Abstract
This article describes the development of the Parenting Premmies Support Program, a mobile health intervention designed to support mothers during the transitional time following their preterm infant’s discharge from hospital. Examples of how research teams give voice to the target population throughout the development and design of mHealth programs is largely missing from the literature. A detailed description of the steps taken in the development of the mHealth intervention that formed the support program is the intention of this paper. An exploratory, sequential, mixed-methods approach with a three-phase design was conducted. In each phase, the experience and perspectives of mothers of preterm infants were acknowledged and included. Phase one sought women’s accounts of their experience collected in semi-structured interviews (n = 9) and subject to a descriptive content analysis. In the second phase, a collaborative, stakeholder interrogation of issues was conducted to develop content of the mHealth protocol. In this phase, two interdependent procedures were used with two participant panels; a stakeholder panel (n = 10) undertook a series of face-to-face meetings, and a user group panel (n = 18) of women who had birthed a preterm infant up to 12 months before undertook an online Delphi survey. In phase three a pilot implementation of the program was undertaken with women whose preterm infants were being discharged home from hospital. The outcome was an mHealth protocol, a resource designed to support women by giving them information to understand and normalise their experience with their preterm infants, and to help them make decisions which may enhance responsive mothering. Collaborative research integrating user feedback in partnership with experts in the field increases the likelihood the final product will be of value and prove supportive and useful to the target audience.
PUBLIC INTEREST STATEMENT
This article describes the development of The Parenting Premmies Support Program, a mobile health intervention designed to support mothers during the transitional time following their infant’s discharge from hospital. While the use of SMS text-based mHealth interventions is broadly reported, the development and pretesting of mHealth interventions are less transparent and limited in the current literature. Examples of how research teams give voice to the target population throughout the development and design of mHealth programs is also lacking. Collaborative research integrating user feedback in partnership with experts in the field increases the likelihood the final product will be of value and prove supportive and useful to the target audience. A detailed description of the steps taken in the development of the mHealth intervention that formed the support program is provided.
1. Background
Families with a preterm infant form a significant proportion of childbearing families, with more than 15 million (1 in 10) babies born preterm annually, and this number is rising (Blencowe et al., Citation2012; Liu et al., Citation2016). In Australia, 8.7% of babies born are preterm, with the median gestational age for all pre-term births 35 weeks (Australian Institute of Health and Welfare, Citation2020). Preterm birth affects the infant’s health and development in the short, medium and longer term (Lasiuk et al., Citation2013; Whittingham et al., Citation2013). It also impacts mothers (Fenwick et al., Citation2008; Wigert et al., Citation2006), parents, family and the wider community (March of Dimes, PMNCH, Save the Children & WHO, Citation2012; McCormick et al., Citation2011). Meeting the health needs of families with a preterm infant requires responsive health services not only during hospital admission but also once transitioning home.
Parenting in hospital neonatal nursery environments is known to be disruptive, stressful and distressing for mothers; challenging the establishment of a secure infant–parent relationship. These challenges are known to manifest in the transition period following discharge of their infant (Jubinville et al., Citation2012; Premji et al., Citation2012). Transition issues for mothers, their parenting and caregiving, as well as family function continue (Hall et al., Citation2013; Howe et al., Citation2014). Following discharge, mothers have reported feeling overwhelmed with concern for their baby’s health and wellbeing (Goto et al., Citation2010; Griffin & Pickler, Citation2011; Swartz, Citation2005). They may continue to experience depression, anxiety and even symptoms of post-traumatic stress (Gray et al., Citation2013; Howe et al., Citation2014; de Oliveira Dornasbach et al., Citation2014). This may be coupled with difficulties in family functioning triggered by stress, anxiety and life changes (Kaaresen et al., Citation2006; Nagulesapillai et al., Citation2013).
The most recent meta-synthesis of available evidence on parental experience of caring for a preterm infant post-discharge identified that parental concern about caring for their infant after discharge was a theme reflected in each of the 12 studies (Adama et al., Citation2016). The review authors emphasised the need for ongoing research with particular focus on ways in which to address maternal fears and anxieties during this period (Adama et al., Citation2016). These issues highlight the need to support parenting as an important agenda in health promotion (Griffin & Pickler, Citation2011; Rowe & Jones, Citation2010) and examine innovative primary healthcare strategies to support and guide mothers in their mothering role beyond the hospital setting (McCormick et al., Citation2011). A tailored mHealth program, with strong theoretical underpinnings in attachment theory (Bowlby, Citation1969) may afford an opportunity to complement traditional health services for mothers of preterm infants as they transition home from hospital, and mitigate the disruption in maternal confidence and infant bonding.
MHealth is a term used to describe health services (including health promotion and education), delivered using mobile communication technologies. MHealth represents a growing health service type which enables opportunistic engagement and intervention with people or groups who may benefit from extended healthcare support and information (WHO, Citation2011). MHealth follows the use of earlier services using communication technologies such as eHealth and telehealth. Text messaging or short message service (SMS) is the most widely adopted, least expensive, can be individually tailored and facilitates instant delivery and feedback. Mobile communications technology is ubiquitous in contemporary society and has widespread acceptability and use by women of childbearing age.
Within the context of maternal and child health studies and implementation trials have demonstrated improvements in attendance at health centre and outpatient appointments (Chen et al., Citation2008), an increase in the use of clinical and social services (Levine et al., Citation2008), and improved postnatal physical activity (Fjeldsoe et al., Citation2012).
While the use of text-based support programs in health care is well reported, the development and pretesting are not transparent and rarely reported in the literature (Fjeldsoe et al., Citation2012). Recommendation to publish development processes has been made to improve quality of interventions (Whittaker et al., Citation2012). Arguably, careful development and pretesting of content is a vital component in health communication campaigns regardless of the medium (Atkin & Freimuth, Citation2013). Willoughby and Furberg (Citation2015) maintain the importance of empirical testing of content with a targeted “audience” (p. 477) and that feedback in both pre-testing and piloting should be used to modify content. More specifically, the published research reporting SMS message development processes lack explanation of the steps involved in creating messages as well as rigorous evaluations of the quality of the health communication messages (Maar et al., Citation2016).
Whilst examples of how researchers have developed and pretested their mHealth interventions are lacking, mechanisms associated with high-quality mHealth interventions have been highlighted. These include the use of a collaborative research approach (Fjeldsoe et al., Citation2010, Citation2012; Gallegos et al., Citation2014) and iterative refinement and adaptation of the program based on key stakeholder and user input (Armin et al., Citation2017; Nourani et al., Citation2019). This demonstrates there is truth in the belief that because social science research can affect the wellbeing of a social group, members of that group have a place in all aspects of the research (Given, Citation2008). To date, few authors have reported on their intervention development methods and it has been noted that published evaluations rarely provide the level of detail required to replicate an intervention (Fjeldsoe et al., Citation2012).
The aim of the overall study was to design, develop and pilot a mobile health intervention to address needs of mothers in the transition period following their preterm infant’s discharge from hospital. This article will specifically detail the development process of a mobile health intervention designed to provide a responsive MHealth service for mothers of preterm infants during the transition home from hospital.
2. Methods
2.1. Research design
A three-phase, sequential, mixed-methods design (Creswell, Citation2011) was undertaken. In Phase one, accounts of maternal transition experiences following preterm infant hospital discharge were collected and used in Phase two in which a SMS message protocol was developed using a collaborative stakeholder procedure. Phase three was a pilot evaluation of the protocol conducted with mothers undertaking the transition as their preterm infant was discharged home. This manuscript will detail methods for phase one and two only, as these were the development phases of the protocol (piloted during phase three).
2.2. Setting
The study was conducted in South East Queensland, Australia over an eight-month period in 2016. summarises the participants, method, data type (qualitative or quantitative) and analysis method used in each phase.
Table 1. Interaction and interface of qualitative and quantitative methods
2.3. Participants
2.3.1. Phase one
Convenience strategies were used to recruit participants to Phase one and two. Participation invitations were distributed via social media, support groups and websites, such as National Premmie Foundation, Preterm Infants Parents Association (PIPA), BubHub and Mater Little Miracles webpages.
Participant inclusion criteria were mothers, 20 years of age or older, experienced a preterm birth, with a birth weight 1500 grams or greater, born between 30 and 37 weeks completed gestation within the past 12 months. Ability to read and understand English was also required. These criteria set exclusion criteria related to age, specifically women <20, gestation, specifically term birth or completed gestation <30 weeks, and English communication ability. Reasons for exclusion criteria were based on project feasibility and the limits of purposive sampling to achieve adequate results from information-rich participants (Guest et al., Citation2006; Patton, Citation2002). The exclusions of mother’s age and the infant’s gestation relate to key aspects which literature suggests would indicate distinct sets of needs for support.
Adolescent mothers 19 years or younger have a unique set of needs and are often contending with several other challenges associated with age and the developmental demands of adolescence (Kroger et al., Citation2010). Similarly, women who birthed an extremely preterm baby (<30 weeks gestation) were excluded. There are increased risks associated with babies born at an earlier gestation period. Babies born less than 30 weeks’ gestation and less than 1500 gm have higher rates of infant mortality and morbidity compared with babies born at or after 30 weeks (McCormick et al., Citation2011). These babies also have an associated intensive intervention needed for survival that is often ongoing (Vohr et al., Citation2006). Support for these mothers may require specific focus and is beyond the scope of the current study.
2.3.2. Phase two
Two panels were required for the key stakeholder consensus:
Stakeholder panel (n = 10) (expert multi-disciplinary team including Maternal & child health nurses; neonatal nurses; consumers; academics and lactation consultants); Participants were recruited through purposeful sampling methods. The sample was sought from a multi-disciplinary perspective to represent as wide a range of experience and expertise as possible.
User-group (n = 18) (mothers of preterm infants). Participants for the Delphi survey were also a purposive sample. The sample of mothers for the Delphi survey was consistent in terms of the maternal profile of interest to this study but were different participants to those who participated in Phase one. The participants were mothers who had previously birthed a preterm infant and met the inclusion criteria.
2.4. Procedures
2.4.1. Phase one
A single semi-structured interview was conducted with each participating mother (n = 9) to gain women’s understanding of the challenges they faced when their preterm infant was discharged from hospital. The purpose of the semi-structured interview was to gather descriptions of a participant’s views with respect to the situation being studied (Kvale, Citation1983), using flexible questions with prompted enquiry into areas of interest. (Baumbusch, Citation2010) (see appendix 1 for interview guide). A combination of telephone (n = 5) and face-to-face (n = 4) interviews took place each lasting between 45 and 60 minutes.
2.4.2. Phase one data analysis
Descriptive content analysis (Morgan, Citation2001) was employed to analyse semi-structured interview data. Descriptive content analysis is a general term for several different strategies used to analyse text (Vaismoradi et al., Citation2013). Each interview was audio recorded and transcribed verbatim. Analysis sought to identify individual and collective understandings directly related to the challenges, issues and support needs of parenting a preterm infant. The transcribed data were summarised and collated using the descriptive content framework as outlined by Morgan (Citation2001). Significant statements were highlighted, labelled and then grouped together under coded categories using the NVivo Version 10 software programme to assist in the management of the data. This information and the coding of the information were interpreted by labelling responses correlating to the key topic questions in the interview. Collated data were labelled and categories (NVivo nodes) were developed.
For the purpose of this study, rigour was examined in the terms of credibility, trustworthiness and applicability (Hammersley, Citation2008; Noble & Smith, Citation2015). Strategies to ensure credibility and trustworthiness in phase one included participant selection, peer debriefing and the establishment of a coding system for analysis of the semi-structured interviews. Peer debriefing was used to assist in the development of credibility. Sharing the developing concepts and data patterns following initial analysis with the experienced maternal and child health academics that formed the supervision team enabled alternative points of view to be discussed and analysis responsibility resulted. The set questions were asked of all participants in the same order; therefore, the structure and order of the interviews and the questions did not change. This enabled a clear set of well described responses to the specific question.
2.4.3. Phase two procedures
In phase two, two interdependent procedures were conducted using a stakeholder panel and a user group panel to ensure a collaborative, informed approach to develop the structure and content of the message protocol. The content and structure were tested through the joint interpretation of the two groups of stakeholders. Collaborative research reflects a belief that because social science research can affect the wellbeing of a social group, members of that group have a place in all aspects of the research (Given, Citation2008). Collaborative researchers maintain that the overriding rationale for the approach is that it elicits data and analysis that are shared, multi-dimensional and grounded in participants’ experiences (Costley et al., Citation2010). Supporters of collaborative research argue the benefits; that it can produce insights that are of higher quality than traditional research and that the results are likely to have greater credibility with potential users (Given, Citation2008; Thorpe & Holt, Citation2008).
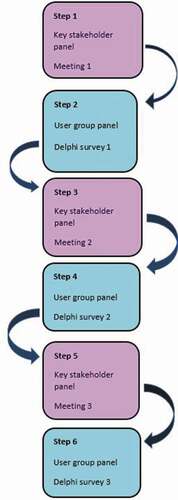
Six steps consisting of two interdependent and alternating procedures, were undertaken, each conducted with a discrete participant group (see ). Procedure One consisted of three key stakeholder panel meetings and Procedure Two involved a three round, online Delphi survey, conducted with a user group panel.
2.4.4. Phase two data analysis
The stakeholder panel took part in three face-to-face, focused meetings (. Steps 1, 3, 5). The user group panel of mothers responded to a three round, online Delphi survey, providing feedback on message themes and content (. Steps 2, 4, 6). The Delphi technique is a quantitative survey procedure aimed at generating consensus (Hsu & Sandford, Citation2007). In three rounds feedback was sought on message themes, content, structure and timing for the protocol. In each survey participants responded to closed items using a 4-point Likert scale (very important, important, not particularly important, not at all important). Round one consisted of 20 items, round two, 74 items and round three, 64 items.
Item content validity index (1-CVI) was used to analyse the responses from each round in the Delphi survey. For each question, the 1-CVI was calculated as the number of participants giving a rating or either 1 (Very Important) or 2 (Important) divided by the number of participants. The level of content validity is dependent on the number of participants and calculated accordingly. 1-CVI is the importance in agreement about relevance with 0.8 or above considered to the limit of acceptability (Polit et al., Citation2007).
Strategies to ensure credibility and trustworthiness in Phase two included triangulation and peer group debriefing for the stakeholder group meetings. The audio from the meetings was used by the researcher to confirm key descriptive decisions which then informed the subsequent step in the process for Phase two. Clarification was sought from the stakeholder panel members at the following meeting to ensure mutual understanding had taken place. The use of Content Validity Index (CVI), the statistic to measure consensus in Delphi surveys. To ensure accurate calculation of this measurement results were generated by a statistical software program thus removing the possibility of human error.
Ethical approval to conduct the study was granted from the Human Research Ethics Committee of the University of the Sunshine Coast (HREC Ethics Approval Number: S/14/720) and the Mater Health Services Research Ethics Committee (HREC/15/MHS/62). All participants provided informed consent and identity kept private and confidential.
3. Results and discussion
3.1. Phase one
Nine mothers were recruited to Phase one, four with twins and five with a singleton pregnancy. All births occurred in Queensland Hospitals, with maternal age ranging from 26 years to 38 years. The infant’s gestation at birth ranged from 31 + 4 weeks to 35 completed weeks. The age of the infants at the time of the interview ranged between 9 weeks to 11 ½ months chronological age. Of the nine mothers six were primiparas (first time mother) and three were multiparas who had birthed a baby or babies before the birth of this premature baby/babies.
The content analysis generated results in 21 categories collated from the five interview topic areas. They are summarised in . Significant challenges identified by participants were concerns about their infants, and self-confidence in their parenting care and decisions. Participants highlighted their need for support and guidance during the transition, particularly in the period immediately following the infant’s discharge, and based on credible and consistent information and resources.
Table 2. Stakeholder panel participants
Table 3. Research question theme and corresponding content topics
The purpose of the first phase in the mHealth protocol/program development was to explore the perspectives of the issue’s mothers face during the transition period following their preterm infant’s discharge from hospital. They reflected on their experience and made suggestions about the sources and type of support that they believed would be helpful to them. This directly informed the development of the message protocol (phase two).
3.2. Phase two
Fundamental topics of discussion and decision-making amongst the key stakeholder panel included identification of the lack of specialised services meeting the needs of preterm mothers, evidenced-based resource provision, promotion of parenting practices aligned with attachment theory and the promotion of maternal instincts and inner mothering wisdom. Four themes were identified by the key stakeholder panel members following the Delphi survey round 1. Messages addressing each of the themes were developed and consensus gained from the user group panel confirmed their relevance and supportive nature. The four themes were:
1) Maternal confidence and wellbeing
2) Professional help and guidance
3) Reassurance about baby
4) Support groups
Messages were adapted in a second version for mothers who birthed two or more preterm infants (twins or triplets). The length of the program and number of messages to be sent each week were determined by the user group panel in the Delphi survey.
The outcome of Phase two was the Parenting Premmies Support Program Protocol. The protocol consisted of 48 SMS messages to be delivered across a four-month period commencing upon discharge of the infant(s). Each mother received the SMS messages as per the message protocol. The mothers received three messages each week, two days apart, delivered at 1000hrs, commencing two days after discharge of their infant/s. Text message character limitation of 160 characters was determined by SMS protocol.
This phase utilised two interdependent procedures to determine the structure and content of the message protocol that formed the Parenting Premmies Support Program. The collaboration process enabled the voice of women who had prior and recent experience in parenting a preterm infant and the collective knowledge of the key stakeholders to come together to develop the message protocol.
4. Discussion
This study has described the development of The Parenting Premmies Support Program which was underpinned by rigorous and transparent methodology. While the use of SMS text based mHealth interventions are broadly reported, the development and pretesting of mHealth interventions are less transparent and limited in the current literature.
To improve future research and program implementation, this research should be accessible for scrutiny, including a description of the development of the SMS content, the theoretical basis of the messages and an analysis of how the content is received by users (U.S. Department of Health and Human Services & Health Resources and Services Administration, Citation2014). Preferably, reporting should include a rationale for the chosen theory, the quality of the evidence on which the messages are based, as well as the fit of the messages within the culture and context of the targeted groups (Waterlander et al., Citation2014).
This study approach embedded the theoretical underpinnings of Bowlby’s attachment theory (Bowlby, Citation1969). Longitudinal benefits have been demonstrated when key components of cue recognition and sensitivity are incorporated into intervention programs with the aim of enhancing maternal–infant interactions (Newnham et al., Citation2009; Ravn et al., Citation2012) which is consistent with attachment theory (Bowlby, Citation1969).
A key objective in the current study was to attend to, document and report the design and development process. The participants provided illustrations of themes that have been previously reported. These included; a lack of confidence in their ability to independently care for their infants. This finding has been reported in earlier research (Murdoch & Franck, Citation2012; Olshtain-Mann & Auslander, Citation2008). Their need to protect and safeguard their infants. Feelings of vulnerability were closely tied with the process of providing protection have also highlighted (Singer et al., Citation2010; Swartz, Citation2005). The importance of sharing and connecting with women who have been through a similar experience has also been identified (Goutaudier et al., Citation2011).
Participants expressed concern for their infants and their own abilities and confidence to assess and care for them, specifically; weight, feeding, sleep and settling. These concerns replicated the findings by Swartz (Citation2005) who found that parental concerns regarding infant health, weight and development were paramount. Apprehension regarding inadequate weight gain and the long-term negative outcomes associated with this has been also been found (Hall et al., Citation2013; Murdoch & Franck, Citation2012) along with uncertainty about the infant’s current health status and possible developmental issues or delay (Gambina et al., Citation2011; Hall et al., Citation2013).
Whilst the mothers felt supported by staff in the neonatal unit, healthcare professionals in the community were perceived as lacking the necessary expertise in the care of premature infants. This desire for consistent information, support and empathy following discharge has been reported previously (Nicolaou et al., Citation2009; de Oliveira Dornasbach et al., Citation2014). The need for social, emotional and professional support following discharge was found also in two recent studies examining the transition from hospital to home (Boykova, Citation2016; Niela-Vilen et al., Citation2014).
Phase one identified many challenges and needs during the period following discharge of their preterm infant. Challenges supported in existing literature included a lack of confidence in their ability to independently care for their infants coupled with a heightened concern about their infant’s weight, feeding, sleep and settling. Lack of expertise from healthcare professionals in the community and a social connection with a supportive peer group was noted.
Fundamental topics of discussion and decision-making amongst the key stakeholder panel in Phase two included identification of the lack of specialised services meeting the needs of preterm mothers, evidenced-based resource provision, promotion of parenting practices known to contribute to the development of secure attachment. Four themes were identified by the key stakeholder panel members following the Delphi survey round 1. Messages addressing each of the themes were developed and consensus gained from the user group panel confirmed their relevance and supportive nature.
The process highlights inclusion and validation of the experiences of the affected population and iterative development characterised by stakeholder collaboration to refine and adapt the product. It has been argued that careful development and pretesting of content is a vital component in health communication campaigns regardless of the medium (Atkin & Freimuth, Citation2013) and empirical testing of content with a targeted “audience” should be used to modify content (Willoughby & Furberg, Citation2015). Adding to the dialogue by reporting these procedures along with evaluation data supports future mHealth researchers to create meaningful interventions.
5. Limitations
The design was well suited to address the research problem as it allowed the research team to explore the topic, establish mothers’ identified needs and challenges, develop the message protocol using a collaborative process. Attention to development and transparent reporting provides the potential for transferability. However, the study was conducted in a single setting and with a small, convenience sample of participants. The protocol acted as a verbal source of information which may act to alter participants’ expectations of their confidence or decision-making; however, findings from the pilot are not reported here.
6. Conclusion
The intention of this study was to clearly describe the rigorous process employed to co-design and develop a mHealth intervention designed to support preterm mothers during their discharge home from hospital. An evidence-based informational resource using contemporary communication technology, designed to support parenting interactions with infants, normalise infant behaviours, caregiving practice and confidence, and provide links to reliable networks and resources resulted. Key aspects of the exploratory multi-phased, mixed-methods research approach enabled the integration of women’s experience and needs, the program to be theoretically informed and collaboratively developed. This study reports formative transparent processes of SMS development which have the potential to improve the quality of mobile health interventions. By incorporating the evaluation and mediating the meaning within a specific demographic target group the quality of the text message-based interventions can enhance quality improving effectiveness.
List of abbreviations
mHealth: Health services delivered using mobile communication technology.
NICU: Neonatal Intensive Care Unit.
SCN: Special Care Nursery.
SFR: Single Family Room.
SMS: Short Message Service.
TAMM: Technology Acceptance Model for Mobile Service.
Authors’ contributions
Each named author has made a significant contribution to the manuscript. KG, JR, MB and LK design, manuscript writing and data analysis.
Availability of data and material
The datasets generated and analysed during the current study are not publicly available due to the ethical approval guidelines – consent was only sought from participants to use the data for this study alone. The data is stored in a secure, password protected file in a re-identifiable format.
Competing interests
The authors have no competing interests to declare.
Consent to publish
Not Applicable
Ethics approval and consent to participate
The study was conducted in accordance with the National Health and Medical Research Council’s guidelines into Human Research [33]. Ethical approval to conduct the study was granted from the Human Research Ethics Committee of the University of the Sunshine Coast (HREC Ethics Approval Number: S/14/720) and the Mater Health Services Research Ethics (HREC/15/MHS/62). Informed consent was obtained in writing from all participants prior to participating in this research study.
Acknowledgements
To the women who participated in this research and gave voice to the experience of mothering a preterm infant. Your willingness to share your stories in an honest and vulnerable way and actively participate throughout this study made this research possible.
Additional information
Funding
Notes on contributors

Kendall George
Dr Kendall George (PhD/MMid/GDip Mid/BNSci) works as a Lecturer in Nursing and Midwifery at the University of the Sunshine Coast, Australia. Kendall also holds a Visiting Research Fellow position at the Sunshine Coast Hospital Health Service and works alongside clinicians using research to improve outcomes in maternal and newborn health. Kendall has a keen interest in the use of innovative technologies to promote health and wellbeing of mothers and babies.
References
- Adama, E. A., Bayes, S., & Sundin, D. (2016). Parents’ experiences of caring for preterm infants after discharge from Neonatal Intensive Care Unit: A meta-synthesis of the literature. Journal of Neonatal Nursing: JNN, 22(1), 27–15. https://doi.org/10.1016/j.jnn.2015.07.006
- Armin, J., Johnson, T., Hingle, M., Giacobbi, P., & Gordon, J. S. (2017). Development of a multi-behavioral mHealth app for women smokers. Journal of Health Communication, 22(2), 153–162. https://doi.org/10.1080/10810730.2016.1256454
- Atkin, C. K., & Freimuth, V. (2013). Guidelines for formative evaluation research in campaign design. In R. E. Rice & C. K. Atkin (Eds.), Public communication campaigns (4th ed., pp. 21–68). Sage.
- Austrailan Institute of Health and Welfare. (2020). Australia’s mothers and babies 2018—in brief. Perinatal statistics series no.36. Cat. no. PER 108. Canberra: AIHW.
- Baumbusch, J. (2010). Semi‐structured interviewing in practice‐close research. Journal for Specialists in Pediatric Nursing, 15(3), 255–258. https://doi.org/10.1111/j.1744-6155.2010.00243.x
- Blencowe, H., Cousens, S., Oestergaard, M. Z., Chou, D., Moller, A. B., Narwal, R., Adler, A., Vera Garcia, C., Rohde, S., Say, L., & Lawn, J. E. (2012). National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: A systematic analysis and implications. Lancet, 379(9832), 2162–2172. https://doi.org/10.1016/s0140-6736(12)60820-4
- Bowlby, J. (1969). Attachment and loss, Vol. 1: Attachment (Vol. 1). Basic Books.
- Boykova, M. (2016). Transition from hospital to home in preterm infants and their families. The Journal of Perinatal & Neonatal Nursing, 30(3), 270–272. https://doi.org/10.1097/jpn.0000000000000198
- Chen, Z.-W., Fang, L.-Z., Chen, L.-Y., & Dai, H.-L. (2008). Comparison of an SMS text messaging and phone reminder to improve attendance at a health promotion center: A randomized controlled trial. Journal of Zhejiang University SCIENCE B, 9(1), 34–38. https://doi.org/10.1631/jzus.B071464
- Costley, C., Elliott, G. C., & Gibbs, P. (2010). Doing work based research: Approaches to enquiry for insider-researchers. SAGE Publications.
- Creswell, J. W. (2011). Designing and conducting mixed methods research (2nd ed.). Sage Publications.
- de Oliveira Dornasbach, J., Barbosa de Freitas, H., Santini Costenaro, R., Filipin Rangel, R., Zamberlan, C., & Ilha, S. (2014). Neonatal intensive care: Feeling of parents after discharge of the child. Journal of Nursing UFPE on Line, 8(8), 2660–2666. https://doi.org/10.5205/reuol.6081-52328-1-SM.0808201412
- Fenwick, J., Barclay, L., & Schmied, V. (2008). Craving closeness: A grounded theory analysis of women’s experiences of mothering in the Special Care Nursery. Women and Birth, 21(2), 71–85. https://doi.org/10.1016/j.wombi.2008.03.006
- Fjeldsoe, B., Miller, Y., & Marshall, A. (2010). MobileMums: A randomized controlled trial of an SMS-based physical activity intervention. Annals of Behavioral Medicine, 39(2), 101–111. https://doi.org/10.1007/s12160-010-9170-z
- Fjeldsoe, B., Miller, Y., O’Brien, J., & Marshall, A. (2012). Iterative development of MobileMums: A physical activity intervention for women with young children. The International Journal of Behavioral Nutrition and Physical Activity, 9(1), 151. https://doi.org/10.1186/1479-5868-9-151
- Gallegos, D., Russell-Bennett, R., Previte, J., & Parkinson, J. (2014). Can a text message a week improve breastfeeding? Bmc Pregnancy And Childbirth, 14(1), 374. https://doi.org/10.1186/s12884-014-0374-2
- Gambina, I., Soldera, G., Benevento, B., Trivellato, P., Visentin, S., Cavallin, F., Trevisanuto, D., & Zanardo, V. (2011). Postpartum psychosocial distress and late preterm delivery. Journal of Reproductive and INFANT Psychology - J REPROD INFANT PSYCHOL, 29(5), 472–479. https://doi.org/10.1080/02646838.2011.653962
- Given, L. M. (Ed.). (2008). The SAGE encyclopedia of qualitative research methods. [SAGE Publications, Inc.]. doi: 10.4135/9781412963909
- Goto, A., Nguyen, Q., Pham, N., Trinh, H., Yabe, J., Sasaki, H., & Yasumura, S. (2010). Associations of psychosocial factors with maternal confidence among Japanese and vietnamese mothers. Journal of Child and Family Studies, 19(1), 118–127. https://doi.org/10.1007/s10826-009-9291-9
- Goutaudier, N., Lopez, A., Séjourné, N., Denis, A., & Chabrol, H. (2011). Premature birth: Subjective and psychological experiences in the first weeks following childbirth, a mixed-methods study. Journal of Reproductive and Infant Psychology, 29(4), 364–373. https://doi.org/10.1080/02646838.2011.623227
- Gray, P. H., Edwards, D. M., O’Callaghan, M. J., Cuskelly, M., & Gibbons, K. (2013). Parenting stress in mothers of very preterm infants — Influence of development, temperament and maternal depression. Early Human Development, 89(9), 625–629. https://doi.org/10.1016/j.earlhumdev.2013.04.005
- Griffin, J., & Pickler, R. H. (2011). Hospital-to-home transition of mothers of preterm infants. Mcn-The American Journal Of Maternal-Child Nursing, 36(4), 252–257. https://doi.org/10.1097/NMC.0b013e31821770b8
- Guest, G., Bunce, A., & Johnson, L. (2006). How many interviews are enough?: An experiment with data saturation and variability. Field Methods, 18(1), 59–82. https://doi.org/10.1177/1525822X05279903
- Hall, E. O. C., Kronborg, H., Aagaard, H., & Brinchmann, B. S. (2013). The journey towards motherhood after a very preterm birth: Mothers’ experiences in hospital and after home-coming. Journal of Neonatal Nursing, 19(3), 109–113. https://doi.org/10.1016/j.jnn.2012.08.002
- Hammersley, M. (2008). Questioning qualitative inquiry. SAGE Publications, Ltd.
- Howe, T. H., Sheu, C. F., Wang, T. N., & Hsu, Y. W. (2014). Parenting stress in families with very low birth weight preterm infants in early infancy. Research in Developmental Disabilities, 35(7), 1748–1756. https://doi.org/10.1016/j.ridd.2014.02.015
- Hsu, C. C., & Sandford, B. A. (2007). The delphi technique: Making sense of consensus. Practical Assessment, Research & Evaluation, 12(10), 1–8. https://doi.org/10.7275/pdz9-th90
- Jubinville, J., Newburn-Cook, C., Hegadoren, K., & Lacaze-Masmonteil, T. (2012). Symptoms of acute stress disorder in mothers of premature infants. Advances in Neonatal Care, 12(4), 246–253. https://doi.org/10.1097/ANC.0b013e31826090ac
- Kaaresen, P. I., Rønning, J. A., Ulvund, S. E., & Dahl, L. B. (2006). A randomized, controlled trial of the effectiveness of an early-intervention program in reducing parenting stress after preterm birth. Pediatrics, 118(1), e9–19. https://doi.org/10.1542/peds.2005-1491
- Kroger, J., Martinussen, M., & Marcia, J. E. (2010). Identity status change during adolescence and young adulthood: A meta-analysis. Journal of Adolescence, 33(5), 683–698. https://doi.org/10.1016/j.adolescence.2009.11.002
- Kvale, S. (1983). The qualitative research interview: A phenomenological and a hermeneutical mode of understanding. Journal of Phenomenological Psychology, 14(2), 171–196. https://doi.org/10.1163/156916283X00090
- Lasiuk, G., Comeau, T., & Newburn-Cook, C. (2013). Unexpected: An interpretive description of parental traumas’ associated with preterm birth. Bmc Pregnancy And Childbirth, 13(s1), 1-10 . https://doi.org/10.1186/1471-2393-13-S1-S13
- Levine, D., McCright, J., Dobkin, L., Woodruff, A. J., & Klausner, J. D. (2008). SEXINFO: A sexual health text messaging service for San Francisco youth. American Journal of Public Health, 98(3), 393. https://doi.org/10.2105/AJPH.2007.110767
- Liu, L., Oza, S., Hogan, D., Chu, Y., Perin, J., Zhu, J., Lawn, J. E., Cousens, S., Mathers, C., & Black, R. E. (2016). Global, regional, and national causes of under-5 mortality in 2000-15: An updated systematic analysis with implications for the sustainable development goals. Lancet, 388(10063), 3027–3035. https://doi.org/10.1016/s0140-6736(16)31593-8
- Maar, M. A., Yeates, K., Toth, Z., Barron, M., Boesch, L., Hua-Stewart, D., Liu, P., Perkins, N., Sleeth, J., Wabano, M. J., Williamson, P., & Tobe, S. W. (2016). Unpacking the Black Box: A formative research approach to the development of theory-driven, evidence-based, and culturally safe text messages in mobile health interventions. JMIR mHealth and uHealth, 4(1), e10. https://doi.org/10.2196/mhealth.4994
- March of Dimes, PMNCH, Save the Children, & WHO. (2012). Born too soon: The global action report on preterm birth. World Health Organization
- McCormick, M. C., Litt, J. S., Smith, V. C., & Zupancic, J. A. (2011). Prematurity: An overview and public health implications. Annual Review of Public Health, 32(1), 367–379. https://doi.org/10.1146/annurev-publhealth-090810-182459
- Morgan, D. L. (2001). Focus group interviewing. In J. F. Gubrium & J. A. Holstein (Eds.), Handbook of interview research (pp. 141–159). SAGE.
- Murdoch, M. R., & Franck, L. S. (2012). Gaining confidence and perspective: A phenomenological study of mothers’ lived experiences caring for infants at home after neonatal unit discharge. Journal of Advanced Nursing, 68(9), 2008–2020. https://doi.org/10.1111/j.1365-2648.2011.05891.x
- Nagulesapillai, T., McDonald, S., Fenton, T., Mercader, H., & Tough, S. (2013). Breastfeeding difficulties and exclusivity among late preterm and term infants: Results from the all our babies study. Canadian Journal of Public Health, 104(4), e351–e356. https://doi.org/10.17269/cjph.104.3803
- Newnham, C. A., Milgrom, J., & Skouteris, H. (2009). Effectiveness of a modified mother-infant transaction program on outcomes for preterm infants from 3 to 24 months of age. Infant Behavior and Development, 32(1), 17–26. https://doi.org/10.1016/j.infbeh.2008.09.004
- Nicolaou, M., Rosewell, R., Marlow, N., & Glazebrook, C. (2009). Mothers’ experiences of interacting with their premature infants. Journal of Reproductive and Infant Psychology, 27(2), 182–194. https://doi.org/10.1080/02646830801922796
- Niela-Vilen, H., Axelin, A., Salanterä, S., & Melender, H.-L. (2014). Internet-based peer support for parents: A systematic integrative review. International Journal of Nursing Studies, 51(11), 1524–1537. https://doi.org/10.1016/j.ijnurstu.2014.06.009
- Noble, H., & Smith, J. (2015). Issues of validity and reliability in qualitative research. Evidence Based Nursing, 18(2), 34. https://doi.org/10.1136/eb-2015-102054
- Nourani, A., Ayatollahi, H., & Mirnia, K. (2019). A smart phone application for the mothers of premature infants. IRBM, 40(5), 263–269. https://doi.org/10.1016/j.irbm.2019.04.006
- Olshtain-Mann, O., & Auslander, G. K. (2008). Parents of preterm infants two months after discharge from the hospital: Are they still at (Parental) risk? Health & Social Work, 33(4), 299. https://doi.org/10.1093/hsw/33.4.299
- Patton, M. Q. (2002). Qualitative research & evaluation methods (3rd ed.). Sage Publications.
- Polit, D. F., Beck, C. T., & Owen, S. V. (2007). Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Research in Nursing & Health, 30(4), 459–467. https://doi.org/10.1002/nur.20199
- Premji, S. S., Young, S. M., Rogers, S. C., & Reilly, S. S. (2012). Transitions in the early-life of late preterm infants: Vulnerabilities and implications for postpartum care. The Journal of Perinatal & Neonatal Nursing, 26(1), 57–68. https://doi.org/10.1097/JPN.0b013e31823f8ff5
- Ravn, I. H., Smith, L., Smeby, N. A., Kynoe, N. M., Sandvik, L., Bunch, E. H., & Lindemann, R. (2012). Effects of early mother-infant intervention on outcomes in mothers and moderately and late preterm infants at age 1 year: A randomized controlled trial. Infant Behavior and Development, 35(1), 36–47. https://doi.org/10.1016/j.infbeh.2011.09.006
- Rowe, J., & Jones, L. (2010). Discharge and beyond. A longitudinal study comparing stress and coping in parents of preterm infants. Journal of Neonatal Nursing, 16(6), 258–266. https://doi.org/10.1016/j.jnn.2010.07.018
- U.S. Department of Health and Human Services & Health Resources and ServicesU.S. Department of Health and Human Services & Health Resources and Services Administration. (2014). Using Health Text Messages to Improve Consumer Health Knowledge, Behaviors, and Outcomes: An Environmental Scan. Retrieved from https://www.hrsa.gov/sites/default/files/archive/healthit/txt4tots/environmentalscan.pdf
- Singer, L. T., Fulton, S., Kirchner, H. L., Eisengart, S., Lewis, B., Short, E., Min, M. O., Satayathum, S., Kercsmar, C., & Baley, J. E. (2010). Longitudinal predictors of maternal stress and coping after very low-birth-weight birth. Archives of Pediatrics & Adolescent Medicine, 164(6), 518–524. https://doi.org/10.1001/archpediatrics.2010.81
- Swartz, K. M. (2005). Parenting preterm infants: A meta-synthesis. MCN, the American Journal of Maternal/Child Nursing, 30(2), 115–120. https://doi.org/10.1097/00005721-200503000-00009
- Thorpe, R., & Holt, R. (Eds.). (2008). The SAGE dictionary of qualitative management research. [Sage Publications Ltd]. https://doi.org/10.4135/9780857020109
- Vaismoradi, M., Turunen, H., & Bondas, T. (2013). Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nursing & Health Sciences, 15(3), 398–405. https://doi.org/10.1111/nhs.12048
- Vohr, B., Poindexter, B., Dusick, A., McKinley, L., Wright, L., Langer, J., & Poole, W. (2006). Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. Pediatrics, 118(1), e115–123. https://doi.org/10.1542/peds.2005-2382
- Waterlander, W., Whittaker, R., McRobbie, H., Dorey, E., Ball, K., Maddison, R., Myers Smith, K., Crawford, D., Jiang, Y., Gu, Y., Michie, J., & Ni Mhurchu, C. (2014). Development of an evidence-based mhealth weight management program using a formative research process. JMIR mHealth and uHealth, 2(3), e18. https://doi.org/10.2196/mhealth.2850
- Whittaker, R., Matoff-Stepp, S., Meehan, J., Kendrick, J., Jordan, E., Stange, P., Cash, A., Meyer, P., Baitty, J., Johnson, P., Ratzan, S., & Rhee, K. (2012). Text4baby: Development and implementation of a national text messaging health information service. American Journal of Public Health, 102(12), 2207. https://doi.org/10.2105/AJPH.2012.300736
- Whittingham, K., Boyd, R. N., Sanders, M. R., & Colditz, P. (2013). Parenting and prematurity: Understanding parent experience and preferences for support. Journal of Child and Family Studies, 23(6), 1050–1061. https://doi.org/10.1007/s10826-013-9762-x
- WHO Global Observatory for eHealth. (2011). mHealth: new horizons for health through mobile technologies: second global survey on eHealth. World Health Organization. https://apps.who.int/iris/handle/10665/44607
- Wigert, H., Johansson, R., Berg, M., & Hellström, A. L. (2006). ‘Mothers’ experiences of having their newborn child in a neonatal intensive care unit. Scandinavian Journal of Caring Sciences, 20(1), 35–41. https://doi.org/10.1111/j.1471-6712.2006.00377.x
- Willoughby, J. F., & Furberg, R. (2015). Underdeveloped or underreported? Coverage of pretesting practices and recommendations for design of text message-based health behavior change interventions. Journal of Health Communication, 20(4), 472–478. https://doi.org/10.1080/10810730.2014.977468