Abstract
Purpose
Anemia is reported to be an independent predictor of hospitalizations and survival in COPD. However, little is known of its impact on short-term survival during severe COPD exacerbations. The primary objective of this study was to determine whether the presence of anemia increases the risk of death in acute respiratory failure due to severe COPD exacerbations.
Patients and methods
Consecutive patients with COPD exacerbation who were admitted to the intensive care unit with the diagnosis of acute respiratory failure and required either invasive or noninvasive ventilation (NIV) were analyzed.
Results
A total of 106 patients (78.3% male; median age 71 years) were included in the study; of them 22 (20.8%) needed invasive ventilation immediately and 84 (79.2%) were treated with NIV. NIV failure was observed in 38 patients. Anemia was present in 50% of patients, and 39 patients (36.8%) died during hospital stay. When compared to nonanemic patients, hospital mortality was significantly higher in the anemic group (20.8% vs 52.8%, respectively; P=0.001). Stepwise multivariate logistic regression analysis showed that presence of anemia and NIV failure were independent predictors of hospital mortality with odds ratios (95% confidence interval) of 3.99 ([1.39–11.40]; P=0.010) and 2.56 ([1.60–4.09]; P<0.001), respectively. Anemia was not associated with long-term survival in this cohort.
Conclusion
Anemia may be a risk factor for hospital death in severe COPD exacerbations requiring mechanical ventilatory support.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
COPD is a major cause of health burden throughout the world.Citation1 COPD often coexists with comorbidities such as cardiovascular diseases, osteoporosis, skeletal muscle dysfunction, depression, and anemia.Citation2,Citation3 The common ground for most of these extrapulmonary problems is the ongoing severe inflammation. Comorbidities have an influence on potentiating the overall morbidity of COPD, leading to increased hospitalizations, health care costs, and eventually death.
Anemia is a well-known comorbidity of COPD with a prevalence ranging from 12.3 to 23%.Citation3–Citation5 Previous studies also showed that the prevalence is much higher during exacerbations.Citation6–Citation8 Anemia in COPD is directly associated with adverse clinical outcomes, including death. Hemoglobin levels correlated with dyspnea scores, exercise capacity, and several inflammatory markers in COPD.Citation9–Citation12 Anemia has also been shown as an independent predictor of recurrent hospitalizations and survival in COPD patients with chronic respiratory failure.Citation13,Citation14
It has been suggested that low hemoglobin levels may impair gas exchange and cardiorespiratory interaction in COPD patients.Citation4,Citation11 This effect is expected to be more prominent in severe COPD exacerbations presenting with acute respiratory failure in which the oxygen demand is supposed to be high due to increased respiratory workload. In this study, we sought to identify whether anemia is related with higher in-hospital deaths in severe COPD exacerbations. Secondary end points were to evaluate the impact of anemia on noninvasive ventilation (NIV) failure and long-term survival.
Patients and methods
Study population
This cohort study was conducted in a 14-bed medical intensive care unit (ICU) of a tertiary reference hospital. The ethics committee of Dışkapı Yıldırım Beyazıt Education and Research Hospital approved the study (approval number: 10/29). Written informed consent was obtained to be included in this study from either the patient him/herself or patient’s relatives. All consecutive COPD exacerbation patients who developed acute respiratory failure were evaluated between April 2012 and September 2015. Diagnosis of COPD was confirmed, according to the Global initiative for chronic Obstructive Lung Disease (GOLD), from medical records, and if available pulmonary function tests (PFTs) within the previous year.Citation1 In patients for whom PFTs were unavailable, COPD diagnosis was confirmed with GOLD clinical criteria (age >40 years, >10 pack-year smoking or biomass history).
The exclusion criteria were as follows: 1) suspected alternative/additional cause for respiratory failure such as pneumonia, pulmonary embolism, cardiogenic pulmonary edema, severe sepsis, acute respiratory distress syndrome, 2) presence of active bleeding, 3) presence of a disease/treatment possibly associated with bone marrow suppression (renal failure with glomerular filtration rate <30 mL/min/1.73 m2, malignancy, hematologic disorders), and 4) recent operation or transfusion history.
Demographic characteristics (age, sex, smoking history), recent PFTs – if available, presence of comorbidities, use of long-term oxygen therapy and domiciliary NIV, duration of hospital stay prior to ICU admission, severity scores of Acute Physiology and Chronic Health Evaluation (APACHE) II and Glasgow Coma Scale (GCS) were recorded.
Laboratory data for admission arterial blood gas analysis, complete blood cell count, and serum CRP were collected. Anemia was defined as hemoglobin levels <12 gm/dL for female patients and <13 gm/dL for male patients according to the World Health Organization (WHO) anemia definition.Citation15
Data collection for mechanical ventilation and follow-up
All patients had acute respiratory failure due to an exacerbation and were supported by either invasive (mechanical ventilation with endotracheal intubation) ventilation or NIV according to the degree of respiratory failure and the patient’s clinical condition. NIV was performed by experienced ICU staff using pressure support mode through an oronasal mask. NIV failure was defined as requiring endotracheal intubation at any time.
Initial mechanical ventilation support type, failure in NIV, total duration of mechanical ventilation support, the lengths of ICU and hospital stays, and ICU and hospital mortality were recorded. For survivors, mortality was evaluated from the national death database system on January 31, 2016.
Statistical analysis
The primary outcome of the study was whether the presence of anemia on admission is a risk factor for hospital mortality in severe COPD exacerbations. Secondary outcomes were the effect of anemia on NIV failure and long-term survival. The sample size (n=106) was calculated assuming an alpha error of 5% to reject the null hypothesis with a statistical power of 80% and anticipating 5% dropout rate.Citation16
All categorical variables are expressed as numbers and percentages, and continuous variables were expressed as median and interquartile range. Categorical variables between groups were compared with chi-square or Fisher’s exact test, continuous variables were compared with Mann–Whitney U-test. The independent effect of anemia on hospital mortality was assessed with stepwise multivariate logistic regression analysis. To build the model, a purposeful selection method was used to select a subset of covariates that were considered to be clinically important, adjusting for confounders and statistical significance. An adjusted odds ratio (OR) and a 95% confidence interval (CI) were reported for each independent factor. A two-tailed P-value of <0.05 was considered statistically significant. Statistical analysis was performed with SPSS (Statistical Package for the Social Sciences Version 20; IBM Corporation, Armonk, NY, USA) program.
Results
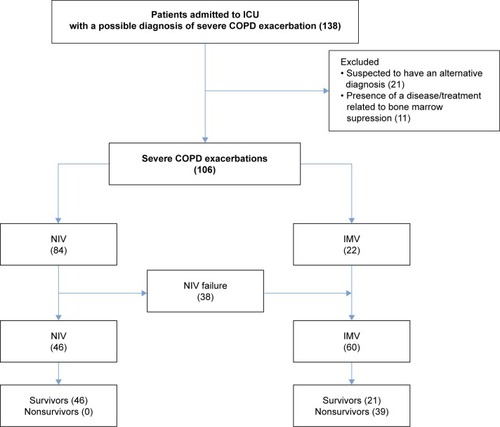
Study flowchart is presented in . A total of 124 patients were screened and 106 patients (78.3% male; median age 71 years) were included in the study. Patient characteristics are shown in . PFTs were available in 62 patients; the median (interquartile range) forced expiratory volume in 1 second (FEV1) % predicted was 31.4% (20.5%–40.2%). Thirty-seven (34.9%) patients were using long-term oxygen therapy and 15 (14.2%) patients were using NIV at home. Hypertension and coronary artery disease were the most common comorbidities. Twelve patients had a respiratory arrest event before ICU admission. On ICU admission, the median APACHE II and GCS scores were 23.0 (18.0–31.0) and 15.0 (8.0–15.0), respectively.
Table 1 General characteristics of study population
Figure 1 Study flowchart and hospital outcomes of the study population.
Mechanical ventilation support and NIV failure
Admission arterial blood gas analysis showed patients had hypercapnic respiratory failure. The median pH and arterial partial pressure of CO2 were 7.26 (7.18–7.31) and 75.8 (62.7–85.1) mmHg, respectively (). Twenty-two patients had invasive mechanical ventilation at the time of ICU admission, whereas 84 patients were first treated with NIV. During follow-up, NIV failure was observed in 38 patients with a median duration of 2.5 (0.3–10.0) days. The statistically significant factors between NIV successful and failed patients are shown in . There was no difference for mechanical ventilation duration between both groups (P=0.917). Hospital mortality was 65.8% in the NIV failed group whereas there were no deaths in the NIV successful group.
Table 2 Clinical characteristics of study population
Table 3 Statistically significant differences between noninvasive ventilation successful and failed patients (n=84)
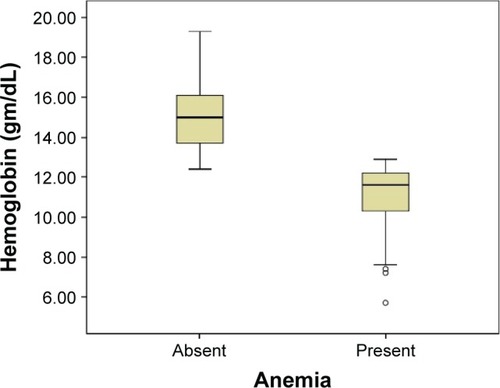
Hemoglobin levels and presence of anemia
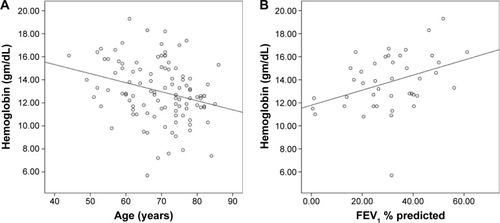
The median hemoglobin level was 12.8 (11.6–15.0) gm/dL in the whole study population. Only one patient had polycythemia (hemoglobin >18.5 gm/dL). Hemoglobin levels were negatively correlated with age (r=−0.293, P=0.002) and positively correlated with FEV1 % predicted (r=0.388, P=0.011) (). Anemia was present in half of the patients (n=53) and there was no difference between sex groups (49.4% [41/83] of male and 52.2% [12/23] of female patients were anemic; P=1.00). The median hemoglobin level in the anemic group was 11.6 (10.2–12.3) gm/dL whereas it was 15.0 (13.7–16.1) gm/dL in the nonanemic group (). Mean corpuscular volume did not differ between anemic and nonanemic patients (86.4 [79.9–91.4] and 88.7 [84.6–91.8] fL, respectively, P=0.245). Anemic patients were older, had lower FEV1 % predicted, and had higher APACHE II score (). NIV failure was observed more in the anemic patients when compared to the nonanemic group (49% vs 22.6%, respectively; P=0.001).
Table 4 Statistically significant differences between anemic and nonanemic patients
Figure 2 Correlations between hemoglobin concentration and age and FEV1% predicted.
Notes: (A) The correlation between hemoglobin and age (Spearman’s correlation coefficient: −0.293; P=0.002). (B) The correlation between hemoglobin and FEV1 % predicted (n=62; Spearman’s correlation coefficient: 0.388; P=0.011).
Abbreviation: FEV1, forced expiratory volume in 1 second.
Short-term mortality
Thirty-nine patients (36.8%) died during hospital stay (). When compared, nonsurvivors had higher APACHE II and lower GCS scores, had more domiciliary NIV use, and low serum ALB. Hospital mortality was 52.8% in the anemic group, whereas it was 20.8% in the nonanemic group (P=0.001). Logistic regression analysis for hospital mortality (), showed presence of anemia and NIV failure were independent predictors of hospital death with ORs (95% CI) of 3.99 ([1.39–11.40]; P=0.010) and 2.56 ([1.60–4.09]; P<0.001), respectively. When hemoglobin levels (continuous variable) were used instead of anemia (categorical variable) in the regression model, OR for hospital mortality was 0.74 (0.59–0.94; P=0.014).
Table 5 Statistically significant factors related with hospital mortality
Table 6 Stepwise multivariate logistic regression analysis for independent predictors of hospital mortality
Long-term mortality
Sixty-seven patients were discharged from hospital. Median follow-up time was 314 (47–773) days. During this period, 26 patients died. Overall mortality was 38.7% (n=41) for 28 days, 50.9% (n=54) for 3 months, and 61.3% (n=65) for 1 year. Hemoglobin levels did not differ between survivors and nonsurvivors (P=0.903).
Discussion
Anemia of chronic disease is relatively common and an important factor in the natural history of COPD. In this study, the presence of anemia was associated with increased hospital mortality in severe COPD exacerbations requiring mechanical ventilation support.
Anemia as a comorbidity in COPD
Anemia is a comorbidity of severe COPD and responsible for increased disease burden.Citation3–Citation6 Anemic patients experience more dyspnea and have decreased functional capacity which in turn results in deterioration in the quality of life.Citation9–Citation11 Additionally these patients exacerbate more and have higher risk of death than nonanemic patients.Citation6,Citation17,Citation18 It is also reported to be an independent negative predictor of the duration of hospitalizations and survival of COPD patients receiving oxygen therapy.Citation14
The prevalence of anemia is approximately 33%–44% in patients hospitalized for an exacerbation.Citation7,Citation8,Citation19 In the present study, anemia was detected in 50% of patients with exacerbations. This result is relatively higher than previously reported, possibly because the study population comprised patients with more severe COPD. We have also found that hemoglobin levels were correlated with FEV1 % predicted and anemic patients had lower FEV1 than nonanemic patients which is consistent with previously reported data.Citation10,Citation14
Anemia and short-term prognosis in severe COPD exacerbations
Although the impact of anemia during stable phase of COPD was reported in many longitudinal cohort studies, the effect of anemia on clinical outcomes for COPD exacerbations, particularly in the ICU setting, was studied less.Citation20–Citation23 In this study, the presence of anemia is associated with an increased risk of death in severe COPD exacerbations with an OR of 3.99. We propose anemia should be considered as a risk stratification factor for severe COPD exacerbations in the ICU.
Anemia has been shown to be associated with increased mortality in COPD-related acute respiratory failure.Citation8,Citation20–Citation23 Rasmussen et alCitation22 evaluated COPD patients who needed invasive ventilation and found that 54.8% of anemic COPD patients died within 30 days with a mortality risk ratio of 3.1 (95% CI 1.6–5.9). Another study reported that hemoglobin level was an independent predictor of hospital mortality (OR: 0.63, 95% CI: 0.45–0.90; P=0.006).Citation23 The impact of anemia on COPD exacerbations was also evaluated in the emergency room setting; a multicenter study performed in Canada showed anemia (hemoglobin <10 gm/dL) was the strongest predictor (OR 4.9; 95% CI 2.1–11.7) of serious adverse events including death in patients admitted to the emergency room.Citation24 All these data suggest that, besides being an important predictor of long-term survival, anemia should also be considered as a risk factor for short-term mortality in severe COPD exacerbations.
The mechanisms of the development of anemia in COPD are complex and outside the scope of this article, nevertheless disease severity seems to be one of the most important factors.Citation25 Anemia was proposed as a marker for end-stage COPD.Citation22 COPD is a systemic inflammatory disease in which many cytokines, including IL-1, IL-6, and TNF-alpha, play a role. These cytokines are also involved in inhibition of erythropoiesis at different steps of the erythropoietic pathway. In the presence of severe systemic inflammation, impairment of erythropoiesis becomes evident as anemia of chronic inflammation.Citation5,Citation25 In addition to chronic changes in the erythropoiesis, acute changes in hemoglobin levels were also reported during exacerbations. Markoulaki et alCitation26 showed that a severe exacerbation itself caused transient changes in hemoglobin levels with a median decrease of 1.3 gm/dL. There was a negative correlation between hemoglobin and erythropoietin (EPO) levels which points out increased EPO resistance during exacerbations. It is already known that EPO resistance is directly correlated with the levels of inflammatory cytokines and therefore the level of systemic inflammation. Repeated exacerbations could further inhibit erythropoiesis, and as a result a significant decrease in hemoglobin levels can occur in severe COPD. Thus, anemia could be accepted as a surrogate of severe systemic inflammation and might be helpful in identifying sicker patients.
Additionally, another important mechanism responsible for the development of anemia of chronic disease is the alteration in iron metabolism.Citation5,Citation7,Citation27 Increased levels of inflammatory cytokines and hepcidin, a peptide hormone that regulates iron homeostasis, also play a significant role in impaired iron utilization which causes functional iron deficiency. It has been shown that functional iron deficiency, even before the onset of anemia, is related to hypoxemia, more frequent self-reported exacerbations, decreased exercise tolerance, and limited response to pulmonary rehabilitation.Citation27,Citation28 Recently, it was suggested that specific attention should be paid to iron deficiency even in the absence of anemia, and iron supplementation may be helpful in anemic COPD patients.Citation29 Researches performed in other chronic inflammatory diseases and one study done in COPD with renal impairment have shown improvement in patient outcomes with iron replacement.Citation7,Citation30 However, more data are needed to understand the importance of functional iron deficiency in COPD and the beneficial effect of iron replacement needs to be confirmed with randomized controlled trials.
On the other hand, COPD patients might be more sensitive to anemia than we think. This hypothesis is supported by the data from two previous studies. COPD patients were reported to have higher a mortality rate during gastrointestinal bleeding when compared to non-COPD patients.Citation31 In the second study, low hematocrit levels were associated with worse outcomes in COPD patients after elective open abdominal aortic aneurysmectomy.Citation32 The reason for this negative effect of anemia on outcomes is still unknown. However, from the physiological point of view, anemia causes a decrease in oxygen transport capacity of blood which could impair physiological and clinical parameters in COPD.Citation4 Yuruk et al showed that low hemoglobin levels were associated with impaired tissue oxygen saturation in the microcirculation, and hemoglobin correction resulted in improvement in oxygen carrying capacity and tissue oxygen saturation.Citation33,Citation34 The negative effect of low hemoglobin levels on tissue oxygenation might be clinically important in severe COPD, especially during exacerbations.
The current study also showed NIV failure is more common in anemic COPD patients. Haja Mydin et alCitation8 looked for prognostic factors in hypercapnic respiratory failure and showed that anemia was related to increased risk of NIV failure. A COPD database study (n=132,424) showed anemic patients had not only more ICU admissions but also needed more ventilatory support.Citation35 Anemia was also reported as a risk factor for extubation and weaning failure.Citation36,Citation37 Depending on its severity, anemia is associated with increased work of breathing and reduced exercise tolerance in COPD.Citation4,Citation9,Citation11 It has been shown that the relationship between muscle oxygenation and peak oxygen consumption varies widely in COPD, and oxygen consumption is highly influenced by blood oxygenation and oxygen utilization level.Citation4,Citation38 Anemic COPD patients also exhibit decreased diffusing capacity corrected for hemoglobin.Citation19 All these changes in oxygen transport lead to decrease in aerobic capacity and therefore skeletal muscle dysfunction in severe COPD during exercise. One can expect these changes to be more evident in patients with low hemoglobin levels, especially during exacerbations because of increased oxygen demand due to increased work of breathing and impaired cardiopulmonary interactions. A case series study done by Schönhofer et alCitation39 showed transfusion decreases minute ventilation and work of breathing in anemic COPD patients. The same group also showed that transfusion helped successful weaning from ventilator in five patients.Citation40 However, the relationship between anemia and ventilation is complex and more data are needed to understand the consequences of anemia on gas exchange and transport during “pump failure” in COPD.
The optimum threshold for hemoglobin in COPD patients is still being debated. Usually a hemoglobin level of >10 gm/dL is considered as a “safe” zone, however this may not be true for COPD patients. The ANTADIR study showed every 5% increase in hematocrit level was associated a relative risk of 0.86 (0.83–0.89) for 3-year mortality.Citation14 Kollert et alCitation13 proposed hemoglobin values greater than 14.3 gm/dL for females and 15.1 gm/dL for males, which are much higher than WHO’s definition, were associated with better outcomes in patients with chronic respiratory failure. Although hemoglobin levels between 7–9 gm/dL are considered as tolerated well in the ICU setting, Rasmussen et alCitation22 reported a cutoff value of hemoglobin level <12 gm/dL was related to increased risk of death in intubated COPD patients. Interestingly, Stiell et alCitation24 showed that patients with exacerbations who ended up with a serious adverse event (including ICU admission, need for mechanical ventilation, and death within 30 days) had hemoglobin levels of 12.3 gm/dL which could be considered as normal. In regard to these findings, the “safe” hemoglobin level for COPD is probably higher than our standard anemia definitions.
Anemia and long-term prognosis in severe COPD exacerbations
Studies done in COPD with chronic respiratory failure have shown the presence of anemia was associated with worse long-term survival, however, we were not able to show such an effect in our cohort.Citation13,Citation14,Citation18 It should be kept in mind that the current study was designed and powered for the primary outcome (hospital mortality). Another important point to consider is study subjects had acute respiratory failure and only one third of the patients had chronic respiratory failure and were using oxygen at home. Finally, the follow-up period might have been too short to see a difference. When compared to previous reports, our median follow-up time was relatively shorter (36 vs 10.5 months, respectively).Citation13
Limitations and strengths of the study
This study has several important limitations. First, it is a single-center study and the results may not be generalizable to other centers. Second, all patients did not have recent PFTs; therefore, we were unable to assess disease severity according to the GOLD classification system in the whole cohort. Third, mortality in the critically ill patients may potentially have been influenced by many confounding factors. Although we have attempted to include a wide range of all possible confounders in the mortality analysis, there is still a lack of data on therapy and complications during ICU stay. Another important point to consider is the etiology of anemia, including data for previous exacerbations and hospitalizations, was not evaluated in this study.
Besides these limitations, the present study has some important strengths. There is limited data about the impact of anemia on severe COPD exacerbations requiring mechanical ventilatory support. Most of the studies done in the ICU setting included not only patients with exacerbations but also patients with other diagnoses such as pneumonia and cardiogenic pulmonary edema.Citation20–Citation23 We were meticulous to include only patients with exacerbations. Moreover, the study cohort consisted of patients with different degrees of acute respiratory failure treated with both NIV and invasive ventilation; therefore, our results might apply to a greater percentage of patients for prediction of prognosis. Finally, comorbidities such as congestive heart failure are known to have an increased risk of death in the presence of anemia. For this reason, instead of using a comorbidity index, each comorbidity was assessed separately in order to understand its own relationship with anemia and mortality.
Conclusion
This study highlights two important results: first, anemia is related with increased risk of death in acute respiratory failure due to severe COPD exacerbations. Second, anemia is associated with NIV failure. Further studies are needed to understand the physiological consequences of anemia in COPD exacerbations and its impact on clinical outcomes. Whether correction of anemia has beneficial effects in COPD is another challenging research question waiting to be answered.
Acknowledgments
The authors would like to thank Gül Ergör and William Vollmer for their valuable comments and contributions to statistical analysis. We also thank American Thoracic Society and Sonia Buist for Methods in Epidemiologic Clinical and Operations Research (MECOR) program for their encouragement and continuous education for research. This study was presented as an oral presentation at the European Respiratory Society Annual Congress 2015, Amsterdam, Holland.
Disclosure
The authors report no conflicts of interest in this work.
References
- Global Initiative for Chronic Obstructive Lung Disease (GOLD) [homepage on the Internet]Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease [updated 2015] Available from: www.goldcopd.orgAccessed June 16, 2016
- ChatilaWMThomashowBMMinaiOACrinerGJMakeBJComorbidities in chronic obstructive pulmonary diseaseProc Am Thorac Soc20085454955518453370
- CavaillesABrinchault-RabinGDixmierAComorbidities in COPDEur Respir Rev20132213045447524293462
- SimilowskiTAgustiAMacNeeWSchönhoferBThe potential impact of anaemia of chronic disease in COPDEur Respir J200627239039616452598
- YohannesAMErshlerWBAnemia in COPD: A systematic review of the prevalence, quality of life, and mortalityRespir Care201156564465221276321
- Martinez-RiveraCPortilloKMunoz-FerrerAAnemia is a mortality predictor in hospitalized patients for COPD exacerbationCOPD20129324325022360381
- SilverbergDSMorRWeuMTSchwartzDSchwartzIFCherninGAnemia and iron deficiency in COPD patients: prevalence and the effects of correction of the anemia with erythropoiesis stimulating agents and intravenous ironBMC Pulm Med2014142424564844
- Haja MydinHMurphySClagueHSridharanKTaylorIKAnemia and performance status as prognostic markers in acute hypercapnic respiratory failure due to chronic obstructive pulmonary diseaseInt J Chron Obstruct Pulmon Dis2013815115723658480
- CoteCZilberbergMDModySHDordellyLJCelliBHaemoglobin level and its clinical impact in a cohort of patients with COPDEur Respir J200729992392917251227
- FerrariMManeaLAntonKAnemia and hemoglobin serum levels are associated with exercise capacity and quality of life in chronic obstructive pulmonary diseaseBMC Pulm Med2015155825952923
- BoutouAKStanopoulosIPitsiouGGAnemia of chronic disease in chronic obstructive pulmonary disease: a case control study of cardiopulmonary exercise responsesRespiration201182323724521576921
- BoutouAKPitsiouGGStanopoulosIKontakiotisTKyriazisGArgyropoulouPLevels of inflammatory mediators in chronic obstructive pulmonary disease patients with anemia of chronic disease: A case-control studyQJM2012105765766322355163
- KollertFTippeltAMüllerCHemoglobin levels above anemia thresholds are maximally predictive for long term survival in COPD with chronic respiratory failureRespir Care20135871204121223232736
- ChambellanAChailleuxESimilowskiTANTADIR Observatory GroupPrognostic value of the hematocrit in patients with severe COPD receiving long-term oxygen therapyChest200512831201120816162707
- World Health OrganizationHaemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information SystemGenevaWorld Health Organization2011 Available from: http://www.who.int/vmnis/indicators/haemoglobin.pdfAccessed June 4, 2016
- DeanAGSullivanKMSoeMMOpenEpi: Open Source Epidemiologic Statistics for Public Health, Version [updated May 4, 2015] Available from: www.OpenEpi.comAccessed June 16, 2016
- OzyılmazEKokturkNTeksutGTatliciogluTUnsuspected risk factors of frequent exacerbations requiring hospital admission in chronic obstructive pulmonary diseaseInt J Clin Pract201367769169723758448
- BoutouAKKarrarSHopkinsonNSPolkeyMIAnemia and survival in chronic obstructive pulmonary disease: a dichotomous rather than continuous variableRespiration201385212613122759351
- GuoJZhengCXiaoQImpact of anaemia on lung functions and exercise capacity in patient with severe chronic obstructive pulmonary diseaseBMJ Open2015510e008295
- AsmundssonTKilburnKHSurvival of acute respiratory failure. 145 patients observed 5 to 8 and one-half yearsAnn Intern Med197480154574810350
- NevinsMLEpsteinSKPredictors of outcome for patients with COPD requiring invasive mechanical ventilationChest200111961840184911399713
- RasmussenLChristensenSLenler-PetersenPJohnsenSPAnemia and 90-day mortality in COPD patients requiring invasive mechanical ventilationClin Epidemiol201031521326654
- UcgunIMetintasMMoralHAlatasFYildirimHErginelSPredictors of hospital outcome and intubation in COPD patients admitted to the respiratory ICU for acute hypercapnic respiratory failureRespir Med20061001667415890508
- StiellIGClementCMAaronSDClinical characteristics associated with adverse events in patients with exacerbation of chronic obstructive pulmonary disease: a prospective cohort studyCMAJ20141866E193E20424549125
- PortilloKMartinez RiveraCRuiz-ManzanoJAnaemia in chronic obstructive pulmonary disease. Does it really matter?Int J Clin Pract201367655856523679907
- MarkoulakiDKostikasKPapatheodorouGHemoglobin, erythropoietin and systemic inflammation in exacerbations of chronic obstructive pulmonary diseaseEur J Intern Med201122110310721238904
- NickolAHFriseMCChengHYA cross-sectional study of the prevalence and associations of iron deficiency in a cohort of patients with chronic obstructive pulmonary diseaseBMJ Open201557e007911
- Barberan-GarciaARodriguezDABlancoINon-anaemic iron deficiency impairs response to pulmonary rehabilitation in COPDRespirology20152071089109526148453
- VasquezALogomarsinoJVAnemia in chronic obstructive pulmonary disease and the potential role of iron deficiencyCOPD201613110010926418826
- AvniTLeiboviciLLGafter-GvilliAIron supplementation for the treatment of chronic heart failure and iron deficiency: systematic review and meta-analysisEur J Heart Fail201214442342922348897
- CappellMSNadlerSCIncreased mortality of acute upper gastrointestinal bleeding in patients with chronic obstructive pulmonary disease. A case controlled multiyear study of 53 consecutive patientsDig Dis Sci19954022562627851186
- UpchurchGRJrProctorMCHenkePKPredictors of severe morbidity and death after elective abdominal aortic aneurysmectomy in patients with chronic obstructive pulmonary diseaseJ Vasc Surg200337359459912618698
- YurukKBartelsSAMilsteinDMBezemerRBiemondBJInceCRed blood cell transfusions and tissue oxygenation in anemic hematology outpatientsTransfusion201252364164621883269
- YürükKAlmacEBezemerRGoedhartPde MolBInceCBlood transfusions recruit the microcirculation during cardiac surgeryTransfusion201151596196721133930
- HalpernMTZilberbergMDSchmierJKLauECShorrAFAnemia, costs and mortality in chronic obstructive pulmonary diseaseCost Eff Resour Alloc200641717042950
- KhamieesMRajuPDeGirolamoAAmoateng-AdjepongYManthousCAPredictors of extubation outcome in patients who have successfully completed a spontaneous breathing trialChest200112041262127011591570
- LaiYCRuanSYHuangCTKuoPHYuCJHemoglobin levels and weaning outcome of mechanical ventilation in difficult to wean patients: A retrospective cohort studyPLoS One201388e7374324015310
- TabiraKHorieJFujiiHThe relationship between skeletal muscle oxygenation and systemic oxygen uptake during exercise in subjects with COPD: a preliminary studyRespir Care20125711602161022417907
- SchönhoferBWenzelMGeibelMKöhlerDBlood transfusion and lung function in chronically anemic patients with severe chronic obstructive pulmonary diseaseCrit Care Med19982611182418289824074
- SchönhoferBBöhrerHKöhlerDBlood transfusion facilitating difficult weaning from the ventilatorAnaesthesia19985321811849534644