Abstract
Background: The population of Nepal are vulnerable to injuries from natural disasters as well as those occurring in the home, at work and on the roads. Aim: To collate and synthesise the published literature reporting injuries to people of any age resident in Nepal. Method: We searched five electronic databases using an inclusive search strategy. Potentially eligible citations were screened by title and abstract and full texts of studies obtained. Data were extracted by two researchers. Synthesis was reported narratively by injury type and study design. Results: We identified 186 publications reporting 176 unique studies. Most studies used designs likely to underestimate the true burden of disease, including 144 case series and 36 cross-sectional studies. No trials were identified. The largest number of publications were related to poisoning and self-harm with only 22 focussing on road traffic injuries. There was minimal exploration of inequalities in injury occurrence other than descriptive reporting by age and gender. Conclusions: There is limited research using study designs at low risk of bias on injuries occurring to residents of Nepal, even on areas of concern such as road traffic injuries. The findings indicate a lack of robust epidemiological evidence to inform strategic approaches to injury prevention and suggest a need for capacity strengthening for injury prevention research.
PUBLIC INTEREST STATEMENT
People living in Nepal are at risk of being injured in road traffic crashes, at home or work, or from natural disasters such as earthquakes and landslides. Many of the injuries sustained in such events are preventable, but if we want to develop interventions to help keep people safe we first need to understand who is getting injured, how, when and where they get injured. At the start of a large programme of injury research, we reviewed all publications reporting injuries in Nepal. We found a large number of publications, but over three quarters were small studies using records of people attending hospital. This type of study underestimates the true burden of injury as many people do not present to a hospital. We found no studies of interventions to prevent injuries. These findings show the need for training opportunities in Nepal for researchers to produce the evidence that policy makers need.
Competing Interests
None of the authors have competing interests to declare.
1. Background
Injury incidence is highly socially patterned, with the most disadvantaged in society being at the greatest risk of injury. Over 90% of injury mortality occurs in low and middle income countries (World Health Organisation, Citation2014). Nepal has been categorised by the United Nations as one of the “least developed” countries of the world, indicating that it has significant levels of poverty and multiple barriers to development (United Nations, Citation2019) and therefore the population is likely to be at high risk of injury. Establishing effective injury prevention policy requires coordinated cross-government action. However, political instability over the last 30 years since the establishment of democracy has created a turbulent environment for social, political and economic progress in Nepal. The new constitution, enacted in 2018, provides an opportunity for the introduction of safety promoting policy and legislation. .
The preparation and ratification of new policy requires reliable and accurate information to both justify the change and to monitor the effectiveness of the new legislation. However, the collation and reporting of injury data in Nepal is very limited; birth and death registration systems are available but are not mandatory and therefore significantly underreport the population size and causes of death. Consequently, estimates of injury deaths and morbidity are frequently modelled. Road traffic deaths reported to the Nepal Traffic Police in 2015 indicated a fatality rate of 7/100,000 persons (World Health Organisation, Citation2018). In contrast, in the same report, estimates of road traffic deaths by the World Health Organisation for 2016 were 16/100,000 indicating the potential scale of under-reporting from routine sources.
As a landlocked mountainous country, roads are the main method of transportation. There are now over 70,000 km of roads across the strategic and local road networks in Nepal, with an average of 1672 km of new roads being built each year to improve access to rural areas (Government of Nepal, Citation2016). In addition, there were over a million new vehicles registered in the four years to 2016/17 (Government of Nepal, Citation2018), mostly motorcycles. Few roads are built with safety infrastructure, all are at risk of severe weather and seismic events, and many are poorly maintained. Rapid motorisation is associated with increased traffic crash injury rates due to the increased exposure of the population to vehicles, particularly in situations where road infrastructure and safety legislation do not keep pace with the increase in vehicle numbers (Towner & Towner, Citation2009). Nepal is the 46th most vulnerable country in the world to climate change(Notre Dame Global Adaption Initiative, Citation2019) and is prone to natural disasters. The earthquake of April 2015 killed over 9000 people and injured over 22,000 (Petal et al., Citation2017). The disaster illustrated the fragility of the housing and road infrastructure, and the poor level of first aid skills and access to healthcare.
The need to address low levels of capacity for injury prevention in low and middle income countries has been recognised for many years (World Health Organization, Citation2007). In 2017, a collaboration was funded between the University of the West of England, Bristol, UK and Kathmandu Medical College to establish an injury research centre in Nepal (National Institute for Health Research, Citation2017). The primary objective of the centre being to build capacity and capability for injury prevention research. In order to better understand the epidemiology of injuries sustained in Nepal, we conducted a systematic review of published studies reporting injury incidence or outcomes. The rationale for the review was a recognition of the need to understand the volume of work published to date, the range of injury types studied, whether these reflected the burden of injuries sustained, and the quality and methodologies used by researchers.
2. Methods
We searched systematically for studies meeting all of the following inclusion criteria: (i) The population studied were any resident, of all ages, in Nepal; (ii) Outcomes, reported as frequencies, rates or proportions, included injuries of any type (e.g. burn, bite, fracture), consequence (e.g. fatal, non-fatal) or intentionality; (iii) Primary studies of any design whose purpose was to capture numbers or rates of injuries. We included journal articles, conference proceedings and book chapters. We excluded case series containing less than 10 cases, studies reporting only the treatment or management of injuries, and not reporting the prevalence or epidemiology of injuries, studies reporting birth trauma (to infants or mothers) and secondary reports of data published elsewhere. No publication date or language restrictions were applied (two authors, SB and PP are Nepalese and were available to translate documents published in Nepali, and translation services would have been sought for other languages). We used the definition of “an injury” as described by the World Health Organisation, i.e. a bodily lesion resulting from acute exposure to energy (mechanical, thermal, electrical, chemical or radiant) in amounts that exceed the threshold of physiological tolerance, or an impairment of function resulting from a lack of one or more vital elements (i.e. air, water, warmth) as in drowning, strangulation or freezing (Holder & Krug, Citation2001).
We searched five electronic databases in September 2017; MEDLINE (via OVID, 1946 to date), Embase (via OVID, 1947 to date), CINAHL (via EBSCO, 1937 to date), SafetyLit (www.safetylit.org) (1995 to date) and Nepal Journals Online (www.nepjol.info) (2007 to date). We developed a sensitive search history using only free text terms in English for MEDLINE; Nepal* or (name of all 75 districts of Nepal combined with “or”) AND injur* or accident* or wound* or burn* or scald* or fracture* or laceration* or cut* or poison* or trauma* or fall* or drown* or strangulat* or chok* or safe* or harm* or bite* or electrocu* or (road adj (crash*or traffic*)) or crush* or suffocat* or (foreign adj bod*) or asphyxi* or sting* or dislocate* or frostbit* or sprain* or (self-harm* or self harm*) or suicid* (where * indicates a truncated word). The search history was adapted for use in the other databases. The reference lists of systematic and non-systematic reviews identified through the search were searched for additional references.
Results of searches from MEDLINE, Embase and CINAHL were exported to reference management software where results from SafetyLit and NepJOL searches were added manually and duplicates were removed. Screening of the titles and abstracts against the inclusion criteria was completed by one author (MT) and studies clearly failing to meet all inclusion criteria were excluded. Queries were resolved through discussion with a second author (JM). The full texts were obtained for all remaining citations except one where the full text was unavailable. The final list of included studies was determined by a review of the full texts by two researchers (SB, JM). A data extraction form in Microsoft Excel was designed, piloted and amended for extracting the key characteristics of included studies (publication details, study design, setting, data sources, participants age and sex, sample size, methods used, duration of study, type of injury, results). Data were extracted by SB and JM, with discrepancies resolved by discussion. Due to the heterogeneous nature of the included studies and data available, synthesis was reported narratively; describing the burden of injuries overall, and by the commonest injury types. Within each injury type data were summarised by study design; reporting first from experimental studies, then cohort and case control studies and lastly by case series. Strength of evidence was assessed by findings being consistently reported across different populations and settings. Individual study data were extracted in a table categorised by injury type.
3. Results
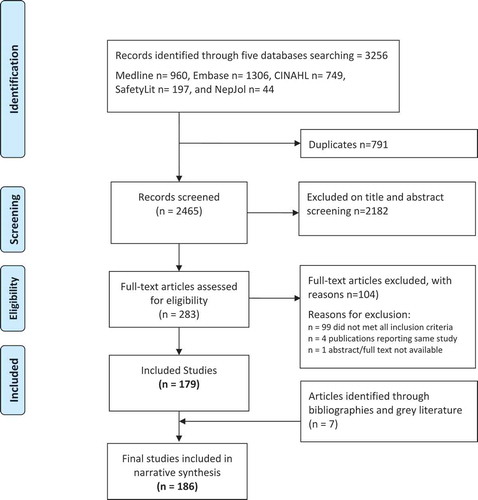
The electronic database searches yielded 3256 papers, with 2465 remaining after duplicates were removed. Following title and abstract screening 283 papers were subject to full text review to identify those meeting the inclusion criteria. Seven additional papers were identified from bibliographies and grey literature sources, resulting in 186 papers reporting 176 unique studies. All included studies were written in English. Figure illustrates the identification of studies. A full list of all included studies is found in Table 1 (supplementary materials).
4. Description of included studies
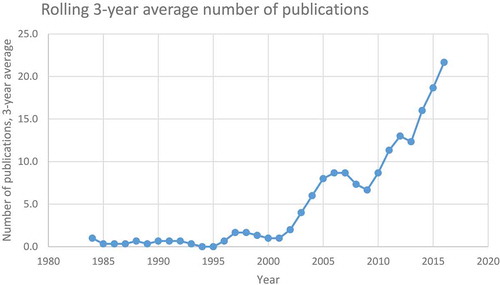
We identified studies published between 1982 and 2017. Prior to 2002 there were, on average, less than one publication per year reporting injury outcomes in Nepal. Numbers have increased steadily since then such that by 2016/17, the 3 yearly rolling average of publications increased to 21.7 (Figure ). The increase may reflect the growing recognition of injury as a public health priority. There was a drop publications between 2006 and 2009.
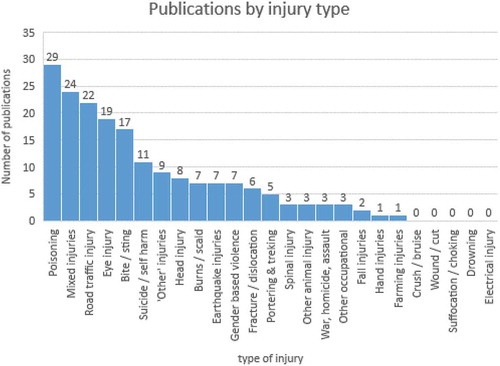
Analysis of publications by injury type (Figure ), indicated that the highest number of publications were for poisoning (29/186, 15.6%). Additionally, there were 11 publications reporting suicide and self-harm, of which eight reported deliberate self-harm by poisoning. The next commonest category was “injuries, unspecified or mixed” (n = 24, 12.9%) which included publications that reported “all” or “any” injuries and did not specify injuries by type. Road traffic injuries were reported in 22 publications (11.8%), followed by eye injuries (n = 19, 10.2%) and bites and stings (n = 17, 9.1%) which were mostly reports of snakebite injuries. Studies reporting other unintentional injury types, such as burns and scalds (n = 7, 3.7%) and falls (n = 2, 1.1%) were seldom published, though falls were commonly the underlying mechanism reported in publications describing head and spinal injuries and fractures. It was noted that no publications were identified specifically reporting drowning, suffocation/choking or electrical/chemical injuries.
Most publications used study designs low in the hierarchy of evidence (Greenhalgh, Citation1997; Guyatt, Sinclair, Hayward, Cook, & Cook, Citation1995) (Figure ); 144 (77%) were case series derived from hospital or clinic records (n = 134) or derived from secondary data analyses of routinely collected police or community based institutional records (n = 10). Thirty-six publications were cross sectional studies, mostly surveys. The authors of these publications seldom acknowledged the limitations associated with the study designs used such as reporting bias and under-reporting. Three case control studies explored risks associated with snakebites (Chappuis, Sharma, Jha, Loutan, & Bovier, Citation2007) and with occupational injuries in children engaged in portering (Doocy, Crawford, Boudreaux, & Wall, Citation2007) and working in brick kilns (Joshi, Dahal, Poudel, & Sherpa, Citation2013). Only one cohort study was identified, which reported the traumatic eye injuries associated with a population-based cohort of 34,902 residents of Bhaktapur followed up between 1992 and 1993 (Upadhyay et al., Citation2001). Only two studies reported an experimental design; one was a before and after study to evaluate the impact on incidence of RTIs and fatalities before and after the introduction of legislation on drink driving (Basnet, Vohra, Bhandari, & Pandey, Citation2013), and the other was a study to explore the feasibility of enabling mothers of preschool children to adopt a community based child safety programme (Pant et al., Citation2015).
Figure 4. Included studies by hierarchy of evidence.
Figure adapted from: “Introduction to EBM” Centre for Evidence Based Medicine, Oxford UK. Available from https://www.cebm.net/cebm-presentations/[Accessed 6 September 2019].
![Figure 4. Included studies by hierarchy of evidence.Figure adapted from: “Introduction to EBM” Centre for Evidence Based Medicine, Oxford UK. Available from https://www.cebm.net/cebm-presentations/[Accessed 6 September 2019].](/cms/asset/ec9ea660-d8ac-4d19-98e0-306bb7618c47/oamd_a_1673654_f0004_oc.jpg)
5. Overall burden of injuries
Nationally representative community-based surveys were few but suggested an incidence of fatal injuries of 42/100,000/year in men and 19/100,000/year in women reported by Sharma ((Citation2006) in a study based on 2001 Census data. Sharma reported suicide and road traffic injuries were the primary causes of death. Non-fatal injury rates were estimated between 28/1,000/year (Gupta et al., Citation2015) and 34/1,000/year (Khanal et al., Citation2017), mostly cuts, falls, road traffic and burn injuries. A predominance of injuries in males compared to females was also found in studies exploring non-fatal injury rates in children where falls were the commonest cause of injury. Six studies reported either prospective or retrospective case series of patients with traumatic injuries seen at hospitals. Injuries accounted for 20–30% of all presentations to hospital, with common causes of being cuts and wounds, RTIs, and falls. Injury events typically occurred on the road (approximately 43%), at home (33–34%) or at work (11–19%) (Bajracharya & Thapa, Citation2012; Joshi & Shrestha, Citation2009).
6. Road traffic injuries
Seven studies reported secondary data analysis of routinely collected traffic police data. Road traffic incident rates increased between 2001 and 2013, from 4/100,000 in 2001–2 to 7/100,000 in 2011–12 (Karkee & Lee, Citation2016). Adhikari analysed 1530 incidents on the Kathmandu to Bhaktapur highway over 3 years; 83% of crashes were reported as due to driver “carelessness”, 10% due to speed, 3% due to vehicle defect, 2% due to alcohol and 2% due to overtaking, suggesting that 97% of RTC were secondary to driver behaviour (Adhikari, Citation2016). Across 11 studies reporting hospital case series of patients with either fatal or non-fatal road traffic injuries consistent findings were that men were about two times more likely to be a victim of an RTI than women, and that most victims were young adults, usually categorised as 15–40 years. Victims were commonly car or motorcycle passengers, pedestrians or motorcycle drivers. Shrestha (Shrestha, Bhatta, Shrestha, Krishna Bahadur, & Paudel, Citation2017) found that 30.4% of RTI victims had health care expenses in excess of 20,000NRs (~£140 or $180). A predominance of working age male victims, often on motorcycles was also found in three studies reporting community-based surveys. Poudel-Tandulkar (Poudel-Tandukar, Nakahara, Ichikawa, Poudel, & Jimba, Citation2007; Poudel-Tandukar, Nakahara, Ichikawa, Poudel, & Wakai, Citation2006) found 23% of 1557 children aged 10–13 years across 14 schools had been hit by a vehicle or motorcycle in the previous 3 months. Basnet (Basnet et al., Citation2013) used an experimental design to explore collisions and injuries the year before and after the introduction of a zero-alcohol limit legislation and an intoxicated driver education programme. Numbers of collisions fell by 22.9% (from 5779 to 4453) and injuries by 23.7% (from 4232 to 3229) over one year.
7. Poisoning
Twenty nine publications reported poisoning; the majority (27/29) were hospital case series reporting admissions or attendances, usually at a single hospital over 1 or more years. The other two studies were cross sectional surveys (Dhimal et al., Citation2017; Gayatri, Amarjeet, & Govinda, Citation2016). Consistent findings across years and settings included; a predominance of young adult patients, with generally more female patients than male (1.1 to 2.0 female to every male patient). Older adult patients appeared more likely to be male and were often farmers or agricultural workers. Most publications reporting the proportion of intentional to unintentional poisoning, described the proportion of intentional poisoning cases to be high; between 58.2% (Khadka & Ale, Citation2005) to 79.6% (Kishore et al., Citation2008). The commonest substances taken were organophosphorus pesticides, particularly Metacid (methyl parathion). In 7 publications reporting only pesticide poisoning case series fatality rates ranged between 3.4% (Bhattarai et al., Citation2006) and 10.1% (Agrawaal & Karki, Citation2014). One publication (Gayatri et al., Citation2016) reported a cross sectional study involving interviews with 125 farmers; 71% reported experiencing symptoms of pesticide poisoning such as skin irritation or headaches, but 82% of these had not sought medical attention suggesting that the seriousness of these symptoms was not appreciated. Five publications reported hospital case series of poisoning in children (Chhetri, Ansari, & Shrestha, Citation2012; Dhakal, Shrestha, Shakya, Shah, & Shakya, Citation2014; Koirala, Rao, Malla, & Malla, Citation2013; Malla et al., Citation2011; Rimal, Tiwari, Ghimire, & Thapa, Citation2017). In children under 5 years of age, most poisoning was unintentional and affected boys, with kerosene and medications being the main substances ingested. For older children, self-harm through ingestion of organophosphorus pesticides was the main reason for admission.
8. Self-harm
Eleven publications reported suicide, near-suicide or self-harm; ten were hospital case series and one (the largest, 2172 cases) was of police reports of successful suicides in persons under 21 years of age, over a 5 year period (Mishra, Shrestha, Poudyal, & Mishra, Citation2013). In this study, the commonest cause of death was hanging (58.8%) followed by self-poisoning (36%). A trigger for the event was only recorded for 551 cases (25.4%); mostly domestic violence (35%), and “mental disorder” (not otherwise specified, 23.9%). Five other studies reported hanging/attempted hanging (Atreya & Kanchan, Citation2015; De et al., Citation2014; Pradhan, Mandal, & Tripathi, Citation2012; Subba et al., Citation2009; Thapa & Carlough, Citation2000). The remaining case series reported suicide or self-harm by poisoning, with the commonest agent being organophosphorus pesticides, followed by rodenticides. Triggers were similar to those for hanging; depression, relationship breakdown, academic failure, financial worries or family dispute.
9. Snake bites
Sixteen publications reported solely snakebite and 2 publications reported snakebites as a larger group of poisoning publications. Estimates of incidence varied with location; Sharma (Sharma et al., Citation2004) surveyed households in Eastern Nepal reporting an annual incidence of 1162/100,000 persons, whilst a household survey by Pandey (Pandey, Citation2007) reported only 110 cases per 100,000 persons per year in a study based in Chitwan, an area in the plains, more centrally located along the southern border with India. In both studies males were more at risk than females and cases increased in the monsoon. This pattern was replicated in 12 hospital case series, with agricultural workers being highlighted as vulnerable. Chappuis (Chappuis et al., Citation2007) completed a case control study comparing cases of indoor snakebite when asleep matched to controls from the same village area. Sleeping under a bednet was a strong protective factor (OR 0.02, p < 0.001). Reasons for not using a bed net included poverty and reluctance to use (e.g. not a mosquito troubled area).
10. Burns and scalds
Seven publications; 6 hospital case series and one community cross sectional study (Gupta et al., Citation2015), reported burns and scalds. From the case series; adult injuries were predominantly flame burns, sustained in the home and more likely to occur to women than men. In contrast, a case series of burns in children under 14 years reported more scalds than flame burns (Shrestha, Citation2006). Lama et al. (Citation2015) reported 329 intentional burn patients; 293 self-inflicted and 36 due to assault. Compared with unintentional burn patients admitted over the same period, patients with intentional burns were more likely to be female, younger, have more extensive burns, and a higher mortality (60% vs 22%). Kerosene was often used as an accelerant.
11. Natural disasters
Seven publications reported case series of patients treated following the 2015 earthquake in central Nepal. Four publications were reports from military or voluntary sector field hospitals staffed by personnel from China (Ding, Hu, Zhang, & Wang, Citation2015; Wang et al., Citation2016), India (Chauhan & Chopra, Citation2016) or Singapore (Ho et al., Citation2016). One publication reported patients attending a tertiary hospital in Kathmandu (Bajracharya, Citation2016) whilst two reported patients with spinal injuries admitted to a rehabilitation hospital (Groves, Poudel, Baniya, Rana, & House, Citation2017; Groves, Poudel, Thapa, & Baniya, Citation2016). Consistent findings across publications were that most injuries were secondary to being hit or buried by falling debris or sustaining injuries whilst fleeing. Fractures were the commonest injury requiring surgical intervention. No injuries associated with landslides were reported.
12. Discussion
This literature review is the most extensive collation of published evidence of injuries sustained in Nepal to date. It provides an indication of the overall burden of injuries and describes the available evidence of the epidemiology of specific injury types. Strengths of the review include the sensitive nature of the search strategy used to identify potentially eligible studies, and that data were extracted by two reviewers. Limitations include the fact that the 186 included studies were not formally critically appraised; instead we chose to report the studies by design according to the hierarchy of evidence, affording the greatest weight to those designs at lower risk of bias. “Bias” refers to errors in the way that studies have been designed or conducted, or in the way that results have been analysed or interpreted, that result in the validity of the findings being brought into doubt. Different study designs are at greater or lesser risk of bias (Higgins, Savović, Page, Elbers & Sterne, Citation2019). Those higher in the hierarchy of evidence (e.g. randomised controlled trials) are less likely to have findings at high risk of bias than those lower in the hierarchy (e.g. cross-sectional studies and case series). A focus on bias is helpful as it signposts those who wish to use research to studies where the findings are more likely to approach the truth and are therefore more appropriate as the basis for health care strategy, policy or decision-making. Despite our attempts to be inclusive of all published studies on injuries in Nepal it is possible that some studies have been missed due to the manner in which some study designs are indexed in electronic databases.
The Global Burden of Disease (GBD) study in 2017 estimated the death rates for all types of injuries in Nepal had fallen from 70 per 100,000 (95%UI: 54–83) in 1990 to 56 per 100,000 (95%UI: 45–69) in 2017 (Institute for Health Metrics and Evaluation [IHME], Citation2017). The GBD study relies on data supplied from each country. Therefore, for a country such as Nepal, where there are a limited number of injury data sources and their quality is still improving, data from the GBD study should be interpreted with some caution. GBD estimates fluctuate by year, as illustrated by the increase in 2015 secondary to the earthquake, when the rate rose to 87 per 100,000 (95%UI: 75–100). These estimates of injury are greater than those reported by Sharma following a census study who found rates of 42 per 100,000 in men and 19 per 100,000 in women in 2006 (Sharma, Citation2006). The estimates for transport injuries in the Global Burden of Disease study in 2017 (25 per 100,000 (95%UI: 15–38) are similarly much higher than any reported in RTI publications identified in this review, which may suggest under-reporting of the true burden of RTIs in hospital and police records.
In common with many systematic reviews of injuries, we found different authors used different definitions of an “injury”, and frequently definitions were not clearly reported. This makes it difficult to know whether it is appropriate to compare results from different studies. A good example of this is how different authors have chosen to report case series of poisoning events; with some authors reporting only on the ingestion of poisonous substances, while other authors included the toxic effects of venomous injuries from snakebites along with pesticide ingestion. There has been an increasing trend in the frequency of publication of studies reporting injuries in Nepal, and this is likely to reflect an increasing recognition of non-communicable diseases as an emerging public health burden. However, the predominant methodology used by authors in this review (hospital case series) is at high risk of bias. These studies will only capture patients attending hospitals, and due to the distances people may need to travel to access hospital care, particularly for rural communities in Nepal, these data are highly likely to underestimate the true burden of these injury types. Other observational study designs, such as case control studies and cohort studies were seldom used by authors. This review failed to identify any randomised controlled trials of interventions to prevent injuries in Nepal and identified only two studies using experimental methods; one before and after study (Basnet et al., Citation2013) and one feasibility study (Pant et al., Citation2015). In contrast, He and colleagues (He et al., Citation2014) in a similar study in China designed to explore the quality and quantity of injury prevention research, identified 25 randomised controlled trials of injury prevention interventions published over the ten years to 2010. The authors were critical of the poor reporting of methods in the majority of these trials. The lack of experimental trials in Nepal indicates that injury prevention research is in its infancy in this country. The very limited publication of study designs above case series in the hierarchy of evidence may reflect a lack of funding to conduct these more expensive study designs but may also indicate a need for greater capacity development and research training to conduct such studies.
The number of publications reporting different types of injuries appears to be dependent upon both researchers’ interest in particular injury types and in their desire to publish, rather than reflecting the true burden of injuries. For example, in this review we identified a relative paucity of research on road traffic injuries despite stakeholders and colleagues reporting that road traffic injuries were the injury type causing greatest concern and burden to the health system in Nepal. In addition, there was an absence of any publications for some injury types such as drowning, though we welcome the recent publication of a study of drowning by Sedain and Pant (Sedain & Pant, Citation2018) since our search was completed. The categorisation of publications by injury type was sometimes problematic. For example, papers reporting poisoning often included intentional and unintentional poisoning cases together (or did not report intentionality at all). The epidemiology of intentional and unintentional poisoning are quite different, as is the epidemiology of poisoning by chemical ingestion and snakebite which were also reported together. Establishing who is at risk of different causes of poisoning, and under which circumstances, is essential in order to develop targeted interventions for prevention and first response.
Other than descriptions of injury cases by gender and age, we identified very little evidence describing inequalities in injury incidence. It is clear from research in other countries that injury occurrence is socially patterned, with those who are most disadvantaged being at the greatest risk of being injured. However, we found almost no reporting of injuries by ethnic group, geographical area (rural/urban, mountain/hill/plains, or other geographical measures of deprivation), type of residence or income level, suggesting that there is significant need to generate the evidence that will highlight such inequalities and enable them to be addressed. As we continue to improve our prevention and management of infectious diseases, the relative burden of injuries in Nepal is likely to increase, yet without routine measurement and reporting of variables illustrating inequalities in injury occurrence, there is a risk that these inequalities will remain unrecognised and even increase.
13. Conclusions
This literature review has identified a large number of publications reporting injuries in Nepal, indicating a growing interest to generate evidence of the epidemiology and burden in this country. However, the lack of methodologies at low risk of bias may indicate an opportunity for training in research methods and may illustrate a need for research grant investment. There is currently a weak and limited evidence base regarding the burden of injuries in Nepal and a poor understanding of who is at risk to inform political, legal and public health decision making.
What is already known on this subject
The global burden of injuries is known to be greatest in low income countries such as Nepal.
Nepal is particularly vulnerable to injuries associated with natural disasters, and the rapid increase in road building and vehicle registration increases the risk of road traffic injuries.
What this study adds
The large volume of literature published on injuries in Nepal comprises mostly hospital case series and cross sectional studies; study designs at high risk of ascertainment bias and under-reporting of the true burden of disease.
There is a relative paucity of evidence for injuries perceived as prevalent (e.g. road traffic injuries) and an absence of evidence for some injury types (e.g. electrical injury).
There has been minimal exploration of inequalities in injury occurrence other than basic reporting of injuries by age and sex.
Author contributorship
All authors qualify for authorship of this manuscript; JM conceived the study, supported the citation searches, oversaw the identification of eligible studies, was second author on data extraction, led the synthesis and drafted the manuscript. MT helped prepare the protocol, led the citation searches, conducted the title and abstract search for eligible studies. SB helped develop the protocol, supported the searches and initial identification of eligible studies, led the full text review stage and data extraction. PRP supported development of the protocol, the citation search and identification of eligible studies. All authors contributed to subsequent drafts of the manuscript.
Data sharing
Only published data were included in this systematic review.
Patient consent
Only published, anonymised and collated data on patient outcomes was used in this research.
Ethical approval
All data used in this research were in the public domain. No ethical approval was required.
Supplymental material
Supplemental data for this article can be accessed here.
Supplemental Material
Download PDF (696.2 KB)Acknowledgements
We acknowledge the support of librarians at the University of the West of England, Bristol and Alessandra Perugini for support in preparing the manuscript for submission.
Additional information
Funding
Notes on contributors
J.A. Mytton
Julie Mytton, is Professor of Child Health at the University of the West of England, Bristol, UK. Julie trained in medicine at St Bartholomews Hospital Medical College, London. She worked in Primary Care and Community Paediatrics before specialising in Public Health. Her research interests are in global health, injury prevention, policy change and building capacity for injury research.
References
- Adhikari, G. P. (2016). Road traffic accidents (RTAs) trends on Kathmandu-Bhaktapur road after addition of lanes. Open Journal of Civil Engineering, 6(03), 388. doi:10.4236/ojce.2016.63033
- Agrawaal, K. K., & Karki, P. (2014). Clinico-epidemiological study on pesticide poisoning in a tertiary care hospital in Eastern Nepal. Journal of the Nepal Medical Association, 52(196), 972–13.
- Atreya, A., & Kanchan, T. (2015). Clinico-epidemiological study of near-hanging cases–An investigation from Nepal. Journal of Forensic & Legal Medicine, 33, 35–38. doi:10.1016/j.jflm.2015.04.001
- Bajracharya, A. R. (2016). Earthquake 2015 in Nepal, an experience at Bir hospital, Kathmandu. Injury Prevention, 22(Suppl 2), A80–A. doi:10.1136/injuryprev-2016-042156.218
- Bajracharya, A. R., & Thapa, B. (2012). Injury surveillance at BIR hospital, Kathmandu, Nepal–Initial 1 year report. Injury Prevention, 18(Suppl. 1), A225–A6. doi:10.1136/injuryprev-2012-040590w.4
- Basnet, B., Vohra, R., Bhandari, A., & Pandey, S. (2013). Road traffic accidents in Kathmandu–An hour of education yields a glimmer of hope. Scandinavian Journal of Trauma, Resuscitation & Emergency Medicine, 21, 19. doi:10.1186/1757-7241-21-19
- Bhattarai, N., Rauniyar, A., Chaudhary, D., Jaiswal, S., Banthia, P., & Rana, B. B. S. (2006). Patterns of organophosphorous poisoning attending a teaching hospital. Journal of the Nepal Medical Association, 45(162), 228–232.
- Chappuis, F., Sharma, S. K., Jha, N., Loutan, L., & Bovier, P. A. (2007). Protection against snake bites by sleeping under a bed net in southeastern Nepal. American Journal of Tropical Medicine & Hygiene, 77(1), 197–199. doi:10.4269/ajtmh.2007.77.197
- Chauhan, A., & Chopra, B. K. (2016). Deployment of medical relief teams of the Indian Army in the aftermath of the Nepal earthquake: Lessons learned. Disaster Medicine and Public Health Preparedness, 11(3), 394–398. doi:10.1017/dmp.2016.146
- Chhetri, U. D., Ansari, I., & Shrestha, S. (2012). Pattern of pediatric poisoning and accident in Patan hospital. Kathmandu University Medical Journal, 10(39), 39–43. doi:10.3126/kumj.v10i3.8016
- Higgins, J. P. T., Savović, J., Page, M. J., Elbers, R. G., Sterne, J. A. C. (2019). Assessing risk of bias in a randomized trial. In J. P. T. Higgins, J. Thomas, J. Chandler, M. Cumpston, T. Li, M. J. Page, V. A. Welch. (Eds.), Cochrane Handbook for Systematic Reviews of Interventions. Retreived from www.training.cochrane.org/handbook
- De, A., Menezes Ritesh, G., Mukherjee, S., Sathian, B., Subba Sonu, H., De, A., … & Chakraborty, P. K.(2014). An analysis of deliberate self-harm in western development region of Nepal: A hospital based study. Research and Reviews: Journal of Medical and Health Sciences, 3(3S), 127–134.
- Dhakal, A. K., Shrestha, D., Shakya, A., Shah, S. C., & Shakya, H. (2014). Clinical profile of acute poisoning in children at a teaching hospital in lalitpur. Journal of Nepal Paediatric Society, 34(2), 100–103. doi:10.3126/jnps.v34i2.10139
- Dhimal, M., Karki, K. B., Aryal, K. K., Dhimal, B., Joshi, H. D., Puri, S., et al. (2017). High blood levels of lead in children aged 6–36 months in Kathmandu valley, Nepal: A cross-sectional study of associated factors. PloS One, 12(6), e0179233. doi:10.1371/journal.pone.0179233
- Ding, S., Hu, Y., Zhang, Z., & Wang, T. (2015). A contrast study of the traumatic condition between the wounded in 5.12 Wenchuan earthquake and 4.25 Nepal earthquake. Chinese Journal of Traumatology, 18(3), 157–160. doi:10.1016/j.cjtee.2015.08.001
- Doocy, S., Crawford, B., Boudreaux, C., & Wall, E. (2007). The risks and impacts of portering on the well-being of children in Nepal. Journal of Tropical Pediatrics, 53(3), 165–170. doi:10.1093/tropej/fmm004
- Gayatri, K., Amarjeet, S., & Govinda, D. (2016). Pesticide poisoning among commercial vegetable farmers of Chitwan, Nepal. Primary Prevention Insights, 6, 19–25. doi:10.4137/PPRI.S40531
- Government of Nepal. (2016). Department of Local Infrastructure Development and Agricultural Roads; Statistics of Local Road Network (SLRN). Ministry of Physical Infrastructure and Transport. Babarmahal.
- Government of Nepal. (2018). Vehicle registration record. Retrieved from https://www.dotm.gov.np/en/vehicle-registration-record/ . [Accessed 7 October 2019].
- Greenhalgh, T. (1997). How to read a paper: Getting your bearings (deciding what the paper is about). BMJ, 315, 243. doi:10.1136/bmj.315.7102.243
- Groves, C. C., Poudel, M. K., Baniya, M., Rana, C., & House, D. R. (2017). Descriptive study of earthquake-related spinal cord injury in Nepal. Spinal Cord, 55(7), 705–710. doi:10.1038/sc.2017.25
- Groves, C. C., Poudel, M. K., Thapa, B. P. J., & Baniya, M. M. (2016). Spinal cord injuries related to 2015 Nepal earthquakes. Journal of Injury, Function & Rehabilitation, 8, S154–S. doi:10.1016/j.pmrj.2016.07.028
- Gupta, S., Mahmood, U., Gurung, S., Shrestha, S., Kushner, A. L., Nwomeh, B. C., & Charles, A. G. (2015). Burns in Nepal: A population based national assessment. Burns, 41(5), 1126–1132. doi:10.1016/j.burns.2014.11.012
- Gupta, S., Wong, E. G., Nepal, S., Shrestha, S., Kushner, A. L., Nwomeh, B. C., & Wren, S. M. (2015). Injury prevalence and causality in developing nations: Results from a countrywide population-based survey in Nepal. Surgery, 157(5), 843–849. doi:10.1016/j.surg.2014.12.020
- Guyatt, G. S., . D., Sinclair, J., Hayward, R., Cook, D., & Cook, R. (1995). Users guide to the medical literature: IX A method for grading health care recommendations. JAMA, 274(22), 1800–1804. doi:10.1001/jama.274.22.1800
- He, Q. K., Kang, W., Tian, D., Huang, Y., Gao, L., Deng, X., … Hu, G. (2014). Analysis of the quantity and quality of published randomised controlled trials related to injury prevention from 2001 to 2010 in China. Injury Prevention, 20, 148–154. doi:10.1136/injuryprev-2013-040843
- Ho, M. L. L., Lim, J. Z. M., Tan, M. Z. W., Kok, W. L., Zhang, J. R., Tan, M. Y., & Tan, A. C. B. (2016). Humanitarian assistance and disaster relief mission by a tripartite medical team led by the Singapore armed forces after the 2015 Nepal earthquake. Singapore Medical Journal, 57(8), 426–431. doi:10.11622/smedj.2016132
- Holder, Y. P. M., & Krug, E. (2001). Injury surveillance guidelines. Geneva: World Health Organisation.
- Institute for Health Metrics and Evaluation (IHME). (2017). Global burden of disease study 2017 seattle, United States: Global burden of disease collaborative network. Retrieved from http://ghdx.healthdata.org/gbd-results-tool. [Accessed 7 October 2019].
- Joshi, S., & Shrestha, S. (2009). Economic and social burden due to injuries and violence in Nepal: A cross-sectional study. Injury Prevention, 16(Suppl 1), A2–A.
- Joshi, S. K., Dahal, P., Poudel, A., & Sherpa, H. (2013). Work related injuries and musculoskeletal disorders among child workers in the brick kilns of Nepal. International Journal of Occupational Safety and Health, 3(2), 2–7. doi:10.3126/ijosh.v3i2.10271
- Karkee, R., & Lee, A. H. (2016). Epidemiology of road traffic injuries in Nepal, 2001–2013: Systematic review and secondary data analysis. BMJ Open, 6(4), e010757. doi:10.1136/bmjopen-2015-010757
- Khadka, S. B., & Ale, S. B. (2005). A study of poisoning cases in emergency Kathmandu medical college teaching hospital. Kathmandu University Medical Journal, 3(4), 388–391.
- Khanal, V., Upreti, R., Oli, U., Sunny, A., Ghimire, A., & Jha, N. (2017). Prevalence of injury and its associated factors in a rural area of eastern Nepal. Journal of Chitwan Medical College, 6(4), 7–13. doi:10.3126/jcmc.v6i4.16708
- Kishore, P., Paudel, S. P. R., Mishra, D., Ojha, P., Alam, K., & Mishra, P. (2008). Pattern of poisoning cases in a teaching hospital in Western Nepal. Journal of Institute of Medicine, 30(1), 26–34.
- Koirala, D. P., Rao, K. S., Malla, K. K., & Malla, T. (2013). A study of clinical features, management and outcome of organophosphate and carbamate poisoning in children. Journal of Nepal Paediatric Society, 33(2), 85–90. doi:10.3126/jnps.v33i2.7799
- Lama, B. B., Duke, J. M., Sharma, N. P., Thapa, B., Dahal, P., Bariya, N. D. … & Wallace, H. J.(2015). Intentional burns in Nepal: A comparative study. Burns, 41(6), 1306–1314. doi:10.1016/j.burns.2015.01.006
- Malla, T., Malla, K. K., Rao, K. S., Gauchan, E., Basnet, S., & Koirala, D. P. (2011). A scenario of poisoning in children in Manipal teaching hospital. Journal of Nepal Paediatric Society, 31(2), 83–88. doi:10.3126/jnps.v31i2.3634
- Mishra, N., Shrestha, D., Poudyal, R. B., & Mishra, P. (2013). Retrospective study of suicide among children and young adults. Journal of Nepal Paediatric Society, 33(2), 110–116. doi:10.3126/jnps.v33i2.7512
- National Institute for Health Research N. (2017). NIHR global health research group on Nepal injury research. Retrieved from https://www.nihr.ac.uk/funding-and-support/documents/global-health-research/groups/JMytton-Plain%20English%20summary.pdf . [Accessed 7 October 2019].
- Notre Dame Global Adaption Initiative. (2019). Vulnerability country rankings. Retrieved from https://gain.nd.edu/our-work/country-index/rankings/ . [Accessed 7 October 2019].
- Pandey, D. P. (2007). Epidemiology of snakebites based on field survey in Chitwan and Nawalparasi districts, Nepal. Journal of Medical Toxicology, 3(4), 164–168. doi:10.1007/bf03160933
- Pant, P. R., Budhathoki, B., Ellis, M., Manandhar, D., Deave, T., & Mytton, J. (2015). The feasibility of community mobilisation for child injury prevention in rural Nepal: A programme for female community health volunteers. BMC Public Health, 15, 430. doi:10.1186/s12889-015-1783-5
- Pant, P. R., Towner, E., Ellis, M., Manandhar, D., Pilkington, P., & Mytton, J. (2015). Epidemiology of unintentional child injuries in the Makwanpur district of Nepal: A household survey. International Journal of Environmental Research & Public Health, 12(12), 15118–15128. doi:10.3390/ijerph121214967
- Petal, M., Baral, M., Giri, S., Rajbanshi, S., Gajurel, S., Green, R. P., Pandey, B., & Shoaf, K.#x00A0; (2017). Causes of deaths and injuries in the 2015 Gorkha (Nepal) earthquake. Save the Children. Kathmandu.
- Poudel-Tandukar, K., Nakahara, S., Ichikawa, M., Poudel, K. C., & Jimba, M. (2007). Risk perception, road behavior, and pedestrian injury among adolescent students in Kathmandu, Nepal. Injury Prevention, 13(4), 258–263. doi:10.1136/ip.2006.014662
- Poudel-Tandukar, K., Nakahara, S., Ichikawa, M., Poudel, K. C., & Wakai, S. (2006). Relationship between mechanisms and activities at the time of pedestrian injury and activity limitation among school adolescents in Kathmandu, Nepal. Accident Analysis & Prevention, 38(6), 1058–1063. doi:10.1016/j.aap.2006.04.004
- Pradhan, A., Mandal, B. K., & Tripathi, C. B. (2012). Hanging: Nature of ligature material applied and type of hanging according to point of suspension. Nepal Medical College Journal, 14(2), 103–106.
- Rimal, H. S., Tiwari, U., Ghimire, K., & Thapa, M. (2017). Hospital based study of poisoning among children, 1 to 18 years of age in Eastern Nepal. Birat Journal of Health Sciences, 2(1), 138–141. doi:10.3126/bjhs.v2i1.17293
- Sedain, B., & Pant, P. (2018). Status of drowning in Nepal: A study of central police data. F1000 Research, 7(576), 1–14. doi:10.12688/f1000research
- Sharma, G. (2006). Leading causes of mortality from diseases and injury in Nepal: A report from national census sample survey. Journal of the Institute of Medicine, 28, 1.
- Sharma, S. K., Chappuis, F., Jha, N., Bovier, P. A., Loutan, L., & Koirala, S. (2004). Impact of snake bites and determinants of fatal outcomes in southeastern Nepal. American Journal of Tropical Medicine & Hygiene, 71(2), 234–238. doi:10.4269/ajtmh.2004.71.234
- Shrestha, S. R. (2006). Burn injuries in pediatric population. Jnma, Journal of the Nepal Medical Association, 45(163), 300–305.
- Shrestha, V. L., Bhatta, D. N., Shrestha, K. M., Krishna Bahadur, G., & Paudel, S. (2017). Factors and pattern of injuries associated with road traffic accidents in hilly district of Nepal. Journal of Biosciences and Medicines, 5(12), 88–100. doi:10.4236/jbm.2017.512010
- Subba, S. H., Binu, V. S., Menezes, R. G., Kanchan, T., Arun, M., Patil, R. … & Rana, M. S. (2009). Pattern and trend of deliberate self-harm in western Nepal. Journal of Forensic Sciences, 54(3), 704–707. doi:10.1111/j.1556-4029.2009.01040.x
- Thapa, B., & Carlough, M. C. (2000). Suicide incidence in the Lalitpur district of Central Nepal. Tropical Doctor, 30(4), 200–203. doi:10.1177/004947550003000406
- Towner, E., & Towner, J. (2009). Child injury in a changing world. Global Public Health, 4(4), 402–4113. doi:10.1080/17441690802449842
- United Nations. UN least developed countries. (2019). Retrieved from http://unohrlls.org/about-ldcs/
- Upadhyay, M. P., Karmacharya, P. C., Koirala, S., Shah, D. N., Shakya, S., Shrestha, J. K. … & Whitcher, J. P. (2001). The Bhaktapur eye study: Ocular trauma and antibiotic prophylaxis for the prevention of corneal ulceration in Nepal. British Journal of Ophthalmology, 85(4), 388–392. doi:10.1136/bjo.85.4.388
- Wang, J., Ding, H., Lv, Q., Chen, J.-H., Sun, Y.-F., Fan, H.-J., & Liu, Q. L. (2016). 2015 Nepal earthquake: Analysis of child rescue and treatment by a field hospital. Disaster Medicine and Public Health Preparedness, 10(5), 716–719. doi:10.1017/dmp.2016.22
- World Health Organisation. (2014). Injuries and violence: The facts. Geneva, Switzerland: World Health Organization.
- World Health Organisation. (2018). Global status report on road safety. Geneva, Switzerland: World Health Organization.
- World Health Organization. (2007). Preventing injuries and violence. A guide for ministries of health. Geneva, Switzerland: World Health Organization.