Abstract
Objective
Pneumonia is one of the most common infectious diseases in patients with COPD. The risk of empyema in COPD is controversial, and its incidence has not been reported. The aim of our study was to determine the risk of empyema in COPD patients and to assess its risk factors.
Patients and methods
We used the National Health Insurance Research Database in Taiwan to conduct an observational cohort study. This study analyzed patients who were diagnosed with COPD between January 1, 2003 and December 31, 2009. The earliest date of COPD diagnosis was designated the index date. Patients who were younger than 40 years or had empyema before the index date were excluded.
Results
We analyzed 72,085 COPD patients in our study. The incidence of empyema was higher in the COPD group than in the non-COPD group (15.80 vs 4.34 per 10,000 person-years). The adjusted hazard ratio for empyema was 3.25 (95% CI =2.73–3.87) in patients with COPD compared with patients without COPD. COPD patients with only comorbidity of stroke, cancer, and chronic renal disease had adjusted hazard ratios of 1.88, 4.84, and 3.90, respectively.
Conclusion
The likelihood of developing empyema is higher in patients with COPD than in those without COPD. Some comorbidities, such as stroke, cancer, and chronic renal disease, are associated with an elevated risk for empyema in COPD patients.
Keywords:
Introduction
COPD is a chronic inflammatory disease characterized by irreversible airway obstruction.Citation1 COPD patients are often colonized with bacteria and viruses that result in airway inflammation. A previous study showed that severe COPD decreased the cytokine response to pathogen-associated molecular patterns and proposed that bacterial colonization may attenuate the systemic innate immune response.Citation2 One of the most common infections in COPD patients is pneumonia.Citation3 Parapneumonic effusions in the pleural spaces represent a complication of pneumonia and are found in ~40% of bacterial pneumonia cases.Citation4 Parapneumonic pleural effusions are divided into uncomplicated parapneumonic effusions, complicated parapneumonic effusions, and empyema. Complicated parapneumonic effusions and empyema result from bacterial infections in the pleural space. Empyema is characterized by pus-like pleural effusions, an offensive odor, and bacterial isolation from the pleural effusion. Dusemund et al used records from a database from Switzerland between 2002 and 2010 to investigate the outcomes of adult patients with community-acquired pneumonia and COPD and found that the most frequent complication was pleural effusion, which was less frequent in COPD patients than in comparison subjects. The frequency of empyema did not differ between COPD patients and comparison subjects.Citation5 Chalmers et al conducted a prospective observational study of patients in the UK and found that COPD was associated with a decreased risk of developing complicated parapneumonic effusions or empyema.Citation6
However, another studyCitation7 showed that COPD is a risk factor for empyema. Although lung infections such as pneumonia more often occur in COPD patients than in the general population, there is little evidence and much controversy related to the association between COPD and empyema. The purpose of this study was to determine the risk of empyema in COPD patients and to assess the risk factors of empyema in COPD.
Patients and methods
Ethics statement
This observational study was evaluated and approved by the Institutional Review Board (IRB) of the Chi Mei Medical Center, Taiwan (IRB: 10601-E01). All personal information from the dataset was de-identified for strict anonymity before further analysis. Informed consent was waived by the approving IRB.
Data sources
National Health Insurance (NHI) is a public, single-payer insurance program with nationwide coverage in Taiwan that has operated since 1995. It covers ~99% of the population and contracts with 97% of health care providers. The NHI Research Database (NHIRD), authorized and released for research purposes, contains all inpatient and outpatient registration and claim data of the NHI program. The data include patients’ demographic characteristics, disease diagnostic, and surgical operation codes (based on the International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM]), prescription records, and medical expenditures. The NHIRD is one of the largest administrative health care databases in the world. We retrospectively obtained a longitudinally linked NHIRD subset of 1 million randomly selected enrollees from 1996 to 2010. Confidential data of the selected subjects were de-identified.
Patients
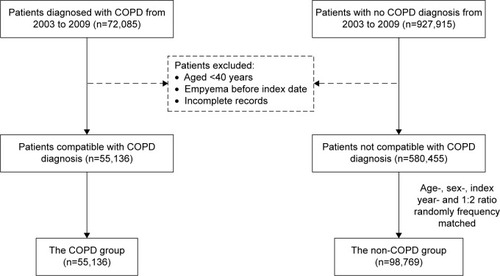
This study analyzed patients who were diagnosed with COPD (ICD-9-CM codes 490–492 and 496) between January 1, 2003 and December 31, 2009. To ensure COPD diagnosis, subjects with at least three outpatient visits or one inpatient admission with a main diagnosis of COPD in the NHIRD database were selected. The last date of the three outpatient visits or the first day of the first hospitalization, whichever came earlier, was designated as the index date used to estimate the risk of empyema. Patients who were younger than 40 years, had empyema before the index date, or had incomplete records were excluded. In total, 72,085 qualified patients with COPD were initially retrieved before exclusion filtering (). Comparison subjects were selected among hospitalized patients without COPD and were matched according to age in year of the index date (±3 years) and sex at a 2:1 ratio.
Empyema and comorbidities
To investigate the risk of empyema, the patients were followed until the occurrence of empyema (ICD-9-CM code 510), death, withdrawal from the NHI, or the end of 2010. Comorbidities including diabetes, hypertension, chronic liver disease, stroke, cancer, and chronic renal disease were identified starting from 1 year before the index day according to ICD-9-CM codes in the outpatient and inpatient records.
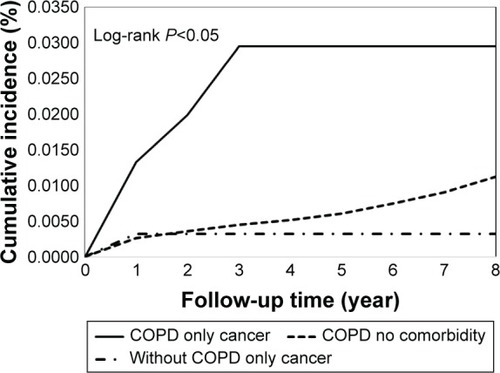
Statistical analysis
The demographic variables and comorbidities of the patients with or without COPD are expressed as frequencies (percentages) or mean (±SD) and were compared using chi-square tests and Student’s t-test, respectively. The demographic characteristics included sex and age (stratification into 40–49, 50–59, 60–69, and >70 years). Cumulative incidence curves for empyema were plotted using the Kaplan–Meier method, and the differences in curves between patients with and without COPD were analyzed by a log-rank test. The incidence rate of empyema was estimated using the total number of empyema events divided by the total follow-up period (per 10,000 person-years). Cox proportional hazards models were used to measure the main effects of comorbidities among patients on the time to empyema occurrence with adjusted variables, age, and sex, which showed significant association with empyema. Hazard ratios (HRs) and their 95% CIs were estimated. Variables with significant values in the univariable model were further examined in the Cox regression model. All statistical tests were two-sided, and a P-value of 0.05 was considered significant. The statistical analyses were performed using SPSS (version 15; SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics
The study groups included 55,136 patients diagnosed with COPD and 98,769 patients without COPD (). In the COPD group, the mean age was 65.4±13.2 years, with 41.3% of the patients aged ≥70 years, and 56.6% of the patients were male (). Likewise, in the non-COPD group, the mean age was 65.7±11.7 years, with 38.7% aged ≥70 years, and 53.2% were male. The distributions of age and sex were similar between both groups.
Table 1 Demographic characteristics and comorbidities of patients with and without COPD
Patients in the COPD group had a higher prevalence of comorbidities than those in the non-COPD group (diabetes [17.8% vs 14.8%], hypertension [43.9% vs 33.4%], chronic liver disease [10.7% vs 6.7%], stroke [13.6% vs 8.0%], cancer [1.4% vs 0.9%], and chronic renal disease [1.7% vs 1.2%]).
Incidence of empyema
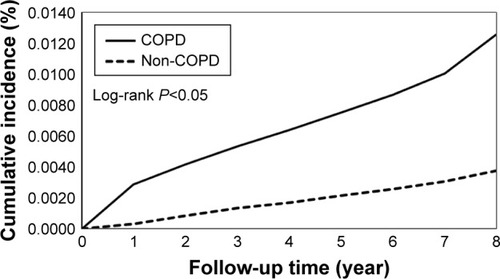
As shown in , the overall incidence rate of empyema was higher in the COPD group than in the non-COPD group (15.8 vs 4.3 per 10,000 person-years). The adjusted HR (aHR 3.25, 95% CI =2.73–3.87) of empyema indicated that the risk of empyema was 3.25 times higher for COPD patients than for non-COPD patients.
Table 2 Incidence of empyema in patients with and without COPD
This relationship was further investigated by examining the associations between age, sex, and comorbidities. In the COPD group, the age-stratified incidence rates of empyema increased with age (7.44, 10.33, 13.26, and 24.15 for subjects aged 40–49, 50–59, 60–69, and >70 years, respectively). Similarly, increased incidence rates with age were also found in the non-COPD group. Cox regression showed that age, sex, and comorbidities were associated with higher risks of empyema in the COPD group than in the non-COPD group (). For example, among patients with diabetes, the aHR of empyema in the COPD group was 2.48 times (95% CI =1.73–3.55; P<0.001) higher than in the non-COPD group.
Comorbidities and empyema occurrence
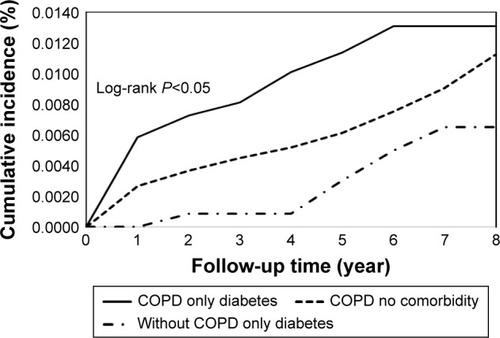
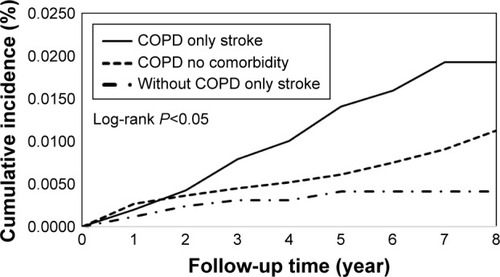
We further investigated the associations between comorbidities and empyema occurrence among COPD patients (). The baseline group (n=20,285) included COPD patients with no comorbidities for comparisons with patients with one comorbidity. COPD patients with only comorbid diabetes had a marginally increased risk of empyema (aHR 1.65, 95% CI =0.98–2.78; P=0.06). Similarly, significantly increased risks of empyema were found with only stroke (aHR 1.88, 95% CI =1.13–3.11; P=0.02), only cancer (aHR 4.84, 95% CI =1.97–11.8; P<0.001), and only chronic renal disease (aHR 3.90, 95% CI =1.24–12.3; P<0.02). The significant values of the aHR increased (from 1.25 to 1.54) when the number of comorbidities increased (from ≥1 to ≥3).
Table 3 Impact of comorbidities on empyema among COPD patients (n=55,136)
Cumulative incidence rates of empyema
Cumulative incidence curves for the COPD and non-COPD groups used to estimate the occurrence of empyema over time () showed significant differences between the two study groups (P<0.05, log-rank test). As shown in , COPD patients with only comorbid diabetes showed a significantly higher risk of empyema than COPD patients with no comorbidities and non-COPD patients with only comorbid diabetes (P<0.05, log-rank test). Similar patterns of empyema risk were also found for COPD patients with only stroke () or only cancer ().
Discussion
In our study, the percentages of comorbidities, including diabetes, hypertension, hyperlipidemia, chronic liver disease, stroke, cancer, chronic renal disease, and autoimmune disease, were much higher in COPD patients than in patients without COPD. The incidence of empyema was higher in COPD patients, with an aHR of 3.25, and age was associated with an increased risk of empyema. The two comorbidities associated with the greatest increase in risk for empyema in COPD patients compared to non-COPD patients were chronic renal disease and cancer, with aHR values of 4.56 and 4.52, respectively. Among the COPD group of patients, an increased number of comorbidities increased the risk of empyema, and the two most serious comorbidities were cancer and chronic renal disease.
Diabetes and empyema
Diabetes is associated with abnormal microvascular and neurologic parameters and a risk of infection.Citation8 Infections are frequently observed in the respiratory system due to inadequate clearance or the disturbance of normal pulmonary immune function.Citation9 Diabetes is an independent risk factor for airway infection, including pneumonia. In addition, patients with both diabetes and pneumonia have an increased risk of complications, such as bacteremia or recurrent pneumonia, and increased mortality rates have been observed in these patients.Citation10,Citation11 A previous study also showed that diabetes is the most common underlying condition in acute thoracic empyema.Citation12 Our study showed that patients with COPD and diabetes, regardless of other comorbidities, have an increased risk of empyema, with an aHR of 2.82. Previous studies have shown that diabetic patients are predisposed to pleural involvement in cases of fungal or aerobic Gram-negative bacterial infections.Citation13–Citation15 As our database lacks laboratory data, we cannot further analyze bacteriology data in patients with empyema.
Stroke and empyema
Stroke patients have an increased risk of complications, and the frequency and type of complications are associated with the severity of neurologic and functional deficits. These complications result in prolonged hospitalization, poor quality of life, and increased mortality.Citation16 One common complication after stroke is aspiration, but the frequency of aspiration may be underreported or underdiagnosed. Pneumonia is a frequent sequela of aspiration in stroke patientsCitation17 and is associated with higher mortality.Citation18 Some stroke patients with pneumonia may progress to empyema, and a delayed diagnosis without prompt treatment due to neurologic deficits can result in a poor prognosis. Few studies have investigated the association between stroke and empyema. Monteiro et alCitation19 conducted an observational study of medical records for lung abscesses or empyema between 2000 and 2008 and found that the most frequent disorder among these patients was stroke-associated disability (46.7%).
Shen at alCitation20 used the NHIRD to examine the risk of developing empyema in patients with stroke and showed that the incidence of empyema was higher in patients with stroke than in patients without stroke, with an aHR of 2.89 (95% CI =2.72–3.08).
They further subdivided the patients with stroke into ischemic and hemorrhagic stroke groups and found that the aHRs of empyema were 2.62 (95% CI =2.45–2.79) for ischemic stroke and 4.53 (95% CI =4.14–4.95) for hemorrhagic stroke, compared with patients without stroke. Stroke patients with ventriculoperitoneal shunt implantation were seven times more likely to develop empyema. In our study, patients with both COPD and stroke had an increased risk of empyema, with an aHR of 4.14, compared with COPD patients without stroke. Stroke is a risk factor of empyema not only in the general population but also in COPD patients. Prompt detection of empyema in stroke patients who are unable to communicate is the most crucial aspect of clinical management.
Cancer and empyema
Empyema in patients with a cancer history may be due to immunosuppression, disease complications of cancer, and the influence of pneumonia or necrotic tissue after chemotherapy or invasive procedures.Citation21 The incidence of empyema in patients with primary lung cancer is low, ranging from 0.1% to 0.3%.Citation22 The differentiation between empyema and cancer is not always clear, and managing empyema in patients with cancer remains challenging. The cause of empyema, whether it is a consequence of lung infection or associated with cancer and lung metastasis, will lead to different clinical management strategies and prognoses. The study of empyema, including differential counts of white blood cells, gram staining, cultures, and cytological examinations, is necessary. A bidirectional relationship exists between cancer and empyema. Patients with cancer had an increased risk of empyema in both the COPD and non-COPD groups. An increased risk of cancer has been reported in patients with inflammatory and infectious diseases.Citation23,Citation24 Previous studies have shown that empyema is associated with an increased incidence of cancer among individuals older than 60 years, male, and patients with comorbidities such as diabetes and liver cirrhosis, compared to the general population.Citation25 Only 13 patients had cancer in our study. Further studies are needed to determine the impact of different types of cancer on the development of empyema.
Chronic renal disease and empyema
Chronic renal disease and end-stage renal disease are associated with disturbances of host defenses and susceptibility to infection due to older age, immune dysfunction, comorbidities, and dialysis.Citation26 Patients with renal impairment are associated with an increased risk of pneumonia.Citation27,Citation28 Chen et al conducted a retrospective study from January 2001 to March 2006 at a medical center to elucidate the clinical features, pathogens, and outcomes among patients with both empyema and chronic renal disease or end-stage renal disease.Citation29 They found that 77.6% of empyema cases were secondary to pneumonia. Klebsiella pneumoniae (34%) was the predominant pathogen in patients before they received hemodialysis, and aerobic Gram-positive organisms were the main pathogens in patients after they received hemodialysis. Previous data have shown that the impaired immune function associated with uremia is related to serum factors and altered membrane functions in cell lines. Uremic concentrations of guanidino compounds can inhibit neutrophil superoxide formation, which has implications for neutrophil function in host defense.Citation30 Shen et al conducted a retrospective cohort study using data from the NHIRD of Taiwan. Their data showed that the incidence of empyema in patients with end-stage renal disease was 2.76-fold higher than in patients without end-stage renal disease (23.7 vs 8.19/10,000 person-years; P<0.001), with an aHR of 3.01 (95% CI =2.67–3.39), but no difference was observed in the risk of empyema between hemodialysis and peritoneal dialysis.Citation31 Our data showed that patients with COPD and chronic renal disease (including before and after receiving hemodialysis) had the highest risk of empyema compared with those with other comorbidities, with an aHR of 4.56. Physicians may need to pay closer attention to patients with COPD and chronic renal disease who have pneumonia due to the high risk of empyema.
Limitations
There are some limitations in our study that should be considered when interpreting the data. First, we used the ICD-9-CM to define patients with COPD, empyema, and other comorbidities. Over- or underdiagnosis could be argued. However, the accuracy of claims data has been evaluated and validated.Citation32 Second, the claims data did not include smoking status, pulmonary function tests, alcohol consumption, socioeconomic status, performance status, the severity of empyema, relevant clinical information on laboratory data, or imaging data. Third, the case numbers were small in the cancer, chronic renal disease, and autoimmune disease groups. We may need larger populations to verify the association between comorbidities and empyema.
Conclusion
The incidence of developing empyema is higher in COPD patients than in patients without COPD. Some comorbidities, such as stroke, cancer, and chronic renal disease, are associated with an elevated risk of empyema in COPD patients. Patients with COPD and comorbidities may require more attention because they have a high risk of developing empyema.
Acknowledgments
The authors express their sincere gratitude to Mr Zhe-Wei Xu (Department of Industrial Engineering and Management, National Yunlin University of Science and Technology) for his effort in organizing data and assisting statistical analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
- Global Initiative for Chronic Obstructive Lung Disease (GOLD): global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease; NHLBI/WHO workshop reportNIH Publication No 2701A Last update 2015. Available from: http://www.goldcopd.comAccessed August 23, 2017
- FanVSGharibSAMartinTRWurfelMMCOPD disease severity and innate immune response to pathogen-associated molecular patternsInt J Chron Obstruct Pulmon Dis20161146747727019597
- LiaoKMLinTCLiCYYangYHDementia increases severe sepsis and mortality in hospitalized patients with chronic obstructive pulmonary diseaseMedicine (Baltimore)20159423e96726061334
- LightRWGirardWMJenkinsonSGGeorgeRBParapneumonic effusionsAm J Med19806945075127424940
- DusemundFChronisJBatyFAlbrichWCBrutscheMHThe outcome of community-acquired pneumonia in patients with chronic lung diseaseSwiss Med Wkly2014144w1401325184329
- ChalmersJDSinganayagamAMurrayMPScallyCFawziAHillATRisk factors for complicated parapneumonic effusion and empyema on presentation to hospital with community-acquired pneumoniaThorax200964759259719131449
- FergusonADPrescottRJSelkonJBWatsonDSwinburnCRThe clinical course and management of thoracic empyemaQJM19968942852898733515
- KozielHKozielMJPulmonary complications of diabetes mellitus. PneumoniaInfect Dis Clin North Am19959165967769221
- MarvisiMBartoliniLdel BorrelloPPulmonary function in non-insulin-dependent diabetes mellitusRespiration200168326827211416247
- BoykoEJLipskyBASandovalRNIDDM and prevalence of nasal Staphylococcus aureus colonization. San Luis Valley Diabetes StudyDiabetes Care19891231891922702909
- CasqueiroJCasqueiroJAlvesCInfections in patients with diabetes mellitus: a review of pathogenesisIndian J Endocrinol Metab201216Suppl 1S27S3622701840
- ChenKYHsuehPRLiawYSYangPCLuhKTA 10-year experience with bacteriology of acute thoracic empyema: emphasis on Klebsiella pneumoniae in patients with diabetes mellitusChest200011761685168910858403
- VarkeyBRoseHDKuttyCPPolitisJEmpyema thoracis during a ten-year period: analysis of 72 cases and comparison to a previous study (1952–1967)Arch Intern Med198114113177117767316625
- MayoPEarly thoracotomy and decortication for nontuberculous empyema in adults with and without underlying diseases: a 25-year reviewAm Surg19855142302363985490
- SmithJAMullerworthMHWestlakeGWTatoulisJEmpyema thoracis: a 14-year experience in a teaching centerAnn Thorac Surg199151139421985571
- KalraLYuGWilsonKRootsPMedical complications during stroke rehabilitationStroke19952669909947762051
- DobkinBNeuromedical complications in stroke patients transferred for rehabilitation before and after diagnostic related groupsJ Neurol Rehabil19871137
- KoenneckeHCBelzWBerfeldeDBerlin Stroke Register InvestigatorsFactors influencing in-hospital mortality and morbidity in patients treated on a stroke unitNeurology2011771096597221865573
- MonteiroRAlfaroTMCorreiaLSimãoACarvalhoACostaJNLung abscess and thoracic empyema: retrospective analysis in an internal medicine departmentActa Med Port201124Suppl 222924022849907
- ShenTCLinCYLinCLRisk of developing pleural empyema in patients with stroke: a propensity-matched cohort studyIntern Emerg Med20171281131113828698956
- Gonzalez BarcalaaFJTemesaEMoldesMPenaAValdesLBronchogenic carcinoma presenting as pleural empyemaRespir Med Ext200624139140
- KoikeTTakizawaTAkamatsuHYuuzouKYokoyamaAHonmaTResection of lung cancer complicated by pleural empyemaNihon Kyobu Shikkan Gakkai Zasshi1995336670673 Japanese7666625
- GrivennikovSIGretenFRKarinMImmunity, inflammation, and cancerCell2010140688389920303878
- LeePCHuYWHungMHThe risk of cancer in patients with benign anal lesions: a nationwide population-based studyAm J Med2013126121143.e9e18
- TengCJHuYWYehCMChenTJLiuCJCancer risk in patients with empyema: a nationwide population-based studyMedicine (Baltimore)2016959e293426945399
- PesantiELImmunologic defects and vaccination in patients with chronic renal failureInfect Dis Clin North Am200115381383211570143
- SarnakMJJaberBLPulmonary infectious mortality among patients with end-stage renal diseaseChest200112061883188711742917
- BermanSJJohnsonEWNakatsuCAlkanMChenRLeDucJBurden of infection in patients with end-stage renal disease requiring long-term dialysisClin Infect Dis200439121747175315578394
- ChenCHHsuWHChenHJDifferent bacteriology and prognosis of thoracic empyemas between patients with chronic and end-stage renal diseaseChest2007132253253917699132
- HirayamaANoronha-DutraAAGordgeMPNeildGHHothersallJSUremic concentrations of guanidino compounds inhibit neutrophil superoxide productionKidney Int Suppl200178S89S9211168990
- ShenTCChenCHWangIKRisk of empyema in patients with end-stage renal disease: a nationwide propensity-matched cohort studyQJM2017110742543028062748
- HsiehCYChenCHLiCYLaiMLValidating the diagnosis of acute ischemic stroke in a National Health Insurance claims databaseJ Formos Med Assoc2015114325425924140108