Abstract
Purpose
Hypoxemia is associated with more severe lung disease and worse outcomes. In some patients with chronic obstructive lung diseases who desaturate on exertion, supplemental oxygen improves exercise capacity. The clinical significance of this exercise response to oxygen supplementation is not known.
Patients and methods
We identified chronic obstructive lung disease patients at our center who underwent a 6-minute walking test (6MWT) for ambulatory oxygen assessment and who desaturated breathing air and therefore had an additional walk test on supplemental oxygen, between August 2006 and June 2016. Responders were defined as walking ≥26 m further with oxygen. Survival was determined up to February 1, 2017. We compared survival in oxygen responders and nonresponders in patients with obstructive lung diseases.
Results
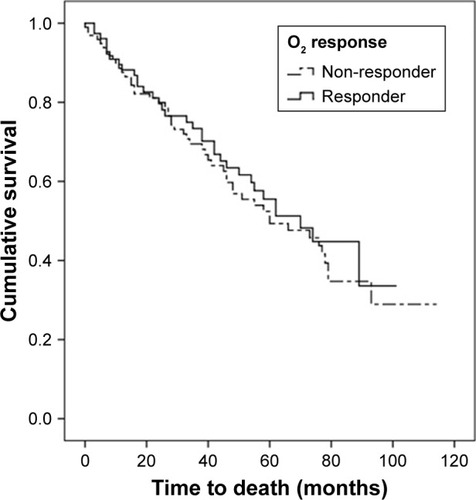
One hundred and seventy-four patients were included in the study, median age 70 years. Seventy-seven (44.3%) of the patients were oxygen responders. Borg dyspnea score improved by 1.4 (±1.4) units (P<0.0005) on oxygen. Median survival was 66 months with death occurring in 84 (48.2%) patients. Kaplan–Meier analysis revealed no survival difference between both responders and nonresponders (P=0.571). Cox regression analysis showed that more 6MWT desaturation, lower 6-minute walking distance on room air, male gender, lower hemoglobin, and body mass index were associated with higher mortality risk.
Conclusion
Acute exercise response to supplemental oxygen is not associated with long-term survival in patients with obstructive lung disease. This supports the use of ambulatory oxygen treatment for symptomatic purposes only.
Introduction
Hypoxemia is a common complication of respiratory disease. Different mechanisms come into play by varying degrees according to the pathology involved, including ventilation–perfusion mismatch, shunting, hypoventilation, and increased alveolar-arterial gradient.Citation1 Long-term supplemental oxygen has been an established treatment for a long time in patients suffering from severe resting hypoxemia. It has been shown to improve quality of life as well as morbidity and mortality.Citation2,Citation3
Hypoxemia usually becomes more manifest during exercise when the cardiorespiratory system is more stressed. This is associated with increasing breathlessness, which is a common exercise limiting factor in patients with lung disease.Citation4 Ambulatory oxygen therapy is currently used in some patients who experience desaturation during exercise. This aims mainly to correct the hypoxemia and relieve the dyspnea; however, the evidence base for its long-term benefits is not well established.Citation5
Exercise-induced desaturation (EID) is a feature of disease severity, but it is not known whether the exercise response to supplemental oxygen is itself a prognostic marker.Citation6 Exercise response is commonly used to test for the efficacy of different therapeutic interventions and for making predictions about lung disease morbidity and mortality. Our aim was to investigate the prognostic significance of response to ambulatory oxygen in respiratory patients with EID. We, therefore, used routinely collected data from our hospital’s ambulatory oxygen assessment service to relate this response to survival in respiratory patients.
Patients and methods
Subjects
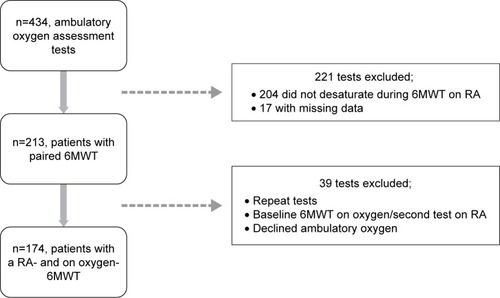
We identified patients who had undergone the 6-minute walking test (6MWT) on air and oxygen, as part of their evaluation for the need of ambulatory oxygen therapy, between April 2006 and July 2016. All patients who showed desaturation (≥4% and/or end oxygen saturation measured by pulse oximetry [SpO2] ≤88%) during exercise while breathing room air (RA) then performed a second 6MWT with supplemental oxygen ().
Study design and procedures
This was a retrospective study and all data were collected from the oxygen assessment team at the Royal Brompton Hospital, London, UK. The 6MWTs were performed as per the ATS/ERS guidelines by an experienced oxygen technician. For each test, the 6-minute walking distance (6MWD) and physiological parameters including the oxygen saturation and heart rate, along with Borg scale of dyspnea at the start and the end were recorded. The titrated oxygen requirement, used for the second test, was estimated according to the level of desaturation during the baseline 6MWT such that the minimum SpO2 is ≥90%. If patients had been tested on more than one occasion the first test was used. Survival data were obtained from the National Health Service spine with a cutoff date for analysis of February 1, 2017. The Royal Brompton ethics committee has ruled that ethical approval is not required for the retrospective analysis of routinely collected data. All patient data were anonymized and patient consent was not deemed to be necessary.
Statistical analysis
Analysis was performed using IBM SPSS® version 22 for Windows®. Results are presented as mean (SD) for normally distributed variables, median (Q1, Q3) for non-normally distributed variables or number (percentage) for dichotomous variables. A P-value ≤0.05 was considered statistically significant. Independent Student’s t-test was used to compare between-group differences, whereas paired t-test was used to compare the change in different parameters of the 6MWT after addition of oxygen.Citation7 A minimum clinically important difference for the 6MWD was defined as 26 m and patients were dichotomized according to “responders” (≥26 m) or “nonresponders” (<26 m).Citation8 Binomial logistic regression was used to identify variables associated with and predictive of improvement. To adjust for the possible impact of comorbidities on 6MWD response and survival, the Charlson comorbidity index (CCI) was calculated. In addition, the presence of a limiting comorbidity (pulmonary hypertension, left-sided heart failure, joint- or neuromuscular disease) was added as a dichotomous variable. Time from provision of ambulatory oxygen therapy to event (death) was used for the Kaplan–Meier analysis and log-rank test, in which patients were stratified according to the two response categories.Citation9 Cox proportional hazards modeling was performed to identify factors which most affected survival.Citation10 Initial selection of the independent variables was based on prior univariate Cox regression analysis along with logical choice relying upon data from previous studies. Variables considered in the models included were age, gender, body mass index (BMI), 6MWD desaturation on RA, baseline SpO2, forced vital capacity (forced vital capacity as a percentage predicted), lung diffusion capacity (TLCO percentage predicted), hemoglobin level, residual volume to total lung capacity ratio (RV/TLC%), and CCI. Backward elimination of covariates (entry threshold, P<0.05; removal threshold, P<0.10) was then used to ascertain the factors that contributed most to mortality. Proportional hazards assumption was tested and bootstrapping for internal validation was done whenever feasible.
Results
Satisfying the inclusion criteria was a cohort of 174 chronic obstructive lung disease patients (50% male) with a median age of 70 (60,76) years. Of these 116 (66.7%), 44 (25.3%), and 13 (7.5%) had a diagnosis of COPD, bronchiectasis, and severe persistent asthma, respectively (major disease entities). Combined provision of long-term oxygen therapy with ambulatory oxygen was present in 80 (46%) patients while 90 (54%) patients received ambulatory oxygen alone. The median baseline saturation on RA was 93% (91%, 94%) with an 11% (7%, 15%) desaturation after the RA-6MWT, for which 4 L per minute of oxygen, was prescribed on average. Baseline characteristics of the studied population are shown in .
Table 1 Characteristics of the study population
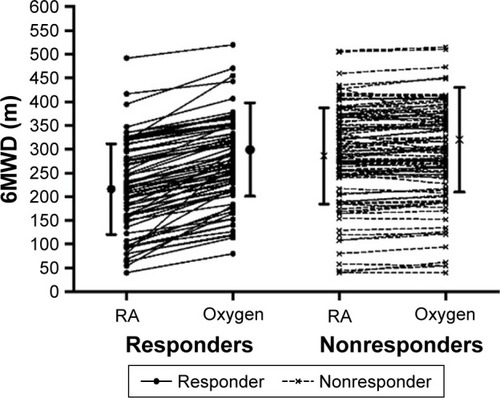
There was a statistically significant improvement in 6MWD after oxygen provision, from 254 (106 m) to 283 m (98 m) (P<0.0005), with a clinically significant response in 6MWD (≥26 m) in 77 (44.3%) patients (different patterns of response are shown in ). Similarly, positive changes in physiological parameters were present after ambulatory oxygen provision, including an improved Borg dyspnea score by 1.4 (±1.4) points (). The differences in the 6MWT parameters are shown in . The mean hemoglobin level was 14.5±1.7 versus 14.0±1.8 g/dL (P=0.064) in the responders and nonresponders, respectively. Logistic regression analysis showed that lower 6MWD on RA was the only significant predictor of clinically significant improvement (OR=0.99, 95% CI 0.985–0.995, P<0.0005).
Table 2 6MWT performance pre- and post-oxygen
Table 3 6MWT (on oxygen) performance in both response groups
Figure 2 Individual response patterns to ambulatory oxygen.
The overall median survival time was 66 months during which 84 (48.2%) patients died. Survival did not differ between oxygen responders and nonresponders (; log-rank test, P=0.571). Cox regression analysis has shown that more 6MWT desaturation on RA, lower initial RA-6MWD, male gender, lower BMI, and hemoglobin level were the significant predictors of mortality in our cohort (). No association was found between mortality and severity of air-flow limitation (P=0.585, Fisher’s exact test).
Table 4 Multivariate Cox proportional hazards model
Discussion
This study investigated the variable response of the 6MWT parameters to ambulatory oxygen and its potential prognostic significance in lung diseases. We found that an improvement in exercise capacity with oxygen supplementation was associated with no difference in survival in obstructive lung diseases. This is likely to reflect the different contributions of ventilatory, cardiac, and peripheral muscle factors in limiting exercise and the extent to which these are in turn influenced by supplementary oxygen.
Significance of the findings
Different pulmonary function parameters have been identified as important predictors of mortality in chronic obstructive lung diseases.Citation11–Citation13 In addition, exercise capacity and physical activity level are now recognized as prognostic factors and important foci for disease management.Citation14 The 6MWT integrates responses of the cardiopulmonary and musculoskeletal systems, making it a useful marker of the burden of the disease and the efficacy of different treatment interventions, including the need for oxygen therapy.Citation15 It was also shown to be more sensitive than incremental cycle ergometry in detecting EID in COPD patients.Citation16 Many parameters of the test, including the 6MWD and oxygen desaturation, have been previously used to prognosticate in patients with COPD. Desaturation during exercise has been shown to be an important predictor of mortality.Citation17–Citation20
Most of the evidence on the use of oxygen in hypoxic respiratory disease comes from COPD patients; however clinically, this is often extrapolated to include other respiratory diseases without robust data to support the different mortality and morbidity outcomes. In line with previous studies, correction of EID in our cohort was associated with reduced exertional dyspnea, as shown in the Borg scores, recovery times, as well as the 6MWD, which is expected to be accompanied by better functional capacity and exercise tolerance.Citation5,Citation21–Citation23 The improvement noted in different aspects of the 6MWT is likely caused by different mechanisms. Decreased stimulation of the respiratory center and chemoreceptor activation, together with improvement in the respiratory pattern and delayed anaerobic threshold are probable explanations. Additionally, oxygen is expected to improve, by different degrees, pulmonary hypertension secondary to hypoxic pulmonary vasoconstriction aiding better ventilation perfusion matching and gas exchange. The resultant decrease in dyspnea is usually associated with a decrease in respiratory rate, an important factor implicated in the progression of dynamic hyperinflation during exercise in COPD.Citation21
The presence of a walking distance improvement response in our cohort was shown not to signify a difference in survival. Pulmonary hypertension, cardiac dysfunction, and skeletal muscle impairment are important factors known to limit exercise and could show variable improvement with oxygen, which might explain the improvement margin. However, the absence of a concomitant survival benefit can be explained by the pathophysiologic basis for the primarily ventilation-limited exercise in obstructive lung disease patients. At rest, air-flow limitation together with the increased static lung compliance leads to an increase in the functional residual capacity. The resultant encroachment on the inspiratory reserve volume is accentuated during exercise with mechanically limiting dynamic hyperinflation. Oxygen therapy would certainly improve gas exchange which would ensure more oxygen delivery to the exercising respiratory and peripheral muscles (important limiting factor in exercise), but will have less effect on the mechanical domain, the primary cause of exercise limitation. This is in line with the finding in our data that improvement was not related to the severity of the disease as assessed by the degree of air-flow limitation. The logistic regression model showed that severity of air-flow obstruction (forced expiratory volume in 1 s as a percentage of predicted), hyperinflation (RV/TLC), desaturation, and baseline oxygen saturation on RA could not predict a positive 6MWD response. This suggests that muscle function properties rather than pulmonary function parameters were the important factors in distance improvement. Pinto-Plata et al have previously demonstrated that 6MWD, rather than airway obstruction markers, is a better predictor of mortality among severe COPD patients.Citation24
The lack of association between mortality and severity of air-flow limitation (P=0.585, Fisher’s exact test) might have been explained by the fact that the burden of comorbidities, especially cardiovascular disease, has been shown to be on the rise over the years in patients with severe COPD as has been shown by Ekstrom et alCitation25 and is also a major cause of mortality in mild and moderate COPD.Citation26,Citation27 However, among the tested sample, comorbidities were not found to be a significant predictor of survival in the adjusted model. Additionally, no difference was found regarding the hemoglobin levels or the presence of comorbidities between both groups of response in our cohort excluding the effect of comorbid conditions on the different improvements in 6MWD. Though low hemoglobin level did not predict response, it was found to be a significant predictor of mortality. This is in agreement with findings of previous studies linking anemia with mortality.Citation28,Citation29 One of the main factors we found to be associated with worse survival in our cohort was the degree of 6MWT desaturation on RA reflecting the failure of the cardiopulmonary system to adequately oxygenate blood during exercise. Given this and the fact that these patients were all prescribed ambulatory oxygen, might refute the utility of oxygen therapy in this cohort of patients. However, lack of objective data on the adequate use of oxygen could undermine such assumption. The association of higher BMI and longer 6MWD with better survival rate has been previously reported, indicating less systemic effect of obstructive lung diseases, especially COPD, on muscle wasting and nutritional status as well as better integrated cardiopulmonary response.Citation14,Citation19,Citation24,Citation30–Citation33
Limitations
This study is retrospective and has some limitations owing to the absence of data about subjects’ exacerbation frequency, completion of a pulmonary rehabilitation program or physical activity levels, which could have affected survival.Citation14,Citation34,Citation35
Conclusion
In summary, we found no association between the exercise response to supplemental oxygen and survival in patients with chronic obstructive lung disease and EID. This supports the practice of using ambulatory oxygen only as a symptomatic treatment in patients who do not have significant resting hypoxia.
Acknowledgments
Fund ing to A.S.S was provided by an Egyptian Ministry of Higher Education and Scientific Research Scholarship. The authors would like to thank Dr AF Elbehairy, PhD, for her comments on the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- HillNSAcute ventilatory failureMurrayJFNadelJABroaddusVCMasonRJErnstJDKingTEMurray & Nadel’s Textbook of Respiratory MedicinePhiladelphiaElsevier Saunders201617231739
- Nocturnal Oxygen Therapy Trial GroupContinuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trialAnn Intern Med19809333913986776858
- CroxtonTLBaileyWCLong-term oxygen treatment in chronic obstructive pulmonary disease: recommendations for future research: an NHLBI workshop reportAm J Respir Crit Care Med2006174437337816614349
- O’DonnellDERevillSMWebbKADynamic hyperinflation and exercise intolerance in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2001164577077711549531
- EjioforSIBaylissSGassammaATurnerAMAmbulatory oxygen for exercise-induced desaturation and dyspnea in chronic obstructive pulmonary disease (COPD): systematic review and meta-analysisChronic Obstr Pulm Dis20163141943428848863
- AndrianopoulosVFranssenFMPeetersJPExercise-induced oxygen desaturation in COPD patients without resting hypoxemiaRespir Physiol Neurobiol2014190404624121092
- StudentThe Probable Error of a MeanBiometrika190861125
- PuhanMAChandraDMosenifarZThe minimal important difference of exercise tests in severe COPDEur Respir J201137478479020693247
- KaplanELMeierPNonparametric estimation from incomplete observationsJ Am Stat Assoc195853282457481
- CoxDRRegression models and life-tablesJ R Stat Soc Series B Methodol1972342187220
- BoutouAKShrikrishnaDTannerRJLung function indices for predicting mortality in COPDEur Respir J201342361662523349449
- MartinezFJFosterGCurtisJLPredictors of mortality in patients with emphysema and severe airflow obstructionAm J Respir Crit Care Med2006173121326133416543549
- LangePNyboeJAppleyardMJensenGSchnohrPRelation of ventilatory impairment and of chronic mucus hypersecretion to mortality from obstructive lung disease and from all causesThorax19904585795852402719
- WaschkiBKirstenAHolzOPhysical activity is the strongest predictor of all-cause mortality in patients with COPD: a prospective cohort studyChest2011140233134221273294
- MoranteFGuellRMayosMEfficacy of the 6-minute walk test in evaluating ambulatory oxygen therapyArch Bronconeumol20054111596600 Spanish16324597
- PoulainMDurandFPalombaB6-minute walk testing is more sensitive than maximal incremental cycle testing for detecting oxygen desaturation in patients with COPDChest200312351401140712740254
- CasanovaCCoteCMarinJMDistance and oxygen desaturation during the 6-min walk test as predictors of long-term mortality in patients with COPDChest2008134474675218625667
- EnrightPLOxygen desaturation during a 6-min walk identifies a COPD phenotype with an increased risk of morbidity and mortalityEur Respir J20164811227365500
- TakigawaNTadaASodaRDistance and oxygen desaturation in 6-min walk test predict prognosis in COPD patientsRespir Med2007101356156716899358
- WaatevikMJohannessenAGomez RealFOxygen desaturation in 6-min walk test is a risk factor for adverse outcomes in COPDEur Respir J2016481829127076586
- SomfayAPorszaszJLeeSMCasaburiRDose-response effect of oxygen on hyperinflation and exercise endurance in nonhypoxaemic COPD patientsEur Respir J2001181778411510809
- EkstromMAhmadiZBornefalk-HermanssonAAbernethyACurrowDOxygen for breathlessness in patients with chronic obstructive pulmonary disease who do not qualify for home oxygen therapyCochrane Database Syst Rev201611CD00642927886372
- UronisHEEkstromMPCurrowDCOxygen for relief of dyspnoea in people with chronic obstructive pulmonary disease who would not qualify for home oxygen: a systematic review and meta-analysisThorax201570549249425472664
- Pinto-PlataVCoteCCabralHTaylorJCelliBThe 6-min walk distance: change over time and value as a predictor of survival in severe COPDEur Respir J2004231283314738227
- EkstromMPWagnerPStromKETrends in cause-specific mortality in oxygen-dependent chronic obstructive pulmonary diseaseAm J Respir Crit Care Med201118381032103621216882
- AnthonisenNRSkeansMAWiseRAThe effects of a smoking cessation intervention on 14.5-year mortality: a randomized clinical trialAnn Intern Med2005142423323915710956
- ZielinskiJMacNeeWWedzichaJCauses of death in patients with COPD and chronic respiratory failureMonaldi Arch Chest Dis199752143479151520
- BoutouAKKarrarSHopkinsonNSPolkeyMIAnemia and survival in chronic obstructive pulmonary disease: a dichotomous rather than a continuous predictorRespiration201385212613122759351
- AhnYHLeeKSParkJHIndependent risk factors for mortality in patients with chronic obstructive pulmonary disease who undergo comprehensive cardiac evaluationsRespiration201590319920526278777
- CelliBRCoteCGMarinJMThe body mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary diseaseN Engl J Med2004350101005101214999112
- Gray-DonaldKGibbonsLShapiroSHMacklemPTMartinJGNutritional status and mortality in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med199615339619668630580
- LandboCPrescottELangePVestboJAlmdalTPPrognostic value of nutritional status in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med199916061856186110588597
- DajczmanEWardiniRKasymjanovaGSix minute walk distance is a predictor of survival in patients with chronic obstructive pulmonary disease undergoing pulmonary rehabilitationCan Respir J201522422522926252533
- SchmidtSAJohansenMBOlsenMThe impact of exacerbation frequency on mortality following acute exacerbations of COPD: a registry-based cohort studyBMJ Open2014412e006720
- CoteCGCelliBRPulmonary rehabilitation and the BODE index in COPDEur Respir J200526463063616204593