Abstract
In Africa, high discontinuation of contraceptive use is thwarting goals for healthy birth spacing or limiting childbearing. This paper investigates how well the contraception program is addressing the needs of women and couples in the Arusha region, Tanzania by studying contraceptive use continuation. We measured the overall and method-specific discontinuation rate, reasons for discontinuation, post-discontinuation reproductive behaviours/outcomes, and examined the determinants of contraceptive discontinuation. We used data from a household survey conducted in Arusha from January to May 2018. Information on contraceptive use during the 31 months preceding the survey was recorded in a monthly calendar. Using the single- and multiple-decrement life-table approach, we calculated the overall and cause-specific discontinuation of contraceptive methods. Logistic regression was used to evaluate the determinants of discontinuation. The 12-month overall discontinuation of contraceptive use was 44.6%. Discontinuation was lowest for implants (12.3%) and highest for male condoms (60.1%), the most common reason being side effects (11.7%). 59.8% of women who discontinued did not switch to another method within 3 months following discontinuation and 20.9% experienced pregnancy. Longer distance to a health facility is associated with higher discontinuation of hormonal methods such as injectables, but lower discontinuation of non-hormonal methods such as condoms. Discontinuation due to side effects is not explained by most of the women’s background characteristics other than the method they used. Discontinuation of contraception is high among Arusha women. Effective contraception programs, especially improved counselling, need to address the reasons for the discontinuation of contraceptive use.
Résumé
En Afrique, le taux élevé d’interruption d’utilisation de contraceptif menace les objectifs d’une limitation ou d’un espacement sain des naissances. Cet article se demande dans quelle mesure le programme de contraception répond aux besoins des femmes et des couples dans la région d’Arusha, République-Unie de Tanzanie, en étudiant l’interruption de l’utilisation de contraceptif. Nous avons mesuré le taux d’interruption global et propre à chaque méthode, les raisons l’expliquant, le comportement/les résultats reproductifs après l’interruption du contraceptif, puis nous avons examiné les déterminants de l’interruption de contraceptif. Nous avons utilisé des données d’une enquête auprès des ménages menée à Arusha de janvier à mai 2018. Les informations sur l’utilisation de contraceptif pendant les 31 mois précédant l’enquête étaient enregistrées dans un calendrier mensuel. À l’aide de la méthode du tableau d’expérience de vie à sorties simples ou multiples, nous avons calculé les taux d’interruption de contraceptif globaux et propres à chaque méthode. Le taux global d’interruption de l’utilisation de contraceptif sur 12 mois était de 44,6%. L’interruption était la plus faible pour les implants (12,3%) et la plus élevée pour les préservatifs masculins (60,1%), la raison invoquée la plus fréquente étant les effets secondaires (11,7%). 59,8% des femmes qui avaient interrompu leur contraception ne passaient pas à une autre méthode dans les trois mois suivant l’interruption et 20,9% sont tombées enceintes. Une plus longue distance jusqu’au centre de santé est associée à un taux supérieur d’interruption des méthodes hormonales comme les contraceptifs injectables, mais à un taux plus faible d’interruption des méthodes non hormonales comme les préservatifs. L’interruption due aux effets secondaires n’est pas expliquée par les caractéristiques personnelles de la plupart des femmes autres que la méthode qu’elles utilisaient. L’interruption de la contraception est élevée parmi les femmes à Arusha. Des programmes de contraception efficaces, spécialement de meilleurs conseils, doivent répondre aux motifs de l’interruption de l’utilisation de contraceptifs.
Resumen
En África, la alta tasa de abandono de anticonceptivos está frustrando los objetivos de espaciamiento de nacimientos saludable o limitando la maternidad. Este artículo investiga cuán bien el programa de anticoncepción atiende las necesidades de las mujeres y parejas en la región de Arusha, en Tanzania, al estudiar la continuación del uso de anticonceptivos. Medimos la tasa de abandono general y con relación a métodos específicos, las razones de abandono y los comportamientos/resultados reproductivos post abandono, y examinamos los determinantes del abandono de anticonceptivos. Utilizamos los datos de una encuesta domiciliaria realizada en Arusha entre enero y mayo de 2018. La información sobre el uso de anticonceptivos durante los 31 meses antes de la encuesta fue anotada en un calendario mensual. Utilizando el enfoque de tabla de vida de decremento único y de decrementos múltiples, calculamos el abandono de métodos anticonceptivos en general y el abandono por causas específicas. Se utilizó regresión logística para evaluar los determinantes del abandono. El abandono general de uso de anticonceptivos durante 12 meses fue de 44.6%. La tasa de abandono más baja fue la de implantes (12.3%); la más alta, la de condones masculinos (60.1%); la razón más común fue por efectos secundarios (11.7%). El 59.8% de las mujeres que abandonaron los métodos no eligieron otro método durante los tres meses posteriores al abandono, y el 20.9% de las mujeres quedaron embarazadas. Mayor distancia a la unidad de salud se asocia con mayor abandono de métodos hormonales tales como inyectables, pero con menor abandono de métodos no hormonales tales como condones. El abandono debido a efectos secundarios no es explicado por la mayoría de las características generales de las mujeres, aparte del método que usaron. La tasa de abandono de anticonceptivos es alta entre las mujeres de Arusha. Es imperativo que los programas de anticoncepción eficaz, en particular mejor consejería, aborden las razones para abandonar el uso de anticonceptivos.
Introduction
Women in sub-Saharan Africa continue to experience high rates of unintended pregnancies with 39% of pregnancies unintended between 2010 and 2014.Citation1 Low contraceptive use is given as a reason for this situation.Citation2,Citation3 Pregnancy and childbirth at an early age and at intervals of less than two years from birth to the next pregnancy are associated with poorer health outcomes for mothers, such as maternal anaemia,Citation4 as well as worse health and long-term economic well-being for newborn babies, such as low birth weight, stunting, mortality, and even lower educational attainment in the long run.Citation5
To improve health outcomes and to meet reproductive goals of women, ensuring accessibility to contraceptives is critical.Citation6 Recently, an increase in contraceptive use has been observed in African countries, including Tanzania, with international and national efforts to improve reproductive health.Citation7 Still, the contraceptive prevalence rate in Tanzania remains at merely 38.4% in 2015.Citation8
The uptake of contraceptive methods is crucial to improving reproductive health, as women who discontinue contraceptives and do not switch in a timely manner to another effective method are at high risk of pregnancy. The prevalence of contraceptive discontinuation is high in developing countries as evident from Demographic and Health Surveys (DHS); over one-third (38%) of women who once used modern contraceptive methods discontinue. This discontinuation rate is even higher in sub-Saharan Africa.Citation9 High discontinuation of contraceptive use thwarts goals for spacing or limiting childbearing and impacts adversely on reproductive health and on achieving the Sustainable Development Goals, particularly Goal 3 to reduce maternal mortality.
Understanding the underlying reasons for high discontinuation is crucial to identifying appropriate programmatic interventions. For example, past studies identify side effects as one of the major reasons for contraceptive discontinuation, especially for oral pills and injectablesCitation10,Citation11 and this finding highlights the importance of comprehensive, balanced, high-quality counselling. However, little is known about determinants of discontinuation due to side effects, or for other reasons. It could be that particular groups of women discontinue due to side effects. For example, the extent to which side effects contribute to the discontinuation of contraceptive use may vary not only by the method but also by women’s age, education, and other background characteristics. This aspect has not been well studied previously.
This paper uses the data set from the Arusha region in Tanzania to address three key questions: what are contraceptive discontinuation rates by method? what are the consequences of discontinuation?, and what are the determinants of contraceptive discontinuation, by method and by reason? To evaluate the determinants of discontinuation by method and by reason, we adapt the conceptual framework on contraception demand by Bertrand et al.Citation12 We include: (1) individual background factors such as age, education, marital status, and wealth level, (2) value for children (the number of children), and (3) service outputs (distance to health facilities offering contraceptive methods).
By addressing these questions, this paper exposes potential problems with contraceptive methods and highlights gaps in service provision. It also provides important information on the reproductive consequences of stopping use. Taken together, the findings can inform on guidance essential for improving contraception programs and contribute to the literature by providing a comprehensive picture of discontinuation, beyond measuring its rate.
Methods
Data source
We use data from a household survey conducted from January to May 2018. The data are originally from a large study called Willows Impact Evaluation (WIE). The region was prioritised by Willows International for a community-based contraception information, counselling and referral intervention. The implementation site comprises urban areas of the Arusha region, in the northern part of Tanzania, where contraceptive use is low despite the availability of services. The WIE project collected data from 3950 women of childbearing age (16–44 years) on reproductive health, including the utilisation of contraceptive methods. The questionnaire for the survey was adapted from the 2015–2016 Tanzania Demographic and Health Survey (TDHS) with additional information to meet the WIE objectives. While the contraceptive calendar in TDHS captures data over 60 months, our study covers a 31-month period preceding the survey, to minimise recall bias. For more information on the contraceptive calendar, see Ali et al.Citation13 and USAIDCitation14.
Sample
presents the flowchart of the analysis sample. We started with 12,203 reproductive and contraceptive events recorded in the calendar data from the 3950 women. We dropped 3216 episodes of contraceptive use initiated before the 31-month calendar period. We also dropped 6104 episodes where the status was indicated as (1) no method used, (2) pregnancy, (3) termination of pregnancy, (4) childbirth. Another 260 episodes were dropped because the initiation of the episodes was within 0–3 months prior to the interview, or because the methods were recorded as “unknown” or “sterilisation”. We dropped the episodes 0–3 months prior to the interview to account for the possibility that some women may have become pregnant but were not yet aware of the pregnancy.
Figure 1. Flowchart of events included in contraceptive calendar
Note: 12,209 episodes are from 3950 women, and the analytical sample of 2623 episodes are from 1966 women in Arusha region, Tanzania
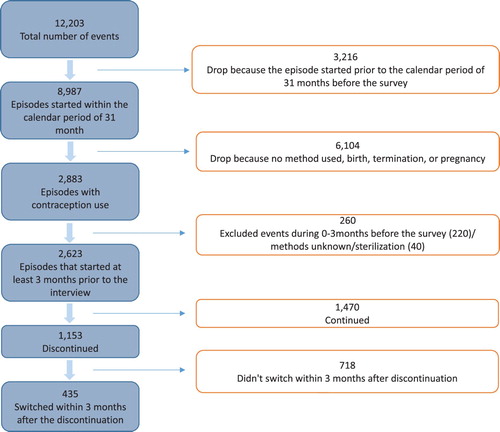
The remaining sample of 2623 episodes from 1966 women was analysed, of which 1153 episodes were discontinued at some point during the 31-month calendar period. Of the discontinued episodes, method switching occurred for 435.
Analysis
To examine the discontinuation of each contraceptive method, cumulative probabilities of discontinuation for all reasons, as well as for specific reasons, at 12 months since the start of use, were estimated using single and multiple-decrement life-table methods. We also examined the consequences of the discontinuation, and of subsequent reproductive behaviours, by evaluating reproductive status at three months post-discontinuation, by method. To do this, calendar status at three months post-discontinuation was used, looking at all contraceptive methods reported by respondents. Discontinuation was expected to differ by the type of contraceptive method. Long-acting methods, such as the intrauterine device (IUD) and implants, were expected to have lower discontinuation as compared to short-term methods, such as injectables, pills, and condoms.
We also evaluated the determinants of discontinuation by method, and by reason for discontinuation, through logistic regression. As we were mainly interested in the difference between women who discontinued and who did not, we chose to use logistic regression for the simple interpretation of determinants of discontinuation, rather than using the survival model to take account of the time factor. Following the conceptual framework on contraception demand by Bertrand et al.,Citation12 we included (1) individual factors, such as age, education, marital status, and wealth level, (2) number of children, and (3) service outputs (distance to health facilities offering contraceptive methods). As Ochako et al.Citation15 suggested, we also included the number of contraceptive methods that respondents knew.
Distance is measured using the GPS coordinates of respondents’ location and that of the nearest health facility that offers the contraception services. Distance can influence not only the uptake of a method but also the discontinuation of use because the inconvenience of the clinic visit might make repeated visits difficult. Distance might be correlated with the discontinuation of methods that require a clinic visit and can have a substitution effect on methods that do not require clinic visits.
Using the wealth index comparable to the one in TDHS, we categorised respondents into five groups: poorest, poorer, medium, richer, and richest. To make the wealth index comparable to the THDS, we first identified variables common to our survey and TDHS. Using these common variables, we re-defined the wealth category, which we confirm is strongly associated with the original wealth category. The same cut-off points as those for TDHS are used to define the wealth category.
Ethics approval
The original study with data used for this paper was reviewed and approved by the Institutional Review Board (IRB) of the Harvard TH Chan School of Public Health (IRB17-1794). The study also received ethical approval from the ethics review boards of the Kilimanjaro Christian Medical College (1085) and Tanzania National Institute for Medical Research (NIMR/HR/R.8a/Vol.IX/2703). Only women who consented to participate in the study were interviewed.
Results
presents descriptive statistics of the 1966 women aged 16–44 years, who contributed to the 2623 contraceptive episodes included in the analysis. More than half (57%) of women had primary education, while about one-third had secondary education. As compared to the nationally representative TDHS, our Arusha sample is concentrated in the second richest category, with 45.7% categorised as richer. If our sample had been similar to a nationally representative sample, then women in each category would have been equally distributed with 20% in each category. Over 80% of respondents are currently married.
Table 1. Distribution of women, by background characteristics, Arusha, 2018
The unit of observation in our analysis is an uninterrupted episode of contraceptive use. presents the proportion of episodes and mean duration of use of different contraceptive methods. On average, one episode of use is about 11 months. The most common contraceptive method used is injectables (28%) with an average duration of use of 10 months. The second most common method is implants (22.2%) with an average of 13 months of continued use, followed by calendar method (15.9%) with 11 months of continuous use on average.
Table 2. Number and per cent of contraceptive episodes and median duration of use, by type of method, Arusha, 2018
Discontinuation and reasons
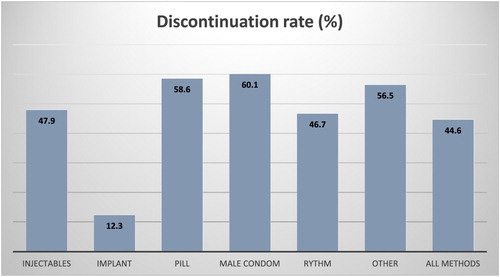
presents the overall discontinuation rate as well as method-specific discontinuation rates. Overall, in 44.6% of episodes, the use was discontinued by the 12th month. The rate is the highest for male condom (60.1%), followed by oral contraceptive pills (58.6%), and injectables (47.9%). The lowest discontinuation is observed for implants (12.3%). For the analysis, we report the results for IUD and withdrawal as “others”, due to the small sample size.
Figure 2. Per cent discontinuing use by 12th month, by type of contraceptive method, Arusha, 2018
Notes: The sample is 2623 episodes which were initiated after the baseline interview among 1966 women. “Other” methods include IUD and withdrawal due to the small size, in addition to Lactational amenorrhoea
presents method-specific discontinuation rates by reason of discontinuation. Overall, the most common reason for discontinuation is side effects/health concerns (11.7%), followed by the desire to become pregnant (9.3%) and other situations, such as infrequent sex, difficulty in getting pregnant, menopause, and marital dissolution (7.3%). The dominant reason for discontinuation varies by the type of method. For example, the main reason for discontinuation among users of the oral pill is side effects or health concerns (19.7%), while the same reason, unsurprisingly, is reported the least by users of rhythm methods (3.5%). In general, hormonal methods, such as injectables and pills, are discontinued more for side effects or health concerns (20%) than for method failure, whereas rhythm is discontinued more for method failure (10%) than for side effects or health concerns (3%). Implants have the lowest discontinuation due to either method failure or side effects; there are no reported discontinuations due to method failure and it also has one of the lowest proportions of discontinuation due to side effects.
Table 3. Percentage discontinuing use, by type of method and reason, Arusha, 2018
Reproductive status post-discontinuation
(Panel A) presents the subsequent contraceptive status three months after the discontinuation of contraceptive use. Overall, 33% of discontinued episodes led to no method used in the three months following discontinuation. One-fifth of discontinued episodes were followed by pregnancy. shows that 4.2% of episodes resulted in pregnancy from method failure. Therefore, in an additional 16.7% of episodes, women must have become pregnant after discontinuing use. Women who were using injectables were more likely to switch to implants (16.5% of episodes) or pills (10%) than to other methods, while women who were using implants or pills were more likely to switch to injectables (21.6% and 21.3%, respectively) than to other methods. On the other hand, women who were using condoms were more likely to switch to the rhythm method (10.8%). It is important to note that 10% of discontinued episodes with condom returned to the same method (condom) within three months. A high percentage of rhythm users experienced a pregnancy (42% of episodes) by the third month after discontinuation, with 10% of episodes already resulting in pregnancy due to failure of this method.
Table 4. Status at three months after discontinuing for any reason, by method discontinued, Arusha, 2018
Subsequent reproductive events might be different, depending on the reason for discontinuation. (Panel B and C) presents the subsequent reproductive events by the reason for discontinuation, desire to get pregnant vs. other reasons. Among discontinuers who had a desire to get pregnant, half became pregnant within three months of the discontinuation, and the other half were not using any method. Among discontinuers who did not have a desire to get pregnant (i.e. in need of contraceptives), the trend is similar to Panel A.
Determinants of discontinuation
presents the regression results of the determinants of discontinuation, by the type of contraceptive method. Column 1 shows the determinants of discontinuation of all methods together. Older age is weakly associated with less risk of the discontinuation but overall, age, education level, marital status, and wealth level are not associated with the likelihood of discontinuation. An increase in the number of miscarriages by one increases the odds of discontinuation by 22.3%, while one additional child is associated with decreased odds of discontinuation by 9.8%, perhaps indicating stronger motivation to use contraception when desired fertility has been achieved.
Table 5. Odds ratios of method discontinuation, by contraceptive method and background characteristics
The discontinuation rate for male condom and the pill is similar to that for injectables but higher than for other methods. This is broadly consistent with . The discontinuation rate is lower among implants and rhythm users by 88.6% and 46.5%, respectively, as compared to injectables. Distance to a health facility is not associated with overall discontinuation.
(columns 2–6) evaluates for each contraceptive method, the differential determinants of discontinuation. As compared to younger women, older women are less likely to discontinue injectables and rhythm methods (column 2). Women in wealthier households are less likely to discontinue condoms. Married women are less likely to discontinue injectables (column 4), while more likely to discontinue rhythm methods (column 6).
Longer distances to health facilities that provide contraception are positively associated with the risk of discontinuation of injectables (column 2), while negatively associated with discontinuation of condoms and rhythm methods (columns 5 and 6). The number of contraceptive methods known is not associated with the likelihood of the discontinuation for any method.
presents discontinuation of contraceptive method by reasons for discontinuation. Higher education is associated with lower discontinuation due to method failure. Using rhythm methods and higher numbers of children are associated with higher method failure (column 1). Older age, being married, using rhythm methods, and the number of miscarriages are positively associated with higher discontinuation due to the desire to get pregnant, while higher numbers of children are negatively associated with higher discontinuation due to the desire to get pregnant (column 2). Using injectables or implants is associated with a lower risk of discontinuation due to fertility problems (column 3), but a higher risk of discontinuation due to side effects (column 4). The number of contraceptive methods known increases the risk of discontinuation due to the desire to have more effective methods (column 5).
Table 6. Odds ratios of method discontinuation, by reason of discontinuation and background characteristics
Discussion
This paper draws a picture of contraceptive discontinuation beyond measuring the rate; it evaluates the discontinuation of contraception, post-discontinuation reproductive behaviours/outcomes, and determinants of discontinuation, by contraceptive method and reasons, among women in the Arusha region, Tanzania.
We find that the overall discontinuation rate of 44.6% is high in northern Tanzania. This is much higher than the discontinuation rate of 26.1% found in the TDHS conducted in 2015/2016 among a representative sample of women in TanzaniaCitation16. While the use of male condoms is associated with the highest discontinuation rate, followed by pills and injectables in Arusha, nationally representative data show that the highest discontinuation is that for the pill, followed by injectables and withdrawal.
The main differences between the Arusha sample and the nationally representative sample from the DHS are in sample size, year of the survey, regions the sample is drawn from, and the length of the period (60 months in TDHS compared to 31 months in our survey) covered by the contraceptive calendar. Our sample is of 3950 women interviewed in 2018 from a district in the Arusha region, while DHS data are for 6825 women surveyed in 2015 and 2016 from nationally representative regions.
Common contraceptive methods with high discontinuation rates and reasons for discontinuation are mostly consistent between our Arusha study and TDHS. Excluding the withdrawal method, due to the small sample size, the three most common methods with high discontinuation rates in both the Arusha sample and the national sample are male condoms, pills, and injectables. The common reasons for discontinuation in both studies are side effects and the desire to get pregnant.
Our analysis on post-discontinuation outcomes reveals important findings on women’s contraceptive preferences. First, the high percentage (33%) of discontinued episodes is followed by no method used or pregnancy (21%) three months after discontinuation. This result indicates that most users who discontinue a contraceptive method do not switch to another method in a timely manner, or they become pregnant within the subsequent three months. The high discontinuation rate and low timely switching can expose many women to a high risk of unintended pregnancy. Second, women have preferences for specific types of methods, even after discontinuation of a particular method. For example, users of hormonal methods, such as injectables, implants, and pills, are likely to switch to a similar type when they decide to switch to other methods. Similarly, users of non-hormonal methods such as condoms and rhythm are also likely to switch between the two but not to other more effective methods. This might reflect the difference in preference for specific types of contraceptive methods. Women who are hesitant to use modern and effective methods, such as injectables, implants, and pills, might have a dislike for methods that need to be inserted/taken into their body. Strauss et al.Citation17 summarised the literature on women’s contraceptive preference, but little has been studied so far about how women’s preferences affect their switching behaviours after the discontinuation of a method. Our paper reveals this important finding: women’s contraception preferences predict the type of contraceptive methods chosen after the discontinuation.
Our paper also contributes to the existing literature by evaluating the predictors of discontinuation by method. One of the highlights of our study is that we find a differential effect of distance to health facility, on contraceptive discontinuation. The further the distance is to the health facility, the more likely that a respondent discontinues modern methods such as injectables. On the other hand, the further the distance to a health facility, the lower the odds of discontinuation of non-hormonal methods such as condoms and rhythm methods, that do not require a visit to a health facility or can be procured easily from a drug store or pharmacy. This result implies that, when physical access to some contraceptives is not easy, there is a greater likelihood of reliance on methods that do not require a clinic visit. While past studies such as Shiferaw et al.Citation18 emphasised the importance of distance to health facility as the determinant of contraceptive adoption, our study sheds light on a new aspect – (dis)continuation of contraceptive use. We also find that the effect of distance on discontinuation varies, depending on the type of method.
In addition, our paper evaluates the predictors of discontinuation according to reasons for discontinuation. While side effects are the most common reason, we failed to find predictors for discontinuation for this reason other than the method type; users of implants and injectables are more likely to discontinue due to side effects than users of other methods. Future study should explore predictors of discontinuation due to side effects, which might be made possible if more detailed data are available such as past experiences of side effects.
To avoid unnecessary discontinuation due to side effects, which can expose women to the risk of unintended pregnancies, future studies also need to consider minimising discontinuation for this reason, for example, by advancing technology to reduce the side effects. Another way is to create improved understanding among potential users about the potential side effects of each method so they can make choices that are informed and suitable for their needs. There is evidence to show that there is little or no counselling on the management of side effects in TanzaniaCitation19 and the need for improved counselling has been emphasised. Finally, we need to advance the study on associations between various women’s characteristics, including social, physiological, and behavioural factors, with the likelihood of experiencing side effects.
Through this analysis, we also find that if women are better informed about alternative methods, they are more likely to discontinue and switch to a more effective method of their preference. The timing with which women acquire information might also be critical; providing sufficient information prior to initiation of any contraceptive use may be the most effective way to avoid unnecessary discontinuation.
Limitations
There are three main limitations to this study. First, due to the limited information available in the survey, we could not conduct a further in-depth analysis of the determinants of discontinuation. For example, discontinuation due to side effects is not associated with any sociodemographic characteristics of women. Therefore, it remains unclear why some women experience side effects using a method while others do not. Biomarkers could perhaps disentangle this issue, but such data were not collected in our survey. Second, the contraceptive calendar is subject to recall bias.Citation20 Third, because the data do not come from a nationally representative sample, our findings cannot be generalised to all of urban Tanzania or nationally.
Conclusions
This study provides an in-depth assessment of contraceptive discontinuation among women in Arusha. We find a high rate of discontinuation (44.6%), and most users who discontinue a contraceptive method do not switch to another method or become pregnant within the subsequent three months. Thus, many women are exposed to high risk of unintended pregnancy, as well as related risks, including unsafe terminations, especially given the legal restrictions on access to abortion in Tanzania. Further research is needed to identify and implement interventions that minimise unnecessary discontinuation and facilitate prompt recourse to an alternative method when discontinuation occurs.
Conflict of interests
Authors declare that there are no conflicts of interest in conducting and publishing this study.
ORCID
Ryoko Sato http://orcid.org/0000-0001-7040-317X
Additional information
Funding
References
- Bearak J, Popinchalk A, Alkema L, et al. Global, regional, and subregional trends in unintended pregnancy and its outcomes from 1990 to 2014: estimates from a Bayesian hierarchical model. The Lancet Global Health. 2018;6(4):e380–e389. doi: 10.1016/S2214-109X(18)30029-9
- Tsui AO, Brown W, Li Q. Contraceptive practice in sub-Saharan Africa. Popul Dev Rev. 2017;43(Suppl 1):166. doi: 10.1111/padr.12051
- Cleland JG, Ndugwa RP, Zulu EM. Family planning in sub-Saharan Africa: progress or stagnation? Bull World Health Organ. 2011;89:137–143. doi: 10.2471/BLT.10.077925
- Patton GC, Sawyer SM, Santelli JS, et al. Our future: a Lancet commission on adolescent health and wellbeing. The Lancet. 2016;387(10036):2423–2478. doi: 10.1016/S0140-6736(16)00579-1
- Fall CH, Sachdev HS, Osmond C, et al. Association between maternal age at childbirth and child and adult outcomes in the offspring: a prospective study in five low-income and middle-income countries (COHORTS collaboration). Lancet Glob Health. 2015;3(7):e366–e377. doi: 10.1016/S2214-109X(15)00038-8
- Dennis ML, Radovich E, Wong KL, et al. Pathways to increased coverage: an analysis of time trends in contraceptive need and use among adolescents and young women in Kenya, Rwanda, Tanzania, and Uganda. Reprod Health. 2017;14(1):130. doi: 10.1186/s12978-017-0393-3
- Tsui AO, Brown W, Li Q. Contraceptive Practice in Sub-Saharan Africa. Popul Dev Rev. 2017;43(Suppl 1):166–191. doi: 10.1111/padr.12051
- United Nations, Department of Economic and Social Affairs, Population Division. (2019). World Contraceptive Use 2019 (POP/DB/CP/Rev2019).
- Jain AK, Obare F, RamaRao S, et al. Reducing unmet need by supporting women with met need. Int Perspect Sex Reprod Health. 2013;39(3):133–141. doi: 10.1363/3913313
- Adal TG. Early discontinuation of long acting reversible contraceptives among married and in union women: a systematic review and meta-analysis. Ann Med Health Sci Res. 2017;7:113–118.
- Rosenberg MJ, Waugh MS. Oral contraceptive discontinuation: a prospective evaluation of frequency and reasons. Am J Obstet Gynecol. 1998;179(3):577–582. doi: 10.1016/S0002-9378(98)70047-X
- Bertrand J, Magnani R, Rutenberg N. Evaluating family planning programs: with adaptations for reproductive health. Chapel Hill (NC): The EVALUATION Project; 1996.
- Ali MM, Cleland JG, Shah IH, et al. Causes and consequences of contraceptive discontinuation: evidence from 60 demographic and health surveys. (2012).
- USAID. DHS contraceptive calendar tutorial. Available from: https://www.dhsprogram.com/data/calendar-tutorial/upload/DHS-Contraceptive-Calendar-Tutorial.pdf.
- Ochako R, Temmerman M, Mbondo M, et al. Determinants of modern contraceptive use among sexually active men in Kenya. Reprod Health. 2017;14(1):56. doi: 10.1186/s12978-017-0316-3
- Ministry of Health. Community Development, Gender, Elderly and Children (MoHCDGEC) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar], National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF. 2016. Tanzania Demographic and Health Survey and Malaria Indicator Survey (TDHS-MIS) 2015–16. Dar es Salaam, Tanzania, and Rockville, MD, USA: MoHCDGEC, MoH, NBS, OCGS, and ICF.
- Institute of Medicine. New frontiers in contraceptive research: a blueprint for action. Washington (DC): National Academies Press; 2004. doi:10.17226/10905.
- Shiferaw S, Spigt M, Seme A, et al. Does proximity of women to facilities with better choice of contraceptives affect their contraceptive utilization in rural Ethiopia? PloS one. 2017;12(11):e0187311. doi: 10.1371/journal.pone.0187311
- Chebet JJ, McMahon SA, Greenspan JA, et al. “Every method seems to have its problems”-Perspectives on side effects of hormonal contraceptives in Morogoro region, Tanzania. BMC Womens Health. 2015;15(1):97. doi: 10.1186/s12905-015-0255-5
- Bradley SE, Winfrey W, Croft TN. (2015). Contraceptive use and perinatal mortality in the DHS: An assessment of the quality and consistency of calendars and histories.
