Abstract
A novel H7N9 avian influenza A virus (IAV) emerged in China in early 2013 causing > 450 cases of respiratory illness and 175 deaths within a 20-month period. Though avian viruses infect humans infrequently, the lack of human immunity to these viruses raises the possibility of a pandemic if they were to acquire the ability to transmit efficiently. Despite the fact that IAV pathogenicity results from the cytopathic effects and tissue damage caused by both viral replication and an overly robust immune response, current IAV therapeutics only target the viral proteins. This has led to the emergence of drug resistance due to the high mutation rates of viruses. The growing obsolescence of our current influenza therapeutics underscores the need for alternative treatment strategies. One promising area of research is the use of drugs that target the host response to IAV infection. This article describes how gene expression profiling can be used to predict drugs that reverse the destructive effects of the host response to H7N9 and other pathogenic influenza viruses.
In February 2013, a novel H7N9 influenza A virus (IAV) emerged in China causing an outbreak of > 450 cases of respiratory illness and 175 deaths within a 20-month period Citation[1]. Though there is evidence that some H7N9 infections resulted in minor symptoms, most infections resulted in influenza-like symptoms such as coughing and fever that developed into pneumonia and acute respiratory distress syndrome Citation[2,3]. Epidemiological studies suggest that most cases of H7N9 influenza resulted from contact with infected poultry. Though avian viruses infect humans infrequently, the lack of immunity to these viruses raises the possibility of a pandemic if they acquired the ability to transmit efficiently. Such a scenario arose when an emergent H1N1 influenza virus killed 50 – 100 million people during the 1918 influenza pandemic Citation[4].
H7N9 is less pathogenic than H5N1 in both humans and animal models, but is more transmissible than H5N1 in both ferret and guinea pig experiments Citation[5]. Additionally, several isolates of H7N9 contain mutations that are associated with mammalian adaptation Citation[5]. In contrast to H5N1, some H7N9 viruses are able to bind human (α2,6-sialic acid) receptors, though their affinity for human receptors is lower than that of highly transmissible viruses such as pH1N1. Of the three residues that are associated with increased human receptor binding (V186, L226, and S228), H7N9 hemagglutinin contains two (V186 and L226), suggesting that additional changes to the virus could lead to efficient human-to-human transmission Citation[6,7]. Additionally, the PB2 of many H7N9 isolates contain residue 627K, which is associated with increased mammalian adaptation, instead of the typical avian 627E. Furthermore, H7N9 isolates that lack PB2 – 627K contain residues such as PB2 – 701N, which also increase mammalian adaptation Citation[8]. This has generated concern over further H7N9 mammalian adaptation and acquisition of sustainable person-to-person transmissibility.
Despite the fact that IAV pathogenicity results from tissue damage caused by both viral replication and an overly robust immune response, current IAV therapeutics only target viral proteins instead of targeting the host response. Unfortunately, IAVs mutate easily and can escape inhibition by acquiring changes that prevent their proteins from interacting with antiviral drugs. In fact, some isolates of H7N9 are resistant to some of the current influenza treatments on the market Citation[9,10]. All H7N9 isolates sequenced thus far contain sequences that render them resistant to the M2-ion channel blockers, amantadine and rimantadine; and some H7N9 isolates have also acquired sequences that provide resistance to neuraminidase inhibitors such as oseltamivir and zanamivir.
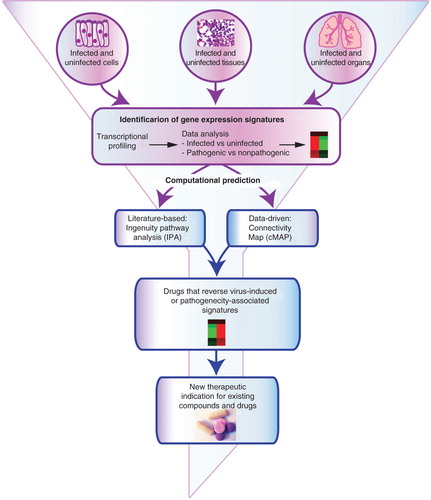
The growing obsolescence of current influenza therapeutics underscores the need for alternative strategies. One promising area of research is the use of drugs that target the host response to infection. Host-targeting drugs could be used alone or in conjunction with antiviral therapy and have shown efficacy in mouse models Citation[11]. A striking feature of severe influenza infections is hypercytokinemia. H7N9-infected patients have high concentrations of proinflammatory cytokines in their blood Citation[12]. Furthermore, the severity of H7N9 influenza correlates with the intensity of the hypercytokinemia Citation[13]. It is clear that host responses can determine disease severity, so understanding the transcriptional programs that drive them can identify host targets for therapeutic intervention. Gene expression profiles from H7N9-infected cells and tissues can be utilized to computationally identify small molecules and FDA-approved drugs that reverse the host gene expression patterns that may drive H7N9 pathogenesis. We have characterized the transcriptional response to H7N9 infection in human airway epithelial cells, BALB/c mice and cynomolgus macaques to identify host transcriptional signatures that distinguish H7N9 from other IAVs and are predictive of influenza pathogenicity across a range of influenza serotypes and strains Citation[14-16]. Our host-directed approach to drug discovery has also identified drugs that could potentially be used to treat severe influenza caused by H7N9 and other pathogenic IAVs. Several of these drugs are FDA-approved and could potentially be repurposed as influenza therapeutics. These potential host-targeting drugs would not have been identified using the virus-targeted approach that is normally undertaken in traditional influenza labs. We will discuss the findings of these studies in the next two paragraphs.
When influenza virus enters the respiratory tract of a human, it initially infects the epithelial cells that line the airways. How these cells first respond to infection drives the recruitment of different immune cell types to the sites of infection leading to viral clearance and/or hypercytokinemia and lung damage. Studies undertaken in polarized human airway epithelial cells therefore offer insights into what the initial host response to IAV entails. When we profiled polarized Calu3 (human airway epithelial) cells infected with H7N9, we found transcriptomic evidence of the human adaptation potential of H7N9; the transcriptomic response to H7N9 was more similar to the response to human H3N2 than to responses to the other avian influenza viruses Citation[14]. Considering the effect of other lung cell types in addition to epithelial cells on host response and disease progression can deliver additional targets for host-directed interventions. To that end, we applied global transcriptomic profiling to whole lungs from H7N9-infected BALB/c mice. Transcriptional responses to H7N9 were intermediate to those caused by pH1N1 and H5N1 early in infection, but grew to resemble the H5N1 response as infection progressed. Infection with H5N1, H7N7 and H7N9, which are lethal in mice, increased transcription of cytokine response genes and decreased transcription of coagulation and lipid metabolism genes Citation[15]. The decreased transcription of coagulation and lipid metabolism genes identified in the mouse study was not identified in Calu3 cells indicating that it is likely driven by non-epithelial cell types or by the crosstalk between multiple cell types in the lung. Strikingly, this gene expression signature also occurs in the whole lung response to the infamous 1918 H1N1 virus, indicating that it may predict pathogenicity across different strains Citation[15]. Experiments in cynomolgus macaques confirmed the validity of the pathways and molecules identified in the H7N9 mouse model Citation[16].
Transcriptome-based antiviral prediction can be accomplished by two independent yet complementary methods: literature-based prediction and data-driven prediction (). Our group used the Ingenuity Knowledge Database, which curates gene expression signatures from the peer-reviewed literature, to identify drugs that were predicted to reverse the gene expression signatures to H7N9 in human lung airway cells, mice and macaques. We also conducted data-driven prediction based on the Connectivity Map (Cmap), a database of > 7,000 gene expression profiles representing cell lines treated with > 1000 compounds Citation[17]. Human airway epithelial cell profiling identified several drugs predicted to reverse the host response to H7N9, including several kinase inhibitors, as well as FDA-approved drugs such as troglitazone and minocycline. Mouse experiments identified some of the same drugs that were associated with the cell line study, but also found molecules that were unique to that dataset, suggesting they may target non-epithelial cell responses. Several of the drugs that had been identified in our Calu3 and mouse studies were also identified in the NHP study suggesting these may be high-priority candidates for efficacy testing. Importantly, we showed that minocycline, which was predicted in more than one study, inhibited H7N9 replication in vitro indicating that our computational approach holds promise for identifying novel antivirals Citation[14]. Minocycline’s protective properties may be due to its ability to prevent inflammation by inhibiting matrix metalloproteinases, scavenging reactive oxygen species and inhibiting apoptosis Citation[18].
Influenza viruses cause 3 – 5 million cases of severe illness and 250,000 – 500,000 deaths per year worldwide Citation[19]. When these enormous numbers are compared to the 5000 deaths caused by the current Ebola outbreak, it is clear that finding new influenza vaccines and therapeutics is an important global health issue. We cannot predict when a new influenza virus will emerge to wreak havoc on the human population, and human cases of H10N8, H6N1 and H9N2 influenza have occurred recently. There will always be a lag between the emergence of a novel virus and the development of vaccines and antivirals against it. Increased focus must be placed on developing therapeutics to treat any new strain of IAV that arises especially as public distrust for the scientific community has lead to a decrease in vaccination rates. Targeting the host responses that are elicited in common by pathogenic IAV will allow us to identify molecules capable of treating illness caused by any emerging influenza strain.
Acknowledgements
We thank Dr. Marcus Korth for his insightful comments on the manuscript.
Declaration of interest
This project has been funded in whole or in part with Federal funds from the National Institute of Allergy and Infectious Diseases, National Institutes of Health, Department of Health and Human Services, under Contract No. HHSN266200700026C. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Bibliography
- WHO risk assessment. Human infections with avian influenza A(H7N9) virus. 2014. Available from: http://www.who.int/influenza/human_animal_interface/influenza_h7n9/riskassessment_h7n9_2Oct14.pdf?ua=12014 [Last accessed 18 November 2014]
- CDC. Emergence of avian influenza A(H7N9) virus causing severe human illness - China, February-April 2013. MMWR Morb Mortal Wkly Rep 2013;62(18):366-71
- Gao HN, Lu HZ, Cao B, et al. Clinical findings in 111 cases of influenza A (H7N9) virus infection. N Engl J Med 2013;368(24):2277-85
- Taubenberger JK, Morens DM. 1918;Influenza: the mother of all pandemics. Emerg Infect Dis 2006;12(1):15-22
- Watanabe T, Watanabe S, Maher EA, et al. Pandemic potential of avian influenza A (H7N9) viruses. Trends Microbiol 2014;22(11):623-31
- Dortmans JC, Dekkers J, Wickramasinghe IN, et al. Adaptation of novel H7N9 influenza a virus to human receptors. Sci Rep 2013;3:3058
- Tharakaraman K, Jayaraman A, Raman R, et al. Glycan receptor binding of the influenza a virus H7N9 hemagglutinin. Cell 2013;153(7):1486-93
- Mok CK, Lee HH, Lestra M, et al. Amino acid substitutions in polymerase basic protein 2 gene contribute to the pathogenicity of the novel A/H7N9 influenza virus in mammalian hosts. J Virol 2014;88(6):3568-76
- Chen Y, Liang W, Yang S, et al. Human infections with the emerging avian influenza A H7N9 virus from wet market poultry: clinical analysis and characterisation of viral genome. Lancet 2013;381(9881):1916-25
- Hu Y, Lu S, Song Z, et al. Association between adverse clinical outcome in human disease caused by novel influenza A H7N9 virus and sustained viral shedding and emergence of antiviral resistance. Lancet 2013;381(9885):2273-9
- Xu L, Bao L, Li F, et al. Combinations of oseltamivir and fibrates prolong the mean survival time of mice infected with the lethal H7N9 influenza virus. J Gen Virol 2014;96(Pt 1):46-51
- Chi Y, Zhu Y, Wen T, et al. Cytokine and chemokine levels in patients infected with the novel avian influenza A (H7N9) virus in China. J Infect Dis 2013;208(12):1962-7
- Wang Z, Zhang A, Wan Y, et al. Early hypercytokinemia is associated with interferon-induced transmembrane protein-3 dysfunction and predictive of fatal H7N9 infection. Proc Natl Acad Sci USA 2014;111(2):769-74
- Josset L, Zeng H, Kelly SM, et al. Transcriptomic characterization of the novel avian origin influenza A (H7N9) virus: specific and intermediate host-response between avian (H5N1 and H7N7) and human (H3N2) viruses and implications for treatment options. mBio 2014;5(1):e01102-13
- Morrison J, Josset L, Tchitchek N, et al. H7N9 and other pathogenic avian influenza viruses elicit a three-pronged transcriptomic signature that is reminiscent of 1918 influenza virus and is associated with lethal outcome in mice. J Virol 2014;88(18):10556-68
- de Wit E, Rasmussen AL, Feldmann F, et al. Influenza virus A/Anhui/1/2013 (H7N9) replicates efficiently in the upper and lower respiratory tracts of cynomolgus macaques. mBio 2014;5(4):e01331-14
- Lamb J. The Connectivity Map: a new tool for biomedical research. Nat Rev Cancer 2007;7(1):54-60
- Griffin MO, Ceballos G, Villarreal FJ. Tetracycline compounds with non-antimicrobial organ protective properties: possible mechanisms of action. Pharmacol Res 2011;63(2):102-7
- WHO. Influenza (Seasonal): Fact sheet 211. 2014. Available from: http://www.who.int/mediacentre/factsheets/fs211/en/2014; [Last accessed 18 November 2014]