ABSTRACT
Background:
Since the introduction of the ‘Test and treat’ approach in the Human Immunodeficiency Virus (HIV) management, various strategies have been devised and implemented by countries to relieve public health facilities of the large numbers of people coming for medicine refills and clinical follow-up. One of the strategies is the dispensing of antiretroviral medicines through community pharmacies. In Rwanda, community pharmacies are not yet involved in antiretrovirals (ARVs) dispensing, and no study has assessed their readiness to provide this service. This study aimed to assess the readiness of community pharmacy staff and infrastructure to implement a decentralised model of antiretroviral medicines dispensing.
Methods:
This cross-sectional study included data from 262 community pharmacies sampled across all districts of Rwanda. Primary data were collected using a structured questionnaire, from February to March 2023. Responses were received for 262 community pharmacies, representing the total sample size. Data analysis was done using quantitative descriptive and inferential statistical approaches. Frequency tables and graphs were produced using STATA15 and the outputs were exported to MS Excel as well as MS Word to allow document framing and designing.
Results:
The research has shown a high proportion of community pharmacy staff trained in HIV prevention (82.4% trained on HIV testing), but a low level of training in treatment (30.5%) and psychosocial support of people living with HIV (29.8%). Infrastructure and storage conditions were found to be adequate, with 99.6% of surveyed Pharmacies having sufficient storage space. Majority (93.9%) expressed their willingness to dispense ARVs in the pharmacy premises. A large number of respondents (92.4%) felt that dispensing of antiretroviral medicines through community pharmacies would lead to an increase in sales of over the counter and other non-HIV related medicines. The main anticipated challenge that should be addressed to ensure effective implementation is the lack of interoperability between reporting systems used by community pharmacies and those used by health facilities providing HIV services (76.7% of respondents).
Conclusion:
Community pharmacies in Rwanda have majority of staff trained in various areas of HIV prevention, but a small proportion have been trained in HIV care and treatment. Community pharmacies have the necessary infrastructure to dispense ARVs, and those with shortcomings, such as the lack of a separate room for individual patient counselling, are willing to obtain such a room if they are authorised to dispense ARVs. Staffs are willing to dispense ARVs in community pharmacies if the model is recommended by policymakers. The model could have several benefits for community pharmacies and the public health system in general, but there are also challenges that should be mitigated to ensure effective implementation. The staff willingness and expected benefits constitute enabling factors that the Ministry of Health and the national HIV control programme may leverage to prepare for introducing the model of ARVs distribution through community pharmacies.
Background
Four decades have elapsed since the Human Immunodeficiency Virus (HIV) was detected. It was first identified in a form of small numbers of isolated cases, but within a decade, the Acquired Immunodeficiency Syndrome (AIDS) was killing millions of people around the globe, making the HIV to become one of the most important epidemics in the history (Sharp & Hahn, Citation2011). Since the start of the HIV epidemic, 84.2 million people on the globe have been infected, while about 40.1 million have died from AIDS-related illnesses. In 2021, 38.4 million people were globally living with HIV. There have been about 1.5 million people newly infected with HIV, whereas around 650,000 people died from AIDS-related illnesses during the same year. People having access to antiretroviral therapy were estimated at 28.7 million as of end December 2021 (UNAIDS, Citation2022).
HIV treatment uses a combination of medicines known as treatment regimens. A treatment regimen generally comprises three medicines from at least two different therapeutic classes. Current World Health Organization (WHO) guidelines recommend the use of Dolutegravir (DTG)-based regimens as the treatment of choice for populations starting antiretroviral therapy and for those on second line who have never been exposed to DTG. The preference for DTG is associated with its efficacy and a high genetic barrier to drug resistance, among other factors, resulting in rapid suppression of viral load (World Health Organization, Citation2021).
Effective and sustainable delivery of Antiretroviral Therapy (ART) to the people living with HIV (PLHIV) on treatment requires the use of innovative approaches that make services more convenient for beneficiaries while at the same time reducing the workload on health systems. One of such strategies used in ART service provision is the community-based model of delivery. The national Community Health Commodity Distribution (CHCD) is implemented in Eswatini. It consists of community-based differentiated service delivery (DSD) models that include community ART groups as well as other outreach models (PEPFAR EP, Citation2021).
Such approaches also include the transitioning of clinically stable patients from public health facilities to obtain their medicines from private sector providers. The decentralisation of ART services to community pharmacies implies that clinically stable patients in public health facilities are devolved to private community pharmacies for antiretroviral medicine refills. Accredited pharmacies receive the medicines from public health facilities and the service is provided either free of charge or is available on a small dispensing fee (USAID/PEPFAR EP, Citation2019).
The WHO promotes and encourages the use of decentralised approaches in the distribution of antiretroviral medicines. Community based ART approaches are overwhelmingly supported as they are a viable strategy for delivering HIV treatment services closer to the people in need. In countries where they are already implemented, these approaches increase ART uptake, retention in care, and decongest public health facilities. The shift from hospital based to primary health centres is being followed by the shift to the community, including the distribution through community pharmacies (Avong et al., Citation2018).
A cross-sectional survey of community pharmacists’ views in South-East Nigeria showed that community pharmacists have high knowledge of HIV and a moderate attitude towards HIV care and treatment services. They have shown a high level of willingness and readiness to provide their contribution to the provision of HIV services. However, the survey also highlighted that more was needed in the aspect of having adequate policies that facilitate further empowerment of more community pharmacists in this specific area of care (Ajagu et al., Citation2017).
The consortium for Strengthening Integrated Delivery of HIV/AIDS Services (SIDHAS) implemented the use of community-based private sector pharmacists to expand ART distribution in Nigeria, Lagos and Rivers States. The intervention has resulted in a decongestion of public hospitals providing ART services, reduced public health facility staffing requirements, improved customer satisfaction and adherence to medicine refill appointments, and mobilised resources for HIV care in a sustainable and cost-effective way. Clients and providers at both public and private facilities willingly embraced the innovative intervention. The private pharmacies reported financial and professional gains, whereas the public health facilities staff confirmed a reduced workload resulting in greater performance and effectiveness (PEPFAR Solutions Platform, Citation2020).
Rwanda adopted and started the implementation of the new WHO recommendation of ‘Treat all’ HIV positive patients in July 2016. On one hand, this was an opportunity to increase the number of PLHIV on treatment. On the other hand, there was a foreseeable burden on the existing health systems given the likelihood of a disproportionate increase in the number of clients versus the health care providers. Rwanda therefore started the implementation of the Differentiated Service Delivery Model (DSDM), which takes into consideration variable patient needs and priorities with respect to their clinical and immunological status. Patients in different categories of the differentiated service delivery get their medicine refills and clinical follow up at different frequencies (Rwanda Ministry of Health (Citation2016).
The distribution of antiretroviral medicines in Rwanda is so far limited to public health facilities (Hospitals and Health Centres), faith based as well as a few accredited private and NGOs owned clinics (Rwanda Ministry of Health, Citation2016). Decentralised models of antiretroviral medicines distribution include distribution through community pharmacies. These models make a major contribution to decongesting public health facilities and enable people living with HIV to access their medicines closer to home, in their communities (USAID/PEPFAR EP, Citation2019). There are no studies conducted on the readiness of community pharmacies in Rwanda to participate in the distribution of antiretroviral medicines. This study was conducted to assess the readiness of community pharmacies as an additional entity that could be leveraged for the decentralised dispensing of antiretroviral medicines. It aimed to assess the readiness in terms of infrastructure, staff training and willingness to dispense ARVs in community pharmacy premises, the anticipated benefits from the model and challenges that should be mitigated. Study results will inform policy makers at responsible entities (Ministry of Health and national HIV programme) for future decision making when expanding the involvement of community pharmacies in the provision of HIV related services.
Methods and materials
Study setting
The study was carried out in 262 community pharmacies sampled across all 30 districts of Rwanda.
Study design
This was a cross-sectional study with quantitative and qualitative features. Data for this study were collected from February to March 2023. We collected data on demographic characteristics of the participants, the training of community pharmacy personnel on HIV related services and antiretroviral medicines as well as the willingness of community pharmacy personnel to implement a decentralised model of antiretroviral medicines dispensing through community pharmacies.
Study population
According to the information obtained from Rwanda Food and Drugs Authority (Rwanda FDA), there were 761 licensed community pharmacies operating in different districts of Rwanda as of November 2022 (Rwanda Food and Drugs Authority, Citation2022). As described under ‘’Sampling technique’’ section, the sample for this study was drawn from the entire population. One respondent (pharmacist or nurse) was interviewed at each of the community pharmacies comprising the sample.
Sampling technique
The study was carried out among 262 community pharmacies sampled across Rwanda. Since the population size was known, Slovin’s formula was applied to determine the sample size. In order to ensure coverage of each district, the probability proportional to size (PPS)- a prorated approach to ensure equitable sample distribution across districts, was used to determine the number of community pharmacies to be surveyed in each of the districts. Given that there was no assumption of heterogeneity in the way community pharmacies operate, nor of regional disparities since they all operate under the same regulatory body, the Rwanda FDA, and knowing the number and names of community pharmacies per district, simple random sampling was applied at district level to obtain the sub-sample allocated to each specific district. Any healthcare professional working in a sampled community pharmacy could take part in the research. The study did not define any other particular requirements regarding the profession of the interviewees.
Data collection instruments, procedure, and analysis
The questionnaire for this study was designed to collect data on pharmacy identification, demographic characteristics of the respondents, training in HIV prevention and management, pharmacy infrastructure, staff willingness to provide HIV-related services, as well as the anticipated benefits and challenges associated with dispensing antiretroviral medicines.
Data were collected using kobo toolbox, one of Open Data Kit (ODK) based platforms that allow the designing of electronic forms with logical controls to ensure validity and completeness. To ensure the validity and reliability of the questionnaire, a pilot exercise was carried out in three community pharmacies in Kigali. The questionnaire was validated by (i) assessing the clarity of language, logical flow and validity of data entries, (ii) testing whether a data collector can access the blank cloud-based kobo form, work offline and/or online and can submit data successfully and (iii) familiarising and empowering the data collectors on research ethics. Feedback from the pre-test enabled to reformulate certain questions, establish relevance constraints, logic and validation rules and/or controls to ensure the smooth running of questions, accuracy and completeness of data. Based on the feedback from the pilot, an improved and final version of the form was deployed for use during data collection.
Data were collected through participant interviews and observations. Participants’ responses were immediately entered into the data collection tool. Data were coded and stored numerically for both quantitative and qualitative variables and as string text for a few open questions. The analysis was done using quantitative descriptive and inferential statistical approaches. Frequency tables and graphs were produced using STATA15 and the outputs were exported to MS Excel as well as MS Word to allow document framing and designing. The chi-square test of independence was used to assess the association between staff profession, qualification and years of service with their training on HIV or their willingness to dispense antiretroviral medicines through community pharmacies. The confidence level was set at 95%, the threshold for p-value at 5%.
Results
Sociodemographic characteristics
Study participants included pharmacists and nurses operating in the community pharmacies. As presented in , majority of respondents were pharmacists representing 55.7% of the study population, whereas 44.3% were nurses. Of all the respondents, 58.8% had a bachelor’s degree as the highest qualification. It is worthy to note that all pharmacists had at least a bachelor’s degree in accordance with Rwanda FDA guidelines. Close to 45% of all the respondents had served for less than 5 years.
Table 1. Sociodemographic characteristics of the respondents.
Training on HIV prevention and management
The majority have been trained on components of HIV prevention that include HIV testing (82.4%), pre/post HIV test counselling (83.2%) and HIV self-testing (80.9%). Smaller proportions have been trained on components such as HIV treatment (30.5%) and psychosocial care and support to PLHIV (29.8%). Community pharmacy staff who had not received any training on HIV prevention or management represented 9.9% of all respondents ().
Table 2. Staff training on HIV prevention and management.
Infrastructure and health commodities storage conditions
In all community pharmacies surveyed, products were protected from direct sunlight, while storage space was adequate in 99.6% of cases. There were no signs of pests, harmful insects or rodents in 257 (98.1%) of the 262 community pharmacies that have been assessed. Availability of fire safety equipment was the least performing element, with 70.6% of the community pharmacies having a fire safety equipment in place. Daily room temperature monitoring was performed by 96.2% of the pharmacies ().
Table 3. Infrastructure and storage conditions in community pharmacies.
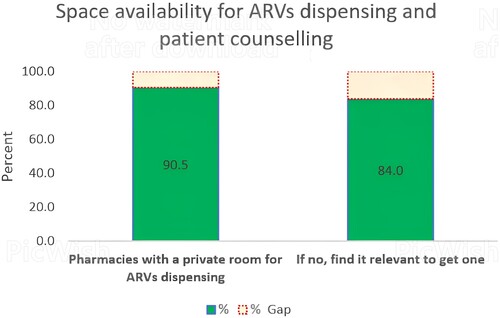
Of the 262 community pharmacies surveyed, 90.5% have a room that, if the community pharmacy model of antiretroviral medicine dispensing is adopted, could be dedicated to special care requiring one-on-one interaction between the provider and the patient. Of the 25 not having such a room, 21 (84.0%) understand the relevance of having a dedicated room for dispensing antiretroviral medicines and providing adherence counselling to the patient ().
Willingness, enabling factors and challenges
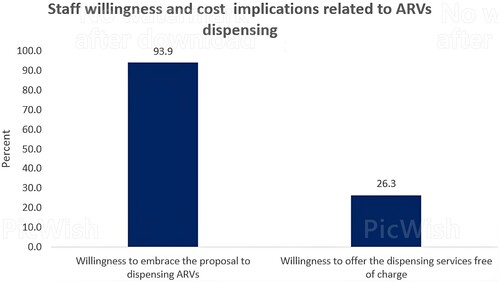
As illustrated in , majority of the community pharmacy personnel (93.9%) are willing to dispense antiretroviral medicines in their premises if this model is adopted by the policy and guidelines. Only 26.3% of respondents felt that the ARVs dispensing service could be offered free of charge to patients.
Association between willingness to dispense ARVs and profession, qualification or working experience
The chi-square test was used to assess the association between staff willingness to dispense ARVs and their professional belonging, qualification or years of working experience. No association was found between test variables since the results obtained for p-value as illustrated in are greater than the threshold that had been set at 5% with a confidence level of 95%.
Table 4. Association between staff willingness to dispense ARVs and their profession, qualification or working experience.
Association between staff training and their willingness to dispense ARVs
The chi-square test was used to analyse the association between staff training in the different areas of HIV prevention and management, and their willingness to dispense ARVs in the community pharmacies. With the confidence level set at 95% and threshold p-value at 5%, the assessment showed that having been trained on two components, namely ‘HIV treatment’ and ‘psychosocial care and support of PLHIV’ were associated with staff willingness to dispense ARVs. The analysis showed Pearson's chi-square values of 8.209 and 5.715 for ‘HIV treatment’ and ‘psychosocial care and support of PLHIV,’ respectively, while the p values were 0.004 and 0.017 ().
Table 5. Association between staff training and their willingness to dispense ARVs.
Potential benefits for community pharmacies
Majority of the respondents (92.4%) feel that dispensing of antiretroviral medicines through community pharmacies would lead to a sales increase for over the counter and other non-HIV related medicines. The results presented in show that, if this strategy is adopted, 86.3% believe that it would expand the role of community pharmacies in overall provision of healthcare to the public, while 83.6% see this model as an opportunity to contribute to addressing the burden at health facility through decentralisation. A lower proportion (67.6%) see the strategy as an opportunity for more staff training and capacity development.
Table 6. Potential benefits for CPs to dispense antiretroviral medicines.
Anticipated challenges
As illustrated in , the major anticipated challenge is the lack of interoperability between reporting systems used by community pharmacies and those used by health facilities providing HIV services (76.7% of respondents). According to 70.2% of respondents, the practice of dispensing antiretroviral medicines through community pharmacies would result in an increased workload. Only 42.4% of the respondents anticipate challenges related to patient counselling and confidentiality management.
Table 7. Anticipated challenges to dispensing ARVs through CPs.
Discussion
Training on HIV
The community pharmacy personnel received training in various areas related to HIV prevention and management. An overall consideration of the perceived skills on HIV/AIDS among the surveyed community pharmacy personnel results in an average of 43.9%. This average is relatively low, but higher than the finding of the South-East Nigerian study that identified a mean score of 39.26% (Ajagu et al., Citation2017). However, the Nigerian study did not assess exactly the same training areas as this research.
The low proportion of staff trained in areas related to HIV treatment and comprehensive care to people living with HIV, underscores the critical need to train this category of health professionals if they are to participate in the dispensing of antiretroviral medicines. The need for training was also recognised by respondents, with 72.1% identifying lack of skills as one of the barriers that should be addressed for effective distribution of antiretroviral medicines through community pharmacies. Due to staff turnover, some health professionals move from public to private health facilities. It is very likely that community pharmacy staff who have been trained in different areas of HIV prevention and management have benefited from this capacity building while working for the public sector.
There was no association between staff willingness to dispense ARVs and their professional belonging, qualification or years of working experience. However, having been trained on ‘HIV treatment’ and ‘Psychosocial care and support of PLHIV’ were associated with staff willingness to dispense ARVs. Indeed, these components of HIV care and treatment are particularly important for staff to be able to effectively dispense ARVs. Training in these areas therefore increases their confidence and willingness to adopt the model.
Infrastructure and storage conditions
This study has shown a high level of infrastructure compliance by community pharmacies. The adequacy of storage space (99.6%) was found to be superior to the results of a study conducted in Pakistan. The storage capacity was sufficient in 81.2% of community pharmacies in the Pakistan study. Protection of medicines from direct sunlight was also high (100%) compared to the findings of the Pakistan study where 40.2% of pharmacies protected products from direct sunlight. Cleanliness conditions were found to be sufficient with surfaces free of signs of rodents, parasites, and insects in 98.1% of cases, compared to 89.8% in the Pakistani study (Shah et al., Citation2016).
The level of infrastructure compliance observed in this study can be justified by the fact that the adequacy of storage space is one of the parameters that are systematically assessed by the Rwanda FDA before a Pharmacy is granted a license and before moving to new premises.
The proportion of community pharmacies having a room that could be dedicated for special care requiring one-on-one interaction between the health care provider and the patient (90.5%) was found to be similar to that of the South-East Nigerian study where >90% of community pharmacies had a counselling section or room (USAID/PEPFAR EP, Citation2019). The finding is higher than the result from an assessment conducted in three counties of Kenya, where 84.7% of the community pharmacies surveyed had a private room that could be used for counselling PLHIV while dispensing ARVs (USAID PHPP, Citation2021). The good results achieved in terms of storage and infrastructure can be linked to the fact that community pharmacy premises are inspected and validated by the regulatory authorities (Rwanda FDA, Citation2022).
Willingness to dispense ARVs, anticipated benefits and challenges
The proportion of community pharmacy personnel who are willing to dispense antiretroviral medicines in their premises (93.9%) was found to be higher than the one from the study in South-East Nigeria where 62.9% of community pharmacists expressed their willingness for the use of pharmacy premises to provide HIV services (PEPFAR EP, Citation2021). However, it is slightly lower than the findings from the assessment in three counties of Kenya, where 95% of community pharmacies that have been interviewed were willing to dispense antiretroviral medicines to clients referred by ART facilities (USAID PHPP, Citation2021). In all the settings, respondents were not yet involved in the dispensing of ARVs, and the level of willingness observed is a sign that capacity building programmes would better prepare them for the provision of these services.
If dispensing of antiretroviral medicines through community pharmacies is adopted, only 26.3% of all the respondents feel that the service should be offered free of charge to clients. This finding is higher than the results of the assessment in Kenya, where 8% of pharmacies surveyed said they would provide the services free of charge to the clients (USAID PHPP, Citation2021). This study did not assess potential beneficiaries’ preference on this aspect, but in a different context, a baseline assessment among PLHIV in Nigeria found in 2016 that only 21% of clients agreeing to receive their antiretroviral medication at community pharmacies were willing to pay a service fee (Ajagu et al., Citation2017). If the leadership of the Ministry of Health and the national HIV programme intend to introduce this model in Rwanda, the necessary consultations must take place to decide on the amount of the dispensing fee, considering factors such as clients’ willingness and ability to pay, the need for community pharmacies to collect the fee, and the costs they incur when dispensing antiretroviral medicines.
The results for anticipated benefits in terms of increased sales of over the counter (OTC) and other medicines, expanded community pharmacies involvement in public health service provision, increased opportunities for capacity building, are higher but comparable to a study conducted in Kenya. The most important anticipated benefit identified by the Kenya study was that pharmacies believed that the model would expand their involvement in public health service delivery (70%) and provide more opportunities for staff training in antiretroviral medicines dispensing (66.3%). They also felt that the distribution of antiretroviral medicines on their premises would lead to an increase in the number of potential clients, including PLHIV and those accompanying them, and therefore an increase in sales (63.7%) for OTC and other non-HIV commodities (USAID PHPP, Citation2021).
Community pharmacy staff in Rwanda see their involvement in ARVs dispensing as an opportunity to help reduce the workload at public health facilities through the decentralisation of services. The expected benefits from the results of all these studies indicate how the involvement of community pharmacies in ARV dispensing would be beneficial to both the public and private sectors.
The high rates of expected benefits combine with the willingness of staff, the availability of counselling rooms for patients, and the understanding of the relevance of obtaining such a room if it is not available, as favourable factors for the introduction of ARVs distribution through community pharmacies in Rwanda.
It is important to note that the community pharmacy personnel that have participated in the study included pharmacists and nurses. The presence of pharmacists and nurses constitutes an opportunity for community pharmacies to appropriately provide patient care to PLHIV. Indeed, effective collaboration between pharmacists and nurses results in positive outcomes regarding medication safety. Different issues that pertain to the patient, provider or system related factors can be addressed through strong collaboration. Collaborative efforts facilitate the assessment and resolution of problems that include inappropriate medicine prescription, patient adherence and education as well as overall lifestyle management (Ravi et al., Citation2022).
Study limitations
This research did not carry out a formal assessment of the knowledge on HIV prevention and management among community pharmacy staff. For each of the pharmacies visited, elements of readiness that were assessed included staff training on HIV, their willingness to dispense antiretroviral medicines, and the infrastructure readiness. A literature review was carried out to assess policy provisions for the dispensing of antiretroviral medicines through community pharmacies. This study did also not assess clients’ willingness to refill their medicines at community pharmacies.
Conclusion
Community pharmacies in Rwanda have majority of staff trained in various areas of HIV prevention, but a small proportion have been trained in HIV care and treatment. Community pharmacies have the necessary infrastructure to dispense ARVs, and those with shortcomings, such as the lack of a separate room for individual patient counselling, are willing to obtain such a room if they are authorised to dispense ARVs. Staff are willing to dispense ARVs in community pharmacies if the model is recommended by policymakers. The model could have several benefits for community pharmacies and the public health system in general, but there are also challenges that should be mitigated to ensure effective implementation. The staff willingness and expected benefits constitute enabling factors that the Ministry of Health and the national HIV control programme may leverage to prepare for introducing the model of ARVs distribution through community pharmacies.
Based on the results of this research, future investigators should explore other factors such as the willingness of stable PLHIV to have their medications refilled by community pharmacies, as well as the feasibility and service cost preferences for ARV dispensing through community pharmacies.
Ethics approval and consent to participate
The ethical approval for this study was obtained from the College of Medicine and Health Sciences of the University of Rwanda through its Institutional Review Board (Reference number: CMHS/IRB/028/2023). Nobody was influenced to participate in the study. A conversation was used to inform the community pharmacy staff of the purpose of the study and the information required from them. Any questions potential participants had about the study were answered, and only staff who gave oral consent to participate were considered for the study. No signed consent was used for this research.
Consent for publication
Not applicable.
Availability of data and materials
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors do not have any conflict of interest; they have no affiliations with or involvement in any organisation or entity with any financial or non-financial interest in the subject matter or materials discussed in this manuscript.
Acknowledgements
The authors of this paper gratefully acknowledge the funding of the Master of Health Supply Chain Management by the German Federal Ministry for Economic Cooperation and Development (BMZ) through KfW Development Bank and the East African Community Regional Centre of Excellence for Vaccines, Immunization, and Health Supply Chain Management. In addition, this research would not have been possible without the assistance of the College of Medicine and Health Sciences, University of Rwanda. Authors’ contribution. CM contributed to the conception, methodology, data collection and their analysis, writing of the original draft and reviewed the final manuscript. JBN and IH contributed to conception of the study and reviewed the manuscript. All authors gave final approval to the version to be published, agreed on the journal to which the article had been submitted, and agreed to be accountable for all aspects of the work.
Additional information
Funding
Notes on contributors
Cyprien Musafiri
Cyprien Musafiri is a Pharmacist with sound experience in public health commodities supply chain management. He holds a Master's degree in Pharmaceutical Sciences/Quality Assurance and Quality Control and a Master's degree in Health Supply Chain Management, both from the University of Rwanda. Cyprien Musafiri has served in a variety of positions that have enabled him to acquire solid experience in health products sourcing, warehousing, inventory management, distribution, promoting rational medicine use, safety monitoring, managing human and financial resources for health, supply chain workforce capacity development and overall system optimization. He has received various training and certifications, including the certification in humanitarian medical logistics practices and the management of medicines in international health. Cyprien Musafiri has held various positions in Rwanda including Director of District Pharmacy, Senior Officer for HIV Commodities Management and Specialist in charge of Pharmaceutical Development and Supply Chain Coordination at the Ministry of Health. He currently works as Health Products Management Specialist for the Global Fund to fight AIDS, Tuberculosis and Malaria.
Jean Baptiste Nyandwi
Dr. Jean Baptiste Nyandwi holds a BPharm degree from National University of Rwanda, a Master's degree in Pharmaceutical Sciences, Quality Control and Quality Assurance from University of Rwanda (Rwanda) in collaboration with University of Liege (Belgium), and a PhD in Science (Convergence Medical Science) from Gyeongsang National University, South Korea in the area of Molecular Pharmacology. Dr. Nyandwi is a Lecturer and Researcher in Pharmacy Department for a decade and former head of Pharmacy Department at the University of Rwanda. He also serves as the Training Coordinator at the EAC Regional Centre of Excellence for Vaccines, Immunization and Health Supply Chain Management (RCE-VIHSCM). He oversees and coordinates capacity building and talent development in the area of vaccines manufacturing, vaccinology, regulatory affairs and supply chain management at the EAC RCE-VIHSCM. Dr. Nyandwi is a member of National Pharmacovigilance Advisory Committee of Rwanda Food and Drugs Authority since 2021 and seats as member of Technical Committee (TC) on Pharmaceutical Products of Rwanda Standards Board (RSB/TC 015) since 2018. He is also a member of Regulatory Capacity Development Sub Technical Committee (RCD- Sub TC) on Vaccines Regulatory Oversight of AUDA-NEPAD. Dr. Nyandwi is a Pharmacist by profession and registered as a Senior Consultant Pharmacist in Rwanda. He has expertise in developing and implementing academic programmes. He has authored a number of peer reviewed papers in peer-reviewed international journals in pharmacology and pharmacy sphere and serves as a reviewer of different peer reviewed Journals.
Innocent Hahirwa
Dr Innocent Hahirwa is a Senior Lecturer and a Senior Consultant Pharmacist with a Ph.D in Biomedical and Pharmaceutical Sciences/Clinical Toxicology from University of Liege (Belgium). Technically, he has an extensive experience in teaching, research, administration and clinics. In addition to the formal academic training, Dr Hahirwa has been trained in different areas of Pharmacy profession including, Pharmacy profession regulation, Drug registration, Pharmacovigilance, Pharmaceutical products (including hazardous products) handling and Clinical Trials. Dr HAHIRWA is teaching different courses related to Toxicology, Pharmacology, Pharmacovigilance and Clinical trials at both Undergraduate and Postgraduate levels, and has supervised a number of research works for UG and PG students. He is also in charge of clinical pharmacy care and training in Kigali University Teaching Hospital. His research areas of interest include mainly Toxicology, Pharmacology, Clinical Biology as well as Pharmacy practice and regulation. Having occupied different managerial positions including being the Chairperson and a member of the National Pharmacy Council Board, Head of Pharmacy Department and Deputy Dean of the School of Medicine and Pharmacy at the University of Rwanda for several years, Dr HAHIRWA has strong leadership and management skills.
References
- Ajagu, N., Anetoh, M. U., & Nduka, S. O. (2017). Expanding HIV/AIDS care service sites: A cross sectional survey of community pharmacists’ views in South-East, Nigeria. Journal of Pharmaceutical Policy and Practice, 10(1), 34. http://joppp.biomedcentral.com/articles/10.1186s40545-017-0122-x.
- Avong, Y. K., Aliyu, G. G., Jatau, B., Gurumnaan, R., Danat, N., Kayode, G. A., Adekanmbi, V., & Dakum, P. (2018). Integrating community pharmacy into community based anti-retroviral therapy program: A pilot implementation in Abuja, Nigeria. PLoS One, 13(1), e0190286. doi:10.1371/journal.pone.0190286
- PEPFAR EP. (2021). Decentralized drug distribution of antiretroviral therapy in Eswatini: Final Report [Internet]. Retrieved Apr 28, 2022, from https://www.fhi360.org /sites/default/files/media/documents/epic-ddd-eswatini-report.pdf..
- PEPFAR Solutions Platform. (2020). Leveraging private pharmacists to expand ART Distributi on, promote adherence, and mobilize resources [Internet]. [cited 2022 Apr 28]. https://static1.squarespace.com/ static/ 5a29b53af9a61e9d04a1cb10/t/ 5ea 080a9264fa24dbb0dd80b/1587577001993/Leveraging(Private(Pharmacies_22April2020.pdf.
- Ravi, P., Pfaff, K., Ralph, J., Cruz, E., Bellaire, M., & Fontanin, G. (2022). Nurse-pharmacist collaborations for promoting medication safety among community-dwelling adults: A scoping review. International Journal of Nursing Studies Advances, 4, 100079. doi:10.1016/j.ijnsa.2022.100079
- Rwanda FDA. (2022). Guidelines for licensing of public and private manufacturers, distributors, wholesalers and retailers of medical products [Internet]. Retrieved Apr 2, 2023, from https://rwandafda.gov.rw/wp-content /uploads /2022/11/Guidelines on licensing _of_public_and_private_manufacturer__distributors_wholesalers_and_retailers_of_medical_products.pdf.
- Rwanda Food and Drugs Authority. (2022). List of licensed human retail pharmacies_November 2022. Retrieved Nov 10, 2022, from https://rwandafda.gov.rw/medicine-inspection-registered-premises/.
- Rwanda Ministry of Health. (2016). National guidelines for prevention and management of HIV and STIs [Internet]. Retrieved May 5, 2022, from http://rbc.gov.rw/fileadmin/userupload/guide/SIGNED%20ENGLISH%20%202016%20VERSION.pdf.
- Shah, S. S. A. M., Naqvi, B. S., Fatima, M., Khaliq, A., Sheikh, A. L., & Baqar, M. (2016). Quality of drug stores: Storage practices & regulatory compliance in Karachi, Pakistan. Pak J Med Sci., 32(5), 1071–1076.
- Sharp, P. M., & Hahn, B. H. (2011). Origins of HIV and the AIDS pandemic. Cold Spring Harbor Perspectives in Medicine, 1(1), a006841. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3234451/.
- UNAIDS. (2022). Latest global and regional statistics on the status of HIV & AIDS-Fact sheet 2022. [Internet]. Retrieved Feb 24, 2023, from https:// www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf.
- USAID/PEPFAR EP. (2019). Decentralized distribution of antiretroviral therapy through the private sector. A strategic guide for scale-up. [Internet]. Retrieved Apr 28, 2022, from https://www.fhi360.org/sites/default/files/media/documents/epic-project-strategic-guide-scale-up.pdf.
- USAID PHPP. (2021). Preferences for antiretroviral refill and pickup through community pharmacies in Busia, Kajiado, and Nairobi Counties. [Internet]. Retrieved Jun 3, 2022.http://www.healthpolicyplus.com/ns/pubs/18523-18927_KenyaARV.pdf.
- World Health Organization. (2021). Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: Recommendations for a public health approach, 548. Retrieved Oct 25, 2023, from https://www.who.int/publications/i/item/9789240031593.