ABSTRACT
Climate change poses a concern globally, as it adversely affects planetary and population health. Extreme heat is one of the largest weather-related causes of mortality, projected to cause severe heatwaves and droughts globally. Current research has focused on the effects of outdoor heat exposure on population health risks, leaving a gap in knowledge regarding indoor exposure to extreme heat. This paper presents evidence for the effects of extreme heat, both indoors and outdoors, on non-communicable diseases (NCDs) in the United Kingdom. This study applies a systematic review methodology to identify, quality appraise, extract, and summarize findings from studies reporting on the associations between extreme heat and population health risk of NCDs. The literature search was conducted across six electronic databases. `There were 244 studies identified. Twenty-three studies met the inclusion criteria, of these 16 studies met the quality benchmark. Fourteen studies examined the links between heat exposure and mortality, while the remaining studies focused on emergency hospital admissions and years of life lost. The review highlights a consistent association between exposure to extreme heat and increased risk of mortality. Further research is needed to explore the effects of indoor extreme heat on the incidence of NCDs and related outcomes.
Introduction
The dangers posed by climate change are of global concern, and the evidence of the adverse effects of climate change on the fundamental pillars of health, food, water and the air is well-established (McMichael et al. Citation2008).
Extreme heat has already been reported to be one of the largest weather-related causes of death in high-income countries (Centre for Disease Control and Prevention Citation2019), yet there are predictions of a rise in global temperature by 1.5°C above pre-industrial levels by 2052 (IPCC Citation2018). The UK climate projections under high emission scenarios forecast a rise in outdoor temperature of up to 5.4°C by 2070 (Met Office Citation2021). Estimates have shown that a 2°C rise in temperature would expose 37% of the global population to at least one form of severe heatwave every 5 years and expose nearly 200 million people to severe drought (Carbon Brief Citation2021). The intensity of the built environment amplifies indoor extreme heat conditions when there are extreme outdoor health conditions. Our previous systematic review of the impact of buildings on health and wellbeing also highlighted gaps in the evidence linking overheating in buildings and health (Ige et al. Citation2019, Ige-Elegbede et al. Citation2020)
A historical examination of the aftermath of heatwaves in the UK provides a stark reminder of the devastating impact of climate change. Over 2000 excess deaths were recorded during the 2003 heatwave in England and Wales (Vardoulakis and Heaviside Citation2012). Evidence linking the effect of urban heat islands (UHIs) on mortality consistently suggests an association between elevated temperatures in urban areas and increased mortality rates, particularly during heatwaves. Vulnerable populations, such as the elderly, children, and individuals with pre-existing health conditions, are at a heightened risk of mortality during extreme heat events in urban environments (Heaviside et al. Citation2016). Extreme heat has also been linked to inequalities in excess mortality and morbidity, particularly among older populations and clinically vulnerable groups (Ormandy and Ezratty Citation2016).
The projected increase in temperature along with further temperature impacts of the urban heat island (i.e. a rise in temperature of urban and metropolitan areas relative to rural areas that is predominantly due to human activities) should be important considerations for policy and action on the planning, development and management of our towns and cities. Unsurprisingly, there have been explicit calls by the Health Protection Agency for further research on the quantification of the impact of extreme heat and other extreme events such as flooding on health and wellbeing (Vardoulakis and Heaviside Citation2012). An analysis of the historic and potential impacts of extreme heat on health and wellbeing is a prerequisite for planning mitigative interventions (Maramba et al. Citation2004).
Beyond physical health, extreme heat also has implications for mental well-being. The study by Page et al. (Citation2007) highlighted an association between heatwaves and an increase in hospital admissions for mental health disorders, while Hansen et al. (Citation2018) reported a rise in the incidence of heat-related stress and exacerbations in pre-existing mental health disorders.
Research on the links between extreme heat and non-communicable diseases (NCDs) has been predominantly focused on outdoor ambient temperature and to our knowledge there is no systematic review evidence of the effects of extreme heat in homes on NCDs and related risk factors. This paper will therefore provide a comprehensive systematic review and synthesis of the evidence for the known and projected impacts of exposure to indoor and outdoor extreme heat on population health outcomes between 1990 and 2021 in the UK.
Methods
This study applies a systematic review methodology to apply objective, reproducible and comprehensive search concepts and strategies to identify, critically appraise and summarise empirical studies between 1990 and 2021 reporting the association between heatwaves, extreme heat and the risk of NCDs. The review start date, 1990, was chosen because pollution controls on aerosols produced by dust, pollution, combustion of biofuels and fossil fuels were implemented globally in that year.
Arbuthnott and Hajat (Citation2017), Arbuthnott et al. (Citation2020) and Petrou et al. (Citation2015) provided strong, narrative literature reviews of this area. Narrative literature review is not as comprehensive or reproducible as systematic review, reviewers select studies, apply individual critical evaluation and discussion. Systematic reviews play an important role in informing research evidence base (Moher et al. Citation2009). They provide a formal assessment of using a systematic approach to identify, select and appraise the quality of existing research that meets the inclusion criteria between the dates and to extract and analyse data from these selected studies, limiting the opportunity for studies to be missed or discarded in error.
Search strategy
A list of potentially relevant databases was compiled from existing narrative reviews across similar topics (Arbuthnott and Hajat Citation2017, Tham et al. Citation2020). A search was conducted by JI across six electronic databases (MEDLINE, GreenFILE, Psych INFO, Applied Social Sciences Index and Abstracts, SocINDEX, Allied and Complementary Medicine). The databases were initially searched by title and abstract to identify relevant publications from 1990 to 2021. The search terms were adapted from a recent systematic review (Tham et al. Citation2020). These terms were categorised into three-word groups relating to indicators of indoor and outdoor exposure to extreme heat, health outcomes and population location. Following an initial draft of search terms, subject area experts were contacted to verify and refine the terms. A pilot search was performed by JI in one database (MEDLINE) to test the search strategy and refine the search terms prior to conducting the full search.
The reference lists of the included papers were also manually searched. Additional searches were conducted on Google and Google Scholar to locate potentially eligible studies and grey literature. presents an example of the search strategy developed for the MEDLINE database.
Table 1. Search strategy for extreme heat.
Study selection inclusion/exclusion criteria
The eligibility criteria for inclusion in the final review were studies that i) report on measurable associations between extreme heat and at least one of the health outcomes in ii) published in English language between January 1990 to 2021 with full text in a peer-reviewed journal or nationally recognised stakeholder website iii) contain secondary data from the United Kingdom or its individual countries. Qualitative studies were automatically excluded from this review as the focus of this study is to identify and quantify the impact of extreme heat on the risk of NCDs and to use findings as a basis for economic evaluation (to be reported elsewhere).
Data extraction
Data extraction tables were designed in Microsoft Excel to collate descriptive data from included studies rated strong or moderate. Data on study location, the population of interest, exposure to extreme heat, health outcome(s), quality of available evidence and key findings were all extracted to a data extraction sheet.
Quality assessment
Effective Public Health Practice Project (EPHPP) Tool was used to rate the quality of rigour of studies deemed eligible for full-text inclusion (EPHPP Citation2023). EPHPP is highly recommended for quality rating empirical studies based on construct validity and acceptable content (Jadad et al. Citation1996, Mulrow et al. Citation1997). The tool features six domains for evaluating quality: (i) the likelihood that populations in the study reflect the intended group (selection bias); (ii) the study’s design; (iii) managing confounding elements; (iv) masking of populations and researchers (blinding); (v) the consistency and accuracy of data gathering techniques; and (vi) the presentation of participant withdrawals and dropout rates. Each of these elements received a rating of high, moderate, or low. An overall rating of ‘Strong (S) = 1’, ‘Moderate = 2’ or ‘low = 3’ quality was defined for each study according to the EPHPP data dictionary guidelines.
Results
The initial database search returned 244 studies which were screened for duplicates. Following the removal of 79 duplicates, the remaining 165 studies were screened by titles. 100 of these were excluded for failing to meet the eligibility criteria. The remaining 65 studies were screened by abstract, and 42 studies were excluded at this stage for a lack of focus of the impact of extreme heat on relevant health outcomes. A total of 23 studies were included in the review; further details of the search are summarised in .
All included studies reported using secondary data sources as exposure and outcome variables. Of the 23 studies selected for inclusion, five were rated Strong (S) high quality, while 16 studies were deemed to be of Moderate (M) quality and the remaining seven studies were rated weak quality. Data from studies deemed to be of moderate and high quality were included in the final synthesis.
Population
In terms of study location, the majority of the studies were described as nationwide studies or included data from multiple cities in the UK (n = 10), although there were a few multi-country studies which included data from the UK (n = 6). However, four of the studies were conducted using data from London only, while one study used data collected in the West Midlands region only.
Exposure
There were significant variations in the definition of heat thresholds used across studies, e.g. 93rd percentile of daily mean temperature, average of lags 0–1 (Vardoulakis et al. Citation2014), 91st percentiles of the mean temperature (Arbuthnott et al. Citation2020). Temperature measurements were retrieved from different sources including the air quality monitoring stations and meteorological stations. Only one of the studies included in the review examined the health impacts of extreme heat indoors (Murage et al. Citation2020).
Outcomes
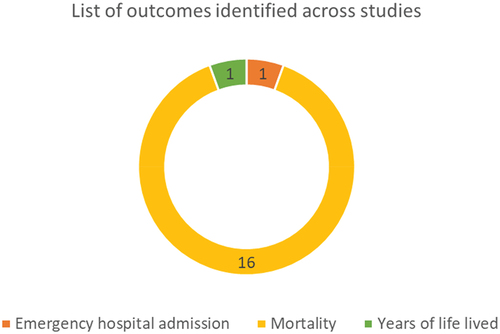
All-cause mortality was by far the most prevalent outcome reported. Other outcomes identified were heat-related/cause specific, suicide, emergency hospital admissions and years of life lost (YLL), .
Mortality
Fourteen studies examined the links between heat exposure and mortality (Pattenden et al. Citation2010, Gasparrini et al. Citation2012, Hajat et al. Citation2014, Vardoulakis et al. Citation2014, Gasparrini et al. Citation2015a, Citation2015b, Petrou et al. Citation2015, Heaviside et al. Citation2016, Zhang et al. Citation2018, Kim et al. Citation2019, Arbuthnott et al. Citation2020, Murage et al. Citation2020, de Schrijver et al. Citation2021, Evangelopoulos et al. Citation2021). The evidence of increased risk of mortality with higher temperatures above threshold levels was consistent across the studies examined except for Gasparrini et al. (Citation2015a) which assessed temporal variations in heat mortality across multiple countries and reported no significant findings ().
Table 2. Main findings from studies on extreme heat and mortality.
The study by Vardoulakis et al. (Citation2014) investigated the relationship between current and future heat exposure and mortality in England and Wales using three Special Report on Emissions Scenarios Low (B1) Medium (A1B) and High (A1FI). Findings showed a 2.5% [95% CI: 1.9, 3.1] increase in mortality per 1°C rise in temperature above the heat threshold [93rd percentile of daily mean temperature]. The authors also predicted a 90% increase in heat-related mortality between the 2020s (n = 1503) and 2050s (n = 2866) under the medium emissions scenario and by approximately 72% between the 2050s (n = 2866) and 2080s (n = 4922). Likewise, the study by Hajat et al. (Citation2014) was conducted to model the projected impacts of temperature exposure and weather variability on mortality in the UK during the 2020s, 2050s and 2080s. The authors reported a 2.1% [95% CI: 1.5 to 2.7] increase in mortality for every 1°C rise in temperature above the heat threshold at the national level. London RR = 1.04 (1.03–1.04) and East Midlands RR = 1.03 (1.02 = 1.03) were the UK regions most vulnerable to heat. Further analysis suggests that the mean estimate of heat-related mortality could increase by approximately 66% (n = 3281), 257% (n = 7,040) and 535% (n = 12,538) in the 2020s, 2050s and 2080s, respectively, from a current baseline of 1974 deaths.
Pattenden et al. (Citation2010) assessed the effects of ozone, heat, and their interaction, on all-cause mortality, cardiovascular and respiratory mortality across 15 conurbations in England and Wales. Findings from the study showed that extreme heat remained independently associated with deaths in all three causal subgroups, with the mean rate ratio for respiratory mortality reaching 1.139 (1.079–1.202), cardiovascular diseases 1.055 (1.025 to 1.087), and all-cause mortality 1.071 (1.050 to 1.093). Arbuthnott et al. (Citation2020) ecological time-series study reported that in London, for each 1°C above the heat threshold the risk of mortality increased by 3.9% [95% CI: 3.5%, 4.3%]. The study by Gasparrini (Citation2012), reported a significant increase in all-cause mortality for a 1°C rise above the England and Wales regional heat threshold RR = 2.1% [95% CI 1.6% to 2.6%]. Among the main causes, the steepest increase in risk was for respiratory mortality 4.1% (3.5% to 4.8%).
Murage et al. (Citation2020) assessed how urban vegetation, housing characteristics and socio-economic factors modify the association between heat exposure and mortality in a large urban area. The authors reported lower daily temperatures in areas with more trees and vegetation cover and where the proportion of properties owned outright was highest, whilst higher daily mean temperatures were recorded in areas with a high proportion of social housing, higher-income deprivation and in areas with a high proportion of non-native English speakers. Although the findings were not always significant, the authors reported the highest odds of death in ports and airport areas (1.149, 0.959–1.376) and the lowest in forested and agricultural land (0.986, 0.848–1.146). Evangelopoulos et al. (Citation2021) looked at the effects of temperature increases on the risk of mortality by the climatic zone of the country of origin for people born outside the UK and reported that UK, tropical and boreal (sub-polar) climate-born people have an increased risk of death from extreme heat, and migrants show little adaptation to their new climate zone. The authors of the study, however, acknowledged potential methodological limitations limiting the power of the study to detect an actual difference if one exists.
The study by Petrou et al. (Citation2015) examined the daily total mortality (DTMORT) from heat exposure in the summer months in Yorkshire and the Humber, West Midlands, North East, North West and South East regions of the UK. Findings showed an increase in DTMORT across all five regions. Another study was conducted by Zhang et al. (Citation2018) to examine the impacts of diurnal temperature range (DTR), which is the difference between the daily maximum and minimum temperature on mortality in England and Wales between 1993 and 2006. Daily DTR varied greatly from 0.8°C to 20.2°C during the study period, but the annual average was 7.3°. DTR extremes (both high and low DTR) exhibited a significant impact on mortality. The authors concluded that there was clear evidence of increased mortality associated with extremely high DTR for all regions except North East, whereas extremely low DTR tended to show some protective effects.
Kim et al. (Citation2019) study investigated the relationship between extreme heat and suicide across multiple countries. Findings from the UK demonstrate a significant relationship between suicide rate and extreme heat in the UK 1.34 (1.22, 1.46) (Kim et al. Citation2019).
The study by Gasparrini et al. (Citation2015b) attempted to quantify the total mortality burden attributable to heat or cold across 13 countries including the UK; the authors reported that the total deaths due to heat in the UK during the study period were 0.3% (0.25%–0.36%).
De Schrijver et al. (Citation2021) conducted a study to critically assess the differences in temperature-related mortality risks and impacts derived from Gridded Climate Datasets (GCDs) and weather stations across two heterogeneous regions (UK and Switzerland). Excess deaths from heat in England and Wales were 2,979 (2,419, 3,493), 2,943 (2,404, 3,465), and 2,906 (2,425, 3,401) for the weather station and local and global GCD, respectively. RR estimates for heat in Greater London were 1.25 (95% CI; 1.19–1.30), 1.24 (95% CI; 1.18–1.29), and 1.26 (95% CI; 1.20–1.33) for the weather station and local and global GCD, respectively.
Urban heat island effect and mortality
The study by Heaviside et al. (Citation2016) investigated the attribution of the Urban Heat Island (UHI) to heat-related mortality in the West Midlands during the heatwave of August 2003 by comparing health impacts based on two modelled temperature simulations. The results suggest that the UHI contributed around 50% of the total heat-related mortality during the 2003 heatwave in the West Midlands. The authors also projected that mortality estimates for a heatwave event similar to that of 2003 could result in a rise in mortality of 53% in the 2020s, 122% in the 2050s and 209% by the 2080s from the baseline of 90 deaths in 2003.
Emergency hospital admission
A study by Kovats et al. (Citation2004) investigated the effects of hot weather and heatwaves on emergency hospital admissions in Greater London, UK. Emergency hospital admissions were stratified by age group and diagnostic groups (cardiovascular disease, respiratory disease, cerebrovascular disease, renal disease, acute renal failure and calculus of the kidney and urethra). Findings were not statistically significant for most of the age groups, but respiratory admissions increased by 10.86% (95% CI = 4.44 to 17.67) for each degree rise in daily mean temperature above 23 degrees in those aged 75 years and above (). The authors also reported that an increase in daily mean temperature above 12°C was associated with increased emergency hospital admissions (0.24% 95%CI = 0.02%–0.46%) in infants and children under 5 years.
Table 3. Main findings from studies on extreme heat and emergency hospital admission.
Years of life lost (YLL)
One study examined the relationship between YLL and temperature in Greater London, West Midlands and Greater Manchester (Arbuthnott et al. Citation2020). Findings () showed that in London, for each 1°C above the heat threshold, the YLL increased by 3.0% (2.5%, 3.5%). A corresponding increase of 1.5% (1.07-2.4%) and 2.4% (1.6-3.3%) was reported for each 1°C temperature increase above the heat threshold for Greater Manchester and West Midlands, respectively.
Table 4. Main findings from studies on extreme heat and YLL.
Discussion
Main findings of this research
The most consistent finding of this review is the impact of extreme heat on mortality. The evidence presented in this review on the projected impacts of extreme heat on mortality is also an important finding with significant implications for future planning.
This review also suggests there is relatively limited evidence on the adverse impact of UHI on mortality in the UK. UHI is a growing problem globally as well as in the UK and could be of greater concern without clear mitigation strategies to promote more sustainable urban development. For example, studies have reported the need for clear guidance for planners on how to mitigate the effects of UHI (O’Malley et al. Citation2014). Anthropogenic heat from vehicular sources also contributes to the urban heat island effect and should be considered in planning (Ebi et al. Citation2021).
Beyond outcomes relating to mortality, however, there was very limited evidence on the impacts of extreme heat on the incidence of NCDs and mental health issues. This is corroborated by findings from existing research which conclude that investigations into the impact of extreme heat on the development of a range of NCDs have received far less attention compared to outcomes relating to deaths (Friel et al. Citation2011).
This review also provides evidence of significant gaps in research on the impact of indoor extreme heat on population health and well-being. A recent review on the effects of indoor temperatures above 24°C on health reported a lack of evidence to establish the link between indoor temperatures and all-cause mortality, heat stroke, hyperthermia, dehydration or hospital admission (Head et al. Citation2018). The lack of reliable longitudinal evidence on indoor heat and health has also been reported in studies conducted within the UK (Anderson et al. Citation2013). A study by A report from the Department of Communities and Local Government (Citation2012) also concluded that although the evidence on the relationship between health impacts and outdoor temperature is well advanced, especially in relation to deaths/hospital admissions during heatwave events, there is a scarcity of longitudinal evidence linking indoor temperatures and health impacts. This highlights the need for further research into the health and well-being impacts of extreme heat indoors.
What is already known about this topic
Extreme heat has previously been reported as a major environmental hazard of global concern (Houghton and English Citation2014). The actual and projected impacts of heat exposure on mortality in the UK have been widely reported in previous literature reviews (Arbuthnott and Hajat Citation2017). Other studies, such as, Wondmagegn et al. (Citation2019) have discussed the global economic burden of heat exposure on health-care systems.
What this study adds
Previous narrative reviews on this topic have literature review methodology (Houghton and English Citation2014, Arbuthnott and Hajat Citation2017, Wondmagegn et al. Citation2019) which is less transparent, less robust and subject to methodological bias. This review utilised a well-established form of evidence synthesis with clear documentation of methods and processes leading to the generation of robust evidence.
This study distinguishes itself by its specific geographic focus at the national level, in contrast to the broader global or regional scopes often seen in existing reviews. The examination of climate change and extreme heat impacts at the country level offers a finer-grained analysis, enabling a more in-depth exploration of their effects on health within unique geographic and sociodemographic contexts. This approach, zooming in on individual countries, yields valuable insights into region-specific vulnerabilities and adaptation strategies, ultimately supporting the development of more precisely targeted policy and public health interventions.
This study also adds to the growing body of evidence calling for more longitudinal and experimental studies to assess the impact of indoor heat exposure on health and well-being (Taylor et al. Citation2018). Findings from this study also highlight the importance of taking a holistic approach to investigating the impacts of extreme heat on a broader range of NCDs including mental health, and respiratory outcomes. It is, however, acknowledged that the detection and attribution of the impacts of extreme heat on the development of NCDs are complex due to the influence and interaction of multiple layers of risk factors (Ebi et al. Citation2020, Mitchell Citation2021). The emergence of advanced tools to evaluate detection and attribution would no doubt prove useful to provide a more robust analysis of the impacts of climate change on NCDs; however, as Ebi et al. (Citation2020) argue, investigating causal links using detection and attribution study designs/tools relies on the availability of long-term data sets.
What this study adds to the UK context
In the UK, the adverse impact of Urban Heat Island (UHI) on mortality appears to be a growing concern, and there is limited evidence connecting it to fatalities (Heaviside et al. Citation2016). Urban development that is sustainable becomes paramount to combat this concern, and the country’s planners require clearer guidance on how to alleviate the effects of UHI. Interestingly, vehicular sources, which contribute to the UHI effect, should also be a focal point when planning urban spaces (Keat et al. Citation2021). This study provides evidence underpinning the need for a better understanding of the links between the indoor and outdoor overheating on health and wellbeing.
Limitations of this study
This review aims to synthesise and appraise existing evidence on the known and projected impacts of extreme heat (indoor and outdoor) on NCDs and related outcomes in the UK. The lack of evidence on the health impacts of indoor extreme heat is a limitation of this study which probably reflects the nature of existing evidence. Another key limitation is that most of the studies included in the review did not necessarily consider the issue of attribution and detection and so makes it difficult to highlight clear causal pathways.
Conclusion
This study aims to provide a comprehensive review of the known and projected impacts of both indoor and outdoor extreme heat on non-communicable diseases (such as diabetes, respiratory illness, cardio-vascular disease, mental health) and related outcomes in the UK. Findings from the review strengthen and provide strong and consistent evidence that extreme heat is associated with increased mortality. However, there is a need to further explore detection and attribution in relation to these findings. The lack of evidence on the health impacts of extreme heat indoors calls for further investigation.
Acknowledgements
The authors would like to acknowledge the invaluable support and guidance received from Daniel Black, Eleanor Eaton and Alistair Hunt in the design and implementation of this study
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Janet Ige-Elegbede
Dr Janet Ige, Dr Paul Pilkington and Professor Jane Powell are members of the Centre for Public Health and Wellbeing at the University of the West of England. Operating within a multidisciplinary framework, the centre focuses on direct interventions for enhanced population health and wellbeing. As a cohesive team, these authors played pivotal roles in shaping the health evidence base through their contributions to the Tackling the Root Causes of Unhealthy Urban Environment Project. This project, funded by the UK Prevention Research Partnership, aims to work with decision makers and communities to prioritise health in urban decision-making processes.
References
- Anderson, M., et al., 2013. Defining indoor heat thresholds for health in the UK. Perspectives in public health, 133 (3), 158–164. doi:10.1177/1757913912453411.
- Arbuthnott, K., et al., 2020. Years of life lost and mortality due to heat and cold in the three largest English cities. Environment international, 144, 105966. doi:10.1016/j.envint.2020.105966
- Arbuthnott, K.G. and Hajat, S., 2017. The health effects of hotter summers and heat waves in the population of the United Kingdom: a review of the evidence. Environmental health, 16 (1), 1–13. doi:10.1186/s12940-017-0322-5.
- Carbon Brief, 2021. The impacts of climate change at 1.5C, 2C and beyond. Available from: https://interactive.carbonbrief.org/impacts-climate-change-one-point-five-degrees-two-degrees/?utm_source=web&utm_campaign=Redirect# [Accessed 7 May 2021].
- Centers for disease Control and Prevention, 2019. CDC’s tracking network in action: extreme heat. Available from: https://www.cdc.gov/nceh/features/trackingheat/index.html#:~:text=%20CDC’s%20Tracking%20Network%20in%20Action%3A%20Extreme%20Heat,or%20death%20are%20preventable%20if%20you…%20More%20
- de Schrijver, E., et al., 2021. A comparative analysis of the temperature-mortality risks using different weather datasets across heterogeneous regions. GeoHealth, 5 (5), e2020GH000363. doi:10.1029/2020GH000363.
- Department of Communities and Local Government, 2012. Investigation into Extreme heat in Homes. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/7604/2185850.pdf [Accessed 19 May 2022].
- Ebi, K.L., et al., 2020. Using detection and attribution to quantify how climate change is affecting health: study explores detection and attribution to examine how climate change is affecting health. Health affairs, 39 (12), 2168–2174. doi:10.1377/hlthaff.2020.01004.
- Ebi, K.L., et al., 2021. Hot weather and heat extremes: health risks. The lancet, 398 (10301), 698–708. doi:10.1016/S0140-6736(21)01208-3.
- Effective Public Healthcare Panacea Project, 2023. [ online]. Available from: https://www.ephpp.ca/quality-assessment-tool-for-quantitative-studies/ [Accessed 20 March 2023].
- Evangelopoulos, D., et al., 2021. Does climatic zone of birth modify the temperature-mortality association of London inhabitants during the warm season? A time-series analysis for 2004–2013. Environmental research, 193, 110357.
- Friel, S., et al., 2011. Climate change, noncommunicable diseases, and development: the relationships and common policy opportunities. Annual review of public health, 32 (1), 133–147. doi:10.1146/annurev-publhealth-071910-140612.
- Gasparrini, A., et al., 2015a. Temporal variation in heat–mortality associations: a multicountry study. Environmental health perspectives, 123 (11), 1200–1207. doi:10.1289/ehp.1409070.
- Gasparrini, A., et al., 2015b. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet, 386 (9991), 369–375. doi:10.1016/S0140-6736(14)62114-0.
- Gasparrini, A., et al., 2012. The effect of high temperatures on cause-specific mortality in England and Wales. Occupational and environmental medicine, 69 (1), 56–61.
- Hajat, S., et al., 2014. Climate change effects on human health: projections of temperature-related mortality for the UK during the 2020s, 2050s and 2080s. Journal of epidemiology and community health, 68 (7), 641–648. doi:10.1136/jech-2013-202449.
- Hansen, A., et al., 2018. The effect of heat waves on mental health in a temperate Australian city. Environmental health perspectives, 116 (10), 1369–1375. doi:10.1289/ehp.11339.
- Head, K., et al., 2018. Report of the systematic review on the effect of indoor heat on health. In: WHO housing and health guidelines. Geneva: World Health Organization. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535282/
- Heaviside, C., Vardoulakis, S., and Cai, X.M., 2016. Attribution of mortality to the urban heat island during heatwaves in the West Midlands, UK. Environmental health: A global access science source, 15 (no. Suppl 1), 27-016-0100–9. doi:10.1186/s12940-016-0100-9.
- Houghton, A. and English, P., 2014. An approach to developing local climate change environmental public health indicators, vulnerability assessments, and projections of future impacts. Journal of environmental and public health, 2014, 1–7. doi:10.1155/2014/132057
- Ige, J., et al., 2019. The relationship between buildings and health: a systematic review. Journal of public health, 41 (2), e121–e132. doi:10.1093/pubmed/fdy138.
- Ige-Elegbede, J., et al., 2020. Designing healthier neighbourhoods: a systematic review of the impact of the neighbourhood design on health and wellbeing. Cities & health, 6 (5), 1–16. doi:10.1080/23748834.2020.1799173.
- IPCC, 2018. Summary for policymakers. In global warming of 1.5°C. An IPCC special report on the impacts of global warming of 1.5°C above pre-industrial levels and related global greenhouse gas emission pathways, in the context of strengthening the global response to the threat of climate change, sustainable development, and efforts to eradicate poverty [V].
- Jadad, A.R., et al., 1996. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Controlled clinical trials, 17 (1), 1–12. doi:10.1016/0197-2456(95)00134-4.
- Keat, W.J., Kendon, E.J., and Bohnenstengel, S.I., 2021. Climate change over UK cities: the urban influence on extreme temperatures in the UK climate projections. Climate dynamics, 57 (11–12), 3583–3597. doi:10.1007/s00382-021-05883-w.
- Kim, Y., et al., 2019. Suicide and Ambient Temperature: A Multi-Country Multi-City Study. Environmental health perspectives, 127 (11), 117007–117001; 117007–10. doi:10.1289/EHP4898.
- Kovats, R.S., Hajat, S., and Wilkinson, P., 2004. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London, UK. Occupational and environmental medicine, 61 (11), 893–898. doi:10.1136/oem.2003.012047.
- Maramba, P.J., et al., 2004. Discharge planning process: applying a model for evidence-based practice. Journal of nursing care quality, 19 (2), 123–129. doi:10.1097/00001786-200404000-00009.
- McMichael, A.J., Neira, M., and Heymann, D.L., 2008. World Health Assembly 2008: climate change and health. Lancet, 371 (9628), 1895–1896.
- Met Office, 2021. UK climate projections: headline findings. Available from: https://www.metoffice.gov.uk/binaries/content/assets/metofficegovuk/pdf/research/ukcp/ukcp18_headline_findings_v3.pdf
- Mitchell, D., 2021. Climate attribution of heat mortality. Nature climate change, 11 (6), 467–468. doi:10.1038/s41558-021-01049-y.
- Moher, D., et al., 2009. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine, 151 (4), 264–269. doi:10.7326/0003-4819-151-4-200908180-00135.
- Mulrow, C.D., Cook, D.J., and Davidoff, F., 1997. Systematic reviews: critical links in the great chain of evidence. Annals of internal medicine, 126 (5), 389–391. doi:10.7326/0003-4819-126-5-199703010-00008.
- Murage, P., et al., 2020. What individual and neighbourhood-level factors increase the risk of heat-related mortality? A case-crossover study of over 185,000 deaths in London using high-resolution climate datasets. Environment international, 134, 105292. doi:10.1016/j.envint.2019.105292
- O’Malley, C., et al., 2014. An investigation into minimizing urban heat island (UHI) effects: a UK perspective. Energy procedia, 62, 72–80. doi:10.1016/j.egypro.2014.12.368
- Ormandy, D. and Ezratty, V., 2016. Thermal discomfort and health: protecting the susceptible from excess cold and excess heat in housing. Advances in building energy research, 10 (1), 84–98. doi:10.1080/17512549.2015.1014845.
- Page, L.A., Hajat, S., and Kovats, R.S., 2007. Relationship between daily suicide counts and temperature in England and Wales. The British journal of psychiatry: The journal of mental science, 191 (2), 106–112. doi:10.1192/bjp.bp.106.031948.
- Pattenden, S., et al., 2010. Ozone, heat and mortality: acute effects in 15 British conurbations. Occupational & Environmental medicine, 67 (10), 699–707. doi:10.1136/oem.2009.051714.
- Petrou, I., Dimitriou, K., and Kassomenos, P., 2015. Distinct atmospheric patterns and associations with acute heat-induced mortality in five regions of England. International journal of biometeorology, 59 (10), 1413–1424. doi:10.1007/s00484-014-0951-0.
- Taylor, J., et al., 2018. Comparison of built environment adaptations to heat exposure and mortality during hot weather, West Midlands region, UK. Environment international, 111, 287–294. doi:10.1016/j.envint.2017.11.005
- Tham, S., et al., 2020. Indoor temperature and health: a global systematic review. Public health, 179, 9–17. doi:10.1016/j.puhe.2019.09.005
- Vardoulakis, S., et al., 2014. Comparative assessment of the effects of climate change on heat- and cold-related mortality in the United Kingdom and Australia. Environmental health perspectives, 122 (12), 1285–1292. doi:10.1289/ehp.1307524.
- Vardoulakis, S. and Heaviside, C., eds., 2012. Health effects of climate change in the UK 2012. London: Health protection agency.
- Wondmagegn, B.Y., et al., 2019. What do we know about the healthcare costs of extreme heat exposure? A comprehensive literature review. Science of the total environment, 657, 608–618. doi:10.1016/j.scitotenv.2018.11.479
- Zhang, Y., et al., 2018. Association of diurnal temperature range with daily mortality in England and Wales: a nationwide time-series study. Science of the total environment, 619–620, 291–300. doi:10.1016/j.scitotenv.2017.11.056