Abstract
The respiratory diaphragm is the most important muscle for breathing. It contributes to various processes such as expectoration, vomiting, swallowing, urination, and defecation. It facilitates the venous and lymphatic return and helps viscera located above and below the diaphragm to work properly. Its activity is fundamental in the maintenance of posture and body position changes. It can affect the pain perception and emotional state. Many authors reported on diaphragmatic training by using special instruments, whereas only a few studies focused on manual therapy approaches. To the knowledge of the authors, the existing scientific literature does not exhaustively examines the manual evaluation of the diaphragm in its different portions. A complete evaluation of the diaphragm is mandatory for several professional subjects, such as physiotherapists, osteopaths, and chiropractors not only to elaborate a treatment strategy but also to obtain information on the validity of the training performed on the patient. This article aims to describe a strategy of manual evaluation of the diaphragm, with particular attention to anatomical fundamentals, in order to stimulate further research on this less explored field.
Introduction
Breathing is a systemic act, involving the whole body, the viscera, the nervous system, and emotions. The diaphragm muscle is the main breathing muscle, influencing with its contractions the respiratory activity.Citation1 The diaphragm collaborates to various processes such as expectoration, vomiting, swallowing, urination, and defecation.Citation1 It facilitates the venous and lymphatic return and helps the viscera above and below the diaphragm to work properly.Citation1 Diaphragm’s activity is fundamental in the maintenance of posture and body position changes and influences the pain perception, usually decreased during the inspiratory apnoea.Citation1,Citation2 Diaphragmatic movements also change the body pressure, as it facilitates the venous and lymphatic return.Citation2 This pressure modulation influences the blood redistribution, which could be probably correlated with the response of baroreceptors and the reduction of pain perception, although there are not scientific studies supporting this hypothesis yet.Citation2
The most important stimulus for the respiratory acts is provided by chemoreceptors, whose task is to maintain the biochemical balance of the body.Citation2 Breathing is also influenced by internal and external conditions, with other ways of neural stimulation beyond the chemoreceptorial stimulation.Citation2 The diaphragmatic activity is not only controlled by metabolic mechanism but also by emotional states such as sadness, fear, anxiety, and anger.Citation2 Breathing stimulates mechanoreceptors of the diaphragm and the visceroceptors of viscera (moving during the respiratory acts), constituting the mechanism of interoception.Citation2 Interoception is the awareness of the body condition obtained from information coming directly from the body itself.Citation2 Diaphragmatic movements also stimulate the skin and the mediastinum; this complex of afferent information determines the central representation of breathing.Citation2 The amygdala, which is part of the limbic system, is reciprocally connected to each of the respiratory areas, just as the medulla oblongata, and is considered the most important area that manages emotive breathing.Citation2 A respiratory disorder certainly alters the emotional framework, such as depression and anxiety, as well as the emotional state can negatively affect the respiratory activity.Citation2
In case of systemic disease, the diaphragm is always involved, negatively contributing to the set of symptoms. In chronic heart failure, the diaphragm is weaker, more commonly placed in expiratory state, with more frequent movements.Citation3,Citation4
The pathological changes are seen in patients with chronic obstructive pulmonary disease (COPD).Citation5
The progressive limitation of the airflow in COPD patients causes a pathological adaptation of the diaphragm, although the reasons for these changes are not fully clear. These changes in position adversely affect the exercise tolerance; more in detail, the dome of the diaphragm is lowered, in inspiratory position.Citation6 The contractile force is decreased, with electrical and metabolic alterations. The muscle thickness is increased, especially on the left side, with decreased mechanical excursion, probably due to fibers’ shortening.Citation7,Citation8 A decrease of anaerobic type fibers (type II) and an increase in aerobic fibers (type I) are observed; this process progressively increases with the pathology worsening.Citation8 The increase in the oxidative process, however, does not correspond to an improvement of the diaphragmatic function. The rate of detectable myosin decreases, resulting in altered sarcomeric organization and further decreasing of the contractile strength.Citation8 The phrenic activity is abnormal, presumably due to the nerve stretching caused by the chronic lowering of the diaphragm, resulting in such a neuropathy.Citation9 The exercise intolerance in patients with congestive heart failure and COPD does not correlate with the common functional indexes (ejection frequency and forced expiratory volume in 1 second); rather it is the peripheral muscle adaptation, including that of the diaphragm, to have a heavy influence on the symptomatic scenario.Citation10,Citation11
As mentioned in the article, the diaphragm influences the patient’s emotional state. In patients with COPD, the incidence of depression varies from 8% to 80%, according to different studies.Citation12 Depression may be considered a predictor of mortality during hospitalization for acute respiratory events.Citation13 Depression and anxiety negatively affect the rehospitalization, but only 33% of patients are treated with a pharmacological process taking into account these psychiatric symptoms.Citation13 Depression affects the physical status of the patient, as demonstrated by some authors who observed a worsening in the test of Cooper (12 minutes run) and an increased mortality rate.Citation13 Anyway, there are not enough data exhaustively explaining this correlation.Citation13 The copresence of depression and anxiety in patients with COPD increases the mortality rate (of 83% according to some authors).Citation14,Citation15 The incidence of depression/anxiety increases with COPD worsening.Citation12,Citation15 Even in this case, the exact mechanisms leading to this correlation are unclear; probably the presence of dyspnea, systemic inflammation, and the effects on the brain system derived from the smoking cessation are involved.Citation12 Anyway, improving respiratory function improves psychiatric symptoms, with exercise and manual therapy.Citation12,Citation16
To the knowledge of the authors, the existing scientific literature does not exhaustively examines the manual evaluation of the diaphragm in its different portions. A complete evaluation of the diaphragm is mandatory for several professional subjects, such as physiotherapists, osteopaths, and chiropractors not only to elaborate a treatment strategy but also to obtain information on the validity of the training performed on the patient. This article aims to describe a hypothesis of manual evaluation of the diaphragm, with particular attention to anatomical fundamentals, in order to stimulate further research on this less explored field.
Anatomy of the diaphragm: origin and insertion
An accurate knowledge of the anatomy of diaphragm is necessary in order to perform a proper manual evaluation of the muscle, with particular focus on hands’ positioning.
According to its insertions, the diaphragm can be divided in costal, lumbar, and sternal portions. The sternal part arises with two small fiber bundles from the posterior aspect of the xiphoid process, near to the apex; the costal (or lateral) portion arises from the inner and superior aspect of the last six ribs, with interdigitation with the transverse muscle of the abdomen.Citation17 The lumbar portions arises from the medial, intermediate, and lateral ligaments of the diaphragm. The medial ligaments, before reaching the vertebral bodies, delimitate with their internal muscular bundles, at the level of D11, the esophageal hiatus for the passage of the esophagus and vagus nerves. The right medial ligament, thicker and longer than the left one, terminates in a flattened tendon on the anterior aspect of L2–L3 (sometimes up to L4).Citation17 Laterally to the right ligament, there is a small ligament (called accessory or intermediate), whose tendon is inserted at the level of L1–L2. Between this ligament and the right medial one, there is a vertical split crossed by the large splanchnic nerve and the medial root of the azygos vein.Citation17 The left medial ligament ends with a flattened tendon between L2 and L3; even in this case an accessory ligament is present, forming a split for the large splanchnic nerve and the medial root of hemiazygos vein.Citation17 The tendons of these two ligaments constitute, at the level of D12, a tendinous arch (called the median arcuate ligament), through which the aorta and the thoracic duct cross the diaphragm.Citation17 The lateral ligaments arise in the form of two thick tendons at the level of the arch of the psoas muscle, constituting the medial arcuate ligament; the latter passes above the psoas muscle, joining the vertebral body of L1 and its transverse apophyses, and more laterally, above the quadrates lumborum muscle, joining the transverse process of L1 and the apex of the 12° rib, forming the lateral arcuate ligament.Citation17
The respiratory diaphragm muscle is innervated by the phrenic nerve (C3–C5) and the vagus nerve (cranial nerve X); the first receives pulses from groups of medullary neurons of the pre-Bötzinger complex and from neurons of the parafacial retrotrapezoid complex (correlated in turn with the retroambiguus nucleus of the medulla); however, it is worth to mention that these connections are still unclear.Citation17 The vagus nerve is part of the parasympathetic autonomic system, originating from the ambiguus nucleus of the medulla.Citation17
The normal position of the diaphragm can be seen in the chest X-ray. On the anterior–posterior projection, the dome of the right hemidiaphragm is located at the level of 5°–6° rib for what regard the anterior part, whereas the posterior one usually lies at the level of the 10° rib.Citation18 The left hemidiaphragm is slightly higher (about one intercostal space).Citation13 In 10% of people, both domes have the same height, becoming difficult to be differentiated in the lateral projection.Citation18 Computed tomography and magnetic resonance imaging are also useful in the morphological evaluation of the diaphragm, even though they are used in second analysis, due to their costs and availability.Citation18 Fluoroscopy and ultrasounds are techniques employed for the real-time evaluation of the moving diaphragm, even though affected by visibility limitations.Citation18 In most cases, the diaphragm shows a symmetrical respiratory excursion of ~2–10 cm, not related to the vital capacity of the lungs.Citation18 The ribs open out laterally in caudal direction during inspiration, and the opposite during expiration.Citation1 By aging, the diaphragm becomes thinner and more frequently located in expiratory position, especially in males.Citation19
Physiotherapy and diaphragm
In literature, there are many physiotherapeutic approaches based on diaphragm’s adaptability. The resistance training in anaerobic regimen, or other training programs in aerobic regimen, with different devices, can be used with increased diaphragm performance in patients affected by respiratory diseases.Citation20,Citation21
The respiratory rehabilitation improves the diaphragmatic motion in both sides (using fluoroscopy imaging) in COPD patients and improves the performance, structural, and metabolic characteristics of the respiratory muscle (muscle strength [PI {max}, cm H2O]), endurance (inspiratory threshold loading, kPa), exercise capacity (Borg scale for respiratory effort, modified Borg scale, work rate maximum, W), dyspnea (transition dyspnea index).Citation20–Citation22
Several tools such as bikes or cycle ergometers for the upper limbs, or breathing stimulators (with different resistances to be overcome during the inspiration), are usually employed.Citation23 Diaphragm training (with the aim to improve lung capacity) is also used in other pathologic scenarios, such as in patients who have undergone sternotomy for cardiac surgery, and in patients affected by stroke.Citation24,Citation25 Diaphragm training also improves other symptoms, such as those cause by gastroesophageal reflux, and improves muscle proprioception of the lumbar–sacral region.Citation26,Citation27
Currently, the literature shows that there are no significant differences in the rehabilitation results of the physical therapy in patients with COPD, in terms of comparison between the use of endurance and resistance training.Citation28–Citation30
Manual therapy and diaphragm
A few studies examined the manual evaluation of the diaphragm; although a review of the literature was not among the aims of this paper, some short texts on the topic need to be mentioned.
Potential therapeutic approaches involving the diaphragm muscle have been proposed among gentle myofascial release techniques, in the context of the therapeutic techniques addressed to other diaphragms of the human body.Citation3,Citation31 The myofascial technique is the application of a low load, long duration, stretch into the myofascial complex, with the aim to restore the optimal length of this complex.Citation32 The operator palpates the fascial restriction and the pressure is applied directly to the skin, into the direction of the restriction, until resistance (the tissue barrier) is manually perceived.Citation32 Once found, the collagenous barrier is engaged for a few minutes, without sliding over the skin or forcing the tissue, until the band starts to yield the complex and a sensation of softening is achieved.Citation32
Other types of manual (osteopathic) techniques employ myofascial approaches, in particular by placing the hands under the chondrocostal junctions, inducing and facilitating respiratory acts.Citation33,Citation34 The same techniques are also used in other fields, such as to improve the symptoms of gastroesophageal reflux, and to alleviate somatic symptoms in pregnant women.Citation35,Citation36
There are several studies evaluating the effects of the manual therapy in COPD. The approach to the patient varies widely, both in terms of techniques and time management: thoracic spinal mobilization, lymphatic drainage or pump, diaphragmatic release trigger points, massage, articulation techniques for ribs, myofascial release to the thoracic outlet, suboccipital decompression, and muscular stretching.Citation16,Citation37,Citation38 The results of the various respiratory parameters are always positive, but we have not enough information to draw definitive conclusions.
Only recently, physiotherapy and manual therapy have been used together in the treatment of patients with COPD. A previous study aims to assess the effect of these two therapeutic strategies, showing that the combination of rehabilitation and osteopathy led to better results in comparison with the single approach (increase in forced expiratory volume in 1 second, 6-minute walk test, decrease in residual volume).Citation39
A recent study on COPD patients shows that many parameters (mobility, exercise capacity, maximal respiratory pressure, and vital capacity) are improved by working the anterior chondrocostal arch with manual diaphragm release technique.Citation40
We need to find the correct technique to manually evaluate the diaphragm, in order to improve the complementary use of the usual rehabilitation and manual therapy.
Proposal of a manual evaluation technique for the diaphragm muscle
The technique for the manual evaluation of the diaphragm proposed in the present article arises from the growing need to combine physiotherapy with manual therapy, considering the new clinical data.
It is well known that, in patients with COPD or congestive heart failure, the diaphragm has a specific preferred position, which can be measured with different clinical tools. According to a recent study, human touch can distinguish any slight variation, measurable in microns.Citation41
We can strongly speculate on the possibility to train the therapist, in terms of palpation technique, to check the mobility and function of the inspiratory muscle, in order to obtain additional clinical information on the therapeutic approach, before and after the physiotherapy (as usually happens for doctors in osteopathy).Citation42
This manual evaluation is based on the experience of authors, consisting in >20 years of clinical practice with patients affected by respiratory and cardiac diseases; the proposed method for COPD patients obviously need to be deepened with further studies. It is important to remember that, as for many other therapeutic techniques, whether manual or otherwise, scientific proof is not available for every existing treatment, this does not mean that, in absence of scientific evidence, something is not valid; otherwise there would not be new treatments or any improvement in rehabilitative practice.Citation31 In this regard, we wish to recall that the evidence-based medicine, originated in the second half of the 19th century, is based on the individual clinical expertise, best external evidence, patient values, and expectations:
External clinical evidence can inform, but can never replace, individual clinical expertise, and it is this expertise that decides whether the external evidence applies to the individual patient at all and, if so, how it should be integrated into a clinical decision.Citation43
There are no previous papers dealing with a comprehensive evaluation of the diaphragm through manual approach, and a description of techniques to be performed to evaluate this muscle in all its portions is currently missing. We do not have complete data on what happens in the different anatomical areas of the diaphragm in patients with respiratory disease; this text could be used as a guideline for researchers for further evaluation.
The patient is supine, in comfortable position. The first step deals with the assessment of the costal movement; this should consist of lateralization during inspiration, with a caudal direction, and the opposite during expiration.Citation44 In case of dysfunction of the diaphragm, this costal movement is usually limited.Citation45 The hands must be gently hold on the lateral sides of the costal margins, in order to have a palpatory feedback of the costal behavior during breathing ().
Figure 1 The hands must be gently placed on the lateral sides of the costal margins to receive palpation feedback of the costal behavior during breathing.

In the following evaluation, respecting the previously described anatomy, the hands can be hold on the costal margins, anteriorly, with the thumbs being at the margin’s level and the other fingers lying on the upper ribs. Since the diaphragm muscle is lowered during inspiration, and then rises during expiration, this manual position can be used to assess the diaphragmatic excursion ().Citation1,Citation17
Figure 2 The hands can be held anteriorly on the costal margins, with the thumbs being at the level of the margins and the other fingers placed across the upper ribs. This manual position can be used to assess the diaphragmatic excursion.

The following manual positions deal with the evaluation of the various portions of the diaphragm: domes, posterolateral area, xyphocostal area, medial ligament, and lateral ligament.
To evaluate the diaphragmatic domes, the operator’s forearm has to be hold parallel to the abdomen of the patient, with the thenar and hypothenar eminences of the hand at the level of the anterior margin of the costal arch; a gentle push must be performed in cranial direction, so as to record the elastic response of the tissue, for the right side as well as for the left one (). As usually observed in manual tests, the elasticity of the tissue is reduced when a reduced movement is obtained in response to the applied stimulus.Citation42
Figure 3 To evaluate the diaphragmatic domes, the operator’s forearm has to be held parallel to the abdomen of the patient, with the thenar and hypothenar eminences of the hand at the level of the anterior margin of the costal arch; a gentle push must be performed in the cranial direction, so as to record the elastic response of the tissue, for both right and let sides.

To evaluate the posterolateral area, the hand must be hold as previously described for the domes, but with the forearm forming an angle of 45° with the patient’s abdomen; a gentle push must be applied obliquely, following the line of the same forearm (). This step needs to be repeated for the other side also. This portion of the diaphragm shows higher movement excursion during the respiration and has a more vertical inclination in comparison with the domes.Citation18
Figure 4 To evaluate the posterolateral area, the hand must be held as previously described for the domes, but with the forearm forming a 45° angle with the patient’s abdomen; a gentle push must be applied obliquely, following the line of the same forearm.

The evaluation of the xyphoid-costal area is used to assess whether, during inspiration and expiration, there is regular elasticity of the tissue, which is necessary for normal breathing; in fact, this area is usually more rigid in case of abnormal diaphragmatic activity.Citation45 The hand and the forearm are positioned as in the evaluation of the domes, but in the xyphoid area; a gentle push must be applied cranially ().
Figure 5 The evaluation of the xyphoid-costal area is used to assess whether there is regular elasticity of the tissue during inspiration and expiration, which is necessary for normal breathing. The hand and the forearm are positioned as in the evaluation of the domes, but in the xyphoid area; a gentle push must be applied cranially.

For medial ligaments, the spinal elasticity needs to be evaluated, with the patient being supine. The operator hold the last phalanges of the fingers (of one or both hands) placed in the interspinous spaces of D11 and D12; by using a gentle push toward the ceiling, a passive extension of the vertebra is obtained, in order to deduce information on its elasticity ().Citation42 The same technique is used to evaluate the lumbar vertebral bodies up to L4.Citation42 The medial ligaments play an important role in the mechanics of the dorsolumbar region, in synergy with the abdominal wall muscles and the thoracolumbar fascia.Citation1,Citation17,Citation46
Figure 6 For medial ligaments, the spinal elasticity needs to be evaluated, with the patient being supine. The operator should hold the last phalanges of the fingers (of one or both hands) placed in the interspinous spaces of D11 and D12; by using a gentle push towards the ceiling, a passive extension of the vertebra is obtained, in order to deduce information on their elasticity.

The lateral ligaments are evaluated by actively soliciting the last rib. On the opposite side compared to the rib to be evaluated, the body of the rib must be hold with one hand, and a gentle traction must be performed toward the operator (). The lateral ligaments play an important role in managing the tension affecting the diaphragm and the thoracolumbar fascia.Citation17,Citation46
Figure 7 The lateral ligaments are evaluated by actively involving the last rib. On the opposite side of the rib to be evaluated, the body of the rib must be held with one hand, and a gentle traction must be performed toward the operator.

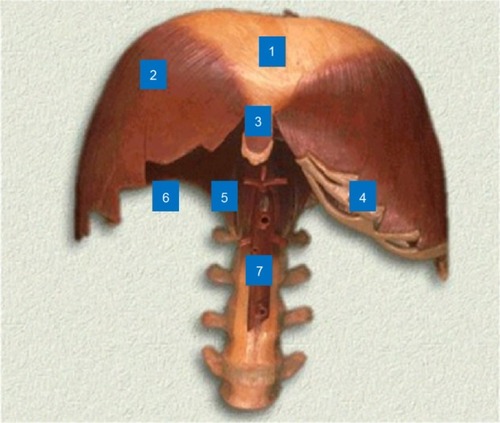
The main purpose of using such manual evaluation is to understand whether there is a restriction of movement in a specific area of the diaphragm muscle, in order to plan a manual treatment focused on the dysfunctional area, combining the manual approach to the usual rehabilitation process (). The combination of several techniques in a multidisciplinary process can be of benefit for the improvement of the respiratory performance.Citation47,Citation48
Figure 8 Anatomical model.
We hope that this article could contribute to the state of the art, representing a starting point, and enhancing the need for further research in this field.
Conclusion
The breath is a systemic activity, able to involve several body parts. The health of the diaphragm muscle is critical for many patients, not just those with respiratory diseases. A proper training of the main respiratory muscle can be of benefit in several clinical scenarios; however, there are not so many authors reporting on therapeutic techniques focused on manual approaches and, more in detail, on the manual evaluation of the diaphragm. This article aims to describe a hypothesis of manual evaluation of the diaphragm, with particular attention to anatomical fundamentals. The technique for the manual evaluation of the diaphragm proposed in the present article arises from the increasing need to combine physiotherapy with manual therapy, considering the new clinical data. We do not have complete knowledge on what happens in the different anatomical areas of the diaphragm in patients with respiratory disease; this text could be used as a guideline for researchers for further evaluation.
Disclosure
The authors report no conflicts of interest in this work.
References
- BordoniBMarelliFFailed back surgery syndrome: review and new hypothesesJ Pain Res20169172226834497
- BordoniBMarelliFBordoniGA review of analgesic and emotive breathing: a multidisciplinary approachJ Multidiscip Healthc201699710227013884
- BordoniBMarelliFThe fascial system and exercise intolerance in patients with chronic heart failure: hypothesis of osteopathic treatmentJ Multidiscip Healthc2015848949426586951
- CaruanaLPetrieMCMcMurrayJJMacFarlaneNGAltered diaphragm position and function in patients with chronic heart failureEur J Heart Fail20013218318711246055
- SalitoCLuoniEAlivertiAAlterations of diaphragm and rib cage morphometry in severe COPD patients by CT analysisConf Proc IEEE Eng Med Biol Soc201520156390639326737755
- HellebrandováLChlumskýJVostatekPNovákDRýznarováZBuncVAirflow limitation is accompanied by diaphragm dysfunctionPhysiol Res Epub2016412
- BariaMRShahgholiLSorensonEJB-mode ultrasound assessment of diaphragm structure and function in patients with COPDChest2014146368068524700122
- OttenheijmCAHeunksLMDekhuijzenPNDiaphragm muscle fiber dysfunction in chronic obstructive pulmonary disease: toward a pathophysiological conceptAm J Respir Crit Care Med2007175121233124017413128
- El-TantawiGAImamMHMorsiTSPhrenic nerve conduction abnormalities correlate with diaphragmatic descent in chronic obstructive pulmonary diseaseCOPD201512551652425774441
- VogiatzisIZakynthinosSThe physiological basis of rehabilitation in chronic heart and lung diseaseJ Appl Physiol (1985)20131151162123620491
- EvansRASinghSJCollierRLokeISteinerMCMorganMDGeneric, symptom based, exercise rehabilitation; integrating patients with COPD and heart failureRespir Med2010104101473148120650624
- SmithMCWrobelJPEpidemiology and clinical impact of major comorbidities in patients with COPDInt J Chron Obstruct Pulmon Dis2014987188825210449
- PoolerABeechRExamining the relationship between anxiety and depression and exacerbations of COPD which result in hospital admission: a systematic reviewInt J Chron Obstruct Pulmon Dis2014931533024729698
- SmithSMSonegoSKetchesonLLarsonJLA review of the effectiveness of psychological interventions used for anxiety and depression in chronic obstructive pulmonary diseaseBMJ Open Respir Res201411e000042
- AtlantisEFaheyPCochraneBSmithSBidirectional associations between clinically relevant depression or anxiety and COPD: a systematic review and meta-analysisChest2013144376677723429910
- WearingJBeaumontSForbesDBrownBEngelRThe use of spinal manipulative therapy in the management of chronic obstructive pulmonary disease: a systematic reviewJ Altern Complement Med201622210811426700633
- BordoniBZanierEAnatomic connections of the diaphragm: influence of respiration on the body systemJ Multidiscip Healthc2013628129123940419
- RobertsHCImaging the diaphragmThorac Surg Clin200919443145020112626
- SuwatanapongchedTGieradaDSSloneRMPilgramTKTuteurPGVariation in diaphragm position and shape in adults with normal pulmonary functionChest200312362019202712796184
- ChunEMHanSJModiHNAnalysis of diaphragmatic movement before and after pulmonary rehabilitation using fluoroscopy imaging in patients with COPDInt J Chron Obstruct Pulmon Dis20151019319925670895
- MillsDEJohnsonMABarnettYASmithWHSharpeGRThe effects of inspiratory muscle training in older adultsMed Sci Sports Exerc201547469169725116085
- GeddesELReidWDCroweJO’BrienKBrooksDInspiratory muscle training in adults with chronic obstructive pulmonary disease: a systematic reviewRespir Med200599111440145815894478
- GeddesELO’BrienKReidWDBrooksDCroweJInspiratory muscle training in adults with chronic obstructive pulmonary disease: an update of a systematic reviewRespir Med2008102121715172918708282
- KodricMTrevisanRTorregianiCInspiratory muscle training for diaphragm dysfunction after cardiac surgeryJ Thorac Cardiovasc Surg2013145381982322938776
- JungJHKimNSThe effect of progressive high-intensity inspiratory muscle training and fixed high-intensity inspiratory muscle training on the asymmetry of diaphragm thickness in stroke patientsJ Phys Ther Sci201527103267326926644689
- Nobre e SouzaMÂLimaMJMartinsGBInspiratory muscle training improves antireflux barrier in GERD patientsAm J Physiol Gastrointest Liver Physiol201330511G862G86724113771
- JanssensLMcConnellAKPijnenburgMInspiratory muscle training affects proprioceptive use and low back painMed Sci Sports Exerc2015471121924870567
- IepsenUWJørgensenKJRingbaekTHansenHSkrubbeltrangCLangePA systematic review of resistance training versus endurance training in COPDJ Cardiopulm Rehabil Prev201535316317225692720
- AlisonJAMcKeoughZJPulmonary rehabilitation for COPD: are programs with minimal exercise equipment effective?J Thorac Dis20146111606161425478201
- EmtnerMWadellKEffects of exercise training in patients with chronic obstructive pulmonary disease – a narrative review for FYSS (Swedish Physical Activity Exercise Prescription Book)Br J Sports Med201650636837126823440
- BordoniBZanierEThe continuity of the body: hypothesis of treatment of the five diaphragmsJ Altern Complement Med201521423724225775273
- BordoniBZanierEUnderstanding fibroblasts in order to comprehend the osteopathic treatment of the fasciaEvid Based Complement Alternat Med2015201586093426357524
- YaoSHassaniJGagneMGeorgeGGilliarWOsteopathic manipulative treatment as a useful adjunctive tool for pneumoniaJ Vis Exp201487e50687
- ValenzaMCCabrera-MartosITorres-SánchezIGarcés-GarcíaAMateos-TosetSValenza-DemetGThe effects of doming of the diaphragm in subjects with short-hamstring syndrome: a randomized controlled trialJ Sport Rehabil201524434234826115420
- DinizLRNesiJCuriACMartinsWQualitative evaluation of osteopathic manipulative therapy in a patient with gastroesophageal reflux disease: a brief reportJ Am Osteopath Assoc2014114318018824567271
- LavelleJMOsteopathic manipulative treatment in pregnant womenJ Am Osteopath Assoc2012112634334622707643
- NollDRJohnsonJCBaerRWSniderEJThe immediate effect of individual manipulation techniques on pulmonary function measures in persons with chronic obstructive pulmonary diseaseOsteopath Med Prim Care20093919814829
- HeneghanNRAdabPBalanosGMJordanREManual therapy for chronic obstructive airways disease: a systematic review of current evidenceMan Ther201217650751822703901
- ZanottiEBerardinelliPBizzarriCOsteopathic manipulative treatment effectiveness in severe chronic obstructive pulmonary disease: a pilot studyComplement Ther Med2012201–2162222305244
- RochaTSouzaHBrandãoDCThe manual diaphragm release technique improves diaphragmatic mobility, inspiratory capacity and exercise capacity in people with chronic obstructive pulmonary disease: a randomised trialJ Physiother201561418218926386894
- BordoniBZanierESutherland’s legacy in the new millennium: the osteopathic cranial model and modern osteopathyAdv Mind Body Med2015292152125831430
- ChilaAGFoundations for Osteopathic Medicine3rd edPhiladelphia, PALippincott Williams & Wilkins2010
- MasicIMiokovicMMuhamedagicBEvidence based medicine – new approaches and challengesActa Inform Med200816421922524109156
- VostatekPNovákDRychnovskýTRychnovskáSDiaphragm postural function analysis using magnetic resonance imagingPLoS One201383e5672423516397
- ChaitowLBradleyDGilbertCRecognizing and Treating Breathing Disorders. A Multidisciplinary Approach2nd edLondonChurchill Livingstone2013
- VleemingASchuenkeMDDanneelsLWillardFHThe functional coupling of the deep abdominal and paraspinal muscles: the effects of simulated paraspinal muscle contraction on force transfer to the middle and posterior layer of the thoracolumbar fasciaJ Anat2014225444746225139243
- EngelRMVemulpadSRBeathKShort-term effects of a course of manual therapy and exercise in people with moderate chronic obstructive pulmonary disease: a preliminary clinical trialJ Manipulative Physiol Ther201336849049624053900
- EngelRVemulpadSThe role of spinal manipulation, soft-tissue therapy, and exercise in chronic obstructive pulmonary disease: a review of the literature and proposal of an anatomical explanationJ Altern Complement Med201117979780121838523
