ABSTRACT
Background
Prior research assessing the psychometric properties of the Global Psychotrauma Screen provided support for its internal consistency reliability, construct validity, convergent validity, and divergent validity in several international samples, but not specifically in a U.S. subsample.
Objective
The purpose of this study was to assess psychometric properties of the GPS in the U.S.
Method
This observational study included a convenience sample of individually recruited participants (N = 231) who completed an initial study with 126-item online questionnaire and a two-week follow-up study with GPS alone through the weblinks provided by the research team. Data analyzes included measuring internal consistency and test–retest reliability, exploratory and confirmatory factor analyzes (EFA and CFA), convergent and divergent validity, sensitivity, specificity, and severity of the GPS symptom items. Additional CFA was conducted with data (N = 947) from the GPS multinational research project, U.S. subsample.
Results
The results showed acceptable internal consistency and test–retest reliability, convergent validity, and divergent validity of the GPS. The construct validity results supported a three-factor structure of the GPS symptoms. The GPS domains showed acceptable sensitivity and specificity with the cut-off scores of 3 for PTSD and 5 for CPTSD domains; and the scores of 1 for the anxiety, depression, and insomnia domains respectively. The GPS risk factors predicted the GPS symptom severity.
Conclusions
This study provides new and additional evidence on the psychometric properties of the GPS which may help health care providers with the selection of an appropriate screening instrument for trauma-related transdiagnostic symptoms. The study limitations should be addressed in future research through the replication of EFA and CFA internationally with larger samples, and the inclusion of a reference standard for dissociation.
Introduction
Exposure to potentially traumatic events (PTEs) may lead to a wide range of symptoms that extend beyond a single disorder and are interconnected across disorders, thus, indicating their transdiagnostic nature (Frewen et al., Citation2021; Hyland et al., Citation2017; Olff et al., Citation2021; Williamson et al., Citation2021). Unlike a traditional discrete-disorder approach, the dimensional transdiagnostic paradigm provides novel insights into the biopsychosocial processes and mechanisms that connect symptoms of mental distress across disorders (Dalgleish et al., Citation2020). Based on the dimensional transdiagnostic paradigm and the network theory of psychopathology (Borsboom et al., Citation2021; Dalgleish et al., Citation2020), transdiagnostic symptoms can be defined as signs of mental distress in response to trauma that co-occur and reinforce each other and are functionally related to and predicted by underlying traumatic experiences.
Several trauma-related assessment instruments have been developed and validated in the U.S. based on the discrete-disorder approach (Cloitre et al., Citation2018; Foa et al., Citation2016; Grasso et al., Citation2019; Prins et al., Citation2015; Weathers et al., Citation2013a, Citation2013b, Citation2018); however, these are not transdiagnostic measures but scales aiming to assess symptoms of posttraumatic stress disorder (PTSD) based on the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5; APA, Citation2022).
To address the need for a free and easily accessible transdiagnostic screening tool for health care providers worldwide, an international group of experts with the Global Collaboration on Traumatic Stress developed the Global Psychotrauma Screen in English (GPS; GC-TS, Citation2023; Olff et al., Citation2020). The GPS is currently available in over 30 languages (Olff et al., Citation2023). Detailed procedures of the GPS development are described in Frewen et al. (Citation2021) and Olff et al. (Citation2020), and the GPS norm scores for the U.S. and other 26 countries are reported in the GPS User Guide (GC-TS, Citation2023). Unlike the trauma assessment instruments that are limited to PTSD, GPS additionally screens for the Disturbances in Self-Organization (DSO) as part of CPTSD, anxiety, depression, sleep problems, dissociation, self-harm, substance abuse, other physical, emotional, and social problems, as well as risk factors, and functioning (Olff et al., Citation2020).
Several studies have assessed the initial psychometric properties of the GPS. A pre-pandemic GPS validation study in Japan found good internal consistency and concurrent validity of the GPS in a clinical sample (Oe et al., Citation2020). Exploratory Factor Analysis (EFA) by Frewen et al. (Citation2021) showed a single-factor structure of the GPS symptoms. However, two other studies found a three-factor structure with such factors as core PTSD, negative affect, and dissociation using EFA and Confirmatory Factor Analysis (CFA) of the GPS data collected in Iran just before the COVID-19 pandemic (Salimi et al., Citation2023) and CFA of the GPS responses in Italy early in the pandemic (Rossi et al., Citation2021).
Furthermore, the GC-TS’s multinational research project on Cross-Cultural Responses to COVID-19 (GPS-CCC) and related studies confirmed the high reliability of GPS (Marengo et al., Citation2022; Olff et al., Citation2021; Williamson et al., Citation2021). The GPS symptoms’ network analysis showed a shared centrality of depression across networks and high interconnectedness among other symptoms (Williamson et al., Citation2021). These findings supported a transdiagnostic approach to the screening of posttraumatic outcomes using the GPS (Frewen et al., Citation2021; Williamson et al., Citation2021). While the GPS-CCC sample in Marengo et al. (Citation2022), Olff et al. (Citation2021), Williamson et al. (Citation2021), and the Amazon Mechanical Turk (MTurk) data in Frewen et al. (Citation2021) included U.S. participants, they did not examine psychometric properties of GPS specifically in the U.S. subsample.
The purpose of this observational study was to evaluate the internal consistency reliability, convergent validity, divergent validity, construct validity, and screening accuracy of the GPS in a convenience sample of participants residing in the U.S. This study aimed to test several hypotheses (see Supplementary Materials). We hypothesized the moderate-to-high levels of internal consistency and test–retest reliability of the GPS symptoms and domains. We expected moderate-to-high levels of sensitivity and specificity of the GPS symptoms and domains, as well as convergent validity and divergent validity. The higher levels of the GPS risk factors would predict higher levels of the GPS symptoms while considering the demographic and COVID-19 variables. Four levels of the GPS symptom severity: low, mild, moderate, and extreme, would predict the GPS functioning scores.
Methods
Study design and ethical considerations
Upon obtaining The Chicago School of Professional Psychology Institutional Review Board exempt determination and addenda approval (No. IRB-20-04-0043), the data collection took place between July 2020 and May 2022. Using a convenience sampling, Research Assistants (RAs) recruited participants from U.S. general population through their professional and social networks. There was no monetary or other compensation provided for participation in this study. The RAs personally screened each interested individual for eligibility to take part in the study using two inclusion criteria: 18 years old or older, currently reside in the U.S. The RAs provided weblinks to the anonymous questionnaires only to eligible individuals and instructed them not to share the weblinks with anyone. The individuals who were under 18 years of age and did not reside in the U.S. were excluded from the study.
The study included initial and follow-up parts. To match the initial study responses with the follow-up study, the participants were instructed to create their unique code and not to share it with anyone. Upon accessing the weblink, the participants were instructed to complete the online informed consent form and the questionnaire. The RAs provided each participant with a list of mental health care providers to contact in case of emotional discomfort due to the study participation.
A total of 231 participants who met the eligibility criteria and consented to take part in the study, completed the initial study questionnaire. The response rate to the initial study was 231 (73.8%) out of 313 eligible individuals and to the follow-up study – 74 (32%) out of 231 participants. While this sample size would allow conducting correlations, comparisons, and EFA, it was not enough for CFA (Kyriazos, Citation2018). Therefore, we added data from the GPS-CCC research, U.S. subsample (Olff et al., Citation2021).
The GPS-CCC study received an exempt determination from the Medical Ethical Review Committee of the Academic Medical Center of the University of Amsterdam (No. W19_481 # 19.556). Participation in the GPS-CCC study was voluntary through an online informed consent. No financial compensation was provided to participants and no personally identifying information was collected. The data from 947 participants who entered their responses through the GC-TS website between April 2020 and August 2022 were used for CFA in this study.
Measures
The initial questionnaire consisted of 13 research instruments with a total of 126 items. The questionnaire started with eight demographic items about age, gender, education, job, ethnic or racial group, marital status, child possession, state or territory of current residence in the U.S. Next, the COVID-19 survey questions developed by Olff et al. (Citation2021), were adapted and utilized in this study to account for the impact of the COVID-19 pandemic (see Supplementary Materials). The main instrument for validation was GPS which consists of three structured exposure items, 22 dichotomous items for trauma-related symptoms, risk factors, and one functioning item on a continuous scale from 1 to 10 (Olff et al., Citation2020; see Supplementary Materials). The reference standard measures were selected based on their theoretical relevance and validation in previous studies.
A reference standard for exposure to PTEs was the Life Events Checklist for DSM-5 (LEC-5) Criterion A (Weathers et al., Citation2013b). The LEC-5 was selected for this study because it was developed based on the theoretical background and epidemiological evidence suggesting that exposure to traumatic events is linked to the symptoms, and the type of events predicts the risk of developing specific symptoms (APA, Citation2022; Kessler et al., Citation2017). Similar relationship between the type of PTEs and the symptoms was supported in previous studies on GPS (Marengo et al., Citation2022; Oe et al., Citation2020; Olff et al., Citation2021). Thus, we expected a positive correlation between the LEC-5 PTEs and GPS Symptoms.
To assess the convergent validity of the GPS PTSD domain, we used the PTSD Checklist for DSM-5 (PCL-5; APA, Citation2022; Weathers et al., Citation2013a) because it has been validated in previous studies (Blevins et al., Citation2015; Bovin et al., Citation2016; Wortmann et al., Citation2016). We expected that the PCL-5 score would positively correlate with the GPS PTSD domain. Moreover, we used the International Trauma Questionnaire (ITQ; Cloitre et al., Citation2018) that assesses for two distinct diagnoses of PTSD and Complex PTSD (CPTSD) based on the International Classification of Diseases and Related Health Problems, 11th Edition (ICD-11; WHO, Citation2018). To our knowledge, ITQ is the only validated instrument that assesses CPTSD resulting from cumulative and prolonged forms of trauma (Cloitre et al., Citation2019, Citation2021). We measured the convergent validity of the GPS PTSD and CPTSD domains assuming that the ITQ PTSD and CPTSD scores would correlate with the respective GPS domains.
Generalized Anxiety Disorder (GAD) and Major Depressive Disorder (MDD) are highly comorbid with PTSD (Price et al., Citation2019). We used GAD-7 (Spitzer et al., Citation2006), and the Patient Health Questionnaire – 9 (PHQ-9; Kroenke et al., Citation2001) as the reference standards for anxiety and depression because these instruments have well-established psychometric properties. We expected that GAD-7 and PHQ-9 would positively correlate with the GPS Anxiety and Depression domains, indicating their convergent validity.
The comorbidity of PTSD with insomnia and other sleep disorders has been documented in previous research (Chinoy et al., Citation2022). We used the Bergen Insomnia Scale (BIS; Pallesen et al., Citation2008) as a reference standard for the GPS Sleep Problems domain because it has been validated in previous research (Pallesen et al., Citation2008). Similar to the recent studies with BIS (Torsvik et al., Citation2023), we used five out of six BIS items, whereas the symptom of ‘not feeling rested enough after waking up’ was removed because it is no longer required in the DSM-5 (APA, Citation2022). We expected that the participants who endorsed the GPS Sleep Problems item would have a higher BIS score, indicating convergent validity.
The co-occurrence of PTSD and Substance Use Disorder is well-known, and these two disorders reinforce each other resulting in increased severity, decreased functioning, and treatment drop-out (Hien et al., Citation2021). The reference measures for assessing convergent validity of the GPS Substance Use item were three items of the World Health Organization’s Alcohol, Smoking, and Substance Involvement Screening Test (WHO ASSIST), which has a well-established validity (Humeniuk et al., Citation2010; López-Lazcano et al., Citation2022). We expected that the participants who endorsed the GPS Substance Use item would have higher scores on the ASSIST (Humeniuk et al., Citation2010).
Resilience serves as a protective factor against traumatic stress (Olff et al., Citation2021; van der Meer et al., Citation2018). The reference standard for resilience was the Resilience Evaluation Scale, which is a validated measure (RES; van der Meer et al., Citation2018). Convergent validity of the GPS Resilience item would be suggested if the participants who endorsed the item, also had a higher RES score. Additionally, we used RES to assess divergent validity of the GPS Symptoms and domains, assuming their negative correlation with the RES.
The impact of traumatic stress on daily life functioning is well-documented (Frewen et al., Citation2021; Olff et al., Citation2021; Weathers et al., Citation2018). To assess the convergent validity of the GPS Functioning item, we used two items from the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5; Weathers et al., Citation2018) to measure functional impairment in the work, school, and social settings; and one item from the World Health Organization’s Quality of Life scale (WHOQOL-BREF; Harper et al., Citation1998) to measure global functioning. Additionally, we used WHOQOL-BREF to assess divergent validity of the GPS Symptoms and domains expecting a negative correlation between them.
Statistical analyzes
The statistical analyzes were conducted in SPSS.26 (IBM, Citation2019) and STATA.17 (StataCorp, Citation2021). The internal consistency of the GPS was measured using the Cronbach’s Alpha (>2 items) and Spearman-Brown’s (≤2 items) coefficients. The missing data analysis was performed using the Little’s Missing Completely At Random (MCAR) test which indicated that the data were missing at random, χ2(17,289) = 17,000.08, p = 0.94. Missing values were excluded automatically for each statistical test. The assumptions of normativity and homoscedasticity were checked with the Shapiro–Wilk’s and Levene’s tests. Spearman’s correlation coefficient was used to examine convergent and divergent validity. Independent t-tests were used for group comparisons.
The EFA and CFA were performed in STATA.17 (StataCorp, Citation2021). The assumption of homogeneity on key variables (Kyriazos, Citation2018) was checked by randomly splitting the sample into two halves and comparing them on key variables. The data suitability for factor analysis was checked using the Kaiser–Meyer–Olkin (KMO) test for sampling adequacy and the Bartlett’s test of sphericity for the appropriateness of EFA for the data. Tetrachoric EFA was conducted because of the GPS’s dichotomous item structure. The principal axis factoring with the oblique Promax rotation was applied to identify latent constructs. CFA was conducted with a maximum likelihood estimation. The overall Goodness of Fit (GoF) was evaluated using the Chi-square test, while the equation level GoF measured Root-Mean-Square Error of Approximation (RMSEA), Comparative Fit Index (CFI), Tucker–Lewis Index (TLI), and Standardized Root-Mean-Square Residual (SRMR).
The sensitivity and specificity analyzes were conducted to assess the screening accuracy of the GPS for detecting trauma-related disorders. We used PCL-5 with a cut-off score of 33 (Weathers et al., Citation2013a) as a reference standard for the DSM-5 PTSD and the GPS PTSD domain score as a classification variable. We used the ITQ diagnostic scoring cut-offs for the ICD-11 PTSD and CPTSD diagnoses (Cloitre et al., Citation2018) for the GPS PTSD, DSO, and CPTSD domains. The reference standards for screening of the GAD and a depressive episode were GAD-7 for the GPS Anxiety domain, and PHQ-9 for the GPS Depression domain with the cut-off scores of 10 (Kroenke et al., Citation2001; Spitzer et al., Citation2006). We used BIS with a cut-off score of 6 (Pallesen et al., Citation2008) as a reference standard for screening of insomnia using the GPS Sleep Problems domain. For the GPS Substance Use domain, the ASSIST risk scores (lower, moderate, or high risk) on item 2 (substance use) and item 3 (substance craving; Humeniuk et al., Citation2010) were used to differentiate between those who were at any level of risk for substance abuse and those who were not at risk.
The Receiver Operating Characteristic (ROC) analysis was performed in STATA.17 (StataCorp, Citation2021) to determine the Area Under the Curve (AUC), sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the GPS domain scores. The Likelihood Ratio (LR) analysis determined the ratio of the probability that a positive or negative result will occur in persons with the disorder (LR+) to the probability that the same result will occur in persons without the disorder (LR-).
The GPS risk factors were assessed using a hierarchical multiple regression. The first model included three blocks: seven demographic variables; the GPS risk factors; and the COVID-19 distress. The second three-block model examined the stressors that contributed to the COVID-19 distress: COVID-19 exposure; the exposure location and occupation; and 18 stressors related to COVID-19.
The severity analysis was conducted by creating the GPS Symptoms’ severity groups based on the percentile cut-off points as follows: low (≤30th percentile), mild (31–74th percentile), moderate (75–94th percentile), and severe (≥95th percentile; Fissette et al., Citation2014; Primasari et al., Citation2021). Lower scores on the GPS functioning were expected in more severe categories of trauma-related symptoms. Because the assumptions for a parametric ANCOVA were not met, the Quade’s rank ANCOVA (Quade, Citation1967) was used to compare the GPS Symptoms severity groups on the GPS Functioning score with the demographic variables as covariates. The post hoc multiple comparisons were performed using the Scheffé test for unequal groups.
Results
Sample characteristics
A sample of 231 participants from 31 states and District of Columbia completed the initial questionnaire. Detailed demographic information is reported in . Responses to the GPS exposure items showed that the participants experienced more of a single than multiple traumatic events. Over a half of the participants reported the time of the event longer than a year ago. The most frequently reported events were physical violence, emotional abuse, and a sudden death of a loved one. Over a half of the participants experienced COVID-19 along with PTEs, while fewer participants reported either COVID-19 or PTEs (see ).
Table 1. Demographic characteristics of participants (N = 231).
Table 2. Exposure characteristics (N = 231).
GPS symptom and risk factor endorsement
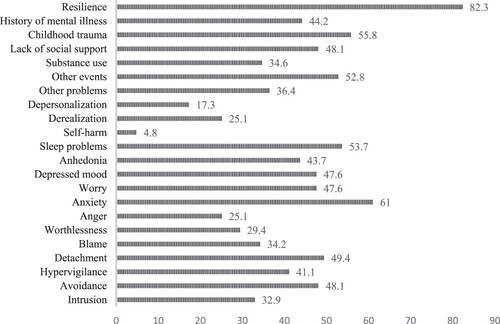
The most frequently reported GPS symptom was anxiety, while the least frequent was self-harm. The most frequent GPS risk factor was childhood trauma. The GPS resilience score was high (see ). The GPS Symptoms sum scores were higher in participants who endorsed the GPS Risk Factors (see Table S2). There was a weak inverse correlation of age with the GPS Symptoms (r = −0.230; p < 0.001) and risk factor scores (r = −0.139; p = 0.043), indicating higher levels of symptoms and risk factors in younger participants. There were no statistically significant differences between males and females on the GPS item-by-item comparisons, except for anxiety (item 8) which was more frequently endorsed by females than males (see Table S3), and on the GPS Symptoms and Risk Factors sum scores (see Table S4). Similarly, there were no statistically significant differences in the GPS Symptoms and Risk Factors scores across other demographic categories (see Table S5).
Reliability of GPS
The results presented in show acceptable internal consistency and test–retest reliability of the GPS symptoms, risk factors, and domains. The Intra-Class Correlation Coefficients (ICC) showed a high level of agreement of the GPS Symptoms and domain sum scores in the initial and follow-up studies.
Table 3. Internal consistency and test–retest reliability of GPS (N = 231).
Construct validity
Exploratory factor analysis
The EFA was conducted with 214 participants after 17 (7.3%) cases with missing GPS values were excluded listwise. The assumption of homogeneity between the randomly split two halves of the sample on key variables was met based on the t-test or χ2 results, thus allowing to proceed with EFA. The KMO of 0.90 indicated high sampling adequacy. The Bartlett’s test of sphericity confirmed the appropriateness of EFA based on large correlations between items, χ2(136) = 1224.2, p < 0.001.
The initial analysis showed that Factors 1, 2, and 3 had Eigenvalues >1, which explained 76% of the total variance (see ), and the uniqueness values were <0.6 on all but the substance use item (see ). In the oblique Promax rotation of the three-factor model, Factor 1 was represented by the PTSD symptoms of intrusion, avoidance, hyperarousal, numbing, and guilt or blame, along with self-harm and substance abuse. Factor 2 included symptoms of anxiety, sleep problems, dissociation, and other problems. Factor 3 was comprised of DSO and depression symptoms. Derealization had marginally contributed to Factor 2, but all other items in this model were above the threshold of 0.4 (Pituch & Stevens, Citation2016) and dependably represented their respective factors. The Cronbach’s Alpha results for the rotated three factor-model showed acceptable internal consistency (see ).
Table 4. The EFA total variance (n = 214).
Table 5. The EFA oblique Promax rotated factor loadings and unique variances (n = 214).
Confirmatory factor analysis
The three-factor model was tested using the CFA maximum likelihood estimation. Because the sample size in this study (n1 = 214) was smaller than projected for CFA, the three-factor model was additionally tested on the GPS-CCC web sample (n2 = 947). The same three factors were used in both samples as follows: Factor 1 – core PTSD, self-harm, and substance abuse; Factor 2 – anxiety, sleep problems, dissociation, and other physical, emotional, and social problems; and Factor 3 – DSO and depression. Covariances were measured between Factors 1 and 2; 2 and 3; and 1 and 3. All the factor loadings were statistically significant in both samples indicating that each factor’s variables contributed to their respective factors. The results of this initial CFA model showed that the RMSEA and SRMR did not reach the acceptable thresholds in this study sample, and none of the CCC-GPS sample fit indices were acceptable (see Table S6). The postestimation modification indices in this study sample displayed the largest changes observed in the omitted covariances between the depression symptoms, followed by the symptoms of guilt or blame and worthlessness; worry and substance use; depersonalization and other problems; and numbing and anhedonia. In the CCC-GPS sample, the postestimation modification indices displayed the largest changes observed in the omitted covariances between the dissociative symptoms, followed by the symptoms of intrusion and hyperarousal; avoidance and anhedonia; and the anxiety symptoms. The inspection of the standardized covariance residuals for these items showed the values >1.96 in the substantial areas of model misspecification (Pituch & Stevens, Citation2016). These omitted covariances were added in each sample’s model respectively as they were theoretically related. The final CFA model results indicated a good fit to the data in both samples (see ).
Table 6. The CFA three-factor final model fit indices.
Convergent validity of the GPS
The factor scores for the GPS observed variables were calculated and the correlations of the GPS factors with the reference measures were assessed for convergent validity in this study sample. All three factors had acceptable correlations with the GPS Symptoms and Risk Factors scores (see ). A further analysis of the convergent validity of the GPS symptoms, risk factors, and domain scores as the predictor variables, and the reference measures as the criterion variables showed positive correlations between them indicating acceptable convergent validity (see ). The convergent validity of the GPS single-item domains of Sleep Problems, Self-harm, Substance Use, and Resilience was evident in the higher scores on the reference measures in the participants who endorsed the GPS items (see Table S7). The GPS Functioning item showed acceptable convergent validity in relation to the PHQ-9 and CAPS-5 functioning items, but the correlations with the ITQ functioning items were below the hypothesized 0.50 (see Table S8).
Table 7. Convergent validity and divergent validity of the GPS factor scores (n = 214).
Table 8. Convergent validity and divergent validity of the GPS domains (>2 items; N = 231).
Divergent validity of the GPS
The divergent validity of the GPS Symptoms and domain scores was evident in the negative correlations with the RES and WHOQOL-BREF scores. The divergent validity of the GPS single-item domains of Substance Use, Other Problems, and Self-harm was evident in the lower scores on the RES and WHOQOL-BREF in the participants who endorsed the GPS items; however, the scores did not differ on the GPS Sleep Problems domain (see Table S7).
Sensitivity and specificity of the GPS
The results of ROC showed acceptable AOC values for most GPS domains, except for Substance Use (see detailed results in , S9–S11, and Figures S1–S11). For the GPS PTSD domain, a count of 3 was the maximum needed to yield minimally 80% sensitivity (91.9% sensitivity; 73.8% specificity); a count of 4 was the maximum needed to yield minimally 70% specificity (86.6% specificity; 75.8% sensitivity) to screen for the DSM-5 PTSD, based on PCL-5. Similarly, a count of 3 was the maximum needed to yield minimally 80% sensitivity (92.5% sensitivity; 65.7% specificity) and a count of 4 was the maximum needed to yield minimally 70% specificity (77.3% specificity; 70% sensitivity) for the ICD-11 PTSD, based on ITQ. The GPS DSO domain needed a count of 1 to achieve minimally 70% sensitivity (85.7% sensitivity; 66.3% specificity), and a count of 2 for minimally 65% specificity (88.7% specificity; 51.4% sensitivity) for the ICD-11 DSO cluster, based on ITQ. The GPS CPTSD domain needed a count of 4 to yield minimally 70% sensitivity (95.5% sensitivity; 66% specificity), and a count of 6 for minimally 65% specificity (86.4% specificity; 63.6% sensitivity) for the ICD-11 CPTSD, based on ITQ.
Table 9. Clinical validity of the GPS Symptoms and domain sum scores (n = 214).
The GPS Anxiety domain score of 1 yielded minimally 65% sensitivity (96.1% sensitivity; 41.4% specificity) and a count of 2 reached minimally 70% specificity (80.9% specificity; 51% sensitivity). The GPS Depression domain score of 1 had minimally 65% sensitivity (87.5% sensitivity; 50.3% specificity), and a count of 2 achieved minimally 70% specificity (73.1% specificity; 67.2% sensitivity). The GPS Sleep Problems item yielded minimally 60% sensitivity (76.4%) and 70% specificity (75%). The GPS Substance Use item achieved minimally 60% sensitivity when differentiating between those who are at any level of risk for substance abuse and those who are not at risk but did not reach 55% specificity: tobacco 85% sensitivity and 48.9% specificity; alcohol 84.6% sensitivity and 46.5% specificity; and other drugs 77% sensitivity and 52% specificity.
Analysis of the GPS risk factors
The results of the first hierarchical multiple regression model showed that the GPS Risk Factors explained most of the variance in the GPS Symptoms. The demographic and COVID-19 related variables only minimally influenced the GPS Symptoms’ variance. Out of seven demographic variables, only age could explain the variance in the symptoms, that is, the younger age was associated with more GPS Symptoms; however, this was a small change. The COVID-19 related distress also produced only a small change. Overall, the first model explained 48% of variance in the GPS Symptoms (see Table S12). The results of the second model showed that the small change in the GPS Symptoms due to the COVID-19 related distress was produced by three out of 18 stressors related to COVID-19: a death of family member(s) or relative(s) affected by COVID-19, an income or job loss due to the pandemic, and an extra psychosocial burden of taking care of loved ones. This model explained 47% of the variance in the COVID-19 related distress (see Table S13).
Severity analysis of the GPS symptoms
The GPS Symptoms mean score was 6.87, 95% CI [6.23, 7.52]. The distribution of the GPS Symptoms’ severity levels showed that most participants had low (64; 31.5%) and mild (95; 46.8%) levels of the GPS Symptoms severity, while 39 (19.2%) participants had a moderate level, and 5 (2.5%) had the highest level of severity. The results of severity analysis showed differences in the GPS functioning scores compared by the GPS Symptoms’ severity levels, F(3, 199) = 11.39; p < 0.001, η2 = 0.147. Pairwise comparisons between the four GPS severity groups showed that the differences in the GPS functioning were between the low and moderate groups (p < 0.001), and the mild and moderate groups (p < 0.001), but not between the low and mild groups. The high severity group comprising of five participants showed no statistically significant differences in functioning from other severity groups.
Discussion
The results of this study supported our hypotheses in that the GPS total and symptom scores had high internal consistency and the GPS domains showed moderate internal consistency, thus, supporting previous reports (Frewen et al., Citation2021; Oe et al., Citation2020; Olff et al., Citation2021; Rossi et al., Citation2021; Salimi et al., Citation2023). This was the first study that examined the GPS test–retest reliability and found it satisfactory. The convergent validity and divergent validity results were acceptable for the GPS Symptoms and all but the Sleep Problems domain scores. The finding that the sleep problems were irrespective of resilience and quality of life could be attributed to the disrupted sleep schedules during the COVID-19 pandemic, work-life imbalance, or some other unknown factors.
Consistent with Frewen et al. (Citation2021) and Salimi et al. (Citation2023), this study established a screening accuracy of the GPS for traumatic stress symptoms with a cut-off score of 8 when prioritizing sensitivity and a score of 9 for optimal sensitivity and specificity. Additionally, this was the first study to establish a screening accuracy of the GPS domains for possible PTSD with the cut-off score of 3, as recommended by Prins et al. (Citation2015), possible CPTSD with the cut-off score of 5, and other GPS domains such as anxiety, depression, and insomnia. However, the GPS Substance Use domain did not reach acceptable AOC and specificity, probably due to the participant bias resulting in underreported illicit drug use.
In terms of the GPS construct validity, our results supported the hypothesized three-factor structure, however, the symptom representation within the factors was different than the hypothesized and previously reported model consisting of core PTSD, negative affect, and dissociation factors (Rossi et al., Citation2021; Salimi et al., Citation2023). In our study, the first factor consisted of the PTSD symptoms as expected but also included self-harm and substance abuse, highlighting a self-destructive potential of PTSD. In fact, all the participants who endorsed the GPS Self-Harm and 62.5% who reported the GPS Substance Use were positive for the GPS PTSD. This finding is consistent with the ICD-11 PTSD which describes suicidal ideation and behavior, and substance abuse as additional clinical features of PTSD (WHO, Citation2018).
The second factor combined dissociative symptoms with anxiety, insomnia, and other problems, partially supporting our hypothesis and consistent with ICD-11 (WHO, Citation2018) but unlike Rossi et al. (Citation2021) and Salimi et al. (Citation2023) where the dissociation factor was in line with DSM-5-TR (APA, Citation2022). One explanation could be that depersonalization co-occurred in over a half of the participants with generalized anxiety, and both depersonalization and derealization co-occurred in over 80% of the participants with insomnia, suggesting that dissociation, as a state of hypoarousal, could be a defensive response (Nicholson et al., Citation2017) to anxiety and insomnia both of which are associated with hyperarousal.
The third factor supported the hypothesized negative affect and consisted of the DSO and depressive symptoms. The ICD-11 defines the DSO symptoms as essential while including depression among additional features of CPTSD (WHO, Citation2018). The DSO symptoms co-occurred in a half of the participants with a depressive episode, supporting previous research (Cloitre et al., Citation2019; Hyland et al., Citation2017) and ICD-11 which suggests the comorbidity of CPTSD with a depressive episode (WHO, Citation2018). Overall, the GPS symptom representation in the three-factor model of this study supported the transdiagnostic approach to screening of trauma- and stress-related disorders.
Our hypothesis about the differences in functioning based on the severity levels of the GPS symptoms was only partially supported. This could be due to the small size of the high severity group, as the severity levels of the GPS Symptoms in most participants were low or mild, thus, having only a small effect on the participants’ self-reported functioning. Another explanation could be a high frequency of resilience in this study sample.
The GPS symptoms’ variance was influenced mostly by the GPS risk factors, while the demographic and COVID-19 variables contributed minimally, which was dissimilar to Rossi et al. (Citation2021) who found a stronger association between the two. This could be due to the different time span for data collection as Rossi et al. (Citation2021) collected data in the beginning of the pandemic within a short period of time (end of March–early April, 2020); while our data collection took almost two years throughout the pandemic (July 2020–May, 2022) and the participants may have adjusted to it, as most of them reported moderate-to-low levels of COVID-19 related distress.
There are several limitations that should be considered when interpreting the findings of this study. The convenience sampling through social networks limits generalizability of the findings. Similar to previous studies on trauma, the sample was predominately female. The projected sample size for CFA was not achieved due to the difficulties with recruitment, but we balanced this limitation by conducting CFA on an additional sample. The use of modification indices to identify and add the omitted covariances in CFA, although theoretically justified, would need a replication in future research. Furthermore, this study did not include a reference standard for dissociation because the study questionnaire, which was already too long, would become overburdening for participants. Future studies on the psychometric properties of GPS should include a reference measure on dissociation to obtain more evidence for the GPS dissociation domain.
In summary, this study provides new and additional evidence on the psychometric properties of the GPS as a valid and reliable tool for rapid screening of a range of transdiagnostic symptoms that are common after PTEs. It adds new findings to the prior international studies on psychometric properties of the GPS, specifically for the U.S., thus, giving health care providers, researchers, and policymakers an opportunity to make informed decisions on the use of GPS when screening for symptoms after trauma.
Ethics compliance
Institutional Review Board Statement: The study was conducted in accordance with the Declaration of Helsinki and received an exempt determination and addenda approval by The Chicago School of Professional Psychology Institutional Review Board (No. IRB-20-04-0043). See details under Methods.
The GPS-CCC study received an exempt determination from the Medical Ethical Review Committee of the Academic Medical Center of the University of Amsterdam (No. W19_481 # 19.556). See details under Methods.
Informed consent
Informed consent was obtained from all participants who took part in the initial and follow-up studies using the online informed consent form.
Informed consent was obtained from all participants who took part in the GPS-CCC study through an online informed consent.
Supplemental Material
Download MS Word (128.2 KB)Acknowledgments
We thank Candace Ford, Adrienne Konstantin, and Amber Fitzwater for their recruitment efforts.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data from this study cannot be made publicly available due to the IRB restrictions. Any inquiries about the data can be made to the corresponding author at [email protected].
References
- American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders: DSM-5-TR (5th ed., text revision.). American Psychiatric Association Publishing. https://doi.org/10.1176/appi.books.9780890425787
- Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. https://doi.org/10.1002/jts.22059
- Borsboom, D., Deserno, M. K., Rhemtulla, M., Epskamp, S., Fried, E. I., McNally, R. J., Robinaugh, D. J., Perugini, M., Dalege, J., Costantini, G., Isvoranu, A. M., Wysocki, A. C., van Borkulo, C. D., van Bork, R., & Waldorp, L. J. (2021). Network analysis of multivariate data in psychological science. Nature: Reviews, Methods, Primers, 1(1), 58. https://doi.org/10.1038/s43586-021-00055-w
- Bovin, M. J., Marx, B. P., Weathers, F. W., Gallagher, M. W., Rodriguez, P., Schnurr, P. P., & Keane, T. M. (2016). Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders-fifth edition (PCL5) in veterans. Psychological Assessment, 28(11), 1379–1391. https://doi.org/10.1037/pas0000254
- Chinoy, E. D., Carey, F. R., Kolaja, C. A., Jacobson, I. G., Cooper, A. D., & Markwald, R. R. (2022). The bi-directional relationship between post-traumatic stress disorder and obstructive sleep apnea and/or insomnia in a large U.S. military cohort. Sleep Health, 8(6), 606–614. https://doi.org/10.1016/j.sleh.2022.07.005
- Cloitre, M., Hyland, P., Bisson, J. I., Brewin, C. R., Roberts, N. P., Karatzias, T., & Shevlin, M. (2019). ICD-11 posttraumatic stress disorder and complex posttraumatic stress disorder in the United States: A population-based study. Journal of Traumatic Stress, 32(6), 833–842. https://doi.org/10.1002/jts.22454
- Cloitre, M., Hyland, P., Prins, A., & Shevlin, M. (2021). The International Trauma Questionnaire (ITQ) measures reliable and clinically significant treatment-related change in PTSD and complex PTSD. European Journal of Psychotraumatology, 12(1), 1930961. https://doi.org/10.1080/20008198.2021.1930961
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., Karatzias, T., & Hyland, P. (2018). The international trauma questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. https://doi.org/10.1111/acps.12956
- Dalgleish, T., Black, M., Johnston, D., & Bevan, A. (2020). Transdiagnostic approaches to mental health problems: Current status and future directions. Journal of Consulting and Clinical Psychology, 88(3), 179–195. https://doi.org/10.1037/ccp0000482
- Fissette, C. L., Snyder, D. K., Balderrama-Durbin, C., Balsis, S., Cigrang, J., Talcott, G. W., Tatum, J., Baker, M., Cassidy, D., Sonnek, S., Heyman, R. E., & Smith Slep, A. M. (2014). Assessing posttraumatic stress in military service members: Improving efficiency and accuracy. Psychological Assessment, 26(1), 1–7. https://doi.org/10.1037/a0034315
- Foa, E. B., McLean, C. P., Zang, Y., Zhong, J., Powers, M. B., Kauffman, B. Y., Rauch, S., Porter, K., & Knowles, K. (2016). Psychometric properties of the posttraumatic diagnostic scale for DSM-5 (PDS-5). Psychological Assessment, 28(10), 1166–1171. https://doi.org/10.1037/pas0000258
- Frewen, P., McPhail, I., Schnyder, U., Oe, M., & Olff, M. (2021). Global Psychotrauma Screen (GPS): psychometric properties in two internet-based studies. European Journal of Psychotraumatology, 12(1), 1–13. https://doi.org/10.1080/20008198.2021.1881725
- Global Collaboration on Traumatic Stress. (2023). Global Psychotrauma Screen (GPS). https://www.global-psychotrauma.net/gps
- Grasso, D. J., Ford, J. D., & Greene, C. A. (2019). Preliminary psychometrics of the Structured Trauma-Related Experiences and Symptoms Screener for Adults (STRESS-A) in an urban prenatal healthcare clinic. Psychological Trauma: Theory, Research, Practice, and Policy, 11(8), 927–935. https://doi.org/10.1037/tra0000476
- Harper, A., Power, M., Orley, J., Herrman, H., Schofield, H., Murphy, B., Metelko, Z., Szabo, S., Pibernik-Okanovic, M., Quemada, N., Caria, A., Rajkumar, S., Kumar, S., Saxena, S., Chandiramani, K., Amir, M., Bar-On, D., Tazaki, M., Noji, A., … Sartorius, N. (1998). Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological Medicine, 28(3), 551–558. https://doi.org/10.1017/S0033291798006667
- Hien, D. A., López-Castro, T., Fitzpatrick, S., Ruglass, L. M., Fertuck, E. A., & Melara, R. (2021). A unifying translational framework to advance treatment research for comorbid PTSD and substance use disorders. Neuroscience and Biobehavioral Reviews, 127, 779–794. https://doi.org/10.1016/j.neubiorev.2021.05.022
- Humeniuk, R. E., Henry-Edwards, S., Ali, R. L., Poznyak, V., & Monteiro, M. (2010). The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): manual for use in primary care. World Health Organization. https://www.who.int/publications-detail/the-alcohol-smoking-and-substance-involvement-screening-test-(assist)
- Hyland, P., Shevlin, M., Brewin, C. R., Cloitre, M., Downes, A. J., Jumbe, S., & Roberts, N. P. (2017). Factorial and discriminant validity of ICD-11 PTSD and CPTSD using the new international trauma questionnaire. Acta Psychiatrica Scandinavica, 136(3), 231–338. https://doi.org/10.1111/acps.12771
- IBM Corp. (Released 2019). Ibm SPSS statistics for windows, version 26.0.
- Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E. J., Cardoso, G., Degenhardt, L., de Girolamo, G., Dinolova, R. V., Ferry, F., Florescu, S., Gureje, O., Haro, J. M., Huang, Y., Karam, E. G., Kawakami, N., Lee, S., Lepine, J. P., Levinson, D., … Koenen, K. C. (2017). Trauma and PTSD in the WHO world mental health surveys. European Journal of Psychotraumatology, 8(sup5), 1353383. https://doi.org/10.1080/20008198.2017.1353383
- Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
- Kyriazos, T. (2018). Applied psychometrics: Sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychology (Savannah, Ga ), 9(08|8), 2207–2230. https://doi.org/10.4236/psych.2018.98126
- López-Lazcano, A. I., López-Pelayo, H., Balcells-Oliveró, M., Segura, L., & Gual Solé, A. (2022). Validation of the alcohol smoking and substance involvement screening test (ASSIST) in acute psychiatric inpatients. Addictions, 34(4), 259–272. https://doi.org/10.20882/adicciones.1496
- Marengo, D., Hoeboer, C. M., Veldkamp, B. P., GPS-txt consortium, & Olff, M. (2022). Text mining to improve screening for trauma-related symptoms in a global sample. Psychiatry Research, 316, 114753. https://doi.org/10.1016/j.psychres.2022.114753
- Nicholson, A. A., Friston, K. J., Zeidman, P., Harricharan, S., McKinnon, M. C., Densmore, M., Neufeld, R. W. J., Théberge, J., Corrigan, F., Jetly, R., Spiegel, D., & Lanius, R. A. (2017). Dynamic causal modeling in PTSD and its dissociative subtype: Bottom-up versus top-down processing within fear and emotion regulation circuitry. Human Brain Mapping, 38(11), 5551–5561. https://doi.org/10.1002/hbm.23748
- Oe, M., Kobayashi, Y., Ishida, T., Chiba, H., Matsuoka, M., Kakuma, T., … Olff, M. (2020). Screening for psychotrauma related symptoms: Japanese translation and pilot testing of the Global Psychotrauma Screen. European Journal of Psychotraumatology, 11(1), 1–11. https://doi.org/10.1080/20008198.2020.1810893
- Olff, M., Bakker, A., Frewen, P., Aakvaag, H., Ajdukovic, D., Brewer, D., Elmore Borbon, D. L., Cloitre, M., Hyland, P., Kassam-Adams, N., & Knefel, M. (2020). Screening for consequences of trauma – An update on the global collaboration on traumatic stress. European Journal of Psychotraumatology, 11(1), 1752504. https://doi.org/10.1080/20008198.2020.1752504
- Olff, M., Bakker, A., & Global Collaboration on Traumatic Stress. (2023). Global Psychotrauma Screen (GPS). https://www.global-psychotrauma.net/gps
- Olff, M., Primasari, I., Qing, Y., Coimbra, B. M., Hovnanyan, A., Grace, E., Williamson, R., Hoeboer, C. M. & the GPS-CCC Consortium. (2021). Mental health responses to COVID-19 around the world. European Journal of Psychotraumatology, 12(1), 1929754. https://doi.org/10.1080/20008198.2021.1929754
- Pallesen, S., Bjorvatn, B., Nordhus, I., Sivertsen, B., Hjørnevik, M., & Morin, C. (2008). A new scale for measuring insomnia: The Bergen Insomnia Scale. Perceptual and Motor Skills, 107(3), 691–706. https://doi.org/10.2466/pms.107.3.691-706
- Pituch, K., & Stevens, J. (2016). Applied multivariate statistics for the social sciences. Routledge Taylor and Francis Group.
- Price, M., Legrand, A. C., Brier, Z. M. F., & Hébert-Dufresne, L. (2019). The symptoms at the center: Examining the comorbidity of posttraumatic stress disorder, generalized anxiety disorder, and depression with network analysis. Journal of Psychiatric Research, 109, 52–58. https://doi.org/10.1016/j.jpsychires.2018.11.016
- Primasari, I., Hoeboer, C., Bakker, A., & Olff, M. (2021). Validation study of Global Psychotrauma Screen (GPS) for assessing trauma related symptoms in Indonesian undergraduate students [Preregistration Report]. https://osf.io/na3zf/
- Prins, A., Bovin, M. J., Kimerling, R., Kaloupek, D. G., Marx, B. P., Pless Kaiser, A., & Schnurr, P. P. (2015). Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) [Measurement instrument]. https://www.ptsd.va.gov/professional/assessment/screens/pc-ptsd.asp
- Quade, D. (1967). Rank analysis of covariance. Journal of the American Statistical Association, 62(320), 1187–1200. https://doi.org/10.1080/01621459.1967.10500925
- Rossi, R., Socci, V., Talevi, D., Cinzia Niolu, C., Pacitti, F., Di Marco, A., … Olff, M. (2021). Trauma-spectrum symptoms among the Italian general population in the time of the COVID-19 outbreak. European Journal of Psychotraumatology, 12(1), 1–12. https://doi.org/10.1080/20008198.2020.1855888
- Salimi, Y., Hoeboer, C., Motevalli Haghi, S. A., Williamson, R. E., Rahimi, M. D., Rajabi-Gilan, N., Almasi, A., & Olff, M. (2023). Trauma and its consequences in Iran: Cross-cultural adaption and validation of the Global Psychotrauma Screen in a representative sample. BMC Psychiatry, 23(1), 65. https://doi.org/10.1186/s12888-023-04564-8
- Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
- StataCorp. (2021). Stata statistical software: Release 17.
- Torsvik, N., Bjorvatn, B., Eliassen, K. E., & Forthun, I. (2023). Prevalence of insomnia and hypnotic use in Norwegian patients visiting their general practitioner. Family Practice, 40(2), 352–359. https://doi.org/10.1093/fampra/cmac103
- United States Census Bureau. (2020). American community survey demographic and housing estimates. https://data.census.gov/cedsci/table?q = United%20States&tid = ACSDP1Y2019.DP05&hidePreview = false
- van der Meer, C. A. I., te Brake, H., van der Aa, N., Dashtgard, P., Bakker, A., & Olff, M. (2018). Assessing psychological resilience: Development and psychometric properties of the English and Dutch version of the Resilience Evaluation Scale (RES). Frontiers in Psychiatry, 9(169), 1–11. https://doi.org/10.3389/fpsyt.2018.00169
- Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013b). The life events checklist for DSM-5 (LEC-5). National Center for PTSD. https://doi.org/10.1177/1073191104269954
- Weathers, F. W., Bovin, M. J., Lee, D. J., Sloan, D. M., Schnurr, P. P., Kaloupek, D. G., Keane, T. M., & Marx, B. P. (2018). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30(3), 383–395. https://doi.org/10.1037/pas0000486
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013a). The PTSD checklist for DSM-5 (PCL-5). National Center for PTSD. https://doi.org/10.1037/t02622-000
- Williamson, R., Hoeboer, C. M., Primasari, I., Qing, Y., Coimbra, B. M., Hovnanyan, A., Grace, E., & Olff, M. (2021). Symptom networks of COVID-19-related versus other potentially traumatic events in a global sample. Journal of Anxiety Disorders, 84, 102476. https://doi.org/10.1016/j.janxdis.2021.102476
- World Health Organization. (2018). International classification of diseases for mortality and morbidity statistics (11th Revision). https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f334423054
- Wortmann, J. H., Jordan, A. H., Weathers, F. W., Resick, P. A., Dondanville, K. A., Hall-Clark, B., Foa, E. B., YoungMcCaughan, S., Yarvis, J. S., Hembree, E. A., Mintz, J., Peterson, A., & Litz, B. T. (2016). Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment, 28(11), 1392–1403. https://doi.org/10.1037/pas0000260