Abstract
Purpose
Chest physiotherapy is an important tool in the treatment of COPD. Intrapulmonary percussive ventilation (IPV) and high-frequency chest wall oscillation (HFCWO) are techniques designed to create a global percussion of the lung which removes secretions and probably clears the peripheral bronchial tree. We tested the hypothesis that adding IPV or HFCWO to the best pharmacological therapy (PT) may provide additional clinical benefit over chest physiotherapy in patients with severe COPD.
Methods
Sixty patients were randomized into three groups (20 patients in each group): IPV group (treated with PT and IPV), PT group with (treated with PT and HFCWO), and control group (treated with PT alone). Primary outcome measures included results on the dyspnea scale (modified Medical Research Council) and Breathlessness, Cough, and Sputum scale (BCSS), as well as an evaluation of daily life activity (COPD Assessment Test [CAT]). Secondary outcome measures were pulmonary function testing, arterial blood gas analysis, and hematological examinations. Moreover, sputum cell counts were performed at the beginning and at the end of the study.
Results
Patients in both the IPV group and the HFCWO group showed a significant improvement in the tests of dyspnea and daily life activity evaluations (modified Medical Research Council scale, BCSS, and CAT) compared to the control group, as well as in pulmonary function tests (forced vital capacity, forced expiratory volume in 1 second, forced expiratory volume in 1 second/forced vital capacity%, total lung capacity, residual volume, diffusing lung capacity monoxide, maximal inspiratory pressure, maximal expiratory pressure) and arterial blood gas values. However, in the group comparison analysis for the same variables between IPV group and HFCWO group, we observed a significant improvement in the IPV group maximal inspiratory pressure, maximal expiratory pressure, BCSS, and CAT. Similar results were observed in changes of sputum cytology with reduction of inflammatory cells (neutrophils and macrophages).
Conclusion
The two techniques improved daily life activities and lung function in patients with severe COPD. IPV demonstrated a significantly greater effectiveness in improving some pulmonary function tests linked to the small bronchial airways obstruction and respiratory muscle strength and scores on health status assessment scales (BCSS and CAT) as well as a reduction of sputum inflammatory cells compared with HFCWO.
Introduction
COPD is a lung disease characterized by chronic airflow limitation associated with an enhanced chronic inflammatory response to noxious particles or gases.Citation1 Mucus hypersecretion in COPD has many common causes; some of these include cigarette smoke, acute and chronic viral infection, bacterial infection, and/or inflammatory cell activation of mucin gene transcription.Citation2 The overproduction of mucus and the hypersecretion from increased degranulation is mediated by neutrophil elastase.Citation3 Moreover, there is a difficulty in clearing secretions because of poor ciliary function, distal airway occlusion, and/or an ineffective cough along with reduced peak expiratory flow. This leads to progressive decline in lung function.Citation1,Citation4 Respiratory chest physiotherapy and assisted mucus-clearing techniques are critically important in COPD patients.Citation5 Postural drainage, assisted cough, active cycle of breathing techniques, autogenic drainage, forced expiratory technique, positive expiratory pressure devices,Citation6 oscillatory positive-expiratory pressure devicesCitation7 and, more recently, high-frequency chest wall oscillation (HFCWO),Citation8 intermittent positive pressure breathing (IPPB),Citation9 intrapulmonary percussive ventilation (IPV),Citation10 and temporary positive expiratory pressureCitation11,Citation12 are the techniques that have been proposed over the years for secretion management. The efficacy of these techniques during acute exacerbation or stable disease remains unclear.Citation13 Osadnik et alCitation13 reviewed twenty-eight studies including 907 participants in a meta-analysis; however, the quality was considered poor due to inadequate blinding and allocation procedure and the results were limited by heterogeneity of outcome measurement and inadequacy of data. The conclusions were that airway clearance techniques are safe for individuals with COPD, but the benefits are less clear. IPV was designed to promote mobilization of bronchial secretions and improve efficiency and distribution of ventilation, providing intrathoracic percussion and vibration and an alternative system for the delivery of the positive pressure to the lungs. HFCWO involves an inflatable jacket that is attached to a pulse generator by hoses that mechanically enable the equipment to perform at variable frequencies (5–25 Hz).Citation14 The generator sends air through the hose, which causes the vest to inflate and deflate rapidly. The vibrations not only separate mucus from the airway walls but also help move it up into the large airways.Citation15 Regarding these two different techniques, we conducted a randomized controlled study aimed at comparing their short-term effects in severe to very severe (Global Initiative for Chronic Obstructive Lung Disease [GOLD] stage 3–4, assessment C–D) COPD patients.
Methods
The study was carried out at the Pulmonary Rehabilitation Center of the Respiratory Diseases Department of General Hospital of Sestri Levante from April 2013 to December 2013 and was approved by Local Ethics Committee. Written informed consent was obtained from all participants and procedures were conducted according to the Declaration of Helsinki. The study was registered with the Chinese Clinical Trial Registry, with the number ChiCTR-TRC-12002133.
Patients
Seventy nine patients with stable severe to very severe COPD admitted to The Rehabilitation outpatient clinic were recruited. Inclusion criteria were as follows: age at least 35 years, presence of chronic bronchitis and airway obstruction on spirometry (GOLD stage 3–4, C–D assessment), bronchial hypersecretion (daily sputum >20 mL for at least 2 consecutive days), and effective cough (peak expiratory cough flow >360 L/min). Exclusion criteria were the following: exacerbation of COPD or hospitalization for COPD within 8 weeks prior to recruitment, history of bronchial asthma, predominant bronchiectasis, presence of tracheostomy, mechanical ventilation, recent pneumothorax, severe abnormalities of sensory, severe cardiac arrhythmias, hemodynamic instability, and chest radiograph changes. The drop-out criteria were the inability to comply to study procedures or the lack of a written informed consent and the occurrence of any of the exclusion criteria.
Protocol
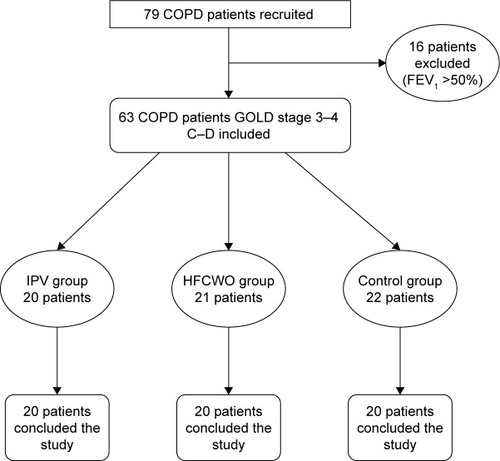
This was a 4-week parallel randomized controlled study comparing IPV, HFCWO, and the best medical therapy. The aim of the study was to verify the effectiveness and the patients’ preference regarding the two methods. Patients who met inclusion criteria were enrolled and randomized into three groups as depicted in the flowchart in . A randomization schedule was generated by an independent statistician using an online random permutation generator from http://www.randomization.com. The randomization assignments were provided to the physicians in sealed envelopes. The investigators who carried out the study data analysis were blinded to patients’ treatment assignment.
Treatments protocols
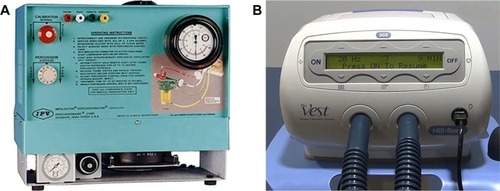
IPV was provided by a respiratory physiotherapist using a percussive ventilator (IPV Impulsator, Percussionaire) (). The impact of calibration (adjustment of inspiratory to expiratory ratio), percussion (frequency of delivered breaths), and source pressure (amplitude/pressure rise of delivered breaths) was adjusted using some suggested setting parameters.Citation10 Each IPV session lasted fifteen minutes and was performed twice a day (morning and afternoon). HFCWO was delivered by a respiratory physiotherapist using a percussive vest (The Vest Airway Clearance System Model 205, Hill-Rom, Batesville, IN, USA) () at 13–15 Hz oscillating frequency, based on patient’s tolerance, and at a pressure setting of 2–5 cm H2O to achieve a tight but comfortable snug fit.Citation14,Citation15 Each HFCWO session lasted 20 minutes and was performed twice a day (morning and afternoon). Subjects for both procedures were kept in a sitting position. The duration of the treatments for each group was 2 weeks. The patients were evaluated one week before the start of airway clearance treatment and one week after the end of the treatment.
Measurements and outcomes
The primary outcomes of the study were the assessment of changes in dyspnea and quality of life as well as daily life activity and healthy status assessment. The secondary outcomes were changes in respiratory function testing, hematological tests, and sputum cell count.
Dyspnea was measured with the Modified Medical Research Council (mMRC) Dyspnea Scale;Citation16 cough and sputum was assessed with the Breathlessness, Cough, and Sputum Scale (BCSS);Citation17,Citation18 daily life activity and healthy status assessment were measured with COPD Assessment Test (CAT).Citation19,Citation20 Pulmonary function testing including forced vital capacity (FVC), forced expiratory volume 1 second (FEV1), FEV1/FVC%, total lung capacity (TLC), residual volume (RV), diffusing lung capacity monoxide (DLCO), maximal inspiratory pressure (MIP), maximal expiratory pressure (MEP), peak cough expiratory flow, and arterial blood gas analysis (Pao2, Paco2, pH) were performed with a computerized body plethysmography (VMAX 20 PFT Sensor Medics, Yorba Linda, CA, USA), according to the ATS/ERS Guidelines.Citation21–Citation23 Inspiratory muscle strength was assessed by measuring the MIP at RV. Expiratory muscle strength was assessed by measuring the MEP at TLC. The value obtained from the best of at least three effort was used. All the measurements were obtained in an upright position.Citation24,Citation25 Diagnosis and severity of COPD were confirmed using the GOLD Guidelines.Citation26
Sputum collection was made on the day the treatment was started and on the day of the last treatment. The patients were instructed by the physiotherapists or by the nurses to expectorate into the sputum cups during the entire duration of the treatment and to continue expectorating if the patient felt the need to cough. Sputum induction was performed using a previously described method. Briefly, the procedure was started 10 minutes after the administration of 200 µg of inhaled salbutamol using a 3% hypertonic saline solution. Sputum samples were processed within 2 hours after the collection.Citation27–Citation29 Sputum samples were considered for analysis if they contained expectorated material with cellular viability greater than 50%, had contamination with oropharyngeal squamous cells at a level lower than 20%, and were of sufficient quantity to enable differential counts of 400 cells.Citation28,Citation29 Finally at the end of treatment, subjects treated with IPV or HFCWO were asked to complete a written questionnaire to rate comfort, effectiveness, ease of use, and convenience of the respective procedures. The answers were given using a 5-point Likert-type scale. The possible responses were extremely =4, very =3, somewhat =2, not very =1, not at all =0.Citation30
Statistical analysis
Clinical data were expressed as counts and mean and SD. We calculated the difference between the two treatments (HFCWO and IPV) and control group using univariate regression analysis. Subsequently, the difference between the two treatments (HFCWO and IPV) was analyzed using univariate regression analysis. In addition, a Wilcoxon test was applied to the patients’ preference rankings. Differences were considered statistically significant when p≤0.05. Data analysis was performed using the statistics software R-Project version 2.13.2.
Results
Sixty-three patients were recruited. Three patients withdrew prior to completing the study. Two patients belonged to the control group and one patient belonged to HFCWO group. Sixty patients completed the study. All patients had similar characteristics. The patient characteristics are given in . No changes in respiratory therapy or COPD exacerbations were observed during the study period.
Table 1 Demographic, clinical, and functional parameters at baseline in the three groups
Primary outcomes
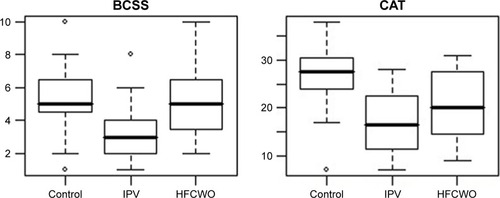
Patients in both the IPV group and the HFCWO group showed a significant improvement in the tests of dyspnea and daily life and health status assessment (mMRC, BCSS, and CAT) compared to those in the control group. Moreover, IPV patients showed an improvement in BCSS (p<0.001) and CAT (p<0.02) scores in comparison with HFCWO. The results are reported in . The box-plots of BCSS and CAT scores are shown in .
Table 2 Results of primary outcomes
Secondary outcomes
Both the techniques improved several parameters in the patient groups compared to control group (white blood cells, neutrophils, and lymphocytes; C-reactive protein; FVC; FEV1; FEV1/FVC%; TLC; RV; RV/TLC%; DLCO; MIP; MEP; PaO2; PaCO2; and pH). However, in the group comparison analysis for the same variables between IPV group and HFCWO group, we observed a significant improvement in the IPV group in TLC and TLC% (p<0.03), RV and RV% (p<0.04), and DLCO, MIP, and MEP (p<0.01). These results are summarized in .
Table 3 Results of secondary outcomes (hematological, biochemical, and respiratory function parameters)
Sputum changes
A significant change in total cell count and neutrophil, lymphocyte, and macrophage counts in sputum samples were observed in the patients receiving either of the two treatments (IPV and HFCWO) compared to control group. Only a slight significant change in neutrophil count was observed in the IPV group compared to HFCWO group (p<0.05). All the results of the sputum cells count measurements are reported in .
Table 4 Changes in sputum cell count
Measurement of patient acceptability
The 40 patients who finished the study (20 in each group) completed the questionnaire and rated the comfort, efficacy, ease of use, and convenience. A similar ranking was expressed by the patients for both the techniques. shows the mean ± SD rating and the ranking.
Table 5 Ratings and ranking of patient preferences for airway clearance techniques
Discussion
Techniques for increasing the normal airway clearance are a vital component of therapy. Mechanisms which can be performed without an assistant or without being dependent on a caregiver provide greater control as well as patient satisfaction and are considered important in many areas of medicine (eg, diabetes). Techniques which can be used in a majority of adolescents and adults with pulmonary disease that lead to an increase in adherence with daily therapy have been developed in the recent years.Citation31 Thus, methods such as the application of positive expiratory pressure and use of flutter valves or high-frequency chest compression vests have been evaluated with good results in cystic fibrosis patients; these techniques have not been well studied in the COPD patient population. There are a few trials that have studied chest physiotherapy or directed coughing techniques in COPD patients. These trials have shown some improvements in mucus clearance, but no changes in lung function.Citation2,Citation32,Citation33 Several studies have been published regarding the two instruments, both in bronchiectasis and cystic fibrosis patients,Citation8,Citation9,Citation30,Citation34–Citation49 or in COPD patients,Citation49–Citation60 but only two studies compared IPV and HFCWO.Citation30,Citation61 In the previously published studies, IPV reduced the incidence of exacerbations,Citation49,Citation53 improved arterial blood gas values,Citation51,Citation53,Citation54,Citation57 reduced diaphragmatic workload,Citation50 and improved dyspnea,Citation34,Citation51 some respiratory functional parameters,Citation34,Citation52,Citation57 and sputum volume.Citation30 HFCWO showed the following findings: improvement of wet weight sputum or greater sputum expectoration,Citation8,Citation40,Citation43 reduction of dyspnea (Borg score),Citation44,Citation59 improvement of healthy scores (CAT and BCSS) and quality of life (St Georges Respiratory Questionnaire),Citation14,Citation60 improvement in ventilation distribution and gas mixing,Citation41 improvement of respiratory function parameters (FVC, and FEV1),Citation8,Citation14,Citation15,Citation41 and changes in sputum cell counts.Citation14 The study by Varekojis et alCitation30 has compared the therapeutic effectiveness and preference of postural drainage and percussion with IPV and HFCWO. Effectiveness was evaluated by measuring the weight of the wet and dry sputum obtained with each method as well as based on the results of preference obtained by using a Likert-type scale. The wet sputum weight differed significantly and was greater in the IPV group. The second study compared IPV and HFCWO in pediatric tracheostomized patients. IPV was more effective than HFCWO in reducing lower respiratory tract infections, steroid and bronchodilator use, as well as the number of hospitalizations.Citation61 Our study has evaluated short-term effects of the two techniques on patients with severe to very severe COPD. We have found a significant improvement in the dyspnea, scores on health status assessment scales, as well as in pulmonary function tests and gas exchange.
Besides, in the group comparison analysis for the same variables between the IPV group and the HFCWO group, a significant improvement in the IPV group in TLC, RV, DLCO, MIP, MEP, BCSS, and CAT was observed. The latter data may suggest that IPV can also act on small bronchial airway obstruction and improve alveolar ventilation. Moreover, the reduction of lung hyperinflation decreases respiratory workload as shown by the reduction of maximal inspiratory and expiratory pressure. Finally, changes in sputum cellularity showed a reduction in the number of inflammatory cells (neutrophils and macrophages) and an increase in the number of lymphocytes as a result of utilization of the two techniques (previously observed for HFCWO)Citation14 and suggests a modulation of inflammatory cells (greater for IPV). This is the first study that has investigated sputum cellularity for COPD patients; further studies need to confirm our findings, particularly concerning its impact on exacerbations.
Limitations
This study has some limitations. It was done in a single center with a relatively modest sample size. We have evaluated only the short-term effects of these techniques; this does not allow us to establish the duration of the effects of the treatment and how many cycles of therapy every patient needs per year.
Moreover, we have not considered the exacerbations; we should have expected a reduction in the number of exacerbations related with the changes in sputum cellularity. Finally, the absence of a sham ventilation therapy group makes our conclusion somewhat less powerful, especially with regard to subjective factors such as dyspnea.
Conclusion
This study shows that both IPV and HFCWO can improve lung function, muscular strength, dyspnea, and scores on health status assessment scales. IPV demonstrated a greater effectiveness in improving test results linked to small bronchial airways and alveolar ventilation (RV and DLCO) and muscular strength (MIP and MEP) as well as scores on daily life and health status assessment scales (BCSS and CAT) compared with HFCWO. These techniques should be considered as additional therapy in patients with severe to very severe COPD.
Acknowledgments
The authors thank Mr Giles Wilson, Sales Manager Percussionaire Corporation for his valuable help in reviewing the manuscript and Dr Sergio Lanata, Histopathology Unit, Hospital of Sestri Levante, for his valuable help in data analysis and collection. The abstract of this manuscript was presented at the Poster session of Chest Annual Meeting, Austin, October 25–30, 2014. The publication was financially supported by a grant from Medigas Italia srl.
Disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. The authors report no conflicts of interest in this work.
References
- MarcoaRRodriguezDMDiasMClassification of Chronic Obstructive Pulmonary Disease (COPD) according to the new Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2017: Comparison with GOLD 2011COPD Epub20171121
- RamosFLKrahnkeJSKimVClinical issue of mucus accumulation in COPDInt J COPD20149139150
- BrightlingCEChronic obstructive pulmonary disease phenotypes, biomarkers and prognostic factorsAllergy Asthma Proc20163743243827931297
- WoodruffPGAgustiARocheNSinghDMartinezFJCurrent concepts in targeting COPD pharmacotherapy: making progress toward personalized managementLancet20153851789179825943943
- BottJBlumenthalSBuxtonMBritish Thoracic Society Physiotherapy guideline development GroupGuidelines for the physiotherapy management of the adult, medical, spontaneously breathing patientsThorax20096415119103870
- Fagevik OlsenMWesterdahlEPositive expiratory pressure in patients with chronic obstructive pulmonary disease. A systematic reviewRespiration20097711011818843173
- SvenningsenSPaulinGASheikhKOscillatory positive expiratory pressure in chronic obstructive pulmonary diseaseCOPD201613667426430763
- PiquetJBrochardLIsabeyDHigh frequency chest wall oscillation in patients with chronic air-flow obstructionAm Rev Respir Dis1987136135513593688638
- NicoliniAMollarEGrecchiBLanducciNComparison of intermittent positive pressure breathing and temporary positive expiratory pressure in patients with severe obstructive pulmonary diseaseArch Bronconeumol201450182424321380
- ToussaintMGuilletMCPaternottSSoudonPHaanJIntrapulmonary effects of setting parameters in portable intrapulmonary percussive ventilation devicesRespir Care20125773574222153619
- VenturelliECrisafulliEDeBiaseAEfficacy of temporary positive expiratory pressure (TPEP) in patients with lung diseases and chronic mucus hypersecretion. The UNIKO® project: a multicentre randomized controlled trialClin Rehabil20132733634622967853
- MascardiVGrecchiBBarlasciniCBanfiPNicoliniAEffectiveness of temporary positive expiratory pressure (T-PEP) at home and at hospital in patients with severe chronic obstructive pulmonary diseaseJ Thor Dis2016828952902
- OsadnikCRMcDonaldCFJonesAPHollandAEAirway clearance techniques for chronic obstructive pulmonary diseaseCochrane Database Syst Rev20123CD008328
- NicoliniACardiniFLanducciNLanataSFerrari-BravoMBarlasciniCEffectiveness of treatment with high-frequency chest wall oscillation in patients with bronchiectasisBMC Pulm Med2013132123556995
- LechtzinNWolfeLFFrickKDThe impact of high-frequency chest wall oscillation on healthcare use in patients with neuromuscular diseasesAnn Am Thorac Soc201613690490926999271
- CazzolaMHananiaMARudellKHackfordCTamimiNA review of the most common patient-reported outcomes in COPD-revisiting current knowledge and estimating challengesInt J COPD201510725738
- LeidyNKRennardSSchmierJJonesKGoldmanMThe breathlessness, cough, and sputum scale. The development of empirically based guidelines for interpretationChest20031242182219114665499
- LeidyNKSchmierJKJonesMKLloydJRocchiccioliKEvaluating symptoms in chronic obstructive pulmonary disease: validation of the Breathlessness, Cough and Sputum ScaleResp Med200397S59S70
- DoddJWHoggLNolanJThe COPD assessment test (CAT): response to pulmonary rehabilitation. A multicentre prospective studyThorax20116642542921398686
- LeeBYLeeSLeeJSValidity and reliability of CAT and Dyspnea-12 in bronchiectasis and tuberculosis destroyed lungTuber Resp Dis201272467474
- MillerMRHankinsonJBrusascoVStandardization of spirometryEur Resp J200526319338
- PellegrinoRViegiGBrusascoVInterpretative strategies for lung function testsEur Resp J200526948968
- MacintyreNCrapoROViegiGStandardization of the single-breath determination of carbon monoxide uptake in the lungEur Resp J200526720735
- American Thoracic Society/European Respiratory SocietyATS/ERS Statement on respiratory muscle testingAm J Resp Crit Care Med2002166528621
- EvansJAWhitelawWAThe assessment of maximal respiratory mouth pressure in adultsRespir Care2009541348135919796415
- VestboJHurdSSAgustiAGGlobal strategies for diagnosis and prediction of chronic pulmonary disease. Gold executive summaryAm J Resp Crit Care Med201318734736522878278
- MoritzPSteidleLJFelisbinoMBKlevestonTPizzichiniMMPizzichiniEDetermination of the inflammatory component of airway diseases by induced sputum cell counts: use in clinical practiceJ Bras Pneumol20083491392119099097
- StaticescuSChereches-PantaPIchimiGValeanuMNanulescuMVThe value of induced sputum in the diagnosis and management of children with bronchial asthmaClujul Med20148717117626528019
- GuptaVSinghDCritical assessment of the value of sputum neutrophilsCOPD20131010711423413897
- VarekojisSMDouceHFluckeRLA comparison of the therapeutic effectiveness of and preference for postural drainage and percussion, intrapulmonary percussive ventilation, and high-frequency chest wall compression in hospitalized cystic fibrosis patientsRespir Care200348242812556258
- PryorJAPhysiotherapy for airway clearance in adultsEur Resp J19991414181424
- WarnockLGatesAvan der SchansCPChest physiotherapy compared to no chest physiotherapy for cystic fibrosisCochrane Database Syst Rev20139CD001401
- van der SchansCPConventional chest physical therapy for obstructive lung diseaseRespir Care2007521198120617716386
- PaneroniMCliniESimonelliCBianchiLDegli AntoniFVitaccaMSafety and efficacy of short-term intrapulmonary percussive ventilation in patients with bronchiectasisRespir Care20115698498821352670
- DmelloDNavakRPMatuschakGMHigh-frequency percussive ventilation for airway clearance in cystic fibrosis: a brief reportLung20103511513
- NewhousePAWhiteFThe intrapulmonary percussive ventilation and flutter device compared to chest physiotherapy in patients with cystic fibrosisClin Pediatr199837427432
- NataleJEPfeifleJHommickDNComparison of intrapulmonary percussive ventilation and chest physiotherapy: a pilot study in patients with cystic fibrosisChest1994105178917938205878
- HomnickDNWhiteFde CastroCComparison of effects of an intrapulmonary percussive ventilator to standard aerosol and chest physiotherapy in treatment of cystic fibrosisPediatr Pulmonol19952050557478782
- Van GinderdeurenFVerbanckSVan CauwelaertKChest physiotherapy in cystic fibrosis: short-term effects of autogenic drainage preceded by wet inhalation of saline versus autogenic drainage preceded by intrapulmonary percussive ventilation with salineRespiration200810015261533
- ArensRGozalDOmlinKJComparison of high frequency chest compression and conventional chest physiotherapy in hospitalized patients with cystic fibrosisAm J Resp Crit Care Med1994150115411577921452
- DarbeeJCKangaJFOhtakePJPhysiologic evidence for high-frequency chest wall oscillation and positive expiratory pressure breathing in hospitalized subjects with cystic fibrosisPhys Ther2005851278128916305267
- PhililipsGEPikeSEJaffe’ABushAComparison of active cycle of breathing and high-frequency oscillation jacket in children with cystic fibrosisPediatr Pulmonol200437717514679493
- KempainenRRMillaCDunitzJComparison of settings used for high-frequency chest-wall compression in cystic fibrosisRespir Care201055669570120507651
- FainardiVLongoFFaverzaniSTripodiMCChettaAPisiGShort-term effects of high-frequency chest compression and positive expiratory pressure in patients with cystic fibrosisJ Clin Med Res20113627928422393338
- OermannCMStrokerMMGilesDSontagMAccursoFJCastileRGComparison of high-frequency chest wall oscillation and oscillating positive expiratory pressure in the home management of cystic fibrosis: a pilot studyPediatr Pulmonol20013237237711596162
- KempainenRRWilliamsCBHazelwoodARubinBKMillaCEComparison of high-frequency chest wall oscillation with differing waveform for airway clearance in cystic fibrosisChest20071321227123217890465
- McllwaineMPAlarieNDavidsonGFLong-term multicentre randomised controlled study of high frequency chest wall oscillation versus positive expiratory pressure mask in cystic fibrosisThorax20136874675123407019
- OsmanLPRoughtonMHodsonMEPryorJAShort-term comparative of high frequency chest wall oscillation and European airway clearance techniques in patients with cystic fibrosisThorax20106519620019703826
- DegreefJMCrepinJLDeroubalxCReduction du nombre de superinfections bronchiques par la ventilation a percussion intrapulmonaire, chez de patients atteints de bronchopneumopaties chroniques obstructives (BPCO) ou de bronchiectasies (DDB)Rev Mal Resp20031S89129
- NavaSBarbaritoNPiaggiGDe MattiaECirioSPhysiological response to intrapulmonary percussive ventilation in stable COPD patientsRespir Med20061001526153316490350
- TestaAGaleriSVillafaneJHCorbelliniCPillastriniPNegriniSEfficacy of short-term intrapulmonary percussive ventilation in patients with chronic obstructive pulmonary diseaseDisabil Rehabil20153789990325098596
- VargasFBoyerABuiHNGuenardHGrusonDHilbertGEffect of intrapulmonary percussive ventilation on expiratory flow limitation in chronic obstructive pulmonary disease patientsJ Crit Care20092421221919327288
- VargasFBuiNHBoyerAIntrapulmonary percussive ventilation in acute exacerbation of COPD patients with mild respiratory acidosis: a randomized controlled trialCrit Care20059R382R38916137351
- AntonagliaVLucangeloUZinWAIntrapulmonary percussive ventilation improves the outcome of patients with acute exacerbations of COPD using helmetCrit Care Med2006342940294517075375
- DimassiSVargasFLyazidiAIntrapulmonary percussive ventilation superimposed on spontaneous breathing: a physiological study in patients at risk for extubation failureIntensive Care Med2011371269127621656293
- IdesKVosWde BackerLAcute effects of intrapulmonary percussive ventilation in COPD patients assessed by using conventional outcome parameters and a novel computational fluid dynamics techniqueInt J COPD20127667671
- CliniEMAntoniFDVitaccaMIntrapulmonary percussive ventilation in tracheostomized patients: a randomized controlled trialIntensive Care Med2006321994200117061020
- BravermanJNozzarellaMJHigh-frequency chest compression: advanced therapy for obstructive lung diseaseRespir Ther200724851
- MahajanAKDietteGBHatipogluUHigh frequency chest wall oscillation for asthma and chronic obstructive pulmonary disease exacerbations: a randomized sham-controlled clinical trialRespir Res2011122021294865
- ChakravortyIChahalKAustinGA pilot study of the impact of high-frequency chest wall oscillation in chronic obstructive pulmonary disease patients with mucus hypersecretionInt J COPD20116693699
- BidiwalaAVolpeLHalabyCFazzariMValsamisCPirzadaMA comparison of high frequency chest wall oscillation and intrapulmonary percussive ventilation for airway clearance in pediatric patients with tracheostomyPostgrad Med201712927628227882804