Abstract
Globally, LGBTQIA+ individuals experience several health disparities. This qualitative exploratory study aimed to understand the experiences of discrimination faced by LGBTQIA+ patients in Indian hospitals using a human rights perspective. Self-identified LGBTQIA+ patients, cis-gender heterosexual employees, and administrators attending/working at public, private, and non-profit trust hospitals were interviewed in Mumbai and Delhi. The “right to non-discrimination” emerged as the central theme, with systemic and organisational discrimination as core themes. LGBTQIA+ patients faced intersectional discrimination, which had implications for their dignity and wellbeing. Discrimination in public hospitals was explicit, whereas discrimination in trust and private hospitals was subtle. Employees of core departments like psychiatry, dermatology, and HIV services, which routinely catered to LGBTQIA+ patients, were more sensitised than other departments. Most administrators and doctors were not familiar with the varied needs of the LGBTQIA+ spectrum and treated them as a homogenous group. Public hospitals did not have separate human resource departments, and most of the gender-affirmative guidelines/policies were not inclusive of the entire LGBTQIA+ spectrum. Trust hospitals, especially those with religious affiliations, tended not to have LGBTQIA+ inclusive policies. Some administrators believed that serving the minuscule LGBTQIA+ population may adversely affect business in private hospitals. Policymakers, government, and executives need to be accountable at the systemic level for better enforcement of ratified treaties and laws, designing inclusive public health policies, and reforming medical curricula. Hospital and healthcare administrators must be accountable for implementing inclusive policies and practices and creating a non-discriminatory environment for LGBTQIA+ patients.
Résumé
Dans le monde, les individus LGBTQIA+ font face à plusieurs disparités dans le domaine de la santé. Cette étude exploratoire qualitative avait pour but de comprendre l’expérience de la discrimination vécue par les patients LGBTQIA+ dans les hôpitaux indiens à l’aide d’une perspective des droits de l’homme. Des patients auto-identifiés comme LGBTQIA+ ainsi que des employés et des administrateurs cisgenres ont été interrogés à Mumbai et Delhi; ils appartenaient à des hôpitaux publics, privés et caritatifs à but non lucratif. Le “droit à la non-discrimination” est apparu comme le thème central, avec la discrimination systémique et organisationnelle comme thèmes de base. Les patients LGBTQIA+ se heurtent à une discrimination intersectionnelle, qui a des conséquences sur leur dignité et leur bien-être. La discrimination dans les hôpitaux publics était explicite, alors que la discrimination dans les hôpitaux privés et caritatifs était subtile. Les employés de départements essentiels comme la psychiatrie, la dermatologie et la prise en charge du VIH, qui soignaient régulièrement les patients LGBTQIA+, étaient plus sensibilisés au problème que d’autres départements. La plupart des administrateurs et des médecins n’étaient pas familiers des différents besoins du spectre LGBTQIA+ et traitaient ces patients comme un groupe homogène. Les hôpitaux publics ne possédaient pas de départements distincts de ressources humaines et la plupart des directives/politiques d’affirmation du genre n’incluaient pas la totalité du spectre LGBTQIA+. En général, les hôpitaux caritatifs, en particulier les établissements ayant des liens religieux, n’avaient pas de politiques d’inclusion des patients LGBTQIA+. Certains administrateurs pensaient que le traitement de la minuscule population LGBTQIA+ pouvait influer négativement sur l’activité des hôpitaux privés. Les décideurs, le gouvernement et les cadres doivent rendre compte au niveau systémique d’une meilleure application des lois et traités ratifiés, en définissant des politiques de santé publique inclusives et en réformant le programme des études médicales. Les administrateurs hospitaliers et des soins de santé doivent rendre compte de la mise en œuvre de politiques et pratiques inclusives et de la création d’un environnement non discriminatoire pour les patients LGBTQIA+.
Resumen
A nivel mundial, las personas LGBTQIA+ sufren graves disparidades de salud. El objetivo de este estudio cualitativo exploratorio era entender las experiencias de la discriminación enfrentada por pacientes LGBTQIA+ en hospitales indios, desde la perspectiva de los derechos humanos. Pacientes que se identificaron como LGBTQIA+ y empleados y administradores heterosexuales cisgénero, que pertenecían a fundaciones hospitalarias públicas, privadas y sin fines de lucro, fueron entrevistados en Mumbai y Delhi. El derecho a la “no discriminación” surgió como tema central, con la discriminación sistémica e institucional como temas fundamentales. Los pacientes LGBTQIA+ enfrentaban discriminación interseccional, con implicaciones para su dignidad y bienestar. La discriminación en hospitales públicos era explícita, mientras que la discriminación en fundaciones hospitalarias y en hospitales privados era sutil. Los empleados de departamentos básicos como psiquiatría, dermatología y servicios de VIH, que rutinariamente atendían a pacientes LGBTQIA+, estaban más sensibilizados que otros departamentos. La mayoría de los administradores y médicos no estaban familiarizados con las diversas necesidades del espectro de personas LGBTQIA+ y las trataban como un grupo homogéneo. Los hospitales públicos no tenían departamentos de recursos humanos por separado, y la mayoría de las directrices/políticas afirmativas de género no incluían todo el espectro de personas LGBTQIA+. Las fundaciones hospitalarias, en particular aquellas con afiliaciones religiosas, tendían a no tener políticas inclusivas de LGBTQIA+. Algunos administradores creían que atender a la minúscula población LGBTQIA+ podría afectar de manera adversa los servicios en los hospitales privados. Los formuladores de políticas, el gobierno y los ejecutivos deben responsabilizarse a nivel sistémico de imponer mejor el cumplimiento de las leyes y los tratados ratificados, de formular políticas inclusivas de salud pública y de reformar los currículos médicos. Los administradores hospitalarios y sanitarios deben responsabilizarse de aplicar políticas y prácticas inclusivas y de crear un entorno no discriminatorio para pacientes LGBTQIA+.
Introduction
Lesbian, Gay, Bisexual men and women, Transgender, Queer, Intersex, Asexual, and other gender spectrums, commonly called LGBTQIA+, have diverse health concerns and needs. Within the LGBTQIA+ community, there may exist wide variations in experiences by age, caste, class, region, religion, and other factors. Globally, individuals of the LGBTQIA+ community often encounter serious human rights violations due to the criminalisation of their sexual orientation or legal non-recognition of their gender.Citation1 LGBTQIA+ persons have reported experiences of abuse, exclusion, discrimination, and prejudice, including in jobs, education, healthcare, and social services.Citation2
Many studies have documented the discrimination experienced by LGBTQIA+ persons in healthcare settings. A global systematic review reported routine discrimination, including some cases of physical and verbal violence during physical examination in healthcare settings, against LGBTQIA+ individuals.Citation3 A 2017 national survey in the US reported that over 50% (of 289) of LGBTQIA+ individuals accessing healthcare services suffered from interpersonal prejudice, including insults, micro-aggression, sexual harassment, and abuse.Citation4 However, there is scarce literature in the Indian context that highlights the experiences of LGBTQIA+ individuals in Indian hospital settings. A recent blogCitation5 highlighted a few layers of discrimination that LGBT+ patients face at Indian hospitals. Forms of discrimination included judgment at the hospital entrance gate, refusal of treatment, lack of understanding about sex- and gender-related diseases, and labelling non-heterosexual sexual orientation as a psychological disorder. The blog also highlighted that admission forms allowed only for gender binaries, personnel refused to use the appropriate pronouns when referring to a person of the LGBTQIA+ community, there were ward allocation challenges, individuals had difficulty explaining same-sex relationships to doctors, the doctors were unequipped or untrained, and there was a lack of medical research on the health problems of the community. All of these impacted on the health-seeking behaviour of LGBTQIA+ individuals.
Health care providers’ (HCP) understanding of LGBTQIA+ individuals is narrow and primarily disease-orientated. Almost half of the interviewed mental health professionals in Mumbai and Pune reported treating homosexuality as a mental health issue and not dealing with the problems of stigmatisation, discrimination, and stressful social experiences of the individual.Citation6 Many HCPs attributed homosexuality to adverse environmental factors like child sexual abuse, early sexual initiation/ exploration, and lack of exposure to the opposite sex.Citation6
Despite growing proposals and initiatives to incorporate LGBTQIA+ concerns into healthcare curricula,Citation7 and numerous publications that distinguish clinical LGBTQIA+ competencies,Citation8 only a few health professional schools provide appropriate LGBTQIA+ health training.Citation9 Studies conducted among nursing,Citation10 medical,Citation11 and dentalCitation12 students, residents of the emergency department,Citation13 oncologists,Citation14 social workers,Citation15 and obstetricians/gynaecologistsCitation16 reveal lack of LGBTQIA+ knowledge and training. LGBTQIA+ patients need HCPs who can identify their unique health needs. However, the LGBTQIA+ community in India still faces rampant bias and discrimination in health care on account of the outlook of the medical fraternity, deficiencies in medical training, outdated curricula and textbooks, and ill-informed and poorly equipped doctors, all of which have a negative impact on health outcomes and also increase health disparities.Citation17
While a modest body of literature is available on LGBTQIA+ health in India, it is mainly limited to viewing LGBTQIA+ individuals as a key population for HIV/AIDS and mental health issues. Evidence of challenges faced by LGBTQIA+ individuals due to administrative procedures, policies, and practices of hospitals and other health facilities is scarce, especially in India. Additionally, there is scarce literatureCitation18,Citation19 that uses a human rights-based approach to analyse discrimination and power imbalances due to human resource policies and guidelines in the healthcare settings, that create challenges for LGBTQIA+ individuals.
Hence, the main aim of the present study is to understand discrimination against LGBTQIA+ patients in Indian hospitals from a human rights perspective. Additionally, the study also tries to understand administrative policies, procedures, processes of Strategic Human Resource Management, and Diversity and Equality Management practices adopted for inclusion of LGBTQIA+ patients in selected Indian hospitals.
Methods
Study design and population
This study was conducted in two metropolitan Indian cities - Mumbai and Delhi, the two most populous cities of India, which have a large presence of LGBTQIA+ individualsCitation20 and a wide network of public, trust, and private hospitals. Mumbai is India's second-most populous metropolis after Delhi.Citation21 By 2030, Delhi is projected to overtake Tokyo as the world's largest city by urban area and Mumbai as the world's 6th largest city by population size.Citation21 According to the recent Ipsos LGBT+ Pride 2021 Global Survey report, 17% of those surveyed in India (n = 500) do not identify with heterosexual sexual orientation.Citation22
Although LGBTQIA+ individuals are diverse in terms of sexual orientation, gender identity and expression, and sex characteristics, and have different healthcare needs, they are considered together for the purpose of this study.
Given the marginalisation and exclusion of the LGBTQIA+ community and the lack of earlier studies on this area, an exploratory qualitative research approach was employed to collect data. Using non-probability and non-random sampling techniques, the study was undertaken in two each public, private and Trust hospitals, with two sets of participants: the first, self-identified LGBTQIA+ patients and the second, heterosexual cis-gendered employees and administrators in each selected hospital. We approached eight hospitals of which six agreed to be part of the study.
We used convenience sampling to interview the employees and administrative staff from the respective hospitals. The employees and administrative staff from the departments such as dermatology, venereology, endocrinology, gynaecology, proctology, and surgery were first interviewed as these specialisations cater to LGBTQIA+ niche needs. Later, the staff from other specialisations were interviewed. The LGBTQIA+ patients were recruited using snowball sampling, given the hidden nature of LGBTQIA+ identity. Our first point of contact for snowballing was a person from the first author's network who had received treatment from any one of the study hospitals and they further connected us with other LGBTQIA+ patients. The total interviewed sample size consists of 15 self-identified LGBTQIA+ patients and 23 cis-gendered (11 men and 12 women) employees and administrative staff.
Data collection
Using key-informant and in-depth interview guidelines, respectively, data was collected between March and August 2019 from the cis-gendered employees, administrators, and LGBTQIA+ patients. The interview guidelines for the employees and administrators covered socio-demographic status, experiences with LGBTQIA+ patients, preparedness of hospitals to provide services to LGBTQIA+ persons, and questions about policies and practices in their respective hospitals. For the LGBTQIA+ patients, the first author spent a good amount of time building rapport before briefing them about the study objectives. Their interview guidelines included socio-demographic status, health care and hospital-specific narratives of the experiences of the LGBTQIA+ patients.
Most interviews lasted for an average of 35–40 minutes and were conducted by the first author in English and local languages. Further probing questions were asked whenever a long answer was not received from the participants. We audio-recorded the interviews. Although no specific questions on discrimination were asked, a lot of narratives and experiences emerged around discrimination. Each of the interviews was carefully analysed before proceeding to the next interview to identify any new or emerging issues. The new probes were included in the subsequent discussions that encouraged more discussions and information. A unique number was allotted to each participant interview for identification and analysis. The interview process stopped when the two sets of the study participants achieved information saturation. All recordings were deleted after being transcribed. All data in the transcripts have been anonymised. The identities of the hospitals and study participants were strictly masked using unique numbers.
Data analysis
The interviews were transcribed and translated into English by the first two authors and analytical, reflective memos were prepared manually using Excel 2013. These were first open coded. Coding and abstraction were done by the authors for each of the thematic categories, after systematic and detailed discussions. Subsequently, through thematic analysis, using a human rights-based approach, the “right to non-discrimination” emerged as the central theme. Two dominant themes emerged within the central theme: “discrimination at systemic level” and “discrimination at organisational level”. Using a selective approach,Citation23 two to six categories/ sub-themes emerged under each theme. An analysis of the relationships between different themes was also undertaken (as presented in of the findings section).
Research team and reflexivity
The authors belong to a social science institute whose core values are protecting dignity, equality, social justice, and human rights for all. The first author has expertise in hospital administration and self-identifies as a queer individual, which helped build rapport and gain the trust of all the research participants. The other authors self-identify as cis-het individuals and have extensive experience in the field of healthcare administration and public health. The first author's inner motivation and lived experience for the research area, and his easy entry into various LGBTQIA+ independent and cultural groups helped get better insights for the study. The expertise of other authors helped shape the analysis through an interdisciplinary approach.
Ethical consideration
All the LGBTQIA+ and heterosexual cis-gender individuals who participated in the research in any way were informed in their language about the research. They were entitled to refuse to participate in the study or to answer questions that made them uncomfortable. Most LGBTQIA+ participants were either closeted or only open to some, hence it was necessary to take all the steps required to protect them from any physical or mental damage. Thus, participants’ privacy and identity were protected by anonymising them and using a unique number to refer to them. In addition, it was ensured that the information given by the participants during the interview and used in the research would not allow the tracing back or monitoring of that person. Formal approval for the study was granted by Tata Institute of Social Sciences, Mumbai (SHSS/SB/AK/PB) on 18th December 2020.
Findings
Socio-demographic profile
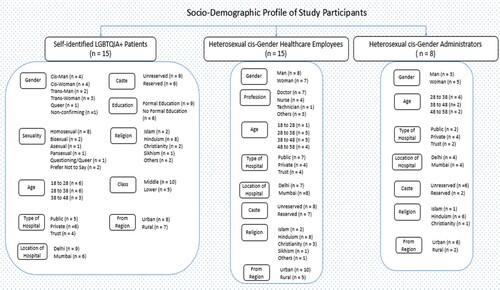
The socio-demographic profiles of participants including self-identified LGBTQIA+ patients (15), cis-gender heterosexual employees of the hospitals (15), and cis-gender heterosexual hospital administrators (8) are given in .
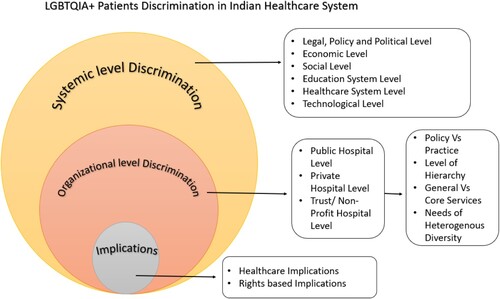
The right to non-discrimination emerged as the central theme of the study. A conceptual framework () was used to understand the multifaceted and interactive impact of discrimination which helped to shed light on systemic and organisational factors and identify explicit and implicit discrimination at the systems level, organisational leverage points, and their implications on LGBTQIA+ health (see ).
Systemic level discrimination
Discrimination is defined as an unreasonable difference in treatment or consequence causally linked to a legally prohibited basis. When a person receives less favourable treatment than others in similar situations, it is known as direct discrimination. However, we sometimes overlook more subtle or indirect discrimination, such as unconscious bias, which is embedded into the system's fabric. Discrimination at the systemic level is often an indirect form of discrimination which has benefits for some and drawbacks for others.Citation24
It is essential to focus on systemic level discrimination because LGBTQIA+ identities have a long history of criminalisation and pathologisation in India and globally. They often experience disproportionate stressors and are held to different standards. Humiliation, persecution, stigmatisation and marginalisation often result in exclusion and systemic harassment. This exclusion and discrimination violates their right to health as it hinders their access to healthcare services and impacts the quality of health achieved.Citation25,Citation26
The backdrop: legal, political, economic and social challenges
Despite several ratified human rights treaties and other High Court and Supreme Court Judgments to improve the rights and wellbeing of the LGBTQIA+ community, their plight has not changed much over the years. Difficulties continue in accessing social welfare schemes and other basic services, including accessing services of the Indian healthcare system. To date, social welfare schemes in India do not cover the whole spectrum of the LGBTQIA+ community.Citation27 Further, although the Indian census has recently included the “others” option when declaring one's gender identity, the same has not been implemented through welfare schemes, and hence the community loses out on the benefits of several welfare schemes.
According to some participants, the community does not have political leverage.
A 52-year-old female doctor of a Mumbai-based private hospital said:
“… LGBT(QIA+) is a minuscule population. They are not the vote bank in India because they are not in the majority. They are discriminated and also have a lot of financial constraints and the vicious circle of poverty, inequity and non-accessibility to healthcare begins …”.
Findings revealed that poverty and unemployment among sexual and gender minorities are widespread and are primarily due to their lack of formal education and skill development because of social segregation.
A 42-year-old trans woman said,
“… One of my Chela (disciple) in Hijra culture came from UP (Uttar Pradesh). She was not able to complete her education. She has taken training in beautification, but no one wanted to take services from her. Her parents disowned her, and now she has to do mangati (begging) […] Even getting a job will not do much good. Even if she earns Rs. 10,000 a month in job, it will go away in travelling, housing, and food. More than that she can earn through continuous sex work and mangati.”
Several participants of the study have shared similar views.
The cis-gender individuals with androgynous expression reported discrimination in recruitment practices, while openly LGB individuals reported appraisal and promotion discrimination resulting in less income, lower positions in the institutional class hierarchy, and frequent incidents of unemployment.
A 26-year-old queer person said, “ … I have to change my jobs multiple times just because of my gender identity. Every time I could not negotiate for the desired salary with employers. This made my CV look bad, and I didn't get further employment … ”.
Intersectional inequalities make the economic challenges harder. A 30-year-old male psychologist at a Mumbai-based public hospital said,
“… Recently in our medical hostel a woman committed suicide stating in the suicide note that she was facing caste-based discrimination. But I felt that the reason for her suicide was also because she was a lesbian, which didn't please the professors, who were reluctant to promote her to a new position in a clinical project in her department, with higher income prospects …”.
The societal stigma associated with being a “deviant” individual in Indian society, especially in the case of visibleFootnote* individuals like hijra, transgender, intersex, queer, or individuals with androgynous expression, translate into societal exclusion.
Lesbian and bisexual women reported double discrimination due to the nature of the patriarchal system that devalues girls in general and for being sexual minorities. For example, a 27-year-old lesbian woman belonging to an upper caste from a rural region of Rajasthan, and seeking treatment in a Delhi-based public hospital said,
“… My way of walking and sitting was different. I was forcefully married to a man who was 8 years older, and “gona” (sexual initiation) was done later. My uncle felt that marrying an experienced man would change my sexuality … My private parts got much pain and blood, but I was not given any medical help as this pain, they felt, will change me …”.
Other invisible sexual minorities described existing social pressures resulting in internalised homophobia, identity crisis, mental health issues, and unmet healthcare needs. These challenges get compounded among people who live in non-metropolitan and rural areas, leading to poor healthcare consequences.
A 39-year-old male gay person interviewed in a Delhi-based Trust hospital narrated, “ … Staying alone with no support system lands me up in treating small ailments at home itself. I have no interest left in life … ”.
Religion seemed to play a major role in shaping the experiences of LGBTQIA+ individuals. This is because some religions do not sanction alternative sexual identities and promote religious healing to “cure” them through “holy chant therapies” or tantrik ritual therapies. Although texts about LGBTQIA+ identities exist in Hinduism, members of the LGBTQIA+ community, especially those from upper-caste families, reported being subjected to conversion therapy from religious healers, that led to huge out-of-pocket expenditures.
A 26 year-old queer patient from a Delhi-based trust hospital said,
“… Social pressure was so huge that they (family) took me to a religious healer who charged 5 lakhs (INR) for a hawan (fire ritual) and Rudraksh (form of bead) … And when I was not converted to straight, they spent another lakh(INR) at a hospital for conversion psychotherapies …”.
Healthcare system challenges
Some common reasons for the discrimination against the LGBTQIA+ community by HCPs are lack of LGBTQIA+ knowledge and skills in medical, paramedical, and nursing educational curricula at the national level and unavailability of LGBTQIA+ specific clinical research.
A 30-year-old male doctor of a Delhi-based private hospital said,
“… In the four-year curriculum, there is less than one hour of LGBT(QIA+) content […] I know when I was doing my MBBS, I was only taught about few genetic syndromes related to X and Y chromosomes. There was no LGBT(QIA+) treatment line or terminologies taught to us. Although the curriculum of MBBS has recently changed in India to include topics like communication and empathy, nothing has been included about LGBT(QIA+) medical science or research … ”.
A 56-year-old male doctor of a Mumbai-based public hospital shared that no doctor known to him was equipped to perform sex reassignment surgery or related treatment “ … Neither the doctors are trained in such treatment and procedures (Gender Affirmative Counseling, Hormone and Surgical Procedures) … nor does India have the very skilled medical workforce to conduct such procedures … ”.
While pointing out the need to strengthen the public health system, the participants stated that easy availability of quacks and affordable self-treatments, absence of LGBTQIA+ affirmative HCPs, and unavailability of need-specific health insurance coverage are key factors for prevailing discrimination in healthcare settings.
A 45-year-old male doctor of a Delhi-based public hospital said,
“… the poor public health system and lack of financial independence on the part of LGBTQIA+ individuals results in trans-sexual persons who are isolated by the society and living in far off Gharanas on the outskirts of Delhi to visit quacks The treatments given by quacks are ineffective and mostly limited to inadequate elixirs, creams, and implants, with silicon content … This makes their cosmetic appearance weird and also harms their bodies in the long run … ”.
Either due to the unavailability of gender-affirmative procedures or associated high costs in private healthcare facilities, many transgender individuals opt for painful, home-based procedures. A 35-year-old trans woman interviewed in Delhi-based private hospital reported,
“… We have a “Gharana Nuskha” too. Take wet dough and put it on the chest. Take two red hot bowls (or jugs as it has handles to hold) and put it on the wet dough. It will create a vacuum between the red hot vessel and the dough. Now we will pull the vessel. This will cause chest mass to pull and expand, giving an appearance like boobs. We can't access or afford hospitals and repeating this easy “nuskha” 7–8 times creates boobs. To create feminine nipples, we use hot cotton wick and pull it over the nipples. These procedures create immense pain but also give us mental satisfaction of identifying with a certain gender …”.
Further, the silence in government policies and the lack of sensitisation about LGBTQIA+ persons encourages spurious cures and procedures to flourish. Some people even claim sex-reassignment through alternative systems of medicine like AYUSH (Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homeopathy). For example, a 23-year-old gay person in a Delhi-based private hospital, reported,
“… Our national policy structure has always been silent on LGBTQIA+. Government was silent when the Section 377 judgment on decriminalizing homosexuality was reversed. There is no provision for the enforcement of anti-discrimination laws in the Transgender Protection Act, 2019. This silence translates to healthcare systems as well […] The website of Dr. Dilbag Clinic still claims total cure for homosexuality. There is hardly any government intervention for LGBTQIA+ sensitization efforts or price regulation in private healthcare practices. Dr. X (a Delhi-based doctor) gave my parents a price quotation for a few lakhs (INR) to cure homosexuality … ”.
Organisational level discrimination
Organisational level discrimination involves unfair or discriminatory treatment within an organisation based on a person's belonging to a specific demographic group. It is important to study discrimination against LGBTQIA+ people at the organisational level in healthcare facilities because the healthcare system itself can cause damage at the institutional level in the absence of inclusive policies, practices, and procedures. Several self-identified LGBTQIA+ patients have faced discrimination at healthcare facilities because of their appearance, orientation, and expression that hinders their right to health.
Organisational policies and procedures
When asked about the recent advancements in the LGBTQIA+ domain, most administrators and doctors were unaware of the legal and policy protections offered to the LGBTQIA+ community in India. As a result, policies inclusive of all genders and sexualities are non-existent in most hospitals.
Our study findings reveal that the public hospitals did not have a Human Resources Department. All human resources-related activities were undertaken by the Medical Superintendent. There are a few gender-affirmative guidelines or policies in public hospitals, such as setting up sexual harassment committees and medically certifying a transgender person; these are usually restricted to the binary gender or do not cover the whole LGBTQIA+ spectrum.
The Trust hospitals (charitable hospitals) in the study did not have any existing diversity and inclusion policies, except the Vishaka Guidelines for sexual harassment of women at the workplace. Further, Trust hospitals with religious affiliations refused discussion of the LGBTQIA+ community. The Trust hospitals reported not enforcing LGBTQIA+ equality policies, as their administrative requirements and social norms, including religious affiliations, are considered inadequate to sustain such policies.
The recent legal changes, such as the Supreme Court judgement recognising non-binary gender identities and partial decriminalisation of same-sex sexual orientation, have not been adopted by the private hospitals in the study. Although the private hospitals need to have inclusive policies to meet the Joint Commission International (JCI) or other accreditation, the affirmative policies are either incomplete (with women's rights as the central theme) or ineffective when available (poor enforcement mechanisms).
Further, some of the unique professional healthcare needs like gender-affirmative surgeries and gender-affirmative hormone therapies are available only in specialised centres or tertiary care facilities, making them inaccessible to many.
A 56-year-old male doctor of a Mumbai-based public hospital said,
“… Endocrinology as a department itself is mostly available in tertiary care centers as a super-speciality. Our hospital's endocrinology department is confined mostly to thyroidism and diabetes, along with special clinics once a week on podiatry, adrenal disorders and pituitary and growth disorders. We have never thought of extending our services to LGBT(QIA+) persons also … ”.
Many private hospital administrators reported that serving the minuscule LGBTQIA+ community was not profitable and feared low returns on investing in addressing their needs. There was also a concern about the repercussions of serving the LGBTQIA+ community; a 30-year- old male doctor at a Delhi-based private hospital said,
“… We call them (visible LGBTQIA+ patients) first in the queue so that they feel comfortable and we also don't lose our “normal” patients because of them. You know, the market is highly competitive and we can't afford losing our regular patients … ”.
Organisational practices
Most often the LGBTQIA+ community was viewed as homogeneous by administrators of the healthcare facilities studied.
Several administrators and doctors expressed a stereotypical view of linking LGBTQIA+ individuals with HIV and psychiatry departments. They often assumed that visibly effeminate individuals belonged to the LGBTQIA+ community. A 54-year-old male hospital administrator at a Mumbai-based public hospital said “ … Our hospital doesn't have any LGBT(QIA+) employee in any of the clinical or non-clinical departments … and when it comes to patients, we follow non-discriminatory policy … you can visit psychiatry department or HIV clinic, and you can easily find them … ”.
A 32-year-old woman human resources manager at a Mumbai-based private hospital revealed “ … When we think of making such HR policies, we feel helpless, where to start? We are keen to help, but what do we offer?”
The above statements testify how administrations often lack knowledge on diversity.
Further, the lack of interdepartmental coordination, ineffective communication between healthcare professionals, lack of sensitisation, and poor service management often contribute to discrimination, including unsafe patient discharges. The same has been echoed by LGBTQIA+ participants: that lack of sensitisation and training of healthcare professionals results in a non-welcoming environment and discriminatory practices in the healthcare facilities.
A 32-year-old male doctor at a Delhi-based trust hospital said,
“… There is a lack of inter-departmental collaboration in our hospital. Although implementing HMIS (Hospital Management Information System) has solved some of the issues regarding laboratory and radio-diagnosis but other departments still need to witness the full potential that new technology has […] In case of the care of a trans-sexual individual, departments like Psychiatry, Surgery, Endocrinology have to be well-coordinated with each other … ”.
A 36-year-old male operations manager at a Delhi-based private hospital said,
“… In the first place, there are rarely any visible or open LGBT(QIA+) patients who get admitted in the hospital, and if the individual is admitted, then hospital staff do not routinely ask LGBT(QIA+) patients if they would have a safe place with necessary healing requirements to return to when they are discharged from the hospital … ”.
LGBTQIA+ participants reported experiencing discrimination in the form of humiliation, verbal assaults, and inaccessibility at entry gates by the guards and receptionists. Although such incidents are reported in all hospitals, more such incidents are reported in public facilities than private and Trust hospitals.
A 38-year-old, trans man at a Delhi-based public hospital shared
“… That guard at the entry gate said to me that I don’t look like a normal patient … Other patients will get frightened from my look … There are many NGOs working on the health of people like me … So, I should either go to NGOs for my healthcare needs instead of visiting this hospital; or I should bring one NGO person to accompany me to the hospital … ”.
An 18-year-old gender-queer pansexual person visiting a Mumbai-based Trust hospital said “ … I went to the senior manager complaining about the humiliation … The manager laughed and said that why are you getting afraid, instead we should be feeling unsafe from you … ”.
Binary structures
In all the hospitals, most of the hijras, transgender, and gender-queer persons experienced discrimination based on inadequate gender representation in Out-patient cards and pathology, microbiology and radiology forms, as there is no provision to enter beyond binary sex. The same is true even for hospitals that have state of the art technologies and hospital management information systems. A few gender minorities and intersex patients reported discriminatory birth certificates, discharge cards, and insurance policies. This resulted in manifestation of the extreme discrimination where such individuals could not write their identities in the records and were forced to fit into binary categories.
A 36-year-old trans woman at a Mumbai-based public hospital said “ … In hospital settings, everything is gendered into binary – be it the OPD (out-patient department) lines, medical records, wards or washrooms. I was comfortable in female settings, but I was kept isolated from all … ”.
Public hospitals, which provide free or subsidised services, are preferred by LGBTQIA+ patients because of their poor economic status. However, the high footfall in public facilities results in several incidents of misbehaviour (e.g. sexually explicit touching, humiliating comments, making the LGBTQIA+ individuals stand between lines, etc.) and discrimination (from other patients and hospital employees), especially in the binary queues of registration, consultation, diagnostics, and pharmacy.
Incidents of not allowing gender non-confirming, intersex, trans men, and trans women to use the washroom were more common in Trust hospitals, followed by private and public facilities. We observed that the intersection of class, caste, trans man identity, or individuals using gender representative products like make-up and clothes made individuals more prone for denial for washroom usage.
A 36 year-old trans woman visiting a Mumbai-based public hospital said “ … The pathology medical form and computer system had gender mismatch[…] And when I was asked for a urine test, they didn’t allowed me to use the washroom … ”.
Gender minorities in hospital wards
Regarding allocating wards for gender minorities, administrators and employees often allocated based on the external appearance and clothes worn by an individual rather than respecting the preference or dignity of the individual concerned.
A 55-year-old female nurse of a Mumbai-based public hospital said “ … We don't want to talk about them. How can you take the name of such people from your mouth? […] They appear mardana (masculine) so we keep them in male ward … ”.
A 48-year-old female nurse of a Delhi-based public hospital said,
“… I am working here since last 20 years […] Firstly, we used to admit them in male ward but later we started admitting them in female ward. Actually, when we used to admit them in male ward, they faced a lot of embarrassment.”
Further, this is also a reflection of lack of a formal policy in the hospitals regarding ward allocation for transgender individuals, which is then left to the discretion of the healthcare provider. For example, a 45-year-old female hospital administrator of a Mumbai-based Trust hospital responded,
“… I have heard of one case. There is a hospital in Bangalore … they have started separate OPD services for transgender people and even created a separate transgender ward … The location of that hospital is such that it is very near to the area at the edge of the city where those transgender live … But as much as I can think of creating separate hospital services for LGBT(QIA+) patients, it's not a good idea for two reasons. Firstly, if we see from social lens, by separating the services we are not giving the inclusive treatment. We are doing the same thing which the society has done to them for many years … Secondly, the cost of a bed in a ward also includes the cost of equipment around the bed, maintenance of those equipment and human resources allocated in that ward. Transgender are very few in the population, and the bed in that ward will occasionally be occupied. Also, no other patient can be shifted to that ward even if the bed is empty because of the stigma in the society around ‘transgender ward’. So, it will not at all be a cost-effective-measure … ”.
Discrimination by healthcare providers
Discrimination by healthcare providers took many forms. In some extreme instances, gay persons were threatened with exposure of their sexual orientation:
A 21-year-old gay person in a Mumbai hospital shared that
“They (private/Trust hospitals) keep collecting lot of data at each step, maybe to make an inventory. I have to give my Aadhar (identity) card details too which had the address of my home. They took the phone number of my father … a lot of sexual history was collected which I was not much comfortable to tell … I was diagnosed VDRL positive … The doctor said that in order to take the penicillin injection in the presence of my parents, he will tell them about my multiple partners so that I stop getting such disease … ”.
Fear of being identified as gay by the HCP, and being exposed to others, was a deterrent to healthcare-seeking: “ … Whenever I went to any doctor for any illness, my hands always shake because of my sexuality, I have feared what if the doctor could know about my sexuality and tell it to my parents?” (Gay male in his early twenties visiting a Mumbai-based private hospital).
The findings demonstrated that LGBTQIA+ patients who act like straight people to access healthcare services, often lose the chance of screening opportunity by HCPs for mental health, sexual and reproductive health, oncology, nutrition, etc., which is often their unique need. While seeking services for other minor problems, LGBTQIA+ individuals who are out were forced into conversion therapies or other medications irrespective of the type of hospital. Such incidents are reported to be higher in the case of economically dependent lesbians belonging to non-metro cities who came to metro cities for healthcare services. HCPs in public, trust, and private facilities are found equally unequipped to handle substance use, intimate partner violence, and lesbian corrective rapeFootnote† issues.
A 32-year-old lesbian at a Mumbai-based private hospital reported “ … She (doctor) prescribed me some medicine without any written prescription which turned out to be high dose psychiatric drug … On questioning, she said she assumed me to be facing family pressures (including cases of molestation, abuse and violence) … ”.
Findings illustrate that gay, bisexual men, “kothi” and cross-dressers were often frightened of visiting proctologists, gastroenterologists, and oncologists for anal diseases and anal cancer-related issues. Most of these services and employees in these sections were found non-welcoming for sexual and gender minorities.
A few hijra, trans-sexual and transgender patients stated that doctors often prescribed expensive hormone treatments in some private hospitals without due consideration of the probable side effects.
Most psychologists and psychiatrists were unaware of the emotional needs of a menstruating trans man, queer and asexual identities. Similarly, in the gynaecology department, a trans man reported facing discrimination based on lack of knowledge among healthcare staff and unavailability of customised menstrual products and services.
A transman undergoing gender-affirmative hormonal therapy encountered this humiliating experience when he visited a physician for a common illness:
“… I started testosterone and started growing beard. When I went to a physician for cough and cold, he was shocked by knowing that I have a beard and a vagina […] He said that I seemed to be an intersex and that's why I am at high risk of diseases […] He forced me to show my private parts and even tried to register me in a clinical trial. But I asked him is cough and cold treated through vagina … ?”
When an asexual participant was navigating through the healthcare facilities, she was also informed about the forced medication in the gynaecology department and forced into hormonal treatment in the endocrinology department to enhance sexual desires. Some asexual participants reported cases of harassment by HCPs to make them sexually active as part of the treatment.
A 23-year-old female asexual at a Mumbai-based public hospital said,
“… Just because I didn’t have any feelings, he (healthcare professional) touched me … And when I wanted to take him to the management, he said that the management will not support me, as this is under the plan of treatment to make me sexually active … ”.
A 35-year-old lesbian said “ … We need more open-minded doctors who don't just make assumptions. I was asked about birth-control measures even after disclosing my sexuality. Doctor even made me feel ashamed … ”.
There are also cases where non-consensual binary sex assignments were carried out on intersex children. For example, A 42-year-old male doctor of a Mumbai-based Trust hospital responded “ … intersex child's parents were pressuring doctors to turn their child into male because sterile males are socially more acceptable … ”
Discussion
This study is a significant contribution to the field of LGBTQIA+ healthcare from an administrative policies perspective using a human rights-based approach to understand the preparedness of Indian healthcare organisations to provide services to LGBTQIA+ patients. The “right to non-discrimination” emerged as a central theme, with profound discrimination present at the systemic and organisational levels. Our findings support earlier research on LGBTQIA+ patients experiencing various forms of covert or overt discrimination in healthcare organisations based on their sexual orientation, sex characteristics, and gender identity.Citation3
Our findings reveal that LGBTQIA+ individuals face discrimination in healthcare institutions, and a lack of treatment protocols, which is similar to the scoping review of 67 articles among transgender people.Citation28 Socio-economic barriers, healthcare system restrictions, gender-based violence, education, exclusion from social assistance schemes, and lack of health insurance are the other obstacles quoted in the review, some of which are also echoed by our study findings.
In addition to constitutional recognition of the right to health under Article 21 of the Indian Constitution, the right to health is recognised in the Universal Declaration of Human Rights (UDHR), 1948 and the International Covenant on Economic, Social and Cultural Rights (ICESCR), 1966, ratified by India. The Yogyakarta Principles have also been recognised as an authoritative statement of international human rights principles linked to sexual orientation, sex characteristics, and gender identity. Following General Comment No 14 (UN ECOSOC, 2000), India is required to provide marginalised populations, including members of the LGBTQIA+ community, goods, and services that are available (in sufficient quantities), accessible (physically, geographically, economically and non-discriminatory), reasonable (respect cultural and medical ethics), and of quality (scientifically and medically appropriate and of good quality) (Section 377 Judgment). Despite these, our study reveals discrimination in healthcare settings at various levels, compounded with the intersectional vulnerability of LGBTQIA+ individuals.
Most hospitals cannot effectively adopt LGBTQIA+ inclusive policies, and huge variations were observed between public, private, and trust healthcare facilities. These variations can be attributed to the nature of the organisation, its location, the type of healthcare providers, cost of services in the organisation, and religious affiliation and accreditation needs of the organisations as mentioned in the Findings section. Most healthcare organisations have not implemented gender and sexual diversity-inclusive policies. Such policies, however, have huge potential to provide safety and security to LGBTQIA+ individuals in healthcare settings. For instance, the Vishakha guidelines to prevent sexual harassment of women at the workplace, implemented in all hospitals in the study, can extend to LGBTQIA+ individuals - both patients and employees - who face incidents of violence and sexual harassment in the workplace in the healthcare setting.
LGBTQIA+ subgroups’ access to, use of, and interactions with health care vary systematically.Citation29 Among the LGBTQIA+ community, individuals who self-identify as transgender, intersex, bi-gender, agender, non-binary, or gender-queer are at greater risk of harassment and discrimination. Some oppressed transgender groups such as Hijras, Trihunangais, and trans men who lack formal education and employment are discriminated against at a greater level in healthcare organisations than other sexual minorities.Citation30,Citation31 Literature also suggests the presence of disproportionate and unique healthcare barriers within different sexual minorities.Citation29 Our study also broadly confirms the findings of the existent literature and some unique experiences of asexual and questioning queer patients (individuals who are unsure, or are in a phase of exploring their sexual identity, sexual orientation, gender or all three, or those who are apprehensive about assigning a social label to oneself). Our findings also support past literature that demonstrates the cases of abuse, discrimination, and pathologisation against sexual minorities in clinical settings.Citation32
While pointing out the need to strengthen the public health system, the participants stated that easy availability of quacks and affordable self-treatments, absence of LGBTQIA+ affirmative healthcare professionals, and unavailability of need-specific health insurance coverage are key factors in the prevalence of discrimination. These represent multiple human rights violations, including the right to life, dignity, and personal liberty, the right to freedom for torture, the right to protection against medical abuse, and the right to the highest attainable standard of health.
Conversion therapies using psychological or spiritual intervention are still rampant, although conversion therapy has been condemned by every major medical and mental health organisation globally, including the Indian Psychiatric Society and the WHO.Citation33,Citation34 Strict enforcement to stop conversion therapy in India would go a long way to providing safety for LGBTQIA+ individuals and is an urgent need for the community.
Our study highlights that the lack of information among healthcare providers largely stems from the discriminatory medical education curriculum. The literature suggests that Indian medical authors do not always support the idea of different sexuality and expressions. Most physiology books describe puberty in typical binary gender roles and opposite-sex attractions. Many psychiatry and forensic books and their teaching methodologies are not updated and respectively represent being LGBTQIA+ as a “mental disorder” or “unnatural offence”, and prescribe behavioural therapies to cure the “disease”. Some microbiology books link HIV and other STIs with “homosexual acts”, causing sub-conscious pathologisation. Some books classify Hijras based on wrong ideas of the “castrated genitalia” and association of “lesbianism” with “masculine type excessive sexual desires, jealousy and homicides”.Citation35 In epidemiological studies, some community medicine books label LGBTQIA+ as a “high risk population” differentiating homosexuals from heterosexuals based on a presumption of dangerous sexual activities.Citation35 Such misinformation has far-reaching consequences on young medical students’ understanding of LGBTQIA+ individuals.
In the Indian context, it is crucial to consider how administrative constraints in the hospitals will impact desired policies on LGBTQIA+ equality. Each individual of the acronym LGBTQIA+ has different experiences and varied health needs. However, the administration views this heterogeneous community under one homogeneous approach while framing the policies. As observed from existing laws and acts, specific legal provisions on LGBTQIA+ patient equality in India are practically non-existent, and local enforcement of LGBTQIA+ equality policies can also be challenging.
LGBTQIA+ inclusive policies
Economic and socio-cultural factors may predominate in making general administrative decisions in the hospitals. To successfully frame and implement LGBTQIA+ inclusive policies, a top-down approach is needed urgently. First, administrators and other hospital employees must be sensitised about different issues of each entity under the acronym LGBTQIA+. Hospitals inclined to diversity and inclusion have to create a welcoming atmosphere for LGBTQIA+ patients where their sexuality, sex characteristics, and gender identity or expressions are respected.
The present study highlights the significance of designing and implementing the policies that weave together the human rights principles as shown in .
Table 1. Thematic representation
To generate increasingly inclusive, diverse, and culturally affirming healthcare practices, existing frameworks push towards organisational-level initiatives.Citation36 This includes training for all employees (in both clinical and non-clinical roles), adding LGBTQIA+ related terms in records, policies, and marketing materials, gathering patient information on gender and sexuality to improve clinical practice, and providing all-gender toilets.Citation8
Creating a supportive health care environment within organisations is perhaps the most effective way to increase access to healthcare for LGBTQIA+ patients. This might also commence before entering the healthcare facility; patients may examine signs of LGBT-welcoming terminology as well as policies on the organisation's website.Citation37 Accommodating signs may include non-discrimination policies at the entrance for all patients and employees, mission statements regarding LGBT+ inclusion, Human Rights Initiative signs, leaflets, posters, or brochures that have LGBT+ photos or are explicitly inclusive of the community. Rainbow flags, gender-neutral/inclusive restrooms, and inclusive intake and registration forms are some other environmental indicators of inclusiveness.Citation37 The data gathering on sexual orientation and gender identity using the two-step gender identity approach has recently become a component of the “Meaningful Use” guideline (stage 3) for electronic medical records.Citation38
Based on our study findings, the following steps can help in building inclusive organisational practices:
Scaling up LGBTQIA+ knowledge among HCPs, hospital employees. and other patients
Creating an environment that welcomes LGBTQIA+ patients through inclusive representation, hospitality, and adopting policies as described in .
Building the psychological resilience of LGBTQIA+ patients
Adopting CSR and philanthropy practices for LGBTQIA+ health needs
Supporting the Allies for Queers Programme
Introducing LGBTQIA+ inclusive Human Resource Management Practices
Strengthening the supply chain through prioritising LGBTQIA+ vendors
Promoting inclusive marketing and branding of the hospital as a LGBTQIA+ supportive place
Table 2. Proposed LGBTQIA+ inclusive policy frameworks for healthcare facilities
Conclusions
Through this study, we explored the experiences of explicit and implicit discrimination faced by individuals of the LGBTQIA+ spectrum at systemic and organisational level in Indian healthcare organisations. We demonstrated differences in experiences of LGBTQIA+ patients, attitudes, and behaviours of healthcare providers and administrators and inclusive policies and procedures in public, private and trust hospitals in the two most populous cities of India. This calls for framing and implementing LGBTQIA+ affirmative policies and procedures in the Indian healthcare system.
To ensure the non-violation of the right against discrimination of LGBTQIA+ patients, there is a need for twofold accountability. Firstly, at the national level the government is accountable for complying with ratified human rights covenants and treaties, implementing inclusive legal statues at societal levels, planning and enforcing LGBTQIA+ inclusive public health policies, and reforming the medical education curriculum. Secondly, healthcare organisations are accountable for framing and implementing LGBTQIA+ inclusive policies and practices, conducting diversity and inclusion, cultural competency and clinical competency trainings, and fostering a hospital environment that welcomes LGBTQIA+ patients.
Limitations
The invisibility of the participants for the research was a great challenge. The study adopted purposive sampling owing to the invisible nature of the study population. Thus findings may not represent the whole community and generalisation is challenging.
Acknowledgements
We are grateful to all the study participants of this research for their time and information shared. We are also grateful to the anonymous reviewers and the guest editor for their valuable comments which have sharpened this paper enormously.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes
* A LGBTQIA+ individual will be called visible when their gender identity or sexual orientation is open and out and the person is perceived in the world as per the experienced orientation or identity.
† Corrective rape is a curative form of hate crime in which often an individual is raped by their close friends or family members trying to convert the perceived deviant sexual orientation or gender identity of the individual into the heterosexual cis-gender identity in conformity with societal gender stereotypes.
References
- Gerber P, Gory J. The UN Human Rights Committee and LGBT rights: what is it doing? What could it be doing? Hum Rights Law Rev. 2014:1–37. DOI: 10.1093/hrlr/ngu019
- Mohan S, Murthy S. Towards gender inclusivity: a study on contemporary concerns around gender. Bangalore: Alternative Law Forum and LesBiT; 2013.
- Ayhan CHB, Bilgin H, Uluman OT, et al. A systematic review of the discrimination against sexual and gender minority in health care settings. Int J Health Serv Plan Admin Eval 2020;50(1):44–61.
- Casey LS, Reisner SL, Findling MG, et al. Discrimination in the United States: experiences of lesbian, gay, bisexual, transgender, and queer Americans. Health Serv Res. 2019;54(S2):1454–1466.
- Just Cling. (2018). Healthcare services for LGBT people in India. [cited 2022Apr]. Available from: https://blog.justcling.com/2018/08/30/healthcare-services-for-lgbt-people-in-india/.
- Ranade K, Hastak Y. Growing up and sexual identity formation: mental health concerns of lesbian women. In: BV Davar, TK Sundari Ravindran, editor. Gendering mental health. Oxford: Oxford University Press; 2015. p. 108–135.
- Hope DA, Chappell CL. Extending training in multicultural competencies to include individuals identifying as lesbian, gay, and bisexual: key choice points for clinical psychology training programs. Clin Psychol Sci Pract. 2015;22(2):105–118.
- Makadon HJ, Mayer KH, Potter J, et al. Fenway guide to lesbian, gay, bisexual, and transgender health. Philadelphia (PA): American College of Physicians; 2015.
- Bonvicini KA. LGBT healthcare disparities: what progress have we made? Patient Educ Couns. 2017;100(12):2357–2361.
- Cornelius JB, Enweana I, Alston CK, et al. Examination of lesbian, gay, bisexual, and transgender health care content in North Carolina Schools of Nursing. J Nurs Educ. 2017;56(4):223–226.
- White W, Brenman S, Paradis E, et al. Lesbian, gay, bisexual, and transgender patient care: medical students’ preparedness and comfort. Teach Learn Med. 2015;27(3):254–263.
- Anderson JI, Patterson AN, Temple HJ, et al. Lesbian, gay, bisexual, and transgender (LGBT) issues in dental school environments: dental student leaders’ perceptions. J Dent Educ. 2009;73(1):105–118.
- Moll J, Krieger P, Moreno-Walton L, et al. The prevalence of lesbian, gay, bisexual, and transgender health education and training in emergency medicine residency programs: what do we know? Acad Emerg Med. 2014;21(5):608–611.
- Shetty G, Sanchez JA, Lancaster JM, et al. Oncology healthcare providers’ knowledge, attitudes, and practice behaviors regarding LGBT health. Patient Educ Couns. 2016;99(10):1676–1684.
- Logie C, Bridge TJ, Bridge PD. Evaluating the phobias, attitudes, and cultural competence of master of social work students toward the LGBT populations. J Homosex. 2007;53(4):201–221.
- Unger CA. Care of the transgender patient: a survey of gynecologists’ current knowledge and practice. J Womens Health (Larchmt). 2015;24(2):114–118.
- Sharma H. Are we being trained to discriminate? Need to sensitize doctors in India on issues of gender and sexuality. RHiME. 2018;5:35–43.
- Fish J, Bewley S. Using human rights-based approaches to conceptualize lesbian and bisexual women's health inequalities. Health Soc Care Commun. 2010;18:355–362. doi:10.1111/j.1365-2524.2009.00902.x.
- Sida. Human rights based approach at Sida: compilation of briefs on lesbian, gay, bisexual, transgender and intersex (LGBTI) persons. Art.no.: sida61920en, urn:nbn:se:Sida-61920en; 2014. Available from: https://cdn.sida.se/publications/files/sida61920en-human-rights-based-approach-at-sida-compilation-of-briefs-on-lesbian-gay-bisexual-transgender-and-intersex-lgbti-persons.pdf.
- Indian Census. Office of Registrar General and Census Commissioner of India, Ministry of Home Affairs, Government of India; 2011.
- United Nations. The world’s cities in 2018 data booklet; 2018. Available from: http://www.un.org/en/development/desa/population/publications/pdf/urbanization/the_worlds_cities_in_2018_data_booklet.pdf.
- Ipsos. LGBT+ Pride 2021Global Survey Report. Ipsos; 2021. Available from: https://www.ipsos.com/sites/default/files/ct/news/documents/2021-06/LGBT%20Pride%202021%20Global%20Survey%20Report_3.pdf.
- Van Manen M. Researching lived experience: human science for an action sensitive pedagogy. Albany (NY): SUNY Press; 1998.
- Agócs C. Systemic discrimination in employment: mapping the issue and the policy responses. In: C Agócs, editor. Workplace equality: international perspectives on legislation, policy and practice. The Hague: Kluwer Law International; 2002. p. 5–11.
- Seng JS, Lopez WD, Sperlich M, et al. Marginalized identities, discrimination burden, and mental health: empirical exploration of an interpersonal-level approach to modeling intersectionality. Soc Sci Med. 2012;75(12):2437–2445. DOI:10.1016/j.socscimed.2012.09.023
- Chatterjee S. Problems faced by LGBT people in the mainstream society: some recommendations. Int J Interdiscip Multidiscip Stud (IJIMS). 2014;1(5):317–331. Available from: https://www.ijims.com/uploads/cae8049d138e24ed7f5azppd_597.pdf.
- N. Anand Venkatesh. J. Madras High Court, W.P.No.7284 of 2021. State PP Ginna argued; 2021N. ANAND VENKATESH.,J.. Available from: https://www.mhc.tn.gov.in/judis/madras-do/index.php/casestatus/viewpdf/WP_7284_2021_XXX_0_0_04102021_177.pdf.
- Pandya AK, Redcay A. Access to health services: barriers faced by the transgender population in India. J Gay Lesbian Ment Health. 2020. DOI: 10.1080/19359705.2020.1850592
- Macapagal K, Bhatia R, Greene GJ. Differences in healthcare access, use, and experiences within a community sample of racially diverse lesbian, gay, bisexual, transgender, and questioning emerging adults. LGBT Health. 2016;3(6): 434–442. DOI: 10.1089/lgbt.2015.0124
- Grant JM, Mottet LA, Tanis J, et al. Injustice at every turn: a report of the national transgender discrimination survey. Washington (DC): National Center for Transgender Equality and National Gay and Lesbian Taskforce; 2011.
- The Humsafar Trust. Stigma reduction, health care provider awareness and knowledge enhancement on transgender issues in India (SHAKTI). The Hijra Health Manual for Healthcare Professionals; 2014.
- Huebner DM, Davis MC. Perceived antigay discrimination and physical health outcomes. Health Psychol. 2007;26(5):627–634.
- Human Rights Campaign. Policy and position statements on conversion therapy; 2018. Available from: https://www.hrc.org/resources/policy-and-position-statements-on-conversion-therapy.
- World Health Organization. Sexual health, human rights, and the law; 2015. Available from: https://apps.who.int/iris/ bitstream/handle/10665/175556/9789241564984_eng. pdf?sequence = 1.
- Thakurta TG. The homophobic doctor. Insight, advice-mind, body and family; 2014 [cited 2019 May 15]. Available from: http://varta2013.blogspot.com/2014/03/the-homophobic-doctor.html?zx = 20d659a5e0297a93.
- Weech-Maldonado R, Dreachslin JL, Epané JP, et al. Hospital cultural competency as a systematic organizational intervention: key findings from the national center for healthcare leadership diversity demonstration project. Health Care Manage Rev. 2018;43(1):30–41.
- Croghan CF, Moone RP, Olson AM. Working with LGBT baby boomers and older adults: factors that signal a welcoming service environment. J Gerontol Soc Work. 2015;58(6):637–651.
- Cahill SR, Baker K, Deutsch MB, et al. Inclusion of sexual orientation and gender identity in stage 3 meaningful use guidelines: a huge step forward for LGBT health. LGBT Health. 2016;3(2):100–102.