Abstract
The aim of this study was to explore service providers’ lived experiences with abortion care in the Republic of Ireland following liberalisation in 2018 via public referendum. Data were collected using semi-structured interviews conducted between February 2020 and March 2021. Thirteen interviews were completed with providers who were directly involved in caring for patients accessing liberalised abortion care in the Republic of Ireland. The sample includes six general practitioners, three midwives, two obstetricians, and two nurses. Interpretative phenomenological analysis identified five super-ordinate themes in the providers’ lived experiences: (1) public reactions to liberalised abortion care; (2) lessons from the service implementation; (3) getting involved in abortion care; (4) moments of moral doubt; and (5) remaining committed to the provision of care. Following liberalisation, providers recalled isolated experiences with anti-abortion sentiments, particularly from those who continue to oppose abortion care. They believed that implementation has been mostly successful in delivering a safe, robust, and accessible service in general practice, though identified ongoing challenges in Irish hospitals. Personally, the providers supported access to care and began providing because they perceived a duty to facilitate access to care. Many, however, reported occasional moral doubts about their work. Despite these, none had considered leaving abortion care and all were proud of their work. They said that patients’ stories were a constant reminder about the importance of safe abortion care. Further work is required to ensure that abortion is fully integrated and normalised and that all providers and patients have access to supports.
Résumé
Le but de cette étude était d’explorer les expériences vécues par les prestataires de services d’avortement dans la République d’Irlande après la libéralisation de l’interruption de grossesse en 2018 par voie de référendum public. Les données ont été recueillies lors d’entretiens semi-structurés réalisés entre février 2020 et mars 2021. Treize entretiens ont été complétés avec des prestataires participant directement aux soins des patientes ayant accès aux soins pour avortement libéralisés en République d’Irlande. L’échantillon incluait six praticiens généralistes, trois sages-femmes, deux obstétriciens et deux infirmières. L’analyse phénoménologique interprétative a identifié cinq thèmes dominants dans les expériences vécues par les prestataires: (1) réactions publiques à la libéralisation de l’avortement; (2) leçons tirées de la mise en œuvre des services; (3) participation aux soins pour avortement; (4) moments de doute moral; et (5) rester engagé en faveur de la prestation des soins. Après la libéralisation, les prestataires ont rappelé des expériences isolées avec des sentiments anti-avortement, en particulier de ceux qui continuent à s’opposer à l’interruption de grossesse. Ils pensaient que la mise en œuvre avait surtout réussi à assurer un service sûr, robuste et accessible en médecine générale, mais identifiaient des obstacles dans les hôpitaux irlandais. Personnellement, les prestataires soutenaient l’accès aux soins et ils ont commencé à les prodiguer car ils ont jugé qu’il était de leur devoir de faciliter l’accès aux soins. Beaucoup, néanmoins, ont fait état de doutes moraux occasionnels sur leur travail. Malgré tout, aucun d’entre eux n’avait envisagé d’abandonner les soins pour avortement et tous étaient fiers de leur travail. Ils ont affirmé que les expériences des patientes étaient un rappel constant de l’importance d’avortements sans risques. De nouvelles mesures sont nécessaires pour veiller à ce que l’avortement soit totalement intégré et normalisé, et que tous les prestataires et les patientes aient accès aux soutiens.
Resumen
El objetivo de este estudio era explorar las vivencias de los prestadores de servicios con la atención al aborto en la República de Irlanda después de la liberalización en 2018 vía referéndum público. Se recolectaron datos por medio de entrevistas semiestructuradas realizadas entre febrero de 2020 y marzo de 2021. Se realizaron trece entrevistas con prestadores de servicios involucrados directamente en brindar atención a pacientes que accedían a servicios de aborto liberalizado en la República de Irlanda. La muestra consiste en seis médicos generales, tres parteras, dos obstetras y dos enfermeras. El análisis fenomenológico interpretativo identificó cinco temas superordinados en las vivencias de los prestadores de servicios: (1) reacciones públicas a los servicios de aborto liberalizado; (2) lecciones de la implementación de los servicios; (3) participación en la prestación de servicios de aborto; (4) momentos de duda moral; y (5) continuo compromiso con la prestación de servicios. Después de la liberalización, los prestadores de servicios recordaron experiencias aisladas con sentimientos antiaborto, en particular de las personas que continúan oponiéndose a los servicios de aborto. Indicaron creer que la implementación ha sido principalmente exitosa en la entrega de un servicio seguro, robusto y accesible en la práctica general, aunque identificaron retos continuos en los hospitales irlandeses. Personalmente, los prestadores de servicios apoyaban el acceso a los servicios y empezaron a proporcionarlos porque percibieron su deber de facilitar ese acceso. Sin embargo, muchos de ellos informaron tener dudas morales ocasionales sobre su trabajo. No obstante, ninguno había considerado dejar de prestar servicios de aborto y todos estaban orgullosos de su trabajo. Dijeron que las historias de sus pacientes eran un recordatorio constante de la importancia de los servicios de aborto seguro. Aún queda más trabajo por delante para garantizar que el aborto sea integrado y normalizado totalmente y que todos los prestadores de servicios y las pacientes tengan acceso a apoyo.
Introduction
In May 2018, the Republic of Ireland voted to liberalise its laws governing abortion care, ending a period of nearly 160 years of legal restrictions.Citation1,Citation2 Abortion care was first regulated in 1861, when the Offences Against the Person Act made it illegal in all circumstances.Citation3 When the Republic of Ireland became independent from the United Kingdom in the early twentieth century, it retained this law and founded itself as a politically conservative, Catholic country.Citation4,Citation5 Abortion was further restricted in 1983 with the passing of the Eighth Amendment to the Irish Constitution via referendum, which vindicated “the right to life of the unborn” as equal to that of the pregnant person.Citation6 Legal restrictions on the island forced thousands of women to travel abroad for abortion care,Citation5,Citation7 while unknown numbers sought clandestine care or decided to continue unwanted or unviable pregnancies.
In light of changing opinions and international condemnation, a referendum to repeal the Eighth Amendment and allow the legislature to regulate abortion care was put to the public in 2018.Citation8,Citation9 Arguments in favour of repeal highlighted the negative impact of restrictions and the need to care for women experiencing medical emergencies, pregnancies affected by fetal anomalies, or who simply do not want to be pregnant.Citation8,Citation10,Citation11 By sharing the stories of real women, liberalisation was also regarded as a pragmatic solution to the risks associated with travelling for abortion or accessing care without medical supervision.Citation8,Citation10,Citation11 Arguments against repeal emphasised fetal personhood and right to life and equated abortion care to murder.Citation12 These campaigns publicised graphic images of fetal remains and warned against introducing an abortion service like the “regime” in England.Citation13 The referendum passed, with 66.4% of the public voting in favour of liberalisation,Citation14 the Health (Regulation of Termination of Pregnancy) Act 2018 came into effect from January 2019.Citation15 The Act allows people in the Republic of Ireland to end a pregnancy under 12 weeks’ gestation without conditionality.Citation15 After 12 weeks, abortion can only be provided when continuing the pregnancy puts the physical or mental health of the pregnant person at risk, in emergency situations, or when the fetus is unlikely to live 28 days after birth due to a physical condition.Citation15
Liberalised abortion care is now offered in general practices and maternity hospitals nationwide. At the time of writing in March 2023, 11 of the 19 maternity hospitals offer abortion careCitation16 and just over 400 of the approximately 3500 general practitioners (GPs) have completed training in early medical abortion (EMA) care.Citation17 GPs offer EMA as an out-patient service up to 8+6 weeks’ gestation. Placing abortion within community-based practice helped to ensure it would be widely accessible.Citation18 Care between 9+0 and 12+0 weeks’ gestation is managed medically in a maternity hospital, with at least five units also routinely giving women the option to access surgical care via vacuum aspiration. After 12 weeks, care is largely managed medically in hospitals, with surgery generally reserved for cases where medical abortion is not appropriate. Prior to the introduction of liberalised abortion care, the Irish College of General Practitioners and the Southern Taskforce for Abortion and Reproductive Topics (START) offered GPs training in EMA, while the Royal College of Physicians Ireland provided training for obstetricians. The World Health Organization also provided values clarification workshops, which rolled out in late 2018. Training in technical and non-technical skills continues nationally.
The abortion process in the Republic of Ireland typically involves two meetings.Citation19,Citation20 When people first present, they partake in pregnancy options counselling where they can discuss abortion and all other options available to them with a trained healthcare professional. If they decide to continue with care, they must wait three days for the second meeting, where they sign a consent form and begin treatment. The three-day wait does not apply to those with a medical or fetal indication. An optional third follow-up meeting to ensure the abortion is complete is available to everyone who receives care. The service is free for those who live in the Republic of Ireland and have a Personal Public Service number.Citation21 In the first three years, 17,820 abortions were performed,Citation22–24 with approximately 98% of these occurring under 12 weeks’ gestation and the majority being medical abortions provided by GPs.Citation25 Despite initial speculation about high demand for the services, rates of abortion care are lower than expected.Citation25 Some continue to travel for care, particularly those beyond the 12-week limit and those with pregnancies affected by non-fatal fetal anomalies, though this figure has vastly reduced.Citation26 The Health Service Executive, Ireland’s national public health service, also funds MyOptions, a phone and online service that offers pregnancy options counselling and directs women to the nearest open-list provider, e.g. a GP willing to accept referrals for abortion care.Citation27
Despite being one of the most common gynaecological procedures, however, international research has found that providers may experience a range of challenges related to their involvement in care. These include stigmatising experiencesCitation28 and moral doubts about their involvement.Citation29,Citation30 Though abortion care can be emotionally and morally demanding work, positive experiences are also widespread within the international literature. Many are proud of their ability to provide women access to careCitation29,Citation31 and noted the high levels of support they receive from colleagues.Citation32 Indeed, some working in countries where abortion was previously illegal, like Ireland, have highlighted the negative impacts of legal restrictions and the importance of safe abortion care.Citation31,Citation33,Citation34 In the Republic of Ireland, we previously found that though providers reported some stigmatising experiences, they also reported high levels of pride in their work.Citation35 The objective of this study was to explore service providers’ lived experiences with liberalised abortion care in the Republic of Ireland.
Methodology
As the aim of this study was to explore providers’ lived experiences, we deemed a qualitative, phenomenological approach the most appropriate. Specifically, we followed guidance from Smith et al. on conducting interpretative phenomenological analysis (IPA).Citation36,Citation37 We collected data via semi-structured interviews conducted between February 2020 and March 2021. Using a mix of purposive, convenience, and snowball sampling strategies, we invited providers of liberalised abortion care working in the Republic of Ireland to talk about their experiences with care. Fourteen providers contacted the research team, though one (a GP) did not respond to follow-up emails. This left a sample of 13 providers who completed an interview. We stopped recruitment at this point as we observed thematic saturation. We followed guidance from Francis et al.,Citation38 whereby an initial sample of 10 interviews was conducted and then a stopping criterion of three interviews was set. As no new themes were discussed in the final three interviews, the stopping criterion was fulfilled and a final sample of 13 providers was considered appropriate.
The interview guide asked providers about their demographics and work in general, their reflections on the referendum, their experiences with the implementation of care, their reasons for providing abortion care, and any memorable experiences and interactions related to their involvement. We developed the guide following a review of the international literature and we refined it by conducting a pilot study with four clinicians and researchers working in the National Maternity Hospital. We gave the guide to providers before the interview so they could think about their answers and identify questions that they did not want to answer. No-one asked to skip a question. We gave providers the option to complete the interview via phone call or in person, with 11 taking place via phone call and two occurring in person. The option to interview via phone call allowed us to speak with providers throughout Ireland and to continue data collection during the pandemic. The first author (BD) conducted, recorded, transcribed verbatim, and anonymised all interviews. The length of the interviews ranged from 25 to 66 minutes, with the average length being 42 minutes. Ethical approval was granted by the National Maternity Hospital Research Ethics Committee (EC37.2019), (November 2019) and the UCD Human Research Ethics Committee – Sciences (LS-20-05-Dempsey-Higgins, 2020).
We analysed data using IPA.Citation36,Citation37 Per guidance from Smith et al.,Citation36,Citation37 analysis began with familiarisation of the first interview. During this stage, initial notes on important quotes and general thoughts and impressions were made. These notes were then transformed into emergent themes, which were then sorted by theoretical association to identify a list of preliminary themes for the first interview. These steps were repeated for each interview. Once all the interviews had been analysed, the full list of preliminary themes was sorted by theoretical association to develop theme clusters. We met to discuss these theme clusters and to decide on the final super-ordinate and sub-ordinate themes. We were in constant contact with the source data to ensure that themes and interpretations were true to the providers’ accounts. Analysis was conducted manually using Microsoft Word.
Finally, it is important to recognise that the providers’ lived experiences have been interpreted through the subjective lens of the researchers.Citation39 All interviews were conducted by BD, who has a psychology background and no personal experience as a healthcare worker of providing abortion care, or of accessing abortion care. This “outsider” perspective helped him to focus on the providers’ experiences, as he had no competing knowledge. It may also be that this “outsider” perspective gave providers a degree of comfort in discussing their experiences, as they had no prior personal or professional connections to the interviewer. BD completed this study as part of a PhD on providers’ experiences with abortion care in the Republic of Ireland and the co-authors acted as supervisors, with MC advising on the methodology and MFH advising on the subject matter.
Results
Sample characteristics and qualitative themes
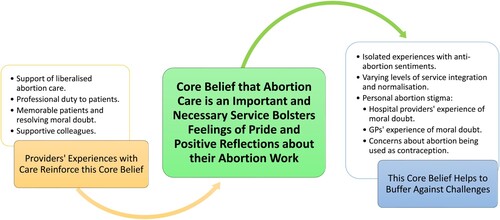
The sample includes 13 providers, see for information on their demography and involvement in abortion care. There was at least one provider from each Irish province and seven of the 11 providing maternity hospitals in the Republic were represented. Three of the providers were in their twenties, one was in their thirties, five were in their forties, two were in their fifties, and two were in their sixties. Region and age are not included in to maintain anonymity. Five super-ordinate themes were identified in the providers’ experiences with liberalised abortion care: (1) public reactions to liberalised abortion care; (2) lessons from the service implementation; (3) getting involved in abortion care; (4) moments of moral doubt; and (5) remaining committed to the provision of care. See for an overview of these themes and their accompanying sub-themes.
Figure 1. Overview of the themes and sub-themes identified by the Interpretative Phenomenological Analysis of providers’ experiences with liberalised abortion care in the Republic of Ireland
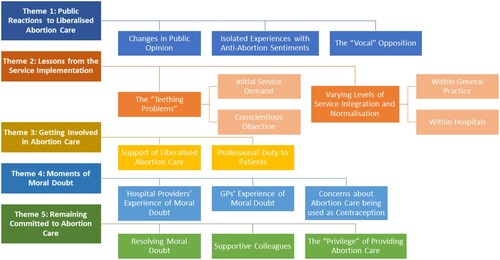
Table 1. Involvement in the provision of liberalised abortion care for the sample of abortion care providers in the Republic of Ireland (n = 13)
Theme 1 – Public reactions to liberalised abortion care
All reflected on the cultural changes that allowed for the repeal of the Eighth Amendment and were happy to see widespread public support. Despite support for liberalised abortion care, however, all had faced isolated experiences with anti-abortion sentiments and many also acknowledged the minority who continue to oppose care in Ireland. See for quotes corresponding to Theme 1.
Box 1. Quotes from the providers of liberalised abortion care in the Republic of Ireland in support of Theme 1 – Public reactions to liberalised abortion care
Changes in public opinion
The providers talked about the “brilliant” repeal campaigns during the referendum, which amplified women’s voices to show the need for a safe and legal abortion service. Common examples included pregnancies affected by fetal anomalies and the need for abortion in a medical emergency. They also said that the campaigns amplified the voices of people “who didn’t necessarily fall into those really tough categories” to ensure that “every sister, every girlfriend, every mother, every grandmother” was represented. Conversely, they said that the campaigns against liberalisation tried to paint abortion as “black and white”, and “went for the jugular” to “scaremonger” those who choose to access or support abortion. They also highlighted the spread of misinformation about abortion care. Many said that the referendum evidenced the “conflict between Irish society in general, it’s the whole the conservative versus the liberal and the two sides are going further apart”. Though many believed that support for abortion was “a generational thing”, one said that older generations lived through the “darkest days” of restrictions on women’s health and knew their true impact. Ultimately, the providers said that by voting to repeal the Eighth Amendment, the public accepted the need for legal, safe abortion care.
Isolated experiences with anti-abortion sentiments
While the providers said that most people are supportive of liberalised abortion, all recalled experiences with anti-abortion sentiments. In their personal lives, common examples included being “cornered” and “intimidated” by family and friends who questioned the providers’ support for or involvement in the services. Another common example was local community members gossiping about their involvement or writing to complain about the provision of care. In response to these experiences, the providers had two key strategies. The first was to affirm that their isolated nature made them easy to tolerate. The more common strategy was to limit or withhold disclosure of their work, saying that it’s important to be aware of mixed views and discussing their work is often “not worth the hassle”. Despite limiting or withholding disclosure, providers were sure “that there’s nothing I am ashamed of here in terms of provision of care”.
Most also faced isolated experiences with anti-abortion sentiments within the workplace. Two GPs said that they have experienced a “definite silence” from staff both within and outside their practice. An obstetrician discussed how they were referred to by colleagues as “the terminator”, and both nurses and a midwife discussed colleagues who openly expressed “judgment”, “nastiness”, and “ill-feeling” about abortion. Despite these, many believed that those who did not support care “would usually just not bring it up”, and that the isolated nature of these experiences made it easy to tolerate.
The “vocal” opposition
The providers believed that the majority of those who did not support abortion during the referendum have “accepted the results” and “moved on”. Prior to the service introduction, some feared the “repercussions for providing the service”, though said that these concerns have been unfounded. They did, however, acknowledge that there is a minority who continue to oppose and protest liberalised abortion care. Five (one GP and four hospital providers) experienced protests at their workplace and more knew of colleagues who had. Though the providers believed that protests had little impact on them due to poor organisation and small numbers, they said that protests could have a greater negative impact on the women accessing care and were “disappointed” at the government’s failure to legislate for safe access zones at practices and hospitals nationwide.
Theme 2 – Lessons from the service implementation
The providers also reflected on the implementation of care and acknowledged the teething problems that they experienced. Beyond implementation, the GPs believed that they had fully integrated and normalised abortion care within their practices, though the hospital providers reported greater issues. See for quotes corresponding to Theme 2.
Box 2. Quotes from the providers of liberalised abortion care in the Republic of Ireland in support of Theme 2 – Lessons from the service implementation
The “teething problems”
Eleven providers described “teething problems inherent in setting up any service” when implementing abortion care. These were related to the initial high demand for the service and challenges created by high levels of conscientious objection. Challenges related to service demand were more common among the GPs, while challenges related to conscientious objection were more prominent in hospitals.
Initial service demand
Five GPs and an obstetrician highlighted the initial demand for the services as a key challenge. They said that many early patients had become pregnant in late 2018 and waited “until the service came into effect” rather than travel or access clandestine care. The services “weren’t in place” in January, however, and the providers said that they were not prepared to deal with high numbers of requests. In addition, many early patients were close to the gestational age limit which, coupled with the mandatory three-day waiting period between counselling and the dispensation of medication, increased the emotional stress for both the patient and the provider. It also forced providers to question if they were acting within the law. They noted that very few GPs initially signed up to the MyOptions open provider list, meaning that a small number of GPs were dealing with the high demand. Some were the only open-list provider in their county, with one being the only open-list provider across three counties. Over time, more GPs have started providing and demand is now at “an acceptable”, if sometimes variable, level. Similar issues were less prominent in hospitals, with many saying that management “were expecting a lot more of a demand”.
Conscientious objection
Though all providers unanimously supported their colleagues’ right to conscientious object, high levels of objection created issues with implementation. The hospital providers, particularly nurses and midwives, noted that high levels of objection meant that they “automatically became the person who provided” care. One midwife discussed having “to cancel [planned days off]” to be available for the service and another said that they had to ask women to return home on multiple occasions because the attending doctors refused to prescribe medication. There were also concerns about “the extent of the conscientious objection” and “would that include if the woman’s life was at risk”. Some felt that hospital management “had agreed to take these women on” and that the services were “very haphazardly” introduced or “railroaded” into their unit, meaning that providers were often tasked with integrating the services as well as providing care. They overcame issues by “taking a very very co-ordinated approach” to ensure that abortions are only provided at specific times, there is always a provider present, and the required resources are available. They believed that conscientious objection would create greater issues in smaller, regional hospitals where “the small number of consultants … means that if there are one or two who conscientiously object, that the whole service then falls to maybe one person”.
Some of the GPs also experienced issues within their practice; for example, one was told by a senior partner that “these women would not be seen in this clinic”. Additionally, some knew about the obstruction of care, with one saying “I have had people, they’ve gone to their own GP for information and haven’t really been able to get any. That has left those women feeling quite vulnerable”.
Varying levels of service integration and normalisation
Many affirmed that “there was always going to be issues at the beginning” and that many of these teething problems have now been “ironed out”. Beyond the implementation of care, we observed that the extent to which abortion care was fully integrated and normalised within the providers’ workplace varied between general practice and hospitals.
Within general practice
The GPs all believed that abortion has been fully integrated and normalised within their practices. They said that the “anonymous” nature of general practice has helped to de-stigmatise those accessing care, and that the existing infrastructure in Irish general practice ensured that the services are widely available. Indeed, many highlighted the success of GP-led abortion care as evidenced by the positive international commentary, saying that the introduction of care in general practice was “a good news story”. Despite this, they acknowledged the remaining issues nationwide. Many noted that some GPs, particularly those in rural areas, do not have the support of a local providing GP or hospital. GPs highlighted the work of the START group in connecting providers, with one describing START as “the best thing I’ve been involved with professionally ever”. The providers were critical that eight hospitals do not provide abortion care, which they believe is primarily due to high levels of objection. One said that “when [conscientious objection] permeates to the level where that service is not possible to run, I think that is catastrophic”. In rural areas, many believed that because “there’s so few GPs providing and then the hospitals aren’t providing, it makes it more difficult for women” and that “GPs who are providing in rural areas probably need more support”.
Within hospitals
By contrast, the hospital-based providers discussed greater ongoing challenges. Three had worked in multiple hospitals post-liberalisation and said that levels of integration and normalisation differed in each unit. While some had fully integrated abortion into the “normal structure of the hospital”, others had not, possibly without enough staff willing to participate, in an “alienated” or unsuitable part of the hospital, or without the option for non-consultant doctors to observe or participate in care. The nurses and midwives also said that continuing high levels of conscientious objection along with low staffing levels meant they often provide care in addition to their general workload, usually without renumeration. They said that while some objecting colleagues help care for patients, others still “have nothing to do with them”. They felt that management ensured that conscientious objectors would not be forced to be involved in care, while there was not enough focus on supporting conscientious providers in their new role. This left nurses and midwives feeling unappreciated for their work, in addition to dealing with the challenges of the work itself.
The providers also noted the importance of normalising abortion care by cultivating open dialogue, which allows them to discuss their work and to challenge misconceptions and anti-abortion sentiments. Where open dialogue was not achieved, they felt that abortion care was a “dirty little secret” and “not something that we want to be providing here”. They also said that some colleagues “wouldn’t even want anybody to mention the name of the person [accessing care] or to talk about it”. They said, however, that open dialogue can be “the trickiest to engender” and believed that they had an important role by trying to “open conversations with people” and “be willing to have the conversation again and again and again and again”. Despite ongoing challenges, they said that they were able to provide women with “a good service” and that “the clinics now are run like clock-work”.
Theme 3 – Getting involved in abortion care
As regards their personal views, the providers all affirmed that they supported access to liberalised abortion care and emphasised that they became involved in care because they perceived a duty to facilitate access to care. See for quotes corresponding to Theme 3.
Box 3. Quotes from the providers of liberalised abortion care in the Republic of Ireland in support of Theme 3 – Getting Involved in abortion care
Support of liberalised abortion care
While some initially held concerns about the introduction of liberalised abortion care, all unanimously believed that restrictive abortion laws had a negative impact on the physical and mental health of women in Ireland. This was mainly informed by personal and professional experiences which evidenced these impacts and highlighted the need for safe and legal abortion care, for example close friends and patients who were forced to travel abroad for care. Some (two GPs, two obstetricians) showed their support by campaigning for repeal, saying that it was important to use their platform as a healthcare worker to advocate for the improvement of women’s health. Others discussed a sense of “Catholic guilt” about abortion. Having grown up in a strongly Roman Catholic influenced, anti-abortion Ireland, they said that seeing the negative impact of restrictive laws forced them to reconsider the anti-abortion stance that they inherited in their youth. Given this belief that abortion is a necessary service, none experienced a conscientious objection.
Professional duty to patients
The providers asserted that they ultimately began providing because they perceived a professional duty as a healthcare worker to facilitate access to care. Many emphasised that their own beliefs and values are irrelevant to their work, proffering sentiments that “you don’t treat somebody differently because of what they’ve done or why they’re there” and that “life is about choices and we’re very lucky to be able to make them and I felt that I just don’t put any judgment on anyone's decisions”. Referencing high levels of conscientious objection within their workplace and among local practices, many also felt that “the rest of us that don’t have an objection … would have had to step up to provide it”, with some saying that they were one of the few who agreed to provide care.
Theme 4 – Moments of moral doubt
Throughout their practice, however, most described moments where they questioned if abortion care is morally justified. Some also expressed concern about abortion being used as a method of contraception. See for quotes corresponding to Theme 4.
Box 4. Quotes from the providers of liberalised abortion care in the Republic of Ireland in support of Theme 4 – Moments of moral doubt
Hospital providers’ experience of moral doubt
As procedures completed in Irish maternity hospitals are provided as an in-patient service, the hospital providers are tasked with handling and disposing of the fetal remains. Some referred to handling the fetal remains as the most difficult part of abortion care, especially when required to do so multiple times a week. One midwife talked about seeing the human features of the fetus, such as “little fingernails”, and said that fetuses can be “so well formed … coming up to that twelve-week mark”. The hospital providers also discussed the challenge of providing abortion care via surgical methods, saying that vacuum aspiration “is not a pleasant procedure”, even though it is no more technically difficult “than any of the other surgical evacuations of the uterus”. In Ireland, surgery is mostly offered under 12 weeks and most procedures after that are managed medically. Contact with the fetal remains made some providers think that abortion results in the loss of potential life. Recalling an experience where a patient returned to the hospital with their baby after deciding not to proceed with abortion, a midwife said that they thought “of all the other little babies that weren’t going to be alive and so that kind of made me think about what I was doing, you know?”
To reduce moral doubt and emotional responses when providing care, the providers said that you “have to take yourself out of the room” and “just have to try and forget about it as quick as you can”. The providers also said that they have become more comfortable with care over time and that increased experience has helped to reduce doubts. They also said that care is made easier when “you go back into the room and [the patients are] so thankful to you”.
GPs’ experience of moral doubt
Generally, the GPs said that they were comfortable with their role in EMA and rarely experienced moral doubts. At present, most women attend early in their pregnancy, typically around “five, six, seven weeks”. On the rare occasions where women were close to the 12-week limit, the GPs referred them to a local hospital. They believed that this system was effective as hospitals provide care that they cannot facilitate as part of an “already stretched service in general practice”. Moments of moral doubt, however, did occur. Some said that they feel guilty when they think about the fetus, while another said that providing “can bring up our own stories, our own prejudices, our baggage that we’re carrying”. While generally comfortable with their involvement, some raised practical and personal concerns about their support for further liberalisation, particularly if asked to provide later-gestation or surgical care. Despite misgivings, however, they acknowledged that potential changes to the laws or clinical guidance were unlikely to affect their role given existing resource constraints.
Concerns about abortion care being used as contraception
Some providers expressed concerns that abortion could be used as a method of contraception. They said that they did not approve of some patients who access care multiple times or who do not use contraception, believing this to be a “devaluing of what pregnancy is”. Some also commented on the lack of free contraception available to people in Ireland, saying that “providing free terminations and not free contraception doesn’t add up”. Despite concerns, these providers resolutely believed that abortion is not used as contraception in Ireland.
Theme 5 – Remaining committed to the provision of care
While acknowledging moments of doubt, all were clear that they have never considered ending their practice. They said that their patients’ stories were a constant reminder of the need for safe and legal abortion care. The providers also talked about the importance of receiving support from colleagues. Finally, all reflected positively on their work. See for quotes corresponding to Theme 5.
Box 5. Quotes from the providers of liberalised abortion care in the Republic of Ireland in support of Theme 5 – Remaining committed to the provision of care
Resolving moral doubt
During their work, all shared sentiments that “there’s certain cases that you don’t forget about”. Common examples of the GPs included women who have had to “fight another journey” and overcome social or geographical barriers to access care. The hospital-based providers said that their work often brings them into contact with “women who are either extremely socially or medically vulnerable”, and memorable cases included patients in domestic abuse situations, patients in medical emergencies, patients with medical conditions, patients with pregnancies affected by fatal fetal anomalies, and patients who reminded providers of themselves or family members. Of those who reported moments of moral doubt, they said that patients’ stories help to reduce doubts by showing the necessity of a safe and legal abortion service. While the emotional challenge of providing care after 12 weeks was high given that they are often “very much wanted pregnancies” and that the fetus may be “a good size”, moral doubts were rare as the providers believed that abortion was the best option for the patient and the fetus.
Four providers said that they have never experienced moments of moral doubt when providing abortion care. Two, aged in their sixties and working in general practice, stressed that a career of seeing the negative impact that restrictive abortion laws had on women is a constant reminder of the need for legal care and saw their duty to their patients as paramount. The other providers, in their twenties and working in hospitals, acknowledged that while aspects of care were “physically and emotionally draining”, they never experienced doubts due to deep-rooted beliefs that abortion is a socially important and necessary service.
Many also stressed the importance of giving all patients empathetic care, which was generally discussed in terms of being non-judgmental and “looking after” patients through the process. The nurses and midwives particularly highlighted the importance of empathy, as they have contact with the patients before, during, and after the procedure. While providers acknowledged that “sometimes [abortion care is] hard and sometimes it’s much sadder than other times”, they believed the emotional weight of care incentivised their involvement. They also noted that their patients’ emotional reactions are variable and that it is important to tailor their response to each patient accordingly.
Many said that their experience of providing care has made them more passionate about ensuring continued access to care. These providers believed that providing abortion care has been a transformative experience and that hearing women’s stories “solidified” their perceived duty to their patients, increased their empathy, and helped to diminish any occasional doubts they may have.
Supportive colleagues
The providers unanimously underlined the importance of receiving support from their colleagues, particularly other providers. Acknowledging that abortion care can be challenging work, they stressed the importance of being able to discuss their concerns and talk about moral doubt without fear of judgment with someone who shares similar experiences. Given that abortion was “so different, it’s so new”, they believed that providers banded together to support one another because “everyone’s learning as you go”. The GPs, particularly those in rural areas, discussed START’s work in fostering peer support. One rural GP said that START “has been absolutely amazing … in terms of professional clinical support and in terms of personal support”. The hospital providers also discussed positive experiences with “social workers”, the “bereavement midwife”, and the “perinatal mental health team” in offering emotional support to both providers and patients.
Some reported challenges if they were one of the few providers in their workplace, though said that they eventually learned who they could talk to. Some also said that the availability of supports within some hospitals could vary “depending on the day”, with one noting the lack of formal support systems, such as access to a mental health team, peer support groups, or values clarification workshops. Those who had completed values clarifications workshops said that they were useful in figuring out their own beliefs and in understanding the views of their non-providing colleagues. They also believed that management needed to hire more abortion-friendly staff to alleviate the workload and to increase opportunities for collegial support.
The “privilege” of providing abortion care
The providers all reflected positively on their work and believed that they make a positive impact to society by providing care. Many shared sentiments that “while [abortion care is] extremely challenging work, it’s very rewarding”, and felt proud that they were able to provide a necessary service, particularly in the context of historical legal restrictions. Some even said that abortion care has been one of the most rewarding duties of their career.
Discussion
This phenomenological qualitative study explored the experiences of 13 providers of liberalised abortion care in the Republic of Ireland. They reflected on the changes in public opinion which allowed for liberalised care, though acknowledged the minority who continue to oppose the service. They also believed that implementation has been successful in delivering a safe, robust, and largely accessible service in general practice, though noted greater challenges in Irish hospitals. Personally, many experienced moments of doubt in their work, though all remained committed to the provision of care, believing abortion to be an important and necessary service.
Public reactions to abortion care
The providers believed that the majority of people in Ireland supported the provision of abortion care, as evidenced by the strength of the referendum result. All reflected positively on this change, believing that Ireland had become more accepting and compassionate. Despite this, all described anti-abortion sentiments from family, friends, colleagues, community members, and strangers related to their support of and involvement in abortion care. This aligns with a previous study, which found that abortion providers in Ireland faced negativity about this part of their work.Citation35 It appears that the providers expected more negativity about their work given the hostile nature of the referendum. Indeed, some discussed unfounded fears of harassment and repercussions related to their work. In reality, they said they tolerated anti-abortion experiences, while many also said they could avoid them by limiting or withholding disclosure of their work.
Additionally, the providers acknowledged the minority who continue to oppose liberalised care. They believed that protesters aim to scaremonger and shame women from accessing care and were frustrated by their refusal to protest at appropriate venues, such as government buildings. They also expressed frustration at the government’s inaction in implementing safe access zones at providing hospitals and community-based practices. While the providers in this study had little experience with protests, it must be noted that they are more common for others nationally.Citation40 Over three and a half years after the introduction of abortion care in Ireland, the government announced in July 2022 that they had approved a bill to legislate for safe access zones that would prevent people from protesting within 100 metres of a maternity hospital or general practice.Citation41 As of the time of writing in March 2023, this bill has not been signed into law and protests continue to occur nationwide.
Reflections on the implementation of liberalised abortion care
Our findings suggest that, from the providers’ perspectives, the implementation of abortion care in general practice was successful in delivering a robust, safe, and largely accessible EMA service. Though initial high demand for care was a challenge for many, they believed that demand had since fallen to an acceptable level. Additionally, the providers said that the anonymous nature of general practice helped to destigmatise abortion and that the existing infrastructure helped ensure that the services are widely available, which is supported by a study exploring the implementation of care in Irish general practice.Citation42
Despite perceived success, however, the providers noted remaining issues in the provision of EMA care. Some GPs, especially those in rural areas, do not have a providing local GP colleague or hospital. Though START has given many GPs access to peer support, the providers believed that the lack of a providing local hospital increased feelings of isolation and made it more difficult to provide. This was supported by another study in Ireland, which found that while START helped to “cocoon providers” during the early stages of implementation, there were increased challenges for GPs if their local hospital did not provide.Citation42 Further work is required to ensure that GPs are supported by a local hospital, which may help to increase the number of providers in rural areas. Some in this study also noted that a minority of GPs obstruct patients from timely access to care. This is in strict opposition to ethical guidelines from the Irish Medical CouncilCitation43 and the World Health Organization,Citation44 and work is needed so that all GPs are aware of their ethical obligation to provide information on how to access care. Lessons from Ireland may be of use in other countries seeking to implement a community-care led abortion service.
By contrast, implementation presented more challenges in Irish hospitals. Initial challenges with conscientious objection were resolved through careful planning and the publication of ethical guidelines on the limits of conscientious objection for doctors, midwives, and nurses.Citation43,Citation45 Beyond implementation, the hospital-based providers noted that high levels of objection mean that those who provide abortion care do so in addition to their other tasks, often without renumeration. These findings are supported by a study that explored the implementation of care in Irish hospitals, which found that abortion care generally relies on a small number of dedicated champions.Citation46 Increasing the number of staff willing to provide abortion care could support hospital staff in their role.
As regards the operation of the abortion care services, while some hospitals had integrated abortion into its “normal structure”, others failed to do so by placing the service in an unsuitable part of the hospital, allocating too few staff, and limiting involvement to a small number of consultants. Many also highlighted the importance of fostering open dialogue among all staff to aid the normalisation of care and some believed they had a role in opening conversations and challenging misinformation and anti-abortion attitudes. Additionally, the providers believed that high rates of objection coupled with low staffing levels in regional hospitals were a leading reason why eight maternity units in Ireland still do not offer abortion care. Though the providers supported their colleague’s right to conscientiously object to care, they did not support that these eight hospitals failed to provide any abortion services and believed that abortion-friendly staff should be hired to provide care in each unit. Further work is required to explore how ongoing issues can be resolved to ensure that abortion is fully integrated and normalised in providing hospitals and to encourage non-providing hospitals to introduce an abortion service.
Resolving moral doubt and remaining committed to abortion care
Although all providers were motivated to provide abortion care, believing it to be an important and necessary service, it was clear that thinking about the fetus constituted a challenge for many providers, which made many think that abortion results in the loss of potential life. This was particularly true for many of the providers, given that they regularly have contact with the fetus when providing in-patient abortion care. Moments of moral doubt centred around care provided under 12 weeks’ gestation, and providers generally did not discuss similar experiences when providing care after 12 weeks (i.e. abortion for medical reasons, emergency situations, or pregnancies affected by fatal fetal anomalies). Additionally, some of the providers discussed concerns that abortion care under 12 weeks could be used as a method of contraception. There was also frustration towards the lack of free contraception in Ireland. Since then, in September 2022, the Irish government announced plans to make contraception free for women aged 16–30 years.Citation47 Though this is a step forward, women outside of this age range and all men still do not have access to free contraception and work is required to ensure contraception is accessible for all, which could help to improve providers’ level of comfort.
While acknowledging moments of doubt during their work, the providers affirmed that these were infrequent and had no influence on their intentions to provide care. In deciding to provide care, all believed that their role is to facilitate access to safe and compassionate care and not to make moral decisions for their patients. Just as women’s stories evidenced the need for a legal abortion service during the referendum, patients’ stories constantly highlighted the importance of liberalised care and motivated the providers to continue their work. They expressed pride in their ability to provide care to a previously marginalised group in Ireland and some even said that their involvement in abortion care is the most rewarding part of their work. The providers also highlighted the importance of collegial support, particularly given that most have no previous experience in abortion care. Just as colleagues offered support in the face of practical challenges when implementing the services, they also allowed providers to reflect on their experiences and discuss doubts about their involvement without the fear of judgment. After liberalisation and in the face of ongoing criticism of liberalised abortion care, it seemed that providers banded together to support one another and overcome challenges as a collective group, especially as many felt that they could not talk about their work with family, friends, and non-providing colleagues. While all discussed feeling supported, further work is needed to ensure that providers, especially those in hospitals, have adequate support. Additionally, future research could aim to investigate formal and informal support systems available to providers in Ireland with the intent of exploring what supports would be most beneficial. models how the providers’ experiences affirmed their belief that abortion care is an important service and how this in turn helped to buffer against the challenges they experienced.
Abortion stigma in the Republic of Ireland
In conducting this study, it is important to consider how the providers’ accounts evidence the stigmatisation of abortion care in the Republic of Ireland. Abortion stigma has been defined as the “shared [societal] understanding that abortion is morally wrong and/or socially unacceptable” that is rooted in cultural beliefs that abortion violates the “feminine ideals” of motherhood, is seen as dirty or unhealthy, and results in the “murder” of an unborn fetus, and the stigma is promoted by anti-abortion groups.Citation48 The most obvious example of abortion stigma was the providers’ experiences with anti-abortion sentiments from family, friends, and colleagues. Many also discussed the anti-abortion attitudes that exist within wider society, as evidenced by the anti-repeal referendum campaigns, experiences within their local communities, and the minority who continue to oppose the safe provision of care. As highlighted, we have found similar findings about anti-abortion experiences among providers in the Republic of Ireland.Citation35 In response to anti-abortion sentiments within their communities, some in the current study opted to withhold disclosure of their abortion work. This perpetuates the legitimacy paradox,Citation49 a cycle whereby choosing not to disclose work means that anti-abortion stereotypes are not challenged, stereotypes then lead to prejudice and discrimination towards providers, which lead providers to hide their work. While providers and patients should not be forced to put themselves at risk of anti-abortion experiences, the normalisation of abortion care requires that the services be visible. Opportunities to support normalisation should be explored.
Additionally, the providers’ own reflections on their work, and particularly their acknowledgement of moments of moral doubt, highlight the abortion stigma that providers may hold. The providers only described moments of moral doubt when providing care under 12 weeks and similar concerns were not discussed for care after 12 weeks, presumably given the evident moral justification for the abortion to protect the patient’s health or life, or if the presence of a medical condition means that the fetus is unlikely to survive after birth. Many also highlighted patients who accessed care after 12 weeks when discussing the memorable cases that motivated their continued involvement in care. This shows an implicit value judgment among many providers that some abortions are “more acceptable” than others. This is most evident among those who admitted that they sometimes judge patients who they believe to use abortion as contraception, signalling that they did not unequivocally support abortion in every circumstance. Importantly, however, all actively challenged these value judgments by asserting that every woman should have the right to choose, that all abortions are valid, and that their role is to treat every patient with empathy and not to make moral judgments on their behalf.
The presence of doubt among the providers is not surprising, especially given Ireland’s morally conservative history and the previous restrictions on the provision of abortion care. Indeed, many providers reflected on the vast changes in societal attitudes towards abortion and on the evolution of their own beliefs over time. Additionally, even after the referendum, anti-abortion groups in Ireland continue to equate abortion care to murder and publicise inaccurate information and graphic images about care in an effort to promote their anti-abortion sentiments. It may be that the culture that providers grew up with, trained and perhaps initially practised in (that of limited access to abortion care), coupled with prominent anti-abortion messaging, are the true cause of occasional moral doubts rather than involvement in the abortion procedure itself. Regardless, it is vital to note again that the providers in the current study actively challenged moments of doubt, highlighting their commitment to safeguard women’s right to access care and efforts to deconstruct their personal abortion stigma. It is important that providers be supported in this process. One option may be to offer periodical values clarification workshops, where groups of providers can reflect on and discuss their beliefs. The providers in this study already have positive experiences with these workshops. Another option may be participation in activities that raise the occupational legitimacy of abortion care within the wider healthcare landscape in Ireland, such as the organisation of academic conferences and professional meetings. Another solution may be to create a national society of abortion care providers in Ireland, similar to the British Society of Abortion Care Providers,Citation50 which could identify new areas for further exploration and champion improvements to the services.
Study limitations
The results of this study must also be considered within some limitations. While a sample of 13 providers is in keeping with typical IPA studies and was sufficient to achieve thematic saturation, it may be that including more obstetricians, midwives, and nurses may have uncovered further experiences within the observed themes. We do, however, believe that the current sample includes a variety of perspectives as there are providers from each province in Ireland, from urban and rural areas, from seven of the 11 providing Irish maternity units, and from group and single GP practices. Our results offer providers the opportunity to reflect on their own experiences, but do not seek to be a representative account for every provider of abortion care in the Republic of Ireland. Secondly, we acknowledge the vast differences between abortion care in early pregnancy and care at later gestations. Our study focused primarily on providers’ experiences with abortion care under 12 weeks, as only four providers had direct experience of providing care after 12 weeks. We recommend future research specifically explores the experiences of those who provide care after 12 weeks. Finally, it may have been preferable to interview providers longitudinally to explore whether their experiences have changed over time as they gather more experience. A longitudinal design was not possible given the constraints of the current study, though we acknowledge that a future study may explore this.
Conclusion
The current study found that providers of liberalised abortion care in the Republic of Ireland experienced challenges related to their involvement in care, many of which highlight the inherent stigmatisation of abortion care in the country. Examples included experiences with anti-abortion sentiments, moments of moral doubt, and ongoing challenges related to the implementation of care. Despite these, the providers all reflected positively on their work and affirmed their commitment to providing care. By prioritising the remaining issues to adequately support providers in all aspects of their work, improvements to providers’ experiences, as well as patients’ experiences, will occur.
Authors’ contributions
B. Dempsey contributed to the conceptualisation of the study, the study methodology, participant recruitment, data collection, qualitative analysis, and writing and editing this manuscript. M. Connolly contributed to the study methodology, participant recruitment, qualitative analysis, and writing and editing this manuscript. M. F. Higgins contributed to the conceptualisation of this study, the study methodology, participant recruitment, qualitative analysis, and writing and editing this manuscript.
Acknowledgements
We would like to thank the providers’ who gave their time to complete interviews and discuss their involvement in providing liberalised care. We would also like to thank all providers working in the Republic of Ireland for choosing to offer this vital service.
Disclosure statement
MH advocated for a change to the constitution to allow expanded abortion care in 2018; no other potential conflicts of interest were reported by the author(s).
Additional information
Funding
References
- The Irish Times. Abortion Referendum Result. Available from: https://www.irishtimes.com/news/politics/abortion-referendum/results (April 1st, 2022)2018 .
- Higgins MF. Ireland’s eighth amendment: I want to care for women, not abandon them. BMJ 2018;361:k2111.
- Offences Against the Person Act. 1861. [Cited on 5th of June, 2022]. (UK) Available from: https://www.legislation.gov.uk/ukpga/Vict/24-25/100/contents.
- Calkin S, Kaminska ME. Persistence and change in morality policy: The role of the Catholic Church in the politics of abortion in Ireland and Poland. Fem Rev. 2020;124(1):86–102.
- Bloomer F, O’Dowd K. Restricted access to abortion in the Republic of Ireland and Northern Ireland: exploring abortion tourism and barriers to legal reform. Cult Health Sex. 2014;16(4):366–380.
- Eighth Amendment of the Constitution Act. 1983. (IE) [cited 4th of June, 2022]. Available from: https://www.irishstatutebook.ie/eli/1983/ca/8/enacted/en/print.
- Earner-Byrne L, Urquhart D. The Irish abortion journey, 1920–2018. London: Palgrave Pivot; 2019.
- McKimmons E, Caffrey L. Discourse and power in Ireland’s Repeal the 8th movement. Interface: J Soc Mov. 2021;13(1):193–224.
- The Citizens’ Assembly. Final Report on the Eighth Amendment of the Constitution. 2017. [Cited on 6th of June, 2022]. Available from: https://2016-2018.citizensassembly.ie/en/The-Eighth-Amendment-of-the-Constitution/Final-Report-on-the-Eighth-Amendment-of-the-Constitution/Final-Report-on-the-Eighth-Amendment-of-the-Constitution.html.
- Carnegie A, Roth R. From the grassroots to the Oireachtas: abortion law reform in the Republic of Ireland. Health Hum Rights. 2019;21(2):109–120.
- Taylor M, Spillane A, Arulkumaran SS. The Irish journey: removing the shackles of abortion restrictions in Ireland. Best Pract Res Clin Obstet Gynaecol. 2020;62:36–48.
- Cullen P, Korolczuk E. Challenging abortion stigma: Framing abortion in Ireland and Poland. Sex Reprod Health Matters. 2019;27(3):1686197.
- Fletcher R. #RepealedThe8th: Translating travesty, global conversation, and the Irish abortion referendum. Fem Leg Stud. 2018;26(3):233–259.
- Abortion Referendum Result. The Irish Times. 2018. [Cited on 1st of April, 2022]. Available from: https://www.irishtimes.com/news/politics/abortion-referendum/results.
- Government of Ireland. Health (Regulation of Termination of Pregnancy) Act 2018. [Cited April 1st, 2022]. Available from: http://www.irishstatutebook.ie/eli/2018/act/31/enacted/en/html.
- The Health Service Executive. Hospitals providing abortion care. [Cited April 1st, 2022]. Available from: https://www2.hse.ie/conditions/abortion/how-to-get/in-hospital/ 2019.
- Murphy E. Less than one in nine GPs are providing abortion services. Newstalk. [Cited April 1st, 2022]. Available from: https://wwwnewstalkcom/news/less-than-one-in-nine-gps-providing-abortion-services-figures-show-1306328. 2022.
- Horgan P, Thompson M, Harte K, et al. Termination of pregnancy services in Irish general practice from January 2019 to June 2019. Contraception. 2021;104(5):502–505.
- The Health Service Executive. Draft Model of Care for the Termination of Pregnancy Service. [Cited 24th of February, 2023]. Available from: https://irishpracticenurses.ie/wp-content/uploads/2019/01/Final-Draft-Termination-of-Pregnancy-Model-ofCare-18.12.18.pdf; 2018.
- Conlon C, Antosik-Parsons K, Butler E. Unplanned pregnancy and abortion care (UnPAC) study. Dublin: Sexual Health and Crisis Pregnancy Programme; 2022.
- Health Service Executive. Where to go for an abortion. 2023. [Cited 21st of February, 2023]. Available from: https://www2.hse.ie/conditions/abortion/how-to-get/where-to-go/.
- Government of Ireland. Health (Regulation of Termination of Pregnancy) Act 2018 - Annual Report on Notifications 2019. [Cited April 1st, 2022]. Available from: https://www.gov.ie/en/publication/b410b-health-regulation-of-termination-of-pregnancy-act-2018-annual-report-on-notifications-2019/.
- Government of Ireland. Health (Regulation of Termination of Pregnancy) Act 2018 - Annual Report on Notifications 2020. [Cited April 1st, 2022]. Available from: https://www.gov.ie/en/publication/ef674-health-regulation-of-termination-of-pregnancy-act-2018-annual-report-on-notifications-2020/.
- Government of Ireland. Health (Regulation of Termination of Pregnancy) Act 2018 - Annual Report on Notifications 2021. 2022. Available from: https://www.gov.ie/en/press-release/7bc58-third-annual-report-on-notifications-in-accordance-with-the-health-regulation-of-termination-of-pregnancy-act-2018/.
- Mullally A, Horgan T, Thompson M, et al. Working in the shadows, under the spotlight - Reflections on lessons learnt in the Republic of Ireland after the first 18 months of more liberal Abortion Care. Contraception. 2020;102(5):305–307.
- Department of Health and Social Care. Abortion Statistics, England and Wales: 2019. 2020. [Cited Accessed on 2nd of June, 2022]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/891405/abortion-statistics-commentary-2019.pdf.
- Grimes L, Shaughnessy O, Roth A, et al. Analysing MyOptions: Experiences of Ireland’s abortion information and support service. BMJ Sex Reprod Health. 2022;48:222–226.
- Harris LH, Debbink M, Martin L, et al. Dynamics of stigma in abortion work: Findings from a pilot study of the Providers Share Workshop. Soc Sci Med. 2011;73(7):1062–1070.
- Nicholson J, Slade P, Fletcher J. Termination of pregnancy services: Experiences of gynaecological nurses. J Adv Nurs. 2010;66(10):2245–2256.
- Mizuno M. Confusion and ethical issues surrounding the role of Japanese midwives in childbirth and abortion: a qualitative study. Nurs Health Sci. 2011;13(4):502–506.
- Britton LE, Mercier RJ, Buchbinder M, et al. Abortion providers, professional identity, and restrictive laws: a qualitative study. Health Care Women Int. 2017;38(3):222–237.
- Debbink MLP, Hassinger JA, Martin LA, et al. Experiences with the Providers Share Workshop method: abortion worker support and research in tandem. Qual Health Res. 2016;26(13):1823–1837.
- Möller A, Öfverstedt S, Siwe K. Proud, not yet satisfied: the experiences of abortion service providers in the Kathmandu Valley, Nepal. Sex Reprod Healthc. 2012;3(4):135–140.
- Teffo ME, Rispel LC. ‘I am all alone’: factors influencing the provision of termination of pregnancy services in two South African provinces. Glob Health Action. 2017;10(1):1347369.
- Dempsey B, Favier M, Mullally A, et al. Exploring providers’ experience of stigma following the introduction of more liberal abortion care in the Republic of Ireland. Contraception. 2021;104(4):414–419.
- Smith JA, Flowers P, Larkin M. Interpretative phenomenological analysis: theory, method, and research. London: SAGE; 2009.
- Smith JA. Qualitative Psychology: a practical guide to research methods. In: Smith JA, editor. Thousand Oaks, California: SAGE; 2015.
- Francis JJ, Johnston M, Robertson C, et al. What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Health. 2010;25(10):1229–1245.
- O’Mullan C, Doherty M, Coates R, et al. Using Interpretative Phenomenological Analysis (IPA) to provide insight into female sexual difficulties. Sex Relatsh Ther. 2017;34(1):75–86.
- Fitzsimons C. Irish healthcare workers experiences of anti-abortion protesters and the case for safe access zones. Available from: https://mural.maynoothuniversity.ie/16215/1/CamillaFitzsimons2022Irish.pdf; 2022.
- Minister Donnelly announces government approval of the heads of bill to legislate for termination of pregnancy safe access zones. (2018). [press release]. [Cited 28th of July 2022]. Available from: https://www.gov.ie/en/press-release/5bedd-minister-donnelly-announces-government-approval-of-the-heads-of-bill-to-legislate-for-termination-of-pregnancy-safe-access-zones/#:~:text=The%20General%20Scheme%20of%20the,healthcare%20premises%20will%20be%20designated.
- Mishtal J, Reeves K, Chakravarty D, et al. Abortion policy implementation in Ireland: Lessons from the community model of care. PLoS One. 2022;17(5):e0264494.
- Irish Medical Council. Guide to Professional Conduct and Ethics for Registered Medical Practitioners (Amended). 2019.
- The World Health Organization. Abortion Care Guideline, Recommendation 22. Available from: https://cdn.who.int/media/docs/default-source/reproductive-health/abortion/supplementary-material-1.pdf?sfvrsn=5bc94f18_7; 2022.
- [Nursing] & Midwifery Board of Ireland. Code of Professional Conduct and Ethics for Registered Nurses and Registered Midwives. 2021.
- Stifani BM, Mishtal J, Chavkin W, et al. Abortion policy implementation in Ireland: successes and challenges in the establishment of hospital-based services. SSM - Qualitative Research in Health. 2022;2:100090.
- Citizens Information. Budget 2023. Available from: https://www.citizensinformation.ie/en/money_and_tax/budgets/budget_2023.html#l605662022.
- Norris A, Bessett D, Steinberg JR, et al. Abortion stigma: a reconceptualization of constituents, causes, and consequences. WHI. 2011;21(3 Suppl):S49–S54.
- Harris LH, Martin L, Debbink M, et al. Physicians, abortion provision and the legitimacy paradox. Contraception. 2013;87(1):11–16.
- British Society of Abortion Care Providers. Hompage. [cited 13th of August 2022]. Available from: https://bsacp.org.uk/.