Abstract
Aim
Although many patients with anxiety and depression suffer from muscular pain and bodily dysfunctions, body is largely ignored in treatment. The aim of this study was to investigate the effectiveness of Learning Oriented Physiotherapy (LOP), based on recent knowledge about overlapping brain networks and the need of awakening body awareness in order to synchronise body and mind.
Methods
Patients with moderate anxiety and/or depression referred to three outpatient psychiatric clinics in Norway during October 2014 to January 2016 were invited to participate. Of eligible patients, 42 were randomised to LOP and 39 to standard psychiatric treatment (controls). Self-reports of anxiety and depression (HADS), health-related quality of life (EQ-5D-5L) and global health (EQ-VAS) were recorded every 6 months from baseline (T1) to 18 months after (T4). Mixed linear model (MLM) analysis was used to estimate overall differences between groups.
Results
After 1 year of follow-up, LOP participants reported higher quality of life and perceived global health than controls. At the end of the trial, there were no mean differences in health outcomes between groups, but LOP participants showed an overall faster rate of recovery than controls.
Conclusions
LOP may be as effective as conventional therapies for patients with moderate anxiety and depression.
Background
Musculoskeletal and mental health disorders are two conditions resulting in some of the highest burdens in terms of disability and health [Citation1–3]. These disorders are commonly associated with reduced quality of life, with negative consequences for third parts like partners and families [Citation4]. Globally, it has been estimated that one in three or four persons will be affected by anxiety, depression or another common mental disorder in the course of their life [Citation5]. The comorbidity between anxiety and depression is high [Citation6,Citation7], as well as it is between mental disorders and somatic symptoms [Citation8,Citation9]. Today, the most common forms of treatment for (moderate) anxiety and depression are different forms of psychotherapy in combination with pharmacological treatment. However, it is estimated that 40% of patients do not seek treatment [Citation7]. Although patients with anxiety and depression largely experience improvement following psychiatric treatment, relapses are frequent (25–60%) and long term effects remain largely unclear [Citation10,Citation11].
Despite that physical activity and lifestyle interventions commonly are recommended for patients with mental disorders [Citation12,Citation13], bodily dysfunctions are largely ignored, not only in the diagnostic and treatment recommendations [Citation14], but also in research. In fact, many patients report symptoms such as tightness in the chest, pain, stiffness, dizziness, numbness, palpitations, breathlessness, exhaustion, sleep disorders or a feeling of detachment from their own body [Citation15,Citation16]. A range of complementary (body mind) treatments are offered [Citation17], but their effectiveness are largely unclear, especially with respect to relapses and long-term effects. High-quality trials have been requested, with longer follow-up time and larger sample sizes, assessing sensitive, validated outcome measures [Citation18]. In this study, therefore, we have investigated the effect of a clinically derived and developed physical therapy intervention named Learning Oriented Physiotherapy (LOP).
LOP has its origin in psycho-motoric physiotherapy, but has been inspired by recent neuroscientific evidence of distributed neural networks as the mechanistic basis of human behaviour and mental life [Citation19–22]. The dynamic interaction of functionally, specialised brain networks may help explain the emergence of many psychiatric symptoms [Citation21,Citation23–25]. Also, the observed close association of bodily and mental symptoms may be understood in terms of network interactions [Citation16,Citation26]. Disorganisation of neural circuits may underly disturbance of normal cognitive, emotional and self-reflective functions, as well as body awareness and ownership [Citation19]. Patients with anxiety and depression may suffer from a range of bodily ailments, but according to amounts of clinical experience, imbalance or dizziness are considered key features shared by most patients.
In order to handle imbalance, many patients compensate with increased tension in antigravity muscles and with the use of their vision fixed on external objects [Citation27,Citation28]. Since vision is primarily meant for navigation, it is considered less suitable as sense organ for updating balance. LOP as therapeutic intervention intends to activate and restore patients’ basic balance system, i.e. proprioceptive information and the vestibular system, but also to unlearn compensatory and inexpedient use of vision. The balance and the use of vision are, therefore, given the main focus of attention in LOP.
In contrast to most mental therapy forms, the patients are invited to and committed as collaborating partners in an active learning process, coached by the physiotherapist. Patients learn how to focus and practise a set of movement patterns integrated into daily life activities (https://www.balansekoden.no/). The simplicity of these activities aims to motivate and easily increase the patients’ sense of achievement [Citation29].
The results of a pilot study (not published) where LOP was tested on 34 selected patients, suggested that symptoms of anxiety, depression and bodily sensations of discomfort declined during 2 years of follow-up and that patients reported improvements in health-related quality of life and functioning with no observed side-effects. Since the pilot study was without controls, we wanted to conduct a pragmatic RCT with the primary aim to investigate the effectiveness of LOP on outpatients diagnosed with moderate symptoms of anxiety and/or depression, both in a shorter and longer term perspective. Secondarily, we wanted to examine the overall effectiveness of LOP on health-related quality of life and perceived global health.
Materials and methods
Trial design
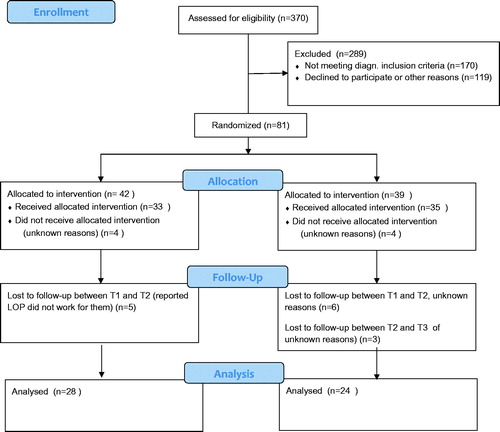
The study was a pragmatic RCT comparing health-related outcomes in patients that received LOP with patients who received standard psychiatric treatment (available psychotherapies). Participants were followed 18 months () with four data assessments. The order of the following section follows the Consort statement [Citation30,Citation31].
Participants
Participants were recruited continuously during the period October 2014 to February 2016 at three public psychiatric clinics geographically located in different parts of Norway. Of 423 patients referred from their general practitioners for symptoms of anxiety and depression, 370 patients met the inclusion criteria of being 18 years of age or older, literate in Norwegian and able to give their consent voluntarily. A total of 170 patients did not meet the diagnostic criteria, leaving 200 eligible for participation. The diagnoses () were confirmed by a psychologist or a psychiatrist at each clinic. Of the 200 patients who were invited, 81 consented to participate in the study. A majority of those who declined to participate (exact number unknown) wanted to receive standard psychotherapy (or treatment as usual). Four patients with anxiety and/or mild or moderate depression as a secondary psychiatric diagnosis were included in the study. Of the 81 patients allocated for participation, the distribution of participants at the three hospital clinics was 36 (44%), 35 (44%) and 10 (12%), respectively.
Table 1. Baseline characteristics of participants (N = 81).
The collected data were mainly obtained from self-reported questionnaires, but information about age, diagnosis and relevant medication was obtained from electronic hospital health records. Administrative staff members at each of the hospitals were responsible for the distribution and collection of all questionnaires during the project period. The participants completed the questionnaires before the first treatment (T1, N = 81), 6 months after the start of treatment (T2, N = 62), 12 months after the start of treatment (T3, N = 56) and 18 months after the start of treatment (T4, N = 52).
If the outpatient treatment was completed, the questionnaires were sent to the participants’ home address, with a prepaid envelope in which to return the completed form. To motivate their response, each participant was informed they would receive two lottery scratch cards upon submission of their questionnaires. A first written reminder was sent from each of the local hospitals after 2–3 weeks. A second reminder was conducted by telephone to motivate participation and to clarify the reasons for missing responses. All telephone contacts were made by one responsible and qualified project assistant at one of the hospitals. One of the three physiotherapists coordinated the work between the hospitals and was responsible for processing, quality assurance and preparation of the data for analysis.
Interventions
LOP as intervention
The intervention was offered by three LOP-authorised and experienced physiotherapists (one at each of the three clinical settings) in their usual clinical settings. In the first weeks of treatment, patients met once a week (60 min). After that, the frequency of consultations varied to some extent depending on patient’s individual needs.
In LOF, the learning aspect is central and the patients are invited to start a learning process that largely intends to be patient-driven. The first meeting, therefore, aims to evaluate the patients’ ability to make changes on their own and the need of support from the therapist. The therapist explains the theoretical basis of LOP and what the treatment involves. Line drawings are used to facilitate the dissemination of information.
A test on an ordinary balance pad enables the patient to become aware of his or her own bodily function/dysfunction, but also the use of their vision as a compensatory mechanism to handle dizziness. Therefore, it is of particular interest for the therapist to observe, and for the patient to experience, how much balance depends on the use of vision. Change of movement patterns requires, of course, unlearning of habitual movements and learning of new ones.
Utilisation of everyday actions as therapeutic tools
All sense organs providing information about the position and movements of the body may contribute to the maintenance of balance [Citation19]. Together with the vestibular apparatus, proprioceptors play a dominant role, but within this group of patients, proprioceptive information commonly seems to be more or less neglected or not integrated with other senses (unconsciously), observed by patients’ imbalance and lack of bodily awareness (e.g. not able to describe the position of their hands without seeing them). In order to reintegrate a more beneficial use of the basic balance system, ten movement sequences have been developed and constitute the therapeutic ‘tools’ in LOP. These are daily life meaningful movements such as e.g. rising to walk, sitting down, walking up and down stairs, getting dressed or undressed, picking up things from the floor – all claiming that patients need to pay full attention to their own bodily balance during the performance. These are directed to the patients in a way characterised by rhythm and flow, and supported by self-commands. Simultaneously, the patients are encouraged to be aware of how the ‘shift of attention’ towards these movement patterns affects them and their symptoms, i.e. the sense of control and the ability to master former challenging situations [Citation29]. Video records of the movements accompanied with explanatory text (only in Norwegian) can be viewed at https://www.balansekoden.no/video-1.html#services.
The idea behind the method is that by utilising these movements systematically, the patient can either prevent loss of mental control or regain control if discomfort occurs. Motivation to learn and practice is, of course, crucial for achieving the expected effect of treatment.
Standard psychiatric treatment as intervention (treatment as usual)
Participants were assigned to different clinicians at each of the three psychiatric outpatient clinics; including psychologists, psychiatrists, psychiatric nurses, milieu therapists and social working clinicians. Participants in the control group received different types of counselling therapy, sometimes in combination with pharmacological treatment. The therapists used cognitive and/or metacognitive therapy, psychodynamic therapy, support therapy or combinations of these approaches, according to the patients’ needs (not recorded).
Outcomes
Symptoms of anxiety and depression and was the primary outcome in this study. Health-related quality of life and perceived global health were included as secondary outcomes. Furthermore, the interactions between follow-up time and treatment were included for all outcomes and are also considered to be secondary outcomes.
In addition, the participants were asked to record background information, including how long (number of years) they had had the symptoms for which they had been referred, their education level (primary and secondary school, and upper secondary school or equivalent, and college and/or university), whether they were in paid employment and if so, how much they worked (full-time or part-time), whether they were students (if so, on a full-time or part-time basis), and whether they received any of the following benefits from the public labour and welfare administration: sickness benefits, unemployment benefits, disability pension and/or a retirement pension.
The Hospital Anxiety and Depression scale (HADS) is a self-reported instrument that records the degrees of anxiety and depression [Citation32]. HADS total consists of 14 items separated into subscales, one for anxiety and one for depression with respectively seven items each, and the severity of symptoms may be calculated both as separate anxiety or depression scores or also as sum-score. A partial scale value of ≥8 is commonly used as cut off for further diagnostic evaluation of anxiety and/or depression [Citation33]. The psychometric qualities HADS based on Norwegian participants (including 9 general population studies and 19 clinical trials) have shown good internal consistency with Chronbach’s alpha ranging from 0.84 (lowest) to 0.91 (highest) [Citation34]. HADS has shown to work well as an instrument to assess the severity of symptoms of anxiety and depression both in observational and clinical studies [Citation33,Citation34].
EuroQol-5 Dimensions, 5 Levels (EQ-5D-5L) is used to provide a standardised, non-disease-specific measure of generic health or health-related quality of life and developed by the EuroQol Group (established in 1987) and introduced in 2009 (https://euroqol.org/). The measurement instrument is recommended by The National Institute for Health and Care Excellence (NICE) and is one of the most widely used instruments internationally, both in clinical studies and in observation studies [Citation35]. It has been found to have satisfactory psychometric measurement characteristics [Citation36–39]. Validation studies have shown that the use of EQ-5D for assessment of cost-effectiveness in mental health care has shown to be more reliable for patients with more moderate symptoms than for those with more severe and complex diagnoses [Citation40].
The EQ-5D-5L index comprises five domains (dimensions), each of which has five answer options (levels), ranging from 1 – no problem, 2 – a slight problem, 3 – a moderate problem, 4 – a severe problem, to 5, which indicates the worst function. The five domains are mobility, self-care, usual activities, pain/discomfort and anxiety/depression. The patients are also asked whether they perceive their health as good or bad ‘today’ (EQ-VAS) by rating health status on a scale from 1 to 100, where 100 is the very best health status. Subscores for each of the five domains, total sum scores, or index scores can be calculated, as well as a separate score for global health, measured on the EQ-VAS scale.
There are no exact limit values to indicate what can be interpreted as a clinically significant improvement, but machine-calculated, country-specific estimates of a minimally important difference (MID) that might be useful in interpreting changes using EQ-5D-5L were used. In our study, therefore, the scores of the five domains were converted into a weighted index score (EQ index) based on studies conducted in the UK [Citation36] since similar weighting did not exist for the Norwegian population. MID was estimated to be 0.037–0.069. According to a Norwegian method study in which a health-economic evaluation of physiotherapy treatment in the primary health service was performed, it was concluded that the EQ-5D-5L had good responsiveness (i.e. ability to capture change over time) [Citation39]. However, the changes will always depend on the treatment and/or health issues being treated [Citation36,Citation41].
Sample size
The required sample size, assuming a significance level of 5% and power of 80%, was calculated in advance of the trial, claiming that with HADS as the primary outcome a sample size of 34 in each study group was needed to demonstrate a moderate difference in HADS total score between the two groups, defined as a standardised effect size of 0.5. To take into account an expected 15% loss to follow-up, all patients who met the inclusion criteria and eligible for participation were included.
Randomisation
Of the 81 participants included, 42 were randomised to LOP and 39 to the control group. Randomisation was done by the use of customised computer software from the Unit for Applied Clinical Research (AKF) at the Norwegian University of Technology and Science, NTNU (https://www.ntnu.edu/mh/akf/forskning), administered by trained clerical personal at each of the three psychiatric clinics.
Blinding
The study was single-blinded. Due to the nature of the interventions, it was not possible to blind participants or therapists. Researchers responsible for data analyses and statistics were blinded.
Statistics
Analyses were performed using IBM SPSS version 24 (IBM SPSS Statistics, Armonk, NY) and Stata, StataCorp. 2017 (Stata Statistical Software: Release 15. StataCorp LLC, College Station, TX). The significance level was set at 0.05. Differences in baseline characteristics between the LOP group and controls were tested by using Independent samples t-tests (means) and Pearson’s chi-square tests (proportions) (). Mean differences in HADS scores, the weighted index score of EQ-5D-5L (EQ-5D index) and (EQ-VAS) between the two groups at each target time (T1–T4) were tested using Independent sample t-tests (). shows the average scores with 95% confidence intervals (95% CI) for each group and health outcome. In order to investigate whether any of the interventions were more effective than the other, mixed linear model (MLM) analysis was performed. MLM analysis is based on all repeated observations, taking the dependency between the data collected for individuals into account and provides the flexibility of modelling not only the means of the data but their variances and covariances as well. Additionally, interaction effects between treatment and time were analysed using the same models, combined with the standard likelihood ratio (LR) tests.
Figure 2. Self-report mean scores (95% CIs) of anxiety and depression (HADS), health-related quality of life (EQ-5D index) and global health (EQ-5D VAS) from baseline to end of the trial, by treatment groups.
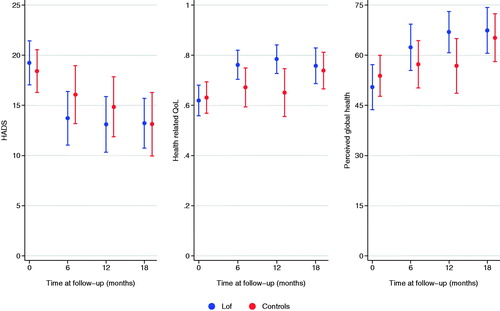
Table 2. Mean scores and mean differencesTable Footnotea in anxiety and depression (HADS), health-related quality of life (EQ-5D index), and global health (EQ-5D VAS) between the LOP group and control group during follow-ups (T1–T4).
Results
Participants flow
shows the participation and the dropout of study participants from allocation (T1) to the end of the trial 18 months later (T4). After allocation, but prior to the initiation of treatment, four participants from the LOP group and 4 from the control group were lost to follow-up for unknown reasons. Between T1 and T2, six controls dropped out without known reason. Five LOP participants who left early in their course of treatment (between T1 and T2), indicated that LOP did not work for them (). A total of 52/81 allocated participants were followed in 18 months with four repeated self-report assessments, including 28/42 in the LOP group and 24/39 in the control group.
According to a dropout analysis, participants with lower education (p = .05) and shorter disease symptom period (<1 year) (p = .04) had a slightly higher dropout rate. Otherwise, there were no statistical significant drop out group differences with regard to gender (p = .198), age (p = .076), diagnoses (p = .243), or other characteristics (). The participants received an average of 14.5 h and 13.8 h of treatment in the LOP and control groups respectively (p = .82). Registered time from the start-up to end of treatment was on average 9 months for participants in the LOP group and 7 months for those in the control group (p = .11). In the study protocol for the trial, the maximum treatment time period set for LOP participants was 1 year. For nine participants, however, the time frame was slightly extended (mean = 15 months). No time limit for treatment time was set for participants in the control group, but four patients received treatment for more than a year.
Characteristics of the participants at baseline
The participants included were in the age range 18–61 years (mean = 32 years). More women (n = 50) than men (n = 31) participated. On average, the participants have had the mental disorder symptoms in 6.6 years, 25% had had them for 10 years or more and 12% for less than 1 year. A total of 60% of the participants indicated that they were in employment at the start of the study.
Primary outcome, anxiety and depression
shows the mean total score (95% CI) for HADS (primary outcome) for patients in both the LOP and control group at 6, 12 and 18 months of follow-up. In both groups, the greatest health improvements (steepest curves) were observed the first 6 months of follow-up (not in table). While half or more had a HADS total score of 19 or more at baseline, this proportion was halved by the end of the trial, and the mean HADS score was 5.6 lower than at baseline. The unadjusted mean summarised or separate HADS scores did not differ between the two groups at any T1–T4 assessment ().
Secondary outcomes, health related quality of life and global health
also shows the unadjusted mean total scores (95% CI) for the EQ-5D index and EQ VAS for patients in both the LOP and control group during follow-up. At 12 months of follow-up (T2), LOP participants reported higher quality of life (p = .02) and also higher global health (p = .05) than controls did.
Overall treatment effects, primary and secondary outcomes
Multivariable adjusted analyses that included all repeated observations from T1 to T4, showed no statistically significant mean differences in treatment effects on mental health or quality of life between participants in the LOP group and the control group (). However, both for HADS (p<.001) and for EQ-5D index (p<.001) there was a statistically significant interaction effect between therapy and follow-up time at T2 and T3, suggesting that LOP patients experienced a slightly faster rate of recovery than controls did during follow-up (). The interaction term between follow-up time and perceived global health was statistically significant at T3 (p = .013), but not at T2.
Table 3. Adjusteda overall differencesb in treatment effects between LOP participants and controls (reference group), including HADS score, EQ index score and EQ 5 D VAS score analysed by the use of Mixed Linear Models (N = 249 observations).
Discussion
After 18 months of follow up, there were no mean differences in health outcomes, suggesting that LOP was as effective as a standard psychiatric treatment for patients included in this study. However, overall findings suggest that LOP participants experienced a slightly faster rate of recovery during follow-up than controls did.
All participants included in this study had initially a HADS score of 8 or higher, which according to literature indicates a need for referral [Citation33]. Results suggest that mental health problems declined in most patients during follow-up and that participants in both groups were recovering. At 6 months of follow-up, no statistically significant differences in health outcomes between the two groups were observed, but after 1 year, LOP participants were slightly more satisfied with their quality of life and rated their global health higher than the controls did. The clinical significance of this finding is unclear, but according to the literature, the difference in health-related quality of life is well above what is considered a MID [Citation41]. At the end of the study, there were no such mean differences between respondents in the two treatment groups.
According to this study, the greatest health improvements in both groups were observed during the first 6 months, but overall results suggest that on average, the time it took to improve health to a certain level was shorter for LOP patients than for controls. Although we found no mean differences in for example symptoms of anxiety and depression at any time point, the multivariable mixed method analyses revealed that there was an interaction between treatment and time, suggesting that on average, the HADS score decreased faster in LOP participants than in controls. To our knowledge, the temporal aspect of psychiatric rehabilitation has received little focus in research, but faster rates of recovery should be considered an advantage not only for the patient, but also in a cost benefit perspective. The finding underscores the advantage of using more advanced statistical modelling [Citation42], in particular, in studies with smaller samples and with many repeated observations. The size and meaning of this finding for clinical practice are, of course, unclear, but the temporal aspect is interesting and thus an object for further investigation.
In spite of the well-known comorbidity between balance and anxiety disorders in adults [Citation43,Citation44] as well as in children [Citation45,Citation46], psychological interventions hardly ever address patients’ balance difficulties. In LOP, the balance is given the main focus of attention, but the therapeutic approach is multifaceted (e.g. thinking, process, therapeutic tools, etc.) and perhaps more composite than ‘standard psychiatric treatment’. All elements included in LOP may be of relevance for the observed effect and also interact, but it is not possible to disentangle the effect of one element from the other. In other words, it is unclear to what extent the focus on e.g. balance, vision or any of the other features explain the progress patients made during follow-up. Although possible effect mechanisms of LOP remain unclear, findings from this clinical trial largely support the idea that bodily balance and mental control affect each other mutually [Citation19,Citation47]. Presumably, clinical improvement is correlated with alterations in the structure and function of neural networks [Citation21,Citation23,Citation24].
Studies have shown that disorganisation of neural networks may disturb normal cognitive, emotional and self-reflective functions, including the sense of body awareness and body ownership [Citation15,Citation16,Citation48]. In LOP, body awareness is considered a prerequisite for improving mental balance and control and in that case, visual awareness may play an important role [Citation27,Citation28]. Years of clinical experience have shown that patients commonly are using their vision as a compensatory mechanism to handle dizziness and imbalance, and in order to improve body awareness, LOP patients have to undergo a learning process claiming both unlearning and relearning of use of their vision. Recent research supports the significance of vision in the interplay between mental and bodily imbalance. According to van der Hoort et al. [Citation49], the sense of body ownership also promotes visual awareness.
Since the turn of the century, different body awareness therapies have emerged [Citation50]. These typically aim to normalise posture, balance, breathing and muscular tension. Although body awareness is central in LOP, the thinking underlying LOP, as well as the therapeutic tools, are quite different from other body awareness therapies, making it both inappropriate and difficult to compare results across studies. Nevertheless, in a previous 3 months follow-up body awareness therapy study based on a very similar sample as in LOP, interventions improved body awareness, self-efficacy, sleep and physical coping resources more than treatment as usual [Citation51]. Despite the dissimilarities between studies, the focus and efforts to increase body awareness within this group of patients seem very appropriate. In a more recent 12 months RCT study, patients that received basic body awareness therapy (BBAT) reported higher body awareness, body attitude, fewer symptoms and improved self-efficacy after 6 months after treatment termination than the controls did. In addition, the BBAT group reported less use of other health and social services 1 year after baseline. In this study, however, BBAT was only used complementary [Citation52].
Contrary to most physiotherapies, LOP is not complementary, but used instead of conventional psychiatric medicine and thus an alternative treatment approach. Unfortunately, there is a lack of high-quality evidence of the effect of both conventional and complementary therapeutic interventions on anxiety and depression, and in particular in patients that suffer from both mental and musculoskeletal disorders. According to a recent scoping review [Citation18], only one out of 111 systematic reviews on the effect of complementary medicine (mind-body therapies) on musculoskeletal and mental disorders, investigated the comorbidity between these disorders. Partly, this may be due to the costs by conducting high-quality clinical trials, but also the complexity of questions and mechanisms that need to be handled. For example, a recent meta-analysis of RCT’s on exercise concluded that exercise was an effective intervention for unipolar depression when given independently, but not in comparison with psychological treatments and antidepressant medication [Citation53]. Future research, therefore, ought to investigate both independent and combined effects of interventions that aim to improve health in patients with comorbid mental and bodily dysfunctions.
Psychological therapies such as cognitive behaviour therapy and antidepressants have proven benefit for treating both depression and anxiety, but relapses are common and many patients do not seek psychiatric treatment [Citation7,Citation54]. Accordingly, there has been increasing interest and use of complementary and alternative medicine (CAM), such as mind-body or lifestyle interventions [Citation55,Citation56]. Findings have shown that CAM may appear as more attractive than conventional psychiatric therapies to many patients. One explanation is that such therapies are more congruent with users’ own values, beliefs and philosophical orientations towards health and life [Citation57]. On the other hand, not seeking psychiatric treatment is not necessarily a result of being dissatisfied or not trusting conventional medicine [Citation57,Citation58]. Studies have shown that an overwhelming majority of patients using CAM approaches do so to complement conventional care rather than as an alternative to conventional care [Citation55]. It is not clear from this clinical trial though, if the effect could have been even more pronounced if LOP was combined with conventional therapies. In fact, some of the patients in both treatment arms were medicated, but the possible adjunctive effect of medication within or between the groups is unclear (no differences in use between groups at baseline).
Although the mechanisms underlying the symptoms ought to be found in the brain, LOP as a therapeutic approach is a result of a thorough collaboration between a group of physiotherapists, a neurobiologist/-scientist and their patients over years in clinical practice [Citation47]. Given that bodily dizziness and dysfunction is kind of a code that needs to be understood as interactions between the body and the brain, bodily expressions should attain more interest in the future, both in clinical practice settings and in research.
Since LOP was conducted as part of the conventional therapies within hospital settings, it is not clear from this study whether results would have been the same if LOP was offered in e.g. primary health care or other settings. The hospital settings may at least theoretically influence patients’ confidence and thus results. The potential effects of treatment settings should, therefore, be tested in future research.
For future use and further improvements in approach, it is also important to get a deeper insight into the mechanisms of LOP as a multifaceted therapeutic intervention (e.g. the learning process, the focus on balance and the therapeutic tools). Although RCT studies are considered the gold standard in effect studies, qualitative methods may contribute to more in-depth knowledge about learning and recovering as a process [Citation59].
Strengths and limitations
The strength of the study is the study design, the use of reliable and validated measurements and the many repeated assessments, as well the long term of follow-up. The study was a pragmatic multicentre RCT, which largely is considered as strength when assessing health service effectiveness. First, it has the advantage of being an RCT, but secondly, the trial was conducted as part of ordinary clinical practice, which may make findings more applicable when it comes to inform decisions about practice [Citation31].
With the exception of the statisticians who did not know which participants belonged to the different groups, it was not possible to blind either the subjects or therapists. This, of course, represents a weakness in such studies. Another aspect that may have influenced results was that the LOP therapists’ with great ownership of the method, might have shown more interest and engagement than therapists/consultants that treated patients in the control group. Such influences cannot be controlled for, but may explain some of the observed temporal differences in health outcomes between the groups.
It is also likely that there has been some sort of selection of patients since more than half of eligible patients declined the invitation to participate. A majority of these preferred to receive standard psychiatric treatment. Participants that were included and followed in this study may, therefore, not be quite representative for patients with moderate anxiety and depression as such. Selection may, for example, explain why more women than men participated, but due to the randomisation of patients, possible selection of patients is not considered to bias the comparisons between groups. It is not clear why a higher proportion of participants in the LOP group compared to controls had higher education, but the overall results were controlled for education level and thus taken into account.
The results suggest that LOP is as effective as ‘psychotherapy’, but controls were given a range of different therapies and we cannot know for sure if results were the same if controls had received a more standardised psychotherapy. On the other hand, these are probably fairly representative of the therapies patients are offered at psychiatric clinics in Norway and comparisons, therefore, considered to be adequate.
The drop-out rate in this study as for many RCT studies represents a limitation, but was quite similar for both treatment arms. One should also keep in mind that the participants were followed over 18 months with several data assessments, i.e. conditions that increase the chance of dropping out.
Conclusions
This study suggests that for patients with moderate anxiety and depression, LOP may be a good alternative to more traditional outpatient therapies.
Ethical approval
Participants were informed of the purpose of the study, data collection, and implementation, both verbally and in writing, and gave their written consent to participate in the study. The research protocol was designed in accordance with the Helsinki Declaration https://www.etikkom.no/Helsinkideklarasjonen and was approved by the Regional Committee for Medical and Health Research Ethics (REC) in South East Norway (ref. 2014/393).
Clinical Trial Registry
The study is registered in ClinicalTrials.gov (ref. NCT02194036).
Acknowledgements
The authors greatly thank neurobiologist and professor emeritus Per Brodal, University in Oslo, for his professional and scientific expertise, support and engagement that have made LOP as well as this study possible.
Disclosure statement
The authors report no conflicts of interest.
Funding
Nord-Trøndelag Hospital Trust financed 7 months of project management costs and 35.000 Norwegian krones (NOK) in grants. Møre og Romsdal Hospital Trust supported the project financially with 100.000 NOK in grants.
References
- Murray CJL, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–2223.
- Patel V, Chisholm D, Parikh R, et al. Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edition. Lancet. 2016;387:1672–1685.
- Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–1586.
- Olatunji BO, Cisler JM, Tolin DF. Quality of life in the anxiety disorders: a meta-analytic review. Clin Psychol Rev. 2007;27:572–581.
- Steel Z, Marnane C, Iranpour C, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int J Epidemiol. 2014;43:476–493.
- Kessler RC, Sampson NA, Berglund P, et al. Anxious and non-anxious major depressive disorder in the World Health Organization World Mental Health Surveys. Epidemiol Psychiatr Sci. 2015;24:210–226.
- Tiller JW. Depression and anxiety. Med J Aust. 2013;199:S28–S31.
- Haug TT, Mykletun A, Dahl AA. The association between anxiety, depression, and somatic symptoms in a large population: the HUNT-II study. Psychosomat Med. 2004;66:845–851.
- Lallukka T, Mekuria GB, Nummi T, et al. Co-occurrence of depressive, anxiety, and somatic symptoms: trajectories from adolescence to midlife using group-based joint trajectory analysis. BMC Psychiatry. 2019;19:236.
- Ijaz S, Davies P, Williams CJ, et al. Psychological therapies for treatment-resistant depression in adults. Cochrane Database Syst Rev. 2018;5:CD010558.
- Scholten WD, Batelaan NM, van Balkom AJ, et al. Recurrence of anxiety disorders and its predictors. J Affect Disord. 2013;147:180–185.
- Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. Int J Psychiatry Med. 2011;41:15–28.
- Harvey SB, Øverland S, Hatch SL, et al. Exercise and the prevention of depression: results of the HUNT cohort study. Am J Psychiatry. 2018;175:28–36.
- Association TAP. The American psychiatric association practice guidelines for the psychiatric evaluation of adults. 3rd ed. Arlington (VA): American Psychiatric Pub; 2015.
- Serino A, Alsmith A, Costantini M, et al. Bodily ownership and self-location: components of bodily self-consciousness. Conscious Cogn. 2013;22:1239–1252.
- Tsakiris M, Schutz-Bosbach S, Gallagher S. On agency and body-ownership: phenomenological and neurocognitive reflections. Conscious Cogn. 2007;16:645–660.
- Asher GN, Gerkin J, Gaynes BN. Complementary therapies for mental health disorders. Med Clin North Am. 2017;101:847–864.
- Lorenc A, Feder G, MacPherson H, et al. Scoping review of systematic reviews of complementary medicine for musculoskeletal and mental health conditions. BMJ Open. 2018;8:e020222.
- Brodal P. The central nervous system. New York (NY): Oxford University Press; 2016.
- Park HJ, Friston K. Structural and functional brain networks: from connections to cognition. Science. 2013;342:1238411–1238411.
- Sporns O, Betzel RF. Modular brain networks. Annu Rev Psychol. 2016;67:613–640.
- Rabinovich MI, Simmons AN, Varona P. Dynamical bridge between brain and mind. Trends Cogn Sci. 2015;19:453–461.
- Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15:483–506.
- Price JL, Drevets WC. Neural circuits underlying the pathophysiology of mood disorders. Trends Cogn Sci. 2012;16:61–71.
- van den Heuvel MP, Sporns O. A cross-disorder connectome landscape of brain dysconnectivity. Nat Rev Neurosci. 2019;20:435–446.
- Browning M, Fletcher P, Sharpe M. Can neuroimaging help us to understand and classify somatoform disorders? A systematic and critical review. Psychosom Med. 2011;73:173–184.
- Agarwal K, Bronstein AM, Faldon ME, et al. Visual dependence and BPPV. J Neurol. 2012;259:1117–1124.
- Cousins S, Cutfield NJ, Kaski D, et al. Visual dependency and dizziness after vestibular neuritis. PLoS One. 2014;9:e105426.
- Leotti LA, Iyengar SS, Ochsner KN. Born to choose: the origins and value of the need for control. Trends Cogn Sci. 2010;14:457–463.
- Schulz KF, Altman DG, Moher D, et al., for the CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332–c332.
- Zwarenstein M, Treweek S, Gagnier JJ, et al., for the CONSORT and Pragmatic Trials in Healthcare (Practihc) groups. Improving the reporting of pragmatic trials: an extension of the CONSORT statement. BMJ. 2008;337:a2390–a2390.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370.
- Bjelland I, Dahl AA, Haug TT, et al. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res. 2002;52:69–77.
- Leiknes KA, Dalsbø TK, Siqveland J. Måleegenskaper ved den norske versjonen av Hospital Anxiety and Depression Scale (HADS). Oslo (Norway): Folkehelseinstituttet; 2016.
- Devlin NJ, Krabbe PF. The development of new research methods for the valuation of EQ-5D-5L. Eur J Health Econ. 2013;14:1–3.
- Luo N, Johnson J, Coons SJ. Using instrument-defined health state transitions to estimate minimally important differences for four preference-based health-related quality of life instruments. Med Care. 2010;48:365–371.
- Solberg TK, Olsen J-A, Ingebrigtsen T, et al. Health-related quality of life assessment by the EuroQol-5D can provide cost-utility data in the field of low-back surgery. Eur Spine J. 2005;14:1000–1007.
- Holm I. Helseøkonomisk evaluering av fysioterapibehandling i primaerhelsetjenesten en metodestudie. Universitetsbiblioteket i Oslo; 2013.
- Kontodimopoulos N, Pappa E, Niakas D, et al. Validity of the EuroQoL (EQ-5D) Instrument in a Greek General Population. Value Health. 2008;11:1162–1169.
- Brazier J, Connell J, Papaioannou D, et al. A systematic review, psychometric analysis and qualitative assessment of generic preference-based measures of health in mental health populations and the estimation of mapping functions from widely used specific measures. Health Technol Asses. 2014;18:188.
- Nolan CM, Longworth L, Lord J, et al. The EQ-5D-5L health status questionnaire in COPD: validity, responsiveness and minimum important difference. Thorax. 2016;71:493–500.
- Brown H, Prescott R. Applied mixed models in medicine. Chichester (UK): John Wiley & Sons; 2014.
- Balaban CD. Neural substrates linking balance control and anxiety. Physiol Behav. 2002;77:469–475.
- Yardley L, Watson S, Britton J, et al. Effects of anxiety arousal and mental stress on the vestibulo-ocular reflex. Acta Otolaryngol. 1995;115:597–602.
- Bart O, Bar-Haim Y, Weizman E, et al. Balance treatment ameliorates anxiety and increases self-esteem in children with comorbid anxiety and balance disorder. Res Dev Disabil. 2009;30:486–495.
- Erez O, Gordon CR, Sever J, et al. Balance dysfunction in childhood anxiety: findings and theoretical approach. J Anxiety Disord. 2004;18:341–356.
- Fadnes BL, K.; Brodal P. Læringsorientert fysioterapi: teori og praksis. Oslo (Norway): Universitetsforlaget; 2013.
- Williams LM. Defining biotypes for depression and anxiety based on large-scale circuit dysfunction: a theoretical review of the evidence and future directions for clinical translation. Depress Anxiety. 2017;34:9–24.
- van der Hoort B, Reingardt M, Ehrsson HH. Body ownership promotes visual awareness. eLife. 2017;6:e26022.
- Gyllensten AL, Skär L, Miller M, et al. Embodied identity–a deeper understanding of body awareness. Physiother Theory Pract. 2010;26:439–446.
- Gyllensten AL, Hansson L, Ekdahl C. Outcome of basic body awareness therapy. A randomized controlled study of patients in psychiatric outpatient care. Adv Physiother. 2003;5:179–190.
- Gyllensten AL, Ekdahl C, Hansson L. Long-term effectiveness of basic body awareness therapy in psychiatric outpatient care. A randomized controlled study. Adv Physiother. 2009;11:2–12.
- Kvam S, Kleppe CL, Nordhus IH, et al. Exercise as a treatment for depression: a meta-analysis. J Affect Disord. 2016;202:67–86.
- Blumenthal R, Endicott J. Barriers to seeking treatment for major depression. Depress Anxiety. 1996;4:273–278.
- Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States. Natl Health Stat Report. 2007;2008:1–23.
- Kessler RC, Soukup J, Davis RB, et al. The use of complementary and alternative therapies to treat anxiety and depression in the United States. Am J Psychiatry. 2001;158:289–294.
- Astin JA. Why patients use alternative medicine: results of a national study. JAMA. 1998;279:1548–1553.
- Eisenberg DM, Kessler RC, Van Rompay MI, et al. Perceptions about complementary therapies relative to conventional therapies among adults who use both: results from a national survey. Ann Intern Med. 2001;135:344–351.
- Verhoef MJ, Casebeer AL, Hilsden RJ. Assessing efficacy of complementary medicine: adding qualitative research methods to the” Gold Standard. J Alternat Complement Med. 2002;8:275–281.