Abstract
Extramarital sexual relations are forbidden in Islam, and sexual health information is not readily available in Islamic communities, especially for women. This review aimed to explore sexually transmitted infection (STI) knowledge and attitudes among Muslim women worldwide. A systematic review was conducted on seven electronic databases. We included qualitative and quantitative studies of female Muslim participants of reproductive age, focusing on STI knowledge and attitudes. A narrative synthesis approach was used with thematic analysis methods. Eighteen studies conducted in 13 countries were included. Three main themes were identified: poor knowledge and misconceptions; sources of sexual health information and information needs; and cultural influences on STI knowledge and attitudes. Generally, Muslim women had poor knowledge regarding STI signs and symptoms, prevention, diagnosis and treatment, in addition to many misconceptions. Negative attitudes towards people infected with HIV/AIDS were common, and attitudes were highly influenced by misconceptions and insufficient knowledge. Infected women tended to be subjected to more blame and judgement compared to men. While the review summarises knowledge and attitudes of Muslim women worldwide, we excluded studies that did not clearly state that the study participants were Muslim women, hence many countries with Muslim populations are not represented in this review. Negative attitudes towards STIs make it harder for women to access sexual health information, STI prevention and treatment. This review highlights the need for culturally sensitive sexual health education for Muslim women. Future sex education interventions would benefit from considering the wider personal and external barriers.
Résumé
Les relations sexuelles extraconjugales sont interdites dans l’Islam et les informations sur la santé sexuelle ne sont pas aisément disponibles dans les communautés islamiques, en particulier pour les femmes. Cet examen souhaitait étudier les connaissances et les attitudes concernant les infections sexuellement transmissibles (IST) chez les musulmanes dans le monde. Un examen systématique a porté sur sept bases de données numériques. Nous avons inclus des études qualitatives et quantitatives sur des participantes musulmanes en âge de procréer, centrées sur les connaissances et les attitudes en matière d’IST. Une synthèse narrative a été utilisée avec des méthodes d’analyse thématique. Dix-huit études menées dans 13 pays ont été incluses. Trois principaux thèmes ont été identifiés: mauvaises connaissances et idées fausses; sources d’information sur la santé sexuelle et besoins en information; et influences culturelles sur les connaissances et les attitudes en matière d’IST. En général, les musulmanes connaissaient mal les signes et les symptômes des IST, leur prévention, leur diagnostic et leur traitement, et avaient aussi beaucoup d’idées erronées. Les attitudes négatives à l’égard des personnes infectées par le VIH/sida étaient fréquentes et les comportements étaient extrêmement influencés par les idées fausses et les connaissances insuffisantes. Les femmes infectées tendaient à être davantage blâmées et jugées que les hommes. Si l’examen résume les connaissances et les attitudes des musulmanes dans le monde, nous avons exclu les études qui n’affirmaient pas clairement que les participantes de l’étude étaient des musulmanes, ce qui explique que beaucoup de pays avec des populations musulmanes ne soient pas représentés dans l’examen. Les attitudes négatives à l’égard des IST rendent plus difficile pour les femmes d’avoir accès aux informations sur la santé sexuelle ainsi qu’à la prévention et au traitement des IST. Cet examen met en lumière la nécessité d’une éducation à la santé sexuelle sensible aux particularités culturelles pour les musulmanes. Les futures interventions d’éducation sexuelle auraient avantage à envisager les obstacles personnels et externes plus généraux.
Resumen
Las relaciones sexuales extramatrimoniales están prohibidas en el islam, y la información sobre salud sexual no está disponible ampliamente en las comunidades islámicas, especialmente para mujeres. Esta revisión procuró explorar las actitudes y conocimientos de las mujeres musulmanas en todo el mundo con relación a las infecciones de transmisión sexual (ITS). Se realizó una revisión sistemática en siete bases de datos electrónicas. Incluimos estudios cualitativos y cuantitativos con mujeres musulmanas en edad reproductiva, enfocados en actitudes y conocimientos relacionados con ITS. Se utilizó un enfoque de síntesis narrativa con métodos de análisis temático. Se incluyeron dieciocho estudios realizados en 13 países. Se identificaron tres temas principales: escasos conocimientos e ideas erróneas; fuentes de información sobre salud sexual y necesidades de información; e influencias culturales en las actitudes y los conocimientos relacionados con ITS. Por lo general, las mujeres musulmanas tenían escasos conocimientos de los signos, síntomas, prevención, diagnóstico y tratamiento de ITS, así como muchas ideas erróneas. Las actitudes negativas hacia personas infectadas con VIH/SIDA eran comunes, y las ideas erróneas y conocimientos insuficientes influían marcadamente en las actitudes. Las mujeres infectadas eran propensas a ser sujetas a más culpa y prejuicios, en comparación con los hombres. Aunque la revisión resume las actitudes y los conocimientos de las mujeres musulmanas mundialmente, excluimos los estudios que no establecieron claramente que las participantes del estudio eran mujeres musulmanas; por ello, muchos países con poblaciones musulmanas no están representados en esta revisión. Debido a las actitudes negativas hacia las ITS, les resulta más difícil a las mujeres acceder a información sobre salud sexual, y sobre prevención y tratamiento de ITS. Esta revisión destaca la necesidad de brindar educación sobre salud sexual culturalmente sensible a las mujeres musulmanas. Futuras intervenciones en educación sexual se beneficiarían de considerar las barreras personales y externas generales.
Introduction
Sexually transmitted infections (STIs) have a significant impact on sexual and reproductive health and are increasingly becoming a public health concern worldwide. According to the World Health Organization, more than one million STIs are acquired each day.Citation1 The majority of these occur among adolescents and young adults who are unaware that they are infected and lack adequate sexual health knowledge.Citation2 If left untreated, some STIs can cause irreparable damage to women’s reproductive organs and could be transmitted from mother to child during pregnancy and childbirth.Citation3
In Islamic countries, extramarital sexual relations are prohibited by religion. It is commonly believed that those countries have the lowest rates of HIV/AIDS.Citation4,Citation5 The prevalence of people living with HIV/AIDS in the Middle East and North Africa (MENA) region, which is predominantly made up of Islamic countries, is much lower than the world average.Citation6 However, it is also believed that HIV/AIDS rates are significantly under reported.Citation7 Recent available data revealed that the number of new HIV cases rose by 26% between 2004 and 2014, making the growth of the HIV epidemic in the MENA region one of the fastest globally.Citation8 While some of this rise could be attributed to enhanced testing and reporting, a significant proportion of cases are new transmissions,Citation7 and the public are commonly unaware of the extent of risk behaviours and the measures of prevention.Citation4
Since sexual relations outside of marriage are forbidden in Islam, it is assumed that people are abstaining from sexual relationships until marriage. However, this is not the case with some young Muslims engaging in extramarital/premarital sexual relations.Citation9–11 Despite efforts by advocates calling for the need to educate young Muslims on sexual health issues, and providing services for those who need it, many countries fail to prioritise the issue. The reluctance is likely to be from the cultural sensitivity surrounding sexuality, and more specifically, young people’s sexuality.Citation12
There is a specific risk of under-detection of HIV/AIDS among women in the MENA region.Citation13 Since sexual activity is influenced by gender roles, particularly in Muslim societies, Muslim women appear to be especially vulnerable. The vast majority of infections in the region are among men, and the main route for HIV transmission among women is marriage.Citation13 For example, in Morocco, 70% of infections among women are due to an infected spouse.Citation14 A study in Lebanon suggested that healthcare providers expressed negative attitudes towards providing sexual health services for women and admitted that they would misrepresent facts about HIV to women whose husbands are infected with HIV, to avoid divorce and to preserve their marriages.Citation15 In addition, risks related to sexual activity for both married and unmarried women are increased due to the lack of available services. This review aimed to explore STI knowledge, information sources, attitudes among Muslim women worldwide, and identify the barriers to STI prevention, diagnosis and treatment.
Methods
Design
A systematic literature review was conducted following the Centre for Reviews and Dissemination guidelines.Citation16 A narrative synthesis approach was employed using thematic analysis methods. A study protocol was registered with Prospero (registration number: CRD42017081999) prior to conducting the review, with no changes to the original plan.
Search strategy
Seven electronic databases were searched: MEDLINE (via OvidSP), EMBASE (via OvidSP), WEB OF SCIENCE, PsycINFO (via OvidSP), Maternity & infant care (via OvidSP), CINAHL (via the EBSCO Host), and POPLINE. We searched a number of grey literature databases (Openlit, Ethos, Popline) but there were a limited number of studies, none of which were eligible for this review. Details of the search strategy can be found in Additional File 1. Where applicable, MeSH terms were selected and exploded to identify articles where different terms were used for the same concept. Where MeSH terms were not available, free-text search terms were used. The search was carried out in January 2017, the start date was set to 2007 onwards. We have limited the search to the last 10 years to provide the most relevant and recent literature because the patterns of STI epidemiology and STI treatment change over time. The search was updated in March 2018. Search terms used fell broadly into three categories: population terms [including Islam; Muslim(s); Islamic countries; Middle East; North Africa; MENA], gender terms [including woman/women; female(s), girl(s), wives/wife; lady/ladies], and sexual health terms [including sexual health; women’s health; sexually transmitted diseases; sexually transmitted infections; sex education; sex counselling].
Eligibility criteria
Inclusion criteria
Participants included female Muslims of reproductive age.Citation15–49 Where studies also included non-Muslim or male participants, findings relevant to Muslim women were extracted.
Studies focusing on STI knowledge, attitudes, information sources, and barriers to STI testing and diagnosis were included.
Both qualitative and quantitative studies were included.
Any country with a Muslim population was included.
Publications in all languages were eligible.
Exclusion criteria
Studies were excluded if the outcomes were not reported, male and female results were not reported separately, or if Muslim results were not reported separately.
Studies conducted in a non-Muslim country or countries where less than 90% of the population are Muslims were excluded, unless it was clearly stated that the study participants were Muslim women.
Intervention studies were excluded because they were measuring the effects of an intervention on a specific population. Studies focusing exclusively on clinical treatments and outcomes, the physiology /pathology of the reproductive health system, and pregnancy outcomes were excluded.
Studies where the participants were healthcare professionals were excluded, as their knowledge/attitudes can be different from those of the general public.
Studies in the form of editorials, conference abstracts, and policy documents were excluded.
Selection criteria
Two reviewers (NA & SA) independently assessed all studies for inclusion and screened title, abstract, and full text. All disagreements were resolved by consensus.
Data extraction
A standardised data extraction form was developed to help in systematically identifying participant characteristics, study design, aims, data collection methods, methods of data analysis and main findings for all included studies. Separate extraction forms were developed for qualitative and quantitative studies. Excel spreadsheets were used to extract the main findings from quantitative studies. NVivo softwareCitation17 was used to facilitate the data management and synthesis processes. First reviewer (NA) extracted all data from all included full texts. Second reviewer (SA) reviewed a random selection of 50% of the extracted data and assessed the quality of 50% of the full texts. All disagreements were resolved by consensus. If reviewers required more information, authors were contacted.
Quality assessment
For this review, the quality of qualitative studies was assessed using the Critical Appraisal Skills Programme tool (CASP).Citation18 This tool is used to evaluate the trustworthiness, relevance, and rigour of published literature.
The quality of quantitative studies was appraised using the quality assessment tool developed by the Centre for Evidence-Based Management.Citation19 This tool is used to appraise the methodological quality of cross-sectional surveys, and address questions on the representativeness of the sample, response rate, validity of the tools used and statistical significance. Both tools have been widely used to assess the quality of qualitative and quantitative evidence. Studies were not excluded based on quality, but the quality assessments were used to help determine confidence in the findings.
Data analysis
The data in this review were synthesised using a narrative synthesis approachCitation20 which allows for the synthesis of both quantitative and qualitative evidence. All relevant data presented in the included studies were extracted, including participant quotes. A meta-analysis was not conducted due to the variation in measurements used across the included studies. Thematic analysis, which is one of the tools that can be used in the process of narrative synthesis and can be applied to both qualitative and quantitative evidence, was used for this review.Citation21 The first author (NA) developed the initial coding and two authors (SA and JB) checked all codes to ensure that the codes reflected the data. Codes were then discussed, and any necessary amendments made until full agreement was reached. After completing the thematic analysis, the codes of both qualitative and quantitative studies were merged and tabulated. The data was then translated into common categories/headings to allow for useful comparisons of the results. Overarching themes were developed and discussed by the review team. Throughout the analysis process, we actively looked to identify negative cases which allowed for further in-depth exploration and understanding of the data and discussion. Finally, all included studies were revisited to ensure the themes were representative of all relevant data. Participant quotations from the primary studies were presented throughout the results to illustrate review findings.
Results
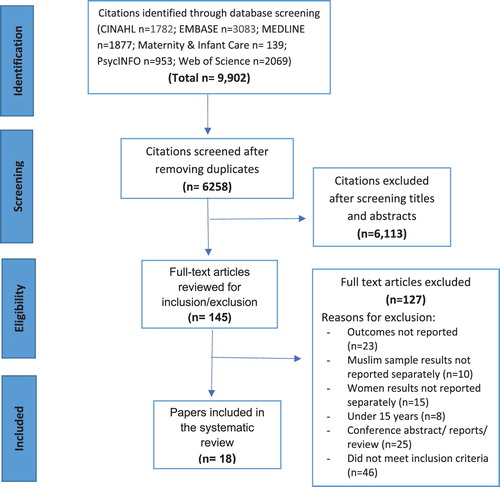
From the database search, 9902 citations were retrieved. After removing duplicates, 6,258 were screened for eligibility (). Our results were based on 18 studies, 16 quantitative and two qualitative. The studies assessed Muslim women’s STI knowledge on modes of transmission, symptoms, prevention, treatment; attitudes towards STIs including HIV; barriers to testing and diagnosis; and the influence of culture and religion on sexual health knowledge and attitudes. Fourteen studies were conducted in the MENA region, and four studies in Australia, Afghanistan, Pakistan and the United Kingdom (UK). Characteristics of the included studies are presented in .
Table 1. Characteristics of the studies included in the review
Quality appraisal
As shown in the critical appraisal and , most included studies were judged to be of acceptable quality. Seven quantitative studies were assessed to be of good quality.Citation22–28 Good quality studies had an appropriate research design and provided clear description of their methodology. Five good quality studies reported on response rates,Citation24–28 which were mostly high, except for one study with a response rate of 50%.Citation26 Seven quantitative studies were assessed to be of fair quality.Citation29–35 Although some of these studies had a sample representative of the target population,Citation29,Citation31,Citation35 poor reporting made it difficult to assess the risk of selection bias in two studiesCitation30,Citation33 and two studies used sampling strategies that had the potential to introduce bias.Citation32,Citation34 Only two studies were judged to be of poor quality.Citation36,Citation37 In these, the method of selecting participants was not clearly described; thus it was difficult to assess the risk of selection bias. Samples in both studies were not based on consideration of sample statistical power.Citation36,Citation37 The two qualitative studies were of good quality, with a clear statement of the aims of the research, for which a qualitative methodology was appropriate.Citation38,Citation39 The results section for included qualitative studies was mostly well discussed and supported with relevant quotations and included appropriate implications for policy, practice and recommendations for new research.
Table 2. Quality appraisal of quantitative studies
Table 3. Quality appraisal of qualitative studies
The findings are presented below in three main themes:
Knowledge, myths and misconceptions about STIs and HIV
Awareness of STI and HIV
Seventeen studies looked at participants’ knowledge about STIs,Citation22–38 with nine specifically focused on HIV/AIDS.Citation22,Citation25–27,Citation29,Citation33–35,Citation37 A significant proportion of women studied had never heard of HIV/AIDS and many other STIs.Citation22–35,Citation37 Two studies conducted in Saudi Arabia reported that only about half of the participants had good knowledge about STIs (defined as having answered 60% or more of the question correctly).Citation22,Citation37 In the studies that examined men’s and women’s knowledge about STIs, Muslim women had better knowledge about STIs compared to Muslim men, although knowledge was low for both groups.Citation28,Citation29 One study in the UK examining knowledge of students from different religious backgrounds found that Muslim students had poorer knowledge than students from all other religions.Citation28 The majority of women who were able to name an STI mainly mentioned HIV/AIDS but had limited knowledge regarding the nature of the infection, modes of transmission, and prevention. Other STIs like chlamydia and human papilloma virus were less recognised.Citation28,Citation30,Citation32,Citation38
“I only know of HIV. I would assume it is transmitted through bodily fluids. I can’t think of any others. I was never taught about them.” (Australia)Citation38
Knowledge about STI signs and symptoms
Generally, Muslim women had poor knowledge regarding signs and symptoms of STIs, in addition to many misconceptions. Women in nine studies believed that you could identify an HIV-infected individual just by looking at them.Citation22–27,Citation33,Citation35,Citation37 In a study from Saudi Arabia, only 5% of university students knew that HIV can be asymptomatic.Citation37 Similarly, a study in Iran conducted on soon-to-be-married women showed that only 4.5% knew that a person with an STI does not necessarily look ill, and 78% did not know that painful urination could be a sign of an STI. A further 51% did not know that the presence of sores in the genital area is an STI symptom in both men and women. Poor knowledge of STIs was found among university students as well as women who were unemployed and illiterate.Citation24,Citation32
Knowledge about modes of transmission of STI
Fifteen studies reported myths and misconceptions regarding modes of transmission of STIs among Muslim women.Citation22–27,Citation29,Citation31–37,Citation39 Women in a number of studies believed STIs can be transmitted through mosquito bites, with proportions ranging from 18% to 58%. Almost 70% of college women in the United Arab Emirates (UAE) believed that they are more likely to be infected when they are menstruating.Citation26,Citation27,Citation29,Citation35–37 Sharing toilets and swimming pools were also mentioned as possible routes of transmission,Citation24,Citation26,Citation29,Citation35–37 as well as physical contact such as hand shaking or hugging.Citation26,Citation27,Citation29,Citation34–37
A number of women in four studies could not identify correct modes of transmission of STIs. HIV transmission through breastfeeding was poorly recognised, with correct answers ranging from 18% to 70%.Citation25,Citation33–35 Only 6% of young girls in one study knew that STIs can be transmitted through vaginal fluids, and 5% knew that HIV can be acquired through blood transfusion.Citation24
“HIV, well […] it’s not exactly an STI. It’s more of a cancer, isn’t it? Also the thing called “crabs.” I learnt that from movies. I don’t know how you get it through.” (Australia)Citation38
Only two studies reported good knowledge about modes of STI transmission.Citation33,Citation35 A study conducted with university students in three Arab countries reported that 90% of women correctly identified modes of STI transmission, although there were also many misconceptions. For instance, over 40% of participants believed that only homosexuals get HIV/AIDS.Citation33
Knowledge about STI prevention and treatment
Lack of knowledge about STI prevention was observed among Muslim women.Citation22–25,Citation27,Citation29–31,Citation33–35,Citation37 Nearly 93% of university students in UAE and 77% in Afghanistan believed that vaccinations could protect against HIV/AIDS.Citation27,Citation29 Women were also generally unaware of condoms for STI prevention,Citation25,Citation29,Citation30,Citation33–35,Citation37,Citation39 and only three studies reported good levels of knowledge regarding condom use, with correct answers ranging from 67% to 74%.Citation23,Citation24,Citation36
“We have heard that HIV/AIDS spreads through sexual relations and by using certain measures such as contraceptives (condoms) we can protect ourselves. But there are people who are not aware of HIV/AIDS and contract the disease from sexual contacts.” (Pakistan)Citation39
Regarding treatment of HIV/AIDS, 43–66% of women in six studies believed that it is curable.Citation23,Citation25–27,Citation29,Citation33 For example, a Demographic Health Survey in Palestine showed that 12.2% of women thought that HIV/AIDS can be treated by a traditional healer or folk medicine.Citation25 Almost 20% of university students in Egypt did not know that if one person is infected, sexual partners need to be tested and treated.Citation31
Sources of information on STI and women’s information needs
Ten studies reported on Muslim women’s sources of sexual health information.Citation23,Citation25,Citation27,Citation29–32,Citation35,Citation38,Citation39 Friends, relatives, magazines and television were the primary sources of information for women and girls.Citation27 Education in schools was a source of STI information for a minority of women (8% to 31%).Citation22,Citation23,Citation25,Citation29,Citation32 A study in Egypt reported that 10% of participants felt ashamed to ask about sexual health-related information.Citation31 Only 10% of university students in Turkey felt that information regarding sexual health issues received in schools was adequate.Citation32
Women and young girls in two studies wanted more information about STI symptoms, transmission, prevention, and treatment, and many wanted to learn about sexual health issues in schools.Citation24,Citation27
“Although my religion says I do not need to know about sexual health before having sex, I think it should be taught because girls are still going to do that stuff [. . .] It could prevent a lot of mistakes from happening.” (Australia)Citation38
Cultural influences on STI knowledge and attitude
Negative attitudes towards HIV-infected individuals
Women in ten of the studies had negative attitudes towards people infected with STIs and HIV/AIDS and were highly influenced by misconceptions and poor knowledge.Citation22,Citation25–27,Citation29,Citation33,Citation35,Citation37,Citation39,Citation40
“Our society considers those who are suffering from HIV/AIDS as having a bad personality, people will never sit, eat or have physical contact with them.” (Pakistan)Citation39
Negative attitudes were reported across studies from a range of different countries. For example, 32% of participants in a study from UAE said that “I do not feel sorry for people who caught HIV/AIDS because it is their own fault”, 81% believed that those who transmit the infection should be punished, and 53% thought that people with HIV/AIDS should be made to live apart from the general public.Citation27 In Palestine, only 15% said that people with HIV/AIDS should be allowed to teach.Citation25 One study from the southwest region of Saudi Arabia reported that 8% of young female students thought that a person with HIV should be killed or punished.Citation22
Infected women tended to be subjected to more blame and judgement compared to men, and this gender inequality was considered normal.Citation39
“The society will disgrace a woman more than a man because our culture is like that.” (Pakistan)Citation39
Attitudes towards STI education, prevention and testing
Nearly 62% of women in one Iranian study believed that education about STIs and unintended pregnancies does not lead to premarital sex.Citation24 However, some women in another qualitative study believed that there was no need for sexual education for Muslims, believing that STIs are not an issue among them, or that religious practices provided them with protection against STIs.Citation39
Negative attitudes towards HIV/AIDS and the perceptions that only certain individuals are at risk acted as a barrier to testing and diagnosis. For example, 38% of participants in a Saudi study said that they would not want to know if they had any kind of STI,Citation30 although 90% believed that their partners had the right to know if they had an STI, and 55% said that they would ask for a divorce if they found out that their partner had an STI.Citation30
Negative attitudes by healthcare providers towards premarital sex acted as a barrier to young girls’ access to sexual health information and services.Citation38
“I would prefer a female GP. If it was male GP I would feel awkward, physically and emotionally, because he might ask me if I am married and judge me because I am not.” (Australia)Citation38
Discussion
This is the first review, to our knowledge, to synthesise qualitative and quantitative evidence on STI knowledge and attitudes among Muslim women worldwide. Barriers to STI prevention, diagnosis and treatment existed on multiple levels, from personal barriers to cultural and religious barriers. Although this review included studies from all countries, the majority of studies in this review were conducted in the MENA region.
A key finding from our review is the poor overall STI knowledge among Muslim women, with HIV/AIDS being the most widely recognised STI. Although this review suggested that Muslim women’s STI knowledge was higher compared to Muslim men, women’s awareness of STI was still found to be suboptimal. This issue is particularly concerning since approximately 50% of included studies in this review focused exclusively on college students. A report on STI evidence from the MENA region confirms the results from this review. The report showed that although the majority of people in the region have heard of HIV/AIDS, they rarely know how the infection is transmitted, and have little knowledge regarding other STIs.Citation41 Poor sexual health knowledge poses a great risk to young Muslim women who engage in premarital sexual relations, and to married women whose husbands are not monogamous or are infected before marriage. These findings support existing evidence that supports the importance of sex education, particularly at school.Citation42–44
Previous literature suggested that better education is associated with higher levels of HIV/AIDS and STI awareness.Citation45 However, this review revealed that poor knowledge existed among women of all educational levels. Since sexual health is not taught in any formal setting in most Islamic countries, educational level might have little impact on STI awareness. Even among highly educated people, lack of knowledge and misconceptions still exist. For example, a study examining physicians’ knowledge in Saudi Arabia reported that almost half of the sample identified casual kissing as a mode of HIV transmission.Citation46
Significant misinformation was also found regarding modes of transmission and prevention. Condom use was poorly recognised as a measure of HIV prevention among Muslim women. However, the literature suggests that Muslims with prior knowledge of condoms expressed difficulty accessing them.Citation15 According to a report by Abu-Raddad and colleagues, awareness of condom use in Arab and Islamic countries did not predict use, and only a “fraction” of those who are aware of condom use as a measure of HIV prevention actually use them.Citation7 It is likely that the majority of extramarital sex in the region is not condom-protected.Citation47 This is likely because premarital sexual relations are forbidden in Islam, making it difficult for young individuals to access condoms openly without being judged or stigmatised.Citation4,Citation41 The issue is even more challenging for women, as they could face severe consequences for having premarital sexual relations (i.e. honour killing). Findings from another systematic review on non-Muslim youth showed that reasons for condom non-use often went beyond lack of knowledge and access barriers to social influences.Citation48 Other reasons documented in the literature for not using condoms included partners’ refusal, high condom prices, and low perceived risk of infection.Citation47 Therefore, addressing awareness without taking into account social and cultural factors would only solve a part of the issue.
Social and cultural factors influence how STIs are perceived in Muslim countries, with many Muslims believing that STIs are not an issue among them.Citation40 STI rates are not commonly reported in some Islamic countries, which might contribute to the perception of low risk found among many Muslims. Stigma surrounding at-risk individuals, particularly men who have sex with men and extramarital sex in general, also adds to the denial of the existence of STIs and HIV/AIDS among Muslims.Citation49 Findings from a review on South African youth suggested that low perceived risk resulted from societies’ tendency to deny the presence of HIV/AIDS, specifically in societies with great stigma attached to HIV/AIDS.Citation50 According to the Health Belief Model, low perceived vulnerability is a risk factor as it reduces the individual’s motivation to take protective measures.Citation51 Research indicates that higher perceived risk of STI is associated with a more responsible sexual behaviour.Citation50
Cultural and religious factors play a crucial role influencing sexual health perceptions, sexual health knowledge and needs. A number of studies on women from different religious backgrounds suggest that conservative views and social disapproval of premarital sex significantly influenced sexual health awareness and safer sex practices.Citation44,Citation52,Citation53 Therefore, for any educational intervention to work, it should be tailored to meet the target population’s specific needs. Our review showed that many women expressed a need for sexual health education. Qualitative evidence on Muslim immigrants from Canada showed that women did not oppose sex education, but felt that the sex education offered did not reflect their needs.Citation51 Research on religious leaders’ views on providing sex education showed that the majority had positive views towards providing sex education for young Muslims, with emphasis on providing a religiously sensitive content.Citation54 Efforts should be directed towards designing sex education programmes that are religiously appropriate and accepted in conservative Muslim societies.
Limitations
The literature search was conducted online, thus some relevant literature may have been missed. We located studies of Muslim women from 13 countries worldwide. However, since we excluded studies that did not clearly state that the population included Muslim women, not all countries with Muslim populations are represented in this body of evidence. Most of the studies in this review were quantitative surveys, with only two qualitative studies. Qualitative evidence facilitates an in-depth exploration of issues and the close-ended nature of survey questions provides little opportunity for participants to give their detailed accounts.Citation55 It was not possible to conduct a meta-analysis in this review as study outcomes were measured differently across included studies.
A number of primary studies in this review lacked rigour in terms of their study design, selection of participants, and reporting of findings. Furthermore, all quantitative studies in this review were of cross-sectional design and provided only simple descriptive results, with none of the results analysed by education or socio-demographic factors. However, due to the existing obstacles to conducting STI and HIV/AIDS research in the MENA region, Haghdoost and colleagues suggest that even simple descriptive studies and convenience sampling are an essential step to improving research in the region.Citation56
Policy implications
The findings from our review could be used to inform the development of a culturally sensitive sexual health education for Muslim youth. Many Muslims depend on guidance from religious leaders on many aspects of their lives. Having religious leaders on board while promoting sexual health education, as well as wider community involvement, is essential to ensure that materials are clearly understood and accepted in conservative Muslim cultures. Therefore, a key implication from this review is the need for providing comprehensive sexual health education, particularly at schools, while working with religious leaders, parents, and teachers. More public health efforts should also be directed towards increasing sexual health communication and awareness using mass media channels and the Internet to reach individuals at risk.
Implications for research
This body of evidence revealed that better quality studies, particularly in the MENA region, are needed. However, conducting high quality research might be a difficult task in some countries due to restrictions on data sharing and reporting.Citation41,Citation56 Improved reporting and better surveillance are essential for accurate future estimates to inform public health policies and prevention measures.
Evidence on barriers to HIV/AIDS and STI testing among Muslims is limited; only one qualitative study examined barriers to testing and diagnosis.Citation38 The limited research done in this area makes it difficult to draw conclusions. However, it provides insight into possible existing obstacles specific to conservative Muslim cultures. More research should be directed towards understanding and tackling barriers to STI testing and diagnosis among Muslims, particularly among women.
Conclusion
This review revealed that many Muslim women lacked proper sexual health knowledge, and that negative attitudes towards STIs acted as a barrier to accessing sexual health information and services. The need for information and education was expressed by many women. This highlights the importance for culturally sensitive sexual health education for Muslim women. The risk of and vulnerability towards STIs among Muslim women went beyond lack of knowledge to wider cultural factors. Future interventions should take into account the wider personal, cultural, and religious barriers when developing sex education interventions.
Acknowledgements
Many thanks to Sophie Pattison Clinical Support Librarian, from University College London (UCL) Library Services who assisted with developing the search strategy.
Disclosure statement
No potential conflict of interest was reported by the author(s).
ORCID
Noura Alomair http://orcid.org/0000-0001-7818-7854
Samah Alageel http://orcid.org/0000-0002-6945-5308
Julia V. Bailey http://orcid.org/0000-0002-5001-0122
Additional information
Funding
References
- WHO. Sexually transmitted infections (STIs) fact sheet; 2016. Available from: http://www.who.int/mediacentre/factsheets/fs110/en/.
- WHO. Department of Reproductive Health and Research. The sexual and reproductive health of younger adolescents: research issues in developing countries; 2011. Available from: https://www.who.int/reproductivehealth/publications/adolescence/rhr_11_15/en/.
- WHO. Global estimates shed light on toll of sexually transmitted infections; 2015 Available from: http://www.who.int/reproductivehealth/news/stis-estimates-2015/en/.
- DeJong J, Shepard B, Roudi-Fahimi F, et al. Young people’s sexual and reproductive health in the middle east and north Africa. Reprod Health Matters. 2007;14(78):8.
- DeJong J, Jawad R, Mortagy I, et al. The sexual and reproductive health of young people in the Arab countries and Iran. Reprod Health Matters. 2005;13(25):49–59.
- McFarland W, Abu-Raddad LJ, Mahfoud Z, et al. HIV/AIDS in the middle east and north Africa: new study methods, results, and implications for prevention and care. AIDS. 2010;24(Suppl 2):S1.
- Abu-Raddad LJ, Ghanem KG, Feizzadeh A, et al. HIV and other sexually transmitted infection research in the Middle East and North Africa: promising progress? Sex Transm Infect. 2013;89:iii1–iii4.
- Roudi-Fahimi F. Women's reproductive health in the Middle East and North Africa. Washington (DC): Population Reference Bureau; 2003.
- Obermeyer CM, Bott S, Sassine AJ. Arab adolescents: health, gender, and social context. J Adoles Health. 2015;57(3):252–262.
- Obermeyer CM. Adolescents in Arab countries: health statistics and social context. DIFI Family Res Proc. 2015 Apr 10;2015(1):1.
- DeJong J, El-Khoury G. Reproductive health of Arab young people. Br Med J. 2006;333(7573):849–851.
- Roudi-Fahimi F, El Feki S. (2011). Facts of life: youth sexuality and reproductive health in the Middle East and North Africa.
- DeJong J, Battistin F. Women and HIV: the urgent need for more research and policy attention in the Middle East and North Africa region. J Int AIDS Soc. 2015;18(1), 20084.
- Mumtaz GR, Kouyoumjian SP, Hilmi N, et al. The distribution of new HIV infections by mode of exposure in Morocco. Sex Transm Infect. 2013 Nov 1;89(Suppl 3):iii49–56.
- Clark KA, Keene DE, Pachankis JE, et al. A qualitative analysis of multi-level barriers to HIV testing among women in Lebanon. Cult Health Sex. 2017;19(9):996–1010.
- Centre for Reviews and Dissemination. Systematic reviews: CRD’s guidance for undertaking reviews in health care: York: Centre for Reviews and Dissemination, University of York; 2009.
- NVIVO Q. NVivo qualitative data analysis software, version 2. Cambridge: QSR International Pty Ltd; 2002.
- CASP. Qualitative research checklist; 2017. Available from: http://docs.wixstatic.com/ugd/dded87_25658615020e427da194a325e7773d42.pdf.
- CEBM. Critical appraisal of a cross-sectional study (Survey); 2014. Available from: https://www.cebma.org.
- Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version 1:b92; 2006.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45.
- Salem R, Mari S, Abd Eaziz M. Assessment of knowledge and attitudes about AIDS among secondary school girls in Mohyeil Asser. Middle East J Nurs. 2012;6(5):3–11.
- Rahimi-Naghani S, Merghati-Khoei E, Shahbazi M, et al. Sexual and reproductive health knowledge among men and women aged 15 to 49 years in metropolitan Tehran. J Sex Res. 2016;53(9):1153–1164.
- Khajehei M, Ziyadlou S, Ghanizadeh A. Knowledge of and attitudes towards sexual and reproductive health in adults in Shiraz: a need for further education. East Mediterr Health J. 2013;19(12):982–989.
- Husseini A, Abu-Rmeileh NME. HIV/AIDS-related knowledge and attitudes of Palestinian women in the occupied Palestinian territory. Am J Health Behav. 2007;31(3):323–334.
- Haroun D, El Saleh O, Wood L, et al. Assessing knowledge of, and attitudes to, HIV/AIDS among university students in the United Arab Emirates. PLoS One. 2016;11(2):e0149920.
- Ganczak M, Barss P, Alfaresi F, et al. Break the silence: HIV/AIDS knowledge, attitudes, and educational needs among Arab university students in United Arab Emirates. J Adoles Health. 2007;40(6):572.e1–572.e8.
- Coleman LM, Testa A. Sexual health knowledge, attitudes and behaviours: variations among a religiously diverse sample of young people in London, UK. Ethn Health. 2008;13(1):55–72.
- Mansoor AB, Fungladda W, Kaewkungwal J, et al. Gender differences in KAP related to HIV/AIDS among freshmen in Afghan universities. Southeast Asian J Trop Med Public Health. 2008;39(3):404–418.
- Fageeh WM. Awareness of sexually transmitted diseases among adolescents in Saudi Arabia. JKAU Med Sci. 2008 Jan 1;15(1):77–90.
- El Gelany S, Moussa O. Reproductive health awareness among educated young women in Egypt. Int J Gynaecol Obstet. 2013;120(1):23–26.
- Ekşi Z, Kömürcü N. Knowledge level of university students about sexually transmitted diseases. Procedia Soc Behav Sci. 2014 Mar 19;122:465–472.
- Badahdah AM, Foote CE. Role of shame in the stigmatization of people with human immunodeficiency virus: a survey of female college students in 3 Arab countries. East Mediterr Health J. 2010;16(9):982–987.
- Alkhasawneh E, McFarland W, Mandel J, et al. Insight into Jordanian thinking about HIV: knowledge of Jordanian men and women about HIV prevention. J Assoc Nurse AIDS C. 2014;25(1):e1–e9.
- Al-Iryani B, Raja'a YA, Kok G, et al. HIV knowledge and stigmatization among adolescents in Yemeni schools. Int Q Community Health Educ. 2010;30(4):311–320.
- Bazarganipour F, Foroozanfard F, Taghavi SA, et al. Evaluation of female youth educational needs about reproductive health in non-medical students in the city of Qom. J Family Reprod Health. 2013;7(2):67–72.
- Bakri MM. Knowledge and attitude towards HIV among academic campus for girls students, Jazan University, Saudi Arabia. Biosci Biotechnol Res Asia. 2013;10(1):241–245.
- Meldrum RM, Liamputtong P, Wollersheim D. Sexual health knowledge and needs: young Muslim women in Melbourne, Australia. Int J Health Serv. 2016;46(1):124–140.
- Hasnain SF, Johansson E, Gulzar S, et al. Need for multilevel strategies and enhanced acceptance of contraceptive use in order to combat the spread of HIV/AIDS in a Muslim society: a qualitative study of young adults in Urban Karachi, Pakistan. Glob J Health Sci. 2013;5(5):57–66.
- George P, Terrion JL, Ahmed R. Reproductive health behaviour of Muslim immigrant women in Canada. Int J Migr Health Social Care. 2014;10(2): 88–101.
- Saba HF, Kouyoumjian SP, Mumtaz GR, et al. Characterising the progress in HIV/AIDS research in the Middle East and North Africa. Sex Transm Infect. 2013;89(Suppl 3):iii5–iii9.
- Rawson H, Liamputtong P. Influence of traditional Vietnamese culture on the utilisation of mainstream health services for sexual health issues by second-generation Vietnamese Australian young women. Sex Health. 2009;6(1):75–81.
- Causarano N, Pole JD, Flicker S. Exposure to and desire for sexual health education among urban youth: associations with religion and other factors. Can J Hum Sex. 2010;19(4):169.
- Ussher JM, Rhyder-Obid M, Perz J, et al. Purity, privacy and procreation: constructions and experiences of sexual and reproductive health in Assyrian and Karen women living in Australia. Sex Cult. 2012;16(4):467–485.
- Yaya S, Bishwajit G, Danhoundo G, et al. Trends and determinants of HIV/AIDS knowledge among women in Bangladesh. BMC Public Health. 2016;16(1):812.
- Mahfouz AA, Alakija W, Al-Khozayem A-A, et al. Knowledge and attitudes towards AIDS among primary health care physicians in the Asir region, Saudi Arabia. J R Soc Health. 1995;115(1):23–25.
- Abu-Raddad L, Akala FA, Semini I, et al. Characterizing the HIV/AIDS epidemic in the Middle East and North Africa: time for strategic action. Washington, DC: The World Bank; 2010.
- Marston C, King E. Factors that shape young people's sexual behaviour: a systematic review. Lancet. 2006;368(9547):1581–1586.
- Speakman S. Comparing the impact of religious Discourse on HIV/AIDS in Islam and Christianity in Africa. Vanderbilt Undergrad Res J. 2012;8. DOI:10.15695/vurj.v8i0.3490
- Eaton L, Flisher AJ, Aarø LE. Unsafe sexual behaviour in South African youth. Soc Sci Med. 2003;56(1):149–165.
- Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2(4):328–335.
- Curtin N, Ward LM, Merriwether A, et al. Femininity ideology and sexual health in young women: a focus on sexual knowledge, embodiment, and agency. Int J Sex Health. 2011;23(1):48–62.
- Wight D, Plummer ML, Mshana G, et al. Contradictory sexual norms and expectations for young people in rural Northern Tanzania. Soc Sci Med. 2006;62(4):987–997.
- Shariati M, Babazadeh R, Mousavi SA, et al. Iranian adolescent girls’ barriers in accessing sexual and reproductive health information and services: a qualitative study. J Family Plan Reprod Health Care. 2014;40(4):270–275.
- Patten ML. Questionnaire research: a practical guide. New York: Routledge; 2016.
- Nasirian M, Karamouzian M, Haghdoost AA. Why is the number of HIV/AIDS-related publications low in the MENA region? Sex Transm Infect. 2013;89(Suppl 3):iii10.