Abstract
COPD is a worsening condition that leads to a pathologic degeneration of the respiratory system. It represents one of the most important causes of mortality and morbidity in the world, and it is characterized by the presence of associated comorbidity. This article analyzes gastroesophageal reflux disease (GERD) and low back pain (LBP) in patients with COPD and tries to produce anatomo-clinical considerations on the reasons of the presence of these comorbidities. The considerations of the authors are based on the anatomic functions and characteristics of the respiratory diaphragm that are not always considered, from which elements useful to comprehend the symptomatic status of the patient can be deduced, finally improving the therapeutic approach. The information contained in the article can be of help to the clinician and for physiotherapy, and to all health professionals who gravitate around the patient’s care, improving the approach to the diaphragm muscle.
Keywords:
Introduction
COPD is a worsening and chronic condition that leads to a pathologic degeneration of the respiratory system. It represents one of the most important causes of mortality and morbidity in the world and is characterized by the presence of many associated comorbidities.
Relapses of the disease during the life of the patient and the comorbidity impoverish clinical results, lengthening the time of hospitalization and worsening the quality of life (QOL).Citation1 It is reported that between 51% and 88% of patients with COPD have at least one comorbidity such as, for example, cardiovascular pathologies, arthritis, osteoporosis, diabetes and chronic pain.Citation1,Citation2
The mechanisms that cause these comorbidities and the precise relation with the presence of COPD are not entirely clear.Citation3
Probably, the systemic inflammatory nature of the disease favors the natural course of these comorbidities, which reflect the systemic roots of COPD.Citation3
Gastroesophageal reflux disease (GERD) is a comorbidity often found in patients. It has the potential of exacerbating the symptoms, increasing the number of events of hospitalization.Citation3
The prevalence of GERD varies between 7.7% and 37%, of which 58% of the cases are asymptomatic.Citation3,Citation4
Nonspecific low back pain (LBP) is another comorbidity present in patients with COPD, with a percentage that varies between 41.2% and 69%.Citation2,Citation5 The percentages of LBP are similar to the ones of a population in the absence of respiratory pathologies, but the level of pain registered in the presence of COPD is higher.Citation2
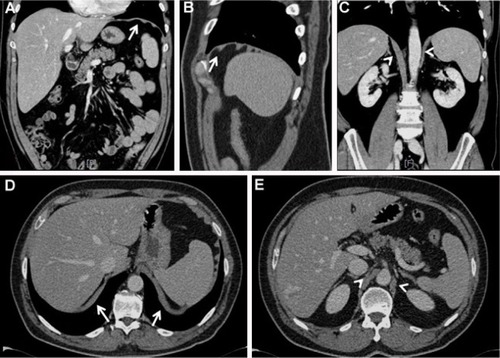
At the moment, there is no direct relation recognized as absolutely valid that could explain the presence of GERD, LBP and COPD.Citation2,Citation5 In the scientific landscape, we do not have enough information to correlate the function of the diaphragm in patients with COPD and such a comorbidity. As described subsequently, we have a lot of information on dysfunction of the respiratory muscle. This article analyzes GERD and LBP in patients with COPD and tries to produce anatomo-clinical considerations on the reasons of the presence of these comorbidities and dysfunction of the diaphragm (). The considerations of the authors are based on the anatomic functions and characteristics of the respiratory diaphragm not always considered, from which elements useful to comprehend the symptomatic status of the patient can be deduced. The article can be of help to better understand the functioning of the diaphragm muscle, helping the clinician, physiotherapist and osteopath for the rehabilitative organization.
Figure 1 CT images.
Abbreviation: CT, computed tomography.
The text represents the first step in a series of other articles, where it will try to decipher the causes of other comorbidities, associating them with the presence of diaphragmatic dysfunction.
GERD and COPD
The esophagogastric junction (EGJ) is a mutual collaboration among different anatomic parts to allow the correct functioning between the esophagus, the diaphragm and the stomach. It consists of the esophagus that crosses the diaphragmatic hiatus to reach the stomach. In EGJ, we can identify the lower esophageal sphincter (LES), the diaphragmatic hiatus and the gastric cardia, which constitute the distal part of the EGJ high-pressure zone.Citation6 LES is a segment of 3–4 cm constituted by smooth muscle; its tone in relation to the intragastric pressure in healthy individuals is 10–30 mmHg.Citation6
Throughout the day, LES endures large pressure variations managed by a complex neurologic mechanism, which involves the central nervous system, and the enteric, sympathetic and vagal systems.
We observe vagal afferences and sympathetic/vagal efferences; vagal efferences are mediated by the neurons of the myenteric plexus through cholinergic synapses.Citation6
These transient relaxations of the tone of LES can be noticed in healthy individuals and in patients with GERD. Its mechanism is stimulated by the vagal afferences of the gastric cardia. The most important trigger of this mechanism is gastric distension. This way, the dorsal motor neurons of the vagal nuclei are stimulated. Their efferences relax the tone of LES, while the esophagus shortens and the diaphragmatic hiatus is inhibited.Citation7 This relaxation stimulates the GERD.
The frequency of this mechanism is similar between healthy individuals and patients with GERD; the difference stands in the quantity of reflux, which doubles in patients with GERD.Citation7
The gastric cardia, where the side wall of the esophagus meets the medial dome of the stomach (called angle of His), looks like a crease and facilitates an increase in intragastric pressure.Citation6
The crura of diaphragm (that surrounds the LES) represent the extrinsic sphincter of the EGJ complex. We will better analyze the topic of the diaphragmatic area in the section dedicated to diaphragm.
The most common causes that determine the presence of GERD are hiatus hernia, positive pressure between the stomach and the esophagus, delayed gastric emptying, inadequate esophageal cleanliness (peristalsis, salivary bicarbonate) and esophageal trauma.Citation7
Other causes can be traced back to peripheral sensitization due to the constant stimulation of inflammatory mediators (pepsin, bile, ATP, cytokines, hydrochloric acid, histamine), lowering the afferential vagal and nociceptive threshold. This reduction increases the permeability to cations of pain receptors, with the appearance of primary hyperalgesia; with time, other nociceptors are activated, such as acid-sensing ion channels, transient receptor potential V1 and P2X purinoceptors (ATP-gated ion channel).Citation7
This scenario would lead to phenomena such as secondary hyperalgesia and allodynia, with central sensitization due to the persistent involvement of medullary neurons and cerebral areas, with the involvement of the neuropsychoimmune system.Citation7
GERD, like COPD, becomes a systemic pathology
The reflux is a risk factor for reaggravation in patients with COPD.Citation1,Citation8,Citation9
One of the causes could be traced back to silent bronchial microsuction, causing bacterial colonization and inflammatory reactions, and bronchoconstriction caused by esophagobronchial reflexes.Citation9
Using a noninvasive method to evaluate the pH of breathing in patients with COPD, the exhaled breath condensate, the presence of pepsin in higher quantities than in individuals without respiratory pathologies has been demonstrated.Citation10 Pepsin was found in the bronchi of 88% of 42 patients without COPD, but with GERD, using a bronchial lavage fluid.Citation8 Pepsin is a gastric enzyme derived from the aspartate protease family and is secreted by the cells of the epithelium of the gastric fundus.Citation8
The clinical difficulty in noticing GERD stands in the fact that patients often do not show the classic symptoms (heartburn or regurgitation) and can be unaware of suffering from reflux.Citation3,Citation7,Citation11
This clinical deficiency leads to a further lowering of the health-related QOL, an evaluation tool to measure the QOL of patients with chronic diseases, which is already low in patients with COPD.Citation12 The frequency scale for the symptoms of GERD (FSSG) allows to evaluate not only the usual symptoms (heartburn or regurgitation) but also the unusual ones such as gastric dysmotility (swollen stomach).Citation4 FSSG applied to patients with asthma and COPD revealed that the most relevant symptom of patients with COPD was gastric dysmotility; the scale also highlighted a higher exacerbation of the symptoms in patients with COPD.Citation4
One of the possible causes of these microaspirations is a pathologic alteration of the vagal laryngeal/pharyngeal reflex with diminished laryngopharyngeal mechanosensitivity.Citation11 Another possible factor responsible for the aspiration could be traced back to the incoordination between the action of swallowing and the respiratory act. In healthy individuals, swallowing usually takes place at the end of inhalation or during exhalation, lowering the risk of inhaling solid material; furthermore, deglutition preferentially takes place when lung volumes are above the residual functional capacity.Citation11 In patients with COPD, deglutition generally takes place during inhalation, increasing the risk of worsening the symptom picture.Citation11
Medicines such as beta-agonist bronchodilators lower the tone of LES in patients with COPD, decreasing the function of the anti-reflux barrier.Citation4,Citation13 Other medicines, such as theophylline and inhaled steroids, increase the reflux, but we still do not know the exact mechanisms that regulate these processes.Citation4
Another observation to make is the entity of hypoxia and of bronchial obstruction with the seriousness of GERD in patients with COPD. Ventilation influences the quality of the bloodstream toward the gastric mucosa and the pH of the mucosa. The presence of COPD has harmful effects on the integrity of the mucosa, especially if the respiratory pathology is longstanding.Citation4 This could increase the reflux.
LBP and COPD
LBP is the most common and painful condition one can suffer from over the course of their life; it is estimated that 84% of the world population suffers from LBP at least once.Citation14 It is classified as acute within 6 weeks from the moment it appears, subacute between 6 and 12 weeks and chronic after the 12th week.Citation14 There are multiple and often concomitant causes, from the emotional sphere to the visceral and somatic sphere. Depression and anxiety caused by the pain can create a vicious circle and increase the painful sensation, causing sleep deprivation.Citation15 LBP can develop after a previous surgery, even though the causes that produce the pain are still not completely clear.Citation16 In some cases, the visceral sphere (viscero-somatic reflex) could be an important contributory cause for the development of LBP.Citation17,Citation18 The viscero-somatic reflexes that reach the nervous system through neural and humoral pathways can be subdivided into two groups. The first one concerns the visceral afferent information that leads to motivational information (satiety, nausea, thirst and so on) and respiratory sensations, traveling through the vagus nerve and the glossopharyngeal nerve, reaching the nucleus of the solitary tract, which will then project it to the hypothalamus, to the ventro-lateral medulla and the parabrachial nuclei with connections with the periaqueductal gray area, the thalamus, the amygdala, the insular cortex and other areas of the cortex.Citation19 The second group consists of visceral afferences that project themselves on the dorsal horn, through lamina 1, constituting the spinothalamic tract and sending information on the local organ functioning, for example, data on pain and heat.Citation19 Lamina 1 receives information from the sympathetic system, other than from the skin and the epithelial mucosae.Citation20 Visceral afferences tend to predominate in nerves of the parasympathetic type and are present in smaller percentages in the sympathetic system, even though they act in perfect harmony; however, visceral painful information travels through the sympathetic system.Citation21 There are multiple main somatic causes linked to direct alterations of the vertebral structure: spinal disc herniation with the involvement of the root, spinal stenosis, spondylolisthesis, fractures, facet joint syndrome and sacroiliac joint syndrome, entrapment of the nerve in myofascial structures and myofascial syndrome.Citation22 Alterations of the skin, such as scars of previous trauma or abdominal surgeries, could cause entrapment of the nerves, derived from the lumbar and sacral plexus, and chronic pain.Citation23 Changes in the physiologic lumbar lordosis that persist after a pregnancy are another cause of LBP.Citation24
The presence of pain is related to the respiratory function (forced expiratory volume in 1 second) in patients with a high percentage of localization in the lumbar area.Citation25 The possible causes are multifactorial, and the presence of many comorbidities can exacerbate the feeling of pain.Citation2
The percentage of osteoporosis is from two to five times higher in patients with COPD than in patients with osteoporosis, but without limitations of the air flow.Citation26,Citation27 LBP in this population of patients could often be related to vertebral compression due to a fracture (collapse), with a concomitant reduction of the vital capacity and the forced expiratory volume in 1 second.Citation26 This reduction could be linked to the postural change that follows the vertebral collapse, with hyperkyphosis and reduction of lung volumes, with the progression of the disease and increase in mortality.Citation26,Citation27 It is not easy to link LBP to COPD. In fact, even though vertebral compression is common in patients with osteoporosis and worsening respiratory disease, the collapse remains unrecognized in at least half of the patients. The lack of experience of the patients in correctly identifying lumbar pain as a fracture probably leads to nonidentification of the problem.Citation27
Another probable cause of the presence of LBP is neuropathic pain. The cytokines produced and their activation in a systemic condition such as COPD could create the basis for chronic and neuropathic pain in patients with COPD.Citation28 The local inflammatory response is perpetuated not only at a pulmonary level but also to distant tissues, thanks to circulation. Tumor necrosis factor-alpha has been demonstrated to stimulate the phenomenon of mechanical allodynia, lowering the threshold of the endings of the fiber of type C.Citation28 Interleukin-1b, just like interleukin-6, is considered a key cytokine to create the conditions for hyperalgesia.Citation28 Dyspnea and pain activate common brain areas such as anterior insula and medial insula, anterior cingulate cortex, somatosensory cortex and motor cortex, amygdala and thalamus.Citation28 Patients with chronic dyspnea and persistent stress of the mentioned brain areas could probably change some zones of pain perception, causing sensitization that could lead to allodynia and neuropathic pain.Citation28
The previously mentioned postural change alters the muscular dynamics and the range of motion of the rib cage and the lumbar area; it limits the degrees of movement. This leads to a higher muscular fatigue for the diaphragm and the associated musculature (thorax and spine), creating an inflammatory environment and microlacerations of the contractile districts of the lumbar area. These muscles are more prone to overuse injury and with presence of delayed onset muscle soreness.Citation28 This inflammation probably worsens the neuropathic conditions. The fear and anxiety of feeling the pain or dyspnea limits the activities of daily life, creating a vicious circle in the limitation of movement.Citation28,Citation29
The diaphragm plays a key role in lumbar posture, and its functional decline leads to LBP.Citation5 Patients with COPD show diaphragmatic fatigue and less postural control, increasing the possibility of falling and of the development of LBP. The diaphragm looks flattened, with a less range of motion and altered breathing schemes in comparison with those of individuals without COPD.Citation5 Hyperinflation forces the diaphragm to work more, leaving out its postural functions, thereby causing imbalances in the bodily oscillations during ambulation, with incorrect distribution of the loads on the lumbar spine and LBP.Citation5,Citation30 In patients with COPD, the reaction of the diaphragm to the movements of the limbs is delayed or absent in comparison with that of healthy individuals, further suggesting lumbar spinal instability and the onset of LBP.Citation31
During the long period of administration, oral corticosteroids have been demonstrated to be a cause of LBP with vertebral fractures following osteoporosis and muscle weakness, creating a vicious circle of pain and lumbar functional impairment.Citation32
Another trigger of LBP in patients with COPD could be pulmonary hypertension. Some patients complain of pain in the lumbar area that occurs in the presence of lumbar spinal stenosis and only at night. Lumbar stenosis is derived from congenital malformations or progressive degeneration of lumbar vertebrae. In patients with COPD, a low right ventricular capacity secondary to diastolic dysfunction or a rise of intrathoracic pressure could lead to an increase of the right atrial pressure; this would cause a rise in pressure (and volumes) of venous return.Citation33 The increase of venous pressure has repercussions on smaller veins, stretching the epidural venous plexus near the roots, triggering nocturnal symptoms of brain ischemia.Citation33
Development of the diaphragm and its innervation
Even though the diaphragm makes up <5% of the total body weight, it is the most important contractile muscle, after the cardiac muscle.Citation34
The diaphragm is derived from progenitor mesodermal cells that become myoblasts, then melt into myotubes and later into myofibers; it is highly probable that myoblasts migrate from cervical somites (region of the brachial plexus) and reach pleuroperitoneal cavities, where they radiate in a mesenchymal substrate.Citation35 Another factor that could determine the maturation and function of the diaphragm is the phrenic nerve. The neural control of the diaphragm begins in the perinatal period, and this neural influence determines the maturation process of the myotubes into myofibers, probably thanks to electrical activity and to the neurotrophic factors transported by the nerve.Citation35
The development of the diaphragm takes place between the 7th and 10th weeks; other than the pleuroperitoneal cavities, we can identify the transversal septum and the dorsal mesentery of the esophagus as precursors of the muscle.Citation36 The transversal septum is a frontal structure that becomes the central tendon; the dorsal mesentery (which contains the primary aorta, the inferior vena cava and the esophagus) becomes the posteromedial part.Citation36 The pleuroperitoneal cavities (made up of what would be the pleural and pericardial tissue) will melt with the rest of the pre-diaphragmatic structures.Citation37 There is a close biunivocal relation of mutual cooperation in the development of the diaphragm and the phrenic nerve; myotubes grow and develop in parallel to the phrenic axonal growth.Citation38 During embryonal development, some phrenic pre-axons exit the cervical area and unite in one single nerve, guiding myogenic precursors toward the pleuroperitoneal cavities (pre-diaphragm); the axon of the nerve is surrounded by myoblasts.Citation35 The nerve only starts to ramify when the structure that would become the diaphragm starts to caudally go down the enlargement of the heart and the lungs.Citation38 The phrenic nerve influences the shape and function of the diaphragm.Citation38 Phrenic neurons are thought to be derived from the hypaxial motor column (located at a spinal level).Citation39
The relation between the vagus nerve and the diaphragm in their development is still obscure, and the vagus nerve has been recently found to play a role in the contractile function of the muscle.Citation40–Citation42
We have no data on when and how the vagus nerve penetrates the diaphragm. The vagus nerve originates from the neural crests, in particular, from somites 1–7; from these areas, enteric neurons are born as well.Citation43 These cells probably leave the neural tube in the ventral direction, since the neurons that form for the enteric system and the peripheral nervous system start their migration in a ventral direction.Citation43 Probably, again, vagus nerves that are located at the sides of the primitive intestine will form branches specialized for the diaphragm. It is important to highlight that the crural region of the diaphragm is derived from the mesentery of the esophagus; the same region is later innervated by the vagus nerve.Citation44
Diaphragm, GERD and new considerations
The crural region of the diaphragm or the extrinsic sphincter of the EGJ complex is not involved in the actions of the breath, but it is influenced by crural mecharenoceptors and gastric distension.Citation44 When the alimentary bolus has to enter the stomach, the crura stop their electric activity, while in the absence of alimentary bolus, they contract together with the rest of the diaphragm during respiratory acts.Citation44,Citation45
This short cessation probably derives from vagal afferences that specifically control the crural area, inhibiting bulbar neurons activated during respiration, and from the direct intervention of esophageal myoenteric neurons.Citation44 The position of the diaphragm is important for the behavior of the crural area and the esophagus. During unforced inhalation, the crura becomes horizontal in comparison with the inclined starting position, with an increase in its diameter and in the diameter of the esophagus.Citation46 If inhalation is forced, there is a shrinkage of the esophageal diameter, caused by the shrinkage of the crus itself due to the major contraction of the muscular fibers of the pillars of the diaphragm.Citation46 The lumbar pillars are considered as important elements for an effective anti-reflux barrier; from their lumbar tendinous insertion (right and left), they go back to the diaphragm, forming an “8” for the passing of the aorta first and of the esophagus later.Citation46,Citation47 In particular, the right pillar fuses with the edge of the central tendinous part of the diaphragm.Citation46 The back wall of the esophagus leans on the anterior and inferior surfaces of the fibers of the left pillar, while he anterior esophageal area is partially covered by a part of the right pillar; this anatomic arrangement creates a physiological costraint.Citation46
The diaphragm of patients with COPD is generally more horizontal, with shorter inhalations and longer exhalations.Citation48–Citation50 We suppose that a smaller lowering of the diaphragm in patients with COPD keeps the diameters of the crura and of the esophagus wider, favoring the presence of GERD.
Not all patients with a respiratory pathology suffer from GERD
This is probably due to the presence of some muscular components of the diaphragm, which are not noticed always: the muscle of Low and the transverse intertendinous muscle. The first one, of maximum width 15 mm, originates from the left medial area of the left pillar. It goes toward the upper fibers of the right pillar, passing behind the esophageal crura; going forward, it crosses the fibers of the crura on the right, touching the hiatus of the vena cava and fusing with the fibers that constitute the crura itself, in the upper part.Citation51 It is another small “8” that starts from the left lumbar area.
Behind the muscle of Low, the transverse intertendinous muscle links the two sides of the crura inferiorly and posteriorly.Citation51
During normal inhalation, when the crura become horizontal and wider, just like the esophageal diameter, these two muscles contract, narrowing the inferior esophageal lumen.Citation51 We suppose that the presence of these components of the diaphragm, despite its flatter and more horizontal position, makes it possible to manage the reflux better. We have no data about this.
The crural area of the diaphragm is less toned in patients with GERD than in individuals without GERD.Citation52 We suppose that another cause of the presence of chronic reflux in patients with COPD is a diminished crural muscle tone, which does not guarantee an efficient anti-reflux barrier.Citation53
Other structures that play a role in managing the reflux are the phrenoesophageal ligaments or the phrenoesophageal membrane or the membrane of Laimer. The LES, located inside the diaphragmatic esophageal hiatus, and the diaphragmatic crura (that surround the LES) represent the intrinsic and extrinsic sphincters, respectively; they are anatomically superimposable and firmly attached to one another through the phrenoesophageal ligaments.Citation54
This very thin membrane (1 or 2 mm) on the diaphragm is the continuation of the transverse fascia, which fuses with the endothoracic fascia and acts as a bridge between the crura and the esophageal wall (tunica externa and submucosa of the esophagus); under the diaphragm, it is located between the crura and the esophagus (esophageal tunica), and it reaches the angle of His.Citation55
The membrane is richly innervated and vascularized, and it contains plenty of lymphatic vessels; it is an elastic tissue with smooth muscular cells, fibroblasts and elastin.Citation55 There is a hypothesis that this membrane can act as an elastic brake for the repositioning of the esophagus with breathing, thanks to its elastic hysteresis, helping to manage the anti-reflux barrier.Citation55 The membrane is innervated by the vagus nerve which, from the elastic tissue, sends mechanical afferences on the distortion that the external and internal sphincters endure.Citation56 There is a triangular space between the esophagus and the crura (paraesophageal space); it is known that hyperinflation alters the natural position of the crura, probably shifting the esophagus upward with translation toward the left (exploiting this space), compromising the function of the phrenoesophageal membrane.Citation11 This scenario could alter the vagal afferences, which follow the same afferences of the respiratory tract and then converge and reach the solitary nucleus in the medulla oblungata.Citation11,Citation57 This afferential alteration could increase the tone of the fascial membrane (through cholinergic routes).Citation58 A closed circuit of non-physiological afferences would form. These afferences would continuously disturb the functional balance between the two sphincters (esophagus and diaphragm).
It is also important to consider the relation between the duodenum and the diaphragm. There is not enough data on the duodenal function and the presence of GERD in COPD.
A muscle stripe coming from the diaphragm, called Hilfsmuskel muscle, moves from the inferior area of the diaphragmatic crura to the arterial celiac trunk or to the superior mesenteric artery, with a close relation to the retropancreatic fascia or the Treitz’s fascia; the latter leans in the upper part on the duodenum.Citation59,Citation60 This muscle stripe is innervated by the phrenic nerve.Citation60 With a bridge of connective tissue, it fuses with the ligament of Treitz or suspensory muscle of duodenum near the arterial celiac trunk or the mesenteric artery.Citation60 The triangle-shaped ligament of Treitz originates from the duodenum or from the duodenojejunal flexure.Citation58,Citation60 Unlike the Hilfsmuskel muscle, made up of contractile fibers, the ligament of Treitz has a strong component of smooth musculature.Citation60
The Hilfsmuskel muscle contrasts the traction of the ligament of Treitz, while the latter has the task of keeping both the small intestine and the C-shape of the duodenum in place.Citation60,Citation61 An alteration of the tensional balance between the two muscles could be a contributory cause of the reduction in blood provision to the diaphragm, demonstrated by the increase in oxidation and by the fall in pressure of microvascular oxygen (PO2).Citation62,Citation63 It could also increase the esophageal reflux, because the tensional alteration of the balance between the two muscles could determine an increase of the duodenal kinesia with hypersecretion, like it happens in patients with GERD. This would determine a reflux coming from the stomach and the duodenum.Citation64 The ligament of Treitz is innervated by the sympathetic celiac and superior mesenteric plexus.Citation60 Its traction, caused by the flattening of the diaphragm, could create a dyskinesia of the esophagus caused by altered shared (esophagus and ligament of Treitz) sympathetic afferences.Citation65 We do not have enough data to substantiate these hypotheses.
An important element that deserves attention is the fascial system that involves the diaphragm, the esophagus and the lungs. The fascial continuum has many properties, for example, it can organize the mechanical tensions of all the body districts, viscera included, influencing their functional expression.Citation66–Citation68 The respiratory diaphragm not only affects the biochemical expression of the body, but, through the fascial system, also influences faraway anatomic areas with its behavior, as already explained in previous reports.Citation69,Citation70 The diaphragm acts as a bridge between the endothoracic fascia in the upper part and the transverse fascia in the lower part.Citation69,Citation70 It is known that, in the presence of COPD, the pulmonary parenchyma loses its elasticity and elastic hysteresis, becoming fibrous and stiffer, influencing negatively the elastic behavior of the pleurae.Citation71 The parietal pleura is covered by the endothoracic fascia, which fuses with the diaphragm and the phrenoesophageal ligaments.Citation55 The diaphragm suffers from lung stiffening, flattening and changing its physiological position, with probable mechanical sub-diaphragmatic fascial tension that has repercussions on the transverse fascia and the phrenoesophageal ligaments.
The esophagus itself is fascially attached to the diaphragm and to the pleurae, not only to allow better movement among different districts but also to preserve its own positional identity.Citation72,Citation73
It is known that when the phrenoesophageal ligaments lose their elasticity, for example, with aging or in the presence of a hiatal hernia, they change their intrinsic structure (fibrillar disorganization, infiltration of adipose cells) and become longer, thinner and more fragile, finally losing their function.Citation74
We suppose that the presence of GERD is also related to a mechanical alteration of the fascial system, caused by pulmonary fibrosis, which has negative effects on the function of the ligaments and on the behavior of the esophagus.
GERD is a systemic pathology and, as such, it must not be treated locally only. When a disease becomes systemic, other diseases appear, making the patient difficult to manage. In these cases, the collaboration of different specialists is fundamental for the clinical approach to the patient.
Diaphragm, LBP and new considerations
When the diaphragm lowers during the respiratory act, the fibers shorten and pull caudally the central connective area, expanding the thorax like a piston; the domes lower, pushing the viscera downward and raising the abdominal pressure.Citation34 The high pressure created forces the last ribs to rotate outward, increasing the lateral expansion of the ribcage; the rotation allows an increase of the muscular tension and a better elastic hysteresis during exhalation.Citation34,Citation75 The abdominal pressure during inhalation creates a “sleeve” that tightens around the lumbar spinal area, stabilizing the spine and diminishing the electrical intervention of the spinal musculature.Citation76 In patients with COPD, this happens to a smaller extent because of the flattening of the diaphragm and of its expiratory attitude; the muscle lowers at a lesser percentage (creating less abdominal pressure) and there is less contractile proprioceptive control.Citation76 Normally, the increased abdominal pressure is compensated by the decreased pulmonary pressure; in patients with COPD, there is an increase of lung volumes and reduced abdominal pressure.Citation76,Citation77 This pathologic mechanism causes increase in lumbar lordosis.Citation77
Considering what has been described up to now, we may suppose that an alteration of the lumbar structure and biomechanics is able to alter the function of the diaphragmatic pillars. With the diaphragm in exhalation position and the lumbar arch more accentuated, there could be a constant strain of the pillars, causing loss of their function (diminished muscle mass and proprioception).
Not only would the problem of LPB worsen, but, probably, a positional and functional malfunction of the pillars could also worsen or determine the problem of the reflux.
Lumbar hyperlordosis causes a decrease of ~20% of the sliding of the different dorsolumbar fascial layers in patients with LBP.Citation78 This decreased tissue excursion creates the conditions for the increase in fascial nociceptive afferences in higher percentage in comparison with the decreased/altered movement of the local muscles.Citation78 The fascial structures become more sensitive to mechanical stimuli and, after a few days of local inflammation, they are able to generate an action potential similar to the initial stimulus causing the dysfunction; this potential can have an anterograde and retrograde propagation, causing inflammation at the extremities of the neural tract, such as in the spinal cord and in the innervated tissues. This mechanism is called ectopic electrogenesis.Citation79 We suppose that LBP in patients with COPD is also caused by the fascial system, despite not having any data that can substantiate this statement.
When one takes charge of a patient, they must consider not only the pulmonary pathology but also, as a routine, different comorbidities, such as GERD and LBP, and evaluation of all the diaphragmatic components. This, in a multi-disciplinary approach, could turn out to be a more efficient therapeutic approach.
LBP is a pathologic condition and not just a symptom. From what is described in the report, it is evident that diaphragm is an important muscle and can become the keystone for rehabilitation and understanding this problem.
Conclusion
COPD is a systemic pathology characterized by the presence of comorbidity. This study analyzed the causes of GERD and LBP recognized by scientific literature. The text took into consideration other mechanisms that could cause reflux and lumbar pain, making hypotheses of different clinical scenarios emphasizing the functions of the diaphragm. These observations are based on the functions and anatomic characteristics of the respiratory diaphragm which are not always considered.
The authors have tried to bring evidence from other scientific disciplines (gastroenterology, biomechanics and anatomy) on the causes of GERD and LBP in the presence of diaphragmatic dysfunction. An alteration of the diaphragm is present in COPD pathology. This is the first study that tries to combine pneumological knowledge with other scientific disciplines.
From this analysis, it could be possible to deduce useful elements to better comprehend the symptomatology status of the patient, finally improving the therapeutic approach in a multidisciplinary context.
Disclosure
The authors report no conflicts of interest in this work.
References
- WesterikJAMettingEIvan BovenJFTiersmaWKocksJWSchermerTRAssociations between chronic comorbidity and exacerbation risk in primary care patients with COPDRespir Res20171813128166777
- ChenYWCampPGCoxsonHOComorbidities that cause pain and the contributors to pain in individuals with chronic obstructive pulmonary diseaseArch Phys Med Rehabil20179881535154327866992
- SmithMCWrobelJPEpidemiology and clinical impact of major comorbidities in patients with COPDInt J Chron Obstruct Pulmon Dis2014987188825210449
- ShimizuYDobashiKKusanoMMoriMDifferent gastoroesophageal reflux symptoms of middle-aged to elderly asthma and chronic obstructive pulmonary disease (COPD) patientsJ Clin Biochem Nutr201250216917522448100
- BeeckmansNVermeerschALysensRThe presence of respiratory disorders in individuals with low back pain: a systematic reviewMan Ther201626778627501326
- KahrilasPJLeeTJPathophysiology of gastroesophageal reflux diseaseThorac Surg Clin200515332333316104123
- BoeckxstaensGERohofWOPathophysiology of gastroesophageal reflux diseaseGastroenterol Clin North Am2014431152524503356
- PomariCMauronerLPaianoSBronchial reacutization and gastroesophageal reflux: is there a potential clinical correlation?Ann Transl Med201641630427668224
- LinYHTsaiCLChienLNChiouHYJengCNewly diagnosed gastroesophageal reflux disease increased the risk of acute exacerbation of chronic obstructive pulmonary disease during the first year following diagnosis – a nationwide population-based cohort studyInt J Clin Pract201569335035725359162
- LeeALButtonBMDenehyLExhaled breath condensate pepsin: potential noninvasive test for gastroesophageal reflux in COPD and bronchiectasisRespir Care201560224425025352687
- HoughtonLALeeASBadriHDeVaultKRSmithJARespiratory disease and the esophagus: reflux, reflexes and microaspirationNat Rev Gastroenterol Hepatol201613844546027381074
- Rascon-AguilarIEPamerMWludykaPCuryJVegaKJPoorly treated or unrecognized GERD reduces quality of life in patients with COPDDig Dis Sci20115671976198021221789
- Del GrandeLMHerbellaFABigataoAMJardimJRPattiMGInhaled beta agonist bronchodilator does not affect trans-diaphragmatic pressure gradient but decreases lower esophageal sphincter retention pressure in patients with Chronic Obstructive Pulmonary Disease (COPD) and Gastroesophageal Reflux Disease (GERD)J Gastrointest Surg201620101679168227350150
- ViolanteFSMattioliSBonfiglioliRLow-back painHandb Clin Neurol201513139741026563799
- SribastavSSPeihengHJunLInterplay among pain intensity, sleep disturbance and emotion in patients with non-specific low back painPeerJ20175e328228533953
- BordoniBMarelliFFailed back surgery syndrome: review and new hypothesesJ Pain Res20169172226834497
- KingHHAddition of osteopathic visceral manipulation to OMT for low back pain decreases pain and increases quality of lifeJ Am Osteopath Assoc2017117533333428459483
- TamerSÖzMÜlgerÖThe effect of visceral osteopathic manual therapy applications on pain, quality of life and function in patients with chronic nonspecific low back painJ Back Musculoskelet Rehabil201730341942527858681
- CritchleyHDHarrisonNAVisceral influences on brain and behaviorNeuron201377462463823439117
- GiamberardinoMAAffaitatiGLerzaRLapennaDCostantiniRVecchietLRelationship between pain symptoms and referred sensory and trophic changes in patients with gallbladder pathologyPain20051141–223924915733650
- KoganezawaTShimomuraYTeruiNThe role of the RVLM neurons in the viscero-sympathetic reflex: a mini reviewAuton Neurosci20081421–2171918457999
- PetersenTLaslettMJuhlCClinical classification in low back pain: best-evidence diagnostic rules based on systematic reviewsBMC Musculoskelet Disord201718118828499364
- BordoniBZanierESkin, fascias, and scars: symptoms and systemic connectionsJ Multidiscip Healthc20137112424403836
- FrankeHFrankeJDFryerGOsteopathic manipulative treatment for nonspecific low back pain: a systematic review and meta-analysisBMC Musculoskelet Disord20141528625175885
- van Dam van IsseltEFGroenewegen-SipkemaKHSpruit-van EijkMPain in patients with COPD: a systematic review and meta-analysisBMJ Open201449e005898
- ShengSZhenzhongSWeiminJYimengWQudongYJinhuiSImprovement in Pulmonary Function of Chronic Obstructive Pulmonary Disease (COPD) Patients With Osteoporotic Vertebral Compression Fractures (OVCFs) After Kyphoplasty Under Local AnesthesiaInt Surg2015100350350925785335
- MasalaSMagriniATaglieriAChronic obstructive pulmonary disease (COPD) patients with osteoporotic vertebral compression fractures (OVCFs): improvement of pulmonary function after percutaneous vertebroplasty (VTP)Eur Radiol20142471577158524744201
- HajGhanbariBHolstiLRoadJDDarlene ReidWPain in people with chronic obstructive pulmonary disease (COPD)Respir Med20121067998100522531146
- HajGhanbariBGarlandSJRoadJDReidWDPain and physical performance in people with COPDRespir Med2013107111692169923845881
- SmithMDChangATSealeHEWalshJRHodgesPWBalance is impaired in people with chronic obstructive pulmonary diseaseGait Posture201031445646020206529
- SynnotAWilliamsMLow back pain in individuals with chronic airflow limitation and their partners – a preliminary prevalence studyPhysiother Res Int20027421522712528577
- WalshLJWongCAOborneJAdverse effects of oral corticosteroids in relation to dose in patients with lung diseaseThorax200156427928411254818
- LaBanMMKucwayEJAeolus myth: chronic obstructive lung disease and nocturnal lumbosacral pain in association with lumbar spinal stenosis and pulmonary hypertensionAm J Phys Med Rehabil200382966066412960906
- AnrakuMShargallYSurgical conditions of the diaphragm: anatomy and physiology. Surgical conditions of the diaphragm: anatomy and physiologyThorac Surg Clin200919441942920112625
- MantillaCBSieckGCKey aspects of phrenic motoneuron and diaphragm muscle development during the perinatal periodJ Appl Physiol (1985)200810461818182718403452
- MaishMThe diaphragmSurg Clin North Am201090595596820955877
- GreerJJAllanDWMartin-CaraballoMLemkeRPAn overview of phrenic nerve and diaphragm muscle development in the perinatal ratJ Appl Physiol (1985)199986377978610066685
- AllanDWGreerJJEmbryogenesis of the phrenic nerve and diaphragm in the fetal ratJ Comp Neurol199738244594689184993
- MachadoCBKanningKCKreisPReconstruction of phrenic neuron identity in embryonic stem cell-derived motor neuronsDevelopment2014141478479424496616
- NiedringhausMJacksonPGEvansSRVerbalisJGGillisRASahibzadaNDorsal motor nucleus of the vagus: a site for evoking simultaneous changes in crural diaphragm activity, lower esophageal sphincter pressure, and fundus toneAm J Physiol Regul Integr Comp Physiol20082941R121R13117977921
- NiedringhausMJacksonPGPearsonRBrainstem sites controlling the lower esophageal sphincter and crural diaphragm in the ferret: a neuroanatomical studyAuton Neurosci20081441–2506018986853
- YoungRLPageAJCooperNJFrisbyCLBlackshawLASensory and motor innervation of the crural diaphragm by the vagus nervesGastroenterology2010138310911101e1e519732773
- KuoBREricksonCAVagal neural crest cell migratory behavior: a transition between the cranial and trunk crestDev Dyn201124092084210022016183
- PickeringMJonesJFThe diaphragm: two physiological muscles in oneJ Anat2002201430531212430954
- ShafikAShafikIEl-SibaiOMostafaRMDoes the crural diaphragm share in the contractile activity of the costal diaphragm? The concept of an “autonomous esophageal crus” and its role in esophageal competenceMed Sci Monit2004108BR268BR27215277987
- CostaMMPires-NetoMAAnatomical investigation of the esophageal and aortic hiatuses: physiologic, clinical and surgical considerationsAnat Sci Int2004791213115088789
- DianboCWeiLBolducJPDeslauriersJCorrelative anatomy of the diaphragmThorac Surg Clin201121228128721477777
- BordoniBMarelliFMorabitoBSacconiBManual evaluation of the diaphragm muscleInt J Chron Obstruct Pulmon Dis2016111949195627574419
- YamadaYUeyamaMAbeTDifference in diaphragmatic motion during tidal breathing in a standing position between COPD patients and normal subjects: time-resolved quantitative evaluation using dynamic chest radiography with flat panel detector system (“dynamic X-ray phrenicography”)Eur J Radiol201787768228065378
- SalitoCLuoniEAlivertiAAlterations of diaphragm and rib cage morphometry in severe COPD patients by CT analysisConf Proc IEEE Eng Med Biol Soc201520156390639326737755
- DowneyRAnatomy of the normal diaphragmThorac Surg Clin201121227327921477776
- LoukasMWartmannChTTubbsRSMorphologic variation of the diaphragmatic crura: a correlation with pathologic processes of the esophageal hiatus?Folia Morphol (Warsz)200867427327919085868
- KahrilasPJAnatomy and physiology of the gastroesophageal junctionGastroenterol Clin North Am19972634674869309398
- da SilvaRCde SáCCPascual-VacaÁOIncrease of lower esophageal sphincter pressure after osteopathic intervention on the diaphragm in patients with gastroesophageal refluxDis Esophagus201326545145622676647
- KwokHMarrizYAl-AliSWindsorJAPhrenoesophageal ligament re-visitedClin Anat199912316417010340456
- YoungRLPageAJCooperNJFrisbyCLBlackshawLASensory and motor innervation of the crural diaphragm by the vagus nervesGastroenterology201013831091110119732773
- LinzDHohlMVollmarJUkenaCMahfoudFBöhmMAtrial fibrillation and gastroesophageal reflux disease: the cardiogastric interactionEuropace2017191162027247004
- UndemBJKollarikMThe role of vagal afferent nerves in chronic obstructive pulmonary diseaseProc Am Thorac Soc20052435536016267362
- YangJDIshikawaKHwangHPMorphology of the ligament of Treitz likely depends on its fetal topographical relationship with the left adrenal gland and liver caudate lobe as well as the developing lymphatic tissues: a histological study using human fetusesSurg Radiol Anat2013351253822777511
- JitIGrewalSSThe suspensory muscle of the duodenum and its nerve supplyJ Anat1977123Pt 2397405870476
- MasoudGHossainSBahmanRZeinabKFatemehANew look at about nature, structure and function of Trietz ligamentAdv Biomed Res201436924627877
- ScheibeNSosnowskiNPinkhasikAVonderbankSBastianASonographic evaluation of diaphragmatic dysfunction in COPD patientsInt J Chron Obstruct Pulmon Dis2015101925193026392767
- PooleDCKindigCABehnkeBJEffects of emphysema on diaphragm microvascular oxygen pressureAm J Respir Crit Care Med200116351081108611316639
- DzhulayGSSekarevaEVGastric and duodenal secretory and motor-evacuatory activity in patients with gastroesophageal reflux disease associated with different types of refluxTer Arkh20168821620 Russian
- SpencerNJZagorodnyukVBrookesSJHibberdTSpinal afferent nerve endings in visceral organs: recent advancesAm J Physiol Gastrointest Liver Physiol20163116G1056G106327856418
- BordoniBMarelliFEmotions in motion: myofascial interoceptionComplement Med Res2017242110113 German28278494
- BordoniBMarelliFThe fascial system and exercise intolerance in patients with chronic heart failure: hypothesis of osteopathic treatmentJ Multidiscip Healthc2015848949426586951
- BordoniBZanierEClinical and symptomatological reflections: the fascial systemJ Multidiscip Healthc2014740141125258540
- BordoniBZanierEThe continuity of the body: hypothesis of treatment of the five diaphragmsJ Altern Complement Med201521423724225775273
- BordoniBZanierEAnatomic connections of the diaphragm: influence of respiration on the body systemJ Multidiscip Healthc2013628129123940419
- BurgessJKMauadTTjinGKarlssonJCWestergren-ThorssonGThe extracellular matrix – the under-recognized element in lung disease?J Pathol2016240439740927623753
- WeijsTJGoenseLvan RossumPSThe peri-esophageal connective tissue layers and related compartments: visualization by histology and magnetic resonance imagingJ Anat2017230226227127659172
- SteccoCSfrisoMMPorzionatoAMicroscopic anatomy of the visceral fasciaeJ Anat2017231112112828466969
- ApaydinNUzAEvirgenOLoukasMTubbsRSElhanAThe phrenico-esophageal ligament: an anatomical studySurg Radiol Anat2008301293618058057
- VostatekPNovákDRychnovskýTRychnovskáSDiaphragm postural function analysis using magnetic resonance imagingPLoS One201383e5672423516397
- JanssensLBrumagneSMcConnellAKHermansGTroostersTGayan-RamirezGGreater diaphragm fatigability in individuals with recurrent low back painRespir Physiol Neurobiol2013188211912323727158
- KolarPSulcJKynclMPostural function of the diaphragm in persons with and without chronic low back painJ Orthop Sports Phys Ther201242435236222236541
- WilkeJSchleipRKlinglerWSteccoCThe lumbodorsal fascia as a potential source of low back pain: a narrative reviewBiomed Res Int20172017534962028584816
- BordoniBMarelliFMorabitoBSacconiBDepression, anxiety and chronic pain in patients with chronic obstructive pulmonary disease: the influence of breathMonaldi Arch Chest Dis201787181128635197
