Abstract
Purpose
Previous studies have described the incidence, risk factors, and outcomes for patients with acute exacerbations of COPD (AECOPD) developing acute kidney injury (AKI). However, little is known about the differences between community-acquired AKI (CA-AKI) and hospital-acquired AKI (HA-AKI) in patients with AECOPD. Thus, in this study, we compared prevalence, risk factors, and outcomes for these patients with CA-AKI and HA-AKI.
Patients and methods
This study was conducted from January 2014 to January 2017, and data from adult inpatients with AECOPD were analyzed retrospectively. A total of 1,768 patients were included, 280 patients were identified with CA-AKI and 97 patients were with HA-AKI.
Results
Prevalence of CA-AKI was 15.8% and that of HA-AKI was 5.5%, giving an overall AKI prevalence of 21.3%. Patients with CA-AKI had a higher prevalence of chronic kidney disease (CKD) and lower prevalence of chronic cor pulmonale than patients with HA-AKI. Risk factors for developing HA-AKI and CA-AKI were similar, such as being elderly, requirement for mechanical ventilation, and a history of coronary artery disease and CKD. Patients with HA-AKI were more likely to have stage 3 AKI and worse short-term outcomes. In comparison with patients with CA-AKI, those with HA-AKI were more likely to require non-invasive mechanical ventilation (31.3% versus 16.8%; P = 0.003) and had a longer duration of mechanical ventilation (11 days versus 8 days; P = 0.020), longer hospitalization (14 days versus 12 days; P = 0.038), and higher inpatient mortality (32.0% versus 13.2%; P < 0.001). Patients with HA-AKI had worse (multivariate-adjusted) inpatient survival than those with CA-AKI (hazard ratio, 1.7 [95% confidence interval, 1.03–2.81; P = 0.038] for the HA-AKI group).
Conclusion
AKI was common in patients with AECOPD requiring hospitalization. CA-AKI was more common than HA-AKI but otherwise demonstrated similar demographics and risk factors. Nevertheless, patients with HA-AKI had worse short-term outcomes.
Introduction
COPD affects 9%–10% of people aged >40 years worldwide.Citation1 Disease exacerbations have a profound effect on patients with COPD, resulting in poor health and high mortality.Citation2,Citation3 Acute kidney injury (AKI) can be a severe complication of COPD. AKI is a multifaceted syndrome that occurs in different settings.
Fabbian et alCitation4 reported that AKI represents a very important predictive factor of in-hospital mortality in patients admitted because of COPD exacerbations. Barakat and coworkersCitation5 stated that the incidence rates of AKI in the COPD cohort and patients with AECOPD were 128/100,000 person-years and 1.9%, respectively. Although they described the incidence, risk factors, and outcomes for patients with AECOPD developing AKI, less attention was focused on AKI that developed in the community and how this may differ from hospital-acquired (HA)-AKI.Citation5
In this study, we compared the incidence, risk factors, and short-term outcomes of patients admitted to the hospital with community-acquired (CA)-AKI with those with HA-AKI.
Patients and methods
Patient selection
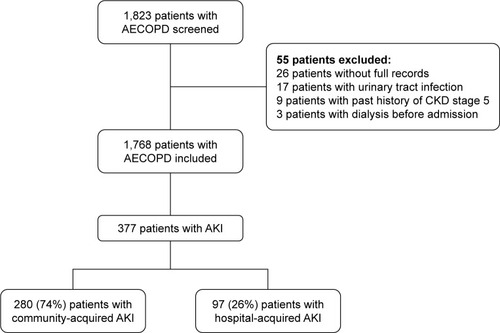
The study protocol was approved by the Regional Human Research Ethics Committee of Nanjing First Hospital (Nanjing, China). Individual patient consent was waived on condition that all patient data were de-identified before evaluation because this study was a retrospective analysis. This study was conducted at Nanjing First Hospital from January 2014 to January 2017. The diagnostic criteria for AECOPD were as follows: 1) a history of COPD (the patient had been clearly diagnosed with COPD, with typical clinical COPD presentations, and the pulmonary functions); 2) a change in the patient’s baseline dyspnea, cough, and/or sputum that was beyond normal day-to-day variations, was acute in onset, and could warrant a change in regular medication in a patient with underlying COPD.Citation6 The inclusion criterion was COPD exacerbation necessitating hospitalization. Exclusion criteria were as follows: patients without full medical records, with a urinary-tract infection, with a history of chronic kidney disease (CKD) stage 5, and undergoing dialysis before hospital admission ().
Definitions of CA-AKI and HA-AKI
AKI was defined as a serum creatinine (SCr) change that met the 2012 Kidney Disease Improving Global Outcomes criteria: an increase in the SCr level by ≥0.3 mg/dL within 48 h or ≥1.5-fold from the baseline within 7 days.Citation7 Any patient admitted to the hospital with AKI (CA-AKI) or who developed AKI during the hospital stay (HA-AKI) was identified and included in the analysis. Patients admitted to hospital with AKI apparent based on the first SCr measured within 24 h of hospital admission were denoted as having CA-AKI. In contrast, patients were identified as having HA-AKI, if AKI was not apparent upon hospital admission, but AKI developed during hospitalization. The baseline level of SCr was defined as the lowest one during hospitalization or during the preceding 12 months.
Data collection
The following data were collected from the medical records: sex, age, preexisting medical conditions (chronic cor pulmonale, pulmonary arterial hypertension, atrial fibrillation, hypertension, diabetes mellitus, coronary artery disease, CKD, chronic liver disease, anemia, cerebrovascular disease, or cancer), complications (acute respiratory failure [ARF] and hypercapnic encephalopathy), requirement for mechanical ventilation (non-invasive mechanical ventilation, invasive mechanical ventilation, and duration of mechanical ventilation), requirement for renal replacement therapy (RRT), intensive care unit (ICU) admission, length of ICU stay, and duration of hospitalization. In-hospital outcomes such as the requirement for mechanical ventilation (non-invasive mechanical ventilation, invasive mechanical ventilation, and duration of mechanical ventilation), RRT and ICU admission, length of ICU stay, duration of hospitalization, and inpatient mortality were also documented.
Data analyses
Data were analyzed using SPSS v22.0 (IBM Corporation, Armonk, NY, USA). Continuous variables are presented as mean ± SD or median values (25th–75th percentile) as appropriate. Categorical variables are shown as percentages. An unpaired Student’s t-test was used to compare mean values between two groups. The Mann–Whitney U-test was employed to compare median values. Comparison between two groups for categorical variables was made using the chi-squared test and the Fisher’s exact test where appropriate.
Univariate binary logistic regression analysis was done to evaluate the potential risk factors associated with CA-AKI and HA-AKI. Multivariate analysis using binary logistic regression enter method showed that the risk factors for CA-AKI (CA-AKI versus non-AKI) and HA-AKI (HA-AKI versus non-AKI), respectively. To construct the Cox model, univariate Cox regression for each predicting variable (sex, age, preexisting medical conditions, complications, requirement for mechanical ventilation, requirement for RRT, ICU admission, AKI severity, presence of HA-AKI, or CA-AKI) was carried out, with the inpatient mortality of patients with AKI as the outcome variable. Variables that were found to be significant on univariate Cox models were entered into the multivariable Cox model. Kaplan–Meier survival analysis was done to assess inpatient mortality. P < 0.05 was considered significant.
Results
AKI prevalence
In this study, there were 1,823 adult admissions to hospital, of which 55 (3.0%) cases were excluded. A total of 1,768 patients were enrolled for evaluation. Most (76%) patients were male. The mean age of the overall cohort was 77.0 years (SD: 9.1). Overall, 377 patients with AKI were identified, giving an overall AKI prevalence of 21.3%. A total of 280 (74.3%) patients had developed AKI in the community and were admitted to hospital with AKI (CA-AKI). The overall prevalence of CA-AKI was 15.8% of all hospital admissions. The remaining 97 (25.7%) AKI episodes were acquired within hospital (HA-AKI). The overall prevalence of HA-AKI was 5.5% of all hospital admissions.
AKI characteristics
Thirteen percent of AKI episodes were severe (stage 3 AKI), 62% had stage 1 AKI, and 25% had stage 2 AKI. Demographic differences between patients with HA-AKI and CA-AKI are shown in .
Table 1 Demographic data: CA-AKI versus HA-AKI
The number of men and women in HA-AKI and CA-AKI groups was similar. There was no significant difference in age between HA-AKI and CA-AKI groups (83 years versus 81 years; P = 0.12). Patients with HA-AKI were more likely to have severe AKI (22% had stage 3 AKI in the HA-AKI group compared with 11% in the CA-AKI group; P = 0.007). Nevertheless, the peak SCr value in the HA-AKI group was similar to that in the CA-AKI group. The prevalence of complications (ARF and hypercapnic encephalopathy) between the two groups was also similar. Comparison of the prevalence of various comorbidities in patients with HA-AKI or CA-AKI revealed approximately equal proportions of anemia, hypertension, diabetes mellitus, cancer, and liver, heart, and cerebrovascular diseases. The only two significant differences were a higher prevalence of chronic cor pulmonale in patients with HA-AKI (61.5% versus 41.8%, respectively; P = 0.001) and CKD in patients with CA-AKI (21.8% versus 10.4%, respectively; P = 0.015). Only ∼10.0% (37/377) of patients with AKI had a nephrology consultation.
Risk factors for CA-AKI and HA-AKI
Risk factors for CA-AKI and HA-AKI were similar. CA-AKI and HA-AKI shared several independent risk factors, such as being elderly, requirement for mechanical ventilation, and a history of coronary artery disease and CKD. However, there were two additional independent risk factors for HA-AKI: chronic cor pulmonale (odds ratio [OR], 1.98; 95% confidence interval [CI], 1.24–3.25; P = 0.004) and cancer (OR, 2.70; 95% CI, 1.28–5.72; P = 0.009).
In-hospital outcomes
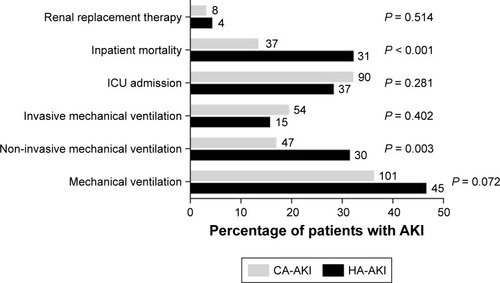
Short-term outcomes in patients with CA-AKI and HA-AKI are shown in . Patients with HA-AKI were more likely to require non-invasive mechanical ventilation compared with patients with CA-AKI (31.3% versus 16.8%; P = 0.003). Moreover, patients with HA-AKI had a longer duration of mechanical ventilation (median, 11 days; interquartile ratio [IQR], 7–17 days) compared with patients with CA-AKI (8 days; 4–15 days) (P = 0.020) (). However, there were no significant differences in the number of patients requiring mechanical ventilation (46.4% for HA-AKI versus 36.1% for CA-AKI), invasive mechanical ventilation (15.5% for HA-AKI versus 19.3% for CA-AKI), RRT (4.1% for HA-AKI versus 2.9% for CA-AKI), and ICU admission (38.1% for HA-AKI versus 32.1% for CA-AKI).
Table 2 Duration of stay in CA-AKI versus HA-AKI
Figure 2 In-hospital outcomes for CA-AKI versus HA-AKI.
Abbreviations: AKI, acute kidney injury; CA-AKI, community-acquired AKI; HA-AKI, hospital-acquired AKI; ICU, intensive care unit.
Duration of hospitalization
Patients with HA-AKI had longer hospitalization (median, 14 days; IQR, 9–20 days) compared with patients with CA-AKI (12 days; 8–17 days) (P = 0.038). However, there was no significant difference between the duration of ICU stay (median, 11 days; IQR, 6–16 days) in the HA-AKI group compared with patients with CA-AKI (9 days; 6–17 days) (P = 0.863) ().
Inpatient mortality
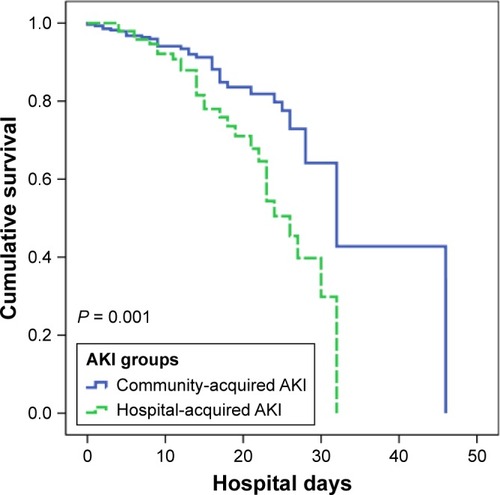
All patients were followed up until death in hospital or upon hospital discharge. During this period, the overall inpatient mortality was 5.9% (105/1768). The overall mortality was 18.0% in inpatients with AKI compared with 2.7% for inpatients without AKI. Moreover, mortality was higher in patients with HA-AKI (32.0%) than in those with CA-AKI (13.2%) (P < 0.001). shows the Kaplan–Meier survival curves for CA-AKI and HA-AKI groups. Patients with HA-AKI carried a greater risk for inpatient mortality than those with CA-AKI (OR, 3.09; 95% CI, 1.78–5.34; P < 0.001, binary regression analysis). demonstrates the independent contribution of listed covariates on the mortality of inpatients with AKI. After adjustment for other significant factors of death, the hazard ratio (HR) for inpatient mortality in the HA-AKI group versus the CA-AKI group was 1.70 (95% CI, 1.03–2.81; P = 0.038).
Table 3 Cox regression survival analyses for inpatient mortality
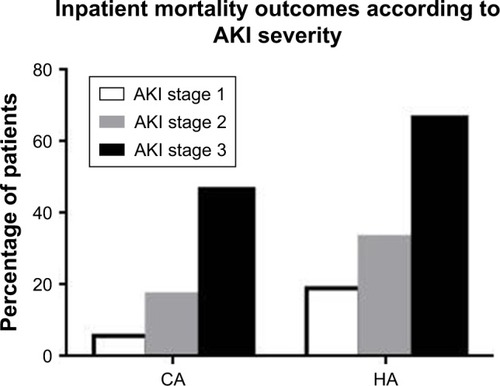
Mortality according to AKI severity
AKI stage 3 was an independent predictor for inpatient mortality (HR, 1.40; 95% CI, 1.02–1.92; P = 0.036) (). Moreover, a significant percentage of patients with stage 3 CA-AKI and HA-AKI had higher mortality (P < 0.001). In particular, 67% of patients with stage 3 HA-AKI and 47% of patients with stage 3 CA-AKI died during hospitalization ().
Figure 4 Inpatient mortality outcomes according to AKI stage.
Abbreviations: AKI, acute kidney injury; CA-AKI, community-acquired AKI; HA-AKI, hospital-acquired AKI.
Discussion
We found that nearly one-fifth of patients with AECOPD requiring hospitalization had evidence of AKI. Of them, three-quarters had CA-AKI, and one-quarter had HA-AKI. CA-AKI and HA-AKI demonstrated similar demographic and risk factors. Nevertheless, patients with HA-AKI had worse short-term outcomes. In comparison with CA-AKI, patients with HA-AKI were more likely to require noninvasive mechanical ventilation and had a longer duration of mechanical ventilation, longer hospitalization, and higher inpatient mortality. After adjustment for other significant factors, HA-AKI (compared with CA-AKI) remained an independent risk factor for the mortality of inpatients with AKI.
We estimated an AKI prevalence of 21.3% in patients with AECOPD requiring hospitalization. Our estimate was much higher than the prevalence of 1.9% reported by Barakat and coworkers.Citation5 Three explanations may account for this difference. First, in the study by Barakat et al,Citation5 AKI was identified through the International Classification of Diseases, which may be presented inaccurately and underestimate the prevalence of AKI. Second, since 2008, the prevalence of AKI coding has been increasing steadily (noted by KolheCitation8 in a study started in 2004). Hence, the AKI prevalence may have been underestimated. Third, nearly one-third of patients in this study were seriously ill, complicated by ARF. Previous studies have demonstrated that the prevalence of AKI in patients with ARF is 35–62%.Citation9–Citation11 Our data showed that CA-AKI was more common than HA-AKI. The prevalence of CA-AKI was approximately threefold higher than that of HA-AKI (15.8% versus 5.5%). This result confirmed the findings from the studies in different practice settings in which the prevalence of CA-AKI was 1.5–4.0-fold higher than that of HA-AKI.Citation12–Citation17 In particular, AKI was common in the community for patients with AECOPD requiring hospitalization. Thus, it was necessary to measure SCr levels and evaluate renal function upon hospital admission for those patients.
This study showed that the risk factors for CA-AKI and HA-AKI were similar. CA-AKI and HA-AKI were more common in elderly patients with preexisting coronary artery disease, CKD, and requiring mechanical ventilation. These data demonstrated the demographic characteristics of people in the community and hospital who may benefit from more frequent blood tests in the event of medication change or an acute illness.
Compared with CA-AKI, patients with HA-AKI had worse short-term outcomes.Citation12–Citation17 Patients with HA-AKI frequently required more care in the ICU,Citation13,Citation14,Citation16,Citation17 RRT,Citation15 and mechanical ventilationCitation12,Citation13 and had longer hospitalizationCitation14–Citation16 and higher inpatient mortality.Citation12,Citation14–Citation17 In this study, patients with HA-AKI were more likely to require non-invasive mechanical ventilation and had a longer duration of mechanical ventilation. Higher inpatient mortality was noted in the HA-AKI group. In addition, patients with HA-AKI had longer hospitalization. Non-invasive ventilation is an evidence-based treatment recommended for patients admitted with AECOPD.Citation18,Citation19 However, mechanical ventilation was also a common risk factor for AKI in this study. Kuiper et alCitation20 reported that mechanical ventilation may lead to AKI through hemodynamic alterations with reduced renal blood flow or ventilator-induced lung injury by triggering a pulmonary inflammatory reaction and subsequent systemic release of pro-inflammatory mediators. Moreover, several studies have examined the release of these mediators during mechanical ventilation.Citation21–Citation24 This may explain (at least in part) why patients developed HA-AKI during hospitalization, and why patients with more severe AKI were in the HA-AKI group. Moreover, our results demonstrated that HA-AKI, severe AKI (stage 3), RRT, and ARF were independent risk factors for inpatient mortality during AKI episodes. In this study, the prevalence of ARF and requirement of RRT in patients with CA-AKI and HA-AKI were similar. However, more patients with severe AKI were in the HA-AKI group, which may explain the higher mortality in inpatients with HA-AKI.
Barakat and coworkersCitation5 reported that mortality among patients with AKI at the first COPD exacerbation was 512/10,000 person-years. Our data showed that the overall mortality of inpatients with AKI upon a COPD exacerbation was 18.0%, and the inpatient mortality in the HA-AKI group and the CA-AKI group was 32.0% and 13.2%, respectively. Importantly, the mortality of inpatients with AKI stage 3 in the HA-AKI group and the CA-AKI group was 67% and 47%, respectively.
Scholars have reported that a delayed nephrology consultation could be associated with worse outcomes.Citation25,Citation26 Ponce et alCitation26 stressed the role of an early nephrology consultation in outcome for AKI patients. The authors concluded that a delayed nephrology consultation was associated with increased mortality among non-dialyzed patients (53% versus 22%, P < 0.01) and dialyzed patients (74% versus 49%, P < 0.006) as well as increased duration of stay in the ICU (17 versus 6 days, P < 0.001) and hospital (median, 19 versus 16 days, P < 0.01).Citation25 Ponce et alCitation26 reported that a delayed nephrology consultation was associated with increased mortality in the ICU (88.2% versus 65.4%, P < 0.001). However, only 10% (37/377) of patients with AKI consulted nephrologists in this study. In future, studies with a larger patient cohort could be employed to explore the association between an early nephrology consultation and outcomes in patients with HA-AKI and CA-AKI.
This study had four main limitations. First, it was a retrospective single-center study. A multicenter prospective study with a larger patient cohort is needed to confirm our conclusions. Second, information was not obtained on the differences in patient care that may have influenced the ultimate outcome. Drugs such as diuretics, non-steroidal anti-inflammatory drugs, and aminoglycosides are risk factors for AKI.Citation27 Third, there was no information on the long-term (eg, mortality, renal) outcomes of AKI. Four, the COPD severity stage is an important characteristic for patients with AECOPD, and we lacked these data.
Conclusion
We found that AKI was common in patients with AECOPD requiring hospitalization. CA-AKI was more common than HA-AKI but otherwise demonstrated similar demographics and risk factors. Nevertheless, patients with HA-AKI had worse short-term outcomes. Therefore, preventive and management strategies for AKI must be identified, implemented, and evaluated to limit the risks to susceptible individuals.
Author contributions
XW conceived the study and is the guarantor of the manuscript. C-CC and D-WC prepared the first draft and finalized the manuscript based on comments from all other authors. JL, M-QM, and Y-BC undertook analyses and interpretation of results. Y-ZC, XH, and WS participated in the preparation and analyses of data and proffered a critique of the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work. All authors agreed to be accountable for all aspects of the work.
Acknowledgments
This study was supported by the Specific Project for Technology Clinical Medicine of Jiangsu Province (BL2014015) and the Key Program for Development of Technology of Nanjing (201405031).
Disclosure
The authors report no conflicts of interest in this work.
References
- World Health Organization [webpage on the Internet]Chronic Obstructive Pulmonary Disease (COPD)2014 [cited July 23, 2014]. Available from: http://www.who.int/respiratory/copd/en/Accessed January 6, 2018
- CelliBRBarnesPJExacerbations of chronic obstructive pulmonary diseaseEur Respir J20072961224123817540785
- WedzichaJASeemungalTACOPD exacerbations: defining their cause and preventionLancet2007370958978679617765528
- FabbianFDe GiorgiAManfrediniFImpact of renal dysfunction on in-hospital mortality of patients with severe chronic obstructive pulmonary disease: a single-center Italian studyInt Urol Nephrol20164871121112727020445
- BarakatMFMcDonaldHICollierTJSmeethLNitschDQuintJKAcute kidney injury in stable COPD and at exacerbationInt J Chron Obstruct Pulmon Dis2015102067207726451102
- VestboJHurdSSAgustiAGGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2013187434736522878278
- KellumJALameireNKDIGO AKI Guideline Work GroupDiagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1)Crit Care201317120423394211
- KolheN webpage on the InternetEpidemiology of Acute Kidney Injury in England – 1998 to 20132014 [cited April 29, 2015]. Available from: https://clinicaltrials.gov/ct2/show/NCT2216695. NLM identifier: NCT2216695Accessed January 6, 2018
- LiuKDGliddenDVEisnerMDPredictive and pathogenetic value of plasma biomarkers for acute kidney injury in patients with acute lung injuryCrit Care Med200735122755276118074478
- MandelbaumTScottDJLeeJOutcome of critically ill patients with acute kidney injury using the Acute Kidney Injury Network criteriaCrit Care Med201139122659266421765352
- SotoGJFrankAJChristianiDCGongMNBody mass index and acute kidney injury in the acute respiratory distress syndromeCrit Care Med20124092601260822732288
- CuiZWangYFanMH医院获得性与社区获得性急性肾功能衰竭临床特点比较 [Comparison of clinical characteristics between hospital-acquired and community-acquired acute renal failure]Zhongguo Wei Zhong Bing Ji Jiu Yi Xue20051710615618 Chinese16259923
- Der MesropianPJKalamarasJSEiseleGPhelpsKRAsifAMathewROLong-term outcomes of community-acquired versus hospital-acquired acute kidney injury: a retrospective analysisClin Nephrol201481317418424361059
- WonnacottAMeranSAmphlettBTalabaniBPhillipsAEpidemiology and outcomes in community-acquired versus hospital-acquired AKIClin J Am Soc Nephrol2014961007101424677557
- HsuCNLeeCTSuCHIncidence, outcomes, and risk factors of community-acquired and hospital-acquired acute kidney injury: a retrospective cohort studyMedicine (Baltimore)20169519e367427175701
- SchisslerMMZaidiSKumarHDeoDBrierMEMcLeishKRCharacteristics and outcomes in community-acquired versus hospital-acquired acute kidney injuryNephrology (Carlton)201318318318723336108
- ObialoCIOkonofuaECTayadeASRileyLJEpidemiology of de novo acute renal failure in hospitalized African Americans: comparing community-acquired vs hospital-acquired diseaseArch Intern Med200016091309131310809034
- National Collaborating Centre for Chronic ConditionsChronic obstructive pulmonary disease. National clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary careThorax200459suppl 11232
- RamFSPicotJLightowlerJNon-invasive positive pressure ventilation for treatment of respiratory failure due to exacerbations of chronic obstructive pulmonary diseaseCochrane Database Syst Rev20043CD004104
- KuiperJWGroeneveldABSlutskyASPlötzFBMechanical ventilation and acute renal failureCrit Care Med20053361408141515942363
- RanieriVMSuterPMTortorellaCEffect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trialJAMA19992821546110404912
- GurkanOUO’DonnellCBrowerRRuckdeschelEBeckerPMDifferential effects of mechanical ventilatory strategy on lung injury and systemic organ inflammation in miceAm J Physiol Lung Cell Mol Physiol20032853L710L71812754185
- ImaiYParodoJKajikawaOInjurious mechanical ventilation and end-organ epithelial cell apoptosis and organ dysfunction in an experimental model of acute respiratory distress syndromeJAMA2003289162104211212709468
- HepokoskiMEnglertJABaronRMVentilator-induced lung injury increases expression of endothelial inflammatory mediators in the kidneyAm J Physiol Renal Physiol20173124F654F66028365585
- MehtaRLMcDonaldBGabbaiFNephrology consultation in acute renal failure: does timing matter?Am J Med2002113645646112427493
- PonceDZorzenon CdePdos SantosNYBalbiALEarly nephrology consultation can have an impact on outcome of acute kidney injury patientsNephrol Dial Transplant201126103202320621765052
- RewaOBagshawSMAcute kidney injury-epidemiology, outcomes and economicsNat Rev Nephrol201410419320724445744