-Microbiome/ngstoolkit) based on USEARCH 11Citation25 to generate denoised zero-radiation operational-taxonomic units (zOTUs).
Statistical analysis
Differences in relative abundance of taxa and/or zOTUs were determined by Kruskal-Wallis Rank Sum test for multiple groups and Wilcoxon Rank Sum test for pairwise comparison. Differences in prevalence were determined by a non-linear Fisher Exact test. Spearman correlation was calculated for associations and continuous variables. Read counts were normalized according to a fixed value of 10.000 reads per sample.
Similarity between samples was estimated based on a distance matrix using generalized UniFrac. Briefly, the package ‘GUniFrac’ using the method ‘GUniFrac’ with alpha settings 0,0.5,1.0 was used on a rooted tree. Afterward by using ‘unifracs’, the generalized unifrac distance was extracted by setting alpha to 0.5. The tree was generated by approximately-maximum-likelihood phylogenetic trees using ‘FastTree’ with the GTR+CAT mode. The tree was generated on an alignment generated by sina (version 1.7.2). Based on the calculated distance, we used the R function metaMDS (package vegan) to generate the graph.
Significance between groups, effect modifier, and confounder were determined by a permutational multivariate analysis of variances (adonis function of the R-package vegan).
For all analyses, p-values were corrected for multiple testing according to Benjamini-Hochberg correction.
The explained variation of co-variables was determined by calculating R2 values and were considered as significant with a p-value ≤0.05. A random forest model was used to classify binary outcome variables based on microbial composition with a fivefold cross-validation by using randomForest from the R package randomForest v4.6–14. To receive a robust and generalizable classification model, the machine-learning algorithm was applied 100 times iteratively. Based on out-of-bag error rates and Gini index, the most important features were selected for each iteration using rfcv from the R package randomForest v4.6–14. Features, which appeared in all 100 random forest models, were considered as classification features for the final model. A generalized linear model for binomial distribution and binary outcome (logit) was generated using the previously selected features.
Results
Association of SARS-CoV-2 status with the gut microbiota
Analysis of the gut microbiota was performed on 251 stool samples (n = 251) from 144 patients (N = 144), of which were 86 COVID-19 patients (n = 150 samples), 21 post COVID-19 patients (n = 60), 11 SC (n = 15) and 26 AC (n = 26) (). No bias between the two sampling phases was observed allowing a combined analysis of the two COVID-19 waves.
Phylogenetic distance analysis of each patient’s microbial profile showed no clustering according to SARS-CoV-2 status. Nevertheless, some patients were found to have an increased relative abundance of Proteobacteria, which was mainly observed with COVID-19 and post COVID-19 samples (). The analysis of alpha-diversity revealed a not normally distributed number of observed species and bacterial diversity (). The number of observed species was reduced in active COVID-19 (richness 133 ± 90) and post COVID-19 patients (richness 103 ± 60) compared to AC (richness 219 ± 68), and bacterial diversity showed a reduced Shannon effective number in SC ().
Considering only the first sampling time point (T1) per individual revealed that parameters related to patient’s health were important effect modifiers (). Interestingly, even though the SARS-CoV-2 status alone did not show a clear pattern in the phylogenetic distance tree, the detection of SARS-CoV-2 in nasopharyngeal swabs significantly influenced the gut microbiota (RCitation2 = 0.04, p = .001), as well as disease-related variables, e.g. the disease severity (RCitation2 = 0.05, p = .001).
Evaluation of confounding factors
Although variables known to influence the microbial composition of the gut such as antibiotics or chemotherapy, appeared to be significant influencing factors (), none of the tested variables were confounders within the analyzed cohort (Supplementary Table 2 and 3). Particular attention was paid to variables related to hospitalization such as artificial feeding, critical care and antibiotic treatment. Since most patients were treated with different groups of antibiotics, we could not elucidate the influence of a specific antibiotic subgroup on the composition of the gut microbiota (Supplementary Figure 1 B). Stratifying the patient cohort according to health status and feeding type showed no differences in microbial composition and bacterial diversity (Supplementary Figure 1 C, D). Additionally, patients’ comorbidities and disease history was tested for confounding, considering type 2 diabetes,Citation26,Citation27 inflammatory bowel disease,Citation28 cancer, as well as chemotherapy and immunotherapyCitation29 within 6 months before stool sampling, or bowel resectionCitation30 (Supplementary Table 3). We further tested whether age and gender, specific SARS-CoV-2 treatment (remdesivir, convalescent plasma, intravenous immunoglobulins, or baricitinib), immunosuppressive therapy, or secondary infections introduced bias in the microbial analysis. Of note, critically ill patients with complications, compared to mild courses, were mainly treated at the ICU and received antibiotics (Supplementary Table 4). However, within the cohort none of the above-mentioned variables had a confounding effect in the analysis of the microbial composition related to COVID-19.
Disease severity and progression are related to altered gut microbiota
Disease severity according to WHO ordinal scale for clinical improvement significantly correlated with the gut bacterial composition of stool samples (p = .001) ( , Supplementary Figure 2). Beta-diversity clearly demonstrated a shift of bacterial profiles comparing controls with COVID-19 and post COVID-19 patients. Thereby, the bacterial composition of patients with a mild disease was more similar to SC and AC and a more severe disease showed a microbial composition more similar to patients who died due to COVID-19. A number of stool samples clustered independently in patients with severe and fatal COVID-19 disease, as well as a few mild courses and SC ( , left cluster). However, patients with mild disease in this cluster, or SC, showed no similarities for clinical or laboratory parameters with severe cases. None of the AC samples fell within this cluster.
Figure 2. Microbial Profile of the Gut is Associated with Disease Severity.
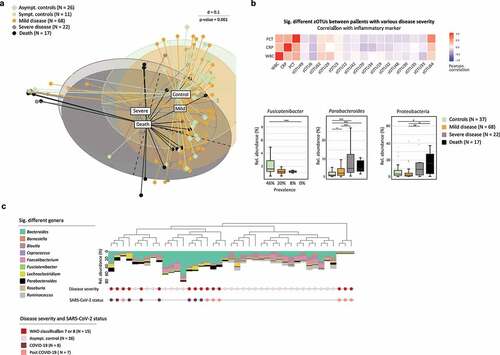
We determined significantly differences between study groups using differentiation analysis. Here, the analysis has been adjusted for confounders including the influence of antibiotic intake, feeding and ward. The zOTUs, which were significantly different between study groups (Supplementary Table 5) correlated with markers of inflammation, such as white blood cells counts (WBC), C-reactive protein (CRP) and procalcitonin (PCT) (). Here, Clostridium innocuum (zOTU62), Ruthenibacterium lactatiformans (zOTU29), and Alistipes finegoldii (zOTU64) correlated positively with inflammatory markers and continued to show a significantly increased relative abundance or prevalence in patients with a severe disease progression. Negatively correlated zOTUs were significantly decreased in severe and fatal cases of COVID-19 and post COVID-19, such as Faecalibacterium prausnitzii (zOTU20), Blautia luti (zOTU6), Dorea longicatena (zOTU32), Gemmiger formicilis (zOTU30), and Alistipes putredinis (zOTU33). In addition, Fusicatenibacter showed a significantly reduced prevalence in severe cases and was totally absent in patients who died (). On the other hand, Parabacteroides significantly increased with a more severe disease (). Beta-diversity analysis already showed some accumulation of patients with an increased relative abundance of Protobacteria (), which was also found to be increased in severe COVID-19 cases ().
To analyze the associations of the gut microbial composition with COVID-19 severity in greater depth, we defined a subset of patients with certain criteria. This included patients presenting with high inflammatory parameters (CRP ≥ 10 mg/dl, PCT ≥ 5 ng/ml, WBC ≥ 15 G/l), FiO2 ≥ 40%, requiring mechanical ventilation (PC, PA, TS), were treated at the ICU, and had at least one complication. In addition, WHO disease severity was set to ≥6. Overall, 15 male patients met the criteria (COVID-19, N = 8; post COVID-19, N = 7) and all of them died, 13 due to acute respiratory distress syndrome (ARDS) and 2 of them due to cerebral hemorrhage. Stratification according to disease severity (corrected for the confounders antibiotic intake, feeding, and ward) showed that the microbial profile of severe and fatal cases clustered together. These profiles were mainly dominated by an increased relative abundance of Parabacteroides, Lachnoclostridium, and a reduced relative abundance of Blautia, Faecalibacterium, and Ruminococcus (), which were shown to be underrepresented in COVID-199. There were no significant differences in the bacterial composition between COVID-19 or post COVID-19 patients. Interestingly, AC showed a higher abundance of Coprococcus, previously demonstrated to be associated with non-COVID-19 patients,Citation10 and Roseburia, which were reported to be more prevalent in healthy individuals compared to COVID-19 patients.Citation9 Although we revealed a strong correlation of the gut bacterial composition, it remains unclear whether the bacterial composition of the gut affects severity, or vice versa.
Microbial analysis of saliva samples
Alterations in the oral microbiome have previously been associated with COVID-19 and suggested as a diagnostic marker.Citation31 To comprehensively analyze the oro-intestinal bacterial composition, saliva samples were collected in addition to fecal samples ( , Supplementary Table 6). In total, 160 saliva samples from 117 patients were analyzed (COVID-19, N = 87, n = 117; post COVID-19, N = 13, n = 24; SC, N = 17, n = 19). Taxonomic differences on phyla level are minor with a reduced relative abundance of Firmicutes in COVID-19 compared to post COVID-19 and SC. Post COVID-19 showed an increased relative abundance of Proteobacteria and a reduction in Actinobacteria. Compared to SC, post COVID-19 and COVID-19 had an increased abundance of Fusobacteria (Supplementary Figure 3 A). Overall, microbial composition between the groups showed no significant differences (Supplementary Figure 3 B). Interestingly, in accordance with our findings regarding the gut bacteria, stratification of patients according to disease severity showed a significant difference in the composition of the oral microbiome (p = .003) (Supplementary Figure 3 C) as well as significant variations according to the number of complications (p = .001) (Supplementary Figure 3 D). However, a random forest model failed to predict mortality in the setting of COVID-19-associated hospitalization for saliva samples.
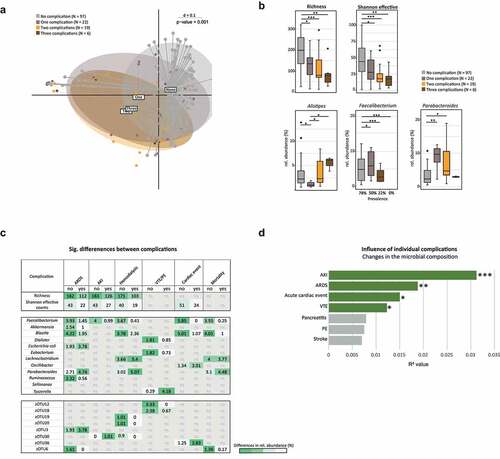
Alterations of the gut microbiota correlate with number and type of complications
Following the association between severity and changes in the gut microbiota, we further investigated whether microbial changes were found in terms of type and number of complications in COVID-19 and post COVID-19 patients and SC. A maximum of three complications per patient were observed. Stratifying patients according to the number of complications revealed a significant distinction between patients with no complications and patients with one or more complications, with a shift in their bacterial profile according to the number of complications (p = .002) (). Furthermore, alpha-diversity showed that the abundance of gut bacteria decreased with the number of complications (). Interestingly, F. prausnitzii was found to be reduced with an increased number of complications and absent in patients with three complications (). Consistent with the findings regarding disease severity (), Parabacteroides was increased in patients with a more complicated course (). Again, models were adjusted for confounding factors (antibiotic intake, feeding, and ward). Some complications showed overlapping bacterial taxa, which were significantly different in their relative abundance compared to patients without the corresponding complication. Patients who developed ARDS, AKI, or had hemodialysis, revealed a significantly reduced gut bacterial richness as well as Shannon effective number, which was also seen in patients with an acute cardiac event (). Specific complications were associated with changes in the relative abundance of individual bacteria (). Hereby, the butyrate producing F. prausnitzii was significantly reduced in patients with ARDS, AKI, hemodialysis, and acute cardiac events and furthermore negatively associated with mortality. Blautia was reduced for most complications except in patients with VTE/PE or AKI. Parabacteroides, on the other hand, was increased in patients with ARDS and hemodialysis and showed a positive association with mortality. Multivariate permutational analyses showed that AKI had the greatest influence on microbial changes, followed by ARDS, acute cardiac events and VTE. However, pancreatitis and stroke were not significantly contributing to microbial differences ().
Figure 3. Association Between Gut Bacterial Composition and Common Complications.
A stable gut bacterial composition is correlated with a favorable disease progression
During this study, 39 patients (COVID-19, post COVID-19, and SC) provided more than one stool sample, enabling the analysis of intra-individual changes during disease course (). Based on generalized UniFrac distances, the stability of the microbial composition of the gut was determined (). On average, the intra-individual distance was 0.33 ± 0.09. The microbial composition was equally dynamic between COVID-19, post-COVID-19, and SC. Compositional changes were not related with ward, nutrition, antibiotics, or disease severity. Stratifying the longitudinal data according to the number of complications supported our previous results () that the onset of complications during inpatient stay significantly correlated with an altered bacterial composition (p = .001) (). Although the intra-individual distance showed no obvious grouping based on SARS-CoV-2 status, a cluster could be detected according to the simple presence or absence of complications. COVID-19 patients without any complication had a more stable microbial composition compared to patients with complications (). Analysis of the intra-individual microbial stability accounting for varying conditions demonstrated the significance of environmental factors in addition to the disease state. In the context of intra-individual examination of the bacterial profiles over time, disease progression could be tracked using inflammation markers (CRP, PCT, WBC) and oxygen demand (FiO2) at the time of each stool sample. Thus, we defined a group of COVID-19 and post COVID-19 patients with severe progression. Criteria for a severe progression had to be met at least for one sampling time point (CRP ≥ 10 mg/dl, PCT ≥ 5 ng/ml, WBC ≥ 15 G/l, FiO2 ≥ 40%) and we compared this group (S-prog, N = 44) with patients not meeting these criteria (NS-prog, N = 62). Indeed, the bacterial composition of S-prog significantly differed from NS-prog ().
Figure 4. Stability of the Bacterial Composition Related to COVID-19 and Longitudinal Analysis.
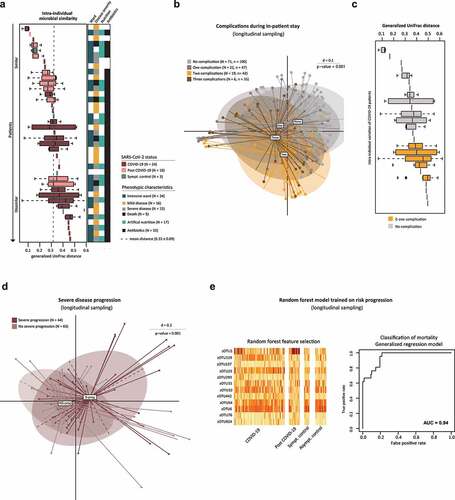
Additionally, machine learning was applied to differentiate between S-prog and NS-prog. Toward this end, a random forest model was trained on COVID-19 patients in a 10-fold cross-validated nested approach (repeated 100 times). In total, 12 zOTUs were selected as important features: Enterococcus durans (zOTU1), Streptococcus thermophilus (zOTU119, zOTU25), Citrobacter freundii (zOTU137, zOTU76), Holdemania massiliensis (zOTU293), Parabacteroides distasonis (zOTU31), D. longicatena (zOTU32), Lactococcus lactis (zOTU442), Blautia spp. (zOTU54, zOTU6), Lacticaseibacillus rhamnosus (zOTU924) ( , Supplementary Table 5). The defined signature was overlapping with zOTUs associated with disease severity within our patient population (). Based on this bacterial signature, a generalized linear model of all patients revealed an area under the curve (AUC) of 0.94 for predicting mortality during the COVID-19 associated inpatient stay (accuracy = 0.94, sensitivity = 0.98, specificity = 0.69) (). The classifiers reached a recall of 50% without any false positive predictions and resulted in an PR-AUC of 0.92 (Supplementary Figure 1 E).
The specificity was verified by applying the signature to other outcomes, e.g. type 2 diabetes (AUC = 0.76) or the presence of complications (AUC = 0.82). Further, 12 random zOTUs were selected as classifiers showing a poor differentiation of mortality (Supplementary Figure 1 E). Also by picking an equal number of cases and controls, as well as an equal number of controls and false-cases (picked randomly from control group) resulted in lower AUC values compared to the original model.
Discussion
The risk of a severe disease course and complications, including thromboembolism, renal failure, and acute cardiac events, is higher for COVID-19 than for influenza.Citation32 GI symptoms in patients with COVID-19 are associated with an increased disease severity and complicationsCitation8 and an exaggerated immune response to the virus is considered to play a crucial role in driving disease progression.Citation15,Citation16 It is well known that gut microorganisms influence the systemic immune response of their hosts through multiple crosstalk with immune cells.Citation33–35
In our study, we demonstrated that the bacterial composition of the gut in patients with COVID-19 disease changes with number and type of complications. Thereby, taxa known for protective and immunosuppressive properties were found to be decreased with an increasing complication rate, whereas rather pathogenic taxa were more prevalent. F. prausnitzii, for example, was undetectable in patients with three complications and relatively reduced in patients with AKI, hemodialysis, ARDS, cardiac event and was negatively correlated with mortality. This bacterium has anti-inflammatory propertiesCitation36,Citation37 and was found to have an inverse correlation with disease severity in COVID-19.9,Citation10 On the other hand, the relative abundance of the genus Alistipes was increased with the number of complications. In terms of functionality, there is conflicting evidence to the protective or pathogenic potential of Alistipes in various diseases, which could be due to different strains present.Citation38 In patients with thromboembolic complications the genus Tyzzerella was the only significantly elevated bacterium. Interestingly, Tyzzerella was previously shown to be associated with an increased risk of cardiovascular diseases.Citation39 Parabacteroides was increased in patients with ARDS and hemodialysis and related to mortality. The associations of individual bacteria with the occurrence of complications suggest a potential role of the gut microbiota in the development of specific complications within COVID-19 and provide additional evidence for an involvement of the gut concerning cardiovascular riskCitation40 and venous thromboembolism.Citation41,Citation42
In addition, differences in the bacterial composition were found dependent on the disease severity. While the microbial profile of patients with mild diseases was comparable to controls, severe and fatal cases showed marked differences with respect to protective bacteria. Congruent with previously published studies in other countries,Citation1,Citation9,Citation10,Citation43 our results confirm a link between disease severity of COVID-19 and microbiota alterations in a large German cohort. Besides an inverse correlation of F. prausnitzii with disease severity of COVID-19Citation10, Blautia was previously shown to be underrepresented in patients with COVID-19 and was associated with SARS-CoV-2 recovery.Citation9 Fusicatenibacter was reported to be enriched in non COVID-19 controlsCitation43 and correlated negatively with inflammatory biomarkers in COVID-19 patientsCitation44 and Parabacteroides correlated positively with disease severity.Citation9
To more deeply examine the associations of the gut bacteria with COVID-19 progression, we considered functional data, such as FiO2, at each time of stool collection. Thereby, the intra-individual microbial stability decreased with a higher complication rate. Based on a distinct microbial profile, the individual risk of mortality due to COVID-19 could be estimated. Thus, while disease severity, inflammatory activity, and complication rate were associated with changes in bacterial composition in COVID-19 patients, the impact of SARS-CoV-2 infection appears to be more modest, indicating that the gut plays a role in shaping severe disease progression. However, it needs to be highlighted that the current model has constraints due to the limited number of cases and controls and thus should be handled as a risk indicator and not used as a predictor.
Regarding the microbiota changes in the oral cavity, differences in bacterial composition related to severity and complications were observed, highlighting the importance of the bacterial oro-intestinal axis in COVID-1931. However, prediction of mortality was not feasible using bacterial patterns in saliva and the results were less conclusive compared to changes in the gut microbiota.
We hypothesize that changes in the microbial composition, especially of the gut, may drive disease, possibly via an involvement in the development of complications. A stable bacterial profile during hospitalization could have a favorable impact on disease progression. A healthy and diverse intestinal microbiota should, therefore, be considered in the therapeutic management of COVID-19.
Because of the often prolonged hospital stay of inpatients of 24 days on average within our cohort, multiple factors could influence the gut microbiota. These include formulated food, antibiotics, or catabolic metabolism during an ICU stay.Citation45 Especially in a clinically heterogeneous disease like COVID-19, these factors must be considered in the interpretation of microbiota analysis. For this reason, we carefully reviewed the results for potential confounders, including concomitant diseases and assessable factors associated with hospitalization. In this context, none of the factors examined was found to be a confounder with significant bias concerning our results. Nevertheless, patients with a severe and complicating disease, in contrast to mild cases, were mainly treated at the ICU and given antibiotics (Supplementary Table 4). Thus, it cannot be ruled out that microbiota changes related to the severity and complications are also influenced by the conditions of medical treatment. It further remains unclear whether the changes in microbiota causally influenced the severity of COVID-19 and occurrence of complications, or vice versa.
Taken together, our results suggest that the gut and salivary microbiota are associated with the occurrence of individual complications in COVID-19, thereby influencing disease severity. A stable gut bacterial composition during hospitalization is associated with a more favorable clinical course. Further studies are needed to investigate direct causality between gut bacterial dysbiosis and COVID-19 and to integrate microbial patterns for prognostic and therapeutic purposes in clinical routine.
Abbreviations
| all T | = | All biosamples of all timepoints |
| AB T1 | = | Antibiotic therapy at the time of the first stool sampling |
| AC | = | Asymptomatic controls |
| AKI | = | Acute kidney injury |
| AP | = | Alkaline phosphatase [U/l] |
| ARDS | = | Acute respiratory distress syndrome |
| Asympt. | = | Asymptomatic |
| COVID-19 | = | Corona virus disease 2019 |
| CRP | = | C-reactive protein [mg/dl] |
| FiO2 | = | Fraction of inspired oxygen (%) |
| GGT | = | Gamma-glutamyltransferase [U/l] |
| GI | = | Gastrointestinal |
| Hb | = | Hemoglobin [g/dl] |
| i.v. | = | Intravenous |
| IBD | = | Inflammatory bowel disease |
| ICU | = | Intensive care unit |
| ICU all T | = | Intensive care stay regarding all time points of stool sampling |
| ICU T1 | = | Intensive care stay at the time of the first stool sampling |
| N | = | Number of patients |
| n | = | Number of samples |
| NA | = | Not available |
| PA | = | Pressure assisted |
| PC | = | Pressure controlled |
| PCT | = | Procalcitonin [ng/ml] |
| PE | = | Pulmonary embolism |
| Rel. | = | Relativ |
| S.p. | = | Status post |
| SARS-CoV-2 | = | Severe acute respiratory syndrome coronavirus 2 |
| SC | = | Symptomatic pneumonia controls |
| Sig. | = | Significant |
| Sympt. | = | Symptomatic |
| T1 | = | Biosample of the first sampling time point only |
| T2-12 | = | Biosamples of consecutive sampling points,starting from T1 |
| T2D | = | Type 2 diabetes mellitus |
| Trp T | = | High-sensitive troponin T [ng/ml] |
| TS | = | Tracheostomy |
| VTE | = | Venous thromboembolism |
| WBC | = | White blood cell counts [G/l] |
| zOTU | = | Zero-radiation operational-taxonomic units |
Authorship contributions
David Schult, Dr. (Conceptualization: Lead; Project administration: Lead; Supervision: Lead; Investigation: Equal; Methodology: Lead; Visualization: Supporting; Validation: Equal; Manuscript – writing: Lead, Manuscript – review & editing: Lead), Sandra Reitmeier, Dr. (Conceptualization: Equal; Project administration: Equal; Investigation: Equal; Methodology: Lead; Visualization: Lead; Validation: Equal; Manuscript – writing: Lead, Manuscript – review & editing: Lead; Formal analysis: Lead), Plamena Koyumdzhieva (Conceptualization: Equal; Investigation: Lead; Methodology: Supporting; Visualization: Supporting; Validation: Equal; Manuscript – writing: Equal, Manuscript – review & editing: Supporting), Tobias Lahmer, Dr., Johanna Erber, Dr., Marina Frolova, Julia Horstmann, Lisa Fricke, Juliane Kager, Katja Steiger, Dr., Moritz Jesinghaus, Prof. Dr. (Investigation: Supporting), Moritz Middelhoff, Dr., Jochen Schneider, Dr. (Conceptualization: Supporting), Klaus-Peter Janssen, Prof. Dr. (Resources: Supporting; Manuscript – review & editing: Supporting), Ulrike Protzer, Prof. Dr. (Resources: Supporting), Klaus Neuhaus, Dr. (Resources: Equal; Validation: Supporting; Manuscript – review & editing: Equal), Roland M. Schmid, Prof. Dr. (Resources: Equal; Funding acquisition: Equal), Dirk Haller, Prof. Dr. (Conceptualization: Supporting, Resources: Equal; Validation: Supporting; Funding acquisition: Equal Manuscript – review & editing: Equal), Michael Quante, Prof. Dr. (Conceptualization: Lead; Project administration: Equal; Supervision: Lead; Funding acquisition: Lead; Manuscript – review & editing: Lead).
Data Availability and Data Transparency Statement
FASTQ files of the 16S rRNA gene sequencing is available under SRA accession number PRJNA756849 (https://www.ncbi.nlm.nih.gov/bioproject/PRJNA756849/).
Supplemental Material
Download Zip (5.2 MB)Acknowledgments
We thank all the healthcare workers of Klinikum rechts der Isar as well as the CoMRI team around Christoph Spinner, MD. We are grateful to Angela Sachsenhauser, Caroline Ziegler and Lukas Mix from the Core Facility Microbiome of the ZIEL Institute for Food & Health for outstanding technical support in sample preparation and 16S rRNA gene amplicon sequencing.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Zuo T, Liu Q, Zhang F, Lui GC, Tso EY, and Yeoh YK, et al. Depicting SARS-CoV-2 faecal viral activity in association with Gut Microbiota composition in patients with COVID-19. Gut 2021. 70:276–15. doi:10.1080/19490976.2020.1747329
- Liang W, Feng Z, Rao S, Xiao C, Xue X, Lin Z, et al. Diarrhoea may be underestimated: a missing link in 2019 novel coronavirus. Gut. 2020;69:1141–1143.
- Cheung KS, Hung IFN, Chan PPY, Lung KC, Tso E, Liu R, et al. Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples From a Hong Kong Cohort: systematic Review and Meta-analysis. Gastroenterology. 2020;159:81–95.
- Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): a Review. Jama. 2020;324:782–793.
- Mao R, Qiu Y, He JS, Tan JY, Li XH, Liang J, et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5:667–678.
- Lamers MM, Beumer J, van der Vaart J, Knoops K, Puschhof J, Breugem TI, et al. SARS-CoV-2 productively infects human gut enterocytes. Science. 2020;369:50–54.
- Xu Y, Li X, Zhu B, Liang H, Fang C, Gong Y, et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020;26:502–505.
- Jin X, Lian JS, Hu JH, Gao J, Zheng L, Zhang YM, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69:1002–1009.
- Zuo T, Zhang F, Lui GCY, Yeoh YK, Ayl L, Zhan H, et al. Alterations in Gut Microbiota of Patients With COVID-19 During Time of Hospitalization. Gastroenterology. 2020;159:944–55 e8.
- Yeoh YK, Zuo T, Lui GC, Zhang F, Liu Q, Li AY, et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut 2021. 70:698–706.
- Middeldorp S, Coppens M, van Haaps TF, Foppen M, Vlaar AP, Muller MCA, et al. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020;18:1995–2002.
- Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147.
- Alhazzani W, Moller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020;46:854–887.
- Legrand M, Bell S, Forni L, Joannidis M, Koyner JL, Liu K, et al. Pathophysiology of COVID-19-associated acute kidney injury. Nat Rev Nephrol. 2021.
- Brodin P. Immune determinants of COVID-19 disease presentation and severity. Nat Med. 2021;27:28–33.
- Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2021;19:141–154.
- Kosiewicz MM, Zirnheld AL, Alard P. Gut microbiota, immunity, and disease: a complex relationship. Front Microbiol. 2011;2:180.
- Schirmer M, Smeekens SP, Vlamakis H, Jaeger M, Oosting M, Franzosa EA, et al. Linking the Human Gut Microbiome to Inflammatory Cytokine Production Capacity. Cell. 2016;167:1125–36 e8.
- Rothschild D, Weissbrod O, Barkan E, Kurilshikov A, Korem T, Zeevi D, et al. Environment dominates over host genetics in shaping human gut microbiota. Nature. 2018;555:210–215.
- Kau AL, Ahern PP, Griffin NW, Goodman AL, Gordon JI. Human nutrition, the gut microbiome and the immune system. Nature. 2011;474:327–336.
- McDonald D, Ackermann G, Khailova L, Baird C, Heyland D, Kozar R, et al. Extreme Dysbiosis of the Microbiome in Critical Illness. mSphere 2016; 1.
- Health Organization R W, Blueprint D. COVID-19 Therapeutic Trial Synopsis, http://www.who.int/blueprint/priority-diseases/key-action/novel-coronavirus/en/ (Accessed August 11, 2021).
- Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N Engl J Med. 2020;382:1787–1799.
- Reitmeier S, Kiessling S, Neuhaus K, Haller D. Comparing Circadian Rhythmicity in the Human Gut Microbiome. Vol. 1, STAR Protoc; 2020. p. 100148.
- Edgar RC, Flyvbjerg H. Error filtering, pair assembly and error correction for next-generation sequencing reads. Bioinformatics. 2015;31:3476–3482.
- Reitmeier S, Kiessling S, Clavel T, List M, Almeida EL, Ghosh TS, et al. Arrhythmic Gut Microbiome Signatures Predict Risk of Type 2 Diabetes. Cell Host Microbe. 2020;28:258–72 e6.
- Qin J, Li Y, Cai Z, Li S, Zhu J, Zhang F, et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature. 2012;490:55–60.
- Franzosa EA, Sirota-Madi A, Avila-Pacheco J, Fornelos N, Haiser HJ, Reinker S, et al. Gut microbiome structure and metabolic activity in inflammatory bowel disease. Nat Microbiol. 2019;4:293–305.
- Gopalakrishnan V, Helmink BA, Spencer CN, Reuben A, Wargo JA. The Influence of the Gut Microbiome on Cancer, Immunity, and Cancer Immunotherapy. Cancer Cell. 2018;33:570–580.
- Agnes A, Puccioni C, D’Ugo D, Gasbarrini A, Biondi A, Persiani R. The gut microbiota and colorectal surgery outcomes: facts or hype? A narrative review. BMC Surg. 2021;21:83.
- Ren Z, Wang H, Cui G, Lu H, Wang L, Luo H, et al. Alterations in the human oral and gut microbiomes and lipidomics in COVID-19. Gut 2021. 70:1253–1265.
- Xie Y, Bowe B, Maddukuri G, Al-Aly Z. Comparative evaluation of clinical manifestations and risk of death in patients admitted to hospital with covid-19 and seasonal influenza: cohort study. Bmj. 2020;371:m4677.
- Atarashi K, Tanoue T, Ando M, Kamada N, Nagano Y, Narushima S, et al. Th17 Cell Induction by Adhesion of Microbes to Intestinal Epithelial Cells. Cell. 2015;163:367–380.
- Honda K, Littman DR. The microbiota in adaptive immune homeostasis and disease. Nature. 2016;535:75–84.
- Mortha A, Chudnovskiy A, Hashimoto D, Bogunovic M, Spencer SP, Belkaid Y, et al. Microbiota-dependent crosstalk between macrophages and ILC3 promotes intestinal homeostasis. Science. 2014;343:1249288.
- Sokol H, Pigneur B, Watterlot L, Lakhdari O, Bermudez-Humaran LG, Gratadoux JJ, et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc Natl Acad Sci U S A. 2008;105:16731–16736.
- Lopez-Siles M, Duncan SH, Garcia-Gil LJ, Martinez-Medina M. Faecalibacterium prausnitzii: from microbiology to diagnostics and prognostics. ISME J. 2017;11:841–852.
- Parker BJ, Wearsch PA, Veloo ACM, Rodriguez-Palacios A. The Genus Alistipes: gut Bacteria With Emerging Implications to Inflammation, Cancer, and Mental Health. Front Immunol. 2020;11:906.
- Kelly TN, Bazzano LA, Ajami NJ, He H, Zhao J, Petrosino JF, et al. Gut Microbiome Associates With Lifetime Cardiovascular Disease Risk Profile Among Bogalusa Heart Study Participants. Circ Res. 2016;119:956–964.
- Wang Z, Klipfell E, Bennett BJ, Koeth R, Levison BS, Dugar B, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature. 2011;472:57–63.
- Liu Y, Dai M. Trimethylamine N-Oxide Generated by the Gut Microbiota Is Associated with Vascular Inflammation: new Insights into Atherosclerosis. Mediators Inflamm. 2020;2020:4634172.
- Roberts AB, Gu X, Buffa JA, Hurd AG, Wang Z, Zhu W, et al. Development of a gut microbe-targeted nonlethal therapeutic to inhibit thrombosis potential. Nat Med. 2018;24:1407–1417.
- Newsome RC, Gauthier J, Hernandez MC, Abraham GE, Robinson TO, Williams HB, et al. The gut microbiome of COVID-19 recovered patients returns to uninfected status in a minority-dominated United States cohort. Gut Microbes. 2021;13:1–15.
- Gu S, Chen Y, Wu Z, Chen Y, Gao H, Lv L, et al. Alterations of the Gut Microbiota in Patients With Coronavirus Disease 2019 or H1N1 Influenza. Clin Infect Dis. 2020;71:2669–2678.
- Otani S, Chihade DB, Coopersmith CM. Critical illness and the role of the microbiome. Acute Med Surg. 2019;6:91–94.
