Abstract
Background
COPD is a major cause of death and morbidity worldwide, and is characterized by persistent airflow obstruction. The evaluation of obstruction is critically dependent on sensitive methods for lung-function testing. A wide body of knowledge has been accumulated in recent years showing that these methods have been significantly refined and seems promising for detection of early disease.
Objectives
This review focuses on research on pulmonary function analysis in COPD performed in Brazil during this century.
Materials and methods
The literature was searched using a systematic search strategy limited to English language studies that were carried out in Brazil from the year 2000 onward, with study objectives that included a focus on lung function.
Results
After we applied our inclusion and exclusion criteria, 94 articles addressed our stated objectives. Among the new methods reviewed are the forced-oscillation technique and the nitrogen-washout test, which may provide information on small-airway abnormalities. Studies investigating the respiratory muscles and thoracoabdominal motion are also discussed, as well as studies on automatic clinical decision-support systems and complexity measurements. We also examined important gaps in the present knowledge and suggested future directions for the cited research fields.
Conclusion
There is clear evidence that improvements in lung-function methods allowed us to obtain new pathophysiological information, contributing to improvement in our understanding of COPD. In addition, they may also assist in the diagnosis and prevention of COPD. Further investigations using prospective and longitudinal design may be of interest to elucidate the use of these new methods in the diagnosis and prevention of COPD.
Introduction
COPD is a major worldwide public health problem that affects the quality of life of patients and causes physical disability and great socioeconomic impact.Citation1 Worldwide, 210 million people suffer from COPD,Citation2 which has been estimated to be the third-leading cause of death.Citation3 Unlike ischemic heart disease and cerebrovascular disease, which are decreasing in prevalence, deaths from COPD are increasing.Citation4,Citation5 Studies and interventions related to COPD diagnosis are necessary for early detection and better disease control. Data from studies published in various regions of the world show that COPD is underdiagnosed.Citation1
In Brazil, Queiroz et alCitation6 reported 71.4% COPD underdiagnosis in individuals with risk factors who were treated in public primary care facilities, while Santos et alCitation7 found that among patients with COPD, 80% had not received a prior diagnosis of the disease from their doctor. Another study showed that COPD prevalence in the Brazilian population varies between 6% and 15.8% in those aged ≥40 years, which is equivalent to 2.8–6.9 million individuals.Citation8 It was observed that the rate of diagnosing new cases in the city of São Paulo at the end of a 9-year follow-up period was similar to the percentages found in European, Asian, and North American countries, with a range from 1.4% to 4%, depending on the spirometric criterion used for diagnosing the disease.Citation9 Moreira et al reported that the functional and clinical changes coherent with COPD in individuals exposed to smoke from woodburning stoves, which are a domestic appliance that is widely used in the Brazilian rural environment, were less pronounced than those in patients exposed to tobacco. These authors also observed that in cases of exposure to woodburning smoke, the disease was predominantly seen in females.Citation10
Pulmonary function tests (PFTs), in addition to being essential tools for the diagnosis and evaluation of the severity of COPD patients, are also of critical importance in a variety of clinical settings, including in prognosis determination and evaluation of the therapeutic response. Spirometry is generally the first functional test performed and is the most important in clinical practice for most patients. However, in recent decades, tremendous technological advancements have been made in the tools used to measure lung function. In addition to the increased technological sophistication of the old functional evaluation methods, new PFTs have been progressively incorporated into clinical practice. All of these developments can have an immediate, positive impact on both early COPD diagnosis and evaluation and the monitoring of the disease. In this regard, many Brazilian researchers have evaluated the use of PFTs on COPD patients using a wide variety of study designs and evaluation techniques.
This paper describes a literature review in which we critically appraise and synthesize the current research on pulmonary function in COPD conducted in Brazil. Based on this analysis, we also discuss gaps in the knowledge that a new study would seek to address.
Materials and methods
The literature was searched using different keywords (Brazil, COPD, emphysema, chronic bronchitis, pulmonary function, spirometry, lung volumes, and respiratory muscles) and database sources (MEDLINE, Scopus, and Web of Science).
Inclusion criteria were research produced by Brazilian researchers, studies in the Brazilian population, studies published since the beginning of this century, and studies reported in English. Exclusion criteria were research where lung function was not included in the study objectives and studies performed outside Brazil.
These processes enabled the researchers to identify 94 appropriate studies for inclusion in the review. The presentation was organized into themes, describing the main areas of research observed in the reviewed literature. A simplified schematic representation of the main themes discussed and the flow of the review is shown in .
Results
Pulmonary function based on spirometry to evaluate bronchodilator response
Spirometry is the most often used diagnostic tool in the evaluation of lung function in COPD patients and is an examination with broad applicability and reproducibility in most patients. In a compatible clinical situation, spirometry is needed for COPD diagnosis and is characterized by persistent obstruction based on a forced expiratory volume in 1 second (FEV1):forced vital capacity (FVC) ratio of <70% after bronchodilator use.Citation1 In a Brazilian study, however, Lundgren et al investigated the use of the FEV1:FEV6 ratio as an alternative to the FEV1:FVC ratio in screening for COPD. This analysis may be more comfortable for patients and permit the use of simpler interpretation algorithms. The diagnostic criterion of airway obstruction (defined as an FEV1:FVC ratio <70%) showed sensitivity (Se) of 92% and specificity (Sp) of 99%. The positive predictive value was 100%, and the negative predictive value was 98%. The Kendall correlation calculation resulted in a correlation coefficient of 0.99 (P<0.0001). The authors concluded that evaluation of the FEV1:FEV6 ratio is accurate in screening for COPD.Citation11 Another (more recent) study involving Brazilian researchers sought to determine the factors associated with a change in the interpretation of spirometry for COPD diagnosis. These authors followed a cohort over a period ranging between 5 and 9 years after initial examination using different criteria to diagnose COPD. In that study, the rate of inconsistent mild COPD diagnosis was 11.7% using an FEV1:FVC ratio <70%, 5.9% using an FEV1:FEV6 ratio below the lower limit of normal (LLN) and 4.1% using Global Initiative for Chronic Obstructive Lung Disease (GOLD) stages II–IV criteria. The most important factor associated with diagnosis inconsistency was the closeness of the FEV1:FVC or FEV1:FEV6 ratio to the LLN during the first examination. The authors concluded that using an FEV1:FEV6 ratio < LLN or GOLD stages II–IV as airflow-obstruction criteria reduced inconsistencies in the diagnosis of mild COPD.Citation12 In addition, using the GOLD classification, Moreira et al determined which of the two GOLD ratings (BCD or II–IV) better reflected the functionality of patients with moderate-to-very severe COPD using 6-minute walking distance (6MWD), activities of daily living (ADLs), and the variables activity/inactivity of daily living evaluated by monitoring activity. These researchers observed that despite the low correlation coefficients, both GOLD ratings showed better association with 6MWD than ADLs evaluated subjectively or objectively.Citation13 In another Brazilian study, Menezes et al showed that the diagnosis of COPD was itself associated with overall mortality (hazard ratio 1.43 for FEV1:FVC < LLN, 2.01 for GOLD stages II–IV, 1.46 for GOLD stages I–IV, and 1.5 for FEV1:FEV6 < LLN).Citation14
The diagnostic and therapeutic approach in COPD patients should take into account the reversibility of airway obstruction determined by a pharmacodynamic test. Tavares et al investigated bronchoconstriction reversibility associated with the use of 400 μg of fenoterol in a sample of 64 patients. The authors evaluated the frequency of responses presented in FVC, slow VC, inspiratory capacity (IC), residual volume (RV), airway resistance (Raw), and specific airway conductance. Several parameters showed clear changes due to bronchodilator use in COPD. The clinical impression reported was that patients may experience alleviation of dyspnea and present clinical progress even without an FEV1 response.Citation15
Usually, the severity of COPD is classified by FEV1 after bronchodilator use, and improvement in FEV1 and decrease in its rate of decline are the most generally used outcomes in clinical research directed at evaluating treatment response and preventing disease progression.Citation1 However, the most important outcomes for COPD patients are symptoms and quality of life, and the correlation between FEV1 and the degree of dyspnea, health status, exercise tolerance, and frequency of exacerbation appears to be poor, which has also been demonstrated by some Brazilian studies.Citation16–Citation18 Pereira et al found a weak association of FEV1 with both total score on the St George’s Respiratory Questionnaire and the activity domain score (r=−0.32, P=0.04, and r=−0.34, P=0.03, respectively).Citation18 Several Brazilian researchers have shown that use of the BODE (body mass index, airway obstruction, dyspnea, and exercise capacity) index, rather than exclusively FEV1, seems to improve the association with quality-of-life markers.Citation19–Citation21 Camargo and Pereira observed that among spirometric variables, only the IC was selected by the multivariate model for 6MWD, with a 32% coefficient of determination.Citation22 Corroborating this finding, another study showed that the IC obtained after bronchodilator use was the better functional predictor of 6MWD and significantly related with GOLD score and BODE index.Citation23 Interestingly, these authors proposed a cutoff IC value after bronchodilation of 70% of that predicted for the Brazilian population as a method to classify COPD patients, as static lung-volume measurement is not always available. Santos et al observed that 59% of the variation in 6MWD could be explained by postbronchodilator IC, prolonged use of home oxygen therapy, and number of medications used in the handling of COPD.Citation7 Another study explored the association between energy expenditure and lung function in COPD patients undergoing indirect calorimetry measures while performing five ADLs. In this study, maximal voluntary ventilation was the only lung-function parameter associated with energy expenditure. Therefore, the authors emphasized the limited extent to which FEV1 is related to the functional performance of COPD patients.Citation24 Interestingly, Mendes et al investigated the influence of the FVC maneuver on the cardiovascular system in COPD patients. They observed that at the beginning of spirometry, the heart rate (HR) decreased (P<0.001) and then gradually increased until the end of the test (P<0.001). After the end of the maneuver, the HR continued to increase to a peak (P<0.001), and then fell rapidly to a value below resting values (P<0.001) before returning to baseline. In that study, blood pressure and HR variability (HRV) did not change during the FVC maneuver.Citation25
Pulmonary function tests in analysis of lung volume and dynamic lung hyperinflation
The measurement of lung volume can provide important information for evaluating the lung function of COPD patients, as it reflects the mechanical behavior of the lung and its elastic properties. In one study conducted in Brazil, Coertjens et al evaluated total lung capacity (TLC) and RV values obtained by the single-breath helium-dilution (SBHD) method and whole-body plethysmography (WBP) in patients with COPD. The study showed that the TLC and RV values were higher in the WBP than the SBHD method, and the difference was related to airway obstruction. The authors described linear equations that allowed adjustment of the TLC and RV values for airflow to predict the lung volume as measured by WBP. This correction can increase the accuracy of the SBHD method for assessing lung volume, and may contribute to the expansion of the use of the SBHD method, which is relatively simple, faster, and more widely available.Citation26
Albuquerque et al showed that the IC:TLC ratio was functionally more representative than traditional airflow-limitation and lung-hyperinflation indices in COPD patients, and was a strong predictor of marked reduction in maximum oxygen consumption. These authors found that IC:TLC values of ≤28% were associated with reduced exercise tolerance, and that increased values were observed in patients with lower loss of functional exercise capacity.Citation27 Interestingly, the IC:TLC ratio also is an independent predictor of mortality in COPD patients.Citation28 Mazzuco et al evaluated 16 sedentary males with COPD to assess the effect of lung function on HRV levels. They observed that HRV-index responses were more prominent during a respiratory sinus arrhythmia maneuver in moderate-to-severe COPD patients, and a worse HR dynamic was related to a greater decline in lung function. Moreover, these authors observed a strong correlation between the diffusing capacity for carbon monoxide and the RR interval during parasympathetic stimulation in these patients (r=−0.77, P<0.05).Citation29
Lung dynamic hyperinflation (DH) is a contributing factor to reduced physical capacity and a pulmonary adaptation to hyperpnea and the high metabolic requirement that occurs during exercise. In this regard, Castro et al investigated DH resulting from ADLs in COPD patients. They observed a reduction in IC after ADLs compared to IC values measured at rest (P=0.04) and a significant correlation between the degree of dyspnea and variation in IC between resting and ADLs (r=0.85).Citation30 Similarly, Silva et al found that patients with moderate-to-severe COPD developed DH after performing common ADLs involving the upper and lower limbs. These researchers observed a significant reduction in IC after all six tested activities, including walking on a treadmill, storing pots, walking 56 m carrying a 5 kg weight, climbing stairs, simulating taking a shower, and putting on shoes.Citation31 Similarly, Cordoni et al studied patients with moderate-to-severe COPD using serial IC measurements during cardiopulmonary exercise testing with a treadmill at a constant speed, and found a DH frequency of 63.3%. The authors also observed greater impairment of resting lung function in patients with DH than in those without DH.Citation32 In another Brazilian study, a randomized work including 30 COPD volunteers without severe hypoxemia, Scuarcialupi et al found that improvement in resting IC after bronchodilator use was associated with increased tolerance to effort, even in patients with COPD without DH. However, patients who showed no increase in resting IC were still able to obtain a functional benefit from bronchodilator use, provided they presented with DH during exercise.Citation33
Lung DH caused by expiratory flow limitation during a reduced expiratory time markedly increases the end- expiratory lung volume (functional residual capacity) in many COPD patients. In this regard, Lopes et al investigated the immediate effect of the application of continuous positive airway pressure (PAP) on hyperinflation and Raw in severe stable COPD patients. They observed that continuous PAP reduced lung volume and Raw for 15 minutes, but lung volume returned to baseline values within 30 minutes.Citation34 Monteiro et al evaluated the effects of expiratory PAP on operating lung volume during exercise in COPD patients. These authors observed that the application of expiratory PAP reduced DH, as demonstrated by lower operating lung volume after submaximal exercise in patients with COPD who had previously exhibited DH during exercise.Citation35
Pulmonary function analysis of small airways and ventilation distribution
Although first described approximately 60 years ago, an increasing interest in recent years has been developed in the use of the nitrogen-washout test (NWT). The NWT is increasingly incorporated in day-to-day pulmonology practice, as it can detect heterogeneity in the distribution of ventilation and small-airway disease when other PFTs still present normal values. In addition to its importance in the pathophysiological understanding of various clinical conditions, the evolution of its technical apparatus justifies the use of the NWT.Citation36 The NWT can facilitate the search for COPD patients whose phenotype consists of an abnormality of the small airways, and this knowledge can be used to facilitate the development of new drug therapies geared specifically toward the small airways. In Brazil, Lopes and Mafort conducted a cross-sectional study evaluating the relationship between the parameters obtained through the nitrogen single-breath washout (N2SBW) test and 6MWD, degree of dyspnea, and quality of life in COPD patients. These authors found a strong correlation between 6MWD and the phase III slope of the N2SBW (r=−0796, P=0.0001) and between 6MWD and RV (r=−0651, P=0.0001). Using multivariate analysis, the authors demonstrated that the N2SBW Phase III slope was the only independent predictor of 6MWD (R2=0703, P=0.0001), COPD Assessment Test (R2=0.586; P=0.0001), and the modified Medical Research Council Scale score (relative risk 1.14, P=0.0001).Citation37
Heterogeneity of ventilation and small-airway disease can also be identified by an increase in the alveolar plateau slope of the exhalation curve of gases, such as CO2, measured during tidal volume breathing using volumetric capnography. Using this tool, Veronez et al measured the normalized Phase III slopes in patients with non cystic fibrosis bronchiectasis and in COPD patients to compare the slopes obtained in both groups. They observed that while COPD patients had worse spirometry and 6MWD values, the mean capnographic variables Phase II slope, Phase III slope normalized by mean EV, and Phase III slope normalized by end-tidal CO2 concentration were similar. The authors concluded that gas-elimination curves were not sufficiently sensitive to monitor the severity of structural abnormalities, although the normalized Phase III slope needed to be studied further as a sensitive index for detecting small-airway diseases in COPD patients.Citation38 In another study conducted in Brazil, Masiero et al evaluated perfused lung fraction in COPD patients using single-photon emission computed tomography. They observed that the lung-volume fraction that receives blood from the pulmonary artery was reduced in these patients and that the degree of underperfusion correlated with the FEV1:FVC value (r=0597; P<0.001).Citation39
Pulmonary function in evaluation of respiratory muscles and chest wall
Respiratory muscle weakness may be related to both an increased respiratory system workload and a reduction or interruption in neural stimulation. Reduced function of the respiratory muscles represents increased physical and functional limitations, as it can cause health conditions that limit normal ADLs. In females with COPD, Mangueira et al found that both maximal inspiratory pressure (MIP) and maximal expiratory pressure were below the normal values for the Brazilian population (P=0.0001). Interestingly, these authors also showed that health-related quality of life had a negative linear correlation with MIP (r=−0.34, P=0.034). The reduced MIP in these females reflects excessive inspiratory effort caused by an abnormally high lung volume, while the reduced maximal expiratory pressure results in changes in expiratory muscle length and loss of exhalation strength.Citation40 Another Brazilian study in this area showed that overweight or obese severe COPD patients had increased inspiratory muscle strength compared to patients with the same degree of airflow obstruction but who were of normal weight or were underweight. The authors concluded that excess weight or obesity can counteract the disadvantages of being overweight and lead to a better prognosis in COPD patients.Citation41 Reis et al observed that the sympathetic–vagal balance is damaged at rest, and additionally that cardiac autonomic HR control is associated with respiratory muscle weakness.Citation42 In another Brazilian study, Donária et al evaluated the relationship between sniff nasal inspiratory pressure and COPD severity. They found that sniff nasal inspiratory pressure had a significant correlation (r=−0.62, P<0.001) with COPD severity, as evaluated by the BODE index, and that the cutoff point of 63 cmH2O showed a better combination of Se and Sp for predicting worse scores on the BODE index for these patients.Citation43
In recent years, interest has increased in the use of ultrasonography (US) to evaluate the diaphragm because it is a noninvasive, radiation-free method that can be repeated often over a short time. Yamaguti et al prospectively evaluated the diaphragmatic mobility of 42 COPD patients over 48 months using US, classifying them as patients with low mobility (≤33.99 mm) or high mobility (≥34 mm). These researchers observed that the group of COPD patients with low diaphragmatic mobility had higher BODE index scores and at the end of the 4-year period had a higher mortality rate than the group of patients with high mobility (15.8%, P=0.02).Citation44 In addition, Paulin et al used US to evaluate the effect of diaphragmatic mobility on exercise tolerance and the degree of dyspnea in COPD patients. They found a significant correlation between diaphragmatic mobility and 6MWD (r=0.38, P=0.005) and the degree of dyspnea (r=−0.36, P=0.007).Citation45
Pulmonary function based on evaluation of thoracoabdominal motion and breathing pattern
Most of the abnormalities suggest malfunction of respiratory muscles, particularly paradoxical motion of the diaphragm.Citation46 In this context, optoelectronic plethysmography (OEP) is a noninvasive tool for indirect measurement of pulmonary ventilation that can evaluate in a three-dimensional, real-time manner breath-to-breath changes in total chest-wall volume and its various compartments, including the pulmonary rib cage, abdominal rib cage, and abdomen. Using OEP, Borges-Santos et al analyzed the thoracoabdominal kinematics of 54 COPD patients at rest and during exercise. They found that anxiety and depression affected the sensation of dyspnea and the clinical management of the disease, although these symptoms did not have any effect on thoracoabdominal mobility or breathing pattern in COPD patients.Citation47 Another Brazilian study used OEP to show increased tidal volume in a sitting position without back support compared to a sitting position with back support in COPD patients (P=0.01). These authors also observed an increase in abdominal contribution to tidal volume in the supine position compared to the sitting position without back support (P<0.01) and the sitting position with back support (P<0.001).Citation48
In order to allow remote evaluation of abnormalities in thoracoabdominal motion (TM), Junior et al developed a telemedicine system for Internet-based home monitoring of TM. Results in patients with COPD showed that the acquisition and analysis of TM motion signals can be accurately performed. The user can also receive medical recommendations, and thus the proposed system may help in a wide range of telemedicine scenarios, including follow-ups and rehabilitation programs. This method may contribute to reducing costs and improving assistance offered to patients with COPD.Citation49
Breathing-pattern and TM abnormalities may contribute to exercise limitation in COPD. Alves et al investigated these changes during exercise in 22 males with stable COPD. The asynchrony was analyzed at rest and during three levels of exercise (30%–50%, 70%–80%, and 100% maximal workload). It was observed that asynchrony increased with exercise level (phase angle 11.95°±7.24° at rest vs 22.2°±15° [P=0.002], 22.6°±9° [P<0.001], and 22.7°±8° [P<0.001], respectively). The authors concluded that the increase in ventilation during exercise in COPD patients was associated with the major motion of the abdominal compartment and with an increase in asynchrony independent of exercise intensity.Citation50
Diaphragmatic breathing (DB) is largely applied in pulmonary rehabilitation of patients with COPD; however, it has been little studied. Yamaguti et al investigated the influence of a DB training program (DBTP) on TM and functional capacity in patients with COPD. Thirty subjects (FEV1 42%±13% predicted) were randomly allocated to either a training group (TG) or a control group (CG). The subjects in the TG performed a 4-week supervised DBTP (three individualized weekly sessions), while those in the CG received their usual care. The 4-week DBTP resulted in greater abdominal motion in the TG group during natural breathing when compared with the CG (F=8.66, P<0.001), as well as increased abdominal motion during voluntary DB (F=4.11, P<0.05) and greater diaphragmatic mobility (F=15.08, P<0.001). An improvement in 6MWD and health-related quality of life was also observed in the TG (F=4.9, P<0.05). It was concluded that DBTP induced increased diaphragm participation during natural breathing, resulting in an improvement in functional capacity of patients with COPD.Citation51
Fernandes et al studied the efficacy of DB in 29 patients with moderate and severe COPD. The protocol started with 4 minutes of tidal breathing, followed by 2 minutes of DB and 4 minutes of natural breathing. The authors observed that five moderate and five severe patients with COPD performed DB with asynchronous TM, which resulted in the worsening of the dyspnea. Effective DB was related to increased diaphragmatic mobility and inspiratory muscular strength, lower scores for dyspnea and hypoxemia, and coordinated TM. This provides evidence that DB can improve breathing pattern and ventilatory efficiency without causing dyspnea in patients whose respiratory muscular system is preserved.Citation52
Cancelliero-Gaiad et al compared the respiratory pattern during natural breathing, DB, and Pilates breathing methods in 15 COPD patients and 15 healthy subjects. DB increased respiratory volumes, times, and SpO2 and reduced respiratory rate in the two studied groups. Pilates breathing resulted in an increase in respiratory volumes in healthy group. No additional improvements in respiratory pattern were observed in the COPD patients. The two groups showed increased thoracoabdominal asynchrony under DB, with a greatest increment in the group composed by healthy volunteers.Citation53
Fernandes et al evaluated breathing pattern, TM, and ventilation in controls and patients with moderate and severe COPD. The volunteers were studied in a semirecumbent position at rest. COPD patients showed increased dead-space ventilation and lower diaphragmatic motion, which are associated with impairment of ventilatory function and changes in breathing patterns. This is initially seen as rapid and shallow breathing with no changes in TM. These findings were more pronounced in severe COPD, but still without changes in TM.Citation54
Pulmonary function tests based on oscillation mechanics
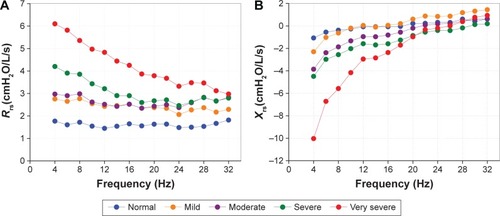
The forced-oscillation technique (FOT) characterizes respiratory impedance and its two components: respiratory system resistance and reactance. The method requires only passive cooperation and no forced expiratory maneuvers. Another important advantage, particularly in pathophysiological research, is that the FOT can be used to provide information on the mechanical characteristics of the respiratory system that is complementary to the information provided by spirometry.Citation55 At the beginning of this century, Melo et alCitation56 reviewed the literature, describing several applications and the high potential of clinical use of this method. As an example, shows typical results obtained in controls and patients with COPD classified according to GOLD.Citation57
Figure 2 Examples of results for the resistance (Rrs; A) and reactance (Xrs; B) obtained in normal subjects and patients with COPD classified according to the GOLD criteria.
The FOT was subsequently used in a series of studies concerning COPD. In these studies, the following parameters were used in the interpretation of the resistance curves: resistance at the intercept (R0), associated with the total resistance of the respiratory system; mean resistance (Rm), related to the airway caliber; and the slope of resistance (S), which is associated with the homogeneity of the resistive properties of the respiratory system. The results presented in the reactance curves were interpreted using mean reactance (Xm), which is associated with the homogeneity of the reactive properties of the respiratory system, and dynamic compliance (Cdyn). The absolute value of respiratory impedance (Z4Hz), which is related to the work performed by the respiratory muscles to overcome resistive and elastic loads, promoting the movement of air in the respiratory system, was also evaluated.
Contribution in pathophysiological studies and evaluation of diagnostic capacity
Di Mango et alCitation58 evaluated the diagnostic potential of the FOT in detecting changes in the respiratory mechanics in patients with COPD, comparing healthy subjects (n=21) with groups of patients with COPD (mild airway obstruction, n=16; moderate, n=23; and severe, n=40). Similar to the behavior observed in , COPD resistance was higher than observed for healthy volunteers. Increasing COPD severity resulted in an increase in total respiratory resistance, especially at lower frequencies, which introduced a frequency dependence of the resistance. Also similar to the example in , respiratory system reactance became more negative with obstruction. The highest changes were observed in the lower frequencies. All of the parameters used to describe resistance changes showed highly significant changes with the degree of airway obstruction (P<0.0001). Considering specifically the comparisons between controls and patients with mild obstruction, R0 and Rm increased significantly, while S did not present significant changes. Similarly to resistive parameters, all reactive parameters showed significant changes with airway obstruction (P<0.006). It is interesting to observe that in the initial condition of obstruction, resistance parameters and curves showed higher changes than reactance. On the other hand, in the later stages, the reactive parameters and curves were the most sensitive. These changes clearly describe the mixed pattern usually presented in the more advanced stages of COPD.
Aiming to contribute to preventing COPD development, Faria et alCitation59 investigated if the FOT would be able to identify the initial abnormal mechanical changes associated with the smoking habit. The study included FOT and spirometry measurements in groups of nonsmokers (n=28) and smokers (n=28). While the spirometric parameters were still at normal levels, showing small, nonsignificant reductions, the FOT parameters presented higher changes. It was observed that R0, resonance frequency, and Z4Hz presented significant increases. Significantly more negative values in Xm and more reduced Cdyn values were also observed. The analysis of the area under the receiver-operating characteristic (ROC) curve (AUC)Citation60 showed that R0, Cdyn, and Z4Hz presented diagnostic accuracies equal to or greater than 75%, providing evidence that these parameters can be useful in the clinical diagnosis of early abnormalities due to the smoking habit. In addition, the comparison of the AUCs obtained among oscillometric and spirometric parameters revealed significantly higher accuracies for FOT parameters, as described in .
Figure 3 Differences in the diagnostic performance of FOT and spirometric parameters, calculated by the difference between AUCs.
Abbreviations: FOT, forced-oscillation technique; AUCs, areas under the curve; Z4Hz, absolute value of respiratory impedance; Cdyn, dynamic compliance; Xm, mean reactance; Rm, mean resistance; R0, resistance at the intercept; FEF, forced expiratory flow; FVC, forced vital capacity; FEV1, forced expiratory volume in 1 second; S, slope of resistance; Fr, resonance frequency.
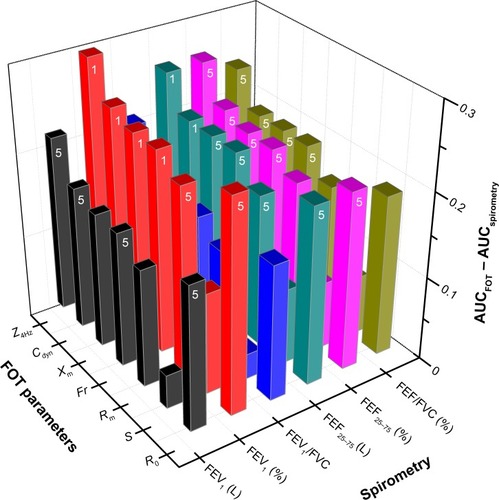
These findings provide evidence of two important points: 1) the FOT may be more sensitive than spirometry in the identification of the precocious abnormalities associated with smoking and 2) this method may help in screening smokers who may develop COPD. Further studies are necessary to investigate these two hypotheses in a wider number of subjects. If they are confirmed, FOT pulmonary function analysis may help in detecting initial changes during a stage at which pathological abnormalities are still potentially reversible. This may contribute significantly to preclusion of the development of COPD.
In the next step of this research, Faria et alCitation61 performed a comparative analysis of the diagnostic accuracy of the FOT and spirometric parameters in volunteers presenting different number of pack-years smoked: a control group and smokers classified as <20, 20–39, 40–59, and >60 pack-years. The precocious abnormal changes due to smoking were adequately identified in the volunteers presenting <20 pack-years by the FOT. The ROC analysis showed significantly higher accuracy for the FOT (P<0.01). Comparisons in groups with higher tobacco consumption (20–39, 40–59, and >60 pack-years) revealed similar diagnostic accuracies for the FOT and spirometry. This work provided additional evidence that the FOT may help in the diagnosis of precocious smoking-related respiratory abnormalities (<20 pack-years). In addition, there is also evidence that the FOT has similar accuracy to spirometry in the diagnostic of more advanced abnormalities (20–39, 40–59, and >60 pack-years).
In recent work from our group, Silva et alCitation62,Citation63 evaluated the diagnostic accuracy of monofrequency oscillometric pulmonary function in smokers and patients with COPD. These studies evaluated mean within-breath respiratory impedance (Zrs) during inspiration (Zi), expiration (Ze), and respiratory cycle dependence (∆Zrs = Ze – Zi). Impedance at the beginning of inspiration (Zbi) and expiration (Zbe), as well as peak-to-peak impedance (Zpp; = Zbe – Zbi), were also analyzed. In general, the within-breath Zrs parameters presented significant moderate-to-good correlations with spirometric indices of airway obstruction. In contrast to the control subjects and the smokers, the patients with COPD presented significant expiratory–inspiratory differences ().
Figure 4 Mean Zrs values during the ventilatory cycle in the studied groups.
Abbreviations: Zrs, respiratory impedance; GOLD, Global Initiative for Chronic Obstructive Lung Disease; ns, not significant; Zbi, impedance at beginning of inspiration; Zi, impedance during inspiration; Zbe, impedance at beginning of expiration; Ze, impedance during expiration.
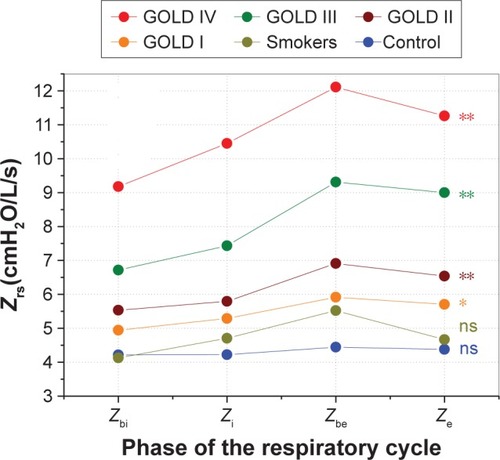
The adverse effects of moderate airway obstruction were adequately identified by the Zpp (AUC =0.83). In addition, mean impedance, Zi, Ze, Zbe, Zpp, and ∆Zrs identified mechanical abnormalities in severe and very severe patients with high accuracy (AUC >0.9). These results indicate that COPD induces respiratory cycle dependence, which is proportional to the degree of airflow obstruction. Another important finding of these studiesCitation62,Citation63 is that the Zrs observed in different phases of the respiratory cycle may be useful in the detection of COPD.
Oscillatory pulmonary function tests in bronchial hyperresponsiveness
The additional information provided by the FOT may help improve our understanding of the changes in respiratory mechanics that occur after the application of a bronchodilator. Based on this hypothesis, Di Mango et alCitation64 compared the changes in R0, S, and Rm measured with the FOT to those in FEV1 in 12 normal subjects, 22 patients with COPD, and eleven asthmatics after salbutamol inhalation. Percentile variations of the difference between postbronchodilator and prebronchodilator values were used to express reversibility of airway obstruction. The inhalation of salbutamol resulted in nonsignificant changes in R0 and S and a reduction in Rm in the control group. Higher changes and significant reductions in R0, Rm, and S were observed in COPD and asthmatic patients. In the COPD group, the variations were smaller than observed in asthmatics.
In a later study,Citation65 the effect of albuterol on respiratory resistance and reactance was evaluated in 70 patients divided into two groups based on spirometry findings: bronchodilator-negative (n=39) and bronchodilator-positive (n=31). It observed significantly smaller values in R0 (P<0.00002) and Rm (P<0.0002). Increased values were observed in S (P<0.0001), as well as in Cdyn (P<0.0001) and Xm (P<0.00004). The cited changes occurred in the two studied groups, and the changes in FOT parameters were higher than those found for spirometric parameters. The authors concluded that the use of albuterol may improve respiratory resistance and reactance in COPD patients, in spite of the FEV1-based classification. Therefore, these results provide evidence that the use of FEV1 alone may not be sufficient to adequately detect all of the physiological changes involved.
Continuing this research, da Costa et alCitation66 investigated the effects of airway obstruction on bronchodilator response and evaluated the utility of the FOT as a complementary measurement in this analysis. This study was conducted in 25 healthy individuals and 82 patients with COPD assessed with the FOT followed by spirometry before and after the use of salbutamol. The changes exhibited by the COPD subgroups were greater than in the healthy individuals (P<0.05). Increased obstruction resulted in decreased reductions in Rm and increased improvements in Xm (P<0.001). In addition, bronchodilation reduced ventilation heterogeneity and the impedance modulus in all COPD stages (P<0.05). The correlation coefficients for the spirometric and FOT changes were low (0.21–0.38). The authors concluded that in the initial phases of COPD (stage I), the effects of bronchodilation were greater than in healthy volunteers. Bronchodilator use improved the oscillatory mechanics in all of the studied groups of COPD patients. These improvements are reduced in more advanced phases of airway obstruction (II–IV). Pulmonary function analysis based on the FOT provides information that complements the data supplied by spirometry, contributing to an improvement in the evaluation of bronchodilator response in COPD.
Improvement of diagnostic accuracy of pulmonary function tests using clinical decision-support systems
Interpretation of the FOT results, resistance and reactance curves, and the associated indices requires adequate expertise. In diagnostic use, it may be a difficult task for the pulmonologist that is not familiar with this method. In addition, the GOLD consensusCitation1 recently noted that diagnostic simplicity is a key feature for the busy nonspecialist clinician.
Several previous studies have shown that efficient clinical decision-support systems may be developed based on machine-learning (ML) methods.Citation67 After being optimized to perform adequate classifications by learning from well-controlled examples, these programs can obtain information from different categories of signals.Citation67 Therefore, an important question is: may an ML-based system associated with FOT measurements provides an accurate method to identify COPD? Only a small number of recent studies have investigated this question.Citation68–Citation70 These studies, however, were based on impulse-oscillation systems, which present differences from classical FOT. These differences are related to the measurement method, data analysis, and related parameters.Citation71–Citation73
In this context, our group has developed and tested several clinical decision-support systems based on ML to simplify the diagnostic of COPD using FOT. The initial system was implemented using artificial neural networks (ANNs) and measurements performed in 15 normal volunteers and 15 COPD patients.Citation74 The system presented adequate accuracy (Se, Sp, and AUC >0.9). This initial result provided evidence that ANN-based clinical decision-support systems can facilitate the diagnosis of COPD by pulmonary function analysis based on the FOT.Citation74
Based on these promising findings, a second study was performed using 25 normal volunteers and 25 patients with COPD. This work included the ANN used in the previous studyCitation74 and six other ML methods.Citation75 The best classifiers reached very accurate performance (Se ≥0.87, Sp ≥0.94, and AUC ≥0.95). A perfect performance was obtained using one of these classifiers (Se, Sp, and accuracy =1). This proved the feasibility of developing an automatic system based on ML algorithms to support clinical decisions, simplifying the diagnosis of COPD by the FOT.Citation75
There is general agreement in the literature that the detection of early smoking-induced respiratory changes while these pathologic changes are still potentially reversible is of utmost importance in the prevention of COPD.Citation1 Therefore, the purpose of the next step of this line of research was the development of a clinical decision-support system to improve the accuracy of the FOT for detecting precocious respiratory abnormalities in smoking patients.Citation76 The study was based on FOT measurements performed in 56 volunteers, 28 controls, and 28 light smokers (11.2±7.3 pack-years). The established baseline was the ROC curve of the most accurate FOT parameter. A tenfold cross-validation using the mean AUC was used to determine the best classifier. A significant improvement in accuracy (0.91) compared with the baseline (0.77) was observed, which allowed for high diagnostic accuracy. These results provide evidence that ML algorithms can improve the accuracy of pulmonary function analysis, contributing to clinical diagnosis of early smoking-induced respiratory changes.
The majority of patients with COPD follow a path of disease progression that tracks the severity of airway obstruction. Therefore, the assessment of airway-obstruction severity is crucial to evaluate the risk of future exacerbations and to guide therapy.Citation1,Citation57 Automatic classifiers could contribute to the simplification of the clinical use and increase in the accuracy of the FOT in the categorization of airway-obstruction level in COPD.Citation77 The study included 168 volunteers, 42 healthy subjects, and 126 COPD subjects, who were classified according to the GOLD criteria as having mild (n=24), moderate (n=50), severe (n=37), or very severe (n=15) airway obstruction.Citation1 Initially, it was showed that FOT parameters alone did not allow high accuracy (AUC ≥0.90) in diagnosing COPD patients in the first levels of airway obstruction or in discrimination between close levels of obstruction. Therefore, ML algorithms were applied only in situations where high categorization accuracy (AUC ≥0.9) was not achieved with the FOT parameter alone. These situations are illustrated in .
Figure 5 Comparisons of the diagnostic accuracy (area under the ROC curve) obtained using the best FOT parameter (BFP) and FOT + best ML methods.
Abbreviations: FOT, forced-oscillation technique; ML, machine learning; ROC, receiver-operating characteristic.
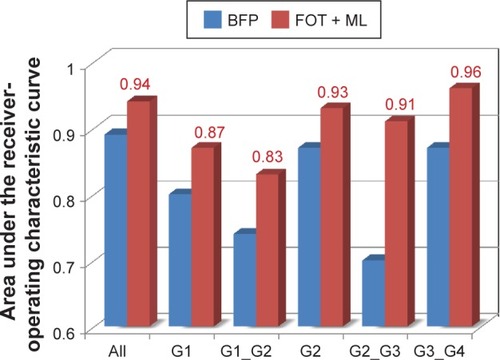
It was observed that the use of ML techniques improved categorization accuracy (). Noticeably, an AUC ≥0.9 was obtained in four of the six studied conditions. A significant improvement in categorization performance was even observed in conditions where high accuracy was not achieved (AUC increases from 0.80 to 0.87 and 0.74 to 0.83). These results show that decision-support systems based on ML classifiers can improve the categorization of COPD. These systems may help clinicians in the evaluation of disease progression, risk of exacerbations, and therapy management, contributing to an improvement in the medical services offered to patients with COPD.
Pulmonary function analysis based on systems medicine and complexity measurements
Historically, since Descartes and the Renaissance, reductionism has been the main paradigm in medicine.Citation78 Although this method has been responsible for tremendous successes in modern medicine, there are also limitations, mainly in the understanding of highly complex diseases like COPD. Complex biological systems cannot be understood only as a sum of their individual parts, and a complementary description must be developed. In this sense, the use of a systems perspective is presently part of an active debate in the respiratory medicine literature.Citation79–Citation81 This perspective investigates the integrative characteristics of a disease, rather than dividing a complex problem into its parts, as traditionally performed in reductionist analysis. Considering the respiratory system’s highly complex structure and function, a systems perspective has been suggested to understanding the respiratory diseases.Citation79 It is widely known that respiratory functions often present complex behavior.Citation79–Citation82 This is an important characteristic, since it may provide clinically relevant information, because complexity appears to be lost in the presence of an illness. GoldbergerCitation83,Citation84 proposed that the increased regularity of signals represents a “decomplexification” characteristic of illness. According to this hypothesis, health is characterized by “organized variability”, and disease is defined by “decomplexification”, increased regularity, and a reduction in variability. These methods have a rich literature in cardiovascular medicine, with important impact on clinical practice.Citation85–Citation87 However, they are just beginning to be used in respiratory physiology and pulmonary function analysis.Citation88
Dames et alCitation89 investigated the influence of airway obstruction in the complexity of the airflow pattern in COPD and its use as a marker of disease activity. It was observed that airflow patterns in COPD exhibited reduced complexity, measured by the sample entropy of the airflow, compared with healthy subjects. Interestingly, airway obstruction resulted in a reduction in complexity that was significantly correlated with spirometric indices of airway obstruction. Early changes due to mild airway obstruction were detected by the sample entropy of the airflow with an accuracy of 84%. Complementary studies investigating the change in respiratory impedance entropy (results not published) showed a reduction in complexity significantly correlated with airway obstruction. These findings are in agreement with the loss-of-complexity hypothesisCitation83,Citation84 and previous studies in asthmaticsCitation90 and may be related to the increased inflammatory characteristics and remodeling process in these patients. These results, together with previous studies,Citation29,Citation91 provide strong evidence that the association of reductionism and complex systems methods constitutes a powerful integrative approach to scientific research and clinical practice in COPD.
What are the gaps? Possible future directions
The FEV1:FVC criterion for COPD functional diagnosis is simple, independent of reference values, and has been used in numerous clinical trials. However, new COPD functional diagnosis indices have been sought by many Brazilians researchers, and the use of the FEV1:FEV6 ratio has been intensely debated.Citation7,Citation8 Different from other screening exams that have high Se, the FEV1:FEV6 ratio may be useful to exclude patients with COPD, and not to identify them.Citation92 Validation of FEV1:FEV6 for other devices using larger samples and the evaluation of its correlation with clinical outcomes may be of great interest in future trials.
The pharmacodynamic test evaluates the immediate functional changes resulting from a change in bronchial muscle tone, which is one of the elements responsible for the genesis of the obstructive process. Tavares et alCitation15 demonstrated that there were responses in RV, specific airway conductance, IC, and slow VC among patients presenting no FEV1 response. The authors recognized that functional outcomes other than FEV1 are useful for determining the reversibility of COPD and must be used to assess more accurately the extent of bronchodilator response in COPD patients. Therefore, new studies should focus on the association between pharmacodynamic response with parameters obtained through plethysmography or oscillometry and clinical outcomes that reflect ADLs.
In Brazil, some researchers have used static lung volumes to seek new markers of COPD severity, progression, and prognosis.Citation18,Citation19,Citation23 The IC, and in particular the IC:TLC ratio, was shown to be important markers of exercise intolerance, and possibly are prognostic indicators. However, additional research is necessary to estimate more accurately disease severity and prognosis in COPD patients. It is necessary to conduct longitudinal trials with large number of participants, in order to evaluate how the possible markers of COPD severity, as well as their respective cutoff points, predict disease progression and prognosis in a particular patient.Citation28
The progression of COPD is associated with impaired quality of life, increased breathlessness, and exercise intolerance. DH caused by expiratory flow limitation is markedly increased in many COPD patients. Indeed, the findings of several Brazilian studies support the concept that DH plays an important role as an etiological factor in exercise limitation in COPD patients.Citation28,Citation29 However, these studies did not measure static lung volumes at rest, and changes in lung volumes were estimated exclusively by IC rather than by end-expiratory lung volume. Therefore, new studies addressing this issue may be of interest to the advancement of current knowledge.
Ventilation inhomogeneity contributes to health status, degree of dyspnea, and functional exercise capacity in COPD patients. The N2SBW test is thought to be useful for stratifying patients and assessing COPD severity. In Brazil, the main merit of the Lopes and Mafort study was that it was the first to evaluate the association between N2SBW parameters and functional exercise capacity as measured by 6MWD in COPD patients. However, longitudinal studies are needed, especially in randomized cohorts and with a greater number of individuals, to confirm the importance of their findings.Citation37 Importantly, the N2SBW test should be used to evaluate patients with more severe COPD, as well as the relationship between the N2SBW Phase III slope and oxygen consumption during incremental testing.
A significant proportion of patients with COPD show abnormalities in TM and breathing pattern. The characterization of these changes at different COPD stages, and its association with ventilation and diaphragmatic function, may provide better pathophysiological understanding and adequate therapeutic planning. Furthermore, future studies are necessary to evaluate the effect of supplemental oxygen on breathing pattern in COPD patients.Citation46
Exacerbations of COPD lead to significant deleterious effects on the patient’s health-related quality of life and can greatly increase resource utilization and cost to the health care system.Citation93 Recently, the European Commission on TelemedicineCitation94 emphasized the high clinical potential of telemedicine in COPD and the urgent demand for research in this area. The ability of the FOT to evaluate respiratory mechanics during tidal breathing could simplify unsupervised pulmonary function monitoring. However, this depends on the development of specialized systems and protocols.Citation95,Citation96 FOT measurements associated with telemonitoring hold the promise of improving our comprehension and the administration of COPD, as well as its exacerbation. This method has the potential to provide risk predictors on a personal basis. This may contribute to evaluation of the efficacy of treatment and/or disease handling in COPD.
From a long-term perspective, future studies may improve the understanding and management of COPD and its exacerbations by integrating ML algorithms and home pulmonary function monitoring using the FOT and telemedicine services. Clinical decision-support systems may also contribute to increasing the accuracy in differential diagnoses between COPD and asthma, which may prevent substantial morbidity.Citation97,Citation98
Conclusion
Since the beginning of this millennium, research on lung function in COPD patients has been gradually increasing in Brazil. These studies used not only traditional methods but also new techniques recently incorporated in the evaluation of pulmonary function. The authors propose new COPD functional diagnosis indices, as well as new functional markers of disease severity, that are associated with quality of life, exercise tolerance, and prognosis. Some Brazilian researchers have assessed the impact of ADLs on the DH in COPD patients, while others have studied the relationship between the N2SBW test and 6MWD in these patients. Interestingly, the FOT was used in a series of studies in COPD patients and showed promising results. Finally, some research has focused on automatic clinical decision-support systems and complexity measurements. Further investigations using prospective and longitudinal design may be of interest to elucidate the use of these new methods in the diagnosis and prevention of COPD.
Acknowledgments
The Brazilian Council for Scientific and Technological Development (CNPq) and Rio de Janeiro State Research Supporting Foundation (FAPERJ) supported this study.
Disclosure
The authors report no conflicts of interest in this work.
References
- Global Initiative for Chronic Obstructive Lung DiseaseGlobal Strategy for the Diagnosis, Management, and Prevention of COPDBethesda (MD)GOLD2016
- World Health OrganizationGuidelines for Primary Health Care in Low-Resource SettingsGenevaWHO2012
- LozanoRNaghaviMForemanKGlobal and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010Lancet201238098592095212823245604
- MathersCDLoncarDProjections of global mortality and burden of disease from 2002 to 2030PLoS Med2006311e44217132052
- JemalAWardEHaoYPThunMTrends in the leading causes of death in the United States, 1970–2002JAMA2005294101255125916160134
- QueirozMCMoreiraMARabahiMFUnderdiagnosis of COPD at primary health care clinics in the city of Aparecida de Goiânia, BrazilJ Bras Pneumol201238669269923288113
- SantosSRLizziESViannaEOCharacteristics of undiagnosed COPD in a senior community centerInt J Chron Obstruct Pulmon Dis201491155116125342900
- MenezesAMJardimJRPérez-PadillaRPrevalence of chronic obstructive pulmonary disease and associated factors: the PLATINO study in São Paulo, BrazilCad Saude Publica20052151565157316158163
- MoreiraGLGazzottiMRManzanoBMIncidence of chronic obstructive pulmonary disease based on three spirometric diagnostic criteria in São Paulo, Brazil: a nine-year follow-up since the PLATINO prevalence studySao Paulo Med J2015133324525126176929
- MoreiraMAMoraesMRSilvaDGComparative study of respiratory symptoms and lung function alterations in patients with chronic obstructive pulmonary disease related to the exposure to wood and tobacco smokeJ Bras Pneumol200834966767418982203
- LundgrenFLCabralMMClimacoDCde MacedoLGCoelhoMADiasALDetermination of the efficacy of FEV6 as a surrogate for FVC in the diagnostic screening for chronic obstructive pulmonary disease through the comparison of FEV1/FVC and FEV1/FEV6 ratiosJ Bras Pneumol200733214815117724533
- Perez-PadillaRWehrmeisterFCde OcaMMInstability in the COPD diagnosis upon repeat testing vary with the definition of COPDPloS One2015103e012183225811461
- MoreiraGLDonariaLFurlanettoKCGOLD B-C-D groups or GOLD II-III-IV grades: which one better reflects the functionality of patients with chronic obstructive pulmonary disease?Chron Respir Dis201512210211025711468
- MenezesAMPerez-PadillaRWehrmeisterFCFEV1 is a better predictor of mortality than FVC: the PLATINO cohort studyPloS One2014910e10973225285441
- TavaresFMSilvaLCRubinASMeasuring forced expiratory volume in one second alone is not an accurate method of assessing response to bronchodilators in chronic obstructive pulmonary diseaseJ Bras Pneumol2005315407414
- BarussoMSGianjoppe-SantosJBasso-VanelliRPRegueiroEMPaninJCDi LorenzoVALimitation of activities of daily living and quality of life based on COPD combined classificationRespir Care201560338839825492955
- FerrariRTanniSEFaganelloMMCaramLMLuchetaPAGodoyIThree-year follow-up study of respiratory and systemic manifestations of chronic obstructive pulmonary diseaseBraz J Med Biol Res2011441465221180880
- PereiraEDPintoRAlcantaraMMedeirosMMotaRMInfluence of respiratory function parameters on the quality of life of COPD patientsJ Bras Pneumol200935873073619750324
- NonatoNLDiazONascimentoOADreyseJJardimJRLisboaCBehavior of quality of life (SGRQ) in COPD patients according to BODE scoresArch Bronconeumol201551731532125622995
- AraujoZTHolandaGDoes the BODE index correlate with quality of life in patients with COPD?J Bras Pneumol201036444745220835591
- SanchezFFFaganelloMMTanniSELuchetaPAPadovaniCRGodoyIRelationship between disease severity and quality of life in patients with chronic obstructive pulmonary diseaseBraz J Med Biol Res2008411086086519037530
- CamargoLAPereiraCADyspnea in COPD: beyond the modified Medical Research Council scaleJ Bras Pneumol201036557157821085822
- FreitasCGPereiraCAViegasCAInspiratory capacity, exercise limitation, markers of severity, and prognostic factors in chronic obstructive pulmonary diseaseJ Bras Pneumol200733438939617982530
- CavalheriVHillKDonariaLCamilloCAPittaFMaximum voluntary ventilation is more strongly associated with energy expenditure during simple activities of daily living than measures of airflow obstruction or respiratory muscle strength in patients with COPDChron Respir Dis20129423924023129801
- MendesFAMorenoILDurandMTPastreCMRamosEMVanderleiLCAnalysis of cardiovascular system responses to forced vital capacity in COPDRev Bras Fisioter201115210210821789359
- CoertjensPCKnorstMMDumkeAPasqualotoASRiboldiJBarretoSSCan the single-breath helium dilution method predict lung volumes as measured by whole-body plethysmography?J Bras Pneumol201339667568524473761
- AlbuquerqueALNeryLEVillacaDSInspiratory fraction and exercise impairment in COPD patients GOLD stages II–IIIEur Respir J200628593994416870665
- GodoyIAssessing the severity and prognosis of chronic obstructive pulmonary disease: is it still sufficient to measure FEV1 alone?J Bras Pneumol2007334xxiiixxiv17982525
- MazzucoAMedeirosWMSperlingMPRelationship between linear and nonlinear dynamics of heart rate and impairment of lung function in COPD patientsInt J Chron Obstruct Pulmon Dis2015101651166126316739
- CastroAAKumpelCRangueriRCDaily activities are sufficient to induce dynamic pulmonary hyperinflation and dyspnea in chronic obstructive pulmonary disease patientsClinics (Sao Paulo)201267431932522522756
- SilvaCSNogueiraFRPortoEFDynamic hyperinflation during activities of daily living in COPD patientsChron Respir Dis201512318919625896955
- CordoniPKBertonDCSquassoniSDScuarcialupiMENederJAFissEDynamic hyperinflation during treadmill exercise testing in patients with moderate to severe COPDJ Bras Pneumol2012381132322407036
- ScuarcialupiMEBertonDCCordoniPKSquassoniSDFissENederJACan bronchodilators improve exercise tolerance in COPD patients without dynamic hyperinflation?J Bras Pneumol201440211111824831394
- LopesAJNeryFPSousaFCCPAP decreases lung hyperinflation in patients with stable COPDRespir Care20115681164116921496367
- MonteiroMBBertonDCMoreiraMAMenna-BarretoSSTeixeiraPJEffects of expiratory positive airway pressure on dynamic hyperinflation during exercise in patients with COPDRespir Care20125791405141222348429
- RobinsonPDLatzinPVerbanckS“Consensus statement for inert gas washout measurement using multiple- and single-breath tests” (vol 41, pg 507, 2013)Eur Respir J20134251432
- LopesAJMafortTTCorrelations between small airway function, ventilation distribution, and functional exercise capacity in COPD patientsLung2014192565365925047513
- VeronezLPereiraMCda SilvaSMVolumetric capnography for the evaluation of chronic airways diseasesInt J Chron Obstruct Pulmon Dis2014998398925284998
- MasieroPRMenna-BarretoSSMoreiraMAMosmannMPMayerCMSpiroBLPerfused lung volume to thoracic gas volume ratio (perfused lung fraction) in patients with COPD and in controlsNucl Med Commun201132653053421519305
- MangueiraNMViegaILMangueiraMDPinheiroANCostaMDCorrelation between clinical parameters and health-related quality of life in women with COPDJ Bras Pneumol200935324825519390723
- SabinoPGSilvaBMBrunettoAFNutritional status is related to fat–free mass, exercise capacity and inspiratory strength in severe chronic obstructive pulmonary disease patientsClinics (Sao Paulo)201065659960520613936
- ReisMSArenaRDeusAPSimoesRPCataiAMBorghi-SilvaADeep breathing heart rate variability is associated with respiratory muscle weakness in patients with chronic obstructive pulmonary diseaseClinics (Sao Paulo)201065436937520454493
- DonáriaLMesquitaRMartinezLRelationship between sniff nasal inspiratory pressure and BODE index in patients with COPDLung2014192689790325270517
- YamagutiWPPaulinESalgeJMChammasMCCukierACarvalhoCRDiaphragmatic dysfunction and mortality in patients with COPDJ Bras Pneumol200935121174118120126918
- PaulinEYamagutiWPChammasMCInfluence of diaphragmatic mobility on exercise tolerance and dyspnea in patients with COPDRespir Med2007101102113211817644365
- SharpJTGoldbergNBDruzWSFishmanHCDanonJThoracoabdominal motion in chronic obstructive pulmonary diseaseAm Rev Respir Dis197711514756138371
- Borges-SantosEWadaJTda SilvaCMAnxiety and depression are related to dyspnea and clinical control but not with thoracoabdominal mechanics in patients with COPDRespir Physiol Neurobiol20152101625620656
- CavalcantiAGLimaCSde SaRBInfluence of posture on the ventilatory pattern and the thoracoabdominal kinematics of patients with chronic obstructive pulmonary disease (COPD)Physiother Theory Pract201430749049424678754
- JuniorEPEstevesGPFariaACMeloPLAn Internet-based system for home monitoring of respiratory muscle disordersConf Proc IEEE Eng Med Biol Soc201020105492549521096291
- AlvesGSBrittoRRCamposFCVilacaABMoraesKSParreiraVFBreathing pattern and thoracoabdominal motion during exercise in chronic obstructive pulmonary diseaseBraz J Med Biol Res2008411194595019099148
- YamagutiWPClaudinoRCNetoAPDiaphragmatic breathing training program improves abdominal motion during natural breathing in patients with chronic obstructive pulmonary disease: a randomized controlled trialArch Phys Med Rehabil201293457157722464088
- FernandesMCukierAFeltrimMIEfficacy of diaphragmatic breathing in patients with chronic obstructive pulmonary diseaseChron Respir Dis20118423724422094449
- Cancelliero-GaiadKMIkeDPantoniCBBorghi-SilvaACostaDRespiratory pattern of diaphragmatic breathing and Pilates breathing in COPD subjectsBraz J Phys Ther201418429129925075999
- FernandesMCukierAAmbrosinoNLeiteJJFeltrimMIRespiratory pattern, thoracoabdominal motion and ventilation in chronic airway obstructionMonaldi Arch Chest Dis200767420921618309699
- OostveenEMacLeodDLorinoHThe forced oscillation technique in clinical practice: methodology, recommendations and future developmentsEur Respir J20032261026104114680096
- MeloPLWerneckMGianella-NetoAAvaliação da mecânica ventilatória por oscilações forçadas: fundamentos e aplicações clínicas [Analysis of the ventilatory mechanics by forced oscillations technique: main concepts and clinical applications]J Bras Pneumol2000264194206 Portuguese
- VestboJHurdSSAgustiAGGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2013187434736522878278
- Di MangoAMLopesAJJansenJMMeloPLChanges in respiratory mechanics with increasing degrees of airway obstruction in COPD: detection by forced oscillation techniqueRespir Med2006100339941016115754
- FariaACLopesAJJansenJMMeloPLEvaluating the forced oscillation technique in the detection of early smoking-induced respiratory changesBiomed Eng Online200982219781078
- SwetsJAMeasuring the accuracy of diagnostic systemsScience19882404857128512933287615
- FariaACCostaAALopesAJJansenJMMeloPLForced oscillation technique in the detection of smoking-induced respiratory alterations: diagnostic accuracy and comparison with spirometryClinics (Sao Paulo)201065121295130421340218
- SilvaKKLopesAJJansenJMde MeloPLTotal inspiratory and expiratory impedance in patients with severe chronic obstructive pulmonary diseaseClinics (Sao Paulo)201166122085209122189734
- SilvaKKFariaACLopesAJde MeloPLWithin-breath respiratory impedance and airway obstruction in patients with chronic obstructive pulmonary diseaseClinics (Sao Paulo)201570746146926222814
- Di MangoAMLopesAJJansenJMMeloPLForced oscillation technique assessing bronchodilator response in asthmatics and COPD patientsChest2002122Suppl 4138s
- CostaGMFariaACDi MangoAMLopesAJJansenJMMeloPLBronchodilation in COPD: beyond FEV1 – the effect of albuterol on resistive and reactive properties of the respiratory systemJ Bras Pneumol200935432533319466270
- da CostaGMFariaACDi MangoAMLopesAJde MeloPLRespiratory impedance and response to salbutamol in healthy individuals and patients with COPDRespiration201488210111124992904
- CleophasTJZwindermanAHMachine Learning in MedicineDordrecht, Portuguese. The NetherlandsSpringer2013
- BarúaMNazeranHNavaPGrandaVDiongBClassification of pulmonary diseases based on impulse oscillometric measurements of lung function using neural networksConf Proc IEEE Eng Med Biol Soc200453848385117271135
- BarúaMNazeranHNazeranHNavaPDiongBGoldmanMClassification of impulse oscillometric patterns of lung function in asthmatic children using artificial neural networksConf Proc IEEE Eng Med Biol Soc2005132733117282180
- MerazENazeranHGoldmanMNavaPDiongBImpulse oscillometric features of lung function: towards computer-aided classification of respiratory diseases in childrenConf Proc IEEE Eng Med Biol Soc200820082443244619163196
- BirchMMacLeodDLevineMAn analogue instrument for the measurement of respiratory impedance using the forced oscillation techniquePhysiol Meas200122232333911411243
- HellinckxJCauberghsMDe BoeckKDemedtsMEvaluation of impulse oscillation system: comparison with forced oscillation technique and body plethysmographyEur Respir J200118356457011589356
- RitzTDahmeBDuboisABGuidelines for mechanical lung function measurements in psychophysiologyPsychophysiology200239554656712236321
- AmaralJLFariaACLopesAJJansenJMMeloPLAutomatic identification of chronic obstructive pulmonary disease based on forced oscillation measurements and artificial neural networksConf Proc IEEE Eng Med Biol Soc201020101394139721096340
- AmaralJLLopesAJJansenJMFariaACMeloPLMachine learning algorithms and forced oscillation measurements applied to the automatic identification of chronic obstructive pulmonary diseaseComput Methods Programs Biomed2012105318319322018532
- AmaralJLLopesAJJansenJMFariaACMeloPLAn improved method of early diagnosis of smoking-induced respiratory changes using machine learning algorithmsComput Methods Programs Biomed2013112344145424001924
- AmaralJLLopesAJFariaACMeloPLMachine learning algorithms and forced oscillation measurements to categorise the airway obstruction severity in chronic obstructive pulmonary diseaseComput Methods Programs Biomed2015118218619725435077
- AhnACTewariMPoonCSPhillipsRSThe limits of reductionism in medicine: could systems biology offer an alternative?PLoS Med200636709713
- KaminskyDAIrvinCGSterkPJComplex systems in pulmonary medicine: a systems biology approach to lung diseaseJ Appl Physiol201111061716172221183622
- MacklemPTComplexity and respiration: a matter of life and deathHamidQShannonJMartinJPhysiologic Basis of Respiratory DiseaseShelton (CT)People’s Medical Publishing House2005605609
- MacklemPTEmergent phenomena and the secrets of lifeJ Appl Physiol200810461844184618202170
- GlennyRWEmergence of matched airway and vascular trees from fractal rulesJ Appl Physiol201111041119112921164156
- GoldbergerALFractal variability versus pathologic periodicity: complexity loss and stereotypy in diseasePerspect Biol Med19974045435619269744
- GoldbergerALPengCKLipsitzLAWhat is physiologic complexity and how does it change with aging and disease?Neurobiol Aging2002231232611755014
- AhmadSTejujaANewmanKDZarychanskiRSeelyAJClinical review: a review and analysis of heart rate variability and the diagnosis and prognosis of infectionCrit Care200913623220017889
- LombardiFChaos theory, heart rate variability, and arrhythmic mortalityCirculation2000101181010618296
- GoldbergerALComplex systemsProc Am Thorac Soc20063646747116921107
- SukiBIn search of complexityJ Appl Physiol201010961571157220847129
- DamesKKLopesAJde MeloPLAirflow pattern complexity during resting breathing in patients with COPD: effect of airway obstructionRespir Physiol Neurobiol2014192394724334010
- VeigaJLopesAJJansenJMMeloPLFluctuation analysis of respiratory impedance waveform in asthmatic patients: effect of airway obstructionMed Biol Eng Comput201250121249125923011080
- TeulierMFiammaMNStrausCSimilowskiTAcute bronchodilation increases ventilatory complexity during resting breathing in stable COPD: toward mathematical biomarkers of ventilatory function?Respir Physiol Neurobiol2013185247748022999916
- EkeAHermanPKocsisLKozakLRFractal characterization of complexity in temporal physiological signalsPhysiol Meas2002231R1R3811876246
- PasqualeMKSunSXSongFHartnettHJStemkowskiSAImpact of exacerbations on health care cost and resource utilization in chronic obstructive pulmonary disease patients with chronic bronchitis from a predominantly Medicare populationInt J Chron Obstruct Pulmon Dis2012775776423152680
- European ParliamentCommunication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions on telemedicine for the benefit of patients, healthcare systems and society2008 Available from: http://eur-lex.europa.eu/legal-content/EN/ALL/?uri=CELEX%3A52008DC0689Accessed May 5, 2016
- RigauJFarréRRocaJMarcoSHermsANavajasDA portable forced oscillation device for respiratory home monitoringEur Respir J200219114615011843313
- DellacaRLGobbiAPastenaMPedottiACelliBHome monitoring of within-breath respiratory mechanics by a simple and automatic forced oscillation technique devicePhysiol Meas2010314N11N2420182000
- PriceDBYawnBPJonesRCImproving the differential diagnosis of chronic obstructive pulmonary disease in primary careMayo Clin Proc201085121122112921123639
- PearsonMAyresJGSarnoMMasseyDPriceDDiagnosis of airway obstruction in primary care in the UK: the CADRE (COPD and Asthma Diagnostic/management REassessment) programme 1997–2001Int J Chron Obstruct Pulmon Dis20061443544318044099