Abstract
We describe a case of minoxidil overdose which led to a prolonged distributive shock. Although this was a case of combined trauma presenting with self-inflicted lacerations and intentional overdose via ingestion of minoxidil-finasteride topical spray and non-steroidal anti-inflammatory drugs (NSAIDs), we believe the hypotension encountered was due to minoxidil’s effects and not exsanguination. In conjunction with poison control, our patient was successfully managed with phenylephrine, vasopressin, midodrine, and several liters of IV hydration despite prolonged refractory hypotension.
Keywords:
Introduction
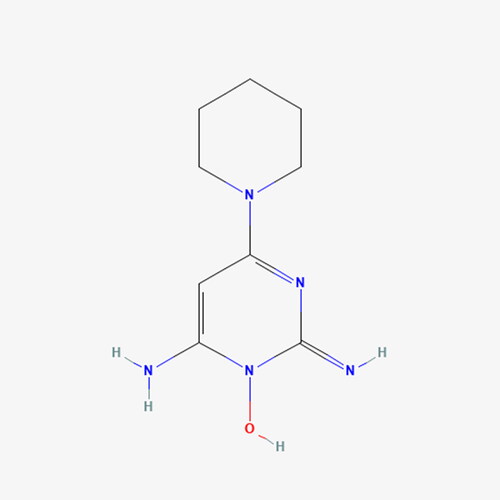
Minoxidil is an anti-hypertensive agent with off-label use for alopecia [Citation1]. It causes vasodilation primarily by hyperpolarization of cell membranes through activation of ATP-sensitive potassium channels to produce smooth muscle relaxation [Citation2, Citation3]. Minoxidil was originally indicated for the treatment of refractory hypertension, and co-administered with a beta-blocker or an alpha-adrenergic blocker to avoid reflex tachycardia.
When used for alopecia, it is normally administered topically either alone or with finasteride. We present, in accordance with CARE Guidelines (https://www.care-statement.org), a case of profound and prolonged hypotension following ingestion of topical minoxidil-finasteride.
Case
An 18 year old male presented to our Trauma Unit with self-inflicted lacerations to the neck, bilateral wrists, and bilateral ankles in a suicide attempt. His initial vital signs included a heart rate of 146 and blood pressure of 91/45 mmHg, with an electrocardiogram showing sinus tachycardia without ST segment or T wave changes. Initial complete blood count revealed a white blood cell count of 27.69, a hemoglobin of 13.4, and hematocrit of 41.4. He was given 3 L of fluids, intubated, and taken to the operating room for exploration of the anterior neck and closure of his four extremity wounds. A small branch of the external jugular vein was successfully ligated. The extremity lacerations were evaluated without any bleeding and subsequently closed. He had minimal bleeding during the procedure. He was extubated and transferred to the post-anesthesia care unit (PACU). The patient remained profoundly hypotensive and tachycardic (pulse 145 bpm, blood pressure 76/33 mmHg). A tertiary exam was performed with no additional findings. He received five doses of ephedrine sulfate 10 mg in the PACU but became further hypotensive and tachycardic (pulse 158 bpm, blood pressure 44/22 mmHg). Phenylephrine was initiated to maintain hemodynamics, and the patient was transferred to the Surgical Intensive Care Unit. Initial chemistry tests also revealed decrease in estimated glomerular filtration, hypernatremia, and increase in creatinine (). At that time, the patient admitted taking 12 tablets of naproxen 220 mg the night prior, 10 tablets of naproxen 220 mg that morning, finasteride hair spray, and a detergent pod. We attempted to transition the patient to norepinephrine from phenylephrine. The patient did not tolerate decreases in phenylephrine dosing and became further hypotensive, requiring norepinephrine at 28 mcg/min and phenylephrine dose of 100 mcg/min.
Table 1. Selected laboratory values.
In the morning, the patient admitted to additionally drinking his combination topical finasteride 0.3%-minoxidil 6% spray bottle with capacity 60 mL, consuming around 30 mL for a total estimated minoxidil dose of 1.8 g. Poison Control recommended continuing phenylephrine and adding midodrine and vasopressin. His hypotension worsened, and we increased his phenylephrine infusion rate to 300 mcg/min to maintain a mean arterial pressure (MAP) of 50. The patient had been given 3 L of fluid resuscitation via a central line. Due to the lower MAP, we initiated vasopressin at 0.04 units/min ().
Overnight, our patient became short of breath and required intubation, with chest x-ray revealing pulmonary edema. He also had an echocardiogram showing heart failure with reduced ejection fraction of 35-40%. At this point, we initiated midodrine 5 mg three times a day. We also added furosemide for diuresis of pulmonary edema. He was successfully extubated and weaned off of all vasopressors five days after admission. On hospital day 12, we obtained a repeat echocardiogram showing resolution of heart failure, with a repeat ejection fraction normal at 55-60%.The patient was successfully discharged.
Discussion
Minoxidil toxicity is sparsely described in the literature. Unintentional or exploratory ingestions in children generally had benign outcomes, and few required hospital treatment [Citation4]. Several case reports in adults have demonstrated more severe effects. One case involved a woman who suffered a myocardial infarction after accidentally ingesting her husband’s minoxidil. She was treated with IV hydration as well as phenylephrine and recovered successfully [Citation5]. In another case, a 36 year old male ingested minoxidil and required dopamine to sustain his blood pressure, but recovered and was eventually discharged [Citation6]. One recent case [Citation7] presented with acute renal failure secondary to hypoperfusion and required norepinephrine and dopamine for resuscitation. More recently, another patient was successfully treated with norepinephrine instead of dopamine, but also required furosemide [Citation8]. Our patient demonstrated that although minoxidil has a half-life of 4.2 h [Citation9], when taken in bulk as an overdose, the effects linger for days and require intensive hemodynamic monitoring. Patients may also present with acute renal failure, acute heart failure, pulmonary edema, and hypernatremia.
An alpha adrenergic vasopressor such as phenylephrine is an appropriate choice to counteract an overdose of minoxidil. Minoxidil is renally cleared. In the case of our patient, his co-ingestion of NSAIDs possibly led to an acute kidney injury, which may have contributed to poor clearance of minoxidil and its metabolites. Our patient successfully recovered after being treated with phenylephrine, vasopressin, midodrine, furosemide, and intravenous fluids.
Disclosure statement
All authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in the paper.
Data availability statement
All data underlying the results are available as part of the article and no additional source data are required.
Additional information
Funding
References
- Sica DA. Minoxidil: an underused vasodilator for resistant or severe hypertension. J Clin Hypertens (Greenwich). 2004;6(5):1–3. doi:10.1111/j.1524-6175.2004.03585.x.
- Lowenthal DT, Affrime MB. Pharmacology and pharmacokinetics of minoxidil. J Cardiovasc Pharmacol. 1980;2 Suppl 2(2):S93–S106. doi:10.1097/00005344-198000022-00002.
- Patel P, Nessel TA, Kumar DD. Minoxidil. [Updated 2023 Nov 15]. In: statPearls [internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482378/
- Forrester MB. Pediatric minoxidil exposures reported to Texas poison centers. Pediatr Emerg Care. 2018;34(6):413–416. doi:10.1097/PEC.0000000000001226.
- Sinha A, Raheja H, Kupfer Y. Myocardial infarction after accidental minoxidil poisoning. Am J Ther. 2018;25(2):e279–e281. doi:10.1097/mjt.00000000000005.
- McCormick MA, Forman MH, Manoguerra AS. Severe toxicity from ingestion of a topical minoxidil preparation. Am J Emerg Med. 1989;7(4):419–421. doi:10.1016/0735-6757(89)90053-3.
- Kikuchi S, Fujita Y, Onodera M, et al. Prolonged hypotension induced by ingesting a topical minoxidil solution: analysis of minoxidil and its metabolites. Acute Med Surg. 2016;3(4):384–387. doi:10.1002/ams2.196.
- Chakar B, Salter M, Roberts DM. Minoxidil overdose with hypotension effectively managed with norepinephrine, rather than dopamine. Clin Toxicol (Phila). 2023;61(2):133–134. doi:10.1080/15563650.2022.2159831.
- Scharman EJ. Minoxidil. Encyclopedia of toxicology. 2nd ed. Philip Wexler ed.; Academic Press 2005. pages 114–115. doi:10.1016/b0-12-369400-0/00631-1, Massachusetts: Cambridge.