Abstract
Purpose
COPD diagnosis is mainly based on clinical judgment of physicians. Physicians do not also refer to COPD guidelines in their daily practice. This study aimed to assess attitudes of physicians regarding COPD diagnosis, treatment, and follow-up and to identify the factors influencing physicians’ decisions in clinical practice.
Patients and methods
Fifty physicians were selected from 12 EuroStat NUTS 2 regions and asked to assess seven fictitious case scenarios. The following five scenarios described patients with COPD: Case Global Initiative for Chronic Obstructive Lung Disease (GOLD) A-smoker and Case GOLD A-nonsmoker were previously undiagnosed patients presenting with dyspnea, Case GOLD D-smoker and GOLD B-exsmoker were COPD patients presenting with exacerbation, Case GOLD B-smoker was a previously diagnosed COPD patient with dyspnea in stable phase, Case asthma–COPD overlap syndrome, and Case obesity hypoventilation syndrome. Patients’ history, physical examination findings, pulmonary function tests, and X-ray images were prepared before the study by an experts’ committee and provided to the physicians upon their request, until they reached a final decision. The physicians completed a questionnaire including information about their clinical practices and institutions.
Results
According to the GOLD 2015 recommendations, of the physicians, 44% performed guideline-concordant diagnosis in the first five scenarios, who were all COPD patients, and 6% performed guideline-concordant diagnosis in all cases. There was a negative correlation between high workload and making a guideline-concordant diagnosis (P=0.038, rho =−0.417). Even when the physicians made a guideline-concordant diagnosis of COPD, only a minority (10%–22%) used the GOLD classification. Logistic regression analysis revealed that working in a tertiary health care center was a significant factor in favor of establishing a guideline-concordant diagnosis of COPD (P=0.029, OR =6.139 [95% CI: 1.20–31.32]).
Conclusion
Management of COPD patients in Turkey does not generally follow the GOLD criteria but is rather based on physicians’ clinical experience. Heavy workload appears to adversely affect the correctness of clinical decisions.
Introduction
COPD is a global public health concern that causes significant morbidity and mortality with an increasing trend.Citation1 In 2011, age and gender standardized national prevalence rates of COPD in Turkey were reported to be 5.3% and 4.0%, respectively, when the disease was diagnosed based on pulmonary function tests (PFTs) and physicians’ assessments.Citation2 Owing to the discordance between these two rates, a practice pattern study (ALPHABET) was conducted to examine how COPD patients were evaluated in real life.Citation3 The ALPHABET study showed that the ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity was ≥70% in 40% of the patients previously diagnosed with COPD. Besides, the most common treatment regimen, which was used in 62% of COPD patients, was triple therapy, ie, the combination of long-acting β2 agonists (LABA), inhaled corticosteroids (ICS), and long-acting muscarinic antagonists (LAMA).Citation3 The same study also showed that physicians’ compliance to multidimensional assessment approach, as outlined by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) strategy, was relatively low. In a study from the United States including the records of 450 patients with COPD confirmed by spirometry, it was demonstrated that 43.6% of the patients were not receiving guideline-based treatment and, of these patients, who were all GOLD stage I, 7.6% were overtreated.Citation4 Moreover, another study from the United States reported that 23.1% of the COPD patients received a treatment that was not consistent with any of the guidelines’ recommendations irrespective of disease severity.Citation5 Based on these findings, the current study, which was called “WHY Study”, was designed to evaluate attitudes of physicians regarding COPD diagnosis, treatment, and follow-up and to identify the factors influencing physicians’ decisions in clinical practice.
Patients and methods
The present study was designed as a practice pattern survey and conducted from April to July 2015. The study was approved by the ethics committee of Dokuz Eylul University Medical Faculty (date: December 18, 2014; no: 2014/37-02). Written and signed informed consents of the physicians to participate in the study were obtained.
No actual patients were enrolled; however, fictitious case scenarios were used to represent patients with COPD. For each case scenario, demographic features, medical histories, physical examination findings, and medical and screening test results were prepared prior to the study.
Fifty physicians who were working in different tertiary (university hospitals or training and research hospitals) and secondary (state hospital or private hospital) health care centers and willing to participate in the study were included. The centers were selected from 12 provinces (Adana, Ankara, Samsun, Balikesir, Trabzon, Bursa, Izmir, Gaziantep, Istanbul, Erzurum, Kayseri, and Van) according to the European Community Regional Policies Level 2 Statistical Regional Units (EuroStat NUTS 2 regions) to provide a representative sample of Turkey. In Turkey, the tertiary health care centers are also academic centers, which have residency programs and train pulmonology fellows. These consist of university hospitals and a total of four research and training hospitals for pulmonary diseases. The secondary health care centers are state hospitals, which only provide patient care.
Case scenarios
All scenarios and related documents were produced by the steering committee of the study based on the recommendations of the GOLD document and the Turkish Thoracic Society’s COPD guideline, similar to the methodology used by Fukuhara et al.Citation6 The members of the committee were physicians with a special interest in COPD, working as consultants in academic institutions. The participants were expected to order the correct diagnostic tests, to evaluate the quality of the spirometry, to use the right parameters (level of FEV1, symptom score, and history of exacerbations) for classifying the patient, and to choose a treatment regimen that was concordant with the guidelines.
The following five scenarios described patients with COPD: Case GOLD A-smoker and Case GOLD A-nonsmoker were previously undiagnosed patients presenting with dyspnea, Case GOLD D-smoker and GOLD B-exsmoker were COPD patients presenting with exacerbation, Case GOLD B-smoker was a previously diagnosed COPD patient with dyspnea in stable phase. The remaining two cases, which are sometimes misdiagnosed and/or treated as COPD, were Case asthma-COPD overlap syndrome (ACOS) and Case obesity hypoventilation syndrome (OHS). Each case scenario included the results of medical and screening tests that are usually used in clinical practice for diagnosing COPD patients. Detailed description of the case scenarios is presented in Table S1.
The same PFT result sheet was used for all COPD cases. However, Case ACOS and Case OHS had distinctive PFT result sheets. In some cases, some tricky PFT results, compatible with a noncooperative patient, were first given to the physicians, expecting them to request an acceptable PFT result sheet. Similarly, chest X-rays of poor technical quality were also given. Thus, a patient dossier was prepared for each case scenario.
During face-to-face interviews, physicians examined the history and laboratory and radiographic findings and requested additional tests, whenever they felt a need, until they reached a decision for each of the seven case scenarios (). In these interviews, the GOLD classification of the cases was not asked to the physicians; however, they were evaluated by checking whether they asked for the correct clinical parameters to classify the patients, namely symptom scores, history of exacerbations, and FEV1 levels.
Table 1 Details of seven case scenarios
The tests requested by the physicians were recorded. There was no limitation in time for the physicians to review the cases in detail. If the physicians required more tests for decision making, the results of all required tests were given and were also recorded. Physicians were also asked to complete the “Physician Questionnaire” that included questions about their institutions, number of patients they examine in routine daily practice, years of working as a clinician, whether PFT and chest X-rays were performed in their institution, his/her routine procedures to examine a new COPD patient, and whether he/she routinely used a questionnaire to assess the symptoms and/or health-related quality of life of patients. All questionnaires were collected by the interviewers and transferred to the study center for data management.
Statistical analyses
Predictive Analytics Software for Windows Version 18.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. In descriptive statistics, categorical variables were expressed as numbers and percentages and numerical variables were expressed as median (minimum–maximum). Two-group comparisons between categorical variables were performed using the Chi-square test or the Fisher’s exact test, as required. The Spearman’s rho test statistics was used in correlations for non-normal distributed numerical data. Multivariate logistic regression analysis was performed to determine the factors affecting the guideline-concordant diagnosis. Statistical significance level was set at a P-value of <0.05.
Results
Of the 50 physicians included in the study, 31 (62%) physicians were working in a tertiary health care center and the remaining 19 physicians were working in a secondary health care center. The median number of years worked as a specialist was 7 years (range, 1–33 years), and 65.3% of the physicians had been working as a specialist for ≤10 years. The median number of patients examined daily by the physicians was 40 (range, 8–90). Spirometry was available in all institutions. Features of the physicians are summarized in .
Table 2 Features of the physicians
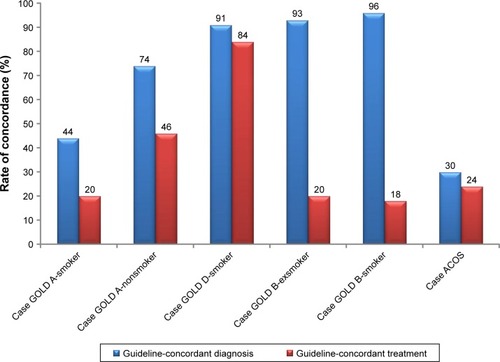
While 44% (n=22) of the physicians performed guideline-concordant diagnosis in the five COPD cases, only 6% (n=3) of the physicians performed guideline-concordant diagnosis in all seven cases (). There was a negative correlation between the workload (≥40 patient examinations per day) of the physicians and the likelihood of making a guideline-concordant diagnosis (P=0.038, rho =−0.417). There was no relationship between a guideline-concordant diagnosis and the working place (tertiary or secondary health care center) as well as the number of years worked as a specialist (P>0.05, for both). In multivariate logistic regression analysis performed to determine the factors (including gender, number of years working as a specialist, working place [secondary or tertiary health care center], and number of patients examined daily) affecting the guideline-concordant diagnosis, working in a tertiary health care center was found to be the only significant factor in favor of establishing a guideline-concordant diagnosis of COPD (P=0.029, OR =6.139 [95% CI: 1.20–31.32]).
Table 3 Summary of the results for each case
Independently from failures in the diagnosis and categorization of COPD patients, guideline-concordant treatment rates were 20%, 46%, 84%, 20%, 18%, and 24% in Cases GOLD A-smoker, GOLD A-nonsmoker, GOLD D-smoker, GOLD B-exsmoker, GOLD B-smoker, and ACOS, respectively. The guideline-concordant treatment rates for guideline-concordant diagnosed and categorized patients were 4%, 6%, 4%, 2%, and 2% in Cases GOLD A-smoker, GOLD A-nonsmoker, GOLD D-smoker, GOLD B-exsmoker, GOLD B-smoker, and ACOS, respectively. While the lowest rates for guideline-concordant diagnosis and guideline-concordant treatment were seen in Case GOLD A-smoker and Case ACOS, Case GOLD D-smoker was associated with the highest rates of correct answers () (details are presented in Table S2).
The rate of guideline-concordant diagnosis among physicians who used appropriate PFT was 38% in Case GOLD A-smoker, whereas the rates increased to 74%, 78%, 80%, and 82% in Case GOLD A-nonsmoker, Case GOLD D-smoker, Case GOLD B-exsmoker, and Case GOLD B-smoker, respectively. However, even when a guideline-concordant diagnosis of COPD was made, only a minority of the physicians (10–24%) used the GOLD classification and gave guideline-concordant treatment ().
Discussion
The present study evaluated the physicians’ behaviors on COPD management using fictitious case scenarios and showed that the patients’ characteristics influenced the physicians’ decision making. This influence was more apparent in newly diagnosed patients. The classification of the cases according to the GOLD 2015 criteria was also problematic. Besides, correct parameters were used by 10%–24% of the physicians and correct classification was performed only by 2%–6%. Moreover, only 4–7 of the physicians used the correct tools for decision making. In spite of the problems in the classification, 18%–84% of the physicians prescribed the appropriate treatment.
Although Case GOLD A-smoker and Case GOLD A-nonsmoker were newly diagnosed patients, they differed in age and smoking status, which might have led to different rates in guideline-concordant diagnosis (38% vs 74%). In contrast, Case ACOS was concordantly diagnosed by a higher proportion of the physicians. Case OHS was previously misdiagnosed and treated as COPD and was concordantly diagnosed only by eight physicians. Thus, a previous diagnosis of COPD appears to mislead the physicians to continue with the same mistake. Each new encounter should give the physicians a chance to re-evaluate their patients.
The distribution of COPD patients among the GOLD categories has been evaluated by several studies. The proportion of cases in GOLD A category is roughly between 30% and 40%.Citation7–Citation9 The national ALPHABET study reported that GOLD A and D were the two most prevalent COPD categories, comprising 41.1% and 25.0% of the patients regularly seen at secondary and tertiary health care centers.Citation3 As these were the most common categories, physicians are expected to diagnose and manage such patients appropriately in accordance with the GOLD guidelines. However, the rates of guideline-concordant diagnosis and treatment were low, possibly due to the tendency of physicians to make decisions based on their clinical experience, particularly in these low-risk groups with lesser symptoms.Citation3 In a multicenter study conducted on 4,094 patients in Italy to investigate whether pulmonologists follow the GOLD guidelines in prescribing COPD treatment, they reported that 62.1% of the patients were receiving inappropriate treatment in accordance with the GOLD recommendations.Citation10 In a study conducted to investigate the rates of adherence to GOLD 2010 guidelines for COPD treatment among pulmonologists in Turkey, overall adherence to GOLD recommendations was 59.5%.Citation11 In another study from Turkey, adherence to guideline recommendations for COPD patients was found to be 48.2%.Citation12 In the present study as well, the rate of guideline-concordant diagnosis among physicians who used appropriate PFT was 38% in Case GOLD A-smoker, while the rates increased to 74%, 78%, 80%, and 82% in Case GOLD A-nonsmoker, Case GOLD D-smoker, Case GOLD B-exsmoker, and Case GOLD B-smoker, respectively. However, even if the guideline-concordant diagnosis of COPD was performed, only a minority (10%–24%) of the physicians used the GOLD classification.
The diagnosis of COPD should be based on the evaluation of PFTs; however, several previous studies which evaluated the practice patterns of physicians to diagnose COPD have shown that clinical experience has a significant impact on diagnosis and frequently replaces spirometry. An Italian study reported that for patients examined by general practitioners, the COPD diagnosis was based on the physicians’ decisions in 30%.Citation13 Similarly, another study from Tasmania reported that 30% of the patients diagnosed with COPD had no spirometric evaluation.Citation14 Moreover, a Chinese study reported that 64.3% of the hospitals lacked spirometers for COPD diagnosis.Citation15 A more recent study from China also reported that knowledge about COPD was fairly low among general practitioners.Citation16 In a multinational study including centers from the Europe and the United States, 24% of the COPD patients reported that they had not undergone a spirometry test.Citation17 As can be seen from different population examples, PFTs are not always incorporated in the diagnosis and management of COPD in several parts of the world. The present study showed that spirometry was frequently overlooked in clinical practice in Turkey and that the physicians had problems in interpreting the results when it was performed.
It thus appears that despite educational efforts including scientific meetings, webinars, and national guidelines, important issues remain in the diagnosis and guideline-concordant management of COPD patients in Turkey. There is a strong need to re-evaluate the effectiveness of the current educational tools, to assess clinicians’ needs, and to focus more on improving the practice and clinical behavior of pulmonologists caring for COPD patients.
Another interesting finding was the relationship between workload and guideline-concordant diagnosis. The median number of patients examined by the physicians was found to be 40 per day, and with a rough calculation, the physicians had only 12 minutes per patient for examination and decision making. The workload was particularly higher in state hospitals. A recent study by Musellim et al,Citation18 however, suggested that in pulmonary practice, the average time allocated to each patient should be 20 minutes and that physicians should spare 25 minutes for patients with chronic lung disorders. In reality, however, under time constraints for each patient, physicians appear to depend more heavily on their clinical experience and possibly use preconceived templates in the evaluation and management of COPD patients. This lack of objective and individual assessment may be another explanation for the low rates of guideline-concordant diagnosis.
One of the limitations of the present study was the use of fictitious cases, which might not reflect real-life practices. However, in order to better evaluate the practice patterns, standard questions on standard clinical problems had to be directed to the physicians. Besides, the findings may be an underestimation of the problem, because the physicians would be less likely to make objective and individualized assessments of patients and be more prone to act on their reflexes due to serious time constraints and several distracting factors in the real-life setting. Another limitation could be the relatively low number of participants, which may raise concerns regarding the generalizability of the findings to the Turkish pulmonologist population. However, each participating physician was from a different medical center and each center was chosen from different provinces according to the EuroStat NUTS 2 regions and, thus, the present study population should be a representative sample.
Conclusion
To the best of our knowledge, this is the first study that evaluated the physicians’ behaviors in the process of diagnosis, treatment, and follow-up of COPD. The results of the present study revealed that the management of COPD patients in Turkey was not in accordance with the GOLD recommendations and was rather based on the physicians’ clinical experience. This appeared to be related to heavy workload. Therefore, medical associations and professional societies should put more efforts for advocacy to decrease patient burden on physicians and to improve the quality of patient care. Besides, more work needs to be done both to raise awareness of physicians on evidence-based management of COPD patients and to reflect this knowledge in their clinical practice. There is a need for further studies evaluating the effects of educational interventions on physicians’ knowledge and behavior.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Acknowledgments
We thank Clinical Research Manager Clinical Research Organization who provided editorial support and performed statistical analysis funded by Novartis Pharmaceuticals, Turkey.
Disclosure
AK is an employee of Novartis Pharmaceuticals, Turkey. The authors report no other conflicts of interest in this work.
References
- VestboJHurdSSAgustíAGGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2013187434736522878278
- Republic of Turkey Ministry of HealthAnkara: Chronic Diseases and Risk Factors Survey in Turkey2013 Available from: http://sbu.saglik.gov.tr/ekutuphane/kitaplar/khrfai.pdfAccessed October 18, 2017
- GunenHYilmazMAktasOCategorization of COPD patients in Turkey via GOLD 2013 strategy document: ALPHABET studyInt J Chron Obstruct Pulmon Dis2015102485249426622176
- SharifRCuevasCRWangYAroraMSharmaGGuideline adherence in management of stable chronic obstructive pulmonary diseaseRespir Med20131071046105223639271
- FodaHDBrehmAGoldsteenKEdelmanNHInverse relationship between nonadherence to original GOLD treatment guidelines and exacerbations of COPDInt J Chron Obstruct Pulmon Dis20171220921428123293
- FukuharaSNishimuraMNordykeRJZaherCAPeabodyJWPatterns of care for COPD by Japanese physiciansRespirology20051034134815955147
- HanMKMuellerovaHCurran-EverettDGOLD 2011 disease severity classification in COPDGene: a prospective cohort studyLancet Respir Med201311435024321803
- SorianoJBAlfagemeIAlmagroPDistribution and prognostic validity of the new global initiative for chronic obstructive lung disease grading classificationChest2013143369470223187891
- CasanovaCMarinJMMartinez-GonzalezCfor COPD History Assessment in SpaiN (CHAIN) CohortNew GOLD classification: longitudinal data on group assignmentRespir Res201415324417879
- CorradoARossiAHow far is real life from COPD therapy guidelines? An Italian observational studyRespir Med201210698999722483189
- SenEGucluSZKibarIAdherence to GOLD guideline treatment recommendations among pulmonologists in TurkeyInt J Chron Obstruct Pulmon Dis2015102657266326715844
- TuranOEmreJCDenizSBaysakATuranPAMiriciAAdherence to current COPD guidelines in TurkeyExpert Opin Pharmacother20161715315826629809
- CaramoriGBettoncelliGTosattoRUnderuse of spirometry by general practitioners for the diagnosis of COPD in ItalyMonaldi Arch Chest Dis200563161216035558
- WaltersJAHansenEMudgePJohnsDPWaltersEHWood-BakerRBarriers to the use of spirometry in general practiceAust Fam Physician200534320120315799676
- ZhengJA nationwide questionnaire survey on clinical application of pulmonary function testing in ChinaZhonghua Jie He He Hu Xi Za Zhi2002252697311953100
- LiFCaiYZhuYThe evaluation of general practitioners’ awareness/knowledge and adherence to the GOLD guidelines in a Shanghai suburbAsia Pac J Public Health2015272N2067N2078
- MenezesAMLandisSHHanMKContinuing to confront COPD international surveys: comparison of patient and physician perceptions about COPD risk and managementInt J Chron Obstruct Pulmon Dis20151015917225653515
- MusellimBBorekciSUzanGWhat should be the appropriate minimal duration for patient examination and evaluation in pulmonary outpatient clinics?Ann Thorac Med20171217718228808489