Abstract
Contraception is essential to preventing unintended pregnancy. While contraceptive use has increased significantly over the past decade, discontinuation and gaps in use remain common. Although women cite side effects as the reason for discontinuing or stopping methods, little is known about the specific ways in which contraception affects women’s sexual experiences. This systematic scoping review aimed to understand how contraceptive-induced side effects relating to women’s sexual experiences have been measured, classified, and explored in the literature, specifically in low- and middle-income countries (LMICs). Studies were eligible for inclusion if they were peer-reviewed, English-language articles published between 2003 and 2018 that examined women’s sexual experiences related to their use of modern contraception, including sexual satisfaction, arousal, sexual dysfunction, discomfort, vaginal dryness, sexual frequency, and relationship or partner dynamics. Study populations were restricted to women of reproductive age in LMICs. Twenty-two studies were deemed eligible for inclusion, comprising a range of methods and geographies. Emergent sexual experience themes included: menstrual issues impacting sexual experience; libido; lubrication; sexual pleasure; dyspareunia; and female sexual function. Results highlight the variability in measures used, lack of a women-centred perspective, and void in research outside of high-income countries to study the influence of contraception on women’s sexual experiences. Very few studies focused on women’s sexual experiences as the primary outcome or predictor. Providers should adopt woman-centred contraceptive counselling that considers women’s relationships. Further research is needed to disentangle the nuanced effects of contraception on women’s sex lives, contraceptive decision-making, and method continuation.
Résumé
La contraception est essentielle pour prévenir les grossesses non désirées. Si l’emploi de contraceptifs a sensiblement augmenté ces dix dernières années, l’interruption de la contraception reste fréquente. Même si les femmes citent les effets secondaires comme raison pour arrêter ou abandonner les méthodes, on sait peu de choses des effets spécifiques de la contraception sur les expériences sexuelles des femmes. Cette étude systématique de portée visait à comprendre comment les effets secondaires induits par la contraception relatifs aux expériences sexuelles des femmes ont été mesurés, classés et étudiés dans les publications, précisément dans les pays à revenu faible ou intermédiaire. Les études susceptibles d’être incluses, des articles en anglais évalués par des pairs et publiés entre 2003 et 2018, examinaient les expériences sexuelles des femmes dans l’optique de leur emploi d’une contraception moderne, notamment la satisfaction sexuelle, l’excitation, les troubles sexuels, la gêne, la sécheresse vaginale, la fréquence des rapports sexuels et les dynamiques avec les relations ou le partenaire. Les populations étudiées ont été limitées aux femmes en âge de procréer dans les pays à revenu faible ou intermédiaire. Vingt-deux études ont été jugées éligibles, englobant un éventail de méthodes et de géographies. Les thèmes émergents sur les expériences sexuelles comprenaient: les problèmes menstruels ayant un impact sur l’expérience sexuelle; la libido; la lubrification; le plaisir sexuel; la dyspareunie; et la fonction sexuelle féminine. Les résultats mettent en évidence la variabilité des mesures utilisées, le manque de perspective axée sur les femmes et un vide au plan des recherches en dehors des pays à revenu élevé pour étudier l’influence de la contraception sur les expériences sexuelles des femmes. Très peu d’études se centraient sur les expériences sexuelles féminines comme principal résultat ou indicateur. Les prestataires devraient prodiguer des conseils contraceptifs axés sur les femmes qui tiennent compte des relations des femmes. De nouvelles recherches sont nécessaires pour démêler les effets nuancés de la contraception sur la vie sexuelle féminine, la prise de décision en matière de contraception et la poursuite de la méthode.
Resumen
La anticoncepción es esencial para evitar el embarazo no intencional. Pese a que el uso de anticonceptivos ha aumentado de manera significativa en la última década, el abandono de uso y las brechas en el uso continúan siendo comunes. Aunque las mujeres citan los efectos secundarios como la razón para abandonar o suspender el uso de anticonceptivos, no se sabe mucho sobre las maneras específicas en que la anticoncepción afecta las experiencias sexuales de las mujeres. Esta revisión sistemática buscó entender cómo se han medido, clasificado y explorado en la literatura los efectos secundarios inducidos por anticonceptivos con relación a las experiencias sexuales de las mujeres, en particular en países de bajos y medianos ingresos (PBMI). Los estudios elegibles para su inclusión eran artículos redactados en inglés, revisados por pares y publicados entre 2003 y 2018, que examinaban las experiencias sexuales de las mujeres relacionadas con su uso de anticonceptivos modernos, incluida su satisfacción sexual, excitación, disfunción sexual, molestia, sequedad vaginal, frecuencia sexual y dinámicas de relación o pareja. Las poblaciones del estudio fueron restringidas a mujeres en edad reproductiva en PBMI. Se determinó que 22 estudios eran elegibles para su inclusión; estos abarcaban una variedad de métodos y geografías. Entre los temas emergentes de experiencias sexuales figuraban: problemas menstruales que afectan la experiencia sexual; libido; lubricación; placer sexual; dispareunia; y función sexual femenina. Los resultados destacan la variabilidad de las medidas utilizadas, la falta de una perspectiva centrada en las mujeres y la escasez de investigaciones realizadas fuera de países de altos ingresos para estudiar la influencia de la anticoncepción en las experiencias sexuales de las mujeres. Muy pocos estudios se enfocaron en las experiencias sexuales de las mujeres como el principal resultado o predictor. Los prestadores de servicios deben adoptar consejería anticonceptiva centrada en la mujer que considere las relaciones de las mujeres. Se necesitan más investigaciones para desenredar los efectos matizados de la anticoncepción en la vida sexual de las mujeres, en su toma de decisiones anticonceptivas y en la continuación del uso de anticonceptivos.
Introduction
Nearly half of all pregnancies worldwide are mistimed or unwanted.Citation1 Unintended pregnancy rates differ substantially between developing and developed regions, varying from 127 to 28 unintended pregnancies per 1000 women in East Africa vs. Western Europe, respectively.Citation1 While contraception is an effective means to prevent unintended pregnancy, many women living in developing countries who want to prevent or delay a pregnancy are not using contraception.Citation2 Among women who are using contraception, discontinuing use while still in need of pregnancy prevention methods remains common.Citation3,Citation4 Family Planning 2020 (FP2020) estimates that one-third of women who start using contraception will stop use within one year and more than half of women will stop within two years.Citation5 The majority of women who discontinue contraception while still in need of family planning do so for method-related concerns, such as side effects.Citation2,Citation5 Concerns about side effects, both those that are clinically recognized and those that are myths or misconceptions, are well-documented as one of the primary deterrents to contraceptive use.Citation6–11
Despite evidence linking side effects to contraceptive use and discontinuation, the majority of research on this relationship is non-specific. Numerous studies have identified general side effects as reasons that women stop or switch methods,Citation4,Citation12 yet very little is known about the distinct types of side effects that increase rates of discontinuation and switching. Due to the ambiguous measurement of contraceptive side effects in most studies, the role of specific emotional, mental, and physical changes on women’s use of contraception remains largely unknown. This is particularly relevant in low- and middle-income countries (LMICs), which bear the burden of unintended pregnancies worldwide; further, many LMICs have made commitments toward achieving the FP2020 goal of enabling 120 million additional women and girls to become users of contraception by 2020.Citation13
The Demographic and Health Surveys (DHS) and Performance Monitoring for Action (PMA), previously Performance Monitoring for Accountability 2020 (PMA2020), are the two nationally representative surveys that constitute the majority of publicly available data on contraceptive use in LMICs. Neither collect information on the specific side effects women are concerned about and/or have experienced.Citation14,Citation15 Studies that have explored the role of specific side effects, such as changes to menstrual bleeding, headaches, or nausea, have generally been conducted in high-income settingsCitation16–18 or have relied on data collected within health facility systems or with special populations, thereby limiting their generalisability.Citation19–21 A recent review from Polis and colleagues, however, highlighted the significant and variable impact that changes to women's menstrual cycles have on their use of contraception.Citation22 This research underscores the importance of moving beyond the monolithic category of “side effects” to developing a more nuanced understanding of this issue.
The ways that contraception influences women’s experiences with sex, and vice versa, remain understudied. Although some research has reported on women’s contraceptive-induced side effects related to sex, including changes in libido or lubrication, many studies focus only on the experiences of women who have discontinued their use of contraception.Citation23,Citation24 Additionally, while there is evidence that contraception can improve women’s sex lives, most notably by separating sex from pregnancy and childbearing, as Higgins and Smith state, “women do not have sex in order to use contraception”.Citation25 Rather, women use contraception for a variety of reasons, one of the most common being the desire to have sex without worrying about an unintended pregnancy.Citation26,Citation27 Understanding the role that contraception-induced changes to women’s sexual experiences play in the calculus that women make about using contraception is critical.
Substantial evidence exists that changes to sexual enjoyment and pleasure affect the use of barrier methods, particularly the male condom. Specifically, decreased sexual satisfaction among men while using male condoms is a widely acknowledged barrier to men’s use of the method.Citation28–32 Other studies have noted men’s decreased sexual pleasure when their partners are using intrauterine devices (IUDs).Citation33,Citation34 While this research is valuable and contributes meaningfully to understanding a couple’s experience with sex, the influence that contraceptive methods have on women’s sexual experiences is far less understood. As the primary users of contraception, women's sex-related side effects of methods should be at the fore of family planning research. However, particularly in LMICs, cultural expectations, coupled with gender and power dynamics, often necessitate sex as an activity for procreation and rarely take into account women’s sexual desires.Citation35,Citation36
A limited, but growing, body of research from studies in the biological and social sciences has demonstrated that hormonal contraception can affect sexual function.Citation37,Citation38 A study in the United Kingdom found that approximately 10% of women using a tailored combination of the pill had lower interest in sex after initiation,Citation18 while 10% and 20% of Australian women using IUDs and implants, respectively, reported lowered libido within six months of initiation.Citation17 Similarly, a US study found that among women who discontinued the pill over the course of one year, decreased sexual thoughts and decreased psychosexual arousal were the strongest predictors of discontinuation.Citation39 These and other studies demonstrate that changes in sexual experience do occur in tandem with the use of contraceptive methods and that these changes can have a significant impact on contraceptive use. However, studies examining these relationships have largely been limited to high-income settings.Citation40–44
Complicating the understanding of this issue is the fact that side effects are generally defined using medical terminology and interpreted through a biomedical framework.Citation23 The issues that women describe, which may fall outside of the clinically expected side effects, including impact on sexual pleasure and desire, are often categorised as “other” or not included in analyses.Citation23 The current study aimed to understand how changes in women’s sexual experiences associated with their use of female-controlled modern contraceptive methods have been measured, classified, and explored in the literature, among women living in LMICs.
Methods
A scoping review was conducted to identify, collate, and summarise studies from LMICs on this topic. Scoping reviews are a useful approach for examining how research on a specific topic is conducted across contexts, clarifying concepts of interest, and identifying gaps in the knowledge base that invoke specific questions for further research.Citation45 Given this paper’s focus on describing the breadth and depth of research examining the influence of modern contraception on women’s sexual experiences, a scoping review was deemed more appropriate than a systematic review, which aims to synthesise the results of a specific research question.
Search and review strategy
Following the systematic process first described by Arskey and O’Malley,Citation46 and later expanded on by Levac, Colquhoun and O’Brien,Citation47 a search strategy was developed to guide queries of the literature (see supplementary material). Parallel searches were implemented in PubMed and Scopus in October 2018. Identified references were reviewed for manual removal of duplicate records and remaining references were then imported into Covidence, an online software program for managing systematic literature reviews. Two researchers screened titles and abstracts of each reference to determine eligibility. Articles preliminarily identified as eligible progressed to full-text screening; any disagreements were resolved by a third researcher. Full-text articles were retrieved from PubMed and Scopus and reviewed by two researchers to determine final eligibility; any disputes were resolved through discussion among team members.
Inclusion criteria
Studies were eligible for inclusion if they were peer-reviewed, English-language articles published between 2003 and 2018, that examined women’s sexual experiences related to their use of modern contraception, including sexual satisfaction, arousal, sexual dysfunction, discomfort, vaginal dryness, sexual frequency, and relationship or partner dynamics. The search was limited to articles published between 2003 and 2018 to focus on recent research that had been published within the past 15 years. Study populations were restricted to women of reproductive age (15–49 years) to capture the breadth and depth of experiences affecting women at greatest risk of pregnancy. To ensure the search captured articles that were comprehensive in terms of modern contraceptive methods and diverse changes in women’s sexual experiences, yet were reflective of the broad-ranging experiences of women of reproductive age at a population-level, exclusion criteria comprised:
Studies that assessed the effect of male-controlled contraception (e.g. condom, vasectomy) and traditional methods (withdrawal, abstinence, rhythm) on sexual experiences
Studies that examined changes in men's sexual experiences resulting from modern contraception
Studies that explored postpartum dyspareunia
Studies focusing exclusively on highly specific sub-populations (e.g. HIV-positive women, women with autoimmune/chronic diseases, women who underwent gynaecological procedures/surgeries or experienced genital mutilation or cutting)
Studies that were conducted in upper-middle-income or high-income economies as specified by the World BankCitation48
Data extraction
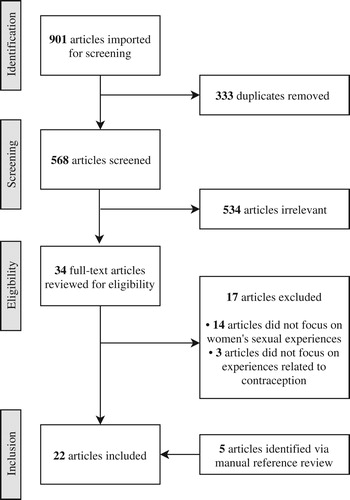
A multi-stage process of study identification and data extraction was conducted to establish the final set of included articles (). The searches in PubMed and Scopus identified 416 and 485 studies, respectively, yielding a total of 901 articles for review. Three hundred and twenty-two articles were manually removed as duplicates; another 11 duplicate records were identified by Covidence and removed (n = 333). A total of 568 articles were screened for title and abstract review, and only 34 advanced to full-text review. Initially, 17 articles were eligible for inclusion. The reference lists of these articles were reviewed in full to identify additional articles for inclusion; five articles were identified and included based on secondary review (total n included = 22). Key characteristics of each article (e.g. objective, population, study design, contraceptive method, sexual experience, results) were described in a table and analysed for similarities and variations by these variables. Study results were synthesised according to contraceptive method.
Results
Overview of studies
Twenty-two studies were deemed eligible for inclusion; study objectives, design, and sexual experience results by contraceptive method are outlined in . Study designs comprised qualitative (focus group discussions (FGDs) and in-depth interviews (IDIs); n = 8), cross-sectional (n = 5), longitudinal (n = 4), case control (n = 1), case cross-over (n = 1), and mixed-methods (n = 3). Included studies were geographically dispersed, including sub-Saharan Africa (n = 11), Asia (n = 7), Latin America (n = 3), and North Africa (n = 1).
Table 1. Overview of included studies
Several studies reported on modern methods of contraception generally (i.e. hormonal methods, barrier methods, sterilisation, lactational amenorrhea, and standard days method) or multiple types of modern contraceptive methods (n = 6). However, the majority of studies focused specifically on one method of contraception, including: female condom (n = 4), injectable (n = 4), vaginal ring (n = 2), diaphragm (n = 2), implant (n = 1), IUD (n = 2), and tubal ligation (n = 1). Most study objectives did not aim to examine sexual experiences or side effects specific to sexual pleasure, and some offered very little insight into women's sexual experiences. Methodological quality was not assessed as part of inclusion criteria; as such, diversity in methodological quality across studies persists and is addressed within the Discussion.
Results are structured by contraceptive method, namely: injectable, implant, IUD, female barrier methods, and female sterilisation, with nonspecific results for all modern contraceptive methods reported at the end. Of note, some studies report on multiple contraceptive methods and may be included within different categories.
Injectable
Four studies focused on sexual side effects specific to injectable contraceptives,Citation49–52 with two additional studies examining the injectable as part of a broader list of contraceptive methods.Citation53,Citation54 Sexual side effects discussed in relation to injectable use included reduced libido, loss of lubrication, prolonged menses, and mixed results for Female Sexual Function Index (FSFI) dimensions. These studies occurred across countries: Kenya (n = 2), Uganda (n = 1), Indonesia (n = 1), Egypt (n = 1), and Bangladesh (n = 1).
Reduced libido and lubrication were the most common side effects reported among studies on injectables. Specifically, a prospective cohort study in Kenya found that of women discontinuing the injectable within six months of initiation, 13.3% discontinued due to reduced libido.Citation52 Further, FGDs and IDIs with women in Uganda identified reduced libido as a reason for women to discontinue injectable use due to relationship strain and threats to relationship stability.Citation51 Interestingly, women in Kenya noted that decreased libido associated with injectable use could be positive, particularly for widows.Citation49 The Ugandan study further discussed contributors to discontinuation of the injectable, specifically vaginal dryness associated with injectable use as a strain to relationships and prolonged or excessive menses and menstrual spotting that began after injectable use.Citation51
Two studies examined the impact of the injectable on female sexual function.Citation50,Citation53 A cross-sectional study in Egypt reported that injectable use was significantly associated with decreased desire, arousal, lubrication, orgasm, satisfaction, and FSFI total score compared to non-users.Citation53 Conversely, a historical cohort study in Indonesia found no significant differences for desire, arousal, lubrication, orgasm, satisfaction, or dyspareunia between injectable users and non-hormonal contraceptive users.Citation50
Implant
One study, in Benin, evaluated the safety, efficacy, and acceptability of the implant. This study reported reduced libido with the use of the implant (7.3% of study participants).Citation55 Qualitative interviews in Bangladesh further explored side effects related to contraceptive use, including the implant, however, sexual side effect results were non-specific to the implant.Citation54
Intrauterine device (IUD)
Two studies specifically focused on side effects related to IUD discontinuation;Citation34,Citation56 two additional studies examined female sexual function as the result of modern contraceptive methods, including the IUD.Citation53,Citation57 One study, in India, reported that IUD discontinuation was generally due to side effects, including pain, though ambiguity remained as to whether this pain was general or exclusive to sex.Citation56 A Bangladeshi study similarly described that 19.4% of recent IUD acceptors reported dyspareunia and this was significantly associated with discontinuation.Citation34 In the two studies examining female sexual function, the Egyptian study found that the IUD was associated with decreased sexual satisfaction,Citation53 whereas the study in Peru did not find significant differences in female sexual function by IUD use.Citation58
Female barrier methods
Female barrier methods discussed in relation to sexual side effects comprised the female condom (n = 5), diaphragm (n = 2), vaginal ring (n = 2). These studies were primarily in sub-Saharan Africa (Zimbabwe (n = 2), Dominican Republic, Rwanda, Swaziland, Kenya, and Nigeria), with an additional study conducted in India.
Sex-related side effects reported in relation to female condom use included lubrication, sexual pleasure, and dyspareunia. In Swaziland, female sex workers discussed increased lubrication with the use of the female condom, attributing this increase in vaginal lubrication to a decrease in their concerns about male condom breakage or condom manipulation by clients.Citation59 Conversely, female condom users in Zimbabwe reported mixed feelings on increased lubrication provided by this method.Citation60 Four female condom studies discussed sexual pleasure, with varying results.Citation59–62 While female sex workers in Swaziland reported increased stimulation from the ring of the device,Citation59 women in Nigeria and India discussed decreased sensation,Citation61,Citation62 and women in Zimbabwe indicated decreased ability for “fondling” or physical stimulation of women’s genitals by male clients or partners.Citation60 Authors in both the Swaziland and India studies indicated that increases in pleasure may be attributed to decreased stress associated with protection from pregnancy and sexually transmitted infection acquisition; further, these studies indicated less potential for reproductive coercion or contraceptive interference by male partners or clients in contraceptive use, through use of the female condom.Citation59,Citation62 Lastly, two studies examined the female condom and dyspareunia.Citation60,Citation61 One study in Nigeria found that 5.2% of women using the female condom reported pain during sexual intercourse;Citation61 similarly, a study in Zimbabwe found the inner ring of the female condom to be “uncomfortable”.Citation60
Studies examining the vaginal ring and diaphragm further reported increased pleasure with usage.Citation63–65 In the Dominican Republic study, sexual satisfaction was only quantitively measured for men, although qualitative interviews with women described increased enjoyment and associated this increase with longer ejaculation time for male partners; the authors also indicated that a few women described the diaphragm as “bothersome” or “painful” during sex.Citation64 One study in Kenya reported reduced libido with use of the contraceptive ring (discussed by one woman in IDIs).Citation66 Lastly, within a randomised controlled trial in Rwanda, women reported an overall increase in lubrication with vaginal ring use, however, felt that lubrication decreased with prolonged use.Citation63
Female sterilisation
One study in India examined the impact of tubal ligation on sexual function and found that after undergoing tubal ligation, 71.1% of women had female sexual dysfunction, compared to 36.7% before tubal ligation.Citation67 Further, the mean of all FSFI dimensions significantly decreased after tubal ligation (p < 0.001).
Unspecified modern methods
Six studies reported results for multiple contraceptive methods.Citation53,Citation57,Citation58,Citation68–70 Three studies’ results were presented non-specific to contraceptive method;Citation57,Citation69,Citation70 these studies reported diverse results, covering dyspareunia, menstrual issues, libido, and sexual pleasure. Three studies specifically reported on the FSFI and related dimensions.Citation53,Citation57,Citation58
Two studies examined dyspareunia associated with contraceptive methods.Citation54,Citation70 The first study, conducted in India, specifically aimed to examine the national prevalence of dyspareunia and related factors; authors found that dyspareunia was higher among users of traditional contraceptive methods and contraceptive non-users, compared to users of modern contraception.Citation70 Another study, in Bangladesh, found that one-third of women experienced pain in the abdomen or vagina during sex; women associated this pain with contraceptive use (pill, injectable, implant, or IUD).Citation54
John et al. in Malawi and Jain et al. in Bangladesh further discussed the impact of contraceptive methods on sexual activity, given irregular menstruation and decreased libido.Citation54,Citation69 John et al. conducted IDIs and FGDs with women, men, and service providers on the links between sexual pleasure and all modern methods of contraception. While not explicitly discussed as an experienced side effect, both men and women perceived that modern methods made women less “sweet” towards men and that decreased libido could lead to partnership dissolution.Citation69 Female participants further discussed that prolonged bleeding due to some contraceptives was seen as disruptive to sex life, given that impromptu sex was favourable for both intimate partners.Citation69 Similarly, in Bangladesh, qualitative data described husbands’ intolerance and women’s difficulty in refusing sex given extended menstruation associated with some modern methods.Citation54
Three studies explicitly examined FSFI dimensions, including arousal, satisfaction, orgasm and pain.Citation53,Citation57,Citation58 Two studies examining any contraceptive use and female sexual function in Colombia and Peru, respectively, found no difference between contraceptive users and non-users.Citation57,Citation58 The Peruvian study further examined emergency contraception and female sexual function, finding a significant increased risk for sexual dysfunction among emergency contraceptive users.Citation58 Similarly, in Egypt, Hassanin et al. examined specific methods and found that neither IUDs or combined oral contraceptive pills impacted female sexual function; however, progestin-only pills and injectables were associated with decreased female sexual function.Citation53 Further, desire, arousal, lubrication dimensions and FSFI total score were lower in women who were using any modern methods vs. non-users.Citation53
Discussion
These results highlight the dearth of literature specific to understanding the influence of contraception on women’s sexual experiences as a side effect of use in LMICs. Nearly 600 unique articles were identified based on the specified PubMed and Scopus search terms, however, 534 were deemed irrelevant. The vast majority of studies were excluded from both full-text review and final inclusion due to a lack of focus on women’s sexual experiences; instead, many articles described side effects unrelated to sexual experiences or the impact of contraception on men’s sexual experiences. Restricting studies of contraceptive-related changes to sexual experience to focus solely on the male partner’s perspective not only limits findings, but largely discounts the importance of women’s sexual experiences. Further, of the included articles, only seven had study objectives specific to female sexual experience,Citation50,Citation53,Citation57,Citation58,Citation62,Citation67,Citation69 with four studies focusing on the wide-ranging outcome of female sexual function.Citation50,Citation53,Citation58,Citation67 As the majority of the included articles focused on alternative study aims, their discussions surrounding side effects specific to sexual experiences were often minimal. The limited reporting of female-focused, sex-specific results relating to contraceptive side effects underscores the need for further work to understand women’s sexual preferences, and perceptions and experiences of sex-related side effects in LMICs.
Articles encompassed a wide range of modern contraceptive methods, including studies specific to the injectable, implant, IUD, female barrier methods (female condom, diaphragm, vaginal ring), and female sterilisation. Of note, six studies reported broadly on contraceptive methods or modern contraceptive methods,Citation53,Citation54,Citation57,Citation58,Citation69,Citation70 with only two disaggregating results by type of method.Citation53,Citation58 Across contraceptive methods, studies overwhelmingly reported the negative impact of contraceptive methods on women’s sexual experience, including reduced libido, lubrication, and sexual pleasure, as well as heightened dyspareunia. Only studies specific to female barrier methods discussed the potentially positive impact of contraception on women’s sexual experience, particularly through increased lubrication and satisfaction; however, these studies reported inconsistent results. Moreover, included studies highlighted that some increases in sexual pleasure may be attributable to reduced stress surrounding pregnancy and sexually transmitted infections that coincides with contraceptive use, rather than side effects attributable to the method itself.Citation59,Citation62 A further understanding of sexual side effects attributed to specific types of contraceptive methods, including side effects that may be positive, is necessary to ensure that contraceptive use maximises women’s sexual health.
Results also highlight the cross-cultural variation in sexual norms and practices that factor into what is perceived as a side effect, as well as the degree of distress or inconvenience that women attribute to contraceptive side effects. For example, all but two studies reporting on lubrication discussed decreased lubrication as a negative effect.Citation51,Citation59,Citation63 However, the Zimbabwean studies described cultural preferences surrounding dryer sex, where increased lubrication was viewed negatively.Citation60,Citation65 Surprisingly, there were few studies that focused on the effect of menstrual changes on sexual experience, though all indicated that menstrual changes were disruptive to sex.Citation51,Citation52,Citation54,Citation56,Citation69 Recent literature highlights that while menstrual changes may be disruptive to sexual activity, increased or decreased menstruation is viewed differently across contexts and is largely based on women’s preferences.Citation22 These seemingly conflicting findings underscore the important role of cultural norms in shaping women’s contraceptive preferences, highlighting the fact that no one method or its side effects will be universally tolerated. Thus, assuring that a range of contraceptive methods are available, including through the development of new methods, as Darroch and colleagues argue, is critical to meeting women’s sexual and reproductive health needs.Citation7 These findings also support the central argument of Higgins and Smith, that the ways in which contraceptive methods influence women’s sexual experiences also independently inform women’s contraceptive practices.Citation25 Though these studies found contradictory evidence related to the tolerability of specific side effects on women’s sexual experience, they collectively confirmed that side effects related to sex played a key role in women’s contraceptive preferences and future use. The understanding that culture influences how acceptable and tolerated sex-related side effects are, is critical for future research and programmes to consider. Recognising women’s sexual preferences in contraceptive decision-making can aid in the design of new contraceptive methods and clinical services that better meet their needs.
This review was not without limitations. Foremost, heterogeneity in measurement of female sexual experience limited comparability of studies across settings, populations, and study designs. Four studies used the FSFI, which measured a broad range of symptoms relating to female sexual experience.Citation50,Citation53,Citation58,Citation67 Its dimensions, however, were difficult to disentangle and classify specifically to one side effect. Differences in study designs and populations further limited comparability; one study was specific to female sex workers,Citation59 whereas other studies included men and policy makers.Citation51,Citation62,Citation64,Citation69 Several studies did not define the study sample, measures, comparison groups, and terminology, including contraceptive methods included within the study. Specifically for the qualitative studies, participant demographics were often unindicated, leading to ambiguity surrounding whether men or women were the ones concerned with sex-related side effects. Lastly, given the dearth of studies specific to female sexual experience, quality of studies was not assessed as part of inclusion criteria nor were studies excluded for poor quality methods.
This review highlighted a number of critical gaps in reproductive and sexual health research. Despite recent calls for a broader understanding of how side effects inform contraceptive use, and the recognition that women’s sexual experiences matter in this equation,Citation7,Citation25,Citation71 this search did not yield any population-based studies that assessed the prevalence of contraceptive-induced side effects related to sexual experience or contraceptive dynamics. Information about how frequently women report changes in their sexual experience in relation to their use of contraception would greatly expand the evidence base for reproductive health research. Secondly, while these findings from LMICs indicate results that align with findings from high-income settings,Citation37,Citation38 significant variation in quality and measurement hindered our ability to draw conclusive results. Only two studies included a prospective evaluation of the impact of changes in sexual experience on continuation.Citation52,Citation55 More research, with higher quality study designs, including prospective cohorts, clearly defined comparison groups, and primary study aims specific to women’s sexual experiences, are necessary to strengthen our understanding of the complex relationships between sex-related side effects and contraceptive use. We encourage researchers to fill this “pleasure deficit”.Citation25,Citation71
Practice implications should focus on the role of providers in counselling on sex-related contraceptive side effects. Without attributing bodily changes to contraception and understanding the degree to which these side effects impact women’s lives, some women may be less likely to seek provider counselling or services. While all included studies examined side effects from the woman’s perspective, the two studies that also interviewed service providers indicated that few providers felt that women’s concerns with sexual side effects were justified.Citation51,Citation69 Providers must adopt woman-centred, rights-based contraceptive counselling approaches that consider women’s relationships and changes to intimacy in order to increase women’s method satisfaction and well-being, and ultimately, decrease contraceptive discontinuation and unintended pregnancy.
Conclusion
In an effort to prevent unintended pregnancy by increasing access to and use of contraception, researchers, practitioners and clinicians must recognise and respond to women’s sexual health needs. The current study underscores a neglected research focus on the ways that contraception affects women’s sexual experiences in LMICs. This limited understanding of sex-related side effects and their influence on contraceptive dynamics hinders progress toward improving satisfaction and continued use of methods. Woman-centred contraceptive counselling that accounts for the myriad effects of contraception on women’s sexual well-being, including menstrual irregularities, changes in libido and sexual pleasure, and dyspareunia, may better equip women to make informed decisions about contraception and address any sex-related contraceptive side effects they experience. Future research should adopt concerted focus on the impact of side effects, particularly those that influence women’s sexual experiences and relationships.
Supplemental Material
Download MS Word (29.4 KB)Acknowledgements
We acknowledge Vaiddehi Bansal and Aley King for assistance with the literature review. SNW, CK, and LZ all contributed to conception and design of search strategy, review of articles, analysis, and interpretation of findings; drafting and revising the article; and final approval of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplementary material for this article can be accessed at https://doi.org/10.1080/26410397.2020.1763652
References
- Bearak J, Popinchalk A, Alkema L, et al. Global, regional, and subregional trends in unintended pregnancy and its outcomes from 1990 to 2014. Lancet Glob Heal. 2018;6(4):e380–e389. DOI:10.1016/S2214-109X(18)30029-9.
- Guttmacher Institute. Adding it up: investing in contraception and maternal and newborn health, 2017. New York (NY): Guttmacher Institute; 2017.
- Ali M, Cleland J. Determinants of contraceptive discontinuation in six developing countries. J Biosoc Sci. 1999;31:343–360. doi: 10.1017/S0021932099003430
- Westhoff CL, Heartwell S, Edwards S, et al. Oral contraceptive discontinuation: do side effects matter? Am J Obstet Gynecol. 2007;196(4):1–14. doi: 10.1016/j.ajog.2006.12.015
- Castle S, Askew I. Contraceptive discontinuation: reasons, challenges, and solutions. New York (NY); 2015.
- Diamond-Smith N, Campbell M, Madan S. Misinformation and fear of side-effects of family planning. Cult Health Sex. 2012;14(4):421–433. doi: 10.1080/13691058.2012.664659
- Darroch JE, Sedgh G, Ball H. Contraceptive technologies: responding to women’s needs. New York (NY): Guttmacher Institute; 2011.
- Bradley SE, Schwandt H, Khan S. Levels, trends, and reasons for contraceptive discontinuation. Washington (DC): MEASURE DHS; 2009.
- Sedgh G, Ashford LS, Hussain R. Unmet need for contraception in developing countries: examining women’s reasons for not using a method. New York (NY): Guttmacher Institute; 2016.
- Abiodun OM, Balogun OR. Sexual activity and contraceptive use among young female students of tertiary educational institutions in Ilorin, Nigeria. Contraception. 2009;79:146–149. DOI:10.1016/j.contraception.2008.08.002.
- Sedgh G, Hussain R. Reasons for contraceptive nonuse among women having Unmet need for contraception in developing countries. Stud Fam Plann. 2014;45(2):151–169. doi: 10.1111/j.1728-4465.2014.00382.x
- Casterline JB, Sinding SW. Unmet need for family planning in developing countries and implications for population policy. Popul Dev Rev. 2000;26(4):691–723. doi: 10.1111/j.1728-4457.2000.00691.x
- Family Planning 2020. Factsheet family planning 2020: new and renewed commitments. Washington (DC); 2016. Available from https://www.familyplanning2020.org/sites/default/files/FP2020_New_Commitments_7.13.2016-FINAL.pdf
- DHS. Demographic and Health Surveys: model woman’s questionnaire. 2016;(1):1–75.
- Zimmerman L, Olson H, Tsui A, et al. PMA2020: rapid turn-around survey data to monitor family planning service and practice in ten countries. Stud Fam Plann. 2017;48(3):293–303. DOI:10.1111/sifp.12031.
- Cristobal I, Ignacio LL, De la Viuda E, et al. One year quality of life measured with SEC-QoL in levonorgestrel 52 mg. Contraception. 2016;93:367–371. doi: 10.1016/j.contraception.2015.12.014
- Wong RC, Bell RJ, Thunuguntla K, et al. Implanon users are less likely to be satisfied with their contraception after 6 months than IUD users. Contraception. 2009;80:452–456. DOI:10.1016/j.contraception.2009.03.021.
- Stephenson J, Shawe J, Panicker S, et al. Randomized trial of the effect of tailored versus standard use of the combined oral contraceptive pill on continuation rates at 1 year. Contraception. 2013;88:523–531. doi: 10.1016/j.contraception.2013.03.014
- Asaye MM, Nigussie TS, Ambaw WM. Early Implanon discontinuation and associated factors among Implanon user women in Debre Tabor Town, public health Facilities, Northwest Ethiopia, 2016. Int J Reprod Med. 2018:1–10. doi: 10.1155/2018/3597487
- Modesto W, Bahamondes MV, Bahamondes L. A randomized clinical trial of the effect of intensive versus non-intensive counselling on discontinuation rates due to bleeding disturbances of three long-acting reversible contraceptives. Hum Reprod. 2014;29(7):1393–1399. DOI:10.1093/humrep/deu089.
- Nanda K, Morrison CS, Kwok C, et al. Discontinuation of oral contraceptives and depot medroxyprogesterone acetate among women with and without HIV in Uganda, Zimbabwe and Thailand. Contraception. 2011;83:542–548. DOI:10.1016/j.contraception.2010.09.003.
- Polis CB, Hussain R, Berry A. There might be blood: a scoping review on women’s responses to contraceptive-induced menstrual bleeding changes. Reprod Health. 2018;15(114):1–17.
- Inoue K, Barratt A, Richters J. Does research into contraceptive method discontinuation address women’s own reasons? A critical review. J Fam Plann Reprod Heal Care. 2015;41:292–299. DOI:10.1136/jfprhc-2014-100976.
- Fruzzetti F, Perini D, Fornaciari L, et al. Discontinuation of modern hormonal contraceptives: an Italian survey. Eur J Contracept Reprod Heal Care. 2016;21(6):449–454. doi: 10.1080/13625187.2016.1234598
- Higgins JA, Smith NK. The sexual acceptability of contraception: reviewing the literature and building a new concept. J Sex Res. 2016;53(4–5):417–456. DOI:10.1080/00224499.2015.1134425.
- Cleland J, Ali MM, Shah I. Trends in Protective Behavior among Single vs. married young women in Sub-Saharan Africa: The Big Picture. Reprod Health Matters. 2006;14(28):17–22. doi: 10.1016/S0968-8080(06)28250-8
- Frost JJ, Lindberg LD. Reasons for using contraception: perspectives of US women seeking care at specialized family planning clinics. Contraception. 2013;87:465–472. doi: 10.1016/j.contraception.2012.08.012
- Higgins JA, Wang Y. The role of young adults’ pleasure attitudes in shaping condom use. Am J Public Health. 2015;105(7):1329–1332. DOI:10.2105/AJPH.2015.302567.
- Geter A, Crosby R. Condom refusal and young black men: the influence of pleasure, sexual partners, friends. J Urban Heal. 2014;91(3):541–546. DOI:10.1007/s11524-014-9869-4.
- Morrison-Beedy D, Carey M, Feng C, et al. Predicting sexual risk behaviours among adolescent and young women using a prospective diary method. Res Nurs Heal. 2008;31:329–340. doi: 10.1002/nur.20263
- Harper G, Hosek S, Contreras R, et al. Psychosocial factors impacting adolescent condom use: a review and theoretical integration. J HIV/AIDS Prev Educ Child Adol. 2003;5:33–69. doi: 10.1300/J129v05n03_03
- Norton T, Bogart L, Cecil H, et al. Primacy of affect over cognition in determining adult men’s condom use behavior: a review. J Appl Soc Psychol. 2005;35:2493–2534. doi: 10.1111/j.1559-1816.2005.tb02112.x
- Urbina J. My boyfriend feels my strings! What do I do? Contraception. 2017;96(4):280. doi: 10.1016/j.contraception.2017.07.069
- Bradley JE, Shbnam F, Beattie TS, et al. Blood, men and tears: keeping IUDs in place in Bangladesh. Cult Health Sex. 2009;11(5):543–558. DOI:10.1080/13691050902919093.
- Gipson JD, Hindin MJ. Marriage means having children and forming your family, so what is the need of discussion? Communication and negotiation of childbearing preferences among Bangladeshi couples. Cult Health Sex. 2007;9(2):185–198. doi: 10.1080/13691050601065933
- Gage AJ. Sexual activity and contraceptive use: the components of the decision making process. Stud Fam Plann. 1998;29(2):154–166. doi: 10.2307/172156
- Elaut E, Buysse A, De SP, et al. Relation of androgen receptor sensitivity and mood to sexual desire in hormonal contraception users. Contraception. 2012;85:470–479. DOI:10.1016/j.contraception.2011.10.007.
- Sabatini R, Cagiano R. Comparison profiles of cycle control, side effects and sexual satisfaction of three hormonal contraceptives. Contraception. 2006;74:220–223. DOI:10.1016/j.contraception.2006.03.022.
- Sanders SA, Graham CA, Bass JL, et al. A prospective study of the effects of oral contraceptives on sexuality and well-being and their relationship to discontinuation. Contraception. 2001;64:51–58. doi: 10.1016/S0010-7824(01)00218-9
- Strufaldi R, Pompei LM, Steiner ML, et al. Effects of two combined hormonal contraceptives with the same composition and different doses on female sexual function and plasma androgen levels. Contraception. 2010;82: 147–154. DOI:10.1016/j.contraception.2010.02.016.
- Zethraeus N, Dreber A, Ranehill E, et al. Combined oral contraceptives and sexual function in women – a double-blind, randomized, placebo- controlled trial. J Clin Endocrinol Metab. 2016;101(11):4046–4053. DOI:10.1210/jc.2016-2032.
- Caruso S, Agnello C, Romano M, et al. Preliminary study on the effect of four-phasic estradiol valerate and dienogest (E2V / DNG) oral contraceptive on the quality of sexual life. Int Soc Sex Med. 2011;8:2841–2850. DOI:10.1111/j.1743-6109.2011.02409.x.
- Caruso S, Sareri MI, Agnello C, et al. Conventional vs. extended-cycle oral contraceptives on the quality of sexual life : comparison between two regimens containing 3 mg drospirenone and 20 mg ethinyl estradiol. Int Soc Sex Med. 2011;8:1478–1485. DOI:10.1111/j.1743-6109.2011.02208.x.
- Enzlin P, Weyers S, Janssens D, et al. Sexual functioning in women using levonorgestrel-releasing intrauterine systems as compared to copper intrauterine devices. J Sex Med. 2011;9:1065–1073. DOI:10.1111/j.1743-6109.2011.02266.x.
- Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(143):1–7.
- Arksey H, Malley LO. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. DOI:10.1080/1364557032000119616.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(69):1–9.
- World Bank. World Bank Country and Lending Groups. 2019. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
- Burke HM, Ambasa-Shisanya C. Qualitative study of reasons for discontinuation of injectable contraceptives among users and salient reference groups in Kenya. Afr J Reprod Health. 2011;15(2):67–78.
- Djami ME I, Mafluha Y, Tjandra O, et al. Sexual function of depot medroxyprogesterone acetate users Akademi Kebidanan. J South India Medicolegal Assoc. 2018;10(2):108–113. DOI:10.5281/zenodo.1462146.
- Hyttel M, Rasanathan JJ, Tellier M, et al. Use of injectable hormonal contraceptives: diverging perspectives of women and men, service providers and policymakers in Uganda. Reprod Health Matters. 2012;20(40):148–157. DOI:10.1016/S0968-8080(12)40654-1.
- Wanyonyi SZ, Stones WR, Sequeira E. Health-related quality of life changes among users of depot medroxyprogesterone acetate for contraception. Contraception. 2011;84:e17–e22. DOI:10.1016/j.contraception.2011.05.022.
- Hassanin AM, El-Halwagy AM, Ismail NN, et al. A study of the impact of the commonly used female contraceptive methods in Egypt on female sexual function. J Sex Marital Ther. 2018;44(6):605–612. DOI:10.1080/0092623X.2018.1437579.
- Jain A, Reichenbach L, Ehsan I, et al. “Side effects affected my daily activities a lot”: a qualitative exploration of the impact of contraceptive side effects in Bangladesh. Open Access J Contracept. 2017;8:45–52. doi: 10.2147/OAJC.S140214
- Aisien A, Safety EM. Efficacy and acceptability of Implanon a single rod implantable contraceptive (etonogestrel) in University of Benin Teaching Hospital. Niger J Clin Pract. 2010;13(3):331–335.
- Sharma M, Joshi S, Nagar O, et al. Determinants of intrauterine contraceptive device discontinuation among Indian women. J Obstet Gynecol India. 2014;64(3):208–211. DOI:10.1007/s13224-014-0516-5.
- Echeverry MC, Arango A, Castro B, et al. Study of the prevalence of female sexual dysfunction in sexually active women 18 to 40 years of age in Medellín, Colombia. J Sex Med. 2010;7:2663–2669. DOI:10.1111/j.1743-6109.2009.01695.x.
- Escajadillo-vargas N, Mezones-Holguin E, Castro-Castro J, et al. Sexual dysfunction risk and associated factors in young Peruvian University women. J Sex Med. 2011;8:1701–1709. DOI:10.1111/j.1743-6109.2011.02259.x.
- Mathenjwa T, Maharaj P. ‘Female condoms give women greater control’: a qualitative assessment of the experiences of commercial sex workers in Swaziland. Eur J Contracept Reprod Heal Care. 2012;17:383–392. DOI:10.3109/13625187.2012.694147.
- Francis-Chizororo M, Natshalaga NR. The female condom: acceptability and perception among rural women in Zimbabwe. Afr J Reprod Health. 2003;7(3):101–116. doi: 10.2307/3583295
- Okunlola M, Morhason-Bello I, Owonikoko K, et al. Female condom awareness, use and concerns among Nigerian female undergraduates. J Obstet Gynaecol. 2006;26(4):353–356. DOI:10.1080/01443610600613516.
- Bowling J, Dodge B, Bindra N, et al. Female condom acceptability in urban India: examining the role of sexual pleasure. J Health Psychol. 2018;23(2):218–228. DOI:10.1177/1359105317745963.
- Kestelyn E, Van Nuil JI, Umulisa MM, et al. High acceptability of a contraceptive vaginal ring among women in Kigali, Rwanda. PLoS One. 2018;13(6):e0199096. doi: 10.1371/journal.pone.0199096
- Coffey PS, Kilbourne-Brook M, Brache V, et al. Comparative acceptability of the SILCS and Ortho ALL-FLEX ® diaphragms among couples in the Dominican Republic. Contraception. 2008;78:418–423. DOI:10.1016/j.contraception.2008.07.001.
- Buck J, Kang M, Van Der SA, et al. Barrier method preferences and perceptions among Zimbabwean women and their partners. AIDS Behav. 2005;9(4):415–422. DOI:10.1007/s10461-005-9013-2.
- McLellan-Lemal E, Ondeng’e K, Gust D, et al. Contraceptive vaginal ring experiences among women and men in Kisumu, Kenya: a qualitative study. Front Womens Heal. 2017;2(1):1–16.
- Kunkeri SP, Rao TS, Andrade C. Study of sexual functioning and disorder in women before and after tubal sterilization (tubectomy). Indian J Psychiatry. 2019;59:63–68. DOI:10.4103/0019-5545.204433.
- Jain AK, Obare F, RamaRao S, et al. Reducing unmet need by supporting women with met need. Int Perspect Sex Reprod Health. 2013;39(3):133–141. DOI:10.1363/3913313.
- John BNA, Chipeta E, John NA. Sexual pleasure, partner dynamics and contraceptive use in Malawi. Int Perspect Sex Reprod Health. 2015;41(2):99–107. DOI:10.1363/4109915.
- Padmadas SS, Stones R, Matthews Z. Dyspareunia and urinary sensory symptoms in India: population-based study. J Sex Med. 2006;3:114–120. DOI:10.1111/j.1743-6109.2005.00103.x.
- Higgins JA, Hirsch JS. The pleasure deficit: revisiting the “sexuality connection” in reproductive health. Int Fam Plan Perspect. 2007;33(3):133–139. doi: 10.1363/3313307