Abstract
Gynaecological cancers are a major global health concern due to the lack of effective screening programmes for ovarian and endometrial cancer, for example, and variable access to vaccination and screening tests for cervical cancer in many countries. Recent research on portable and cost-effective lab-on-a-chip (LoC) technologies show promise for mass screening and diagnostic procedures for gynaecological cancers. However, most LoCs for gynaecological cancer are still in development, with a need to establish and clinically validate factors such as the type of biomarker, sample and method of detection, before patient use. Multiplex approaches, detecting a panel of gynaecological biomarkers in a single LoC, offer potential for more reliable diagnosis. This review highlights the current research on LoCs for gynaecological cancer screening and diagnosis, emphasizing the need for further research and validation prior to their widespread adoption in clinical practice.
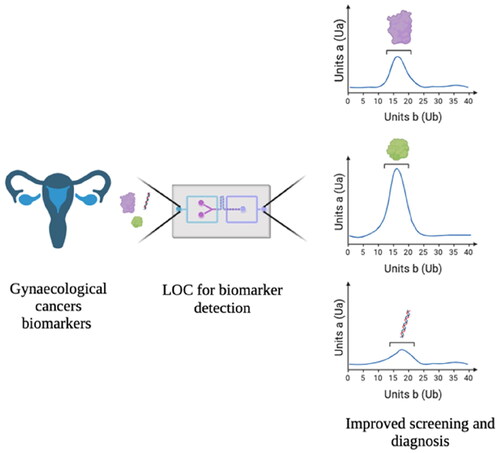
Graphical Abstract
Introduction
Gynaecological cancers are a group of malignancies that originate in the female reproductive system, including vaginal, cervical, ovarian, uterine and vulvar cancers [Citation1]. In the UK, there are over 22,000 new cases and 8,000 deaths due to gynaecological cancers every year [Citation1,Citation2].
Uterine or endometrial cancer is the most common gynaecological cancer in the UK, with nearly 10,000 new cases per year [Citation3]. Nonetheless, mortality rate for uterine cancer is relatively low although, with increasing cases of obesity, a strong risk factor for endometrial cancer, mortality rates have increased in the last decades [Citation4]. Most patients present with post-menopausal bleeding and more than 70% of women in England present with stage I endometrial cancer [Citation5].
Ovarian cancer is the sixth most common female cancer in the UK and one of the deadliest around the world. This cancer affects the ovaries but it can also rise from neighbouring structures, such as fallopian tubes and the peritoneum, facilitating its spread and often challenging its classification [Citation6]. Due to lack of clear symptoms, it is challenging to diagnose at early stages (stage I or II) [Citation7] and in England only about 40% of new cases are stage I and II [Citation5]. Advanced stages of the disease (stage III and IV) are much more likely to relapse or progress, negatively impacting on survival despite recent advances in systemic therapy. In fact, the 5-year survival rate in early-stage ovarian cancer is over 90%, while late-stage diagnosis is estimated at less than 15% [Citation7,Citation8].
Cervical cancer is the 14th most common cancer in the UK with over 70% of cases linked to the human papillomavirus virus (HPV) infection. Oncogenes E6 and E7 allow HPV to chronically infect cells, leading to dysplasia and oncogenesis in the cervix [Citation9,Citation10]. Screening tests and preventive HPV vaccinations have enabled early disease detection and limited the number of cervical cancer cases [Citation11].
Finally, vaginal and vulval cancers, which are also associated with HPV infections [Citation12,Citation13], are rarer gynaecological cancers accounting for less than 2,000 new cases a year in the UK, combined. There are no established screening programmes for the general population for these cancers.
More information on the biological aspects of gynaecological cancers can be found in Ledford and Lockwood [Citation1], Low et al. [Citation14] and McCluggage [Citation15]. The scope of this literature review is to report and compare some of the recent advances in gynaecological screening and diagnostic tools and their potential to be incorporated in the healthcare system for improved clinical benefits.
Screening versus diagnosis
Screening refers to the testing of an asymptomatic population to define the likelihood of developing a particular condition. Screening differs from diagnostic tests, in that diagnostic tests detect the presence or absence of a condition in the current state or moment [Citation16,Citation17].
Some screening and diagnostic tests may share similar techniques, for example, measuring disease biomarker levels and/or imaging, but their purpose and advantages differ. Screening allows preventive care to be introduced for continued wellness. Diagnostic tests are ordered when an individual is symptomatic or presents with ambiguous or positive screening tests to determine whether the condition has already developed. A diagnostic evaluation can determine the course of treatment, prognosis and survival estimate for a patient [Citation18].
Screening tests need to be simpler, cost-effective and less invasive to enable rapid, mass screening programmes while diagnostic tests are generally more complex and expensive as they are usually performed in specific circumstances. Additionally, screening tests are designed to achieve high sensitivity to avoid missing the potential development of a disease while diagnostic tests require high specificity to identify true positives and negatives to ensure effective treatment strategies and avoid harm [Citation19]. For example, mammography (X-ray of breasts) is the screening test for breast cancer detection. Given the simplicity of the test as an imaging scan, a mammography can be offered as a national screening programme for the high-risk population (50–70 years old women in the UK). However, to understand changes in the breast tissues visualized on a mammograph, a biopsy is offered as a diagnostic test for breast cancer. The diagnostic biopsy is more invasive, costly and time-consuming but more specific and reliable for an accurate clinical evaluation [Citation20].
Clinically available screening and diagnostic tests
Current screening tests
Screening programmes, especially on a national level, are resource intensive. Consequently, the social, economic and clinical benefits of screening a population must be significant. This criterium imposes a great obstacle in incorporating numerous effective screening tests in regular healthcare [Citation16,Citation21].
Currently, the only gynaecological cancer to possess a national screening programme in the UK is cervical cancer, with the HPV or cervical screening test [Citation10]. In this, cervical smear samples are collected during the cervical cancer screening visit to detect for pre-invasive cervical cancer. Although most HPV infections are self-curable, some chronic infections by specific types of HPV may induce cervical cancer development. Therefore, it is vital to establish HPV type through cervical smear tests. HPV type is detected by molecular analysis of HPV’s DNA or RNA profile. There are various DNA-targeting assays such as in situ hybridization and hybrid capture assays, with polymerase chain reaction (PCR) and in situ PCR being used more commonly [Citation22]. For mRNA analysis, there are reverse transcriptase (RT) PCR or nucleic acid sequence base amplification [Citation23]. HPV16 and HPV18 are the most common types of viruses responsible for cervical cancer development [Citation24].
The lack of a national screening programme, both in the UK and worldwide, for ovarian cancer is a serious unmet need as its non-specific symptoms are often overlooked. However, it is challenging to develop a screening test for ovarian cancer due to a lack of reliable biomarkers specific to early stages of the disease (stage I, II or earlier). In 2001, a large, randomized control trial, The United Kingdom Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) was established. The trial enrolled over 202,000 asymptomatic women between the ages of 50 and 74 to screen for ovarian cancer over a period of more than 16 years. The participants were divided into ‘no screening’, ‘screening with annual biomarker cancer antigen 125 (CA125) serum test with transvaginal ultrasound (TVUS)’ and ‘annual TVUS only’ categories. CA125 is a weak diagnostic biomarker for ovarian cancer; however, it was hypothesized that combined biomarker analysis and imaging scans (TVUS) may have offered a more accurate disease detection. The trial concluded that the expected earlier detection of ovarian cancer through these three screening methods did not significantly reduce mortality rates, indicating a lack of benefit of combined CA125 levels and TVUS for ovarian cancer screening [Citation7,Citation25].
Endometrial cancer does not have a screening programme due to lack of means to accurately detect the disease prior to its onset. Biopsies of the endometrial tissue can be collected to search for cancerous cells in high-risk populations, such as those suffering with irregular bleeding or with Lynch syndrome. Nonetheless, it is not yet proven that endometrial screening biopsies can lower the cancer mortality rate [Citation26].
Finally, due to the rarity of vaginal and vulvar cancers cases, currently, there are no mass screening programmes for them, nor is it an area of active research [Citation27].
Current diagnostic tests
Diagnostic tests for gynaecological cancers are limited and non-specific. Blood tests are part of the diagnostic process for gynaecological cancers; however, they only provide a general health overview, except for the CA125 test, which is the only serum analysis clinically associated with the detection of a gynaecological cancer. Testing for CA125 is part of the standard diagnostic work up for a potential ovarian cancer diagnosis, yet the biomolecule has poor specificity and sensitivity for ovarian cancer [Citation28,Citation29]. In fact, CA125 levels can also be elevated in non-cancerous gynaecological conditions, such as endometriosis and pregnancy [Citation30]. Nonetheless, CA125 may be beneficial for disease reoccurrence although imaging scans, such as TVUS, CT and MRI, are more reliable diagnostic tests for ovarian cancer detection [Citation31]. Unfortunately, their inability to distinguish between malignant masses and benign cysts highlights the need for additional diagnostic tests with reliable biomarkers for ovarian cancer [Citation8,Citation32].
For cervical cancer, colposcopy allows visual identification of abnormal cells in the patient’s cervix but requires laboratory analysis for diagnostic confirmation [Citation33]. Hence, cervical cancer diagnostic procedures remain invasive and complex. Identifying reliable biomarker(s) might enable designing simpler and more cost-effective tests.
Lastly, biopsies are the most accurate, albeit most invasive, techniques to establish a cancer diagnosis. For gynaecological cancers, affected tissues or cells are collected via various methods: image-guided percutaneous, laparoscopy, laparotomy, hysteroscopy, excision (vaginal cancer) and incision (vulval cancer) [Citation12,Citation13,Citation34].
Screening and diagnostic biosensors in development
Lack of reliable screening and/or early diagnostic tests prevents early detection of gynaecological cancers [Citation16,Citation17]. Novel clinical research is focusing on detecting specific signature biomolecules associated with a condition (biomarkers) to address the early disease detection challenge. The known biomarkers can then be detected using biosensor devices as disease screening and diagnostic tools. Biosensors are analytical devices that combine a biological recognition ligand specific to a biomarker with physical or chemical signalling devices (transducers). The recorded biomolecular interactions are transformed into digital signals that are interpreted by a computer-aided readout, thereby providing the user with a biomarker measurement in the sample to indicate disease presence and/or stage [Citation35].
Most biomarker detection assays are currently performed in centralized labs, requiring trained personnel, and resulting in long wait times for results, which is problematic for time-sensitive medical conditions [Citation36]. To address this, there is a growing focus on developing point-of-care (PoC) tests that can be operated by untrained individuals at the patient’s location. These tests aim to provide accurate, sensitive and rapid results at a relatively low cost. Ideally, PoC tests would be self-sustaining, allowing non-trained operators to load a sample and obtain informative results with minimal intervention. Lab-on-a-chip (LoC) technologies, which integrate all analysis steps into a single device, have the potential to advance PoC medical diagnostics significantly () [Citation36,Citation41,Citation42]. LoCs focus on processing a sample to identify biomarkers (e.g. via antibodies, aptamers, etc.) in a chip. Detection may be performed separately, for example, with plate readers or microscopes for fluorescent signal detection. However, LoCs with detection properties would promote at-home testing and circumventing the need for skilled personnel or specialized equipment for screening or diagnosis. For instance, blood glucose monitors, such as the FreeStyle Libre by Abbott are patch tests with Bluetooth-enabled sensors that send live results on glucose levels to a phone app for the patient to view and monitor [Citation43]. Therefore, biosensors can be combined with LoC technologies, and microfluidic techniques to enable portability, PoC detection and cost-effectiveness by removing the need for laboratories and highly skilled personnel for sample processing and analysis [Citation42,Citation44]. Devices currently in development (but not yet clinically or commercially available) for various gynaecological cancers are listed in . Upon clinical validation, these devices hold the potential to become effective diagnostic and screening tests for detecting gynaecological cancers.
Figure 1. Layouts of lab-on-chip (LoC) devices in development for gynaecological cancer detection. (a) Schematic of gold nanoparticles on a self-assembled monolayer (SAM) interdigitated electrode-based microfluidic biosensor for immunocapture of CA125 [Citation37]; (b) construction of aptamer-linked magnetic nanoclusters and circulating tumor cell capture with biomimetic microfluidic system [Citation38]; (c, i) integrated microfluidic chip (IMC) illustration for cell-free DNA (cfDNA) capture; (c, ii) design of the IMC for cfDNA capture [Citation39]; (d) ExoSearch chip for continuous mixing, isolation and in situ, multiplexed detection of circulating exosomes; (d i, ii) bright-field microscope images of immunomagnetic beads manipulated in microfluidic channel for mixing and isolation of exosomes; (d iii) exosome-bound immunomagnetic beads aggregated in a microchamber with on/off switchable magnet for continuous collection and release of exosomes; (d iv) TEM image of exosome-bound immunomagnetic bead in a cross-sectional view [Citation40].
![Figure 1. Layouts of lab-on-chip (LoC) devices in development for gynaecological cancer detection. (a) Schematic of gold nanoparticles on a self-assembled monolayer (SAM) interdigitated electrode-based microfluidic biosensor for immunocapture of CA125 [Citation37]; (b) construction of aptamer-linked magnetic nanoclusters and circulating tumor cell capture with biomimetic microfluidic system [Citation38]; (c, i) integrated microfluidic chip (IMC) illustration for cell-free DNA (cfDNA) capture; (c, ii) design of the IMC for cfDNA capture [Citation39]; (d) ExoSearch chip for continuous mixing, isolation and in situ, multiplexed detection of circulating exosomes; (d i, ii) bright-field microscope images of immunomagnetic beads manipulated in microfluidic channel for mixing and isolation of exosomes; (d iii) exosome-bound immunomagnetic beads aggregated in a microchamber with on/off switchable magnet for continuous collection and release of exosomes; (d iv) TEM image of exosome-bound immunomagnetic bead in a cross-sectional view [Citation40].](/cms/asset/71d6d8cb-d91b-4876-ad8e-f8ef8f739c17/ianb_a_2274047_f0001_c.jpg)
Table 1. List of lab-on-a-chip devices to detect gynaecological cancer biomarkers using microfluidic technology.
Biomarkers: the research gap
Numerous LoC devices utilizing microfluidics technology, currently in development, demonstrate promising results in detecting gynaecological cancer biomarkers with high sensitivity and specificity (). However, integrating these devices as functional screening and/or diagnostic tests in clinical settings is challenging due to lack of clinically validated biomarker levels associated with the disease. Furthermore, biomarker validation for this purpose, encounters further obstacles, such as the limited availability of high integrity biological tissues resulting from variations in biospecimen preparation and storage conditions, heavily affecting biomarker analysis. Moreover, antibody-dependent assays used to detect biomarkers lack standardized protocols, due to variations in antibody type and stability, in turn impacting reproducibility of results [Citation52]. These challenges prolong the biomarker validation process. Without establishing threshold or range values for the disease biomarker levels corresponding to high risk (screening) or affected (diagnosis) individuals, biosensors cannot become effective clinical tools.
Most LoC devices under development for gynaecological cancers focus on detecting biomarkers for ovarian cancer () as there are known biomarkers for the disease and this is area of greatest unmet need. The most investigated biomarker is CA125; however, CA125 levels are associated with low sensitivity and specificity for the malignancy [Citation25]. Other ovarian cancer-associated biomarkers, such as EpCAM, HE4, mutant BRCA1 and BRCA2 genes, have also been explored in biosensors to enhance accuracy for ovarian cancer detection [Citation39,Citation40,Citation53,Citation54]. For instance, germ-line mutations in BRCA 1/2 genes accounted for 16.6% of serous ovarian cancer patients of which, 22.6% were high grade serous in a cohort of 1001 women with ovarian cancer patients [Citation55]. Moreover, patients with germline BRCA 1/2 mutations present with overall favourable survival and response to plan-based therapy [Citation55]. Therefore, different biomarkers show association with specific subtypes of ovarian cancer development and in consequence, have also different effect on prognosis and treatment course. Nonetheless, germline mutations in BRCA genes account for only 10–15% of all ovarian cancers (and if identified, undergo prophylactic surgery, and hence detected early) while ∼5% are a somatic BRCA mutation. The remaining ovarian cancer cases are wildtype BRCA genes [Citation56]. Furthermore, BRCA gene mutations, EpCAM and HE4 are all associated with other malignancies, including breast and lung cancers [Citation7,Citation29,Citation39]. As a result, despite device efficiency, usage of non-specific and non-sensitive biomarkers leads to device failure to reliably detect ovarian cancer.
Biomarkers for other gynaecological cancers are less explored: cervical cancer has an established world-wide screening programme (cervical smears) detecting HPV-induced morphological changes that successfully helps prevent malignant cases; hence, identifying additional biomarkers is not a priority. Nonetheless, to enable accurate biosensing of cervical cancer, further biomarkers may be required, for instance, CEA and ADAM9 are being investigated to characterize malignancy [Citation49,Citation57]. For endometrial cancer, a CA125 test can be performed upon diagnosis; however, CA125 is non-specific for gynaecological conditions and hence the test may not be accurate. Finally, due to the low incidence for vaginal and vulvar cancers, biomarkers for these cancers are rarely researched; hence, microfluidic devices specific for vaginal and vulvar cancers are not available [Citation12,Citation13].
Apart from proteinaceous biomarkers, other promising biomarkers include cell-free DNA (cfDNA) and circulating tumour cells (CTCs). cfDNA are fragments of extracellular DNA released in the blood by both healthy and cancerous cells. Secretion levels elevate as the cancer progresses and therefore measuring cfDNA levels is a promising indication of disease screening and diagnosis [Citation39]. cfDNA are also highly sensitive biomarkers as they are associated with tumour type, stage and size. Furthermore, isolation of cfDNA from patient blood allows genetic testing to identify oncogenes and determine a more personalized screening and diagnosis evaluation with an appropriate reference database [Citation58]. As genetic analysis is still costly and complex, cfDNA analysis may not be an appropriate screening technique; although, it could be more relevant when it comes to screening of genetically predisposed individuals. CTCs are established biomarkers for various cancers. In fact, CellSearch® is an FDA-approved test to isolate CTCs from blood samples and determine patient prognosis and survival for breast, colorectal and prostate cancers [Citation59]. In terms of CTC for gynaecological cancer detection, a few LoC devices have been fabricated for the purpose, such as the biomimetic microfluidic system (BMS) by Zhang et al. (), which uses aptamer-linked magnetic nanoclusters to collect ovarian cancer biomarker EpCAM-positive CTCs from blood samples () [Citation38]. However, CTCs play a role in cancer metastasis and their levels are not elevated until late stages of the disease. Consequently, CTCs are not reliable markers for early disease detection and hence unsuitable for screening and early diagnostic purposes [Citation60].
Again, due to low incidence, the search for biomarkers specific to vulval and vaginal cancer is not as prominent. Also, physical examinations can be requested during cervical screenings to screen for abnormal cell growths in these parts [Citation12]. Furthermore, although endometrial incidence is high, mortality rate is relatively low, and the overall prognosis is good [Citation16,Citation61]. Hence, research into biomarkers for the early detection of endometrial, vulvar and vaginal cancers is uncommon.
Lab-on-a-chip device design: biomarker capture and detection
The most common method for trapping disease biomarkers for detection, within microfluidic devices is through antibody capture. Antibodies are proteins that are relatively easy to integrate within a microfluidic structure and engineerable to be highly specific to target biomarkers for in situ detection [Citation35,Citation62]. In such systems, antibodies are often immobilized on a sensing platform, or on the surface of microfluidic channels and the sample perfused or introduced as a droplet in the sensing platform to promote binding of the biomarker [Citation63]. The captured biomarker levels can be quantified through electrical, optical or chemical sensing methods.
Numerous LoC biosensors use antibody-coated nanoparticles for biomarker capture [Citation37,Citation64]. The unique surface chemistry, electrical properties and comparable size range of nanoparticles to target biomolecules improve biosensing efficiency. Noble metal-based nanoparticles, including gold, silver and platinum, are biocompatible, which enables them to bond with various functional groups, for example, proteins, ligands, peptides, DNA, fatty acids and plasmids [Citation65]. Gold nanoparticles show promise for biosensing due to their high stability and biocompatibility, which are ideal for integration in microfluidic biosensors [Citation37,Citation49,Citation66]. For instance, Nunna et al. used gold nanoparticles to enhance the sensor signal response and provided experimental results of the capacitance difference during CA125 antigen–antibody conjugation at multiple concentrations of CA125 antigens () [Citation37]. However, the economic and environmental impact of using gold nanoparticles, especially, for mass production for national-level screening programmes, will need to be weighed up before their adoption for disease screening technologies [Citation67].
Other types of antibody-coated nanoparticles used for biomarker capture are magnetic beads (immunomagnetic isolation) typically, iron oxide nanoparticles [Citation39]. Magnetic beads are cheaper and more easily available than gold but more laborious as magnetic field gradients are necessary to collect the captured biomarkers to perform analysis. For example, the LoC device developed by Cheng et al., uses cfDNA-probe-coated magnetic beads for BRCA1 detection in ovarian cancer (; ) [Citation39]. The process comprises of several successive steps on-chip: (i) plasma samples are mixed with magnetic beads to capture the cfDNA; (ii) the cfDNA-bead complexes are then retained within the device using an external magnetic field; (iii) samples are washed to remove any unbound material; (iv) finally, a quantitative PCR of eluted cfDNA is performed.
Microfluidic channels can also be functionalized with antibodies, though antibody stability can be weak and may require reinforcement strategies for optimal biomarker capture and detection. For example, Zhao et al. integrated Zinc to enhance signal detection and antibody stability within the microchannels of the microfluidic device [Citation48]. The most common method to detect the captured antibodies is through fluorescence. Fluorophores are effective signal-emitting compounds, but they require specialized imaging platforms to be visualized and analysed, which will be unsuitable for PoC devices [Citation68,Citation69]. For instance, Cetin et al. fluorescently labelled cells with fluorescein diacetate to detect relevant CTCs captured by EpCAM antibodies immobilized on gold surfaces [Citation46]. However, a fluorescent microscope was necessary to visualize the captured CTCs, which is an unfavourable requirement for mass screening programmes especially, for potential at-home testing.
Another optical detection method is chemiluminescence where light is emitted, similar to fluorescence, but through a chemical reaction, usually with horseradish peroxidase (HRP)-conjugated secondary antibodies. As shown by Fan et al., a multi-step process to detect ovarian cancer-associated biomarker, AFP is fabricated, where primary antibodies were first introduced in microchannels followed by samples containing the antigen, and finally secondary antibodies (HRP-conjugated secondary antibodies) that generates a chemiluminescent signal readout. However, several calibrations are required to standardize the procedure and identify the LOD, which requires qualified and experienced personal to operate [Citation50].
Electrochemical detection is less common but offers accurate numerical results [Citation70]. In this case, the sensing probe is usually an electrode, and the output signal is a change in voltage or current that can be associated to the presence of the target biomarker. Multiple self-testing tools incorporate electrochemical sensors to successfully measure analyte levels, such as the Freestyle Libre (Abbott, Chicago, IL) [Citation71] patch for glucose monitoring in diabetic patients, therefore, electrochemical microfluidic devices may hold potential for self-testing clinical tools for gynaecological cancer biomarker assessments as well.
Sample type for microfluidic screening and diagnosis
The sample type used to investigate device functionality and performance is a critical factor to consider when validating new devices prior to clinical care. Some devices from , such as those by Zhao et al. [Citation48], Fan et al. [Citation50] and Bahavarnia et al. [Citation45], use antigen solutions of the target biomarker for pre-clinical testing of the device. Although, there is effective capture and sensing of the biomarker tested on the LoC, antigen solutions are irrelevant for assessing clinical performance – concentrations and compositions of antigen solutions differ from biological samples, which are to be the target sample type for clinical testing. Cell culture-derived samples are better suited than antigen solutions for testing and validation, as performed by Cetin et al. [Citation46,Citation47,Citation51], as cancer cell lines offer better molecular representation of the disease. However, actual patient samples of interest are the most ideal – by using patient samples, the device’s performance can be evaluated under real-world conditions, providing an accurate assessment of the effectiveness and accuracy of the screening and diagnostic tests being developed.
Patient samples, such as blood and urine, hold great promise for screening and diagnostic tests due to their ability to be obtained through minimally invasive methods. Many devices from , such as those by Wang et al. [Citation39,Citation49], successfully use blood serum or plasma to detect disease biomarker levels for device validation, demonstrating that microfluidic LoCs are effective with blood derivatives for disease detection. However, the aim for more patient-friendly (and eventually self-testing) LoC devices can be achieved by using non-invasive samples, such as sputum, urine, stool and tears. Only when such samples are not ideal for biomarker detection, more invasive samples such as ascites and blood should be considered. Nonetheless, urine is a preferred and highly investigated sample to test for cancers and other diseases given its ease of collection in relatively large volumes as well as its cellular content derived from glomerular filtration of plasma, renal tubule excretion and urogenital tract secretions that accurately reflect an individual’s metabolic and pathophysiologic state [Citation72]. Hence, urine holds great potential in gynaecological cancer detection in LoC devices in comparison to other sample types [Citation73].
Performance
Device performance depends on specificity, sensitivity and efficiency of the device for disease detection [Citation74]. This can be assessed using various parameters such as limit of detection (LOD), sample flow rate, efficiency in biomarker detection, and sample residence time. Furthermore, appropriate control samples are necessary to ensure validity of device performance as measured ( details the control samples used for the devices listed). Additionally, calculating the rate of false positives and negatives is essential to understand the clinical significance of the device [Citation74,Citation75] – high sensitivity is essential for screening purposes, to avoid missing potential disease cases (false negatives) and ensure timely treatment while high specificity (in detecting disease type, stage and other associated factors) is essential for diagnosis to facilitate effective treatment planning.
The performance of microfluidic LoCs is influenced by various factors, including the biomarker capture method [Citation65,Citation76]. For instance, microfluidic LoCs with antibody-functionalized microchannels are relatively easier and cheaper to manufacture but tend to be less stable and prone to poorer performance. In contrast, metal nanoparticles, particularly, gold nanoparticles, offer excellent stability and strong biomarker binding abilities enabling high specificity and sensitivity in microfluidic device. For devices relying on continuous sample perfusion, the flow rate is another key factor affecting performance. While a higher flow rate reduces test duration, it can also reduce efficiency of biomarker capture and detection leading to inaccuracy and poor device performance [Citation77]. One route to circumvent this issue is to tailor the flow rate to the microfluidic processing step (sample entry, washing, secondary antibody entry, etc.) to maximize biomarker capture without delaying the other stages. This approach is demonstrated by Li et al. where the device operates at a lower flow rate (10 µL.s−1) when sample is in the antibody chamber (to maximize antibody–antigen interaction) but at a higher flow rate (50 µL.s−1) during washing steps reducing overall residence time of the sample [Citation78].
Multiplex assay
The choice of biomarker(s) is key to effective disease detection [Citation29]. As mentioned previously, the lack of specific and sensitive biomarkers for gynaecological cancers makes it challenging to develop accurate LoC biosensors for clinical screening and diagnosis. Even if LoCs successfully isolate biomarkers rapidly, with minimal sample volume and low LOD, their effectiveness would be compromised without detecting for an appropriate biomarker. One route to overcome this is to expand the biosensor into a multiplex assay. Multiplex assays detect a panel of biomarkers thereby minimizing the occurrence of false positives and false negatives often encountered when relying on a single biomarker [Citation37]. By employing multiplex approaches within a single LoC and combining the read-outs, the accuracy of screening and diagnosis can be significantly improved [Citation29,Citation40,Citation78]. provides detailed examples of such multiplex microfluidic LoCs.
Table 2. List of multiplex microfluidic LoCs for detection of gynaecological cancer biomarkers.
ExoSearch (; ) is a highly promising LoC that detects multiple gynaecological cancer biomarkers from extracellular vesicles subtypes, called exosomes, released by cancer cells in bodily fluids. ExoSearch uses as little as 20 μL of blood sample and can reach 100% capture affinity with immunomagnetic beads [Citation40], achieved by slow flow rates (50 nL.min−1). However, faster, and more practical flow rates also provided satisfactory results, for instance, 1 μL.min−1 resulted in a good exosome capture efficiency of 72% from a 20 μL plasma in just 20 min. Similarly, although the performances of devices by Li et al. [Citation78,Citation79] and the p-BNC [Citation53] (), are highly encouraging, however, without bridging the knowledge gap in terms of biomarker expression profiles at different stages and forms of gynaecological cancers, these devices fail as reliable microfluidic assays for screening and diagnosis. In contrast, the device by Wu et al. [Citation54] (), can differentiate between stages and forms of ovarian cancers. The device is a multiplex microfluidic platform with capture antibody arrays for a large biomarker panel detection using several microscale sample volumes, simultaneously. It allows detection of nine biomarkers associated with ovarian cancers (CA125, HE4, OPN, MSLN, Hsp70, CA153, AFP, IL-6, IL-8) from 2 μL of blood serum samples. The results of the clinical testing to differentiate between stages and type of ovarian conditions using this multi-biomarker panel device was very encouraging: 22 clinical samples (18 ovarian cancer patients of different stages and types and four healthy control samples), all conducted on one chip, were analysed, and then grouped based on the level of the different biomarkers. High levels of OPN, MSLN and Hsp70 were consistent with early-stage ovarian cancer. Based on these findings, 91% of the samples were successfully diagnosed and differentiated between stages using the multi-biomarker panel chip. The LOD is very low (1 pg.mL−1 and 0.01 U.mL−1), which is on average a few hundred times lower than other PoC devices and therefore, more sensitive. However, this is a novel research tool and requires extensive testing with clinical samples to further identify reliable and specific biomarker panels for ovarian cancer differentiation and early detection [Citation54].
Unmet needs
As presented, microfluidic LoCs for cervical cancer detection are an active area of gynaecological cancer research to improve screening and diagnosis protocols. Even cervical cancer, with an existing national screening routine [Citation10], can further benefit from development for screening, such as self- or at-home testing, especially in developing countries. This further development includes the ability to use unprocessed, minimally invasive bodily fluids (a key barrier to patient acceptability of the smear test) as testing samples, such as urine, sputum and whole blood, in a single, portable, analytical device (LoC). Overcoming the need for sample processing for cervical cancer screening tests as well as, other gynaecological cancer detection tests, would help reduce waiting times for clinical appointments, training for personnel, advanced laboratory equipment and reagents to process samples (e.g. centrifuge and anticoagulants are needed to refine whole blood into plasma, which is currently the most common type of testing sample in LoCs for gynaecological cancer detection due to its low complexity in biological composition) and backlogs of tests analysis in medical labs [Citation16,Citation69]. Nonetheless, cervical cancer diagnostic tests are much less researched since cervical cancer prevention (i.e. screening) holds more weight than diagnosis, considering that HPV infection is proven to be a strong predisposing factor for the disease.
Another impediment for integrating LoCs in healthcare systems, and especially in multiplex microfluidic biosensors, is the level of cross-binding or non-specific binding due to the presence of multiple capture elements (e.g. antibodies). Non-specific binding can either intensify or diminish biomarker signal, affecting device performance but this issue can be overcome by applying appropriate negative control samples to establish a background signal [Citation80]. Additionally, most of the LoCs listed in and predominantly quantify biomarker presence through fluorescence. Reading a fluorescent signal requires specific imaging devices for signal quantification and analysis, imposing another challenge in incorporating microfluidic devices in healthcare systems or for at-home testing. Auto-fluorescence also further challenges the use of fluorescently labelled biomarker detection [Citation81]. For quicker and easier readouts, devices with a visual signal (e.g. colour change from specific enzymatic reactions upon biomarker binding) may be more promising strategies [Citation76].
Screening and diagnosis of gynaecological cancers is difficult, time-consuming, and currently performed with generic tests. Cervical cancer is the only gynaecological malignancy with a routine screening test offered, with ovarian cancer posing a great clinical burden due to its inability to be diagnosed early and high mortality [Citation25]. Hence, most researched screening and diagnostic techniques focus on detecting ovarian cancer.
LoC devices are ideal platforms for screening and diagnosis due to their low-cost, ease of use and fabrication, allowing potential commercialization of accurate, self-testing technologies. However, the deficiency of numerous, specific and sensitive markers significantly challenges the development of reliable LoCs worthy of clinical adoption. Devices relying on single biomarkers (), although relatively effective at capturing and quantifying the target biomarker, are inaccurate for early gynaecological cancer detection. For instance, levels of CA125 levels did not change between stages and forms of ovarian cancer samples, demonstrating the importance of additional biomarker information. Multiplex LoCs using multi-biomarker panels have been examined () and show better analysis of gynaecological cancers. Larger panels, as suggested by Wu et al. [Citation54], show ability to differentiate between forms and stages of ovarian cancer although larger clinical testing is required to validate these findings. However, a fine balance between the size of the panel and its impact on complexity, and hence device costs and ease of mass manufacturing, need to be achieved. Most LoCs for gynaecological cancer detection reported in literature are at an early stage of development and hence do not always report on the fabrication and running costs. Moreover, not many LoC devices are tested for reusability and durability, which again significantly impact the overall device costs. However, given that the materials usually used are relatively inexpensive (e.g. polydimethylsiloxane), it is deducible that LoCs would be more cost-effective to the existing screening and diagnostic tests. Furthermore, current screening and diagnostic tests generally require trained personnel as well as specialized equipment (X-ray machines, probes for sample collection, reagents for sedation/anaesthesia, etc.), which further increase costs making them unsuitable for mass screening programmes [Citation82]. Further evidence of the economic efficiency of LoCs over current screening and diagnostic tests may aid the development and integration of LoCs within the healthcare system and provision of more accurate and reliable screening and diagnostic evaluations for gynaecological cancers [Citation83].
Conclusions
In summary, gynaecological cancers are a healthcare burden both within the UK and globally. More effective and specific screening and diagnostic tests will enable early intervention thereby improving quality of life and reducing mortality rates. To introduce a screening or diagnostic test as part of routine healthcare, the benefits must outweigh the costs and risks of testing. Microfluidic LoCs allow cost-effective, rapid and efficient detection of disease biomarkers from minimal sample volumes making them ideal candidates for screening and diagnostic tests. Various LoCs for detecting different gynaecological cancers, are in development. However, there is a clear need for robust clinical validation and overcoming limitation, such as cost, fabrication time, complexity and data interpretation challenges before fully realizing the clinical potential of these tools screening and diagnosis of gynaecological cancers.
Author contributions
SN conceived the ideas, drafted and revised the complete manuscript; HSL conceived the ideas and revised the manuscript (with focus on microfluidics); MDL revised the manuscript (with focus on microfluidics and biosensors); RB revised the manuscript (with focus on the clinical aspects of gynaecology and oncology); SM conceived the ideas, revised the manuscript (with focus on biomarkers), and provided final approval. All authors agree to be accountable for all aspects of the work.
Disclosure statement
The authors report no conflict of interest.
Data availability statement
Not applicable.
Additional information
Funding
References
- Ledford LRC, Lockwood S. Scope and epidemiology of gynecologic cancers: an overview. Semin Oncol Nurs. 2019;35(2):147–150. doi: 10.1016/j.soncn.2019.03.002.
- Fenton CL, McGauran MJ, Richards AM. Menopausal hormonal therapy in gynaecological cancers: an evidence-based approach for clinical management. Aust N Z J Obstet Gynaecol. 2020;60(6):942–945. doi: 10.1111/ajo.13237.
- Walker S, Hyde C, Hamilton W. Risk of uterine cancer in symptomatic women in primary care: case-control study using electronic records. Br J Gen Pract. 2013;63(614):e643–e648. doi: 10.3399/bjgp13X671632.
- Zhao S, Chen L, Zang Y, et al. Endometrial cancer in lynch syndrome. Int J Cancer. 2022;150(1):7–17. doi: 10.1002/ijc.33763.
- Cancer Research UK. Early diagnosis data hub; 2022. Available from: https://crukcancerintelligence.shinyapps.io/EarlyDiagnosis/
- Stewart C, Ralyea C, Lockwood S. Ovarian cancer: an integrated review. Semin Oncol Nurs. 2019;35(2):151–156. doi: 10.1016/j.soncn.2019.02.001.
- Menon U, Karpinskyj C, Gentry-Maharaj A. Ovarian cancer prevention and screening. Obstet Gynecol. 2018;131(5):909–927. doi: 10.1097/AOG.0000000000002580.
- Penny SM. Ovarian cancer: an overview. Radiol Technol. 2020;91(6):561–575.
- Crosbie EJ, Einstein MH, Franceschi S, et al. Human papillomavirus and cervical cancer. Lancet. 2013;382(9895):889–899. doi: 10.1016/S0140-6736(13)60022-7.
- Chrysostomou AC, Stylianou DC, Constantinidou A, et al. Cervical cancer screening programs in Europe: the transition towards HPV vaccination and population-based HPV testing. Viruses. 2018;10(12):729. doi: 10.3390/v10120729.
- Basoya S, Anjankar A. Cervical cancer: early detection and prevention in reproductive age group. Cureus. 2022;14(11):e31312. doi: 10.7759/cureus.31312.
- Shrivastava SB, Agrawal G, Mittal M, et al. Management of vaginal cancer. Rev Recent Clin Trials. 2015;10(4):289–297. doi: 10.2174/1574887110666150923112958.
- Weinberg D, Gomez-Martinez RA. Vulvar cancer. Obstet Gynecol Clin North Am. 2019;46(1):125–135. doi: 10.1016/j.ogc.2018.09.008.
- Low EL, Simon AE, Waller J, et al. Experience of symptoms indicative of gynaecological cancers in UK women. Br J Cancer. 2013;109(4):882–887. doi: 10.1038/bjc.2013.412.
- McCluggage WG. Progress in the pathological arena of gynecological cancers. Int J Gynaecol Obstet. 2021;155(Suppl. 1):107–114. doi: 10.1002/ijgo.13871.
- Lee J, Nair N. The current and future states of screening in gynecologic cancers. Obstet Gynecol Clin North Am. 2021;48(4):705–722. doi: 10.1016/j.ogc.2021.06.001.
- Loud JT, Murphy J. Cancer screening and early detection in the 21st century. Semin Oncol Nurs. 2017;33(2):121–128. doi: 10.1016/j.soncn.2017.02.002.
- Chauhan N. A wrong diagnosis. Indian J Cancer. 2020;57(2):212–215. doi: 10.4103/ijc.IJC_418_19.
- Maxim LD, Niebo R, Utell MJ. Screening tests: a review with examples. Inhal Toxicol. 2014;26(13):811–828. doi: 10.3109/08958378.2014.955932.
- Cancer Research UK. Getting diagnosed with breast cancer; 2023 [cited 2023 Sep 3].
- Hall IJ, Tangka FKL, Sabatino SA, et al. Patterns and trends in cancer screening in the United States. Prev Chronic Dis. 2018;15:e97. doi: 10.5888/pcd15.170465.
- Kelesidis T, Aish L, Steller MA, et al. Human papillomavirus (HPV) detection using in situ hybridization in histologic samples: correlations with cytologic changes and polymerase chain reaction HPV detection. Am J Clin Pathol. 2011;136(1):119–127. doi: 10.1309/AJCP03HUQYZMWATP.
- Nolan T, Hands RE, Bustin SA. Quantification of mRNA using real-time RT-PCR. Nat Protoc. 2006;1(3):1559–1582. doi: 10.1038/nprot.2006.236.
- Westra WH. Detection of human papillomavirus (HPV) in clinical samples: evolving methods and strategies for the accurate determination of HPV status of head and neck carcinomas. Oral Oncol. 2014;50(9):771–779; Chatzistamatiou K, Moysiadis T, Moschaki V, et al. Comparison of cytology, HPV DNA testing and HPV 16/18 genotyping alone or combined targeting to the more balanced methodology for cervical cancer screening. Gynecol Oncol. 2016;142(1):120–127; Bebyn MG, Sledzinska P, Wojtysiak J, et al. HPV RNA and DNA testing in Polish women screened for cervical cancer – a single oncological center study. Eur J Obstet Gynecol Reprod Biol. 2022;268:129–134.
- Nash Z, Menon U. Ovarian cancer screening: current status and future directions. Best Pract Res Clin Obstet Gynaecol. 2020;65:32–45. doi: 10.1016/j.bpobgyn.2020.02.010.
- Meyer LA, Broaddus RR, Lu KH. Endometrial cancer and lynch syndrome: clinical and pathologic considerations. Cancer Control. 2009;16(1):14–22. doi: 10.1177/107327480901600103.
- Stephens S, Chatterjee A, Coles V, et al. The costs of treating vaginal and vulval cancer in England (2009–2015). BMC Public Health. 2020;20(1):453. doi: 10.1186/s12889-020-08545-4.
- Vukovic A, Kuna K, Loncar Brzak B, et al. The role of salivary and serum CA125 and routine blood tests in patients with ovarian malignancies. Acta Clin Croat. 2021;60(1):55–62. doi: 10.20471/acc.2021.60.01.08.
- Dochez V, Caillon H, Vaucel E, et al. Biomarkers and algorithms for diagnosis of ovarian cancer: CA125, HE4, RMI and ROMA, a review. J Ovarian Res. 2019;12(1):28. doi: 10.1186/s13048-019-0503-7.
- Haga Y, Sakamoto K, Egami H, et al. Evaluation of serum CA125 values in healthy individuals and pregnant women. Am J Med Sci. 1986;292(1):25–29.
- Sharma D, Vinocha A. Benign ovarian cysts with raised CA-125 levels: do we need to evaluate the fallopian tubes? J Lab Physicians. 2020;12(4):276–280. doi: 10.1055/s-0040-1722547.
- Albers CE, Ranjit E, Sapra A, et al. Clinician beware, giant ovarian cysts are elusive and rare. Cureus. 2020;12(1):e6753. doi: 10.7759/cureus.6753.
- Burness JV, Schroeder JM, Warren JB. Cervical colposcopy: indications and risk assessment. Am Fam Physician. 2020;102(1):39–48.
- Zhang H, Cui J, Jia L, et al. Comparison of laparoscopy and laparotomy for endometrial cancer. Int J Gynaecol Obstet. 2012;116(3):185–191. doi: 10.1016/j.ijgo.2011.10.022.
- Byrne B, Stack E, Gilmartin N, et al. Antibody-based sensors: principles, problems and potential for detection of pathogens and associated toxins. Sensors. 2009;9(6):4407–4445. doi: 10.3390/s90604407.
- Arshavsky-Graham S, Segal E. Lab-on-a-chip devices for point-of-care medical diagnostics. Adv Biochem Eng Biotechnol. 2022;179:247–265. doi: 10.1007/10_2020_127.
- Nunna BB, Mandal D, Lee JU, et al. Detection of cancer antigens (CA-125) using gold nano particles on interdigitated electrode-based microfluidic biosensor. Nano Converg. 2019;6(1):3. doi: 10.1186/s40580-019-0173-6.
- Zhang F, Wu L, Nie W, et al. Biomimetic microfluidic system for fast and specific detection of circulating tumor cells. Anal Chem. 2019;91(24):15726–15731. doi: 10.1021/acs.analchem.9b03920.
- Cheng YH, Wang CH, Hsu KF, et al. Integrated microfluidic system for cell-free DNA extraction from plasma for mutant gene detection and quantification. Anal Chem. 2022;94(10):4311–4318. doi: 10.1021/acs.analchem.1c04988.
- Zhao Z, Yang Y, Zeng Y, et al. A microfluidic ExoSearch chip for multiplexed exosome detection towards blood-based ovarian cancer diagnosis. Lab Chip. 2016;16(3):489–496. doi: 10.1039/c5lc01117e.
- Sanjay ST, Fu G, Dou M, et al. Biomarker detection for disease diagnosis using cost-effective microfluidic platforms. Analyst. 2015;140(21):7062–7081; Gubala V, Harris LF, Ricco AJ, et al. Point of care diagnostics: status and future. Anal Chem. 2012;84(2):487–515.
- Lee J, Lee SH. Lab on a chip for in situ diagnosis: from blood to point of care. Biomed Eng Lett. 2013;3(2):59–66. doi: 10.1007/s13534-013-0094-y.
- Alva S, Bailey T, Brazg R, et al. Accuracy of a 14-day factory-calibrated continuous glucose monitoring system with advanced algorithm in pediatric and adult population with diabetes. J Diabetes Sci Technol. 2022;16(1):70–77. doi: 10.1177/1932296820958754.
- Sukanya VS, Rath SN. Microfluidic biosensor-based devices for rapid diagnosis and effective anti-cancer therapeutic monitoring for breast cancer metastasis. Adv Exp Med Biol. 2022;1379:319–339. doi: 10.1007/978-3-031-04039-9_13.
- Bahavarnia F, Saadati A, Hassanpour S, et al. Paper based immunosensing of ovarian cancer tumor protein CA 125 using novel nano-ink: a new platform for efficient diagnosis of cancer and biomedical analysis using microfluidic paper-based analytical devices (muPAD). Int J Biol Macromol. 2019;138:744–754. doi: 10.1016/j.ijbiomac.2019.07.109.
- Cetin D, Okan M, Bat E, et al. A comparative study on EpCAM antibody immobilization on gold surfaces and microfluidic channels for the detection of circulating tumor cells. Colloids Surf B Biointerfaces. 2020;188:110808. doi: 10.1016/j.colsurfb.2020.110808.
- Chikaishi Y, Yoneda K, Ohnaga T, et al. EpCAM-independent capture of circulating tumor cells with a 'universal CTC-chip’. Oncol Rep. 2017;37(1):77–82. doi: 10.3892/or.2016.5235.
- Zhao D, Wu Z, Zhang W, et al. Substrate-induced growth of micro/nanostructured Zn(OH)F arrays for highly sensitive microfluidic fluorescence assays. ACS Appl Mater Interfaces. 2021;13(24):28462–28471. doi: 10.1021/acsami.1c04752.
- Wang Y, Xu H, Luo J, et al. A novel label-free microfluidic paper-based immunosensor for highly sensitive electrochemical detection of carcinoembryonic antigen. Biosens Bioelectron. 2016;83:319–326. doi: 10.1016/j.bios.2016.04.062.
- Fan F, Shen H, Zhang G, et al. Chemiluminescence immunoassay based on microfluidic chips for alpha-fetoprotein. Clin Chim Acta. 2014;431:113–117. doi: 10.1016/j.cca.2014.02.003.
- Wang R, Wu J, He X, et al. A sample-in-answer-out microfluidic system for the molecular diagnostics of 24 HPV genotypes using palm-sized cartridge. Micromachines. 2021;12(3):263. doi: 10.3390/mi12030263.
- Voskuil J. How difficult is the validation of clinical biomarkers? F1000Res. 2015;4:101. doi: 10.12688/f1000research.6395.1.
- McRae MP, Simmons GW, Wong J, et al. Programmable bio-nano-chip system: a flexible point-of-care platform for bioscience and clinical measurements. Lab Chip. 2015;15(20):4020–4031. doi: 10.1039/c5lc00636h.
- Wu Y, Wang C, Wang P, et al. A high-performance microfluidic detection platform to conduct a novel multiple-biomarker panel for ovarian cancer screening. RSC Adv. 2021;11(14):8124–8133. doi: 10.1039/d0ra10200h.
- Alsop K, Fereday S, Meldrum C, et al. BRCA mutation frequency and patterns of treatment response in BRCA mutation-positive women with ovarian cancer: a report from the Australian Ovarian Cancer Study Group. J Clin Oncol. 2012;30(21):2654–2663. doi: 10.1200/JCO.2011.39.8545.
- Neff RT, Senter L, Salani R. BRCA mutation in ovarian cancer: testing, implications and treatment considerations. Ther Adv Med Oncol. 2017;9(8):519–531. doi: 10.1177/1758834017714993.
- Mohd Isa S, Md Salleh A, Ismail MS, et al. ADAM9 expression in uterine cervical cancer and its associated factors. Asian Pac J Cancer Prev. 2019;20(4):1081–1087. doi: 10.31557/APJCP.2019.20.4.1081.
- Ignatiadis M, Sledge GW, Jeffrey SS. Liquid biopsy enters the clinic – implementation issues and future challenges. Nat Rev Clin Oncol. 2021;18(5):297–312. doi: 10.1038/s41571-020-00457-x.
- Riethdorf S, O'Flaherty L, Hille C, et al. Clinical applications of the CellSearch platform in cancer patients. Adv Drug Deliv Rev. 2018;125:102–121; Millner LM, Linder MW, Valdes R Jr. Circulating tumor cells: a review of present methods and the need to identify heterogeneous phenotypes. Ann Clin Lab Sci. 2013;43(3):295–304.
- Gkountela S, Castro-Giner F, Szczerba BM, et al. Circulating tumor cell clustering shapes DNA methylation to enable metastasis seeding. Cell. 2019;176(1–2):98–112.e14; Pineiro R, Martinez-Pena I, Lopez-Lopez R. Relevance of CTC clusters in breast cancer metastasis. Adv Exp Med Biol. 2020;1220:93–115.
- Njoku K, Barr CE, Hotchkies L, et al. Impact of socio-economic deprivation on endometrial cancer survival in the North West of England: a prospective database analysis. BJOG. 2021;128(7):1215–1224. doi: 10.1111/1471-0528.16618.
- Gaa R, Menang-Ndi E, Pratapa S, et al. Versatile and rapid microfluidics-assisted antibody discovery. MAbs. 2021;13(1):1978130. doi: 10.1080/19420862.2021.1978130.
- Kim D, Herr AE. Protein immobilization techniques for microfluidic assays. Biomicrofluidics. 2013;7(4):41501. doi: 10.1063/1.4816934.
- Li Q, Tang D, Tang J, et al. Magneto-controlled electrochemical immunosensor for direct detection of squamous cell carcinoma antigen by using serum as supporting electrolyte. Biosens Bioelectron. 2011;27(1):153–159. doi: 10.1016/j.bios.2011.06.034.
- Malekzad H, Zangabad PS, Mirshekari H, et al. Noble metal nanoparticles in biosensors: recent studies and applications. Nanotechnol Rev. 2017;6(3):301–329. doi: 10.1515/ntrev-2016-0014.
- Zhu L, Sun HT, Wang S, et al. Isolation and characterization of exosomes for cancer research. J Hematol Oncol. 2020;13(1):152. doi: 10.1186/s13045-020-00987-y.
- Costanzo H, Gooch J, Frascione N. Nanomaterials for optical biosensors in forensic analysis. Talanta. 2023;253:123945; Hu X, Zhang Y, Ding T, et al. Multifunctional gold nanoparticles: a novel nanomaterial for various medical applications and biological activities. Front Bioeng Biotechnol. 2020;8:990.
- Liu M, Qiu JG, Ma F, et al. Advances in single-molecule fluorescent nanosensors. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2021;13(5):e1716. doi: 10.1002/wnan.1716.
- Qian CN. At-home cancer screening: a solution for China and other developing countries with a large population and limited number of healthcare practitioners. Chin J Cancer. 2017;36(1):68. doi: 10.1186/s40880-017-0235-2.
- Kim JH, Suh YJ, Park D, et al. Technological advances in electrochemical biosensors for the detection of disease biomarkers. Biomed Eng Lett. 2021;11(4):309–334. doi: 10.1007/s13534-021-00204-w.
- Oppel E, Kamann S, Heinemann L, et al. Freestyle libre 2: the new isobornyl acrylate free generation. Contact Dermatitis. 2020;83(5):429–431. doi: 10.1111/cod.13638.
- Harpole M, Davis J, Espina V. Current state of the art for enhancing urine biomarker discovery. Expert Rev Proteomics. 2016;13(6):609–626. doi: 10.1080/14789450.2016.1190651.
- Geng C, Li LC, Yan W, et al. A simple fabricated microfluidic chip for urine sample-based bladder cancer detection. J Micromech Microeng. 2018;28(11):115011. doi: 10.1088/1361-6439/aae016.
- Lavin A, Vicente J, Holgado M, et al. On the determination of uncertainty and limit of detection in label-free biosensors. Sensors. 2018;18(7):2038. doi: 10.3390/s18072038.
- Shreffler J, Huecker MR. Diagnostic testing accuracy: sensitivity, specificity, predictive values and likelihood ratios. StatPearls; 2023.
- Morales MA, Halpern JM. Guide to selecting a biorecognition element for biosensors. Bioconjug Chem. 2018;29(10):3231–3239. doi: 10.1021/acs.bioconjchem.8b00592.
- Chen K, Georgiev TZ, Sheng W, et al. Tumor cell capture patterns around aptamer-immobilized microposts in microfluidic devices. Biomicrofluidics. 2017;11(5):054110. doi: 10.1063/1.5000707.
- Li N, Shen M, Xu Y. A portable microfluidic system for point-of-care detection of multiple protein biomarkers. Micromachines. 2021;12(4):347. doi: 10.3390/mi12040347.
- Xie L, Cao Y, Hu F, et al. Microfluidic chip electrophoresis for simultaneous fluorometric aptasensing of alpha-fetoprotein, carbohydrate antigen 125 and carcinoembryonic antigen by applying a catalytic hairpin assembly. Mikrochim Acta. 2019;186(8):547. doi: 10.1007/s00604-019-3594-3.
- Kohler K, Seitz H. Validation processes of protein biomarkers in serum – a cross platform comparison. Sensors. 2012;12(9):12710–12728. doi: 10.3390/s120912710.
- Goda K, Hatta-Ohashi Y, Akiyoshi R, et al. Combining fluorescence and bioluminescence microscopy. Microsc Res Techn. 2015;78(8):715–722. doi: 10.1002/jemt.22529.
- Nguyen HT, Thach H, Roy E, et al. Low-cost, accessible fabrication methods for microfluidics research in low-resource settings. Micromachines. 2018;9(9):461. doi: 10.3390/mi9090461.
- Gharib G, Butun I, Muganli Z, et al. Biomedical applications of microfluidic devices: a review. Biosensors. 2022;12(11):1023. doi: 10.3390/bios12111023.
