Abstract
Background
Thirty-day readmission in COPD is common and costly, but potentially preventable. The emergency department (ED) may be a setting for COPD readmission reduction efforts.
Objective
To better understand COPD readmission through the ED, ascertain factors associated with 30-day readmission through the ED, and identify subgroups of patients with COPD for readmission reduction interventions.
Patients and methods
A retrospective cohort study was conducted from January 2009 to September 2015 in patients with COPD of age ≥18 years. Electronic health record data were abstracted for information available to admitting providers in the ED. The primary outcome was readmission through the ED within 30 days of discharge from an index admission for COPD. Logistic regression was used to examine the relationship between potential risk factors and 30-day readmission.
Results
The study involved 1,574 patients who presented to the ED within 30 days on an index admission for COPD. Of these, 82.2% were readmitted through the ED. Charlson score (odds ratio [OR]: 3.6; 95% CI: 2.9–4.4), a chief complaint of breathing difficulty (OR: 1.6; 95% CI: 1.1–2.6), outpatient utilization of albuterol (OR: 4.1; 95% CI: 2.6–6.4), fluticasone/salmeterol (OR: 2.3; 95% CI: 1.3–4.2), inhaled steroids (OR: 3.8; 95% CI: 1.3–10.7), and tiotropium (OR: 1.8; 95% CI: 1.0–3.2), as well as arterial blood gas (OR: 4.4; 95% CI: 1.3–15.1) and B-type natriuretic peptide (OR: 2.2; 95% CI: 1.4–3.5) testing in the ED were associated with readmission (c-statistic =0.936). Seventeen-point-eight percent of patients with COPD presented to the ED and were discharged home; 56% presented with a complaint other than breathing difficulty; and 16% of those readmitted for breathing difficulty had a length of stay <48 hours.
Conclusion
Intensive outpatient monitoring, evaluation, and follow-up after discharge are needed to help prevent re-presentation to the ED, as practically all patients with COPD who represent to the ED within 30 days are readmitted to the hospital and for a variety of clinical complaints. Among those patients with COPD who present with breathing difficulty, improved decision support algorithms and alternative management strategies are needed to identify and intervene on the subgroup of patients who require <48-hour length of stay.
Background
COPD is a prevalent disease that is of immense concern to the US public health and health care systems. An estimated 24 million Americans (7.5%) suffer from COPD, with the highest prevalence of disease being found in the states of Michigan (7.4%), Tennessee (8.7%), Alabama (9.1%), and Kentucky (9.3%).Citation1 The economic burden of COPD is significant. In 2010, the cost of COPD was $49.9 billion or ~$4,000 per patient per year.Citation2 Hospital admissions and readmissions for patients with COPD are high, are on the rise, and have become a focus of pay-for-performance and quality improvement programs.Citation3 Published evidence has shown a 7.1% 30-day readmission rate for a principal diagnosis of COPD and 20.5% for all-cause 30-day readmission among discharged patients with COPD.Citation4
Interventions have attempted to reduce COPD readmissions.Citation5 However, currently, there is inadequate evidence to endorse specific recommendations to reduce readmissions among patients with COPD.Citation5 Despite a lack of explicit guidance, establishment of the Medicare Hospital Readmission Reduction Program (MHRRP) has prompted hospitals to examine and intervene all aspects of COPD patients’ care, including their re-entry into the hospital through the emergency department (ED).Citation6
Decision support algorithms are available to physicians to assist in determining appropriate hospital admission vs observation and/or discharge home in COPD.Citation7–Citation12 However, the adoption and utility of these tools is unclear, and decisions to admit patients with COPD are often based on clinical judgment. With increasing attention on the ED as a potential setting to reduce 30-day COPD readmissions, our objectives were to better understand COPD readmission through the ED, ascertain clinical and demographic factors driving decisions to readmit patients to the hospital through the ED, and identify subgroups of patients with COPD for potential readmission reduction efforts.
Patients and methods
Study design
A retrospective cohort study was conducted on all patients presenting with COPD of age ≥18 years from Beaumont Health (BH) between January 1, 2009 and September 30, 2015. BH is a large health care system serving patients across south-eastern Michigan, including greater Detroit. To be included, the criteria were as follows: 1) patients discharged from an inpatient stay with an index diagnosis of COPD, 2) patients who presented to the ED for any reason within 30 days of discharge, and 3) those who were readmitted through the ED or discharged home from the ED within 30 days of discharge. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes were used to identify patients with COPD: 491–491.22, 492–492.8, 493.2, and 496. All patient data utilized for this study were de-identified prior to obtainment and analysis. The BH Research Institute for Human Investigation Committee approved this study (institutional review board number 2015-443). This manuscript was prepared in accordance with Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis and Strengthening the Reporting of Observational Studies in Epidemiology.Citation13,Citation14
BH’s electronic health record (EHR; Epic Systems, Verona, WI, USA) was queried between the study dates to identify patients meeting the inclusion criteria and to obtain the clinical, demographic, and outcome data necessary for the analysis. It was possible for patients to have multiple COPD admissions and readmissions during the study period. To ensure that we analyzed unique patients, we limited the sample to only the first occurrence of when a patient visited the ED within 30 days of a discharge for COPD.
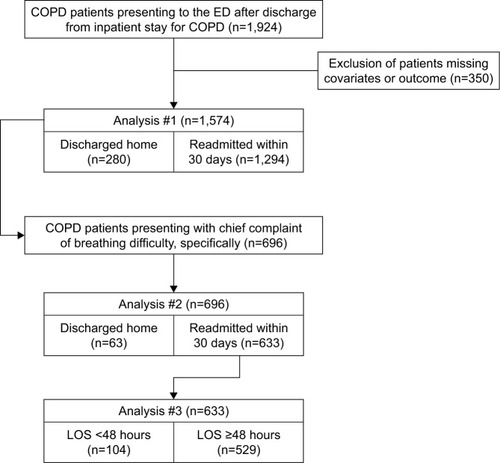
Outcomes
The primary outcome of this study was readmission through the ED within 30 days of discharge from an index admission for COPD. Second, we examined readmission through the ED within 30 days of discharge from an index admission for COPD for patients who presented with a chief complaint of breathing difficulty. Third, among patients with COPD who were readmitted within 30 days through the ED, we evaluated predictors for readmission length of stay (LOS) ≥48 hours.
Predictors
Clinical and demographic variables were identified based on the clinical input of the authors. Clinical data included, but were not limited to, arterial blood gas (ABG) testing, B-type natriuretic peptide (BNP) testing and results, weight (kg), height (m), Glasgow Coma Score, presenting and last-collected vital signs, oxygen saturation, FiO2%, O2 (L/min) supplementation, method of O2 delivery, Charlson score, prescribed outpatient COPD medications, chief complaint in ED, time to ED visit (days), time in ED (hours), length of prior inpatient stay (days), and length of second inpatient stay (days). Demographic data included age (years), gender, race/ethnicity, primary insurance, marital status, smoking status, and smoking pack years (packs/year).
Statistical analysis
Patients with missing covariates were excluded to conduct a complete case analysis. Univariate analyses were used to examine characteristics by 30-day readmission status. All factors associated with 30-day readmission through the ED in univariate analyses were used to build a multivariate logistic regression model, where the outcome was modeled as a binary indicator (ie, whether the patient was admitted to the hospital through the ED or not). A P-value of 0.25 was used as a cutoff for inclusion in the final model, as more traditional levels such as 0.05 can fail in identifying variables known to be important.Citation15,Citation16 Certain patient characteristics (ie, age, gender, insurance, and smoking) were incorporated into the model regardless of univariate statistical significance, as they have previously been identified as risk factors for readmission.Citation7–Citation12 The c-statistic was used to approximate the predictive validity of the model.Citation17
Next, we limited the sample to patients presenting to the ED within 30 days with a chief complaint of breathing difficulty. The purpose of this analysis was to identify potential predictors of 30-day readmission among patients with likely COPD exacerbation vs those with chief complaints unrelated to their underlying COPD.
Finally, we examined potential predictors of a readmission LOS ≥48 hours among patients readmitted with breathing difficulty. The goal of this analysis was to identify features that have a relationship with LOS. All analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA).
Ethics approval and consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the BH Research Institute for Human Investigation Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. A waiver of informed consent was obtained for participants of this study, given the retrospective nature of the investigation (BH institutional review board number 2015-443).
Results
All patients
The final sample consisted of 1,574 patients with COPD who presented to the ED within 30 days of an index admission for COPD (). Of these patients, 82.2% (n=1,294) were readmitted through the ED. displays patient characteristics by readmission status. Multivariate logistic regression model revealed significant relationships between 30-day readmission and a number of patient characteristics (). For every single unit increase in Charlson score, the odds of 30-day readmission increased by 3.6 (95% CI: 2.9–4.4). Prescribed outpatient COPD medications, including albuterol (odds ratio [OR]: 4.1; 95% CI: 2.6–6.4), fluticasone/salmeterol (OR: 2.3; 95% CI: 1.3–4.2), inhaled steroids (OR: 3.8; 95% CI: 1.3–10.7), and tiotropium (OR: 1.8; 95% CI: 1.0–3.2), were found to be independent predictors of 30-day readmission through the ED. In addition, a chief complaint of breathing difficulty (OR: 1.7; 95% CI: 1.1–2.6), and ABG (OR: 4.4; 95% CI: 1.3–15.1) and BNP (OR: 2.2; 95% CI: 1.4–3.5) testing were associated with 30-day readmission (c-statistic =0.936).
Table 1 Demographic and clinical characteristics of COPD patients presenting to the ED by 30-day readmission status
Table 2 Multiple logistic regression results for COPD patients presenting to the ED by 30-day readmission status
Breathing difficulty
Out of the final sample, 44.2% (n=696) presented to the ED with a chief complaint of breathing difficulty. Of these patients, 90.9% (n=633) were readmitted through the ED (Table S1). Among patients who presented with breathing difficulty, our multivariate regression model revealed that Charlson score (OR: 2.3; 95% CI: 1.7–3.2), albuterol utilization (OR: 7.2; 95% CI: 3.2–16.3), being a former smoker (OR: 3.5; 95% CI: 1.0–12.6), and having an increased pulse rate in the ED (OR: 1.0; 95% CI: 1.0–1.1) were independent predictors of readmission through the ED (Table S2; c-statistic =0.936).
Readmission length
Out of the 633 patients with breathing difficulty who were readmitted, 83.6% (n=529) had an LOS ≥48 hours. Readmitted patients with an LOS ≥48 hours remained in the hospital on an average of 8.1 days (Table S3). Multivariate logistic regression revealed that a longer LOS during the previous COPD inpatient stay (OR: 1.2; 95% CI: 1.1–1.3) predicted a readmission length ≥48 hours. Furthermore, a Glasgow score of 15 (OR: 0.1; 95% CI: 0.01–0.7) was negatively associated with readmission length (Table S4; c-statistic =0.762).
Discussion
We observed that 82% of patients with COPD who presented to the ED within 30 days of an index admission for COPD were readmitted through the ED. Significant risk factors for 30-day readmission through the ED included Charlson score, prescribed outpatient COPD medications (albuterol, fluticasone/salmeterol, and inhaled steroids), a chief complaint of breathing difficulty, and the conduct of ABG and BNP testing in the ED. Among patients with COPD who presented with breathing difficulty, 91% were readmitted. Outpatient albuterol utilization, smoking history, and an increased pulse rate were risk factors for readmission in this group. Among patients with COPD who were readmitted with breathing difficulty, ~84% had a readmission stay ≥48 hours, with an average LOS of 8 days. Risk factors for a readmission stay ≥48 hours included previous COPD admission LOS and a Glasgow score of <15 in the ED.
Readmission events among patients with COPD are common, costly, and potentially preventable. Since incorporation of COPD into the MHRRP, there has been interest in identifying and mitigating the risk factors for readmission in patients with COPD.Citation18,Citation19 In 2003, Garcia-Aymerich et al published what has become a prominent study of risk factors for COPD readmission. Among 340 patients with COPD, ≥3 admissions for COPD in the previous year, anti-cholinergic drug use, oral corticosteroid use, and long-term oxygen therapy significantly predicted readmission at 1 year, while forced expiratory volume in 1 second, oxygen tension, and higher levels of physical activity were protective.Citation20 We found that outpatient COPD medications (albuterol, fluticasone/salmeterol, and inhaled steroids) were associated with 30-day readmission through the ED. This relationship is likely explained by the severity of a patient’s baseline disease. In other words, a patient with more severe baseline COPD is likely prescribed a more extensive and complex medication regimen consistent with standard therapy, and is sicker and at increased need for readmission than the patients who are not prescribed such medications. Outpatient albuterol use alone may also be a reflection of uncontrolled disease after discharge in these patients.
In 2015, Genao et al published a claims-based analysis examining the risk factors for repeat acute care visits within 30 days of an index COPD admission among 18,306 patients. The authors identified age ≥80 years, dual-eligibility status, long-term oxygen use, and several pulmonary comorbidities as risk factors for repeat acute care visits.Citation21 We did not examine specific pulmonary comorbidities, but our findings are in agreement that multimorbidity drives COPD readmission. In addition, our study confirms breathing difficulty as a risk factor for readmission.Citation22,Citation23 However, unlike previous research, we found that gender, age, insurance, and number of inpatient admissions over the previous year were not associated with 30-day readmission.Citation24,Citation25 Interestingly, we did observe an association between ABG and BNP testing and 30-day readmission through the ED. ABG testing is an important clinical tool used to dictate emergent treatment, especially in critically ill patients; therefore, it is not surprising that its use would be associated with readmission. In this setting, ABG testing likely serves as a marker for severe respiratory disease and/or identifies patients presenting with a clinical impression of respiratory distress, rather than serving as a laboratory test that independently predicts readmission. In the acute care setting, BNP is used to distinguish dyspnea secondary to cardiac vs other etiologies, and is often used in the ED to identify acute exacerbations of congestive heart failure. We found that BNP testing was associated with 30-day readmission among all patients, but not when the sample was limited to patients who presented with breathing difficulty. The latter finding is likely explained by the fact that although BNP testing can be used to help determine the etiology of dyspnea among patients who present to the ED, it is not considered to have a profound impact on hospitalization rates or patient outcomes,Citation26 and in our case did not significantly impact the decision to readmit. Comorbid congestive heart failure may explain our observed relationship between BNP testing and 30-day readmission in all patients, regardless of presenting chief complaint. Although requiring additional study, this finding could also represent improper and/or overuse of BNP testing in patients with COPD who present to the ED for non-dyspnea reasons, resulting in an unwarranted increased tendency among providers to readmit.
The ED has been identified as a potential setting to target COPD readmission reduction efforts.Citation6 We agree with this notion as 82% and 91% of patients with COPD who presented to the ED for any cause or with breathing difficulty, specifically, were readmitted to the hospital through ED within 30 days in our sample. Sweeping COPD readmission reduction programs have proven to be largely ineffective to date.Citation27 However, there is promise in targeting specific subgroups of patients with COPD to reduce overall readmission rates.Citation27 In accordance with this thinking, we limited our sample to patients with COPD presenting to the ED with breathing difficulty and then subdivided this group of patients by subsequent readmission length.
Only 44% of the patients in our study presented to the ED with breathing difficulty; 56% presented due to reasons such as chest pain, fatigue, abdominal pain, musculoskeletal complaint, or blood sugar problem. A significant proportion of this 56% could likely benefit from an outpatient primary care visit immediately after discharge or discharge directly to a subacute rehab facility where low-risk health complaints could be addressed, and thereby potentially avoid needing to visit the ED. Almost 91% of patients with COPD who presented to the ED with breathing difficulty were readmitted to the hospital. Among these patients, we found the following to predict 30-day readmission: outpatient albuterol utilization, being a former smoker, having a higher Charlson score, and having an increased pulse rate in the ED. These risk factors may be mitigated through better access to and follow-up with generalists and specialists to improve management of comorbid conditions as well as better stabilization and normalization of patients in the ED.
One intervention that may prove to be beneficial in preventing re-presentation to the ED is an early and automatic outpatient visit after discharge. If patients with COPD can be seen in person or connected with using telehealth modalities within 48 hours of discharge, this would provide clinicians with an opportunity to clinically assess the patient, evaluate the effect of medication changes made during the previous admission, monitor medication adherence patterns, and discuss other non-COPD-related health concerns the patient has. The ultimate goal of this intervention would be to prevent re-presentation to the ED to begin with. Although such an intervention may be difficult for individual attending physicians, a supervised resident or associate provider clinic and workforce could potentially make a significant impact in this arena.
In an effort to identify patients who could have been safely discharged home or managed in the ED longer rather than being readmitted, we examined the LOS for readmitted patients with COPD with breathing difficulty. We found that 83.6% of readmitted patients had an LOS of ≥48 hours, with an average LOS of 8 days. LOS of their index COPD admission and Glasgow score in the ED predicted the length of their second inpatient stay. The index COPD admission LOS of the 16.4% of patients with a second LOS <48 hours was 1.3 days. These observations suggest that there are two distinct populations of patients with COPD who are readmitted within 30 days: those likely requiring minimal therapy and those requiring more advanced management and a justifiable, increased LOS. Different readmission reduction interventions can be designed to target these two groups, and prior admission LOS may be a useful piece of information for the readmission decision-making process in the ED.
In today’s climate of bundled payments and MHRRP, having 82%–91% of patients with COPD readmitted through the ED within 30 days of an inpatient discharge is a quality of care and financial issue for hospitals. From an equally important perspective, we have shown that 9%–18% of patients with COPD who present to the ED are discharged home without being readmitted. These patients are healthier and have less comorbidity than patients who are readmitted to the hospital, suggesting that these individuals presented to the ED unnecessarily. We have also shown that a large percentage of patients with COPD are readmitted through the ED, but more than half of the time (56%) with complaints other than breathing difficulty. Even if patients present with troubled breathing, 16% are readmitted to the hospital for <48 hours. These results may speak to the need for better education at discharge regarding when it is appropriate for a COPD patient to present to the ED vs primary care provider with a health concern after discharge. Our findings may also provide additional evidence for the role of immediate outpatient follow-up after discharge or discharge to a subacute rehab facility rather than directly home. Furthermore, given the high rate of readmissions observed in this study, the ED is a logical setting in which to target certain COPD readmission reduction efforts that identify patients who would not benefit from readmission or could be managed in an alternative manner, such as more thoughtful monitoring in an observation unit. ED and admitting providers should be willing to examine their decision making regarding readmission to the hospital, significant risk factors for readmission, and be willing to mitigate potentially modifiable ones, such as unstable vital signs and potentially unnecessary testing.
Strengths of our study include a large sample size and the use of EHR data to obtain a robust set of variables. These aspects help improve the study’s generalizability. The weakness is our use of ICD-9-CM codes to identify patients with COPD. The sensitivity of ICD-9-CM codes for COPD is low and ranges from 12% to 25%, whereas the specificity is >99%.Citation28 Our study may suffer from an increased number of false negatives, which inappropriately undercounted COPD hospitalizations. We may also have missed patients who presented to unaffiliated hospitals. In addition, despite our use of EHR data, we were missing important covariates such as forced expiratory volume in 1 second, COPD medication adherence, physical activity level, quality of life, a primary care provider visit before ED presentation, and the subjective assessment of the patient’s clinical picture. In particular, lack of data related to functional assessment and disease severity (frequent exacerbations vs nonfrequent exacerbations) is an important limitation of this study that needs to be noted, as predictors of readmission are likely influenced by underlying disease activity and comorbidities. We attempted to address this limitation by controlling for the number of inpatient admissions over the previous year, Charlson score, and smoking status. However, proxies for disease severity and comorbidity burden likely underestimate the impact of these factors on readmission risk.
Conclusion
Our findings demonstrate the need for intensive outpatient monitoring, evaluation, and follow-up after discharge to help prevent re-presentation to the ED, as practically all patients with COPD who represent to the ED are readmitted to the hospital and for a variety of clinical complaints. Among those patients with COPD who present with breathing difficulty, improved decision support algorithms and alternative management strategies are needed to identify and intervene on the subgroup of patients who require <48-hour LOS.
Acknowledgments
Charlotte E Ward is supported by the training grant T32 HS000084 awarded to Northwestern University and the University of Chicago, by the Agency of Healthcare Research and Quality, as part of her doctoral program.
Dr Michael Rezaee and Mr Daniel Rezaee are siblings. However, Dr Michael Rezaee is a physician based in southeastern Michigan, while Mr Daniel Rezaee is a population health specialist based in Boston, Massachusetts. All authors declare that their relationship as siblings did not impact the conduct of this study or the development of this manuscript in any way.
Supplementary materials
Table S1 Demographic and clinical characteristics of COPD patients presenting to the ED with breathing difficulty by 30-day readmission status
Table S2 Multiple logistic regression results for COPD patients presenting to the ED with breathing difficulty by 30-day readmission status
Table S3 Demographic and clinical characteristics of COPD patients readmitted through the ED with breathing difficulty by readmission length
Table S4 Multiple logistic regression results for COPD patients presenting to the ED with breathing difficulty by 30-day readmission length ≥48 hours
Disclosure
The authors report no conflicts of interest in this work.
References
- Centers for Disease Control and PreventionChronic Obstructive Pulmonary Disease (COPD)2014 Available from: http://www.cdc.gov/copd/data.htmAccessed February 4, 2016
- American Lung AssociationCOPD Fact Sheet2011 Available from: http://www.lung.org/lung-disease/copd/resources/facts-figures/COPD-Fact-Sheet.htmlAccessed February 4, 2016
- FordESHospital discharges, readmissions, and ED visits for COPD or bronchiectasis among US adults: findings from the nationwide inpatient sample 2001–2012 and Nationwide Emergency Department Sample 2006–2011Chest2015147498999825375955
- ElixhauserAHuDAPodulkaJReadmissions for Chronic Obstructive Pulmonary Disease, 2008. Statistical Brief #121Healthcare Cost and Utilization Project2011 Available from: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb121.pdfAccessed December 23, 2016
- Prieto-CenturionVMarkosMARameyNIInterventions to reduce rehospitalizations after chronic obstructive pulmonary disease exacerbations. A systematic reviewAnn Am Thorac Soc201411341742424423379
- American College of Emergency PhysiciansMedicare’s hospital readmission reduction program FAQ2015 Available from: http://www.acep.org/Physician-Resources/Practice-Resources/Administration/Financial-Issues-/-Reimbursement/Medicare-s-Hospital-Readmission-Reduction-Program-FAQ/Accessed February 4, 2016
- Garcia-GutierrezSQuintanaJMAguirreUInvestigación en Resultados y Servicios Sanitarios (IRYSS) COPD GroupExplicit criteria for hospital admission in exacerbations of chronic obstructive pulmonary diseaseInt J Tuberc Lung Dis201115568068621756522
- Garcia-GutierrezSQuintanaJMBarrioIApplication of appropriateness criteria for hospitalization in COPD exacerbationIntern Emerg Med20138434935723508735
- QuintanaJMEstebanCBarrioIIRYSS-COPD GroupThe IRYSS-COPD appropriateness study: objectives, methodology, and description of the prospective cohortBMC Health Serv Res20111132222115318
- RoweBHBhutaniMSticklandMKCydulkaRAssessment and management of chronic obstructive pulmonary disease in the emergency department and beyondExpert Rev Respir Med20115454955921859274
- Garcia-AymerichJMonsoEMarradesRMRisk factors for hospitalization for a chronic obstructive pulmonary disease exacerbation. EFRAM studyAm J Respir Crit Care Med200116461002100711587986
- AmalakuhanBKiljanekLParvathaneniAHesterMCheriyathPFischmanDA prediction model for COPD readmissions: catching up, catching our breath, and improving a national problemJ Community Hosp Intern Med Perspect20122110.3402/jchimp.v2i1.9915
- CollinsGSReitsmaJBAltmanDGMoonsKGTransparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statementBr J Surg2015102314815825627261
- VandenbrouckeJPvon ElmEAltmanDGStrengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaborationPLoS Med2007410e29717941715
- BendelRBAfifiAAComparison of stopping rules in forward “Stepwise” regressionJ Am Stat Assoc1977723574653
- MickeyRMGreenlandSThe impact of confounder selection criteria on effect estimationAm J Epidemiol198912911251372910056
- HarrellFRegression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival AnalysisNY, USASpringer-Verlag New York2001
- US Centers for Medicare & Medicaid ServicesHospital Readmissions Reduction Program2016 Available from: https://www.medicare.gov/hospitalcompare/readmission-reduction-program.htmlAccessed December 23, 2016
- GlaserJBPauDManiatisTDifferential risk factors for chronic obstructive pulmonary disease 30-day readmissions according to indication for readmissionAnn Am Thorac Soc2016133447
- Garcia-AymerichJFarreroEFelezMAIzquierdoJMarradesRMAntoJMEstudi del Factors de Risc d’Agudització de la MPOC investigatorsRisk factors of readmission to hospital for a COPD exacerbation: a prospective studyThorax200358210010512554887
- GenaoLDurheimMTMiXToddJLWhitsonHECurtisLHEarly and long-term outcomes of older adults after acute care encounters for chronic obstructive pulmonary disease exacerbationAnn Am Thorac Soc201512121805181226394180
- BahadoriKFitzGeraldJMRisk factors of hospitalization and readmission of patients with COPD exacerbation systematic reviewInt J Chron Obstruct Pulmon Dis20072324125118229562
- CaoZOngKCEngPTanWCNgTPFrequent hospital readmissions for acute exacerbation of COPD and their associated factorsRespirology200611218819516548905
- PouwEMTen VeldeGPCroonenBHKesterADScholsAMWoutersEFEarly non-elective readmission for chronic obstructive pulmonary disease is associated with weight lossClin Nutr2000192959910867726
- GroenewegenKHScholsAMWoutersEFMortality and mortality-related factors after hospitalization for acute exacerbation of COPDChest2003124245946712907529
- CarpenterCRKeimSMWorsterARosenPBEEM (Best Evidence in Emergency Medicine)Brain natriuretic peptide in the evaluation of emergency department dyspnea: is there a role?J Emerg Med201242219720522123173
- BerryCEKalhanRChronic obstructive pulmonary disease rehospitalization. A big problem that now needs solutionsAnn Am Thorac Soc201512121741174226653184
- SteinBDBautistaASchumockGTThe validity of International classification of diseases, ninth revision, clinical modification diagnosis codes for identifying patients hospitalized for COPD exacerbationsChest20121411879321757568