Abstract
Background
COPD is a common cause for hospital admission. Conventional studies of the epidemiology of COPD involved large patient number and immense resources and were difficult to be repeated. The present study aimed at assessing the utilization of a computerized data management system in the collection and analysis of the epidemiological and clinical data of a large COPD cohort in Hong Kong (HK).
Patients and methods
It was a computerized, multicenter, retrospective review of the characteristics of patients discharged from medical departments of the 16 participating hospitals with the primary discharge diagnosis of COPD in 1 year (2012). Comparison was made between the different subgroups in the use of medications, ventilatory support, and other health care resources. The mortality of the subjects in different subgroups was traced up to December 31, 2014. The top 10 causes of death were analyzed.
Results
In total, 9,776 subjects (82.6% men, mean age = 78 years) were identified. Of the 1,918 subjects with lung function coding, 85 (4.4%), 488 (25.5%), 808 (42.1%), and 537 (28.0%) subjects had the Global Initiative for Chronic Obstructive Lung Disease (GOLD) 1, 2, 3, and 4 classes, respectively. Patients with higher GOLD classes had higher number of hospital admissions, longer hospital stay, increased usage of noninvasive mechanical ventilation (NIV), combinations of long-acting bronchodilators, and higher mortality. Of the 9,776 subjects, 2,278 (23.3%) received NIV, but invasive mechanical ventilation was uncommon (134 of 9,776 subjects [1.4%]); 4,427 (45.3%) subjects had died by the end of 2014. The top causes of death were COPD, pneumonia, lung cancer, and other malignancies.
Conclusion
Patients admitted to hospitals for COPD in HK had significant comorbidities, mortality, and imposed heavy burden on health care resources. It is possible to collect and analyze data of a large COPD cohort through a computerized system. Suboptimal coding of lung function results was observed, and underutilization of long-acting bronchodilators was common.
Introduction
COPD is a common disease that imposes a high burden on health care resources worldwide.Citation1,Citation2 The prevalence of COPD varied from 11.4% to 26.1%.Citation1 In Hong Kong (HK), the prevalence rates of COPD in the elderly population aged ≥60 years were 25.9% and 12.4% based on two different definitions with different spirometric criteria (postbronchodilator FEV1/FVC <70% or lower limit of normal range).Citation3 In HK, the crude mortality rate of COPD was 29.1/100,000, while the crude hospitalization rate was 193/100,000 in 2005.Citation4 COPD ranked second (to respiratory infections) as a respiratory cause for hospitalization and inpatient bed-days. In elderly subjects aged ≥75 years, the hospitalization rate for COPD was as high as 2,225/100,000.Citation4 The economic burden of COPD on the society is enormous.Citation5,Citation6
Previous studies gave information on the overall morbidity, mortality,Citation4 and the prevalence of COPD in HK.Citation3,Citation7 COPD patients in HK were undertreated compared with those in other countries. For example, the use of inhaled long-acting anti-muscarinic agent (LAMA) in HK (3.9%) was much lower than that in the other countries.Citation8 No large-scale study has looked into other details of COPD patients in HK.Citation9 There was no information on the severity of illness of a large COPD cohort requiring hospital admission in HK and how much resources they require in terms of length of hospital stay, medications, noninvasive mechanical ventilation (NIV), and invasive mechanical ventilation (IMV). There was also little information on the outcome of these patients over time.
Detailed studies of a large population of COPD patients involve immense resources. Demographic data of the COPD patients, their severity of disease, comorbidities, use of health care resources, and mortality would be invaluable for health care planning to manage the disease in the public sector. In HK, almost 95% of the population relied on the Hospital Authority (HA) for hospital medical service. All patient admissions under the HA were computerized and recorded in the clinical management system (CMS), but additional diagnosis and procedure coding had to be performed by the attending physician. It is possible to perform data retrieval with the HA Clinical Data Analysis and Reporting System (CDARS) software program.Citation10,Citation11 A pilot study was carried out in one center in 2010.Citation10 Patients with the principal discharge diagnosis of COPD were identified, and a computerized report of their demographic data and the use of medical resources was generated using CDARS. Some of the data still required manual capture and case record review. We have extended the study to include a large COPD cohort based entirely on the CDARS and without the need of individual patient record review. No additional research assistant had been employed for the purpose of this study.
Patients and methods
Study design and patient recruitment
This was a multicentered retrospective study of COPD patients discharged from the medical departments of 13 public regional hospitals and 3 chest hospitals of the HA in HK, during the period from 1 January to 31 December 2012. A list of participating hospitals is provided in the Supplementary material. This list included all except one public acute regional hospital (with 24-hour acute emergency service) and all except one chest hospital in HK from 2012 to 2014. Data retrieval was performed with the HA CDARS.Citation10,Citation11 All patients with the principal diagnosis of COPD (International Classification of Diseases [ICD] codes 491, 491.2, 491.21, 492, 492.8, and 496) on discharge in 2012 were included. The inclusion criteria were as follows: 1) aged >40 years; 2) principal discharge diagnosis of COPD (with ICD codes as described earlier); and 3) discharge from the medical departments of the respective hospitals. The exclusion criteria included the following: 1) aged ≤40 years and 2) patients discharged from specialties other than Department of Medicine.
Case record review and data entry of individual patients were not required. The group data that were retrieved by CDARS included the following: 1) demographic data; 2) total number of admissions for each subject between 1 January and 31 December 2012; 3) total length of hospital stay in 2012; 4) number of attendances at accident and emergency departments (A&E) and at specialist outpatient clinics (SOPCs); 5) coding of lung function tests and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) classification (ever performed, if available); 6) treatment modalities including acute NIV (ICD code 93.9) and IMV (ICD code 96.70, 96.71, and 96.72); 7) medications used including inhaled corticosteroids (ICSs), long-acting beta-agonists (LABA), LAMA, or their combinations; 8) comorbidities (including hypertension, ischemic heart disease, diabetes mellitus, chronic effects of tuberculosis [old TB], bronchiectasis, congestive heart failure, and asthma) that were coded in previous hospital admissions; 9) mortality of those recruited patients from 1 January, 2012, to 31 December, 2014; and 10) the cause of death estimated from the principal diagnosis for the episode of hospital discharge which ended up in death.
The data that require coding by physicians included the principal and secondary diagnosis, procedure coding, and lung function coding. Coding for lung function was not mandatory for the diagnosis coding of COPD. For patients with spirometry data available, the GOLD criteria of post-bronchodilator FEV1/FVC ratio <70% and FEV1% predicted were used for the diagnosis and staging of COPD.Citation12
The study was approved by the Clinical Research Ethics Committees of all the participating hospitals. As this was a retrospective study with no active intervention, patient consent was not required by our Clinical Research Ethics Committees for research projects that involve only review of medical information. Furthermore, individual case record was not performed for this study. Only clinical data without patients’ personal information were sent to the coinvestigators for analysis.
Statistical analysis
The CDARS provided simple statistical analysis with mean and SD of the whole group and subgroups defined by different parameters. Additional statistical evaluations, eg, comparisons between subgroups, were performed using the SPSS Version 22 software package (IBM Corporation, Armonk, NY, USA). Data were expressed as mean ± SD. Comparisons between two groups were made by using the χ2 test for categorical data, and unpaired student t-tests were used for continuous data where appropriate. Different stages of GOLD classification were compared by one-way analysis of variance and the Games-Howell post hoc tests. To test for any trend across stages of GOLD classification, the χ2 tests for linear trend were used for categorical data. All reported p-values were two-sided. A p-value <0.05 is considered statistically significant.
Results
Patient characteristics
There were a total of 9,776 patients with the principal diagnosis of COPD during the study period with a total of 19,795 hospitalization episodes. shows the demographic characteristics of the subjects. The subjects were mostly elderly with a mean age of 78.0±9.4 years, and 82.6% were men; 1,918 subjects (19.6%) had lung function tests ever performed that was coded in the admissions in 2012, and 85 (4.4%), 488 (25.5 %), 808 (42.1%), and 537 (28.0%) of the 1,918 subjects with lung function coding had GOLD 1, 2, 3, and 4 classes, respectively. The lung function test might have been performed in 2012 or earlier. The version of CDARS in 2012 was not able to ascertain the year of lung function performed. Patients with GOLD 3 and 4 COPD were 3 years younger than those with GOLD 1 and 2 COPD (74.9 vs 77.8 years, p<0.001). The mean age of female patients (F) was higher than that of male patients (M) for the whole group, all GOLD classes and those without lung function coding ().
Table 1 Demographic characteristics of the subjects (obtained from the first admission within the year 2012) with or without lung function coding
Use of health care resources
shows the use of health care resources of the subjects including attendance at A&E and SOPC, number of hospital admissions, and use of NIV and IMV. The subjects had an average of 3.8 emergency department visits and an average of 2.0 hospitalizations during the year 2012. Increasing GOLD stages were associated with more hospital admissions, longer length of hospital stay, SOPC attendances, higher percentage of NIV use during hospitalizations, and higher mortality (in the same year and after 2 years). Overall, 2,278 of 9,776 (23.3%) subjects required NIV during admission, whereas 309 of 537 (57.5%) patients with GOLD 4 disease had been treated with NIV. The use of IMV was low among all GOLD classes (overall 1.4%). Compared with patients without lung function coding (n=7,858), patients with lung function coding (n=1,918) had more attendance at A&E and SOPC, more hospitalizations, longer hospital stay (17.9 vs 11.0 days, p<0.001), and more requirement of NIV (39.8% vs 19.3%, p<0.001).
Table 2 Use of health care resources of subjects according to the GOLD classification
Pharmacotherapy and GOLD class
shows the pharmacotherapy for COPD among recruited subjects. Overall, 9.9% of subjects were on LABA alone, 1% on LAMA alone, and 33.6% on ICS alone; 16.4% on LABA and LAMA combination, 10.1% on ICS and LABA, and 3.4% on ICS with LAMA; and 10.5% on triple therapy with ICS, LABA, and LAMA. Among subjects with and without lung function coding, 79.6% and 44.3% of the subjects were on at least one long-acting bronchodilator (LAMA and/or LABA), respectively. Patients without lung function coding were more likely to be on ICS alone (37.8% vs 16.3%, p<0.001). With increasing severity of GOLD class, more subjects were on combination of LABA and LAMA with or without ICS.
Table 3 Medications use of subjects according to the GOLD classification
Comorbidities and GOLD class
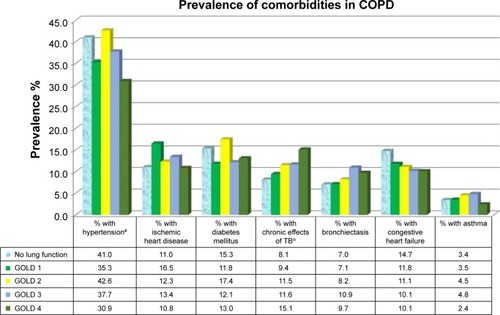
shows the comorbidities of COPD subjects. In total, 5,923 subjects (60.6%) had at least one of the comorbidities listed (hypertension, ischemic heart disease, diabetes mellitus, old TB, bronchiectasis, congestive heart failure, and asthma). Hypertension and diabetes mellitus were more common in patients with GOLD 1 and 2 (41.5% and 16.6%, respectively) than in patients with GOLD 3 and 4 diseases (35.0% and 12.5%, respectively). shows the comorbidities of the subjects in relation to the GOLD class of lung function. Patients with lower GOLD classes were more likely to have hypertension (p=0.001), while patients with higher GOLD classes were more likely to have chronic effect of TB (p=0.048). There were no significant differences for ischemic heart disease, bronchiectasis, congestive heart failure, or asthma with different GOLD classes.
Table 4 Comorbidities of subjects according to the GOLD classification
Mortality and causes of death
The causes of death could only be retrieved by CDARS for patients who died in the HA hospitals. For patients who died outside the HA hospitals (including those who were certified dead at A&E), the identity of the patients could be retrieved from the death registry, but the cause of death could not be ascertained by the CDARS. For patients who died in the HA hospitals, 503 of 9,776 (5.1%) patients died in 2012 due to COPD (5.1%), while the total all-cause mortality was 1,585 of 9,776 (16.2%). Review of the cumulative all cause-mortality in the HA hospitals showed that 2,877 (29.4%) patients had died by the end of 2013 and 3,867 (39.6%) patients had died by the end of 2014 (). The top common causes of death were pneumonia (32.3%), COPD (30.1%), lung cancer (6.3%), other malignancies (4.0%), and respiratory failure (3.9%). Death from ischemic heart disease (2.7%), heart failure (1.8%), and cerebrovascular accident (1.0%) accounted for 5.5% of deaths due to cardiovascular causes.
Table 5 Cumulative mortality as on 31 December 2014 in the different groups of patients
As on 31 December, 2014, 3,876 of 9,776 (39.6%) and 560 of 9,776 (5.7%) of patients had died in and outside the HA hospitals, respectively (). Of the 560 cases with death outside the HA hospitals, 397 (70.9%) patients were certified dead at A&E department. The total mortality rate was 4,427/9,776 (45.3%) as in December 2014. The mortality rate of patients with GOLD 4 disease (51.6%) was significantly higher than in all other GOLD classes. The overall mean ages at death were 80.5 years for men and 86.4 years for women, respectively, which were very close to the life expectancy of 81.3 years for men and 87.3 years for women in the general population of HK. There was an inverse relationship of GOLD class with the age at death. Patients with GOLD 4 disease had the lowest mean age at death of 75.4 years for men and 81.0 years for women. The difference was statistically significant for men but not for women, probably because of the smaller number of female patients. For patients without lung function coding, the mean age at death (M: 81.1 years, F: 86.8 years) was greater than that of those with lung function coding (M: 78.2 years, F: 83.0 years; p<0.0001).
In total, 1,585 of 9,776 (16.2%) patients died in the HA hospitals in 2012, while 8,191 of 9,776 patients (83.8%) survived after their last discharge from the HA hospitals in 2012. Using the last discharge date from the HA hospitals in 2012 as the index date, the top 5 causes of death of these patients in the HA hospitals in 2012, at 1 year (1–365 days) after discharge and at 2 years (366–730 days) after discharge, are listed in . The top 5 causes of death in the HA hospitals were COPD, pneumonia, lung cancer, respiratory failure, and other malignancies with no significant variation observed over the 2-year period. The 1-year mortality rate after discharge in 2012 was 1,175/8,191 (14.3%); 1,245 patients died in the second year. The 2-year mortality rate was 2,420/8,191 (29.5%).
Table 6 Top 5 causes of in-hospital mortality in 2012 and at 1 year and 2 years of discharge from hospital
Discussion
The use of electronic medical record databases makes it possible to study large patient cohorts. Studies had been carried out with the UK Clinical Practice Research Datalink GOLD to study exacerbations in COPD patients in primary care.Citation13 We have collected hospital admission data of a large COPD cohort using a computerized system (CDARS).Citation10,Citation11 To the best of our knowledge, this is the first study of this kind for COPD patients in HK. We have chosen to investigate the common parameters including demographic data, use of hospital services such as hospital stays, A&E attendance, use of NIV, and medication prescription in patients with different GOLD classes. These parameters provide important statistical figures for the estimation of disease burden and consumption of health care resources. In future, it is possible to extend the study to other parameters and make correlations between different subgroups. As most of the analytical work with CDARS can be performed with statistical manipulation, but without additional data entry, it is possible to repeat the study within a short period at low cost and have near real-time monitoring of the parameters of interest. It is also possible to track information and outcome of subgroups over time.
HK is a densely populated city with >7.3 million citizens. There are more women than men in HK with a male-to-female ratio of around 1:1.18. The expectation of life for men and women as in 2016 was 81.3 and 87.3 years, respectively (Census and Statistics Department, the Government of HK Special Administrative Region [HKSAR]).Citation14 About 95% of the population depended on the HA for hospital service, which is heavily subsidized by the government. Free ambulance service is provided to patients in need in any area of the territory. The most significant “bottleneck” to hospital admission appears to be the availability of hospital beds, and only patients with more severe diseases could be admitted.
The present study included all except one regional acute general medical department and all except one chest hospital in HK in 2012–2014. We believed that the information obtained from this study would be a representative of the total picture of COPD admissions in HK. This study will help to provide information on the burden of COPD on the public hospital health care system, the case mix, and severity of COPD in HK and provide reference for resource and manpower allocation in the future. The information would probably also provide useful reference for other countries in Asia.
This study captured the data of 19,795 episodes of admissions with >9,000 patients admitted to public hospitals in HK with the principal diagnosis of COPD in 2012. We found that the majority of COPD patients were elderly men. The predominance of male patients may limit the generalization of our findings to female patients. Many patients were not using the appropriate medications as recommended by the GOLD guidelines.Citation12 In total, 61% of our patients had at least one of the comorbid illnesses (hypertension, ischemic heart disease, diabetes mellitus, old TB, bronchiectasis, congestive heart failure, and asthma).
Only about 20% of our patients had lung function coding entered in 2012. The lung function could have been performed in 2012 or earlier. The coding would also include the severity of COPD according to the ranges of the GOLDCitation12 stages once it was entered. The coding of lung function is not mandatory for the CMS in HA. The attending physician could choose not to code the lung function even if it had been performed. We expected the percentage of patients with lung function ever performed to be much >20%. Our previous pilot study with case record reviewCitation10 showed that 64% of COPD patients admitted to hospital had at least one spirometry that was ever performed. It appeared from the present study () that patients with more A&E attendance, hospitalizations, and clinic follow-ups were more likely to have the spirometry coding entered by the attending physicians. It also appeared that the group with spirometry coding had more severe COPD and/or exacerbation as their hospital stay was longer (17.9 vs 11.0 days, p<0.001), and many more of them required NIV support (39.8% vs 19.3%, p<0.001) compared with patients without lung function coding. The group without lung function coding appeared to have less severe disease/exacerbation, but their mortality rate was paradoxically higher than that of the group with lung function coding (46.1% vs 42.1%, p<0.002). The mean ages at death of the group without lung function coding were 81.1 and 86.8 years for men and women, respectively, which were very close to the life expectancy for the general population (81.3 and 87.3 years, respectively). The higher mortality in this group could perhaps be explained by a natural course of disease toward the end of life.
A recent study in the USA found that about 70% of the participants of the surveys had undiagnosed COPD as revealed with spirometry. For those with airflow obstruction, their risk of death was increased compared with subjects without airflow obstruction.Citation15 Another recent study found that airflow obstruction at the age of 55 years was an important risk factor for future COPD hospitalizations.Citation16 Poor lung function has been associated with an increased risk of exacerbations. Previous studies had shown that exacerbations became more frequent and more severe as the severity of COPD increased.Citation13,Citation17,Citation18 We have the same observation in this study in which those with poorer lung function had more admissions for COPD, more frequent need for NIV support, longer length of hospital stay as well as higher mortality.
Our data did not allow us to group the subjects according to the GOLD guideline12-recommended A, B, C, and D groups as we did not have the symptoms scores coding in the CMS. As all these subjects had at least one admission for COPD in 2012, they should all belong to group C or D according to the GOLD guidelineCitation12 after their first admission to hospital in 2012. For subjects in GOLD group C or D, it is recommended that subjects should be on at least ICS + LABA and/or LAMA. However, we found that only 24% of our patients were given prescriptions according to this guideline after discharge from hospital. Recent published data from HK also showed that there was suboptimal adherence to GOLD guideline, and overprescription of ICS was identified.Citation19 Optimization of the drug therapy would help to reduce the risk of developing acute exacerbation of COPD (AECOPD). Combination of ICS and LABA could lead to around a quarter fewer AECOPD than were seen with placebo.Citation20 Tiotropium can also reduce the odds of COPD exacerbations (OR =0.74, 95% CI =0.66–0.83) and related hospitalizations (OR =0.64; 95% CI =0.51–0.82) compared with placebo or ipratropium.Citation21
A recent studyCitation22 has shown that with the omission of spirometry in 2017 GOLD ABCD classification,Citation23 the revised system shifted many patients from C and D to A and B, possibly leading to reduced intensity of therapies. On the other hand, treatment with acute NIV for COPD admissions was more likely guided by the arterial blood gases. Our study showed that patients with GOLD 3 and 4 diseases were more likely to be treated with NIV than patients with GOLD 1 and 2 diseases. An earlier longitudinal study had also demonstrated that FEV1 was one of the factors associated with mortality risk in COPD.Citation24 Patients with compensated and decompensated respiratory acidosis had poorer lung function and higher risk of death/life-threatening events compared with patients with normocapnia.Citation25 Exacerbations were also more common in patients with poorer lung function.Citation13,Citation17,Citation18 Further studies are warranted to find out whether spirometry may have prognostic value in predicting the frequent exacerbators, development of type 2 respiratory failure, need of NIV, and mortality in patients with COPD.
Among the comorbidities, hypertension (40% of all subjects) was the commonest comorbidity followed by diabetes mellitus (15%) and cardiac diseases (congestive heart failure: 13.9%; and ischemic heart disease: 11.3%). A previous studyCitation26 found that hypertension, hyperlipidemia, and coronary artery diseases are the 3 commonest comorbidities, and this was similar to the findings in the present study. Other comorbidities including anxiety/depression, heart failure, pulmonary hypertension, and metabolic syndrome had been reported.Citation27 Clinicians should screen their COPD patients for the presence of comorbidities for which specific treatments are available and are associated with better COPD outcomes.Citation28 Vascular comorbidities in COPD may have a direct impact on patient survival.Citation29 In total, 9.0% and 7.5% of our subjects had chronic effects of TB and bronchiectasis, respectively. Self-reported TB was a risk factor for COPD in nonsmokers.Citation30 A history of TB should be considered as a potentially important cause of obstructive lung disease, particularly where TB is common.Citation31 HK has quite a high prevalence of TB (in 2015, total notifications of 4,498 cases with a notification rate of 61.63 per 100,000 population).Citation32
The all-cause mortality rate in the HA hospitals was 16.2% in 2012. This was much higher than the yearly mortality rate (4%–5%) in a study from the USA for AECOPD.Citation33 In this study, about 3% and 6% of the subjects required NIV and IMV support, respectively. In total, 23.3% of our COPD patients required NIV support, but a much lower rate of IMV (1.4%). A previous study found that the assignment of do-not-resuscitate status was the most significant independent predictor of avoiding intubation (OR =0.11, 95% CI =0.03–0.37).Citation34 As we have not collected the data of do-not-resuscitate status, we were not sure if this could have contributed to the lower rate of IMV in our subjects.
On 31 December 2014 (after >2 years of discharge from hospital for the first episode of COPD in 2012), 4,427 (45.3%) of the original cohort of 9,776 patients had died (3,867 [39.6%] within the HA hospitals; ). The high mortality in our group of patients was comparable to the previously reported high mortality of 22%–43% after 1 year and 36%–48% after 2 years following hospital admission reported from the USA, the Netherlands, and Spain.Citation35–Citation38 The high cumulative mortality in our group of patients could perhaps be explained by their relatively older age (mean age at death of 80 and 86 years for men and women, respectively) and the severity of their illness as reflected by the high percentage of patients requiring NIV. The availability of hospital beds precludes the admission of patients with milder disease, and only patients with more severe disease could be admitted. The lower denominator would increase the mortality rate in areas where bed availability is a problem.
A study conducted in Spain showed that the mortality rate was 35.6% at 2 years following hospital discharge for COPD; 50% of patients died from respiratory diseases and 19% from cardiovascular diseases.Citation37 An earlier single-center, prospective study in HK (243 COPD subjects) showed a mortality rate of 25% over 3 years.Citation39 The common causes of death were COPD (24.9%), pneumonia (6.6%), and lung cancer (13.1%). In our present study, the 2-year mortality rate after hospital discharge was 29.5% (). The top causes of death were similar – pneumonia, COPD, and lung cancer, but the percentages were somewhat different (32.2%, 21.8%, and 4.4% respectively), probably related to case selection in the earlier prospective study. Cardiovascular comorbidities were common in COPD patients in HKCitation10,Citation39 (; [in the present study]), but the incidence of cardiovascular deaths was disproportionately low in the present study (5.5%; ) as well as in earlier studies in HK.Citation10,Citation39 It is possible that the cardiovascular symptoms were masked by the overwhelming respiratory events in our critically ill COPD patients. A significant proportion of the subjects might have died of cardiovascular or cerebrovascular diseases outside hospital.
Limitations
The potential limitations of this study were the following: some parameters requiring physician coding may be inaccurate and/or incomplete. Coding for COPD remains a physician-led diagnosis in HK, and unlike the UK system, lung function coding is not mandatory. Only about 20% of the subjects had coding for lung function. For the remaining patients, lung function might or might not be performed. The timing of lung function was also not available in the earlier version of the CMS. This information was recently incorporated in the latest version of the CMS, but manual capture of data is still required. These problems may be solved in future with automatic uploading of the spirometric data to the CMS. The Medical Research Council dyspnea grade and exacerbation rate (apart from the severe exacerbations resulting in hospital admissions) were not included in the present format of the CMS, and a low coding rate is expected even if they are included. Exploration of clinical or biochemical parameters (eg, PaO2 and pCO2) that do not require manual coding will assist in the development of computerized data collection and analysis for COPD in the future.
Conclusion
It is possible to collect and analyze data of a large COPD cohort using a computerized system. COPD is a disease with high morbidity and mortality. Most subjects were elders with recurrent hospital admissions, and NIV support was required in 23% of subjects. Many of them were not on optimal medical therapy for COPD. Pneumonia and COPD were common causes of mortality. Improved care of COPD patients by optimizing their pharmacological treatment and management of their comorbidities may improve outcomes. Palliative care could be planned in advance for patients with poor prognostic factors.
Acknowledgments
We would like to thank Ms Carrie Wong and Ms Reling Tse of Medial Records Office for generating the patient statistics from CDARS and Dr YL Cheng for his assistance in statistical analysis. We would also like to thank Dr Thomas Mok, Dr KS Lau, Dr KL Choo, Dr KK Chan, Dr CH Chau, Dr CM Chu, Dr ML Wong, Dr Wilson KS Yee, and Dr PY Tse who worked as coordinators for the hospitals involved in this study and the HK Lung Foundation for sponsoring this project.
Supplementary material
List of hospitals included in the study
General hospitals
Alice Ho Miu Ling Nethersole Hospital, Caritas Medical Centre, Kwong Wah Hospital, North District Hospital, Pamela Youde Nethersole Eastern Hospital, Queen Elizabeth Hospital, Queen Mary Hospital, Prince of Wales Hospital, Princess Margaret Hospital, the Ruttonjee and Tang Shiu Kin Hospital, Tseung Kwan O Hospital, Tuen Mun Hospital, and United Christian Hospital.
Chest hospitals
Grantham Hospital, Haven of Hope Hospital, and Kowloon Hospital.
Disclosure
The authors received no personal fee from any grant or commercial companies and report no other conflicts of interest in this work.
References
- BuistASMcBurnieMAVollmerWMInternational variation in the prevalence of COPD (the BOLD Study): a population-based prevalence studyLancet200737074175017765523
- KoFWHuiDSLaiCKWorldwide burden of COPD in high- and low-income countries. Part III. Asia-Pacific studiesInt J Tuberc Lung Dis20081271371718544193
- KoFWWooJTamWPrevalence and risk factors of airflow obstruction in an elderly Chinese populationEur Respir J2008321472147818684847
- Chan-YeungMLaiCKChanKSThe burden of lung disease in Hong Kong: a report from the Hong Kong Thoracic SocietyRespirology200813S133S16518945323
- ManninoDMBramanSThe epidemiology and economics of chronic obstructive pulmonary diseaseProc Am Thorac Soc2007450250617878461
- DarkowTKadlubekPJShahHPhillipsALMartonJPA retrospective analysis of disability and its related costs among employees with chronic obstructive pulmonary diseaseJ Occup Environ Med200749223017215710
- LauACIpMSLaiCKVariability of the prevalence of undiagnosed airflow obstruction in smokers using different diagnostic criteriaChest2008133424817989159
- MiravitllesMMurioCTirado-CondeGGeographic differences in clinical characteristics and management of COPD: the EPOCA studyInt J Chron Obstruct Pulmon Dis2008380381419281096
- SteerJGibsonGJBourkeSCPredicting outcomes following hospitalization for acute exacerbations of COPDQJM201010381782920660633
- AuLHChanHSSeverity of airflow limitation, co-morbidities and management of chronic obstructive pulmonary disease patients acutely admitted to hospitalHong Kong Med J20131949850323784531
- ManLPHoAWWongSHExcess mortality for operated geriatric hip fracture in Hong KongHong Kong Med J20162261026494900
- Global Initiative for Chronic Obstructive Lung DiseaseGlobal Strategy for the diagnosis, management, and prevention of chronic obstructive lung disease Updated 2015. Available from: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2015_Apr2.pdfAccessed April 7, 2016
- MullerovaHShuklaAHawkinsAQuintJRisk factors for acute exacerbation of COPD in a primary care population: a retrospective observational cohort studyBMJ Open20144e006171
- Census and Statistics Department, The Government of the HKSAR Available from: http://www.censtatd.gov.hkAccessed February 10, 2018
- MartinezCHManninoDMJaimesFACurtisJLHanMKHanselNNDiazAAUndiagnosed obstructive lung disease in the United States. Associated factors and long-term mortalityAnn Am Thorac Soc2015121788179526524488
- ZaighamSWollmerPEngstromGLung function, forced expiratory volume in 1 s decline and COPD hospitalisations over 44 years of follow-upEur Respir J20164774275026647443
- HurstJRVestboJAnzuetoASusceptibility to exacerbation in chronic obstructive pulmonary diseaseN Eng J Med201036311281138
- CalverleyPMTetzlaffKDusserDDeterminants of exacerbation risk in patients with COPD in the TIOSPIR studyInt J Chron Obstruct Pulmon Dis2017123391340529238184
- ChanKPKoFWChanHSAdherence to a COPD treatment guideline among patients in Hong KongInt J Chron Obstruct Pulmon Dis2017123371337929238182
- NanniniLJCatesCJLassersonTJPoolePCombined corticosteroid and long-acting beta-agonist in one inhaler versus long-acting beta-agonists for chronic obstructive pulmonary diseaseCochrane Database Syst Rev20074CD00682917943918
- BarrRGBourbeauJCamargoCARamFSInhaled tiotropium for stable chronic obstructive pulmonary diseaseCochrane Database Syst Rev20052CD00287615846642
- TanWCBorbeauJAaronSDGOLD 2017 classification and lung function decline in chronic obstructive pulmonary diseaseAm J Resp Crit Care Med2018197567067328858570
- Global Initiative for Chronic Obstructive Lung DiseaseGlobal strategy for the diagnosis, management, and prevention of chronic obstructive lung disease Updated 2017. Available from: http://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-COPD/Accessed November 22, 2017
- TerzanoCContiVDi StefanoFComorbidity, hospitalization, and mortality in COPD: results from a longitudinal studyLung201018832132920066539
- LunCTTsuiMSNChengSLChanVLLeungWSCheungPSChuCMDifferences in baseline factors and survival between normocapnia, compensated respiratory acidosis and decompensated respiratory acidosis in COPD exacerbations: a pilot studyRespirology20162112813626603971
- DivoMCoteCde TorresJPComorbidities and risk of mortality in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med201218615516122561964
- SmithMCWrobelJPEpidemiology and clinical impact of major comorbidities in patients with COPDInt J Chron Obstruct Pulmon Dis2014987188825210449
- BrownJPMartinezCHChronic obstructive pulmonary disease comorbiditiesCurr Opin Pulm Med20162211311826814720
- CavaillesABrinchault-RabinGDixmierAComorbidities of COPDEur Respir Rev20132245447524293462
- LeeSHHwangEDLimJEThe risk factors and characteristics of COPD among nonsmokers in Korea: an analysis of KNHANES IV and VLung201619435336127038474
- AmaralAFCotonSKatoBTuberculosis associates with both airflow obstruction and low lung function: BOLD resultsEur Respir J2015461104111226113680
- Center for Health Protection HKSARTuberculosis notification2016 Available from: http://www.chp.gov.hk/en/data/1/10/26/43/5104.htmlAccessed April 7, 2016
- LimaFVYenTYMPatelJKTrends in in-hospital outcomes among adults hospitalized with exacerbation of chronic obstructive pulmonary diseaseCOPD20151263664226263035
- DigbyGCKeenanSPParkerCMNoninvasive ventilation practice patterns for acute respiratory failure in Canadian tertiary care centres: a descriptive analysisCan Respir J20152233134026469155
- ConnorsAFDawsonNVThomasCOutcomes following acute exacerbation of severe chronic obstructive lung diseaseAm J Respir Crit Care Med19961549599678887592
- GroenewegenKHScholsAMWoutersEFMortality and mortality-related factors after hospitalization for acute exacerbation of COPDChest200312445946712907529
- AmagroPCalboEOchoa de EchaguenAMortality after hospitalization for COPDChest20021211441144812006426
- Soler-CatalunaJJMartinez-GarciaMARoman SanchezPSalcedoENavarroMOchandoRSevere acute exacerbations and mortality in patients with chronic obstructive pulmonary diseaseThorax20056092593116055622
- KoFWTamWTungAHA longitudinal study of serial BODE indices in predicting mortality and readmissions for COPDRespir Med201110526627320655186