Abstract
Background
Patient-ventilator asynchrony is a common problem in mechanically ventilated patients; the problem is especially obvious in COPD. Neutrally adjusted ventilatory assist (NAVA) can improve patient-ventilator asynchrony; however, the effect in COPD patients with prolonged mechanical ventilation is still unknown. The goals of this study are to evaluate the effect of NAVA and conventional weaning mode in patients with COPD during prolonged mechanical ventilation.
Methods
The study enrolled a total of 33 COPD patients with ventilator dependency for more than 21 days in the weaning center. A diaphragm electrical activity (Edi) catheter was inserted in patients within 24 hours after admission to the respiratory care center, and patients were randomly allocated to NAVA or conventional group. A spontaneous breathing trial was performed every 24 hours. The results correlated with the clinical parameters.
Results
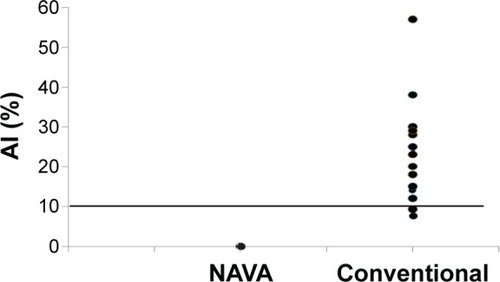
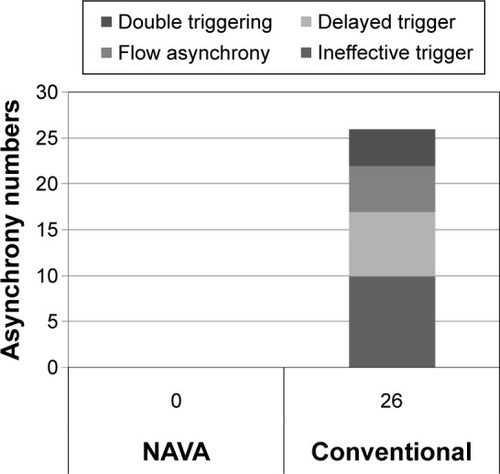
There were significantly higher asynchrony incidence rates in the whole group after using Edi catheter (before vs post-Edi catheter insertion =60.6% vs 87.9%, P<0.001). Asynchrony index: before vs post-Edi catheter insertion =7.4%±8.5% vs 13.2%±13.5%, P<0.01. Asynchrony incidence: NAVA vs conventional =0% vs 84.2%, P<0.001. Asynchrony index: NAVA vs conventional =0 vs 11.9±11.2 (breath %), P<0.001. The most common asynchrony events were ineffective trigger and delayed trigger.
Conclusion
Compared to conventional mode, NAVA mode can significantly enhance respiratory monitoring and improve patient-ventilator interaction in COPD patients with prolonged mechanical ventilation in respiratory care center.
Background
In patients with COPD, the process of weaning from mechanical ventilation is frequently complicated and prolonged by physiological and psychological circumstances. The reported rate of weaning failure in COPD is very high, approximately 61%, and as a result, in observed cases, there is 46%–59% prolonged invasive mechanical ventilation.Citation1,Citation2 Asynchrony is a particular problem in patients with mechanical ventilation and noninvasive mechanical ventilation,Citation3,Citation4 with a reported incidence between 10% and 88% during assisted mechanical ventilation.Citation3 Patients with COPD commonly experience asynchrony, primarily due to intrinsic positive end-expiratory pressure (PEEP), air trapping, expiratory flow limitation, excessive sedation, and suboptimal ventilator settings during assisted mechanical ventilation. Asynchrony is also associated with prolonged mechanical ventilation, longer intensive care unit stay, mortality, and respiratory muscle dysfunction; and air leaks are also a major cause of asynchrony during noninvasive ventilation.Citation5–Citation9
Two recent studies found an incidence of asynchrony in 25%–40% of patients on ventilatory assistance. They also found that an asynchrony index >10% is associated with a significantly prolonged time on ventilatory assistance.Citation10,Citation11 In contrast to the findings of Thille and Brochard, De Wit et al, and Chao et al, in the patient group with asynchrony, only 16% were successfully weaned, while 57% in the group without asynchrony were successfully weaned.Citation11–Citation13 In addition, another study by Doorduin et al also demonstrated that poor synchrony (timing errors above 20% between neural drive and pneumatic timing; NeuroSync index) is associated with the number of wasted efforts, which increases the work of breathing and causes NIV failure; worst case scenario will mean intubation in patients with COPD.Citation5
Traditional pneumatic modes used for mechanical ventilation are fixed on the basis of pressure and flow within the airways. Unlike the traditional pneumatic modes, neutrally adjusted ventilatory assist (NAVA) is a spontaneous mode, which triggers, cycles, and regulates gas delivery based on the diaphragmatic electromyography signal via a specially designed nasogastric tube (diaphragm electrical activity [Edi]).Citation14–Citation16 The level of ventilatory assistance is proportional to the patient’s breathing effort, there is no influence of auto-PEEP during the ventilator cycle, since the assistance starts with the patient’s breathing effort, and there should not be any influence from leaks during NIV due to better patient-ventilator interaction.Citation14,Citation17
Several studies have compared pneumatic modes (pressure support) to NAVA, with the majority of studies showing that NAVA improves patient-ventilator interaction, diaphragm efficiency, patient comfort (through synchrony), and sleep quality by increasing the slow-wave sleep. Moreover, NAVA can avoid the risk of excessive assistance and reduced ventilatory drive, and improve physiological parameters, with the delivery of lung protective tidal volumes while allowing patients to breathe spontaneously.Citation16,Citation18–Citation23
This study hypothesizes that in patients with severe COPD who underwent prolonged mechanical ventilation, NAVA will improve weaning outcome compared to conventional weaning methods by improving patient-ventilator interaction. To date, no clinical studies have been published about the effectiveness of NAVA in COPD patients with prolonged mechanical ventilation. The goal of this study is to compare the effect of NAVA to conventional mode in a randomized controlled trial in patients with severe COPD.
Patients and methods
This study was designed as a prospective, randomized, controlled clinical study to determine the weaning efficacy of NAVA vs conventional modes in patients with COPD who endured weaning failure for more than 21 days. The clinical trial registration number is CMRPGB0382. The study enrolled a total of 37 COPD patients with prolonged mechanical ventilation in the respiratory care center (RCC) of Chang Gung Memorial Hospital between June 2012 and October 2014. This work was performed at Kaohsiung Chang Gung Memorial Hospital, Taiwan. The study was approved by the institutional review board of Chang Gung Memorial Hospital (IRB: 104-09970) and informed consent was obtained from the next of kin prior to start of the study. Inclusion criteria were: 1) older than or equal to 45 years with an established diagnosis of COPD, and 2) mechanical ventilation via intubation or tracheotomy, >21 days. Exclusion criteria were: 1) consent refused, 2) hemodynamic instability, 3) unable to breathe spontaneously, 4) poor short-term prognosis (defined as a high risk of death within 3 months), and 5) contraindications to the insertion of a nasogastric tube (such as face and nose fracture, recent nose surgery, esophageal obstruction).
After admission to the RCC, all patients were ventilated with a SERVO-i (Maquet, Solna, Sweden), with a clinician-set pressure support level or assist-control. An Edi catheter was inserted within 24 hours if the patient met the inclusion criteria and did not meet any of the exclusion criteria. The breathing capability of the patient was then tested by confirming a stable Edi signal >2 µV. If the Edi signal remained below this level, the ventilatory assistance has to decrease 30% and observe for 10 minutes. After decreasing the ventilatory 30% for 10 minutes and the Edi signal was still below 2 µV, or end-tidal CO2 reached 60 mmHg, the patient was excluded from the study and previous settings were restored. If the Edi signal was still below 2 µV, the patient was excluded from the study and previous settings were restored. Patients able to trigger the ventilator were then randomized to two groups: NAVA and conventional mode. A spontaneous breathing trial (SBT) was performed every 24 hours if the patient met the following criteria: 1) no fever or infection, 2) hemodynamic stability, 3) fraction of inspired oxygen (FiO2) <50%, and 4) PEEP <8 cmH2O. The SBT was performed with a PEEP of 5 cmH2O and pressure-support ventilation (PSV) level of 8 cmH2O. If the SBT was successful, the patient was evaluated for extubation and noninvasive ventilation. If the patient failed the SBT, he was returned to assisted ventilation with a NAVA setting corresponding to 50% of the peak Edi level during the SBT. The PSV group was returned to a PSV level mandated by the conventional weaning protocol.
Asynchrony events were obtained from the Edi signal and ventilator graphic waveform. The asynchrony index was calculated by comparing the Edi to the flow waveform during 1 minute. The primary outcomes of the study were to establish the detection rate of asynchrony events using waveform analysis or Edi, respectively, and to evaluate the weaning outcome in COPD patients with prolonged mechanical ventilation using NAVA or conventional weaning mode. The secondary outcomes included total length of mechanical ventilation, the length of RCC stay, hospital stay, and mortality rate after 90 days.
Data analysis
Data collection was performed before Edi catheter insertion, post-Edi catheter insertion, after randomization and implementation of the SBT every 24 hours. Data collection included demographic data, prognostic scores, and ventilator and hemodynamic values. Descriptive statistics were expressed as mean ± standard deviation or median and interquartile range depending on the nature and distribution of the variables. Variables normally distributed were compared by the Student’s t-test. For variables without a normal distribution, the Mann–Whitney U rank test was used for comparison. Categorical variables were compared using Fisher’s exact test. For all comparisons, a difference of P<0.05 was considered statistically significant. All analyses were performed using SPSS 17.0 software.
Results
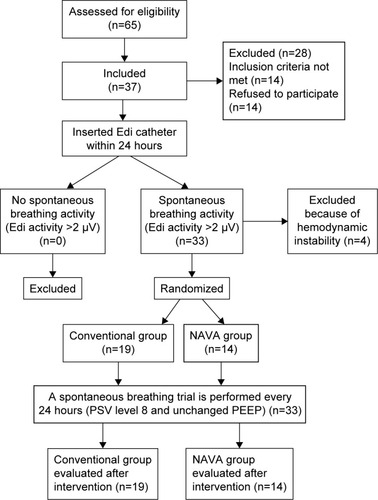
We included 37 COPD patients with ventilator dependency for more than 21 days, from June 2012 to October 2014. Four patients were excluded from the analysis due to hemodynamic instability. Flowchart of registered patients was presented in . The demographic and patient characteristics were presented in . Clinical data were collected during three different periods: T0: immediately after Edi catheter insertion, T1: after intervention, and T2: at the end of the SBT trial ().
Table 1 Patient characteristics
Table 2 Clinical data collection by T0, T1, T2Table Footnotea
Figure 1 Flowchart of registered patients.
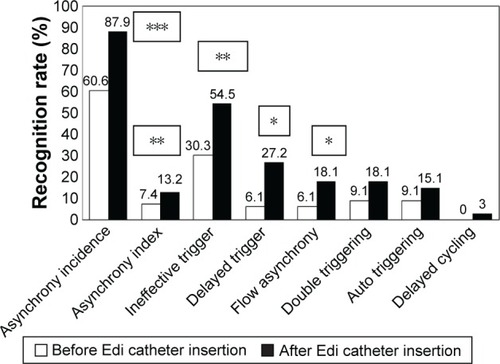
After admission to the RCC, an Edi catheter was inserted in all study subjects within 24 hours. Asynchrony recognition rates before and after Edi catheter insertion were described in . Asynchrony incidence diagnosed without Edi catheter was 60.6% and after Edi catheter insertion was 87.9% (P<0.001). Asynchrony index without Edi catheter was 7.4% and after Edi catheter insertion was 13.2% (P<0.01). The asynchrony events calculated from the flow waveforms and Edi signals, respectively, were: ineffective trigger 30.3% vs 54.5% (P<0.005); delayed trigger 6.1% vs 27.2% (P<0.008); flow asynchrony 6.1% vs 18.1% (P<0.04); double triggering 9.1% vs 18.1% (P<0.08); auto triggering 9.1% vs 15.1% (P<0.15), and delayed cycling 0% vs 3.0% (P<0.15).
Figure 2 Asynchrony recognition rate before and after Edi catheter insertion.
Abbreviation: Edi, diaphragm electrical activity.
Asynchrony classification and incidence for NAVA and conventional group were shown in . Asynchrony index in NAVA vs conventional mode was 0% vs 11.9% (P<0.001); ineffective trigger 0% vs 52.6% (P<0.001); delayed trigger 0% vs 36.8% (P<0.001); flow asynchrony 0% vs 26.3% (P<0.001); and double triggering 0% vs 21.1% (P<0.001). The main asynchrony events in this study were ineffective triggering (42.1%), delayed trigger (31.6%), flow asynchrony (26.3%), and double triggering (21.1%) in the conventional group. The asynchrony index was displayed in and the accumulated asynchrony numbers were displayed in . Outcomes in the NAVA and control group were described in . Mortality rate in NAVA vs the control group in the RCC was 7.1% vs 31.6% (P=0.09); 90-day mortality was 28.6% vs 31.6% (P=0.85); total RCC stay days were 20.3 d ±12.2 d vs 22.1 d ±21.1 d (P=0.78); and total ventilator days were 47.3 d ±28.8 d vs 49.2 d ±36.0 d (P=0.94).
Table 3 Asynchrony index between NAVA and control group (n=33)
Table 4 Weaning outcome after NAVA and conventional mode
Discussion
The main finding of this study demonstrates that NAVA improves patient-ventilator interaction compared to conventional mode in COPD patients with prolonged mechanical ventilation. COPD patients with acute respiratory failure requiring mechanical ventilation have frequent episodes of patient-ventilator asynchrony.Citation3,Citation7,Citation24 According to Thille et al and Thille and Brochard, one quarter of all patients had a high rate of asynchrony during assisted ventilation; interestingly, the incidence of asynchrony was nearly 82% in patients who received PSV and 18% during assist-control ventilation.Citation10,Citation11 In our study, 80% (N=23) of the patients who were transferred to our RCC, had a high level of pressure support (PSV level >15 cmH2O) or assist-control ventilation, and incidence of asynchrony was nearly 84% in the control group (N=16). This demonstrates that poor patient-ventilator interaction is a common problem in patients with COPD during invasive mechanical ventilation.
On the other hand, in our study, the Edi catheter could effectively provide a real-time demonstration of the degree of synchrony/asynchrony between the patient’s diaphragmatic activity and the conventionally triggered assisted breath.Citation25 Our asynchrony recognition rate after insertion of the Edi catheter was significantly different (P<0.05), indicating that monitoring based on the Edi signal could increase the ability to recognize the rate and the type of asynchrony in difficult to wean patients. The benefit of the Edi signal is enhanced respiratory monitoring. Respiratory monitoring using the Edi signal not only increases the ability to recognize the rate and the type of asynchrony, but may also aid clinical staff in resolving problems earlier.Citation26 Moreover, NAVA will improve patient-ventilator interaction owing to the fact that the pressure applied by the ventilator to the airway opening is proportional to the Edi signal. Sixty-nine percent (N=9) of patients in the NAVA group had better triggering after the change from conventional mode to NAVA mode.
Patients with COPD are regarded as particularly difficult to wean after prolonged mechanical ventilation, in our experience more than 21 days.Citation27 Our patients were characterized by old age (>75 years), high Acute Physiology and Chronic Health Enquiry (APACHE) II score (18.2±4.6), moderate obstructive pulmonary disease with multiple organ failure (Sequential Organ Failure Assessment [SOFA] Scale 4.1±2.5), and hypo-albuminuria (albumin [ALB] <3 g/dL). In patients with COPD, the process of weaning from mechanical ventilation is frequently complicated and prolonged by physiological and psychological circumstances such as old age, poor lung function, expiratory flow limitation, air trapping, increased intrinsic PEEP, patient discomfort, dyspnea, and sleep fragmentation, leading to a prolonged weaning process.Citation21,Citation28,Citation29
The weaning outcome and mortality in the NAVA group was better than the conventional group, although the weaning outcome was not significantly different, and some significant physiological results were also found in this study. Hence, further research should focus on enrolling a larger number of patients and recording some index of comfort in order to demonstrate better comfort than pneumatic modes and shorter weaning time in patients with COPD after prolonged mechanical ventilation.
Limitations
There is one major limitation in this study. Our study population was small and it was a single-center trial, hence, the result in weaning outcome is not statistically significant in this study. Although a better drive in NAVA mode, it could be improved if we measure index of comfort in this study.
Conclusion
Compared to conventional monitoring, Edi signal can significantly enhance respiratory monitoring, increasing the ability to recognize the rate and type of asynchrony. Compared to conventional pneumatic trigger, NAVA Edi trigger significantly improved patient-ventilator asynchrony, reduced work of breathing, and enhanced patient comfort by better synchrony in our COPD patients with prolonged mechanical ventilation. The NAVA mode also shows a trend in outcome benefit in the field of RCC mortality.
Author contributions
All authors contributed toward data analysis, drafting, and critically revising the paper, gave final approval of the version to be published, and agreed to be accountable for all aspects of work.
Acknowledgments
This study was supported by a grant from the Kaohsiung Chang Gung Memorial Hospital, Taiwan (CMRPGB0382). We are grateful to all the staff of the RCC who supported this project.
Disclosure
The authors report no conflicts of interest in this work.
References
- QuinnellTGPilsworthSShneersonJMSmithIEProlonged invasive ventilation following acute ventilatory failure in COPD: weaning results, survival, and the role of noninvasive ventilationChest2006129113313916424423
- PatthumAPetersMLockwoodCEffectiveness and safety of Neurally Adjusted Ventilatory Assist (NAVA) mechanical ventilation compared to standard conventional mechanical ventilation in optimizing patient-ventilator synchrony in critically ill patients: a systematic review protocolJBI Database System Rev Implement Rep20151333146
- JollietPTassauxDClinical review: patient-ventilator interaction in chronic obstructive pulmonary diseaseCrit Care200610623617096868
- NavaSPisaniLNeurally adjusted non-invasive ventilation in patients with chronic obstructive pulmonary disease: does patient-ventilator synchrony matter?Crit Care201418667025672776
- DoorduinJSinderbyCABeckJvan der HoevenJGHeunksLAutomated patient-ventilator interaction analysis during neurally adjusted non-invasive ventilation and pressure support ventilation in chronic obstructive pulmonary diseaseCrit Care201418555025307894
- de WitMPedramSBestAMEpsteinSKObservational study of patient-ventilator asynchrony and relationship to sedation levelJ Crit Care2009241748019272542
- EpsteinSKHow often does patient-ventilator asynchrony occur and what are the consequences?Respir Care2011561253821235836
- SinderbyCNavalesiPBeckJNeural control of mechanical ventilation in respiratory failureNat Med19995121433143610581089
- BransonRDBlakemanTCRobinsonBRAsynchrony and dyspneaRespir Care201358697398923709195
- ThilleAWRodriguezPCabelloBLelloucheFBrochardLPatient-ventilator asynchrony during assisted mechanical ventilationIntensive Care Med200632101515152216896854
- ThilleAWBrochardLPromoting patient-ventilator synchronyClin Pulm Med2007146350359
- De WitMMillerKBGreenDAOstmanHEGenningsCEpsteinSKIneffective triggering predicts increased duration of mechanical ventilationCrit Care Med200937102740274519886000
- ChaoDCScheinhornDJStearn-HassenpflugMPatient-ventilator trigger asynchrony in prolonged mechanical ventilationChest19971126159215999404759
- LelloucheFBrochardLAdvanced closed loops during mechanical ventilation (PAV, NAVA, ASV, SmartCare)Best Pract Res Clin Anaesthesiol2009231819319449618
- BarwingJAmboldMLindenNQuintelMMoererOEvaluation of the catheter positioning for neurally adjusted ventilatory assistIntensive Care Med200935101809181419652950
- SinderbyCNeurally adjusted ventilatory assist: insufficient evidence of broad clinical outcomesRespir Care20135811e153e15424155361
- SinderbyCBeckJNeurally adjusted ventilatory assist: first indications of clinical outcomesJ Crit Care201429466666724810731
- Diniz-SilvaFMoriyaHAlencarAAmatoMCarvalhoCFerreiraJUse of neurally adjusted ventilatory assist and pressure support ventilation to delivery protective mechanical ventilation in patients with acute respiratory distress syndrome: a randomized crossover clinical trialAm J Respir Crit Care Med2015191A3898
- DemouleAClavelMRolland-DebordCComparison of neurally adjusted ventilatory assist and pressure support ventilation during the early phase of weaning from mechanical ventilation – a randomized controlled studyAm J Respir Crit Care Med2015191A1189
- SpahijaJde MarchieMAlbertMPatient-ventilator interaction during pressure support ventilation and neurally adjusted ventilatory assistCrit Care Med201038251852620083921
- DelisleSOuelletPBellemarePTétraultJPArsenaultPSleep quality in mechanically ventilated patients: comparison between NAVA and PSV modesAnn Intensive Care2011114221955588
- UmbrelloMFormentiPUltrasonographic assessment of diaphragm function in critically ill subjectsRespir Care Epub2016126
- Di Mussi SpadaroSMirabellaLImpact of prolonged assisted ventilation on diaphragmatic efficiency: NAVA versus PSVCrit Care2016201126728475
- PowersSKWiggsMPSollanekKJSmuderAJVentilator-induced diaphragm dysfunction: cause and effectAm J Physiol Regul Integr Comp Physiol20133055R464R47723842681
- NavalesiPLonghiniFNeurally adjusted ventilatory assistCurr Opin Crit Care2015211586425486574
- RowleyDDLowsonSMCarusoFJDiaphragmatic electrical activity signaling unmasks asynchrony and improves patient-ventilator interactionRespir Ther200945153
- HeunksLMvan der HoevenJGClinical review: the ABC of weaning failure – a structured approachCrit Care201014624521143773
- MamaryAJKondapaneniSVanceGBGaughanJPMartinUJCrinerGJSurvival in patients receiving prolonged ventilation: factors that influence outcomeClin Med Insights Circ Respir Pulm Med20115172621573034
- WhiteACLong-term mechanical ventilation: management strategiesRespir Care201257688989722663965