Abstract
Background
Patients with COPD have had a lower tendency to quit smoking compared to patients with coronary heart disease (CHD). We wanted to investigate if this is still true in a Norwegian population.
Methods
Our data came from the fifth and sixth Tromsø surveys, which took place in 2001–2002 and 2007–2008. The predictors of smoking cessation were evaluated in a cohort of 4,497 participants who had stated their smoking status in both surveys.
Results
Of the 4,497 subjects in the cohort, 1,150 (25.6%) reported daily smoking in Tromsø 5. In Tromsø 6, 428 had quit (37.2%). A new diagnosis of obstructive lung disease (asthma or COPD) and CHD were both associated with increased quitting rates, 50.6% (P=0.01) and 52.1% (P=0.02), respectively. In multivariable logistic regression analysis with smoking cessation as outcome, the odds ratios (ORs) of a new diagnosis of obstructive lung disease and of CHD were 1.7 (1.1–2.7) and 1.7 (1.0–2.9), respectively. Male sex had an OR of 1.4 (1.1–1.8) compared to women in the multivariable model, whereas the ORs of an educational length of 13–16 years and ≥17 years compared to shorter education were 1.6 (1.1–2.2) and 2.5 (1.5–4.1), respectively.
Conclusion
The general trend of smoking cessation in the population was confirmed. Increased rates of smoking cessation were associated with a new diagnosis of heart or lung disease, and obstructive lung disease was just as strongly linked to smoking cessation as was CHD. This should encourage the pursuit of early diagnosis of COPD.
Background
Smoking cessation is crucial for a better prognosis in patients with coronary heart disease (CHD)Citation1–Citation3 and COPD.Citation2,Citation4,Citation5 Acute heart attacks are associated with high smoking cessation rates. In patients with a first myocardial infarction (MI) in the 1970s,Citation3 among whom 78% were smoking, the quitting rate was 55%. In a systematic review from 2003, the mean rate of smoking cessation within a year after a new diagnosis of CHD was found to be 45%.Citation1 A lower quitting rate was observed in patients with COPD, in particular in subjects not participating in smoking cessation programs. Among smoking COPD patients in a Swedish study, 10% of those receiving usual care had stopped smoking after 3 years, compared to 38% of those who took part in smoking cessation groups.Citation6 Among hospitalized patients with respiratory and cardiac diseases who took part in an intensive smoking cessation program in Singapore, 60% of the cardiac patients and 40% of the respiratory patients were still abstinent from smoking after 2 months.Citation7
The mortality due to CHD has decreased considerably in the Western world in the last few decades.Citation8 Evidence shows that decreased smoking prevalence in the general population, particularly among patients with heart disease, is an important reason for this decrease.Citation8–Citation11 The mortality due to COPD has decreased less.Citation12 A stronger tendency of persistent smoking among COPD patients may partly explain this difference.
COPD patients’ reluctance to quit smoking may lead to a feeling of hopelessness among the doctors who treat them.Citation13 Our aim was to determine how the quitting rate in adults is influenced by getting a diagnosis of obstructive lung disease in the population-based Tromsø study. We also wanted to investigate whether influence from this life event differs from being diagnosed with CHD.
Methods
Subjects
A large proportion of the adult population in Tromsø has participated in health surveys (the Tromsø study) since 1974. Tromsø is a university city in northern Norway with ~72,600 inhabitants. The Tromsø study so far consists of six surveys, and this study deals with subjects who participated in both Tromsø 5 (2001–2002) and Tromsø 6 (2007–2008). The attendance rates (of those invited) in Tromsø 5 and Tromsø 6 were 79% and 66%, respectively. Details of the participants have previously been described.Citation14 We included participants who answered the questions on smoking in both surveys. No smoking cessation support was offered during the surveys.
The Regional committee for Medical and Health Research Ethics and the Norwegian Data Inspectorate approved the Tromsø 5 and Tromsø 6 surveys with a license for further analysis on non-identifiable data, like this study. All the participants gave written informed consent.
Examinations
In both surveys, the invitation included a questionnaire with questions on smoking habits, education, and diseases. We classified subjects reporting daily smoking in Tromsø 5, but not in Tromsø 6, as quitters. We divided length of education into three categories, ≤12 years, 13–16 years, and ≥17 years. shows the reported diseases. For each disease in the questionnaire the participants were asked whether they have or have had the disease in question. We classified diseases reported in Tromsø 6 and not in Tromsø 5 as new diagnoses. We categorized MI and angina pectoris as “CHD” and asthma and COPD as “obstructive lung disease”.
Table 1 Daily smoking according to characteristics of the cohort of 4,497 participants in Tromsø 5 (2001–2002) who also took part in Tromsø 6 (2007–2008)
Statistical analysis
The frequencies of current smoking at baseline (in Tromsø 5) and smoking cessation among smokers were calculated by subject characteristics, and the statistical differences between subgroups were analyzed by chi-square statistics. We analyzed predictors of smoking cessation by binary logistic regression. Significant variables in univariable analysis (P<0.1), as well as age and sex, were entered in the multivariable analysis. For the statistical analyses, we used the IBM SPSS statistic, Version 21 (IBM Corporation, Armonk, NY, USA).
Results
A total of 4,631 subjects participated in both the fifth and the sixth surveys of the Tromsø study, and 4,497 subjects comprising 1,852 men and 2,645 women answered the questions on smoking in both surveys. The mean time difference between attending the two surveys was 6.2 years (standard deviation 0.5 years). The mean age at Tromsø 5 was 61.1 years (range 30–81 years); 1,150 (25.6%) reported daily smoking and 1,753 (39.0%) reported former smoking. The highest prevalence of smoking (43.8%) was found in subjects with self-reported COPD, whereas the frequency among those with self-reported CHD was 19.0%. The characteristics of the population in Tromsø 5 and the respective frequencies of smoking are listed in .
In the sixth survey, 765 subjects (17.0%) reported current smoking, and 428 of the 1,150 who had been smoking in Tromsø 5 had quit (37.2%). A significantly higher quitting rate was found in men compared to women, and the quitting rate increased with the length of education. Self-reported diseases registered in Tromsø 5 had no significant impact on the quitting rate (). The number of days between attending the two surveys had no impact on the quitting rate (odds ratio =1, P=0.8).
Table 2 Smoking cessation between 2001–2002 (Tromsø 5) and 2007–2008 (Tromsø 6) according to characteristics of 1,150 smoking participants in Tromsø 5
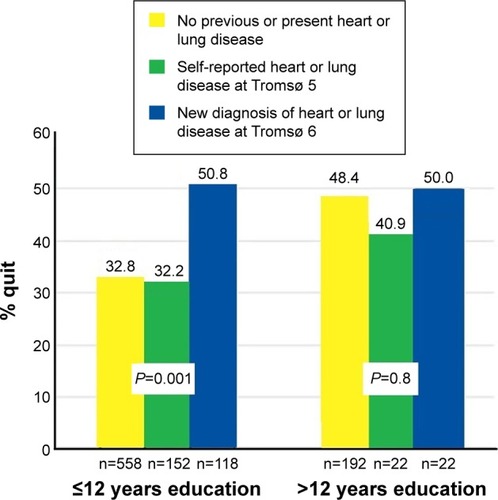
shows the frequencies of new self-reported diseases reported in Tromsø 6, but not in Tromsø 5, and the association between a new diagnosis and smoking cessation. New diagnoses of asthma/COPD (n=79) and CHD (n=73) were both associated with increased frequency of quitting, 50.6% (P=0.01) and 52.1% (P=0.008), respectively. A new diagnosis of asthma/COPD or CHD was reported in 144 subjects. Both men and women belonging to any of these diagnostic groups showed increased quitting rates, 54.9% vs 39.8% (P=0.02) in men and 47.1% vs 32.7% (P=0.009) in women. The impact of getting these new diagnoses was particularly strong among the subjects with education length no longer than 12 years (P=0.001; ). Subjects with education length up to 12 years were also more frequently diagnosed with these diseases compared to those with higher education, 16.0% and 9.5% (P=0.01), respectively. Among subjects with higher education, a high quitting rate was independent of a new diagnosis ().
Table 3 Smoking cessation between 2001–2002 (Tromsø 5) and 2007–2008 (Tromsø 6) according to new diagnosis in the same period
Figure 1 Percentage of participants who quit smoking between 2001–2002 (Tromsø 5) and 2007–2008 (Tromsø 6) among 1,064 participants, by education length, and heart and lung disease.
A new diagnosis of both CHD and obstructive lung disease was significantly associated with smoking cessation when analyzed by logistic regression and also after adjusting for sex and education level in multivariable logistic regression analyses ().
Table 4 ORs for smoking cessation between Tromsø 5 (2001–2002) and Tromsø 6 (2007–2008) according to characteristics of 1,024 smoking participants in Tromsø 5 and new diagnosis reported in Tromsø 6
Discussion
Main findings
Half of the participants with a new diagnosis of asthma/COPD or angina/MI quit smoking during the 6 years of follow-up. However, the association between these new diagnoses and smoking cessation was found only in participants with education length up to 12 years. The much higher smoking rate among those with asthma and, in particular, those with COPD at baseline than in those with CHD indicates a shift in attitude toward smoking cessation among subjects with COPD.
Strengths and limitations
The high number of participants and the high attendance rates among those invited are strengths of the study. The prevalences of daily smoking among all the attendees in Tromsø 5 and Tromsø 6 were 31% and 22%, respectively,Citation11 which are close to the national prevalences of 29% and 21%, as registered by Statistics Norway (https://www.ssb.no)Citation15 in 2002 and 2008, respectively. In our study sample, the prevalence was lower at both points of time, 25.6% and 17.0%, respectively, and a healthy survivor effect may have contributed to the low frequency of daily smoking in our subsample. The study is based on questionnaires and not on objective measurements of smoking, such as cotinine and thiocyanate. In a previous Norwegian study, self-reported smoking was strongly related to serum thiocyanate if the question was asked in a neutral setting.Citation16 Although the questions on smoking were included in a self-administered questionnaire, underreporting of daily smoking among those with a new diagnosis cannot be ruled out.
All diagnoses were self-reported, and their correctness could not be confirmed. Shift in diagnosis based on the same illness from Tromsø 5 to Tromsø 6, for instance, between asthma and COPD, may have taken place in some subjects. Such a change has been counted as a new diagnosis. This is no longer a problem when asthma and COPD are combined into one category (asthma and/or COPD) and subjects with a new diagnosis of any of these diseases are compared with those with neither of the diagnoses at both Tromsø 5 and Tromsø 6.
Although we have found associations between a new diagnosis and smoking cessation, we do not know for sure whether the extra cessations in the subgroups with a new diagnosis were really preceded by a new diagnosis. Subjects in these subgroups could have stopped smoking before the diagnosis was given. In these cases, it is likely that symptoms from a pulmonary or heart disease had raised their awareness of the risk of continued smoking.
Comparisons with previous studies
No previous study has, to our knowledge, described smoking cessation in relation to a new diagnosis of heart or lung disease. Most previous studies evaluated smoking cessation programs, and control groups in such studies can be compared with our participants. However, the quitting rate of 41.7% among subjects with a COPD diagnosis reported in Tromsø 5 was more similar to the rate of 38% among the COPD patients, who had taken part in the smoking cessation program in a Swedish study, than the rate of 10% among the COPD patients on usual care.Citation6 In a study from primary care, where smokers received smoking cessation advice and were followed up annually with spirometry, higher rates of abstinence were found among those with COPD than among those with normal lung function.Citation17 This result is in line with our findings. We found that the quitting rate increased with increasing length of education, and this association is well known from previous studies.Citation18
Qualitative studies have shown that patients with a COPD diagnosis may have several reasons for not quitting despite the knowledge of harming themselves,Citation19 and they do not always believe that quitting would give them a better life.Citation20 COPD patients often show little interest in receiving help from medication and describe unassisted quitting as the best method to stop smoking, based on willpower, strong motivation, and internal strength.Citation21 In our study, a new diagnosis of COPD or CHD might have given many participants the motivation they needed to quit without assistance. In another qualitative study, the interviewees who had stopped smoking emphasized that persons close to them had a strong influence on their decision to quit.Citation22 This gives a reason to believe that the decreasing acceptance of smoking in the society also influences COPD patients.
Conclusion
It has been suggested that a hard core of smokers will constitute an increasing proportion of COPD patients who still smoke.Citation23 The high quitting rates among subjects with both an established and a new diagnosis of COPD in our study contradicts this pessimism. The study supports pursuit of early diagnosis of COPD and gives reasons for a more optimistic attitude among health workers when they discuss smoking cessation with their COPD patients.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
The authors would like to thank the participants of the Tromsø study.
Disclosure
The authors report no conflicts of interest in this work.
References
- CritchleyJACapewellSMortality risk reduction associated with smoking cessation in patients with coronary heart disease: a systematic reviewJAMA20032901869712837716
- ThunMJCarterBDFeskanichD50-year trends in smoking-related mortality in the United StatesN Engl J Med2013368435136423343064
- AbergABergstrandRJohanssonSCessation of smoking after myocardial infarction. Effects on mortality after 10 yearsBr Heart J19834954164226838729
- AnthonisenNRConnettJEMurrayRPSmoking and lung function of Lung Health Study participants after 11 yearsAm J Respir Crit Care Med2002166567567912204864
- AnthonisenNRSkeansMAWiseRAThe effects of a smoking cessation intervention on 14.5-year mortality: a randomized clinical trialAnn Intern Med2005142423323915710956
- SundbladBMLarssonKNathellLHigh rate of smoking abstinence in COPD patients: smoking cessation by hospitalizationNicotine Tob Res200810588389018569763
- OngKCCheongGNPrabhakaranLEarnestAPredictors of success in smoking cessation among hospitalized patientsRespirology2005101636915691240
- DalenJEAlpertJSGoldbergRJWeinsteinRSThe epidemic of the 20(th) century: coronary heart diseaseAm J Med2014127980781224811552
- AspelundTGudnasonVMagnusdottirBTAnalysing the large decline in coronary heart disease mortality in the Icelandic population aged 25–74 between the years 1981 and 2006PLoS One2010511e1395721103050
- YoungFCapewellSFordESCritchleyJACoronary mortality declines in the U.S. between 1980 and 2000 quantifying the contributions from primary and secondary preventionAm J Prev Med201039322823420709254
- MannsverkJWilsgaardTMathiesenEBTrends in modifiable risk factors are associated with declining incidence of hospitalized and nonhospitalized acute coronary heart disease in a populationCirculation20161331748126582781
- BurneyPGPatelJNewsonRMinelliCNaghaviMGlobal and regional trends in COPD mortality, 1990–2010Eur Respir J20154551239124725837037
- RisorMBSpigtMIversenRThe complexity of managing COPD exacerbations: a grounded theory study of European general practiceBMJ Open2013312e003861
- VoldMLAaseboUMelbyeHLow FEV1, smoking history, and obesity are factors associated with oxygen saturation decrease in an adult population cohortInt J Chron Obstruct Pulmon Dis201491225123325364242
- Statistics Norway Available from: https://www.ssb.no/en/helse/statistikker/roykAccessed May 31, 2016
- FossOPHaugKHeslaPELund-LarsenPGVasliLRKan vi stole på egenerklærte røykevaner? [Can we rely on self-reported smoking habits?]Tidsskr Nor Laegeforen199811814216521689656812
- StratelisGMolstadSJakobssonPZetterstromOThe impact of repeated spirometry and smoking cessation advice on smokers with mild COPDScand J Prim Health Care200624313313916923621
- GorenAAnnunziataKSchnollRASuayaJASmoking cessation and attempted cessation among adults in the United StatesPLoS One201493e9301424676348
- EklundBMNilssonSHedmanLLindbergIWhy do smokers diagnosed with COPD not quit smoking? – a qualitative studyTob Induc Dis20121011723088811
- van EerdEARisørMBvan RossemCRvan SchayckOCKotzDExperiences of tobacco smoking and quitting in smokers with and without chronic obstructive pulmonary disease-a qualitative analysisBMC Fam Pract201516116426537703
- MorphettKPartridgeBGartnerCWhy don’t smokers want help to quit? A qualitative study of smokers’ attitudes towards assisted vs unassisted quittingInt J Environ Res Public Health20151266591660726068089
- MedboAMelbyeHRudebeckCEI did not intend to stop. I just could not stand cigarettes any more.” A qualitative interview study of smoking cessation among the elderlyBMC Fam Pract2011124221627833
- EmerySGilpinEAAkeCFarkasAJPierceJPCharacterizing and identifying “hard-core” smokers: implications for further reducing smoking prevalenceAm J Public Health200090338739410705856
