ABSTRACT
Background: The COVID-19 pandemic is a health emergency resulting in multiple stressors that may be related to posttraumatic stress disorder (PTSD).
Objective: This study examined relationships between risk and protective factors, pandemic-related stressors, and PTSD during the COVID-19 pandemic.
Methods: Data from the European Society of Traumatic Stress Studies (ESTSS) ADJUST Study were used. N = 4,607 trauma-exposed participants aged 18 years and above were recruited from the general populations of eleven countries (Austria, Croatia, Georgia, Germany, Greece, Italy, Lithuania, the Netherlands, Poland, Portugal, and Sweden) from June to November 2020. We assessed sociodemographic (e.g. gender), pandemic-related (e.g. news consumption), and health-related (e.g. general health condition) risk and protective factors, pandemic-related stressors (e.g. fear of infection), and probable PTSD (PC-PTSD-5). The relationships between these variables were examined using logistic regression on multiple imputed data sets.
Results: The prevalence of probable PTSD was 17.7%. Factors associated with an increased risk for PTSD were younger age, female gender, more than 3 h of daily pandemic-related news consumption (vs. no consumption), a satisfactory, poor, or very poor health condition (vs. a very good condition), a current or previous diagnosis of a mental disorder, and trauma exposure during the COVID-19 pandemic. Factors associated with a reduced risk for PTSD included a medium and high income (vs. very low income), face-to-face contact less than once a week or 3–7 times a week (vs. no contact), and digital social contact less than once a week or 1–7 days a week (vs. no contact). Pandemic-related stressors associated with an increased risk for PTSD included governmental crisis management and communication, restricted resources, restricted social contact, and difficult housing conditions.
Conclusion: We identified risk and protective factors as well as stressors that may help identify trauma-exposed individuals at risk for PTSD, enabling more efficient and rapid access to care.
HIGHLIGHTS
N = 4,607 trauma-exposed adult participants were recruited from the general population during the first year of the COVID-19 pandemic.
The prevalence for probable posttraumatic stress disorder was 17.7%.
We identified risk factors (e.g. poor health condition) and protective factors (e.g. social contact) associated with posttraumatic stress disorder.
Antecedentes: La pandemia COVID-19 es una emergencia sanitaria que genera múltiples estresores que pueden estar relacionados con el trastorno de estrés postraumático (TEPT).
Objetivo: Este estudio examinó las relaciones entre los factores de riesgo y protectores, estresores relacionados con la pandemia y TEPT durante la pandemia de COVID-19.
Métodos: Se utilizaron los datos del estudio ADJUST de la Sociedad Europea de Estudios de Estrés Traumático (ESTSS por sus siglas en ingles). N=4.607 participantes mayores de 18 años expuestos a trauma fueron reclutados de la población general de once países (Austria, Croacia, Georgia, Alemania, Grecia, Italia, Lituania, Países Bajos, Polonia, Portugal y Suecia) desde junio a noviembre 2020. Evaluamos factores de riesgo y protectores sociodemográficos (p.ej. género), relacionados con la pandemia (p.ej. consumo de noticias) y relacionados con la salud (p.ej. estado de salud general), estresores relacionados con la pandemia (p.ej. temor a la infección) y TEPT probable (PC-PTSD-5 por sus siglas en ingles). Las relaciones entre estas variables se examinaron mediante regresión logística en múltiples conjuntos de datos imputados.
Resultados: La prevalencia de TEPT probable fue del 17.7%. Los factores asociados con un mayor riesgo de TEPT fueron edad más joven, sexo femenino, más de 3 horas de consumo diario de noticias relacionadas con la pandemia (frente a ningún consumo), un estado de salud satisfactorio, malo o muy malo (frente a un estado muy bueno), un diagnóstico de trastorno mental actual o previo y exposición a un trauma durante la pandemia de COVID-19. Los factores asociados con un riesgo reducido de TEPT incluyeron ingresos medios y altos (frente a ingresos muy bajos), contacto cara a cara menos de una vez a la semana o de 3 a 7 veces por semana (frente a ningún contacto) y contacto social digital menos de una vez a la semana o de 1 a 7 días a la semana (frente a ningún contacto). Los estresores relacionados con la pandemia asociados con un mayor riesgo de TEPT incluyeron la gestión y comunicación de crisis gubernamental, recursos restringidos, contacto social restringido y condiciones de vivienda difíciles.
Conclusiones: Identificamos factores de riesgo y protectores, así como estresores que pueden ayudar a identificar a las personas expuestas a traumas en riesgo de TEPT, lo que permite un acceso más eficiente y rápido a la atención.
背景:COVID-19 疫情是一种健康紧急情况,导致可能与创伤后应激障碍 (PTSD) 相关的多种应激源。
目的:本研究考查了 COVID-19 疫情期间风险和保护因素、疫情相关应激源和 PTSD 之间的关系。
方法:使用来自欧洲创伤应激研究协会 (ESTSS) ADJUST 研究的数据。从2020年 6 月至 11 月,从 11 个国家(奥地利、克罗地亚、格鲁吉亚、德国、希腊、意大利、立陶宛、荷兰、波兰、葡萄牙和瑞典)的一般人群中招募了 4,607 名 18 岁及以上的创伤暴露参与者。我们评估了社会人口学(如性别)、疫情相关(如新闻使用)和健康相关(如一般健康状况)风险和保护因素、疫情相关应激源(如对感染的恐惧),以及可能的PTSD(PC-PTSD-5)。对多重插补数据集使用逻辑回归考查这些变量之间的关系。
结果:可能的 PTSD 流行率为 17.7%。与 PTSD 风险增加相关的因素包括年龄较小、女性、每天超过 3 小时的疫情相关新闻使用(相对于不使用)、令人满意、差或非常差的健康状况(相对于非常好的状况)、当前或以前的精神障碍诊断以及 COVID-19 疫情期间的创伤暴露。与 PTSD 风险降低相关的因素包括中等和高收入(相对于极低收入)、每周少于一次或每周 3-7 次(相对于无联系)的面对面联系以及电子社交联系少于一次或每周 1-7 天(相对于不联系)。与 PTSD 风险增加相关的疫情相关应激源包括政府危机管理和沟通、资源受限、社会联系受限和住房条件困难。
结论:我们确定了可能有助于识别有PTSD风险创伤暴露个体的风险和保护因素以及应激源,使得更有效、更快速的护理成为可能。
1. Introduction
With the global COVID-19 pandemic, Europe has faced one of the most significant challenges in decades, with unique and devastating impacts on whole populations. It has caused multiple stressors, illnesses, deaths, and strain on healthcare and economic systems. In a recent study conducted during the early phase of the COVID-19 pandemic, the researchers found that most participants (75%) found the pandemic to be very stressful (Dragan et al., Citation2021). People were afraid of contracting COVID-19, were burdened by the COVID-19 disease, or suffered from physical distancing and quarantine (Dragan et al., Citation2021).
In addition to the multiple pandemic-specific stressors, a subset of people were exposed to potentially traumatic events, such as natural disasters or unnatural death (American Psychiatric Association, Citation2013). In the case of the COVID-19 pandemic, hospitalisation for a COVID-19 infection or the death of loved ones due to COVID-19 may qualify as traumatic events according to DSM-5 PTSD criteria. After exposure to such severe events, individuals are at risk for developing symptoms of posttraumatic stress disorder (PTSD). PTSD is characterised by re-experiencing the traumatic event, avoidance of thoughts of the traumatic event(s), negative alterations in cognitions and mood such as fear, guilt, or shame, and heightened physiological arousal (American Psychiatric Association, Citation2013). Symptoms of PTSD usually emerge within 3 months of the stressor and can cause significant impairment in personal, family, social, educational, and occupational functioning (American Psychiatric Association, Citation2013). With its cascading chronic effects, some experts have viewed the COVID-19 pandemic itself as a collective trauma that may lead to PTSD (Kendall-Tackett, Citation2020; Kira et al., Citation2021; Masiero et al., Citation2020). An infectious disease pandemic causes continuous threats to safety and health that might be perceived as even more severe than other types of trauma due to its uncontrollability and invisibility (Kira et al., Citation2021).
During the COVID-19 pandemic, biological (e.g. gender, age, COVID-19 infection), psychological (e.g. previous mental disorder), and social (e.g. living and working conditions) risk and protective factors may buffer or deepen the effects of the pandemic-related stressors on mental health (Lotzin et al., Citation2020). However, knowledge about which of these risk factors are related to PTSD in European populations is scarce (Rajkumar, Citation2020). A recently published meta-analysis including studies from Asian, American and European countries found that older age and working in COVID-19 health care were risk factors associated with higher levels of PTSD symptoms during the pandemic (Yunitri et al., Citation2022). However, heterogeneous measures and designs of the included studies made it difficult to integrate and compare the research findings. A study conducted in the Italian general population (Rossi et al., Citation2020) found that female gender, younger age, exposure to stressful life events, discontinued work due to COVID-19, quarantine due to infection and close proximity to infected people were associated with higher PTSD symptom levels. A larger study assessing a wide range of relevant risk and protective factors and their associations with PTSD including different European countries could further elucidate these relationships.
This exploratory study aimed to examine cross-sectional relationships between risk and protective factors, stressors, and probable PTSD during the first year of the COVID-19 pandemic in eleven European countries. We hypothesised that the assessed risk factors and stressors would be associated with an increased risk for probable PTSD, while the assessed protective factors would be associated with a reduced risk for PTSD. The gained knowledge from these relationships could inform public health strategies to promote recovery from pandemic-related stressors.
2. Methods
2.1. Study design and setting
Data of this study stem from the first wave of the European Society of Traumatic Stress Studies (ESTSS) pan-European study, named ‘ADJUST study’ (Lotzin et al., Citation2020). The ADJUST study investigates longitudinal associations between risk and protective factors, stressors, and symptoms of adjustment disorder and PTSD during the COVID-19 pandemic in eleven European countries (Austria, Croatia, Georgia, Germany, Greece, Italy, Lithuania, the Netherlands, Poland, Portugal, Sweden). The cross-sectional results on symptoms of adjustment disorder are reported elsewhere (Lotzin, Krause, et al., Citation2021).
2.2. Participants
We recruited participants from the general populations of the eleven countries that participated in the ADJUST study (see above). Inclusion criteria for this data analysis were (1) Trauma exposure before and/or during the COVID-19 pandemic according to DSM-5 PTSD criteria, assessed with the Live Events Checklist (LEC-5) of the PTSD Checklist for DSM-5 (PCL-5; Weathers et al., Citation2013), (2) at least 18 years of age, (3) ability to read and write in the respective language, and (4) willingness to participate in the study.
2.3. Procedure
Participants were recruited from June to November 2020. Recruitment was predominantly done online, given that face-to-face contact was restricted during the pandemic. To increase the variability of the sample in terms of gender, age, and education, we used a broad range of different recruitment strategies. The study was promoted via social networks (e.g. Facebook), newsletters of leisure and interest groups as well as large companies, and advertisements in newspapers and magazines. The study information was circulated through universities, stakeholders, and professional organisations, and distributed via printed flyers in public venues. A detailed description of the recruitment strategy for each country can be found elsewhere (Lotzin, Krause, et al., Citation2021). Individuals interested in study participation received an invitation to participate by a website link.
2.4. Measures
2.4.1. PTSD symptoms
Symptoms of PTSD were assessed using the Primary Care PTSD Screen for DSM-5 (PC-PTSD-5; Prins et al., Citation2015). The PC-PTSD-5 is a brief 5-item screening measure to assess the risk for PTSD according to DSM-5. Respondents rate on dichotomous items whether the respective PTSD symptom was experienced within the last month (0 = no; 1 = yes). The total PC-PTSD-5 score is obtained by summing the scores of the five items. A cut-off score of >3 indicates probable PTSD. The PC-PTSD-5 is based on the PTSD-4, a widely used screening measure for PTSD according to DSM-IV that has shown sound psychometric characteristics in community settings (Spoont et al., Citation2015). The PC-PTSD-5 has demonstrated good to excellent diagnostic accuracy (Prins et al., Citation2015) and is well-validated against the Clinician-Administered DSM-5 scale for PTSD (Bovin et al., Citation2021).
2.4.2. Risk and protective factors
We used the WHO framework for social determinants of health (Solar & Irwin, Citation2010) to select risk and protective factors, which we adapted for the specific context of the COVID-19 pandemic (Lotzin et al., Citation2020). We assessed sociodemographic (), pandemic-related (), and health-related () potential risk and protective factors. As there were no validated measures available, items were self-constructed. Trauma exposure before and during the COVID-19 pandemic was assessed using the LEC of the PCL-5 (Weathers et al., Citation2013).
Table 1. Sociodemographic characteristics (N = 4607).
Table 2. Pandemic-related characteristics (N = 4607).
Table 3. Health-related characteristics (N = 4607)
On the basis of previous research (Xiong et al., Citation2020; Yunitri et al., Citation2022), we hypothesised that the following variables would be related to an increased risk for probable PTSD: younger age, female gender (vs. male gender), being in training or study, very low or low income, reduced income due to the pandemic, and working in an area with an increased risk for a COVID-19 infection (e.g. healthcare, public security); spending more time at home due to the pandemic (e.g. due to quarantine), longer duration of daily pandemic-related news consumption; trauma exposure during or before the pandemic, a current or previous mental disorder, a COVID-19 infection, being at risk for a severe COVID-19 disease, a perceived poor or very poor health status, and a perceived high risk for severe COVID-19. We hypothesised the following variables to be related to a lower risk for probable PTSD: perceived good or very good health status; male gender, medium or high income, governmental financial support; face-to-face contact with loves ones or friends, and digital contact with loves ones or friends.
2.4.3. Burden of pandemic-related stressors
The burden of pandemic-related stressors was assessed by a self-constructed 30-item questionnaire, the Pandemic Stressor Scale (Lotzin et al., Citation2022). The PaSS measures the burden of pandemic-related stressors in nine domains (Restricted social contact; Problems with childcare; Work-related problems; Fear of infection; Restricted activity; Crisis management and communication; Restricted access to resources, Difficult housing conditions; and Burden of infection) on four-point scales ranging from 0 to 3 (0 = ‘Not at all burdened’; 1 = ‘Somewhat burdened’; 2 = ‘Moderately burdened’; 3 = ‘Strongly burdened). Participants were asked to indicate for each stressor how much it has burdened them due to the COVID-19 pandemic within the last month. The subscale scores are the average of the item scores that belong to the respective scale. The PaSS has shown first evidence for its factorial validity and reliability (Lotzin et al., Citation2022).
2.4.4. Stringency and country differences
To adjust for possible differences in the strictness of lockdown policies during the COVID-19 pandemic, the Oxford stringency index (https://ourworldindata.org/covid-stringency-index) was registered for the day of the data assessment for each participant. For Croatia, the stringency index from the start date of the assessment period was chosen, as individual assessment dates were not available.
To adjust for between-country differences, a variable indicating the respective country was computed.
2.5. Data analysis
We did not conduct a priori sample size calculation for the analysis reported in this manuscript, as the power calculation was designed for the larger longitudinal study (Lotzin et al., Citation2020). In this analysis, we examined a logistic regression model with 76 predictors. Following the sample size calculation for multivariable prediction modelling proposed by Riley et al. (Citation2019), a sample size of N = 4169 would be sufficient to calculate a model with 76 candidate predictors assuming a Cox–Snell R2 of 0.15 which we found in our model. Hence, our study seems adequately powered with a sample size of N = 4607.
We computed a logistic regression model which included the dichotomised PTSD values (PC-PTSD-5; probable PTSD vs. no PTSD diagnosis) as the dependent variable. As independent variables, the defined risk and protective factors and the nine PaSS stressor subscales were included in the analysis. To adjust our analysis for stringency and country, these two variables were also included in our model. To enable comparable interpretations of the effect sizes of the continuous variables, those variables were scaled to a mean of zero and a standard deviation of one before including them in the regression models.
Missing values of all independent variables were imputed using multiple imputation following the guidelines by White and colleagues (Citation2011). We checked multicollinearity using the generalised variance inflation factor, as well as the linearity assumption by plotting the logit of the outcome versus each continuous predictor variable and assessing these plots for linearity visually. We did not find any indications for violations of these assumptions. As this is an exploratory study, p-values were not adjusted for multiplicity. Descriptive statistics were computed for all variables that were used in the regression model for the whole sample as well as stratified by country. Mean and standard deviation or median and interquartile range were computed, as appropriate, for the continuous variables; absolute and relative frequencies were computed for categorical variables. All analyses were conducted with R-3.5.3 for Windows.
3. Results
3.1. Sample characteristics
Our sample of trauma-exposed individuals drawn from the general population can be characterised as high-educated with varying ages and incomes (). About six out of seven participants stated to have spent more time at home due to the COVID-19 pandemic (). On average, participants spent about 5 h per day outside their homes. The prevalence of probable PTSD was 17.7% (). 87.6% reported trauma exposure before the COVID-19 pandemic, 23.2% reported trauma exposure during the COVID-19 pandemic.
Burden related to the pandemic-stressors were highest for fear of infection, followed by, restricted activity and restricted social contact ().
Table 4. Pandemic-related stressors (N = 4607).
3.2. Risk factors for PTSD
Increased risk for probable PTSD was related to the following variables (see for a graphical presentation and for effect estimates and p-values): younger age, female gender, more than 3 h of daily pandemic-related news consumption (vs. no pandemic-related news consumption), a satisfactory, poor or very poor health condition (vs. a very good health condition), a current or previous diagnosis of a mental disorder, and trauma exposure during the COVID-19 pandemic.
Figure 1. Effect estimates of regression analysis.
Notes. Effect estimates are unstandardised regression coefficients. Reference categories: a Male. b Less than 10 years of schooling. c Very low. d No. e No. f Other. g No. h No personal contact with other people. i No contact by phone, skype, etc. j I do not watch, read or listen to news about the coronavirus pandemic. k Very good. l No. m No. n No. o No. ≥ 10 years = 10 or more years of schooling. Reduced income = Reduced monthly household income due to the coronavirus. Financial support = Receiving financial support from the government. Maintenance/repair/etc.= Maintenance, repair, construction. More at home = Spent more time at home due to the coronavirus pandemic. social dist. = Spent more time at home as a precautionary measure (social distancing). Self-isolation = Stayed at home in self-isolation because of self-infection. quarantine = Stayed at home due to contact with infected people or being in risk areas. Face contact = Face-to-face contact to loved ones or friends. Face contact at work = Work involve (almost) daily face-to-face contact with other people. Digital contact = Digital contact with loved ones or friends, e.g. by phone, Skype or Zoom. News = Hours a day watching, reading or listening to news or other information about the coronavirus pandemic. COVID-19 inf. = Infected (i.e. tested positive) with the coronavirus.
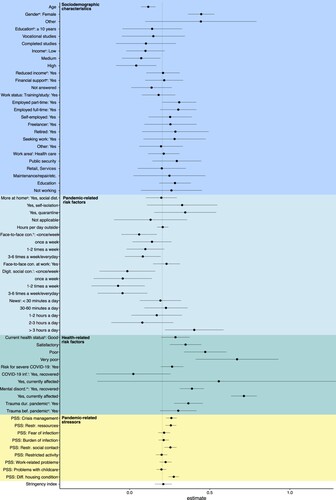
Table 5. Effect estimates of regression analysis (N = 4607).
3.3. Protective factors for PTSD
Reduced risk for probable PTSD was associated with the following factors: medium and high income (vs. very low income), face-to-face contact of less than once a week or 3–7 times a week (vs. no face-to-face contact), and digital social contact less than once a week or 1–7 days a week (vs. no digital social contact).
3.4. Burden of pandemic stressors related to PTSD
Out of the nine assessed pandemic stressor domains, four domains were significantly related to an increased risk for probable PTSD (, ). These included ‘Governmental crisis management and communication’, ‘Restricted Resources’, ‘Restricted social contact’, and ‘Difficult housing conditions.’ The five remaining stressor domains ‘Fear of Infection’, ‘Burden of infection’, Restricted activity’, ‘Work-related problems’, and ‘Problems with childcare’ were unrelated to the risk for probable PTSD.
We did not find an association between the stringency (i.e. the strictness of lockdown policies) and the risk for probable PTSD. Between-country differences in the risk for probable PTSD were only found for one country (Greece; ), which showed an increased risk for probable PTSD.
4. Discussion
This study examined the relationships between risk and protective factors, stressors, and probable PTSD in individuals exposed to a traumatic event from the general population of eleven countries in the first year of the COVID-19 pandemic. In our sample of N = 4607 trauma-exposed participants, we found a prevalence rate for probable PTSD of 17.7%. The found prevalence rate is consistent with the results of recent meta-analyses on Asian, American, and European general population studies during the COVID-19 pandemic, which found pooled prevalence rates ranging between 17.3% and 21% (Cénat et al., Citation2021; Salehi et al., Citation2021; Yunitri et al., Citation2022). Different phases of the pandemic might be related to different severity and chronicity of stressor exposure and therefore associated with different PTSD prevalence rates. Government stringency (i.e. extent, severity, and duration of social restriction measures) might be another factor contributing to different PTSD prevalence rates, as it could be related to risk (e.g. high COVID-19 incidence rates) and protective factors (e.g. social support). However, our study showed that stringency was unrelated to the risk for probable PTSD. Differences in healthcare provision and quality, as well as cultural views on the adequacy of reporting mental health problems in surveys might be additional factors impacting PTSD prevalence rates.
Overall, the general population studies conducted so far during the COVID-19 pandemic (Cénat et al., Citation2021; Salehi et al., Citation2021; Yunitri et al., Citation2022), as well as this study on trauma-exposed individuals from the general population, are consistent in reporting high proportions of the individuals scoring above the at-risk threshold for PTSD.
4.1. Risk factors for PTSD symptoms
4.1.1. Sociodemographic risk factors
Younger age was related to an increased risk for probable PTSD in our study, in line with earlier research showing that an age younger than 30 was related to higher PTSD symptom levels (Yuan et al., Citation2021). Younger people might be disproportionally affected by the COVID-19 pandemic because of closure of schools, universities and other support services, and the reduced peer contact and social activities (Conrad et al., Citation2021).
Female gender was associated with an increased risk for probable PTSD. This finding is consistent with earlier general population studies conducted during the COVID-19 pandemic (Brotto et al., Citation2021; Rossi et al., Citation2020). Women have been found to be at higher risk for developing PTSD compared to men; this difference has been linked to both biological and psychosocial factors (Olff, Citation2017). In contrast to our results, a meta-analysis (Yuan et al., Citation2021) did not find significant differences in PTSD prevalence rates between females and males, although women showed higher prevalence rates descriptively.
4.1.2. Pandemic-related risk factors
More than 3 h of daily news consumption about COVID-19 was related to an increased risk for probable PTSD. Earlier research conducted during the pandemic found associations between the duration of COVID-19-related media consumption and higher levels of symptoms of depression and anxiety (Bendau et al., Citation2021). Frequent social media consumption may increase anxiety due to potential misinformation about the risks.
4.1.3. Health-related risk factors
A perceived satisfactory, poor, or very poor health condition was linked to an increased risk for probable PTSD. Interestingly, not only perceived poor health but also satisfactory health (vs. very good health) was associated with an increased risk. Pre-pandemic research documented relationships between physical health and increased PTSD symptom levels (Ryder et al., Citation2018).
Another risk factor for probable PTSD was a current or previous diagnosis of a mental disorder. Individuals with a mental disorder may be vulnerable to worsening their mental health condition. A recent systematic review that synthesised study data from different pandemics (Neelam et al., Citation2021) found that a pre-existing mental disorder was associated with elevated PTSD symptoms. For example, patients with major depressive disorder showed elevated prevalence rates of PTSD symptoms (Concerto et al., Citation2022). Among psychiatric inpatients with mental disorders, restricted visits from loved ones, restricted interactions with other patients, limited out-of-room activities, and meals taken alone were factors associated with increased levels of clinical symptoms (Russ et al., Citation2021). In individuals with a previous mental disorder, the multiple stressors during the pandemic might reactivate or worsen mental health problems (Hall et al., Citation2008).
As expected, current trauma exposure during the COVID-19 pandemic was related to an increased risk for probable PTSD. For traumatic events that occurred before the pandemic, there was a trend in the expected direction. An Israeli study found that a history of trauma exposure was significantly related to elevated levels of peritraumatic stress symptoms during the pandemic (Lahav, Citation2020). Features of the COVID-19 pandemic, such as uncontrollability, perceived threat of death, and coercive force of public health restrictions might reactivate PTSD symptoms related to previous traumatic events in some individuals (Masiero et al., Citation2020).
4.2. Protective factors for PTSD symptoms
4.2.1. Sociodemographic protective factors
A medium and high household income was associated with a reduced risk for PTSD, which is consistent with earlier studies (Currie, Citation2021; Karatzias et al., Citation2020; Kira et al., Citation2021). A high income provides access to financial resources (e.g. health care, childcare) which might facilitate effective adaptation to the challenges of the COVID-19 pandemic.
4.2.2. Pandemic-related protective factors
Having face-to-face contact either less than once a week or 3–7 times a week with others (vs. no face-to-face contact) was related to a reduced risk for PTSD. Having digital social contact less than once a week or 1–7 times a week (vs. no digital contact) was also related to a reduced risk for PTSD. It is well-known that social support reduces the risk for PTSD (Brewin et al., Citation2000).
4.3. Burden of pandemic stressors related to PTSD symptoms
Burden related to inefficient Crisis management and communication was related to an increased risk for probable PTSD, indicating the need for an effective governmental crises strategy to promote mental health in the general population. Consistent with this result, earlier research found that public trust in the government was related to lower psychological distress and higher well-being (Barrafrem et al., Citation2021; Olagoke et al., Citation2020).
Burden due to Restricted access to resources such as food, regular health care, or medication was related to an increased risk for probable PTSD. Earlier studies conducted in the USA reported associations between food insecurity and distress, as well as depressive and anxiety symptoms during the COVID-19 pandemic (Fang et al., Citation2021; Wolfson et al., Citation2021; Yenerall & Jensen, Citation2021).
Burden related to Restricted social contact was associated with probable PTSD. In earlier research conducted during the COVID-19 pandemic, social support showed relationships with lower PTSD symptom levels (Liu et al., Citation2021).
Burden associated with Difficult housing conditions (e.g. limited living space and conflicts at home), were related to an increased risk for probable PTSD. A systematic review on PTSD symptoms after pandemics of infectious diseases (Yuan et al., Citation2021) found that limited living space was related to higher PTSD symptom levels.
4.4. Stringency and between-country differences
The stringency of lockdown policies was unrelated to the risk for probable PTSD in our study. Between-country differences in the risk for probable PTSD were only found for one of the eleven countries (Greece). A global population study (Olff et al., Citation2021) found that the COVID-19-related mental health burden was higher in countries with a lower perceived effectiveness of government interventions to combat infections, but lower in countries with lower COVID-19 infection exposure. Further studies need to examine which of these factors are related to between-country differences in PTSD.
4.5. Strengths and limitations
A strength of this study is the large sample size and the inclusion of eleven countries. Such large cross-cultural studies during the COVID-19 pandemic are rare. We used an established measure to assess probable PTSD, in addition to custom-made measures to assess the specific stressors relevant in the context of the COVID-19 pandemic. A limitation of this study is that participants were self-selected from the general population. We might have overrepresented people with a higher burden as they might be more inclined to fill out a survey on mental health problems. Due to the digital nature of this study, we could not reach individuals with no or poor internet accessibility. The study is further limited by using self-report measures that could have introduced systematic bias. Several measures used were self-constructed, as no suitable measures existed. Therefore, we developed new measures such as the PaSS to measure pandemic-specific stressor domains. While we found the first evidence for their validity (Lotzin et al., Citation2022), the measure has not been evaluated previously. Furthermore, the cross-sectional design of this study makes it impossible to examine causal relationships and the direction of effects. As this is an exploratory study, p-values were not adjusted for multiplicity. While we controlled for country-level stringency and country-level differences, we did not consider different regions of the countries, which might be related to different stages and severities of the pandemic.
The data of this study stems from the early phase of the pandemic, i.e. summer and autumn 2020. It might be possible that psychological distress peaked at the beginning of the outbreak when individuals experienced an entirely unfamiliar situation. On the other hand, people might experience increased PTSD symptoms when they need to cope with the chronicity of stressors over time. Future studies need to examine trajectories of PTSD over the pandemic to understand the long-term impact during different pandemic phases.
5. Conclusions
The multiple pandemic-specific stressors seem to have taken a toll on mental health. We found high rates of probable PTSD (17.7%) during the first year of the COVID-19 pandemic. Given the high rates of probable PTSD among trauma-exposed individuals found in this study, monitoring mental health problems should be a public health priority in this vulnerable group.
A broad range of protective and risk factors was related to probable PTSD, such as trauma exposure during the pandemic, a current or previous mental disorder, and restricted social contact. To prevent long-term consequences, targeted measures for vulnerable individuals are needed. Brief psychosocial programmes for individuals who show subclinical PTSD symptoms may help to promote recovery and prevent the development of PTSD (Lotzin, Hinrichsen, et al., Citation2021). Individuals who fulfil the diagnostic criteria for PTSD should receive guideline-compliant trauma-focused psychotherapeutic support.
Author contributions
AL designed the study in cooperation with all members of the ADJUST consortium. All authors recruited study participants. All authors coordinated the data management within the respective country, AL coordinated the overall data management. LK conducted the data analysis, in cooperation with AL. AL drafted the manuscript. All authors substantially contributed to the revision of the manuscript and approved the final version.
Data protection and quality assurance
Integrated data for data analysis was stored on a server of the coordinating site (Centre for Interdisciplinary Addiction Research, CIAR, at University of Hamburg). Data handling followed the EU General Data Protection Regulation (DSGVO); data will be stored for at least 10 years.
Data sharing
Data used in this analysis will be made available in a public repository at a later timpoint (OSF registry, 10.17605/OSF.IO/8XHYG).
Ethics, consent, and permissions
The study was registered in a study registry before its start (OSF registry, 10.17605/OSF.IO/8XHYG). Each country obtained ethical approval of the study: Ethics Committee of the University of Vienna, 00554. Ethics Committee of the University of Urbino ‘Carlo Bo’, 34, 22/07/2020. Ethics Committee of the Department of Psychology, Faculty of Humanities and Social Sciences, University of Zagreb: 21 May 2020. Ethics Review Board of the Faculty of Social and Behavioural Sciences, Utrecht University, Number 20-360. Ilia State University Faculty of Arts and Science Research Ethics Committee: 12/06/2020. Local Psychological Ethics Committee at the Centre for Psychosocial Medicine, LPEK-0149. Social Sciences Ethics Review Board (SSERB), University of Nicosia, SSERB 00109. The Swedish Ethical Review Authority, 2020-03217. Vilnius University Ethics Committee of Research in Psychology, 44. Ethics Committee of the Faculty of Psychology, University of Warsaw, 6/7/2020. Ethics Committee of the Medical Faculty, University of Porto and Centro Hospitalar São João, Porto, CE 201-20. The National Ethical Review Board in Sweden, 2020-03217. All participants provided informed consent before taking part in the study. Participants were informed that they were under no obligation to participate and that they could withdraw from the study without consequences.
Acknowledgements
The authors thank the collaborators for their support and contribution to the present paper: Ozan Demirok, Stella Perziani (team Austria); Marina Adjukovic, Helena Bakic, Ines Rezo Bagaric, Tanja Franciskovic (team Croatia); Nino Makhashvili and Sophio Vibliani (team Georgia); Eleftheria Eugeniou, George Fevgas, Kostas Messas, Marianna Philippidou, Eleni Papathanasiou, Anastasia Selidou (team Cyprus/Greece); Ilaria Cinieri, Alessandra Gallo and Chiara Marangio (team Italia); Monika Kvedaraite and Auguste Nomeikaite (team Lithuania); Joanne Mouthaan, Suzan Soydas, Marloes Eidhof, Marie José van Hoof and Simon Groen (team Netherlands); Magdalena Skrodzka and Monika Folkierska-Żukowska (team Poland); Aida Dias, Camila Borges, Diana Andringa, Guida Manuel, Joana Beker and João Veloso, Francisco Freitas (team Portugal); Kristina Bondjers, Josefin Sveen, Rakel Eklund, Kerstin Bergh Johannesson and Ida Hensler (team Sweden). The authors greatly thank the study team of the coordinating site at University Medical Centre Hamburg-Eppendorf (team Germany) that administered the data management, in particular Laura Kenntemich and Leonie von Huelsen, who were supported by Eike Neumann-Runde, Sven Buth, Kaenaat Khan, Theresa Klinger, Ronja Ketelsen, Lennart Schwierzke, Julia Groß, and Laura Gutewort. We also thank Ann-Kathrin Ozga for her statistical advice.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability
The detailed sociodemographic and clinical information of the dataset does not fully protect the anonymity of the respondents. For this reason, the entire dataset cannot be made publicly available. However, excerpts of the data on a higher aggregation level can be provided upon justified request by the first author.
Additional information
Funding
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association.
- Barrafrem, K., Tinghög, G., & Västfjäll, D. (2021). Trust in the government increases financial well-being and general well-being during COVID-19. Journal of Behavioral and Experimental Finance, 31, Article 100514. https://doi.org/10.1016/j.jbef.2021.100514
- Bendau, A., Petzold, M. B., Pyrkosch, L., Mascarell Maricic, L., Betzler, F., Rogoll, J., Große, J., Ströhle, A., & Plag, J. (2021). Associations between COVID-19 related media consumption and symptoms of anxiety, depression and COVID-19 related fear in the general population in Germany. European Archives of Psychiatry and Clinical Neuroscience, 271(2), 283–291. https://doi.org/10.1007/s00406-020-01171-6
- Bovin, M. J., Kimerling, R., Weathers, F. W., Prins, A., Marx, B. P., Post, E. P., & Schnurr, P. P. (2021). Diagnostic accuracy and acceptability of the primary care posttraumatic stress disorder screen for the diagnostic and statistical manual of mental disorders (fifth edition) among US veterans. JAMA Network Open, 4(2), e2036733. https://doi.org/10.1001/jamanetworkopen.2020.36733
- Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766. https://doi.org/10.1037/0022-006X.68.5.748
- Brotto, L. A., Chankasingh, K., Baaske, A., Albert, A., Booth, A., Kaida, A., Smith, L. W., Racey, S., Gottschlich, A., Murray, M. C. M., Sadarangani, M., Ogilvie, G. S., & Galea, L. (2021). The influence of sex, gender, age, and ethnicity on psychosocial factors and substance use throughout phases of the COVID-19 pandemic. PLoS One, 16(11), e0259676. https://doi.org/10.1371/journal.pone.0259676
- Cénat, J. M., Blais-Rochette, C., Kokou-Kpolou, C. K., Noorishad, P.-G., Mukunzi, J. N., McIntee, S.-E., Dalexis, R. D., Goulet, M.-A., & Labelle, P. R. (2021). Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Research, 295, 113599. https://doi.org/10.1016/j.psychres.2020.113599
- Concerto, C., Rodolico, A., Sturiale, S., Caligiore, G., Signorelli, M. S., Petralia, A., Battaglia, F., & Aguglia, E. (2022). Prevalence and factors associated with PTSD-like symptoms linked to the COVID-19 pandemic among patients with major depressive disorders seeking emergency care. Journal of Nervous & Mental Disease, 210(4), 246–248. https://doi.org/10.1097/NMD.0000000000001468
- Conrad, R. C., Hahm, H., “Chris,” Koire, A., Pinder-Amaker, S., & Liu, C. H. (2021). College student mental health risks during the COVID-19 pandemic: Implications of campus relocation. Journal of Psychiatric Research, 136, 117–126. https://doi.org/10.1016/j.jpsychires.2021.01.054
- Currie, C. L. (2021). Adult PTSD symptoms and substance use during Wave 1 of the COVID-19 pandemic. Addictive Behaviors Reports, 13, 100341. https://doi.org/10.1016/j.abrep.2021.100341
- Dragan, M., Grajewski, P., & Shevlin, M. (2021). Adjustment disorder, traumatic stress, depression and anxiety in Poland during an early phase of the COVID-19 pandemic. European Journal of Psychotraumatology, 12(1), Article 1860356. https://doi.org/10.1080/20008198.2020.1860356
- Fang, D., Thomsen, M. R., & Nayga, R. M. (2021). The association between food insecurity and mental health during the COVID-19 pandemic. BMC Public Health, 21(1), 1–8. https://doi.org/10.1186/s12889-020-10013-y
- Hall, R. C., Hall, R. C., & Chapman, M. J. (2008). The 1995 Kikwit Ebola outbreak: Lessons hospitals and physicians can apply to future viral epidemics. General Hospital Psychiatry, 30(5), 446–452. https://doi.org/10.1016/j.genhosppsych.2008.05.003
- Karatzias, T., Shevlin, M., Murphy, J., McBride, O., Ben-Ezra, M., Bentall, R. P., Vallières, F., & Hyland, P. (2020). Posttraumatic stress symptoms and associated comorbidity during the COVID-19 pandemic in Ireland: A population-based study. Journal of Traumatic Stress, 33(4), 365–370. https://doi.org/10.1002/jts.22565
- Kendall-Tackett, K. (2020). A social history of the coronavirus. Psychological Trauma: Theory, Research, Practice, and Policy, 12(1), S1–S2. https://doi.org/10.1037/tra0000955
- Kira, I. A., Shuwiekh, H. A. M., Ashby, J. S., Elwakeel, S. A., Alhuwailah, A., Sous, M. S. F., Baali, S. B. A., Azdaou, C., Oliemat, E., & Jamil, M., & J, H. (2021). The impact of COVID-19 traumatic stressors on mental health: Is COVID-19 a new trauma type. International Journal of Mental Health and Addiction, https://doi.org/10.1007/s11469-021-00577-0
- Lahav, Y. (2020). Psychological distress related to COVID-19 – The contribution of continuous traumatic stress. Journal of Affective Disorders, 277, 129–137. https://doi.org/10.1016/j.jad.2020.07.141
- Liu, C., Huang, N., Fu, M., Zhang, H., Feng, X. L., & Guo, J. (2021). Relationship between risk perception, social support, and mental health among general Chinese population during the COVID-19 pandemic. Risk Management and Healthcare Policy, 14, 1843–1853. https://doi.org/10.2147/RMHP.S302521
- Lotzin, A., Aakvaag, H., Acquarini, E., Ajdukovic, D., Ardino, V., Böttche, M., Bondjers, K., Bragesjö, M., Dragan, M., Braga, M. M. C. de F. F., Gelezelyte, O., Grajewski, P., Javakhishvili, D., Kazlauskas, E., Knefel, M., Lueger-Schuster, B., Makhashvili, N., Mooren, T., Sales, L., Stevanovic A., Schäfer, I. (2020). Stressors, coping and symptoms of adjustment disorder in the course of the COVID-19 pandemic—Study protocol of the European Society for Traumatic Stress Studies (ESTSS) pan-European study. European Journal of Psychotraumatology, 11(1), 1780832. https://doi.org/10.1080/20008198.2020.1780832
- Lotzin, A., Hinrichsen, I., Kenntemich, L., Freyberg, R.-C., Lau, W., & O’Donnell, M. (2021). The SOLAR group program to promote recovery after disaster and trauma-A randomized controlled feasibility trial among German trauma survivors. Psychological Trauma: Theory, Research, Practice and Policy, 14(1), 161–171. https://doi.org/10.1037/tra0001105
- Lotzin, A., Ketelsen, R., Zrnic, I., Lueger-Schuster, B., Böttche, M., & Schäfer, I. (2022). The Pandemic Stressor Scale: Factorial validity and reliability of a measure of stressors during a pandemic. BMC Psychology, 10(1), 92. https://doi.org/10.1186/s40359-022-00790-z
- Lotzin, A., Krause, L., Acquarini, E., Ajdukovic, D., Ardino, V., Arnberg, F., Böttche, M., Bragesjö, M., Dragan, M., Figueiredo-Braga, M., Gelezelyte, O., Grajewski, P., Anastassiou-Hadjicharalambous, X., Javakhishvili, J. D., Kazlauskas, E., Lenferink, L., Lioupi, C., Lueger-Schuster, B., Tsiskarishvili, L., Mooren, T., … ADJUST study Consortium. (2021). Risk and protective factors, stressors, and symptoms of adjustment disorder during the COVID-19 pandemic – First results of the ESTSS COVID-19 pan-European ADJUST study. European Journal of Psychotraumatology, 12(1), 1964197. https://doi.org/10.1080/20008198.2021.1964197
- Masiero, M., Mazzocco, K., Harnois, C., Cropley, M., & Pravettoni, G. (2020). From individual to social trauma: Sources of everyday trauma in Italy, the US and UK during the COVID-19 pandemic. Journal of Trauma & Dissociation, 21(5), 1–7. https://doi.org/10.1080/15299732.2020.1787296
- Neelam, K., Duddu, V., Anyim, N., Neelam, J., & Lewis, S. (2021). Pandemics and pre-existing mental illness: A systematic review and meta-analysis. Brain, Behavior, & Immunity - Health, 10, 100177. https://doi.org/10.1016/j.bbih.2020.100177
- Olagoke, A. A., Olagoke, O. O., & Hughes, A. M. (2020). Psychological pathways linking public trust during the Coronavirus pandemic to mental and physical well-being. Frontiers in Psychology, 11, 570216. https://doi.org/10.3389/fpsyg.2020.570216
- Olff, M. (2017). Sex and gender differences in post-traumatic stress disorder: An update. European Journal of Psychotraumatology, 8(sup4), 1351204. https://doi.org/10.1080/20008198.2017.1351204
- Olff, M., Primasari, I., Qing, Y., Coimbra, B. M., Hovnanyan, A., Grace, E., Williamson, R. E., Hoeboer, C. M., & Consortium, the G.-C. (2021). Mental health responses to COVID-19 around the world. European Journal of Psychotraumatology, 12(1), 1929754. https://doi.org/10.1080/20008198.2021.1929754
- Prins, A., Bovin, M. J., Kimerling, R., Kaloupek, D. G., Marx, B. P., Pless Kaiser, A., & Schnurr, P. P. (2015). The primary care PTSD screen for DSM-5 (PC-PTSD-5). Scale Available from the National Center for PTSD Web Site Www. Ptsd. va. Gov. Updated April, 7, 2017.
- Rajkumar, R. P. (2020). COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 52, Article 102066. https://doi.org/10.1016/j.ajp.2020.102066
- Riley, R. D., Snell, K. I. E., Ensor, J., Burke, D. L., Harrell Jr, F. E., Moons, K. G. M., & Collins, G. S. (2019). Minimum sample size for developing a multivariable prediction model: Part I – Continuous outcomes. Statistics in Medicine, 38(7), 1262–1275. https://doi.org/10.1002/sim.7993
- Rossi, R., Socci, V., Talevi, D., Mensi, S., Niolu, C., Pacitti, F., Di Marco, A., Rossi, A., Siracusano, A., & Di Lorenzo, G. (2020). COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Frontiers in Psychiatry, 11, 790. https://doi.org/10.3389/fpsyt.2020.00790
- Russ, M. J., Parish, S. J., Mendelowitz, R., Mendoza, S., Arkow, S. D., Radosta, M., Espinosa, L., Sombrotto, L. B., Anthony, D., Wyman, D. A., Baptista-Neto, L., & Wilner, P. J. (2021). The interface of COVID-19 and inpatient psychiatry: Our experience and lessons learned. Journal of Psychiatric Practice, 27(3), 172–183. https://doi.org/10.1097/PRA.0000000000000551
- Ryder, A. L., Azcarate, P. M., & Cohen, B. E. (2018). PTSD and physical health. [Review]. Current Psychiatry Reports, 20(12), 12. https://doi.org/10.1007/s11920-018-0977-9
- Salehi, M., Amanat, M., Mohammadi, M., Salmanian, M., Rezaei, N., Saghazadeh, A., & Garakani, A. (2021). The prevalence of post-traumatic stress disorder related symptoms in Coronavirus outbreaks: A systematic-review and meta-analysis. Journal of Affective Disorders, 282, 527–538. https://doi.org/10.1016/j.jad.2020.12.188
- Solar, O., & Irwin, A. (2010). A conceptual framework for action on the social determinants of health. World Health Organization.
- Spoont, M. R., Williams, J. W., Kehle-Forbes, S., Nieuwsma, J. A., Mann-Wrobel, M. C., & Gross, R. (2015). Does this patient have posttraumatic stress disorder?: Rational clinical examination systematic review. JAMA, 314(5), 501–510. https://doi.org/10.1001/jama.2015.7877
- Weathers, F. W., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). PTSD Checklist for DSM-5 (PCL-5) with Criterion A. https://www.ptsd.va.gov/professional/assess-ment/adult-sr/ptsd-checklist.asp
- White, I. R., Royston, P., & Wood, A. M. (2011). Multiple imputation using chained equations: Issues and guidance for practice. Statistics in Medicine, 30(4), 377–399. https://doi.org/10.1002/sim.4067
- Wolfson, J. A., Garcia, T., & Leung, C. W. (2021). Food insecurity is associated with depression, anxiety, and stress: Evidence from the early days of the COVID-19 pandemic in the United States. Health Equity, 5(1), 64–71. https://doi.org/10.1089/heq.2020.0059
- Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., Chen-Li, D., Iacobucci, M., Ho, R., Majeed, A., & McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64. https://doi.org/10.1016/j.jad.2020.08.001
- Yenerall, J., & Jensen, K. (2021). Food security, financial resources, and mental health: Evidence during the COVID-19 pandemic. Nutrients, 14(1), 161. https://doi.org/10.3390/nu14010161
- Yuan, K., Gong, Y.-M., Liu, L., Sun, Y.-K., Tian, S.-S., Wang, Y.-J., Zhong, Y., Zhang, A.-Y., Su, S.-Z., Liu, X.-X., Zhang, Y.-X., Lin, X., Shi, L., Yan, W., Fazel, S., Vitiello, M. V., Bryant, R. A., Zhou, X.-Y., Ran, M.-S., Bao Y.-P., … Lu, L. (2021). Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: A meta-analysis and systematic review. Molecular Psychiatry, 26, 1–17. https://doi.org/10.1038/s41380-021-01036-x
- Yunitri, N., Chu, H., Kang, X. L., Jen, H.-J., Pien, L.-C., Tsai, H.-T., Kamil, A. R., & Chou, K.-R. (2022). Global prevalence and associated risk factors of posttraumatic stress disorder during COVID-19 pandemic: A meta-analysis. International Journal of Nursing Studies, 126, Article 104136. https://doi.org/10.1016/j.ijnurstu.2021.104136
