ABSTRACT
Dendritic- cells (DCs) have received considerable attention as potential targets for the development of anticancer vaccines. DC-based anticancer vaccination relies on patient-derived DCs pulsed with a source of tumor-associated antigens (TAAs) in the context of standardized maturation-cocktails, followed by their reinfusion. Extensive evidence has confirmed that DC-based vaccines can generate TAA-specific, cytotoxic T cells. Nonetheless, clinical efficacy of DC-based vaccines remains suboptimal, reflecting the widespread immunosuppression within tumors. Thus, clinical interest is being refocused on DC-based vaccines as combinatorial partners for T cell-targeting immunotherapies. Here, we summarize the most recent preclinical/clinical development of anticancer DC vaccination and discuss future perspectives for DC-based vaccines in immuno-oncology.
Introduction
The presentation of antigenic material to cells of the adaptive immune system, notably CD4+ helper T cells and CD8+ cytotoxic T lymphocytes (CTLs), is a crucial function of myeloid cells,Citation1,Citation2 as it stands at the basis of both antigen-specific immune activation and tolerance.Citation3–Citation11 Professional antigen-presenting cells (APCs) are specialized at executing this function, and dendritic cells (DCs) are largely viewed as the most proficient of APCs.Citation7,Citation8,Citation12–Citation18 Indeed, DCs not only present extracellular antigens on MHC Class II molecules to CD4+ T cells,Citation19,Citation20 in thus far resembling macrophages and B cells,Citation21–Citation23 but they also efficiently mediate cross-presentation, i.e., the presentation of extracellular antigens on MHC Class I molecules to CD8+ CTLs, which is key for anticancer immunity.Citation8,Citation24–Citation31 Pioneering research by the team of the Canadian physician Ralph Steinman uncovered the existence of DCs in 1973, an achievement for which he was eventually awarded the 2011 Nobel Prize in Physiology or Medicine.Citation32–Citation35 The name DC reflects the distinguishing morphology of these cells, which can acquire a tree-like shape (from the Greek term “dendron”, translating to “tree”).Citation36–Citation38 Following the discovery of DCs by the Steinman laboratory, considerable efforts have been dedicated to characterize their unique phenotypic and functional features, which firmly position DCs at the interface between innate and adaptive immunity.Citation8,Citation13,Citation39–Citation51
DCs are common throughout the body, although they are relatively more abundant in tissues that are in contact with the external environment, such as epithelial tissues.Citation5,Citation16,Citation52–Citation66 DCs are highly heterogeneous in terms of ontogeny,Citation67–Citation69 function, responsiveness to selected stimuli and preference for specific sources of antigens for presentation.Citation16,Citation70–Citation77 These features have been harnessed to generate ever more refined biological classifications of DCs into different subsets.Citation76,Citation78–Citation81 In particular, both human and mouse DCs can be morphologically classified into 2 major subsets: myeloid DCs, which are also known as conventional or classical DCs (cDCs) and (prior to activation) resemble circulating monocytes,Citation82–Citation84 and plasmacytoid DCs (pDCs), which resemble plasma cells.Citation85–Citation88 Two other DC subsets have been described: CD16+ monocyte-derived (or inflammatory) DCs, and Langerhans cells (LCs), a skin-resident population of DCs with potent immunosuppressive activity.Citation86,Citation89–Citation92 Here, cDCs derive from a common myeloid precursor and can be further classified into two subsets: (1) cDC1, which express CD8α or CD103 in mice, or CD141 in humans; and (2) cDC2, which express CD11b in mice, or CD1c in humans.Citation93 In contrast, pDCs are believed to originate from a poorly defined lymphoid precursor, and are characterized by co-expression of CD45R/B220 and Ly-6C in mice, or CD123 and CD304 in humans.Citation85 An alternative classification for DCs reflects the differential expression of master transcription factors like basic leucine zipper transcription factor ATF-like 3 (BATF3), which is critical for the development of CD8α+ DCs in lymphoid tissues and CD103+CD11b− DCs in peripheral tissues.Citation94–Citation97 High-dimensional analysis techniques (e.g., mass cytometry, single-cell RNA sequencing) have further expanded our understanding on the complexity of DCs, while casting some doubts on the accuracy of the aforementioned classifications.Citation85,Citation86,Citation98
Different DC subsets exhibit functional specialization on a number of immunological levels, including: (1) capturing, processing and presenting antigens (e.g., human CD141+ DCs and mouse CD8α+ DCs are highly proficient at cross-presentation, while CD11b+ DCs efficiently mediate conventional MHC Class II presentation);Citation97,Citation99–Citation105 (2) preferential engagement of adaptive immune cell populations (e.g., CD14+ DCs enriched in the dermis and LCs tend to specifically drive humoral responses and CD8+ T cell effectors, respectively);Citation106,Citation107 and (3) secretion of antiviral and immunomodulatory cytokines such as type I interferon (IFN) (e.g., pDCs mount stronger type I IFN responses as compared to other DC subsets).Citation108–Citation112
In homeostatic conditions, blood-borne as well as tissue-resident DCs exist in an immature functional state, which is key for the preservation of peripheral tolerance to self antigens.Citation113 In particular, immature DCs (iDCs) potently suppress the activity (or even promote the clonal deletion) of self-reactive T cells,Citation45,Citation114 and favor the proliferation of immunosuppressive CD4+CD25+FOXP3+ regulatory T (TREG) cells.Citation27,Citation115–Citation117 The most salient features of iDCs are: (1) prominent potential for the uptake of extracellular material, especially cell corpses, vesicles and other small non-soluble entities, coupled to the secretion of homeostatic cytokines and chemokines; (2) expression of specific chemokine receptors that enable rapid chemotaxis to sites of inflammation; (3) retention of MHC Class II molecules within late endosomes; and (4) minimal surface expression of co-stimulatory molecules like CD40, CD70, CD80, CD83, CD86 and tumor necrosis factor (ligand) superfamily, member 4 (TNFSF4, also known as OX40L).Citation118
In pathological settings, a plethora of microbial cues commonly known as microbe-associated molecular patterns (MAMPs)Citation8,Citation119–Citation121 and endogenous danger signals cumulatively referred to as damage-associated molecular patterns (DAMPs)Citation58,Citation122–Citation128 drive the rapid phenotypic and functional conversion of iDCs into mature DCs (mDCs).Citation129–Citation137 Here, mDCs differ from their immature counterparts as they display: (1) limited phagocytic activity; (2) altered profile of chemokine receptors including high levels of chemokine (C-C motif) receptor 7 (CCR7), which favors DC homing and persistence in lymph nodes; (3) robust exposure of peptide-bound MHC molecules and co-stimulatory ligands on the cell surface; and (4) secretion of pro-inflammatory cytokines such as interleukin 12 (IL12) and T cell-targeting chemokines such as C-X-C motif chemokine ligand 10 (CXCL10).Citation38,Citation116,Citation118,Citation138–Citation149 Thus, mDCs acquire the anatomical location and all the functional properties that are required for optimal T cell priming.Citation150–Citation153
Since the cross-priming of CD8+ CTLs against tumor-associated antigens (TAAs) is critical for the elicitation of robust and durable anticancer immune responses, and this process is often disabled in developing tumors (by a multitude of immunosuppressive strategies deployed by cancer cells),Citation154,Citation155 DCs have attracted considerable attention as potential targets for the development of therapeutic cancer vaccines.Citation156–Citation159 This approach generally involves the differentiation of DCs from autologous, patient-derived monocytes, followed by ex vivo DC exposure to an appropriate source of TAAs in the context of potent maturation cocktails,Citation160 and culminating with the reinfusion of mDCs to the patient. Accumulating clinical evidence demonstrates that this approach often promotes at least some degree of TAA-specific CTLs-driven immunity in patients.Citation8,Citation156,Citation157,Citation161 However, the efficacy of therapeutic DC vaccination is often limited by the robust immunosuppressive circuits that are in place in the microenvironment of most tumors.Citation98,Citation162
Therapeutic DC vaccines developed so far can be broadly classified in different groups based on the approach for TAA-delivery or molecular modifications imposed on DCs before reinfusion.Citation163,Citation164 These groups are: (1) DCs not pulsed with TAAs and employed either in an immature form or used upon maturation with pro-inflammatory cytokines and/or MAMPs or DAMPs;Citation138,Citation165–Citation169 (2) DCs pulsed ex vivo with tumor lysates or tumor-derived mRNA (both of which cover either a broad array of TAAs), specific TAA-based peptides (generally consisting of one or a few selected peptides), or precise TAA-coding mRNAs;Citation59,Citation170–Citation221 (3) DCs provided in vivo with TAAs;Citation222–Citation233 (4) DCs stimulated in situ by immunostimulatory agents applied peritumorally or intratumorally;Citation234 (5) DCs transfected (virally or biochemically) with a genetic vector coding for one or a few TAAs and/or immunostimulatory factors;Citation235 or (6) DC-derived exosomes.Citation236–Citation240 That said, the most common approach to therapeutic cancer vaccination with DCs consists of DCs pulsed with TAAs or tumor lysates and stimulated with standard maturation cocktails.Citation241 Herein, iDC pulsing is usually achieved by: (1) co-incubation with autologous or allogeneic tumor lysates;Citation170–Citation179,Citation242–Citation244 (2) co-incubation with recombinant TAAs or peptides thereof;Citation59,Citation180–Citation186 (3) transfection of TAA-encoding plasmids or mRNAs;Citation187–Citation211,Citation245–Citation248 and, (4) fusion of DCs with inactivated malignant cells, resulting in the generation of so-called “dendritomes”.Citation177–Citation179,Citation212–Citation219,Citation249 The possibility of creating DC vaccines in situ or in vivo by direct TAA delivery has been explored with DC-targeting immunoliposomes,Citation250–Citation252 DC-targeting genetic vectors,Citation253–Citation256 or TAAs fused to monoclonal antibodies or other moieties targeting DC surface receptors.Citation222–Citation228,Citation230,Citation231,Citation233,Citation257,Citation258 The possibility of creating DC vaccines exploiting specific (naturally available) DC subsets has also been explored.Citation259,Citation260 Particularly, specific DC subsets including pDCs, LCs and CD1c+ DCs have been successfully utilized in the clinic for the vaccination of cancer patients.Citation259–Citation261 Notably, sipuleucel-T (commercially sold as Provenge®) is the sole tumor-targeting cellular therapy involving (but not restricted to) DCs that is currently approved by the US Food and Drug Administration (FDA) for use in individuals with asymptomatic or minimally-symptomatic metastatic castration-resistant prostate cancer.Citation262–Citation264
Here, we summarize preclinical and clinical progress in the development of therapeutic cancer vaccines based on DCs. As the cancer immunotherapy landscape is currently dominated by other therapeutic modalitiesCitation265–Citation269 such as immune checkpoint blockers (ICBs) and adoptive T-cell transfer (ACT),Citation270,Citation271 interest is being refocused on implementing DC-based vaccines as part of multimodal (immuno)therapeutic regimens.Citation15,Citation43,Citation272–Citation278 That said, the number of clinical trials currently open to investigate the safety and therapeutic profile of DC vaccination in cancer patients remains high.
Recent preclinical developments
Several preclinical reports dealing with anticancer DC vaccines were published since our last Trial Watch on this topic (February 2017).Citation279 Of this abundant preclinical literature, we found of particular interest the following selected studies, which are largely representative of the overall trends in the field (not discussed in any specific order). Nimanong et al. (from Medical School Hannover, Hannover, Germany) combined DC vaccination with a co-stimulatory cocktail consisting of a CD40 agonistic antibody,Citation280 an agonist of Toll-like receptor 3 (TLR3) (and different combinations of neoantigen-based or TAA-based peptides) and achieved successful remission of large murine subcutaneous MC38 tumors, accompanied by robust antigen-specific T-cell responses.Citation281 Moreno Ayala et al. (from Universidad de Buenos Aires, Buenos Aires, Paraguay) reported that combining DC vaccines with a FOXP3-targeting synthetic peptide (P60) that inhibits TREG cells results in superior antitumor efficacy against murine LM3 or 4T1 mammary carcinomas.Citation282 Liu et al. (from Chinese PLA General Hospital, Beijing, China) tested the efficacy of DC vaccines involving DCs pulsed with glioma-derived exosomes and α-galactosylceramide (α-GalCer), an agonist for invariant natural killer T (iNKT) cells, in combination with adoptively transferred iNKT cells, in an orthotopic rat glioma model, observing efficient induction of antitumor immunity.Citation283 Similarly, Escriba-Garcia et al. (from Hospital de la Santa Creu i Sant Pau, Barcelona, Spain) found that DC vaccines combined with α-GalCer enabled 100% tumor-free survival in a murine model of B-cell lymphoma, correlating with increased effector T-cell functions and expansion of iNKT cells secreting interferon gamma (IFNG).Citation284 Vo et al. (from Chonnam National University Hwasun Hospital, Jeollanamdo, Republic of Korea) successfully combined TAA-based DC vaccination with the immunomodulatory drug lenalidomide, achieving potent antitumor immunity against murine MC38 colorectal carcinoma tumors, which was accompanied by reduction in myeloid-derived suppressor cells (MDSCs)Citation285 and induction of lymphoid effector functions.Citation286 Dammeijer et al. (from Erasmus MC, Rotterdam, Netherlands) documented that the pharmacological inhibitor of colony stimulating factor 1 receptor (CSF1R), PLX3397 (also known as pexidartinib),Citation287,Citation288 which causes depletion of tumor-associated macrophages (TAMs), synergizes with DC vaccines to achieve eradicating immunity in mouse models of mesothelioma.Citation289 Moreno Ayala et al. (from Universidad de Buenos Aires, Buenos Aires, Paraguay) combined DC vaccines with different TLR7 or TLR9 agonists, observing that whereas DCs activated through TLR9 enabled prolonged tumor- and metastasis-free survival, dual TLR7/TLR9 activation impaired vaccination efficacy, a disparity that could be ameliorated by inhibiting nitric oxide synthase (NOS) and indoleamine-pyrrole-2,3-dioxygenase 1 (IDO1).Citation290,Citation291 Ebrahimi-Nik et al. (from University of Connecticut, Farmington, CT, USA) reported DCs to be superior to macrophages at eliciting neoantigen-targeted eradicating immunity in a DC vaccination setup, but surprisingly found CD11c+MHC-IIlow DCs to be the best APCs in this particular setting.Citation26 Montico et al. (from Centro di Riferimento Oncologico, Aviano, Italy) pulsed human DCs with mantle cell lymphoma (MCL) or diffuse large B-cell lymphoma (DLBCL) cells undergoing immunogenic cell death (ICD)Citation292,Citation293 in response to 9-cis-retinoic acid plus type I IFN, which mediated robust anticancer immunity upon inoculation in immunodeficient tumor-bearing mice reconstituted with human peripheral blood mononuclear cells (PBMCs).Citation42 Antonios et al. (from University of California, Los Angeles, California, USA) treated orthotopic glioma-bearing mice with DC vaccines combined with antibodies against programmed cell death 1 (PDCD1, best known as PD-1) and PLX3397, reporting therapeutic benefits only in the context of vaccination.Citation294 Arab et al. (from Tehran University of Medical Sciences, Tehran, Iran) achieved pronounced inhibition of tumor growth and antitumor immunity upon combining DC vaccination with blockade of adenosine A2A receptor (ADORA2A) and 5ʹ-nucleotidase ecto (NT5E, best known as CD73).Citation295 Komorowski et al. (from Roswell Park Comprehensive Cancer Center, Buffalo, NY, USA) achieved robust therapeutic effects against murine neuroblastomas by combining DC vaccines with an oncolytic vaccinia virusCitation296,Citation297 expressing a C-X-C chemokine receptor type 4 (CXCR4) antagonist.Citation298 Stefanski et al. (from University of Minnesota, Minneapolis, Minnesota, USA) pulsed DCs genetically-engineered to overexpress CCL21 with TAAs, and reported the induction of efficient anticancer immunity in mouse models of leukemia.Citation299 Van Woensel et al. (from KU Leuven, Leuven, Belgium) found that combining DC-based vaccines with the intranasal administration of chitosan nanoparticles loaded with small interfering RNAs targeting galectin 1 (LGALS1) drives robust tumor-targeting immune responses in a murine model of orthotopic glioma, correlating with dramatic changes in the tumor microenvironment in favor of M1-polarized macrophages and effector T cells.Citation300 Huang et al. (from Xinhua Hospital and Shanghai Jiaotong University School of Medicine, Shanghai, China) observed that vaccines obtained by pulsing DCs with exosomes from transforming growth factor beta 1 (TGFB1)-defective cancer cells induce superior anti-leukemia immunity in vivo.Citation301 Lu et al. (from Tianjin Medical University, Tianjin, China) found that DC-derived exosomes from DCs expressing a hepatocellular carcinoma (HCC)-associated antigen are very efficient at eliciting CD8+ T cell-dependent eradicating immunity in 3 different mouse models of the disease.Citation302 Bryson et al. (from University of Southern California, Los Angeles, CA, USA) used a Sindbis virus-based method to deliver breast cancer-associated antigens to tumor-resident DCs, resulting in a potent vaccination effect in situ that amplified CD8+ CTL-dependent immunity against murine breast cancer.Citation303 Liu et al. (from University of North Carolina at Chapel Hill, Chapel Hill, NC, USA) formulated a nanoparticle-based method to deliver mucin 1 (MUC1)-coding mRNA to lymph node-resident DCs in a mannose receptor-dependent fashion, culminating with expansion of MUC1-reactive T cells and regression of MUC1-expressing 4T1 mammary carcinomas, especially in the context of cytotoxic T-lymphocyte associated protein 4 (CTLA4) blockage.Citation304 Oberli et al. (from Harvard Medical School, Boston, Massachusetts, USA) created a cancer vaccine consisting of DCs, macrophages and neutrophils transfected with an mRNA coding for melanoma antigens and delivered with lipid nanoparticles, which effectively eradicated B16 melanomas in a CD8+ CTL-dependent manner.Citation305 Wennhold et al. (from University Hospital of Cologne, Cologne, Germany) compared the efficacy of antigen-pulsed and CD40-activated B cell and DC vaccines against B16 melanoma and E.G7 lymphoma, observing that B cell-based vaccines perform as efficiently as DC vaccines at inducing antitumor immunity.Citation306 Wculek et al. (from Centro Nacional de Investigaciones Cardiovasculares, Madrid, Spain) showed that splenic cDC1s pulsed with cancer cells undergoing ICD were able to induce therapeutic immune responses that synergized with PD-1 blockade,Citation307 supporting a mechanistic link between ICD-inducing systemic anticancer therapies and cDC1-dependent antigen cross-presentation.Citation307–Citation320 This finding extends prior observations indicating that human CD1c+ DCs are critical for the presentation of tumor antigens from cancer cells succumbing to ICD.Citation8,Citation103,Citation321–Citation323 Finally, Ventura et al. (Yale University School of Medicine, New Haven, CT, USA) identified a novel approach to generate potent, cytokine-independent DCs, that involves the physical interaction of circulating monocytes with platelets, potentially opening a completely unexplored avenue to DC-based vaccine.Citation324
These are only a few examples of the abundant preclinical literature on therapeutic DC vaccines with oncological applications, demonstrating a persistent interest in this promising but only partially realized therapeutic paradigm.
Completed clinical studies
We identified 34 peer-reviewed papers published since the release of our latest Trial Watch on therapeutic DC-based vaccines for oncological indications (February 2017)Citation279 reporting safety and efficacy data from clinical trials assessing this therapeutic paradigm in patients with cancer.
The majority of these studies () tested autologous DCs pulsed with: TAAs or peptides thereof,Citation325–Citation342 autologous cancer cell lysates,Citation343–Citation348 or TAA-coding RNAs.Citation276,Citation349–Citation352 The predominant use of these TAA sources for the generation of DC-based vaccines is in line with previous trends, as documented in our previous Trial Watch on this subject,Citation279 de facto reflecting a broad consensus in the field. Additional TAA sources explored in recent clinical studies include (): lysates of autologous (tumor) stem cells, lysates of allogeneic cancer cell lines, and TAA-encoding viral vectors.Citation353–Citation355 Of note, one of these clinical studies involved DC vaccines based on personalized antigenic peptides.Citation335 Moreover, a Phase I clinical study investigated an acute myeloid leukemia (AML)-derived cell line as allogeneic DC vaccine (DCP-001), owing to its DC-like behavior and expression of AML-relevant antigens.Citation356 Finally, autologous DCs have been investigated in combination with cytokine-induced killer (CIK) cellsCitation357 for the therapy of advanced pancreatic carcinoma.Citation358
Figure 1. Overview of current strategies of dendritic cell vaccination for cancer therapy. ACPP, acid phosphatase, prostate; AML, acute myeloid leukemia; CEA, carcinoembryonic antigen; CLL, chronic lymphocytic leukemia; CRC, colorectal cancer; DC, dendritic cell; DKK1, dickkopf WNT signaling pathway inhibitor 1; EPS8, epidermal growth factor receptor pathway substrate 8; HCC, hepatocellular carcinoma; KRAS, KRAS proto-oncogene, GTPase; MUC1, mucin 1, cell surface associated; NSCLC, non-small cell lung cancer; NY-ESO-1 (official name: CTAG1B), cancer/testis antigen 1B; CMV pp65, cytomegalovirus 65 kDa phosphoprotein; PSA (official name: KLK3), kallikrein related peptidase 3; RCC, renal cell carcinoma; RNF43, ring finger protein 43; TAA, tumor-associated antigen; TERT, telomerase reverse transcriptase; WT1, WT1 transcription factor.
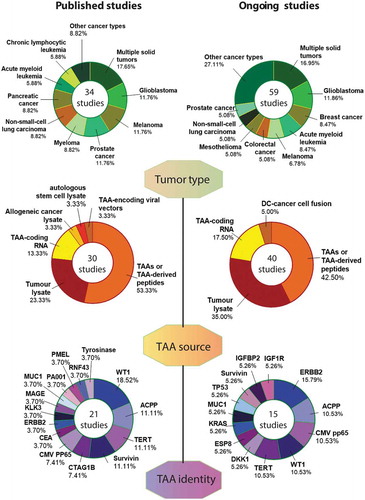
Most of the aforementioned clinical studies based on specific TAAs focused on WT1 transcription factor (WT1),Citation327,Citation328,Citation337,Citation342,Citation349 acid phosphatase, prostate (ACPP),Citation276,Citation325,Citation329 telomerase reverse transcriptase (TERT)Citation276,Citation333,Citation351 or baculoviral IAP repeating containing 5 (BIRC5, best known as survivin)Citation276,Citation333,Citation340 (). This configuration partly deviates from the trend identified in our latest Trial Watch dealing with DC-based vaccines.Citation279 Indeed, while WT1 remains amongst the most commonly targeted TAAs, interest in melanoma-associated differentiation antigens has decreased,Citation337 irrespective of melanoma remaining among the most common indications for experimental DC vaccination ().
While most of these clinical studies were basket trials enrolling patients with multiple solid tumors (),Citation326,Citation331,Citation336,Citation348 studies focusing on single indications most commonly enrolled patients with melanoma,Citation332,Citation337,Citation339,Citation343 prostate cancer,Citation276,Citation325,Citation329,Citation353 or glioblastoma (GBM).Citation341,Citation346,Citation350,Citation352 This was followed by pancreatic cancer,Citation327,Citation333,Citation358 non-small cell lung carcinoma (NSCLC),Citation338,Citation340,Citation354 and myelomaCitation330,Citation334,Citation345 (). This trend was very similar to the one we described in 2017,Citation279 with the single exception of studies enrolling subjects with renal cell carcinoma (RCC), which declined over the past 2 years.
In most clinical studies, DC vaccines were administered in combination with standard-of-careCitation348 or off-label chemotherapeutics (e.g., gemcitabine, cyclophosphamide, S-1, temozolomide, carboplatin, paclitaxel or docetaxel),Citation276,Citation326–Citation328,Citation337,Citation338,Citation341,Citation344,Citation346,Citation350,Citation358 radiotherapy,Citation335,Citation341,Citation346 targeted anticancer agents (e.g., tyrosine kinase inhibitors),Citation328,Citation344 or specific immunotherapeutic regimens, including recombinant colony stimulating factor 2 (CSF2, best known as GM-CSF), recombinant IL2, ACT, and TL3 agonists.Citation326,Citation333,Citation344,Citation352,Citation353
Importantly, the vast majority of these clinical studies confirmed that DC-based vaccines are safe for cancer patients,Citation359 causing mild-to-moderate side effects including fever, erythema, flu-like symptoms, rash and/or fatigue, in a small proportion of patients.Citation328,Citation333,Citation335,Citation340,Citation341,Citation348 Signs of ongoing TAA- or tumor-targeting effector responses upon vaccination, including (but not limited to) increased antigen-specific T- or B-cell activity and tumor infiltration by CD8+ CTLs, were consistently documented.Citation327,Citation332,Citation355 Moreover, multiple clinical studies reported promising clinical responses to vaccination, including disease stabilizationCitation326,Citation328,Citation333,Citation342,Citation344,Citation354 as well as a few partial and complete responses.Citation330,Citation335,Citation345,Citation347–Citation349 Encouragingly, a few cases of robust extension in patient survival were also documented.Citation327,Citation351,Citation356,Citation358 For example, DCs pulsed with TAAs from GBM stem cells provided significant progression-free and overall survival advantage (as compared to placebo) to a cohort of 43 patients with GBM enrolled in a Phase II clinical trial.Citation341 Similarly, AML patients at very high risk of relapse receiving DCs transfected with WT1 mRNA exhibited a higher 5-year overall survival rate as compared to historical controls.Citation349 Altogether, these publications capture the promise offered by DC vaccination in specific oncological settings.
Ongoing clinical trials
For the period between February 2017 to February 2019, official sources (http://www.clinicaltrials.gov/) list no less than 59 clinical trials evaluating the safety and therapeutic profile of DC-based vaccines in cancer patients. The specifics of these clinical trials are summarized in .
Table 1. Overview of clinical trials currently testing dendritic cell-based immunotherapy in cancer patients.
In these studies, the most common approaches consist of autologous DCs pulsed with TAAs or peptides thereof, lysates from autologous tumor cells, or TAA-coding RNA ( and ). The clinical trials targeting specific TAAs focus on WT1, erb-b2 receptor tyrosine kinase 2 (ERBB2), ACPP, and the human cytomegalovirus protein 65 kDa phosphoprotein (pp65) ( and ). As an alternative, multiple ongoing clinical trials favor the use of TAA or TAA-derived peptide mixtures, including blends of mutated peptides or neoantigens (pre-defined or personalized), or melanoma-specific TAA-derived peptides ().
As for indication, most of ongoing clinical studies focusing on DC vaccines are basket trials and enroll patients with multiple solid tumors ( and ). Restricted studies most commonly accrue patients with breast carcinoma and GBM, followed by patients with colorectal carcinoma, melanoma, mesothelioma and prostate cancer ( and ). Notably, there are at least three advanced-phase clinical trials testing therapeutic DC-based vaccines in cancer patients: a Phase II/III study enrolling GBM patients (NCT03548571), a Phase II/III trial enrolling patients with mesothelioma (NCT03610360), and a Phase III study open to individuals with prostate cancer (NCT03686683) (). This indicates that at least some DC-based vaccines have reached advanced clinical development, and may soon be evaluated for approval by regulatory authorities.Citation158,Citation278
Interestingly, the majority of the ongoing clinical trials administer DC-based vaccines in combination with ICBs targeting PD-1, such as pembrolizumab or nivolumab, CD274 (best known as PD-L1), such as avelumab, or CTLA4, like ipilimumab, alone or in different combinations (). Alternatively, DC vaccination is performed in combination with other immunotherapeutic modalities, including adoptively transferred chimeric antigen receptor (CAR)-expressing T cells, CIK cells or autologous NK cells,Citation360 recombinant cytokines,Citation361,Citation362 immunostimulatory antibodies (e.g., varlilumab),Citation363,Citation364 or MAMP-based immunostimulants (e.g. tetanus toxoid or tetanus-diphtheria vaccine).Citation250,Citation365,Citation366 Additional combinatorial partners for DC-based vaccines in clinical development include: (1) standard-of-care neoadjuvant chemotherapy based on ICD inducers like cyclophosphamide or non-ICD inducers like temozolomide and decitabine;Citation291,Citation367 (2) radiotherapy;Citation368 or (3) targeted therapies (e.g. the tyrosine kinase inhibitor axitinib).Citation289,Citation369,Citation370 Finally, some clinical studies are testing innovative strategies that may support immunity, such as hyperthermia.Citation371,Citation372
In summary, as compared to the clinical trials we discussed in the previous Trial Watch dealing with DC-based vaccination,Citation279 the tendency for currently described studies is to combine DC-based vaccines with other forms of immunotherapy (rather than traditional treatments), which largely reflects the progress of immuno-oncology for the past 2 years.Citation270,Citation271
Status update on clinical trials
These following clinical trials have changed status since the publication of our latest Trial Watch on DC-based vaccination for cancer therapy (February 2017):Citation279 NCT02432846, NCT02366728, NCT02405338, NCT02529072, NCT02692976 and NCT02728102 were previously listed as “Recruiting” but are now listed as “Active, not recruiting”; NCT02993315 shifted from “Active” to “Recruiting”; NCT02709993 and NCT02775292 are now “Recruiting”; and NCT02248402 was previously listed as “Completed” but is now “Unknown”. Moreover, NCT02615574, NCT02745756 and NCT02705703 have been “Withdrawn”, the latter following the decision of the study sponsor to discontinue development, whereas NCT02548169 was “Terminated” due to loss of funding and NCT02851056 is “Suspended”, pending interim analyses.
Concluding remarks
The number of published and ongoing clinical trials testing DC vaccination as a therapeutic approach to malignant disorders suggest that there is a persisting interest in identifying indications for which this immunotherapeutic regimen would offer a good alternative to (or improve the efficacy of) ICBs and ACT. Current efforts in this sense appear to focus on GBM, which is known to be particularly susceptible to DC vaccination.Citation158,Citation373,Citation374
In a scenario in which several new immunotherapies are constantly entering clinical development, such as the current one,Citation270,Citation375–Citation383 it is evident that only clinical trials demonstrating a clear survival advantage may drive the approval of DC-based vaccines by regulatory authorities. It is therefore encouraging to note that there are at least three advanced (Phase II/III-III) clinical trials currently testing DC-based vaccines in patients with cancer. The results of these studies are eagerly awaited, especially since data from another highly anticipated Phase III trial testing DC-based vaccines in subjects with GBM were not as promising as expected.Citation384
The clinical development of DC-based vaccines for oncological indications has been negatively impacted by the commercial failure of Sipuleucel-T as well as by disappointing efficacy in multiple (sometimes poorly designed) clinical studies completed so far.Citation385–Citation387 Indeed, although DC-based vaccines have demonstrated at least some degree of clinical activity in some studies,Citation158 their long-term efficacy depends on a number of parameters that are often underestimated, encompassing the immunosuppressive circuitries that are in place in the microenvironment of most solid tumors,Citation130,Citation271,Citation363,Citation388 the evolution of antigen-loss variants,,Citation389 and the overall immunological competence of the patient.Citation156,Citation157 Furthermore, manufacturing DC-based vaccines involves elevated production costs and robust regulatory scrutiny, which constitute additional obstacles to development.Citation157
Finally, the lack of robust predictive biomarkers of response to DC-based vaccines limit enthusiasm, in particular when production costs are considered.Citation342,Citation390–Citation394 At odds with ICBs,Citation267 DC-based vaccines are indeed associated with mild side effects,Citation156,Citation157 implying that current efforts to identify predictive biomarkers are mainly aimed at increasing signal-to-noise ratio and support the design of clinical trials focused on patient subsets that are most likely to benefit from treatment. Our hope is that such efforts will soon be successful and drive the development of safe and effective DC-based vaccines for oncological indications.
Acknowledgements
ADG and PA are supported by Research Foundation Flanders’ (FWO) Excellence of Science (EOS) grant (30837538) for the ‘DECODE’ consortium. ADG is supported by KU Leuven via POR award funds (POR/16/040) and FWO Postdoctoral Fellowship (2016–2019). PA is supported by the FWO fundamental research grants (G0584.12N, K202313N, GA01111N) and KU Leuven (C16/15/073). AC is supported by the Kom Op Tegen Kanker (Stand up to Cancer), the Flemish cancer society (2016/10728/2603), the Olivia Fund (2017/LUF/00135) and the KU Leuven (C24/18/064). GK is supported by the Ligue contre le Cancer (équipe labellisée); Agence National de la Recherche (ANR) – Projets blancs; ANR under the frame of E-Rare-2, the ERA-Net for Research on Rare Diseases; Association pour la recherche sur le cancer (ARC); Cancéropôle Ile-de-France; Chancelerie des universités de Paris (Legs Poix), Fondation pour la Recherche Médicale (FRM); a donation by Elior; European Research Area Network on Cardiovascular Diseases (ERA-CVD, MINOTAUR); Gustave Roussy Odyssea, the European Union Horizon 2020 Project Oncobiome; Fondation Carrefour; High-end Foreign Expert Program in China (GDW20171100085 and GDW20181100051), Institut National du Cancer (INCa); Inserm (HTE); Institut Universitaire de France; LeDucq Foundation; the LabEx Immuno-Oncology; the RHU Torino Lumière; the Seerave Foundation; the SIRIC Stratified Oncology Cell DNA Repair and Tumor Immune Elimination (SOCRATE); and the SIRIC Cancer Research and Personalized Medicine (CARPEM). LG is supported by a Breakthrough Level 2 grant from the US DoD, Breast Cancer Research Program (BCRP) [#BC180476P1], by a startup grant from the Dept. of Radiation Oncology at Weill Cornell Medicine (New York, US), by industrial collaborations with Lytix (Oslo, Norway) and Phosplatin (New York, US), and by donations from Phosplatin (New York, US), the Luke Heller TECPR2 Foundation (Boston, US) and Sotio a.s. (Prague, Czech Republic).
References
- Inglesfield S, Cosway EJ, Jenkinson WE, Anderson G. Rethinking Thymic Tolerance: lessons from Mice. Trends Immunol. 2019;40:279–21. doi:10.1016/j.it.2019.01.011.
- Schuijs MJ, Hammad H, Lambrecht BN. Professional and ‘Amateur’ Antigen-Presenting Cells In Type 2 Immunity. Trends Immunol. 2019;40:22–34. doi:10.1016/j.it.2018.11.001.
- Veglia F, Gabrilovich DI. Dendritic cells in cancer: the role revisited. Current Opinion in Immunology. 2017;45:43–51. doi:10.1016/j.coi.2017.01.002.
- Nilsson JS, Abolhalaj M, Lundberg K, Lindstedt M, Greiff L. Dendritic cell subpopulations in nasopharyngeal cancer. Oncology Letters. 2019;17:2557–2561. doi:10.3892/ol.2018.9835.
- Sautes-Fridman C, Petitprez F, Calderaro J, Fridman WH. Tertiary lymphoid structures in the era of cancer immunotherapy. Nature Reviews Cancer. 2019;19:307–325. doi:10.1038/s41568-019-0144-6.
- Grees M, Sharbi-Yunger A, Evangelou C, Baumann D, Cafri G, Tzehoval E, Eichmüller SB, Offringa R, Utikal J, Eisenbach L, et al. Optimized dendritic cell vaccination induces potent CD8 T cell responses and anti-tumor effects in transgenic mouse melanoma models. Oncoimmunology. 2018;7:e1445457. doi:10.1080/2162402X.2018.1445457.
- Berraondo P, Labiano S, Minute L, Etxeberria I, Vasquez M, Sanchez-Arraez A, Teijeira A, Melero I. Cellular immunotherapies for cancer. Oncoimmunology. 2017;6:e1306619. doi:10.1080/2162402X.2017.1306619.
- Bol KF, Schreibelt G, Rabold K, Wculek SK, Schwarze JK, Dzionek A, Teijeira A, Kandalaft LE, Romero P, Coukos G, et al. The clinical application of cancer immunotherapy based on naturally circulating dendritic cells. J Immunother Cancer. 2019;7:109. doi:10.1186/s40425-019-0580-6.
- Mulder WJM, Ochando J, Joosten LAB, Fayad ZA, Netea MG. Therapeutic targeting of trained immunity. Nat Rev Drug Discov. 2019;18:553–566. doi:10.1038/s41573-019-0025-4.
- Weller M, Roth P, Preusser M, Wick W, Reardon DA, Platten M, Sampson JH. Vaccine-based immunotherapeutic approaches to gliomas and beyond. Nature Reviews Neurology. 2017;13:363–374. doi:10.1038/nrneurol.2017.64.
- Nagaoka K, Hosoi A, Iino T, Morishita Y, Matsushita H, Kakimi K. Dendritic cell vaccine induces antigen-specific CD8(+) T cells that are metabolically distinct from those of peptide vaccine and is well-combined with PD-1 checkpoint blockade. Oncoimmunology. 2018;7:e1395124. doi:10.1080/2162402X.2017.1395124.
- Fang S, Agostinis P, Salven P, Garg AD. Decoding cancer cell death-driven immune cell recruitment: an in vivo method for site-of-vaccination analyses. Methods in Enzymology: Academic Press. 2019. doi:10.1016/bs.mie.2019.04.013.
- Chrisikos TT, Zhou Y, Slone N, Babcock R, Watowich SS, Li HS. Molecular regulation of dendritic cell development and function in homeostasis, inflammation, and cancer. Molecular Immunology. 2019;110:24–39. doi:10.1016/j.molimm.2018.01.014.
- Avigan D, Rosenblatt J. Vaccine therapy in hematologic malignancies. Blood. 2018;131:2640–2650. doi:10.1182/blood-2017-11-785873.
- Garg AD, Agostinis P. Cell death and immunity in cancer: from danger signals to mimicry of pathogen defense responses. Immunol Rev. 2017;280:126–148. doi:10.1111/imr.12574.
- Qian C, Cao X Dendritic cells in the regulation of immunity and inflammation. Seminars in immunology 2018; 35:3–11. doi: 10.1016/j.smim.2017.12.002.
- Kim YS, Park HJ, Park JH, Hong EJ, Jang G-Y, Jung ID, Han HD, Lee S-H, Vo M-C, Lee -J-J, et al. A novel function of API5 (apoptosis inhibitor 5), TLR4-dependent activation of antigen presenting cells. Oncoimmunology. 2018;7:e1472187. doi:10.1080/2162402X.2018.1472187.
- Lee J-H, Tak WY, Lee Y, Heo M-K, Song J-S, Kim H-Y, Park SY, Bae SH, Lee JH, Heo J, et al. Adjuvant immunotherapy with autologous dendritic cells for hepatocellular carcinoma, randomized phase II study. Oncoimmunology. 2017;6:e1328335. doi:10.1080/2162402X.2017.1328335.
- Nanaware PP, Jurewicz MM, Leszyk JD, Shaffer SA, Stern LJ. HLA-DO Modulates the Diversity of the MHC-II Self-peptidome. Molecular & Cellular Proteomics: MCP. 2019;18:490–503. doi:10.1074/mcp.RA118.000956.
- Axelrod ML, Cook RS, Johnson DB, Balko JM. Biological Consequences of MHC-II Expression by Tumor Cells in Cancer. Clinical Cancer Research: an Official Journal of the American Association for Cancer Research. 2019;25:2392–2402. doi:10.1158/1078-0432.CCR-18-3200.
- Kelly A, Trowsdale J. Genetics of antigen processing and presentation. Immunogenetics. 2019;71:161–170. doi:10.1007/s00251-018-1082-2.
- Guerriero JL. Macrophages: their Untold Story in T Cell Activation and Function. International Review of Cell and Molecular Biology. 2019;342:73–93 doi: 10.1016/bs.ircmb.2018.07.001.
- Saez JJ, Lennon-Dumenil AM, Yuseff MI. Studying MHC Class II Presentation of Immobilized Antigen by B Lymphocytes. Methods in Molecular Biology. 2019;1988:419–437. doi: 10.1007/978-1-62703-218-6_39.
- Allen F, Bobanga ID, Rauhe P, Barkauskas D, Teich N, Tong C, Myers J, Huang AY. CCL3 augments tumor rejection and enhances CD8(+) T cell infiltration through NK and CD103(+) dendritic cell recruitment via IFNγ. Oncoimmunology. 2018;7:e1393598. doi:10.1080/2162402X.2017.1393598.
- Borst J, Ahrends T, Babala N, Melief CJM, Kastenmuller W. CD4(+) T cell help in cancer immunology and immunotherapy. Nature Reviews Immunology. 2018;18:635–647. doi:10.1038/s41577-018-0044-0.
- Ebrahimi-Nik H, Corwin WL, Shcheglova T, Das Mohapatra A, Mandoiu II, Srivastava PK. CD11c(+) MHCII(lo) GM-CSF-bone marrow-derived dendritic cells act as antigen donor cells and as antigen presenting cells in neoepitope-elicited tumor immunity against a mouse fibrosarcoma. Cancer Immunology, Immunotherapy: CII. 2018;67:1449–1459. doi:10.1007/s00262-018-2202-4.
- Steinman RM, Hawiger D, Nussenzweig MC. Tolerogenic dendritic cells. Annual Review of Immunology. 2003;21:685–711. doi:10.1146/annurev.immunol.21.120601.141040.
- Hsu JL, Bryant CE, Papadimitrious MS, Kong B, Gasiorowski RE, Orellana D, McGuire HM, Groth BFDS, Joshua DE, Ho PJ, et al. A blood dendritic cell vaccine for acute myeloid leukemia expands anti-tumor T cell responses at remission. Oncoimmunology. 2018;7:e1419114. doi:10.1080/2162402X.2017.1419114.
- Sharbi-Yunger A, Grees M, Cafri G, Bassan D, Eichmuller SB, Tzehoval E, Utikal J, Umansky V, Eisenbach L. A universal anti-cancer vaccine: chimeric invariant chain potentiates the inhibition of melanoma progression and the improvement of survival. Int J Cancer. 2019;144:909–921. doi:10.1002/ijc.31795.
- Jakubzick CV, Randolph GJ, Henson PM. Monocyte differentiation and antigen-presenting functions. Nature Reviews Immunology. 2017;17:349–362. doi:10.1038/nri.2017.28.
- Kroemer M, Spehner L, Mercier-Letondal P, Boullerot L, Kim S, Jary M, Galaine J, Picard E, Ferrand C, Nguyen T, et al. SALL4 oncogene is an immunogenic antigen presented in various HLA-DR contexts. Oncoimmunology. 2018;7:e1412030. doi:10.1080/2162402X.2017.1412030.
- Lanzavecchia A, Sallusto F. Ralph M. Steinman 1943-2011. Cell. 2011;147:1216–1217. doi:10.1016/j.cell.2011.11.040.
- Nussenzweig MC, Mellman I. Ralph Steinman (1943-2011). Nature. 2011;478:460. doi:10.1038/478460a.
- Mellman I, Nussenzweig M. Retrospective. Ralph M. Steinman (1943-2011). Science. 2011;334:466. doi:10.1126/science.1215136.
- Steinman RM, Cohn ZA. Identification of a novel cell type in peripheral lymphoid organs of mice. I. Morphology, quantitation, tissue distribution. J Exp Med. 1973;137:1142–1162. doi:10.1084/jem.137.5.1142.
- Banchereau J, Steinman RM. Dendritic cells and the control of immunity. Nature. 1998;392:245–252. doi:10.1038/32588.
- Steinman RM, Banchereau J. Taking dendritic cells into medicine. Nature. 2007;449:419–426. doi:10.1038/nature06175.
- Merad M, Sathe P, Helft J, Miller J, Mortha A. The dendritic cell lineage: ontogeny and function of dendritic cells and their subsets in the steady state and the inflamed setting. Annual Review of Immunology. 2013;31:563–604. doi:10.1146/annurev-immunol-020711-074950.
- Dudek AM, Martin S, Garg AD, Agostinis P. Immature, Semi-Mature, and Fully Mature Dendritic Cells: toward a DC-Cancer Cells Interface That Augments Anticancer Immunity. Frontiers in Immunology. 2013;4:438. doi:10.3389/fimmu.2013.00438.
- Liu Z, Hao X, Zhang Y, Zhang J, Carey CD, Falo LD Jr., Storkus WJ, You Z. Intratumoral delivery of tumor antigen-loaded DC and tumor-primed CD4(+) T cells combined with agonist alpha-GITR mAb promotes durable CD8(+) T-cell-dependent antitumor immunity. Oncoimmunology. 2017;6:e1315487.
- Dominguez‐Andres J, Netea MG. Long-term reprogramming of the innate immune system. J Leukoc Biol. 2019;105:329–338. doi:10.1002/JLB.MR0318-104R.
- Montico B, Lapenta C, Ravo M, Martorelli D, Muraro E, Zeng B, Comaro E, Spada M, Donati S, Santini SM, et al. Exploiting a new strategy to induce immunogenic cell death to improve dendritic cell-based vaccines for lymphoma immunotherapy. Oncoimmunology. 2017;6:e1356964. doi:10.1080/2162402X.2017.1356964.
- Van Acker HH, Versteven M, Lichtenegger FS, Roex G, Campillo-Davo D, Lion E, Subklewe, M., Van Tendeloo, V.F., Berneman, Z.N., Anguille, S. Dendritic Cell-Based Immunotherapy of Acute Myeloid Leukemia. Journal of Clinical Medicine. 2019:8. doi: 10.3390/jcm8050579.
- Santegoets S, de Groot AF, Dijkgraaf EM, Simoes AMC, van der Noord VE, van Ham JJ, Welters MJP, Kroep JR, van der Burg SH. The blood mMDSC to DC ratio is a sensitive and easy to assess independent predictive factor for epithelial ovarian cancer survival. Oncoimmunology. 2018;7:e1465166. doi:10.1080/2162402X.2018.1465166.
- Yu H, Tian Y, Wang Y, Mineishi S, Zhang Y. Dendritic Cell Regulation of Graft-Vs.-Host Disease: immunostimulation and Tolerance. Frontiers in Immunology. 2019;10:93. doi: 10.3389/fimmu.2019.00093.
- Moussion C, Mellman I. The Dendritic Cell Strikes Back. Immunity. 2018;49:997–999. doi:10.1016/j.immuni.2018.12.007.
- Mitchell D, Chintala S, Dey M. Plasmacytoid dendritic cell in immunity and cancer. Journal of Neuroimmunology. 2018;322:63–73. doi:10.1016/j.jneuroim.2018.06.012.
- Vacchelli E, Vitale I, Eggermont A, Fridman WH, Fucikova J, Cremer I, Galon J, Tartour E, Zitvogel L, Kroemer G. Trial watch: dendritic cell-based interventions for cancer therapy. Oncoimmunology. 2013;2:e25771. doi:10.4161/onci.25771.
- Mastelic-Gavillet B, Balint K, Boudousquie C, Gannon PO, Kandalaft LE. Personalized Dendritic Cell Vaccines-Recent Breakthroughs and Encouraging Clinical Results. Frontiers in Immunology. 2019;10:766. doi:10.3389/fimmu.2019.00766.
- Payandeh Z, Yarahmadi M, Nariman-Saleh-Fam Z, Tarhriz V, Islami M, Aghdam AM, Eyvazi S. Immune therapy of melanoma: overview of therapeutic vaccines. Journal of Cellular Physiology. 2019. doi:10.1002/jcp.28181.
- Bryant CE, Sutherland S, Kong B, Papadimitrious MS, Fromm PD, Hart DNJ. Dendritic cells as cancer therapeutics. Seminars in Cell & Developmental Biology. 2019;86:77–88. doi:10.1016/j.semcdb.2018.02.015.
- Penafuerte C, Feldhammer M, Mills JR, Vinette V, Pike KA, Hall A, Migon E, Karsenty G, Pelletier J, Zogopoulos G, Tremblay ML. Downregulation of PTP1B and TC-PTP phosphatases potentiate dendritic cell-based immunotherapy through IL-12/IFNgamma signaling. Oncoimmunology. 2017;6:e1321185. doi: 10.1080/2162402X.2017.1321185.
- Mikyskova R, Indrova M, Stepanek I, Kanchev I, Bieblova J, Vosahlikova S, Moserova I, Truxova I, Fucikova J, Bartunkova J, et al. Dendritic cells pulsed with tumor cells killed by high hydrostatic pressure inhibit prostate tumor growth in TRAMP mice. Oncoimmunology. 2017;6:e1362528. doi:10.1080/2162402X.2017.1362528.
- Swain S, Roe MM, Sebrell TA, Sidar B, Dankoff J, VanAusdol R, Smythies LE, Smith PD, Bimczok D. CD103 (αE Integrin) Undergoes Endosomal Trafficking in Human Dendritic Cells, but Does Not Mediate Epithelial Adhesion. Frontiers in Immunology. 2018;9:2989. doi:10.3389/fimmu.2018.02989.
- Huo CW, Hill P, Chew G, Neeson PJ, Halse H, Williams ED, Henderson MA, Thompson EW, Britt KL. High mammographic density in women is associated with protumor inflammation. Breast Cancer Research: BCR. 2018;20:92. doi:10.1186/s13058-018-1010-2.
- Bashaw AA, Leggatt GR, Chandra J, Tuong ZK, Frazer IH. Modulation of antigen presenting cell functions during chronic HPV infection. Papillomavirus Research (Amsterdam, Netherlands). 2017;4:58–65. doi:10.1016/j.pvr.2017.08.002.
- Ren J, Gwin WR, Zhou X, Wang X, Huang H, Jiang N, Zhou L, Agarwal P, Hobeika A, Crosby E, et al. Adaptive T cell responses induced by oncolytic Herpes Simplex Virus-granulocyte macrophage-colony-stimulating factor therapy expanded by dendritic cell and cytokine-induced killer cell adoptive therapy. Oncoimmunology. 2017;6:e1264563. doi:10.1080/2162402X.2016.1264563.
- Yatim N, Cullen S, Albert ML. Dying cells actively regulate adaptive immune responses. Nature Reviews Immunology. 2017;17:262–275. doi:10.1038/nri.2017.9.
- Ossevoort MA, Feltkamp MC, van Veen KJ, Melief CJ, Kast WM. Dendritic cells as carriers for a cytotoxic T-lymphocyte epitope-based peptide vaccine in protection against a human papillomavirus type 16-induced tumor. J Immunother Emphasis Tumor Immunol. 1995;18:86–94. doi:10.1097/00002371-199508000-00002.
- Wu C-J, Tsai Y-T, Lee I-J, Wu P-Y, Lu L-S, Tsao W-S, Huang Y-J, Chang -C-C, Ka S-M, Tao M-H. Combination of radiation and interleukin 12 eradicates large orthotopic hepatocellular carcinoma through immunomodulation of tumor microenvironment. Oncoimmunology. 2018;7:e1477459. doi:10.1080/2162402X.2018.1477459.
- Raaijmakers TK, Ansems M. Microenvironmental derived factors modulating dendritic cell function and vaccine efficacy: the effect of prostanoid receptor and nuclear receptor ligands. Cancer Immunology, Immunotherapy: CII. 2018;67:1789–1796. doi:10.1007/s00262-018-2205-1.
- Xie K, Xu L, Wu H, Liao H, Luo L, Liao M, Gong J, Deng Y, Yuan K, Wu H, et al. OX40 expression in hepatocellular carcinoma is associated with a distinct immune microenvironment, specific mutation signature, and poor prognosis. Oncoimmunology. 2018;7:e1404214. doi:10.1080/2162402X.2017.1404214.
- Chyuan IT, Tsai HF, Wu CS, Hsu PN. TRAIL suppresses gut inflammation and inhibits colitogeic T-cell activation in experimental colitis via an apoptosis-independent pathway. Mucosal Immunology. 2019;12:980–989. doi:10.1038/s41385-019-0168-y.
- Roan F, Obata-Ninomiya K, Ziegler SF. Epithelial cell-derived cytokines: more than just signaling the alarm. The Journal of Clinical Investigation. 2019;129:1441–1451. doi:10.1172/JCI124606.
- Branchett WJ, Lloyd CM. Regulatory cytokine function in the respiratory tract. Mucosal Immunology. 2019;12:589–600. doi:10.1038/s41385-019-0158-0.
- Jones AT, Shen X, Walter KL, LaBranche CC, Wyatt LS, Tomaras GD, Montefiori DC, Moss B, Barouch DH, Clements JD, et al. HIV-1 vaccination by needle-free oral injection induces strong mucosal immunity and protects against SHIV challenge. Nat Commun. 2019;10:798. doi:10.1038/s41467-019-08739-4.
- Rhodes JW, Tong O, Harman AN, Turville SG. Human Dendritic Cell Subsets, Ontogeny, and Impact on HIV Infection. Frontiers in Immunology. 2019;10:1088. doi:10.3389/fimmu.2019.01088.
- Bassler K, Schulte-Schrepping J, Warnat-Herresthal S, Aschenbrenner AC, Schultze JL. The Myeloid Cell Compartment-Cell by Cell. Annual Review of Immunology. 2019;37:269–293. doi:10.1146/annurev-immunol-042718-041728.
- Strobl H, Krump C, Borek I Micro-environmental signals directing human epidermal Langerhans cell differentiation. Seminars in cell & developmental biology 2019; 86:36–43. Seminars in cell & developmental biology 10.1016/j.semcdb.2018.02.016
- Ohmatsu H, Humme D, Gonzalez J, Gulati N, Mobs M, Sterry W, Krueger JG. IL-32 induces indoleamine 2,3-dioxygenase(+)CD1c(+) dendritic cells and indoleamine 2,3-dioxygenase(+)CD163(+) macrophages: relevance to mycosis fungoides progression. Oncoimmunology. 2017;6:e1181237. doi:10.1080/2162402X.2016.1181237.
- Pellegatta S, Eoli M, Cuccarini V, Anghileri E, Pollo B, Pessina S, Frigerio S, Servida M, Cuppini L, Antozzi C, et al. Survival gain in glioblastoma patients treated with dendritic cell immunotherapy is associated with increased NK but not CD8(+) T cell activation in the presence of adjuvant temozolomide. Oncoimmunology. 2018;7:e1412901. doi:10.1080/2162402X.2017.1412901.
- Truxova I, Kasikova L, Hensler M, Skapa P, Laco J, Pecen L, Belicova L, Praznovec I, Halaska MJ, Brtnicky T, et al. Mature dendritic cells correlate with favorable immune infiltrate and improved prognosis in ovarian carcinoma patients. J Immunother Cancer. 2018;6:139. doi:10.1186/s40425-018-0446-3.
- Kiss M, Van Gassen S, Movahedi K, Saeys Y, Laoui D. Myeloid cell heterogeneity in cancer: not a single cell alike. Cell Immunol. 2018;330:188–201. doi:10.1016/j.cellimm.2018.02.008.
- Huber A, Dammeijer F, Aerts J, Vroman H. Current State of Dendritic Cell-Based Immunotherapy: opportunities for in vitro Antigen Loading of Different DC Subsets?. Frontiers in Immunology. 2018;9:2804. doi:10.3389/fimmu.2018.02804.
- Pyfferoen L, Brabants E, Everaert C, De Cabooter N, Heyns K, Deswarte K, Vanheerswynghels M, De Prijck S, Waegemans G, Dullaers M, et al. The transcriptome of lung tumor-infiltrating dendritic cells reveals a tumor-supporting phenotype and a microRNA signature with negative impact on clinical outcome. Oncoimmunology. 2017;6:e1253655. doi:10.1080/2162402X.2016.1253655.
- Segura E. Review of Mouse and Human Dendritic Cell Subsets. Methods in Molecular Biology. 2016;1423:3–15. doi:10.1007/978-1-4939-3606-9_1.
- Thordardottir S, Schaap N, Louer E, Kester MG, Falkenburg JH, Jansen J, Radstake TRD, Hobo W, Dolstra H. Hematopoietic stem cell-derived myeloid and plasmacytoid DC-based vaccines are highly potent inducers of tumor-reactive T cell and NK cell responses ex vivo. Oncoimmunology. 2017;6:e1285991. doi:10.1080/2162402X.2017.1285991.
- Vanpouille-Box C, Galluzzi L. CD103(+) cells at the forefront of anticancer immunity. Oncoimmunology. 2017;6:e1356154. doi:10.1080/2162402X.2017.1356154.
- Murgaski A, Bardet PMR, Arnouk SM, Clappaert EJ, Laoui D. Unleashing Tumour-Dendritic Cells to Fight Cancer by Tackling Their Three A’s: abundance, Activation and Antigen-Delivery. Cancers. 2019;11:670. doi:10.3390/cancers11050670.
- Olingy CE, Dinh HQ, Hedrick CC. Monocyte heterogeneity and functions in cancer. J Leukoc Biol. 2019.106:309–322. doi: 10.1002/JLB.4RI0818-311R.
- Clark GJ, Silveira PA, Hogarth PM, Hart DNJ. The cell surface phenotype of human dendritic cells. Seminars in Cell & Developmental Biology. 2019;86:3–14. doi:10.1016/j.semcdb.2018.02.013.
- Ovcinnikovs V, Ross EM, Petersone L, Edner NM, Heuts F, Ntavli E, Kogimtzis A, Kennedy A, Wang CJ, Bennett CL, Sansom DM. CTLA-4-mediated transendocytosis of costimulatory molecules primarily targets migratory dendritic cells. Science Immunology. 2019:4.:eaaw0902. doi:10.1126/sciimmunol.aaw0902.
- MacNabb BW, Kline DE, Albright AR, Chen X, Leventhal DS, Savage PA, Kline J. Negligible Role for Deletion Mediated by cDC1 in CD8(+) T Cell Tolerance. J Immunol. 2019;202:2628–2635. doi:10.4049/jimmunol.1801621.
- Mundt S, Mrdjen D, Utz SG, Greter M, Schreiner B, Becher B. Conventional DCs sample and present myelin antigens in the healthy CNS and allow parenchymal T cell entry to initiate neuroinflammation. Science Immunology. 2019;4:eaau8380. doi: 10.1126/sciimmunol.aau8380.
- See P, Dutertre CA, Chen J, Gunther P, McGovern N, Irac SE, Gunawan M, Beyer M, Händler K, Duan K, Sumatoh HR. Mapping the human DC lineage through the integration of high-dimensional techniques. Science. 2017:356:eaag3009. doi: 10.1126/science.aag3009.
- Villani AC, Satija R, Reynolds G, Sarkizova S, Shekhar K, Fletcher J, Griesbeck M, Butler A, Zheng S, Lazo S, Jardine L. Single-cell RNA-seq reveals new types of human blood dendritic cells, monocytes, and progenitors. Science. 2017:356:eaah4573. doi: 10.1126/science.aah4573.
- Ali S, Mann-Nuttel R, Schulze A, Richter L, Alferink J, Scheu S. Sources of Type I Interferons in Infectious Immunity: plasmacytoid Dendritic Cells Not Always in the Driver’s Seat. Frontiers in Immunology. 2019;10:778. doi:10.3389/fimmu.2019.00778.
- Vangeti S, Gertow J, Yu M, Liu S, Baharom F, Scholz S, Friberg D, Starkhammar M, Ahlberg A, Smed-Sörensen A. Human Blood and Tonsil Plasmacytoid Dendritic Cells Display Similar Gene Expression Profiles but Exhibit Differential Type I IFN Responses to Influenza A Virus Infection. J Immunol. 2019;202:2069–2081. doi:10.4049/jimmunol.1801191.
- Loughland JR, Woodberry T, Boyle MJ, Tipping PE, Piera KA, Amante FH, Kenangalem E, Price RN, Engwerda CR, Anstey NM, et al. Plasmodium falciparum Activates CD16+ Dendritic Cells to Produce Tumor Necrosis Factor and Interleukin-10 in Subpatent Malaria. The Journal of Infectious Diseases. 2019;219:660–671. doi:10.1093/infdis/jiy555.
- Bouteau A, Kervevan J, Su Q, Zurawski SM, Contreras V, Dereuddre-Bosquet N, Le Grand R, Zurawski G, Cardinaud S, Levy Y, et al. DC Subsets Regulate Humoral Immune Responses by Supporting the Differentiation of Distinct Tfh Cells. Frontiers in Immunology. 2019;10:1134. doi:10.3389/fimmu.2019.01134.
- Wang Z, Wang W, Chai Q, Zhu M. Langerhans Cells Control Lymphatic Vessel Function during Inflammation via LIGHT-LTβR Signaling.. J Immunol. 2019;202:2999–3007. doi:10.4049/jimmunol.1801578.
- Sumpter TL, Balmert SC, Kaplan DH. Cutaneous immune responses mediated by dendritic cells and mast cells. JCI Insight. 2019;4. doi: 10.1172/jci.insight.123947.
- Eisenbarth SC. Dendritic cell subsets in T cell programming: location dictates function. Nature Reviews Immunology. 2019;19:89–103. doi:10.1038/s41577-018-0088-1.
- Michea P, Noel F, Zakine E, Czerwinska U, Sirven P, Abouzid O, Goudot C, Scholer-Dahirel A, Vincent-Salomon A, Reyal F, et al. Adjustment of dendritic cells to the breast-cancer microenvironment is subset specific. Nat Immunol. 2018;19:885–897. doi:10.1038/s41590-018-0145-8.
- Macri C, Pang ES, Patton T, O’Keeffe M. Dendritic cell subsets. Seminars in Cell & Developmental Biology. 2018;84:11–21. doi:10.1016/j.semcdb.2017.12.009.
- Durai V, Murphy KM. Functions of Murine Dendritic Cells. Immunity. 2016;45:719–736. doi:10.1016/j.immuni.2016.10.010.
- Shortman K, Heath WR. The CD8+ dendritic cell subset. Immunol Rev. 2010;234:18–31. doi:10.1111/j.0105-2896.2009.00870.x.
- Lavin Y, Kobayashi S, Leader A, Amir EAD, Elefant N, Bigenwald C, Remark R, Sweeney R, Becker CD, Levine JH, et al. Innate Immune Landscape in Early Lung Adenocarcinoma by Paired Single-Cell Analyses. Cell. 2017;169:750–65 e17. doi:10.1016/j.cell.2017.04.014.
- Bachem A, Guttler S, Hartung E, Ebstein F, Schaefer M, Tannert A, Salama A, Movassaghi K, Opitz C, Mages HW, et al. Superior antigen cross-presentation and XCR1 expression define human CD11c+CD141+ cells as homologues of mouse CD8+ dendritic cells. J Exp Med. 2010;207:1273–1281. doi:10.1084/jem.20100348.
- Crozat K, Guiton R, Contreras V, Feuillet V, Dutertre C-A, Ventre E, Vu Manh T-P, Baranek T, Storset AK, Marvel J, et al. The XC chemokine receptor 1 is a conserved selective marker of mammalian cells homologous to mouse CD8alpha+ dendritic cells. J Exp Med. 2010;207:1283–1292. doi:10.1084/jem.20100223.
- Poulin LF, Salio M, Griessinger E, Anjos-Afonso F, Craciun L, Chen J-L, Keller AM, Joffre O, Zelenay S, Nye E, et al. Characterization of human DNGR-1+ BDCA3+ leukocytes as putative equivalents of mouse CD8alpha+ dendritic cells. J Exp Med. 2010;207:1261–1271. doi:10.1084/jem.20092618.
- Jongbloed SL, Kassianos AJ, McDonald KJ, Clark GJ, Ju X, Angel CE, Chen CJJ, Dunbar PR, Wadley RB, Jeet V, et al. Human CD141+ (BDCA-3)+ dendritic cells (DCs) represent a unique myeloid DC subset that cross-presents necrotic cell antigens. J Exp Med. 2010;207:1247–1260. doi:10.1084/jem.20092140.
- Di Blasio S, Wortel IM, van Bladel DA, de Vries LE, Duiveman-de Boer T, Worah K, de Haas N, Buschow SI, de Vries IJM, Figdor CG, et al. Human CD1c(+) DCs are critical cellular mediators of immune responses induced by immunogenic cell death. Oncoimmunology. 2016;5:e1192739. doi:10.1080/2162402X.2016.1192739.
- Ghinnagow R, De Meester J, Cruz LJ, Aspord C, Corgnac S, Macho-Fernandez E, Soulard D, Fontaine J, Chaperot L, Charles J, et al. Co-delivery of the NKT agonist alpha-galactosylceramide and tumor antigens to cross-priming dendritic cells breaks tolerance to self-antigens and promotes antitumor responses. Oncoimmunology. 2017;6:e1339855. doi:10.1080/2162402X.2017.1339855.
- Joffre OP, Segura E, Savina A, Amigorena S. Cross-presentation by dendritic cells. Nature Reviews Immunology. 2012;12:557–569. doi:10.1038/nri3254.
- Klechevsky E, Morita R, Liu M, Cao Y, Coquery S, Thompson-Snipes L, Briere F, Chaussabel D, Zurawski G, Palucka AK, et al. Functional specializations of human epidermal Langerhans cells and CD14+ dermal dendritic cells. Immunity. 2008;29:497–510. doi:10.1016/j.immuni.2008.07.013.
- Ueno H, Klechevsky E, Morita R, Aspord C, Cao T, Matsui T, Di Pucchio T, Connolly J, Fay JW, Pascual V, et al. Dendritic cell subsets in health and disease. Immunol Rev. 2007;219:118–142. doi:10.1111/j.1600-065X.2007.00551.x.
- Siegal FP, Kadowaki N, Shodell M, Fitzgerald-Bocarsly PA, Shah K, Ho S, Antonenko S, Liu YJ. The Nature of the Principal Type 1 Interferon-Producing Cells in Human Blood. Science. 1999;284:1835–1837. doi:10.1126/science.284.5421.1835.
- Cella M, Facchetti F, Lanzavecchia A, Colonna M. Plasmacytoid dendritic cells activated by influenza virus and CD40L drive a potent TH1 polarization. Nat Immunol. 2000;1:305–310. doi:10.1038/79747.
- Gilliet M, Boonstra A, Paturel C, Antonenko S, Xu X-L, Trinchieri G, O’Garra A, Liu Y-J. The development of murine plasmacytoid dendritic cell precursors is differentially regulated by FLT3-ligand and granulocyte/macrophage colony-stimulating factor. J Exp Med. 2002;195:953–958. doi:10.1084/jem.20020045.
- Medler T, Patel JM, Alice A, Baird JR, Hu HM, Gough MJ. Activating the Nucleic Acid-Sensing Machinery for Anticancer Immunity. International Review of Cell and Molecular Biology. 2019;344:173–214. doi: 10.1016/bs.ircmb.2018.08.006.
- Sprooten J, Agostinis P, Garg AD. Type I interferons and dendritic cells in cancer immunotherapy. International Review of Cell and Molecular Biology. 2019. doi:10.1016/bs.ircmb.2019.06.001.
- Galluzzi L, Yamazaki T, Kroemer G. Linking cellular stress responses to systemic homeostasis. Nat Rev Mol Cell Biol. 2018;19:731–745. doi:10.1038/s41580-018-0068-0.
- Collignon A, Silvy F, Robert S, Trad M, Germain S, Nigri J, André F, Rigot V, Tomasini R, Bonnotte B, et al. Dendritic cell-based vaccination: powerful resources of immature dendritic cells against pancreatic adenocarcinoma. Oncoimmunology. 2018;7:e1504727. doi:10.1080/2162402X.2018.1504727.
- Idoyaga J, Fiorese C, Zbytnuik L, Lubkin A, Miller J, Malissen B, Mucida D, Merad M, Steinman RM. Specialized role of migratory dendritic cells in peripheral tolerance induction. The Journal of Clinical Investigation. 2013;123:844–854. doi:10.1172/JCI65260.
- Garg AD, Romano E, Rufo N, Agostinis P. Immunogenic versus tolerogenic phagocytosis during anticancer therapy: mechanisms and clinical translation. Cell Death and Differentiation. 2016;23:938–951. doi:10.1038/cdd.2016.5.
- Garg AD, Krysko DV, Verfaillie T, Kaczmarek A, Ferreira GB, Marysael T, Rubio N, Firczuk M, Mathieu C, Roebroek AJM, et al. A novel pathway combining calreticulin exposure and ATP secretion in immunogenic cancer cell death. The EMBO Journal. 2012;31:1062–1079. doi:10.1038/emboj.2011.497.
- Palucka K, Banchereau J. Cancer immunotherapy via dendritic cells. Nature Reviews Cancer. 2012;12:265–277. doi:10.1038/nrc3258.
- Sistigu A, Yamazaki T, Vacchelli E, Chaba K, Enot DP, Adam J, Vitale I, Goubar A, Baracco EE, Remédios C. Cancer cell-autonomous contribution of type I interferon signaling to the efficacy of chemotherapy. Nature Medicine. 2014;20:1301–1309. doi:10.1038/nm.3708.
- Aznar MA, Labiano S, Diaz-Lagares A, Molina C, Garasa S, Azpilikueta A, Etxeberria I, Sanchez-Paulete AR, Korman AJ, Esteller M, et al. CD137 (4-1BB) Costimulation Modifies DNA Methylation in CD8 + T Cell–relevant Genes. Cancer Immunology Research. 2018;6:69–78. doi:10.1158/2326-6066.CIR-17-0159.
- Zafar S, Parviainen S, Siurala M, Hemminki O, Havunen R, Tahtinen S, Bramante S, Vassilev L, Wang H, Lieber A, et al. Intravenously usable fully serotype 3 oncolytic adenovirus coding for CD40L as an enabler of dendritic cell therapy. Oncoimmunology. 2017;6:e1265717. doi:10.1080/2162402X.2016.1265717.
- Garg AD, Dudek AM, Agostinis P. Cancer immunogenicity, danger signals, and DAMPs: what, when, and how?. Biofactors. 2013;39:355–367. doi:10.1002/biof.1125.
- Gonzalez FE, Chernobrovkin A, Pereda C, Garcia-Salum T, Tittarelli A, Lopez MN, Salazar-Onfray F, Zubarev RA. Proteomic Identification of Heat Shock-Induced Danger Signals in a Melanoma Cell Lysate Used in Dendritic Cell-Based Cancer Immunotherapy. Journal of Immunology Research. 2018;2018:3982942. doi:10.1155/2018/3982942.
- Venkateswaran K, Verma A, Bhatt AN, Shrivastava A, Manda K, Raj HG, Prasad A, Len C, Parmar VS, Dwarakanath BS. Emerging Roles of Calreticulin in Cancer: implications for Therapy. Current Protein & Peptide Science. 2018;19:344–357. doi:10.2174/1389203718666170111123253.
- Moserova I, Truxova I, Garg AD, Tomala J, Agostinis P, Cartron PF, Vosahlikova S, Kovar M, Spisek R, Fucikova J. Caspase-2 and oxidative stress underlie the immunogenic potential of high hydrostatic pressure-induced cancer cell death. Oncoimmunology. 2017;6:e1258505. doi:10.1080/2162402X.2016.1258505.
- Patidar A, Selvaraj S, Sarode A, Chauhan P, Chattopadhyay D, Saha B. DAMP-TLR-cytokine axis dictates the fate of tumor. Cytokine. 2018;104:114–123. doi:10.1016/j.cyto.2017.10.004.
- Carrington EM, Tarlinton DM, Gray DH, Huntington ND, Zhan Y, Lew AM. The life and death of immune cell types: the role of BCL-2 anti-apoptotic molecules. Immunology and Cell Biology. 2017;95:870–877. doi:10.1038/icb.2017.72.
- Riganti C, Lingua MF, Salaroglio IC, Falcomata C, Righi L, Morena D, Picca F, Oddo D, Kopecka J, Pradotto M, et al. Bromodomain inhibition exerts its therapeutic potential in malignant pleural mesothelioma by promoting immunogenic cell death and changing the tumor immune-environment. Oncoimmunology. 2018;7:e1398874. doi:10.1080/2162402X.2017.1398874.
- Garg AD, Galluzzi L, Apetoh L, Baert T, Birge RB, Bravo-San Pedro JM, Breckpot K, Brough D, Chaurio R, Cirone M. Molecular and Translational Classifications of DAMPs in Immunogenic Cell Death. Frontiers in Immunology. 2015;6:588. doi:10.3389/fimmu.2015.00588.
- Umansky V, Adema GJ, Baran J, Brandau S, Van Ginderachter JA, Hu X, Jablonska J, Mojsilovic S, Papadaki HA, Pico de Coaña Y, et al. Interactions among myeloid regulatory cells in cancer. Cancer Immunology, Immunotherapy: CII. 2019;68:645–660. doi:10.1007/s00262-018-2200-6.
- Zom GG, Willems M, Khan S, van der Sluis TC, Kleinovink JW, Camps MGM, van der Marel GA, Filippov DV, Melief CJM, Ossendorp F. Novel TLR2-binding adjuvant induces enhanced T cell responses and tumor eradication. J Immunother Cancer. 2018;6:146. doi:10.1186/s40425-018-0455-2.
- Land WG, Agostinis P, Gasser S, Garg AD, Linkermann A. DAMP-Induced Allograft and Tumor Rejection: the Circle Is Closing. American Journal of Transplantation: Official Journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2016;16:3322–3337. doi:10.1111/ajt.14012.
- Santillo BT, Reis DDS, da Silva LT, Romani NT, Duarte A, Oshiro TM. Phenotypic and functional profile of IFN-alpha-differentiated dendritic cells (IFN-DCs) from HIV-infected individuals. Human Vaccines & Immunotherapeutics. 2019;15:2140–2149. doi: 10.1080/21645515.2018.1547603.
- Krzastek SC, Goliadze E, Zhou S, Petrossian A, Youniss F, Sundaresan G, Wang L, Zweit J, Guruli G. Dendritic cell trafficking in tumor-bearing mice. Cancer Immunology, Immunotherapy: CII. 2018;67:1939–1947. doi:10.1007/s00262-018-2187-z.
- Li X, Dong W, Nalin AP, Wang Y, Pan P, Xu B, Zhang Y, Tun S, Zhang J, Wang L-S, et al. The natural product chitosan enhances the anti-tumor activity of natural killer cells by activating dendritic cells. Oncoimmunology. 2018;7:e1431085. doi:10.1080/2162402X.2018.1431085.
- Ho HNI, In ‘t Veld LGM, Raaijmakers TK, Adema GJ. Adjuvants Enhancing Cross-Presentation by Dendritic Cells: the Key to More Effective Vaccines?. Frontiers in Immunology. 2018;9:2874. doi:10.3389/fimmu.2018.02874.
- Zafar S, Sorsa S, Siurala M, Hemminki O, Havunen R, Cervera-Carrascon V, Santos JM, Wang H, Lieber A, De Gruijl T, et al. CD40L coding oncolytic adenovirus allows long-term survival of humanized mice receiving dendritic cell therapy. Oncoimmunology. 2018;7:e1490856. doi:10.1080/2162402X.2018.1490856.
- Yang SC, Hillinger S, Riedl K, Zhang L, Zhu L, Huang M, Atianzar K, BY K, Gardner B, Batra RK, et al. Intratumoral administration of dendritic cells overexpressing CCL21 generates systemic antitumor responses and confers tumor immunity. Clinical Cancer Research: an Official Journal of the American Association for Cancer Research. 2004;10:2891–2901. doi:10.1158/1078-0432.CCR-03-0380.
- Valentine FT, Golomb FM, Harris M, Roses DF. A novel immunization strategy using cytokine/chemokines induces new effective systemic immune responses, and frequent complete regressions of human metastatic melanoma. Oncoimmunology. 2018;7:e1386827. doi:10.1080/2162402X.2017.1386827.
- Mitchell JP, Carmody RJ. NF-kappaB and the Transcriptional Control of Inflammation. International Review of Cell and Molecular Biology. 2018;335:41–84 doi: 10.1016/bs.ircmb.2017.07.007.
- Garg AD, Vandenberk L, Fang S, Fasche T, Van Eygen S, Maes J, Van Woensel M, Koks C, Vanthillo N, Graf N, et al. Pathogen response-like recruitment and activation of neutrophils by sterile immunogenic dying cells drives neutrophil-mediated residual cell killing. Cell Death and Differentiation. 2017;24:832–843. doi:10.1038/cdd.2017.15.
- Chow MT, Ozga AJ, Servis RL, Frederick DT, Lo JA, Fisher DE, Freeman GJ, Boland GM, Luster AD. Intratumoral Activity of the CXCR3 Chemokine System Is Required for the Efficacy of Anti-PD-1 Therapy. Immunity. 2019;50:1498–1512.e5. doi:10.1016/j.immuni.2019.04.010.
- Jing W, McAllister D, Vonderhaar EP, Palen K, Riese MJ, Gershan J, Johnson BD, Dwinell MB. STING agonist inflames the pancreatic cancer immune microenvironment and reduces tumor burden in mouse models. J Immunother Cancer. 2019;7:115. doi:10.1186/s40425-019-0573-5.
- Gianello V, Salvi V, Parola C, Moretto N, Facchinetti F, Civelli M, Villetti G, Bosisio D, Sozzani S. The PDE4 inhibitor CHF6001 modulates pro-inflammatory cytokines, chemokines and Th1- and Th17-polarizing cytokines in human dendritic cells. Biochemical Pharmacology. 2019;163:371–380. doi:10.1016/j.bcp.2019.03.006.
- Lu F, Mosley YC, Carmichael B, Brown DD, HogenEsch H. Formulation of aluminum hydroxide adjuvant with TLR agonists poly(I:C) and CpG enhances the magnitude and avidity of the humoral immune response. Vaccine. 2019;37:1945–1953. doi:10.1016/j.vaccine.2019.02.033.
- Oreskovic Z, Nechvatalova K, Krejci J, Kummer V, Faldyna M. Aspects of intradermal immunization with different adjuvants: the role of dendritic cells and Th1/Th2 response. PLoS One. 2019;14:e0211896. doi: 10.1371/journal.pone.0211896.
- Baert T, Garg AD, Vindevogel E, VAN HOYLANDT AVANH, VERBIST G, AGONISTINIS P, VERGOTE I, COOSEMANS ANP. In Vitro Generation of Murine Dendritic Cells for Cancer Immunotherapy: an Optimized Protocol. Anticancer Research. 2016;36:5793–5802. doi:10.21873/anticanres.11163.
- Luty J, Ruckemann-Dziurdzinska K, Witkowski JM, Bryl E. Immunological aspects of autoimmune thyroid disease - Complex interplay between cells and cytokines. Cytokine. 2019;116:128–133. doi:10.1016/j.cyto.2019.01.003.
- Vieyra-Garcia P, Crouch JD, O’Malley JT, Seger EW, Yang CH, Teague JE, Vromans AM, Gehad A, Win TS, Yu Z, et al. Benign T cells drive clinical skin inflammation in cutaneous T cell lymphoma. JCI Insight. 2019:4. doi: 10.1172/jci.insight.124233.
- Steinman RM. Decisions about dendritic cells: past, present, and future. Annual Review of Immunology. 2012;30:1–22. doi:10.1146/annurev-immunol-100311-102839.
- Maldonado-Lopez R, De Smedt T, Michel P, Godfroid J, Pajak B, Heirman C, Thielemans K, Leo O, Urbain J, Moser M. CD8α + and CD8α − Subclasses of Dendritic Cells Direct the Development of Distinct T Helper Cells In Vivo. J Exp Med. 1999;189:587–592. doi:10.1084/jem.189.3.587.
- Pulendran B, Smith JL, Caspary G, Brasel K, Pettit D, Maraskovsky E, Maliszewski CR. Distinct dendritic cell subsets differentially regulate the class of immune response in vivo. Proc Natl Acad Sci U S A. 1999;96:1036–1041. doi:10.1073/pnas.96.3.1036.
- Dudziak D, Kamphorst AO, Heidkamp GF, Buchholz VR, Trumpfheller C, Yamazaki S, Cheong C, Liu K, Lee H-W, Park CG, et al. Differential antigen processing by dendritic cell subsets in vivo. Science. 2007;315:107–111. doi:10.1126/science.1136080.
- Rao S, Gharib K, Han A. Cancer Immunosurveillance by T Cells. International Review of Cell and Molecular Biology. 2019;342:149–173.
- Chalmin F, Humblin E, Ghiringhelli F, Vegran F. Transcriptional Programs Underlying Cd4 T Cell Differentiation and Functions. International Review of Cell and Molecular Biology. 2018;341:1–61. doi:10.1016/bs.ircmb.2018.07.002.
- Sabado RL, Balan S, Bhardwaj N. Dendritic cell-based immunotherapy. Cell Research. 2017;27:74–95. doi:10.1038/cr.2016.157.
- Bol KF, Schreibelt G, Gerritsen WR, de Vries IJ, Figdor CG. Dendritic Cell-Based Immunotherapy: state of the Art and Beyond. Clinical Cancer Research: an Official Journal of the American Association for Cancer Research. 2016;22:1897–1906. doi:10.1158/1078-0432.CCR-15-1399.
- Anguille S, Smits EL, Lion E, van Tendeloo VF, Berneman ZN. Clinical use of dendritic cells for cancer therapy. The Lancet Oncology. 2014;15:e257–67. doi:10.1016/S1470-2045(13)70585-0.
- Palucka K, Banchereau J. Dendritic-cell-based therapeutic cancer vaccines. Immunity. 2013;39:38–48. doi:10.1016/j.immuni.2013.07.004.
- Vanpouille-Box C, Demaria S, Formenti SC, Galluzzi L. Cytosolic DNA Sensing in Organismal Tumor Control. Cancer Cell. 2018;34:361–378. doi:10.1016/j.ccell.2018.05.013.
- Romero P, Banchereau J, Bhardwaj N, Cockett M, Disis ML, Dranoff G, Gilboa E, Hammond SA, Hershberg R, Korman AJ, et al. The Human Vaccines Project: A roadmap for cancer vaccine development. Science Translational Medicine. 2016;8:334ps9. doi:10.1126/scitranslmed.aaf0685.
- Truxova I, Hensler M, Skapa P, Halaska MJ, Laco J, Ryska A, Spisek R, Fucikova J. Rationale for the Combination of Dendritic Cell-Based Vaccination Approaches With Chemotherapy Agents. International Review of Cell and Molecular Biology. 2017;330:115–156.
- Gilboa E. DC-based cancer vaccines. The Journal of Clinical Investigation. 2007;117:1195–1203. doi:10.1172/JCI31205.
- Tacken PJ, de Vries IJ, Torensma R, Figdor CG. Dendritic-cell immunotherapy: from ex vivo loading to in vivo targeting. Nature Reviews Immunology. 2007;7:790–802. doi:10.1038/nri2173.
- Satoh Y, Esche C, Gambotto A, Shurin GV, Yurkovetsky ZR, Robbins PD, Watkins SC, Todo S, Herberman RB, Lotze MT, et al. Local administration of IL-12-transfected dendritic cells induces antitumor immune responses to colon adenocarcinoma in the liver in mice. J Exp Ther Oncol. 2002;2:337–349. doi:10.1046/j.1359-4117.2002.01050.x.
- Nishioka Y, Hirao M, Robbins PD, Lotze MT, Tahara H. Induction of systemic and therapeutic antitumor immunity using intratumoral injection of dendritic cells genetically modified to express interleukin 12. Cancer Res. 1999;59:4035–4041.
- Hu J, Yuan X, Belladonna ML, Ong JM, Wachsmann-Hogiu S, Farkas DL, Black KL, Yu JS. Induction of potent antitumor immunity by intratumoral injection of interleukin 23-transduced dendritic cells. Cancer Res. 2006;66:8887–8896. doi:10.1158/0008-5472.CAN-05-3448.
- Endo H, Saito T, Kenjo A, Hoshino M, Terashima M, Sato T, Anazawa T, Kimura T, Tsuchiya T, Irisawa A, et al. Phase I trial of preoperative intratumoral injection of immature dendritic cells and OK-432 for resectable pancreatic cancer patients. J Hepatobiliary Pancreat Sci. 2012;19:465–475. doi:10.1007/s00534-011-0457-7.
- Galluzzi L, Vanpouille-Box C, Bakhoum SF, Demaria S. SnapShot: CGAS-STING Signaling. Cell. 2018;173:276- e1. doi:10.1016/j.cell.2018.03.015.
- Nair SK, Snyder D, Rouse BT, Gilboa E. Regression of tumors in mice vaccinated with professional antigen-presenting cells pulsed with tumor extracts. Int J Cancer. 1997;70:706–718. doi:10.1002/(sici)1097-0215(19970317)70:6<706::aid-ijc13>3.0.co;2-7.
- DeMatos P, Abdel-Wahab Z, Vervaert C, Hester D, Seigler H. Pulsing of dendritic cells with cell lysates from either B16 melanoma or MCA-106 fibrosarcoma yields equally effective vaccines against B16 tumors in mice. J Surg Oncol. 1998;68:79–91. doi:10.1002/(sici)1096-9098(199806)68:2<79::aid-jso3>3.0.co;2-h.
- DeMatos P, Abdel-Wahab Z, Vervaert C, Seigler HF. Vaccination with dendritic cells inhibits the growth of hepatic metastases in B6 mice. Cell Immunol. 1998;185:65–74. doi:10.1006/cimm.1998.1277.
- Fields RC, Shimizu K, Mule JJ. Murine dendritic cells pulsed with whole tumor lysates mediate potent antitumor immune responses in vitro and in vivo. Proc Natl Acad Sci U S A. 1998;95:9482–9487. doi:10.1073/pnas.95.16.9482.
- Chen Z, Moyana T, Saxena A, Warrington R, Jia Z, Xiang J. Efficient antitumor immunity derived from maturation of dendritic cells that had phagocytosed apoptotic/necrotic tumor cells. Int J Cancer. 2001;93:539–548. doi:10.1002/ijc.1365.
- Paczesny S, Beranger S, Salzmann JL, Klatzmann D, Colombo BM. Protection of mice against leukemia after vaccination with bone marrow-derived dendritic cells loaded with apoptotic leukemia cells. Cancer Res. 2001;61:2386–2389.
- Kokhaei P, Choudhury A, Mahdian R, Lundin J, Moshfegh A, Osterborg A, Mellstedt H. Apoptotic tumor cells are superior to tumor cell lysate, and tumor cell RNA in induction of autologous T cell response in B-CLL. Leukemia. 2004;18:1810–1815. doi:10.1038/sj.leu.2403517.
- Kokhaei P, Rezvany MR, Virving L, Choudhury A, Rabbani H, Osterborg A, Mellstedt H. Dendritic cells loaded with apoptotic tumour cells induce a stronger T-cell response than dendritic cell-tumour hybrids in B-CLL. Leukemia. 2003;17:894–899. doi:10.1038/sj.leu.2402913.
- Albert ML, Sauter B, Bhardwaj N. Dendritic cells acquire antigen from apoptotic cells and induce class I-restricted CTLs. Nature. 1998;392:86–89. doi:10.1038/32183.
- Albert ML, Pearce SF, Francisco LM, Sauter B, Roy P, Silverstein RL, Bhardwaj N. Immature Dendritic Cells Phagocytose Apoptotic Cells via α v β 5 and CD36, and Cross-present Antigens to Cytotoxic T Lymphocytes. J Exp Med. 1998;188:1359–1368. doi:10.1084/jem.188.7.1359.
- Mayordomo JI, Zorina T, Storkus WJ, Zitvogel L, Celluzzi C, Falo LD, Melief CJ, Ildstad ST, Kast WM, Deleo AB, et al. Bone marrow-derived dendritic cells pulsed with synthetic tumour peptides elicit protective and therapeutic antitumour immunity. Nature Medicine. 1995;1:1297–1302. doi:10.1038/nm1295-1297.
- Mayordomo JI, Loftus DJ, Sakamoto H, De Cesare CM, Appasamy PM, Lotze MT, Storkus WJ, Appella E, DeLeo AB. Therapy of murine tumors with p53 wild-type and mutant sequence peptide-based vaccines. J Exp Med. 1996;183:1357–1365. doi:10.1084/jem.183.4.1357.
- Paglia P. Murine dendritic cells loaded in vitro with soluble protein prime cytotoxic T lymphocytes against tumor antigen in vivo. J Exp Med. 1996;183:317–322. doi:10.1084/jem.183.1.317.
- Mackey MF, Gunn JR, Maliszewsky C, Kikutani H, Noelle RJ, Barth RJ Jr. Dendritic cells require maturation via CD40 to generate protective antitumor immunity. J Immunol. 1998;161:2094–2098.
- Zitvogel L, Mayordomo JI, Tjandrawan T, DeLeo AB, Clarke MR, Lotze MT, Storkus WJ. Therapy of murine tumors with tumor peptide-pulsed dendritic cells: dependence on T cells, B7 costimulation, and T helper cell 1-associated cytokines. J Exp Med. 1996;183:87–97. doi:10.1084/jem.183.1.87.
- Mayordomo JI, Zorina T, Storkus WJ, Zitvogel L, Garcia‐Prats MD, DeLeo AB, Lotze MT. Bone Marrow‐Derived Dendritic Cells Serve as Potent Adjuvants for Peptide‐Based Antitumor Vaccines. Stem Cells. 2009;15:94–103. doi:10.1002/stem.150094.
- Fernandez NC, Lozier A, Flament C, Ricciardi-Castagnoli P, Bellet D, Suter M, Perricaudet M, Tursz T, Maraskovsky E, Zitvogel L, et al. Dendritic cells directly trigger NK cell functions: cross-talk relevant in innate anti-tumor immune responses in vivo. Nature Medicine. 1999;5:405–411. doi:10.1038/7403.
- Boczkowski D. Dendritic cells pulsed with RNA are potent antigen-presenting cells in vitro and in vivo. J Exp Med. 1996;184:465–472. doi:10.1084/jem.184.2.465.
- Ashley DM, Faiola B, Nair S, Hale LP, Bigner DD, Gilboa E. Bone marrow-generated dendritic cells pulsed with tumor extracts or tumor RNA induce antitumor immunity against central nervous system tumors. J Exp Med. 1997;186:1177–1182. doi:10.1084/jem.186.7.1177.
- Boczkowski D, Nair SK, Nam JH, Lyerly HK, Gilboa E. Induction of tumor immunity and cytotoxic T lymphocyte responses using dendritic cells transfected with messenger RNA amplified from tumor cells. Cancer Res. 2000;60:1028–1034.
- Irvine AS, Trinder PK, Laughton DL, Ketteringham H, McDermott RH, Reid SC, Haines AMR, Amir A, Husain R, Doshi R, et al. Efficient nonviral transfection of dendritic cells and their use for in vivo immunization. Nat Biotechnol. 2000;18:1273–1278. doi:10.1038/82383.
- Manickan E, Kanangat S, Rouse RJ, Yu Z, Rouse BT. Enhancement of immune response to naked DNA vaccine by immunization with transfected dendritic cells. J Leukoc Biol. 1997;61:125–132. doi:10.1002/jlb.61.2.125.
- Song W, Kong H-L, Carpenter H, Torii H, Granstein R, Rafii S, Moore MAS, Crystal RG. Dendritic cells genetically modified with an adenovirus vector encoding the cDNA for a model antigen induce protective and therapeutic antitumor immunity. J Exp Med. 1997;186:1247–1256. doi:10.1084/jem.186.8.1247.
- Tuting T, DeLeo AB, Lotze MT, Storkus WJ. Genetically modified bone marrow-derived dendritic cells expressing tumor-associated viral or “self” antigens induce antitumor immunity in vivo. Eur J Immunol. 1997;27:2702–2707. doi:10.1002/eji.1830271033.
- Wan Y, Bramson J, Carter R, Graham F, Gauldie J. Dendritic cells transduced with an adenoviral vector encoding a model tumor-associated antigen for tumor vaccination. Hum Gene Ther. 1997;8:1355–1363. doi:10.1089/hum.1997.8.11-1355.
- McArthur JG, Mulligan RC. Induction of protective anti-tumor immunity by gene-modified dendritic cells. J Immunother. 1998;21:41–47. doi:10.1097/00002371-199801000-00005.
- Ishida I, Chada C, Stipanov S, Nadaf N, Ciernik C, Gabrilovich G, Carbone DP. Dendritic cells transduced with wild-type p53 gene elicit potent anti-tumour immune responses. Clin Exp Immunol. 1999;117:244–251. doi:10.1046/j.1365-2249.1999.00913.x.
- Tuting T, Steitz J, Bruck J, Gambotto A, Steinbrink K, DeLeo AB, Robbins P, Knop J, Enk AH. Dendritic cell-based genetic immunization in mice with a recombinant adenovirus encoding murine TRP2 induces effective anti-melanoma immunity. J Gene Med. 1999;1:400–406. doi:10.1002/(SICI)1521-2254(199911/12)1:6<400::AID-JGM68>3.0.CO;2-D.
- Wan Y, Emtage P, Zhu Q, Foley R, Pilon A, Roberts B, Gauldie J. Enhanced immune response to the melanoma antigen gp100 using recombinant adenovirus-transduced dendritic cells. Cell Immunol. 1999;198:131–138. doi:10.1006/cimm.1999.1585.
- Klein C, Bueler H, Mulligan RC. Comparative analysis of genetically modified dendritic cells and tumor cells as therapeutic cancer vaccines. J Exp Med. 2000;191:1699–1708. doi:10.1084/jem.191.10.1699.
- Ribas A, Butterfield LH, Hu B, Dissette VB, Chen AY, Koh A, Amarnani SN, Glaspy JA, McBride WH, Economou JS, et al. Generation of T-cell immunity to a murine melanoma using MART-1-engineered dendritic cells. J Immunother. 2000;23:59–66. doi:10.1097/00002371-200001000-00008.
- Okada N, Saito T, Masunaga Y, Tsukada Y, Nakagawa S, Mizuguchi H, Mori K, Okada Y, Fujita T, Hayakawa T, et al. Efficient antigen gene transduction using Arg-Gly-Asp fiber-mutant adenovirus vectors can potentiate antitumor vaccine efficacy and maturation of murine dendritic cells. Cancer Res. 2001;61:7913–7919.
- Koido S, Kashiwaba M, Chen D, Gendler S, Kufe D, Gong J. Induction of antitumor immunity by vaccination of dendritic cells transfected with MUC1 RNA. J Immunol. 2000;165:5713–5719. doi:10.4049/jimmunol.165.10.5713.
- Nair SK, Heiser A, Boczkowski D, Majumdar A, Naoe M, Lebkowski JS, Vieweg J, Gilboa E. Induction of cytotoxic T cell responses and tumor immunity against unrelated tumors using telomerase reverse transcriptase RNA transfected dendritic cells. Nature Medicine. 2000;6:1011–1017. doi:10.1038/79519.
- Yamanaka R, Zullo SA, Tanaka R, Blaese M, Xanthopoulos KG. Enhancement of antitumor immune response in glioma models in mice by genetically modified dendritic cells pulsed with Semliki forest virus-mediated complementary DNA. J Neurosurg. 2001;94:474–481. doi:10.3171/jns.2001.94.3.0474.
- Insug O, Ku G, Ertl HC, Blaszczyk-Thurin M. A dendritic cell vaccine induces protective immunity to intracranial growth of glioma. Anticancer Research. 2002;22:613–621.
- Van Meirvenne S, Straetman L, Heirman C, Dullaers M, De Greef C, Van Tendeloo V, Thielemans K. Efficient genetic modification of murine dendritic cells by electroporation with mRNA. Cancer Gene Ther. 2002;9:787–797. doi:10.1038/sj.cgt.7700499.
- Minami T, Nakanishi Y, Izumi M, Harada T, Hara N. Enhancement of antigen-presenting capacity and antitumor immunity of dendritic cells pulsed with autologous tumor-derived RNA in mice. J Immunother. 2003;26:420–431. doi:10.1097/00002371-200309000-00005.
- Schmidt T, Ziske C, Marten A, Endres S, Tiemann K, Schmitz V, Gorschlüter M, Schneider C, Sauerbruch T, Schmidt-Wolf IGH, et al. Intratumoral immunization with tumor RNA-pulsed dendritic cells confers antitumor immunity in a C57BL/6 pancreatic murine tumor model. Cancer Res. 2003;63:8962–8967.
- Jung CW, Kwon JH, Seol JG, Park WH, Hyun JM, Kim ES, Kim ST, Lee SJ, Kim BK, Lee YY, et al. Induction of cytotoxic T lymphocytes by dendritic cells pulsed with murine leukemic cell RNA. Am J Hematol. 2004;75:121–127. doi:10.1002/ajh.10471.
- Liu BY, Chen XH, Gu QL, Li JF, Yin HR, Zhu ZG, YZ L. Antitumor effects of vaccine consisting of dendritic cells pulsed with tumor RNA from gastric cancer. World J Gastroenterol. 2004;10:630–633. doi:10.3748/wjg.v10.i5.630.
- Zeis M, Siegel S, Wagner A, Schmitz M, Marget M, Kuhl-Burmeister R, Adamzik I, Kabelitz D, Dreger P, Schmitz N, et al. Generation of cytotoxic responses in mice and human individuals against hematological malignancies using survivin-RNA-transfected dendritic cells. J Immunol. 2003;170:5391–5397. doi:10.4049/jimmunol.170.11.5391.
- Celluzzi CM, Falo LD Jr. Physical interaction between dendritic cells and tumor cells results in an immunogen that induces protective and therapeutic tumor rejection. J Immunol. 1998;160:3081–3085.
- Wang J, Saffold S, Cao X, Krauss J, Chen W. Eliciting T cell immunity against poorly immunogenic tumors by immunization with dendritic cell-tumor fusion vaccines. J Immunol. 1998;161:5516–5524.
- Tanaka H, Shimizu K, Hayashi T, Shu S. Therapeutic immune response induced by electrofusion of dendritic and tumor cells. Cell Immunol. 2002;220:1–12. doi:10.1016/S0008-8749(03)00009-1.
- Orentas RJ, Schauer D, Bin Q, Johnson BD. Electrofusion of a weakly immunogenic neuroblastoma with dendritic cells produces a tumor vaccine. Cell Immunol. 2001;213:4–13. doi:10.1006/cimm.2001.1864.
- Kjaergaard J, Shimizu K, Shu S. Electrofusion of syngeneic dendritic cells and tumor generates potent therapeutic vaccine. Cell Immunol. 2003;225:65–74. doi:10.1016/j.cellimm.2003.09.005.
- Sukhorukov VL, Reuss R, Endter JM, Fehrmann S, Katsen-Globa A, Gessner P, Steinbach A, Müller KJ, Karpas A, Zimmermann U, et al. A biophysical approach to the optimisation of dendritic-tumour cell electrofusion. Biochem Biophys Res Commun. 2006;346:829–839. doi:10.1016/j.bbrc.2006.05.193.
- Cathelin D, Nicolas A, Bouchot A, Fraszczak J, Labbe J, Bonnotte B. Dendritic cell-tumor cell hybrids and immunotherapy: what’s next?. Cytotherapy. 2011;13:774–785. doi:10.3109/14653249.2011.553593.
- Errington F, Jones J, Merrick A, Bateman A, Harrington K, Gough M, O’Donnell D, Selby P, Vile R, Melcher A, et al. Fusogenic membrane glycoprotein-mediated tumour cell fusion activates human dendritic cells for enhanced IL-12 production and T-cell priming. Gene Ther. 2006;13:138–149. doi:10.1038/sj.gt.3302609.
- Chevalier MF, Bobisse S, Costa-Nunes C, Cesson V, Jichlinski P, Speiser DE, Harari A, Coukos G, Romero P, Nardelli-Haefliger D, et al. High-throughput monitoring of human tumor-specific T-cell responses with large peptide pools. OncoImmunology. 2015;4:e1029702. doi:10.1080/2162402X.2015.1029702.
- Fromm PD, Papadimitrious MS, Hsu JL, Van Kooten Losio N, Verma ND, Lo TH, Silveira PA, Bryant CE, Turtle CJ, Prue RL, et al. CMRF-56+ blood dendritic cells loaded with mRNA induce effective antigen-specific cytotoxic T-lymphocyte responses. OncoImmunology. 2016;5:e1168555. doi:10.1080/2162402X.2016.1168555.
- Bonifaz LC, Bonnyay DP, Charalambous A, Darguste DI, Fujii S, Soares H, Brimnes MK, Moltedo B, Moran TM, Steinman RM, et al. In vivo targeting of antigens to maturing dendritic cells via the DEC-205 receptor improves T cell vaccination. J Exp Med. 2004;199:815–824. doi:10.1084/jem.20032220.
- Bonifaz L, Bonnyay D, Mahnke K, Rivera M, Nussenzweig MC, Steinman RM. Efficient targeting of protein antigen to the dendritic cell receptor DEC-205 in the steady state leads to antigen presentation on major histocompatibility complex class I products and peripheral CD8+ T cell tolerance. J Exp Med. 2002;196:1627–1638. doi:10.1084/jem.20021598.
- Hawiger D, Inaba K, Dorsett Y, Guo M, Mahnke K, Rivera M, Ravetch JV, Steinman RM, Nussenzweig MC. Dendritic cells induce peripheral T cell unresponsiveness under steady state conditions in vivo. J Exp Med. 2001;194:769–780. doi:10.1084/jem.194.6.769.
- Adotevi O, Vingert B, Freyburger L, Shrikant P, Lone Y-C, Quintin-Colonna F, Haicheur N, Amessou M, Herbelin A, Langlade-Demoyen P, et al. B Subunit of Shiga Toxin-Based Vaccines Synergize with α-Galactosylceramide to Break Tolerance against Self Antigen and Elicit Antiviral Immunity. J Immunol. 2007;179:3371–3379. doi:10.4049/jimmunol.179.5.3371.
- Berraondo P, Nouze C, Preville X, Ladant D, Leclerc C. Eradication of large tumors in mice by a tritherapy targeting the innate, adaptive, and regulatory components of the immune system. Cancer Res. 2007;67:8847–8855. doi:10.1158/0008-5472.CAN-07-0321.
- Tacken PJ, de Vries IJ, Gijzen K, Joosten B, Wu D, Rother RP, Faas SJ, Punt CJA, Torensma R, Adema GJ, et al. Effective induction of naive and recall T-cell responses by targeting antigen to human dendritic cells via a humanized anti-DC-SIGN antibody. Blood. 2005;106:1278–1285. doi:10.1182/blood-2005-01-0318.
- Klechevsky E, Flamar A-L, Cao Y, Blanck J-P, Liu M, O’Bar A, Agouna-Deciat O, Klucar P, Thompson-Snipes L, Zurawski S, et al. Cross-priming CD8+ T cells by targeting antigens to human dendritic cells through DCIR. Blood. 2010;116:1685–1697. doi:10.1182/blood-2010-01-264960.
- Cruz LJ, Tacken PJ, Pots JM, Torensma R, Buschow SI, Figdor CG. Comparison of antibodies and carbohydrates to target vaccines to human dendritic cells via DC-SIGN. Biomaterials. 2012;33:4229–4239. doi:10.1016/j.biomaterials.2012.02.036.
- Schreibelt G, Klinkenberg LJ, Cruz LJ, Tacken PJ, Tel J, Kreutz M, Adema GJ, Brown GD, Figdor CG, de Vries IJM, et al. The C-type lectin receptor CLEC9A mediates antigen uptake and (cross-)presentation by human blood BDCA3+ myeloid dendritic cells. Blood. 2012;119:2284–2292. doi:10.1182/blood-2011-08-373944.
- Tacken PJ, Ginter W, Berod L, Cruz LJ, Joosten B, Sparwasser T, Figdor CG, Cambi A. Targeting DC-SIGN via its neck region leads to prolonged antigen residence in early endosomes, delayed lysosomal degradation, and cross-presentation. Blood. 2011;118:4111–4119. doi:10.1182/blood-2011-04-346957.
- Tacken PJ, Ter Huurne M, Torensma R, Figdor CG. Antibodies and carbohydrate ligands binding to DC-SIGN differentially modulate receptor trafficking. Eur J Immunol. 2012;42:1989–1998. doi:10.1002/eji.201142258.
- Tacken PJ, Zeelenberg IS, Cruz LJ, van Hout-kuijer MA, van de Glind G, Fokkink RG, Lambeck AJA, Figdor CG. Targeted delivery of TLR ligands to human and mouse dendritic cells strongly enhances adjuvanticity. Blood. 2011;118:6836–6844. doi:10.1182/blood-2011-07-367615.
- Hammerich L, Bhardwaj N, Kohrt HE, Brody JD. In situ vaccination for the treatment of cancer. Immunotherapy. 2016;8:315–330. doi:10.2217/imt.15.120.
- Fotaki G, Jin C, Kerzeli IK, Ramachandran M, Martikainen -M-M, Karlsson-Parra A, Yu D, Essand M. Cancer vaccine based on a combination of an infection-enhanced adenoviral vector and pro-inflammatory allogeneic DCs leads to sustained antigen-specific immune responses in three melanoma models. Oncoimmunology. 2018;7:e1397250. doi:10.1080/2162402X.2017.1397250.
- Zitvogel L, Regnault A, Lozier A, Wolfers J, Flament C, Tenza D, Ricciardi-Castagnoli P, Raposo G, Amigorena S. Eradication of established murine tumors using a novel cell-free vaccine: dendritic cell-derived exosomes. Nature Medicine. 1998;4:594–600. doi:10.1038/nm0598-594.
- Thery C, Regnault A, Garin J, Wolfers J, Zitvogel L, Ricciardi-Castagnoli P, Raposo G, Amigorena S. Molecular characterization of dendritic cell-derived exosomes. Selective accumulation of the heat shock protein hsc73. J Cell Biol. 1999;147:599–610. doi:10.1083/jcb.147.3.599.
- Viaud S, Thery C, Ploix S, Tursz T, Lapierre V, Lantz O, Zitvogel L, Chaput N. Dendritic cell-derived exosomes for cancer immunotherapy: what’s next?. Cancer Res. 2010;70:1281–1285. doi:10.1158/0008-5472.CAN-09-3276.
- Van Deun J, Mestdagh P, Agostinis P, Akay Ö, Anand S, Anckaert J, Martinez ZA, Baetens T, Beghein E, Bertier L, et al. EV-TRACK: transparent reporting and centralizing knowledge in extracellular vesicle research. Nature Methods. 2017;14:228–232. doi:10.1038/nmeth.4185.
- Muller L, Simms P, Hong C-S, Nishimura MI, Jackson EK, Watkins SC, Whiteside TL. Human tumor-derived exosomes (TEX) regulate Treg functions via cell surface signaling rather than uptake mechanisms. Oncoimmunology. 2017;6:e1261243. doi:10.1080/2162402X.2016.1261243.
- Fotaki G, Jin C, Ramachandran M, Kerzeli IK, Karlsson-Parra A, Yu D, Essand M. Pro-inflammatory allogeneic DCs promote activation of bystander immune cells and thereby license antigen-specific T-cell responses. Oncoimmunology. 2018;7:e1395126. doi:10.1080/2162402X.2017.1395126.
- Fucikova J, Rozkova D, Ulcova H, Budinsky V, Sochorova K, Pokorna K, Bartůňková J, Špíšek R. Poly I: C-activated dendritic cells that were generated in CellGro for use in cancer immunotherapy trials. Journal of Translational Medicine. 2011;9:223. doi:10.1186/1479-5876-9-223.
- Fucikova J, Kralikova P, Fialova A, Brtnicky T, Rob L, Bartunkova J, Spisek R. Human tumor cells killed by anthracyclines induce a tumor-specific immune response. Cancer Res. 2011;71:4821–4833. doi:10.1158/0008-5472.CAN-11-0950.
- Bercovici N, Haicheur N, Massicard S, Vernel-Pauillac F, Adotevi O, Landais D, Gorin I, Robert C, Miles Prince H, Grob -J-J, et al. Analysis and characterization of antitumor T-cell response after administration of dendritic cells loaded with allogeneic tumor lysate to metastatic melanoma patients. J Immunother. 2008;31:101–112. doi:10.1097/CJI.0b013e318159f5ba.
- Li M, You S, Ge W, Ma S, Ma N, Zhao C. Induction of T-cell immunity against leukemia by dendritic cells pulsed with total RNA isolated from leukemia cells. Chin Med J (Engl). 2003;116:1655–1661.
- Lee J, Boczkowski D, Nair S. Programming human dendritic cells with mRNA. Methods in Molecular Biology. 2013;969:111–125.
- Garg NK, Dwivedi P, Prabha P, Tyagi RK. RNA pulsed dendritic cells: an approach for cancer immunotherapy. Vaccine. 2013;31:1141–1156. doi:10.1016/j.vaccine.2012.12.027.
- Sayour EJ, De Leon G, Pham C, Grippin A, Kemeny H, Chua J, Huang J, Sampson JH, Sanchez-Perez L, Flores C, et al. Systemic activation of antigen-presenting cells via RNA-loaded nanoparticles. Oncoimmunology. 2017;6:e1256527. doi:10.1080/2162402X.2016.1256527.
- He J, Zheng R, Zhang Z, Tan J, Zhou C, Zhang G, Jiang X, Sun Q, Zhou S, Zheng D, et al. Collagen I enhances the efficiency and anti-tumor activity of dendritic-tumor fusion cells. Oncoimmunology. 2017;6:e1361094. doi:10.1080/2162402X.2017.1361094.
- Copland MJ, Baird MA, Rades T, McKenzie JL, Becker B, Reck F, Tyler PC, Davies NM. Liposomal delivery of antigen to human dendritic cells. Vaccine. 2003;21:883–890. doi:10.1016/S0264-410X(02)00536-4.
- van Broekhoven CL, Parish CR, Demangel C, Britton WJ, Altin JG. Targeting dendritic cells with antigen-containing liposomes: a highly effective procedure for induction of antitumor immunity and for tumor immunotherapy. Cancer Res. 2004;64:4357–4365. doi:10.1158/0008-5472.CAN-04-0138.
- Badiee A, Davies N, McDonald K, Radford K, Michiue H, Hart D, Kato M. Enhanced delivery of immunoliposomes to human dendritic cells by targeting the multilectin receptor DEC-205. Vaccine. 2007;25:4757–4766. doi:10.1016/j.vaccine.2007.04.029.
- Yang L, Yang H, Rideout K, Cho T, Joo KI, Ziegler L, Elliot A, Walls A, Yu D, Baltimore D, et al. Engineered lentivector targeting of dendritic cells for in vivo immunization. Nat Biotechnol. 2008;26:326–334. doi:10.1038/nbt1390.
- Hangalapura BN, Oosterhoff D, de Groot J, Boon L, Tuting T, van den Eertwegh AJ, Gerritsen WR, van Beusechem VW, Pereboev A, Curiel DT, et al. Potent antitumor immunity generated by a CD40-targeted adenoviral vaccine. Cancer Res. 2011;71:5827–5837. doi:10.1158/0008-5472.CAN-11-0804.
- Thacker EE, Nakayama M, Smith BF, Bird RC, Muminova Z, Strong TV, Timares L, Korokhov N, O’Neill AM, de Gruijl TD, et al. A genetically engineered adenovirus vector targeted to CD40 mediates transduction of canine dendritic cells and promotes antigen-specific immune responses in vivo. Vaccine. 2009;27:7116–7124. doi:10.1016/j.vaccine.2009.09.055.
- Korokhov N, de Gruijl TD, Aldrich WA, Triozzi PL, Banerjee PT, Gillies SD, Curiel TJ, Douglas JT, Scheper RJ, Curiel DT, et al. High efficiency transduction of dendritic cells by adenoviral vectors targeted to DC-SIGN. Cancer Biology & Therapy. 2005;4:289–294. doi:10.4161/cbt.4.3.1499.
- Apostolopoulos V, Thalhammer T, Tzakos AG, Stojanovska L. Targeting antigens to dendritic cell receptors for vaccine development. Journal of Drug Delivery. 2013;2013:869718.
- Cauwels A, Van Lint S, Garcin G, Bultinck J, Paul F, Gerlo S, Van der Heyden J, Bordat Y, Catteeuw D, De Cauwer L, et al. A safe and highly efficient tumor-targeted type I interferon immunotherapy depends on the tumor microenvironment. Oncoimmunology. 2018;7:e1398876. doi:10.1080/2162402X.2017.1398876.
- Tel J, Aarntzen EH, Baba T, Schreibelt G, Schulte BM, Benitez-Ribas D, Boerman OC, Croockewit S, Oyen WJG, van Rossum M, et al. Natural human plasmacytoid dendritic cells induce antigen-specific T-cell responses in melanoma patients. Cancer Res. 2013;73:1063–1075. doi:10.1158/0008-5472.CAN-12-2583.
- Schreibelt G, Bol KF, Westdorp H, Wimmers F, Aarntzen EH, Duiveman-de Boer T, van de Rakt MWMM, Scharenborg NM, de Boer AJ, Pots JM, et al. Effective Clinical Responses in Metastatic Melanoma Patients after Vaccination with Primary Myeloid Dendritic Cells. Clinical Cancer Research: an Official Journal of the American Association for Cancer Research. 2016;22:2155–2166. doi:10.1158/1078-0432.CCR-15-2205.
- Chung DJ, Carvajal RD, Postow MA, Sharma S, Pronschinske KB, Shyer JA, Singh-Kandah S, Dickson MA, D’Angelo SP, Wolchok JD, et al. Langerhans-type dendritic cells electroporated with TRP-2 mRNA stimulate cellular immunity against melanoma: results of a phase I vaccine trial. Oncoimmunology. 2018;7:e1372081. doi:10.1080/2162402X.2017.1372081.
- Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, Redfern CH, Ferrari AC, Dreicer R, Sims RB, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. The New England Journal of Medicine. 2010;363:411–422. doi:10.1056/NEJMoa1001294.
- Higano CS, Small EJ, Schellhammer P, Yasothan U, Gubernick S, Kirkpatrick P, Kantoff PW. Sipuleucel-T. Nat Rev Drug Discov. 2010;9:513–514. doi:10.1038/nrd3220.
- Cheever MA, Higano CS. PROVENGE (Sipuleucel-T) in prostate cancer: the first FDA-approved therapeutic cancer vaccine. Clinical Cancer Research: an Official Journal of the American Association for Cancer Research. 2011;17:3520–3526. doi:10.1158/1078-0432.CCR-10-3126.
- Vacchelli E, Eggermont A, Sautes-Fridman C, Galon J, Zitvogel L, Kroemer G, Galluzzi L. Trial watch: oncolytic viruses for cancer therapy. Oncoimmunology. 2013;2:e24612. doi:10.4161/onci.24612.
- Galluzzi L, Chan TA, Kroemer G, Wolchok JD, Lopez-Soto A. The hallmarks of successful anticancer immunotherapy. Science Translational Medicine. 2018;10.
- Martins F, Sofiya L, Sykiotis GP, Lamine F, Maillard M, Fraga M, Shabafrouz K, Ribi C, Cairoli A, Guex-Crosier Y, et al. Adverse effects of immune-checkpoint inhibitors: epidemiology, management and surveillance. Nature Reviews Clinical Oncology. 2019;16:563–580. doi:10.1038/s41571-019-0218-0.
- Hendriks D, Choi G, de Bruyn M, Wiersma VR, Bremer E. Antibody-Based Cancer Therapy: successful Agents and Novel Approaches. International Review of Cell and Molecular Biology. 2017;331:289–383.
- de la Cruz-merino L, Chiesa M, Caballero R, Rojo F, Palazon N, Carrasco FH, et al. Breast Cancer Immunology and Immunotherapy: current Status and Future Perspectives. International Review of Cell and Molecular Biology. 2017;331:1–53.
- Havel JJ, Chowell D, Chan TA. The evolving landscape of biomarkers for checkpoint inhibitor immunotherapy. Nature Reviews Cancer. 2019;19:133–150. doi:10.1038/s41568-019-0116-x.
- O’Donnell JS, Teng MWL, Smyth MJ. Cancer immunoediting and resistance to T cell-based immunotherapy. Nature Reviews Clinical Oncology. 2019;16:151–167.DOI: 10.1038/s41571-018-0142-8.
- Gardner JK, Mamotte CDS, Jackaman C, Nelson DJ. Modulation of dendritic cell and T cell cross-talk during aging: the potential role of checkpoint inhibitory molecules. Ageing Research Reviews. 2017;38:40–51. doi:10.1016/j.arr.2017.07.002.
- Zhao Y, Qiao G, Wang X, Song Y, Zhou X, Jiang N, Zhou L, Huang H, Zhao J, Morse MA, et al. Combination of DC/CIK adoptive T cell immunotherapy with chemotherapy in advanced non-small-cell lung cancer (NSCLC) patients: a prospective patients’ preference-based study (PPPS). Clinical & Translational Oncology: Official Publication of the Federation of Spanish Oncology Societies and of the National Cancer Institute of Mexico. 2019;21:721–728. doi:10.1007/s12094-018-1968-3.
- Turgeon G-A, Weickhardt A, Azad AA, Solomon B, Siva S. Radiotherapy and immunotherapy: a synergistic effect in cancer care. The Medical Journal of Australia. 2019;210:47–53. doi:10.5694/mja2.12046.
- Liu Y, Bewersdorf JP, Stahl M, Zeidan AM. Immunotherapy in acute myeloid leukemia and myelodysplastic syndromes: the dawn of a new era?. Blood Reviews. 2019;34:67–83. doi:10.1016/j.blre.2018.12.001.
- Kongsted P, Borch TH, Ellebaek E, Iversen TZ, Andersen R, Met Ö, Hansen M, Lindberg H, Sengeløv L, Svane IM, et al. Dendritic cell vaccination in combination with docetaxel for patients with metastatic castration-resistant prostate cancer: A randomized phase II study. Cytotherapy. 2017;19:500–513. doi:10.1016/j.jcyt.2017.01.007.
- Hansen M. The role of dendritic cells in cancer. Mediators of Inflammation. 2017;39:307–316.
- Garg AD, Coulie PG, Van den Eynde BJ, Agostinis P. Integrating Next-Generation Dendritic Cell Vaccines into the Current Cancer Immunotherapy Landscape. Trends Immunol. 2017;38:577–593. doi:10.1016/j.it.2017.05.006.
- Garg AD, Vara Perez M, Schaaf M, Agostinis P, Zitvogel L, Kroemer G, Galluzzi L. Trial watch: dendritic cell-based anticancer immunotherapy. Oncoimmunology. 2017;6:e1328341. doi:10.1080/2162402X.2017.1328341.
- Aranda F, Vacchelli E, Eggermont A, Galon J, Fridman WH, Zitvogel L, Kroemer G, Galluzzi L. Trial Watch: immunostimulatory monoclonal antibodies in cancer therapy. Oncoimmunology. 2014;3:e27297. doi:10.4161/onci.27297.
- Nimanong S, Ostroumov D, Wingerath J, Knocke S, Woller N, Gurlevik E, Falk CS, Manns MP, Kühnel F, Wirth TC, et al. CD40 Signaling Drives Potent Cellular Immune Responses in Heterologous Cancer Vaccinations. Cancer Res. 2017;77:1918–1926. doi:10.1158/0008-5472.CAN-16-2089.
- Moreno Ayala MA, Gottardo MF, Imsen M, Asad AS, Bal de Kier JE, Casares N, Lasarte JJ, Seilicovich A, Candolfi M. Therapeutic blockade of Foxp3 in experimental breast cancer models. Breast Cancer Research and Treatment. 2017;166:393–405. doi:10.1007/s10549-017-4414-2.
- Liu H, Chen L, Liu J, Meng H, Zhang R, Ma L, Wu L, Yu S, Shi F, Li Y, et al. Co-delivery of tumor-derived exosomes with alpha-galactosylceramide on dendritic cell-based immunotherapy for glioblastoma. Cancer Letters. 2017;411:182–190. doi:10.1016/j.canlet.2017.09.022.
- Escriba-Garcia L, Alvarez-Fernandez C, Tellez-Gabriel M, Sierra J, Briones J. Dendritic cells combined with tumor cells and α-galactosylceramide induce a potent, therapeutic and NK-cell dependent antitumor immunity in B cell lymphoma. Journal of Translational Medicine. 2017;15:115. doi:10.1186/s12967-017-1219-3.
- Heine A, Held SAE, Schulte-Schrepping J, Wolff JFA, Klee K, Ulas T, Schmacke NA, Daecke SN, Riethausen K, Schultze JL, et al. Generation and functional characterization of MDSC-like cells. Oncoimmunology. 2017;6:e1295203. doi:10.1080/2162402X.2017.1295203.
- Vo M-C, Nguyen-Pham T-N, Lee H-J, Jaya Lakshmi T, Yang S, Jung S-H, Kim H-J, Lee -J-J. Combination therapy with dendritic cells and lenalidomide is an effective approach to enhance antitumor immunity in a mouse colon cancer model. Oncotarget. 2017;8:27252–27262. doi:10.18632/oncotarget.15917.
- Merry TL, Brooks AES, Masson SW, Adams SE, Jaiswal JK, Jamieson SMF, Shepherd PR. The CSF1 receptor inhibitor pexidartinib (PLX3397) reduces tissue macrophage levels without affecting glucose homeostasis in mice. International Journal of Obesity. 2019. doi:10.1038/s41366-019-0355-7.
- Lee J-H, Chen TW, Hsu C-H, Yen Y-H, Yang JC, Cheng A-L, Sasaki S-I, Chiu L, Sugihara M, Ishizuka T, et al. A phase I study of pexidartinib, a colony-stimulating factor 1 receptor inhibitor, in Asian patients with advanced solid tumors. Investigational New Drugs. 2019. doi:10.1007/s10637-019-00745-z.
- Dammeijer F, Lievense LA, Kaijen-Lambers ME, van Nimwegen M, Bezemer K, Hegmans JP, van Hall T, Hendriks RW, Aerts JG. Depletion of Tumor-Associated Macrophages with a CSF-1R Kinase Inhibitor Enhances Antitumor Immunity and Survival Induced by DC Immunotherapy. Cancer Immunology Research. 2017;5:535–546. doi:10.1158/2326-6066.CIR-16-0309.
- Moreno Ayala MA, Gottardo MF, Gori MS, Nicola Candia AJ, Caruso C, De Laurentiis A, Imsen M, Klein S, Bal de Kier Joffé E, Salamone G, et al. Dual activation of Toll-like receptors 7 and 9 impairs the efficacy of antitumor vaccines in murine models of metastatic breast cancer. J Cancer Res Clin Oncol. 2017;143:1713–1732. doi:10.1007/s00432-017-2421-7.
- Vacchelli E, Aranda F, Eggermont A, Galon J, Sautes-Fridman C, Cremer I, Zitvogel L, Kroemer G, Galluzzi L. Trial Watch: chemotherapy with immunogenic cell death inducers. Oncoimmunology. 2014;3:e27878. doi:10.4161/onci.27878.
- Galluzzi L, Kroemer G. Calreticulin and type I interferon: an unsuspected connection. Oncoimmunology. 2017;6:e1288334. doi:10.1080/2162402X.2017.1288334.
- Garg AD, More S, Rufo N, Mece O, Sassano ML, Agostinis P, Zitvogel L, Kroemer G, Galluzzi L. Trial watch: immunogenic cell death induction by anticancer chemotherapeutics. Oncoimmunology. 2017;6:e1386829. doi:10.1080/2162402X.2017.1386829.
- Antonios JP, Soto H, Everson RG, Moughon D, Orpilla JR, Shin NP, Sedighim S, Treger J, Odesa S, Tucker A, et al. Immunosuppressive tumor-infiltrating myeloid cells mediate adaptive immune resistance via a PD-1/PD-L1 mechanism in glioblastoma. Neuro Oncol. 2017;19:796–807. doi:10.1093/neuonc/now287.
- Arab S, Kheshtchin N, Ajami M, Ashurpoor M, Safvati A, Namdar A, Mirzaei R, Mousavi Niri N, Jadidi-Niaragh F, Ghahremani MH, et al. Increased efficacy of a dendritic cell-based therapeutic cancer vaccine with adenosine receptor antagonist and CD73 inhibitor. Tumour Biol. 2017;39:1010428317695021. doi:10.1177/1010428317695021.
- Pol J, Kroemer G, Galluzzi L. First oncolytic virus approved for melanoma immunotherapy. Oncoimmunology. 2016;5:e1115641. doi:10.1080/2162402X.2015.1115641.
- Pol J, Bloy N, Obrist F, Eggermont A, Galon J, Cremer I, Erbs P, Limacher J-M, Preville X, Zitvogel L, et al. Trial Watch:: oncolytic viruses for cancer therapy. Oncoimmunology. 2014;3:e28694. doi:10.4161/onci.28694.
- Komorowski M, Tisonczyk J, Kolakowska A, Drozdz R, Kozbor D. Modulation of the Tumor Microenvironment by CXCR4 Antagonist-Armed Viral Oncotherapy Enhances the Antitumor Efficacy of Dendritic Cell Vaccines against Neuroblastoma in Syngeneic Mice. Viruses. 2018;10. doi: 10.3390/v10090455.
- Stefanski HE, Jonart L, Goren E, Mule JJ, Blazar BR, Labrecque N. A novel approach to improve immune effector responses post transplant by restoration of CCL21 expression. PLoS One. 2018;13:e0193461. doi:10.1371/journal.pone.0193461.
- Van Woensel M, Mathivet T, Wauthoz N, Rosiere R, Garg AD, Agostinis P, Mathieu V, Kiss R, Lefranc F, Boon L, et al. Sensitization of glioblastoma tumor micro-environment to chemo- and immunotherapy by Galectin-1 intranasal knock-down strategy. Sci Rep. 2017;7:1217. doi:10.1038/s41598-017-01279-1.
- Huang F, Wan J, Hao S, Deng X, Chen L, Ma L. TGF-β1-silenced leukemia cell-derived exosomes target dendritic cells to induce potent anti-leukemic immunity in a mouse model. Cancer Immunology, Immunotherapy: CII. 2017;66:1321–1331. doi:10.1007/s00262-017-2028-5.
- Lu Z, Zuo B, Jing R, Gao X, Rao Q, Liu Z, Qi H, Guo H, Yin H. Dendritic cell-derived exosomes elicit tumor regression in autochthonous hepatocellular carcinoma mouse models. Journal of Hepatology. 2017;67:739–748. doi:10.1016/j.jhep.2017.05.019.
- Bryson PD, Han X, Truong N, Wang P. Breast cancer vaccines delivered by dendritic cell-targeted lentivectors induce potent antitumor immune responses and protect mice from mammary tumor growth. Vaccine. 2017;35:5842–5849. doi:10.1016/j.vaccine.2017.09.017.
- Liu L, Wang Y, Miao L, Liu Q, Musetti S, Li J, Huang L. Combination Immunotherapy of MUC1 mRNA Nano-vaccine and CTLA-4 Blockade Effectively Inhibits Growth of Triple Negative Breast Cancer. Mol Ther. 2018;26:45–55. doi:10.1016/j.ymthe.2017.10.020.
- Oberli MA, Reichmuth AM, Dorkin JR, Mitchell MJ, Fenton OS, Jaklenec A, Anderson DG, Langer R, Blankschtein D. Lipid Nanoparticle Assisted mRNA Delivery for Potent Cancer Immunotherapy. Nano Letters. 2017;17:1326–1335. doi:10.1021/acs.nanolett.6b03329.
- Wennhold K, Weber TM, Klein-Gonzalez N, Thelen M, Garcia-Marquez M, Chakupurakal G, Fiedler A, Schlösser HA, Fischer R, Theurich S, et al. CD40-activated B cells induce anti-tumor immunity in vivo. Oncotarget. 2017;8:27740–27753. doi:10.18632/oncotarget.7720.
- Wculek SK, Amores-Iniesta J, Conde-Garrosa R, Khouili SC, Melero I, Sancho D. Effective cancer immunotherapy by natural mouse conventional type-1 dendritic cells bearing dead tumor antigen. J Immunother Cancer. 2019;7:100. doi: 10.1186/s40425-019-0565-5.
- Yang M, Li C, Zhu S, Cao L, Kroemer G, Zeh H, Tang D, Kang R. TFAM is a novel mediator of immunogenic cancer cell death. Oncoimmunology. 2018;7:e1431086. doi:10.1080/2162402X.2018.1431086.
- Castoldi F, Vacchelli E, Zitvogel L, Maiuri MC, Pietrocola F, Kroemer G. Systemic autophagy in the therapeutic response to anthracycline-based chemotherapy. Oncoimmunology. 2019;8:e1498285. doi: 10.1080/2162402X.2018.1498285.
- Roselli E, Araya P, Nunez NG, Gatti G, Graziano F, Sedlik C, Benaroch P, Piaggio E, Maccioni M. TLR3 Activation of Intratumoral CD103+ Dendritic Cells Modifies the Tumor Infiltrate Conferring Anti-tumor Immunity. Frontiers in Immunology. 2019;10:503. doi:10.3389/fimmu.2019.00503.
- Cancel J-C, Crozat K, Dalod M, Mattiuz R. Are Conventional Type 1 Dendritic Cells Critical for Protective Antitumor Immunity and How?. Frontiers in Immunology. 2019;10:9. doi:10.3389/fimmu.2019.00009.
- Huang F-Y, Lei J, Sun Y, Yan F, Chen B, Zhang L, Lu Z, Cao R, Lin -Y-Y, Wang -C-C, et al. Induction of enhanced immunogenic cell death through ultrasound-controlled release of doxorubicin by liposome-microbubble complexes. Oncoimmunology. 2018;7:e1446720. doi:10.1080/2162402X.2018.1446720.
- Bottcher JP, Reis ESC. The Role of Type 1 Conventional Dendritic Cells in Cancer Immunity. Trends in Cancer. 2018;4:784–792. doi:10.1016/j.trecan.2018.09.001.
- Hotblack A, Holler A, Piapi A, Ward S, Stauss HJ, Bennett CL. Tumor-Resident Dendritic Cells and Macrophages Modulate the Accumulation of TCR-Engineered T Cells in Melanoma. Mol Ther. 2018;26:1471–1481. doi:10.1016/j.ymthe.2018.03.011.
- Meyer MA, Baer JM, Knolhoff BL, Nywening TM, Panni RZ, Su X, Weilbaecher KN, Hawkins WG, Ma C, Fields RC, et al. Breast and pancreatic cancer interrupt IRF8-dependent dendritic cell development to overcome immune surveillance. Nat Commun. 2018;9:1250. doi:10.1038/s41467-018-03600-6.
- Giglio P, Gagliardi M, Tumino N, Antunes F, SmailiSu SJ, Cotella D, Santoro C, Bernardini R, Mattei M, Piacentini M, et al. PKR and GCN2 stress kinases promote an ER stress-independent eIF2alpha phosphorylation responsible for calreticulin exposure in melanoma cells. Oncoimmunology. 2018;7:e1466765. doi:10.1080/2162402X.2018.1466765.
- Bottcher JP, Bonavita E, Chakravarty P, Blees H, Cabeza-Cabrerizo M, Sammicheli S, Rogers NC, Sahai E, Zelenay S, Reis E Sousa C, et al. NK Cells Stimulate Recruitment of cDC1 into the Tumor Microenvironment Promoting Cancer Immune Control. Cell. 2018;172:1022–37 e14. doi:10.1016/j.cell.2018.01.004.
- Sanchez-Paulete AR, Teijeira A, Cueto FJ, Garasa S, Perez-Gracia JL, Sanchez-Arraez A, Sancho D, Melero I. Antigen cross-presentation and T-cell cross-priming in cancer immunology and immunotherapy. Annals of Oncology: Official Journal of the European Society for Medical Oncology. 2017;28:xii44–xii55. doi:10.1093/annonc/mdx237.
- Santegoets SJ, Stam AG, Lougheed SM, Gall H, Jooss K, Sacks N, Hege K, Lowy I, Scheper RJ, Gerritsen WR, et al. Myeloid derived suppressor and dendritic cell subsets are related to clinical outcome in prostate cancer patients treated with prostate GVAX and ipilimumab. J Immunother Cancer. 2014;2:31. doi:10.1186/s40425-014-0031-3.
- Bezu L, Sauvat A, Humeau J, Leduc M, Kepp O, Kroemer G. eIF2α phosphorylation: A hallmark of immunogenic cell death. Oncoimmunology. 2018;7:e1431089. doi:10.1080/2162402X.2018.1431089.
- Wang L, Fan J, Ye W, Han J, Zhang Y, Zhao L, Duan J, Yin D, Yi Y. The Expression of ILT4 in Myeloid Dendritic Cells in Patients with Hepatocellular Carcinoma. Immunological Investigations. 2019:1–15. doi: 10.1080/08820139.2019.1571507.
- Rajendran M, Looney S, Singh N, Elashiry M, Meghil MM, El-Awady AR, Tawfik O, Susin C, Arce RM, Cutler CW, et al. Systemic Antibiotic Therapy Reduces Circulating Inflammatory Dendritic Cells and Treg-Th17 Plasticity in Periodontitis. J Immunol. 2019;202:2690–2699. doi:10.4049/jimmunol.1900046.
- Stankovic B, Bjorhovde HAK, Skarshaug R, Aamodt H, Frafjord A, Muller E, Hammarström C, Beraki K, Bækkevold ES, Woldbæk PR, et al. Immune Cell Composition in Human Non-small Cell Lung Cancer. Frontiers in Immunology. 2019;9:3101. doi:10.3389/fimmu.2018.03101.
- Ventura A, Vassall A, Robinson E, Filler R, Hanlon D, Meeth K, Ezaldein H, Girardi M, Sobolev O, Bosenberg MW, et al. Extracorporeal Photochemotherapy Drives Monocyte-to-Dendritic Cell Maturation to Induce Anticancer Immunity. Cancer Res. 2018;78:4045–4058. doi:10.1158/0008-5472.CAN-18-0171.
- Wei XX, Perry J, Chang E, Zhang L, Hiatt RA, Ryan CJ, Small EJ, Fong L. Clinical Variables Associated With Overall Survival in Metastatic Castration-Resistant Prostate Cancer Patients Treated With Sipuleucel-T Immunotherapy. Clinical Genitourinary Cancer. 2018;16:184–90 e2. doi:10.1016/j.clgc.2017.12.004.
- Hijikata Y, Okazaki T, Tanaka Y, Murahashi M, Yamada Y, Yamada K, Takahashi A, Inoue H, Kishimoto J, Nakanishi Y, Oda Y. A phase I clinical trial of RNF43 peptide-related immune cell therapy combined with low-dose cyclophosphamide in patients with advanced solid tumors. PLoS One. 2018;13:e0187878. doi: 10.1371/journal.pone.0187878.
- Yanagisawa R, Koizumi T, Koya T, Sano K, Koido S, Nagai K, Kobayashi M, Okamoto M, Sugiyama H, Shimodaira S, et al. WT1-pulsed Dendritic Cell Vaccine Combined with Chemotherapy for Resected Pancreatic Cancer in a Phase I Study. Anticancer Research. 2018;38:2217–2225. doi:10.21873/anticanres.12464.
- Ogasawara M, Miyashita M, Ota S. Vaccination of Urological Cancer Patients With WT1 Peptide-Pulsed Dendritic Cells in Combination With Molecular Targeted Therapy or Conventional Chemotherapy Induces Immunological and Clinical Responses. Ther Apher Dial. 2018;22:266–277. doi:10.1111/1744-9987.12694.
- Antonarakis ES, Kibel AS, Yu EY, Karsh LI, Elfiky A, Shore ND, Vogelzang NJ, Corman JM, Millard FE, Maher JC, et al. Sequencing of Sipuleucel-T and Androgen Deprivation Therapy in Men with Hormone-Sensitive Biochemically Recurrent Prostate Cancer: A Phase II Randomized Trial. Clinical Cancer Research: an Official Journal of the American Association for Cancer Research. 2017;23:2451–2459. doi:10.1158/1078-0432.CCR-16-1780.
- Oostvogels R, Kneppers E, Minnema MC, Doorn RC, Franssen LE, Aarts T, Emmelot ME, Spierings E, Slaper-Cortenbach I, Westinga K, et al. Efficacy of host-dendritic cell vaccinations with or without minor histocompatibility antigen loading, combined with donor lymphocyte infusion in multiple myeloma patients. Bone Marrow Transplant. 2017;52:228–237. doi:10.1038/bmt.2016.250.
- Davis ID, Quirk J, Morris L, Seddon L, Tai TY, Whitty G, Cavicchiolo T, Ebert L, Jackson H, Browning J, et al. A pilot study of peripheral blood BDCA-1 (CD1c) positive dendritic cells pulsed with NY-ESO-1 ISCOMATRIX™ adjuvant.. Immunotherapy. 2017;9:249–259. doi:10.2217/imt-2016-0132.
- Wimmers F, de Haas N, Scholzen A, Schreibelt G, Simonetti E, Eleveld MJ, Brouwers HMLM, Beldhuis-Valkis M, Joosten I, de Jonge MI, et al. Monitoring of dynamic changes in Keyhole Limpet Hemocyanin (KLH)-specific B cells in KLH-vaccinated cancer patients. Sci Rep. 2017;7:43486. doi:10.1038/srep43486.
- Mehrotra S, Britten CD, Chin S, Garrett-Mayer E, Cloud CA, Li M, Scurti G, Salem ML, Nelson MH, Thomas MB, et al. Vaccination with poly(IC:LC) and peptide-pulsed autologous dendritic cells in patients with pancreatic cancer. J Hematol Oncol. 2017;10:82. doi:10.1186/s13045-017-0459-2.
- Franssen LE, Roeven MWH, Hobo W, Doorn R, Oostvogels R, Falkenburg JHF, van de Donk NW, Kester MGD, Fredrix H, Westinga K, et al. A phase I/II minor histocompatibility antigen-loaded dendritic cell vaccination trial to safely improve the efficacy of donor lymphocyte infusions in myeloma. Bone Marrow Transplant. 2017;52:1378–1383. doi:10.1038/bmt.2017.118.
- Shen J, Wang L-F, Zou Z-Y, Kong -W-W, Yan J, Meng F-Y, Chen F-J, Du J, Shao J, Xu Q-P, et al. Phase I clinical study of personalized peptide vaccination combined with radiotherapy for advanced hepatocellular carcinoma. World J Gastroenterol. 2017;23:5395–5404. doi:10.3748/wjg.v23.i29.5395.
- Lowenfeld L, Mick R, Datta J, Xu S, Fitzpatrick E, Fisher CS, Fox KR, DeMichele A, Zhang PJ, Weinstein SP, et al. Dendritic Cell Vaccination Enhances Immune Responses and Induces Regression of HER2 pos DCIS Independent of Route: results of Randomized Selection Design Trial. Clinical Cancer Research: an Official Journal of the American Association for Cancer Research. 2017;23:2961–2971. doi:10.1158/1078-0432.CCR-16-1924.
- Fukuda K, Funakoshi T, Sakurai T, Nakamura Y, Mori M, Tanese K, Tanikawa A, Taguchi J, Fujita T, Okamoto M, et al. Peptide-pulsed dendritic cell vaccine in combination with carboplatin and paclitaxel chemotherapy for stage IV melanoma. Melanoma Res. 2017;27:326–334. doi:10.1097/CMR.0000000000000342.
- Saka H, Kitagawa C, Ichinose Y, Takenoyama M, Ibata H, Kato T, Takami K, Yamashita M, Maeda T, Takeo S, et al. A randomized phase II study to assess the effect of adjuvant immunotherapy using α-GalCer-pulsed dendritic cells in the patients with completely resected stage II–IIIA non-small cell lung cancer: study protocol for a randomized controlled trial. Trials. 2017;18:429. doi:10.1186/s13063-017-2103-4.
- Gasser O, Sharples KJ, Barrow C, Williams GM, Bauer E, Wood CE, Mester B, Dzhelali M, Caygill G, Jones J, et al. A phase I vaccination study with dendritic cells loaded with NY-ESO-1 and α-galactosylceramide: induction of polyfunctional T cells in high-risk melanoma patients. Cancer Immunology, Immunotherapy: CII. 2018;67:285–298. doi:10.1007/s00262-017-2085-9.
- Ge C, Li R, Song H, Geng T, Yang J, Tan Q, Song L, Wang Y, Xue Y, Li Z, et al. Phase I clinical trial of a novel autologous modified-DC vaccine in patients with resected NSCLC. BMC Cancer. 2017;17:884. doi:10.1186/s12885-017-3859-3.
- Yao Y, Luo F, Tang C, Chen D, Qin Z, Hua W, Xu M, Zhong P, Yu S, Chen D, et al. Molecular subgroups and B7-H4 expression levels predict responses to dendritic cell vaccines in glioblastoma: an exploratory randomized phase II clinical trial. Cancer Immunology, Immunotherapy: CII. 2018;67:1777–1788. doi:10.1007/s00262-018-2232-y.
- Zhang W, Lu X, Cui P, Piao C, Xiao M, Liu X, Wang Y, Wu X, Liu J, Yang L, et al. Phase I/II clinical trial of a Wilms’ tumor 1-targeted dendritic cell vaccination-based immunotherapy in patients with advanced cancer. Cancer Immunology, Immunotherapy: CII. 2019;68:121–130. doi:10.1007/s00262-018-2257-2.
- Geskin LJ, Damiano JJ, Patrone CC, Butterfield LH, Kirkwood JM, Falo LD. Three antigen-loading methods in dendritic cell vaccines for metastatic melanoma. Melanoma Res. 2018;28:211–221. doi:10.1097/CMR.0000000000000441.
- Palma M, Hansson L, Mulder TA, Adamson L, Nasman-Glaser B, Eriksson I, Heimersson K, Ryblom H, Mozaffari F, Svensson A, et al. Lenalidomide as immune adjuvant to a dendritic cell vaccine in chronic lymphocytic leukemia patients. Eur J Haematol. 2018;101:68–77. doi:10.1111/ejh.13065.
- Jung S-H, Lee H-J, Lee Y-K, Yang D-H, Kim H-J, Rhee JH, Emmrich F, Lee -J-J. A phase I clinical study of autologous dendritic cell therapy in patients with relapsed or refractory multiple myeloma. Oncotarget. 2017;8:41538–41548. doi:10.18632/oncotarget.14582.
- Inoges S, Tejada S, de Cerio AL, Gallego Perez-Larraya J, Espinos J, Idoate MA, Domínguez PD, de Eulate RG, Aristu J, Bendandi M, et al. A phase II trial of autologous dendritic cell vaccination and radiochemotherapy following fluorescence-guided surgery in newly diagnosed glioblastoma patients. Journal of Translational Medicine. 2017;15:104. doi:10.1186/s12967-017-1202-z.
- Miwa S, Nishida H, Tanzawa Y, Takeuchi A, Hayashi K, Yamamoto N, Mizukoshi E, Nakamoto Y, Kaneko S, Tsuchiya H, et al. Phase 1/2 study of immunotherapy with dendritic cells pulsed with autologous tumor lysate in patients with refractory bone and soft tissue sarcoma. Cancer. 2017;123:1576–1584. doi:10.1002/cncr.30606.
- Herbert GS, Vreeland TJ, Clifton GT, Greene JM, Jackson DO, Hardin MO, Hale DF, Berry JS, Nichol P, Yin S, et al. Initial phase I/IIa trial results of an autologous tumor lysate, particle-loaded, dendritic cell (TLPLDC) vaccine in patients with solid tumors. Vaccine. 2018;36:3247–3253. doi:10.1016/j.vaccine.2018.04.078.
- Anguille S, Van de Velde AL, Smits EL, Van Tendeloo VF, Juliusson G, Cools N, Nijs G, Stein B, Lion E, Van Driessche A, et al. Dendritic cell vaccination as postremission treatment to prevent or delay relapse in acute myeloid leukemia. Blood. 2017;130:1713–1721. doi:10.1182/blood-2017-04-780155.
- Batich KA, Reap EA, Archer GE, Sanchez-Perez L, Nair SK, Schmittling RJ, Norberg P, Xie W, Herndon JE, Healy P, et al. Long-term Survival in Glioblastoma with Cytomegalovirus pp65-Targeted Vaccination. Clinical Cancer Research: an Official Journal of the American Association for Cancer Research. 2017;23:1898–1909. doi:10.1158/1078-0432.CCR-16-2057.
- Khoury HJ, Collins RH Jr., Blum W, Stiff PS, Elias L, Lebkowski JS, Reddy A, Nishimoto KP, Sen D, Wirth ED, et al. Immune responses and long-term disease recurrence status after telomerase-based dendritic cell immunotherapy in patients with acute myeloid leukemia. Cancer. 2017;123:3061–3072. doi:10.1002/cncr.30696.
- Reap EA, Suryadevara CM, Batich KA, Sanchez-Perez L, Archer GE, Schmittling RJ, Norberg PK, Herndon JE, Healy P, Congdon KL, et al. Dendritic Cells Enhance Polyfunctionality of Adoptively Transferred T Cells That Target Cytomegalovirus in Glioblastoma. Cancer Res. 2018;78:256–264. doi:10.1158/0008-5472.CAN-17-0469.
- Sonpavde G, McMannis JD, Bai Y, Seethammagari MR, Bull JMC, Hawkins V, Dancsak TK, Lapteva N, Levitt JM, Moseley A, et al. Phase I trial of antigen-targeted autologous dendritic cell-based vaccine with in vivo activation of inducible CD40 for advanced prostate cancer. Cancer Immunology, Immunotherapy: CII. 2017;66:1345–1357. doi:10.1007/s00262-017-2027-6.
- Lee JM, Lee M-H, Garon E, Goldman JW, Salehi-Rad R, Baratelli FE, Schaue D, Wang G, Rosen F, Yanagawa J, et al. Phase I Trial of Intratumoral Injection of CCL21 Gene–modified Dendritic Cells in Lung Cancer Elicits Tumor-Specific Immune Responses and CD8 + T-cell Infiltration. Clinical Cancer Research: an Official Journal of the American Association for Cancer Research. 2017;23:4556–4568. doi:10.1158/1078-0432.CCR-16-2821.
- Laurell A, Lonnemark M, Brekkan E, Magnusson A, Tolf A, Wallgren AC, Andersson B, Adamson L, Kiessling R, Karlsson-Parra A, et al. Intratumorally injected pro-inflammatory allogeneic dendritic cells as immune enhancers: a first-in-human study in unfavourable risk patients with metastatic renal cell carcinoma. J Immunother Cancer. 2017;5:52. doi:10.1186/s40425-017-0255-0.
- van de Loosdrecht AA, van Wetering S, Santegoets S, Singh SK, Eeltink CM, den Hartog Y, Koppes M, Kaspers J, Ossenkoppele GJ, Kruisbeek AM, et al. A novel allogeneic off-the-shelf dendritic cell vaccine for post-remission treatment of elderly patients with acute myeloid leukemia. Cancer Immunology, Immunotherapy: CII. 2018;67:1505–1518. doi:10.1007/s00262-018-2198-9.
- Chen C-L, Pan Q-Z, Weng D-S, Xie C-M, Zhao -J-J, Chen M-S, Peng R-Q, Li -D-D, Wang Y, Tang Y, et al. Safety and activity of PD-1 blockade-activated DC-CIK cells in patients with advanced solid tumors. Oncoimmunology. 2018;7:e1417721. doi:10.1080/2162402X.2017.1417721.
- Jiang N, Qiao G, Wang X, Morse MA, Gwin WR, Zhou L, Song Y, Zhao Y, Chen F, Zhou X, et al. Dendritic Cell/Cytokine-Induced Killer Cell Immunotherapy Combined with S-1 in Patients with Advanced Pancreatic Cancer: A Prospective Study. Clinical Cancer Research: an Official Journal of the American Association for Cancer Research. 2017;23:5066–5073. doi:10.1158/1078-0432.CCR-17-0492.
- Zhang B, Wu Q, Zhou YL, Guo X, Ge J, Fu J. Immune-related adverse events from combination immunotherapy in cancer patients: A comprehensive meta-analysis of randomized controlled trials. International Immunopharmacology. 2018;63:292–298. doi:10.1016/j.intimp.2018.08.014.
- Mehta RS, Rezvani K. Chimeric Antigen Receptor Expressing Natural Killer Cells for the Immunotherapy of Cancer. Frontiers in Immunology. 2018;9:283. doi:10.3389/fimmu.2018.00283.
- Klener Jr P Jr., Etrych T, Klener P. Biological Therapy of Hematologic Malignancies: toward a Chemotherapy- free Era. Current Medicinal Chemistry. 2019;26:1002–1018. doi:10.2174/0929867324666171006144725.
- Berraondo P, Sanmamed MF, Ochoa MC, Etxeberria I, Aznar MA, Perez-Gracia JL, Rodríguez-Ruiz ME, Ponz-Sarvise M, Castañón E, Melero I, et al. Cytokines in clinical cancer immunotherapy. British Journal of Cancer. 2019;120:6–15. doi:10.1038/s41416-018-0328-y.
- Vonderheide RH. The Immune Revolution: A Case for Priming, Not Checkpoint. Cancer Cell. 2018;33:563–569. doi:10.1016/j.ccell.2018.03.008.
- Marin-Acevedo JA, Soyano AE, Dholaria B, Knutson KL, Lou Y. Cancer immunotherapy beyond immune checkpoint inhibitors. J Hematol Oncol. 2018;11:8. doi:10.1186/s13045-017-0552-6.
- Mangsbo SM, Fletcher EAK, van Maren WWC, Redeker A, Cordfunke RA, Dillmann I, Dinkelaar J, Ouchaou K, Codee JDC, van der Marel GA, et al. Linking T cell epitopes to a common linear B cell epitope: A targeting and adjuvant strategy to improve T cell responses. Molecular Immunology. 2018;93:115–124. doi:10.1016/j.molimm.2017.11.004.
- Brooks N, Hsu J, Esparon S, Pouniotis D, Pietersz GA. Immunogenicity of a Tripartite Cell Penetrating Peptide Containing a MUC1 Variable Number of Tandem Repeat (VNTR) and A T Helper Epitope. Molecules. 2018;23. doi: 10.3390/molecules23092233.
- Pol J, Vacchelli E, Aranda F, Castoldi F, Eggermont A, Cremer I, Sautès-Fridman C, Fucikova J, Galon J, Spisek R, et al. Trial Watch: immunogenic cell death inducers for anticancer chemotherapy. Oncoimmunology. 2015;4:e1008866. doi:10.1080/2162402X.2015.1008866.
- Hwang WL, Pike LRG, Royce TJ, Mahal BA, Loeffler JS. Safety of combining radiotherapy with immune-checkpoint inhibition. Nature Reviews Clinical Oncology. 2018;15:477–494. doi:10.1038/s41571-018-0046-7.
- Taylor J, Pavlick D, Yoshimi A, Marcelus C, Chung SS, Hechtman JF, Benayed R, Cocco E, Durham BH, Bitner L, et al. Oncogenic TRK fusions are amenable to inhibition in hematologic malignancies. The Journal of Clinical Investigation. 2018;128:3819–3825. doi:10.1172/JCI120787.
- Dummer R, Ramelyte E, Schindler S, Thurigen O, Levesque MP, Koelblinger P. MEK inhibition and immune responses in advanced melanoma. Oncoimmunology. 2017;6:e1335843. doi:10.1080/2162402X.2017.1335843.
- Candeias SM, Gaipl US. The immune system in cancer prevention, development and therapy. Anti-cancer Agents in Medicinal Chemistry. 2016;16:101–107. doi:10.2174/1871520615666150824153523.
- Lee S, Son B, Park G, Kim H, Kang H, Jeon J, Youn H, Youn B. Immunogenic effect of hyperthermia on enhancing radiotherapeutic efficacy. International Journal of Molecular Sciences. 2018:19. doi: 10.3390/ijms19092795.
- Garg AD, Vandenberk L, Koks C, Verschuere T, Boon L, Van Gool SW, Vandenberk L, Koks C, Verschuere T, Boon L, et al. Dendritic cell vaccines based on immunogenic cell death elicit danger signals and T cell-driven rejection of high-grade glioma. Science Translational Medicine. 2016;8:328ra27. doi:10.1126/scitranslmed.aae0105.
- Garg AD, Vandenberk L, Van Woensel M, Belmans J, Schaaf M, Boon L, De Vleeschouwer S, Agostinis P. Preclinical efficacy of immune-checkpoint monotherapy does not recapitulate corresponding biomarkers-based clinical predictions in glioblastoma. Oncoimmunology. 2017;6:e1295903. doi:10.1080/2162402X.2017.1295903.
- Adams S, Gatti-Mays ME, Kalinsky K, Korde LA, Sharon E, Amiri-Kordestani L, Bear H, McArthur HL, Frank E, Perlmutter J, et al. Current Landscape of Immunotherapy in Breast Cancer: A Review. JAMA Oncol. 2019;5:1205. doi:10.1001/jamaoncol.2018.7147.
- Le QT, Colevas AD, O’Sullivan B, Lee AWM, Lee N, Ma B, Siu LL, Waldron J, Lim C-M, Riaz N, et al. Current Treatment Landscape of Nasopharyngeal Carcinoma and Potential Trials Evaluating the Value of Immunotherapy. J Natl Cancer Inst. 2019;111:655–663. doi:10.1093/jnci/djz044.
- Xiao Y, Ma D, Zhao S, Suo C, Shi J, Xue M-Z, Ruan M, Wang H, Zhao J, Li Q, et al. Multi-omics profiling reveals distinct microenvironment characterization and suggests immune escape mechanisms of triple-negative breast cancer. Clinical Cancer Research: an Official Journal of the American Association for Cancer Research. 2019;25:5002–5014. doi:10.1158/1078-0432.CCR-18-3524.
- Kong BY, Bolton H, Kim JW, Silveira PA, Fromm PD, Clark GJ. On the Other Side: manipulating the Immune Checkpoint Landscape of Dendritic Cells to Enhance Cancer Immunotherapy. Frontiers in Oncology. 2019;9:50. doi:10.3389/fonc.2019.00050.
- Vitale I, Sistigu A, Manic G, Rudqvist N-P, Trajanoski Z, Galluzzi L. Mutational and Antigenic Landscape in Tumor Progression and Cancer Immunotherapy. Trends Cell Biol. 2019;29:396–416. doi:10.1016/j.tcb.2019.01.003.
- Jiang N, Schonnesen AA, Ma K-Y. Ushering in Integrated T Cell Repertoire Profiling in Cancer. Trends in Cancer. 2019;5:85–94. doi:10.1016/j.trecan.2018.11.005.
- Pai CS, Huang JT, Lu X, Simons DM, Park C, Chang A, Tamaki W, Liu E, Roybal KT, Seagal J, et al. Clonal Deletion of Tumor-Specific T Cells by Interferon-γ Confers Therapeutic Resistance to Combination Immune Checkpoint Blockade. Immunity. 2019;50:477–92 e8. doi:10.1016/j.immuni.2019.01.006.
- Nadal E, Massuti B, Domine M, Garcia-Campelo R, Cobo M, Felip E. Immunotherapy with checkpoint inhibitors in non-small cell lung cancer: insights from long-term survivors. Cancer Immunology, Immunotherapy: CII. 2019;68:341–352. doi:10.1007/s00262-019-02310-2.
- Camidge DR, Doebele RC, Kerr KM. Comparing and contrasting predictive biomarkers for immunotherapy and targeted therapy of NSCLC. Nature Reviews Clinical Oncology. 2019;16:341–355. doi:10.1038/s41571-019-0173-9.
- Liau LM, Ashkan K, Tran DD, Campian JL, Trusheim JE, Cobbs CS, Heth JA, Salacz M, Taylor S, D’Andre SD, et al. First results on survival from a large Phase 3 clinical trial of an autologous dendritic cell vaccine in newly diagnosed glioblastoma. Journal of Translational Medicine. 2018;16:142. doi:10.1186/s12967-018-1507-6.
- Gulley JL, Mulders P, Albers P, Banchereau J, Bolla M, Pantel K, Powles T. Perspectives on sipuleucel-T: its role in the prostate cancer treatment paradigm. Oncoimmunology. 2016;5:e1107698. doi:10.1080/2162402X.2015.1107698.
- Anselmo da Costa I, Stenzl A, Bedke J. Inmunotherapy in prostate cancer. Archivos Espanoles De Urologia. 2019;72:211–222.
- DeMaria PJ, Bilusic M. Cancer Vaccines. hematology/oncology Clinics of North America. 2019;33:199–214. doi:10.1016/j.hoc.2018.12.001.
- Bates JP, Derakhshandeh R, Jones L, Webb TJ. Mechanisms of immune evasion in breast cancer. BMC Cancer. 2018;18:556. doi:10.1186/s12885-018-4441-3.
- Vitale LA, Thomas LJ, He L-Z, O’Neill T, Widger J, Crocker A, Sundarapandiyan K, Storey JR, Forsberg EM, Weidlick J, et al. Development of CDX-1140, an agonist CD40 antibody for cancer immunotherapy. Cancer Immunology, Immunotherapy: CII. 2019;68:233–245. doi:10.1007/s00262-018-2267-0.
- Pan L, Shang N, Shangguan J, Figini M, Xing W, Wang B, Sun C, Yang J, Zhang Y, Hu S, et al. Magnetic resonance imaging monitoring therapeutic response to dendritic cell vaccine in murine orthotopic pancreatic cancer models. American Journal of Cancer Research. 2019;9:562–573.
- Leeman H, Kaminska E, Green D, Bodman-Smith M, Gravett A, Bodman-Smith K, Copier J, Coulton G, Fusi A, Dalgleish AG, et al. Serum Apolipoprotein E and Other Inflammatory Markers Can Identify Non-Responding Patients to a Dendritic Cell Vaccine. Translational Oncology. 2019;12:397–403. doi:10.1016/j.tranon.2018.11.002.
- Ni M, Hoffmann J-M, Schmitt M, Schmitt A. Progress of dendritic cell-based cancer vaccines for patients with hematological malignancies. Expert Opinion on Biological Therapy. 2016;16:1113–1123. doi:10.1080/14712598.2016.1196181.
- Hsu SC, Lu LC, Chan KY, Huang CH, Cheng SL, Chan YS, Yang YS, Lai YT, Yao CL. Large-scale production and directed induction of functional dendritic cells ex vivo from serum-free expanded human hematopoietic stem cells. Cytotherapy. 2019;21:755–768. doi:10.1016/j.jcyt.2019.04.059.
- Fennemann FL, de Vries IJM, Figdor CG, Verdoes M. Attacking Tumors From All Sides: personalized Multiplex Vaccines to Tackle Intratumor Heterogeneity. Frontiers in Immunology. 2019;10:824. doi:10.3389/fimmu.2019.00824.
