?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Sitagliptin, a dipeptidyl peptidase-4 inhibitor, has been reported to promote cardioprotection in diabetic hearts by limiting hyperglycemia and hyperlipidemia. However, little is known about the involvement of the Janus kinase/signal transducer and activator of transcription (JAK/STAT) pathway modulation in the cardioprotective effects of sitagliptin. The current study aimed to investigate the protective effects of sitagliptin against diabetic cardiomyopathy (DCM), focusing on the modulation of the JAK/STAT pathway. Diabetes was induced by streptozotocin injection, and rats received sitagliptin orally and daily for 90 days. Diabetic rats exhibited hyperglycemia, hyperlipidemia, and a significant increase in heart-to-body weight (HW/BW) ratio. Serum troponin I and creatine kinase MB, cardiac interleukin-6 (IL-6), lipid peroxidation, and nitric oxide levels showed significant increase in diabetic rats. In contrast, both enzymatic and nonenzymatic antioxidant defenses were significantly declined in the heart of diabetic rats. Histopathological study revealed degenerations, increased collagen deposition in the heart of diabetic rats. Sitagliptin alleviated hyperglycemia, hyperlipidemia, HW/BW ratio, histological architecture, oxidative stress, and inflammation, and rejuvenated the antioxidant defenses. In addition, cardiac levels of pJAK2 and pSTAT3 were increased in diabetic rats, an effect which was remarkably decreased after sitagliptin treatment. In conclusion, these results confer an evidence that sitagliptin has great therapeutic potential on DCM through down-regulation of the JAK/STAT signaling pathway.
Introduction
Cardiovascular complications represent the main cause of hospitalization and death in diabetic patients.Citation1 Diabetic cardiomyopathy (DCM) is an independent complication of diabetes characterized by myocardial dysfunction in the absence of other heart diseases.Citation2 Diabetic patients have a worse prognosis and are more susceptible to heart failure than hypertension or ischemic heart disease patients.Citation3 Previous studies have demonstrated that hyperglycemia, hyperlipidemia, inflammation, apoptosis, and oxidative stress are probably involved in DCM pathophysiology.Citation4–Citation6 Hyperglycemia-derived reactive oxygen and nitrogen species (ROS and RNS) play a central role in DCM.Citation7 In addition, chronic low-grade inflammation is a feature of DCM in human diabetics.Citation8 As an early response to myocardial injury, inflammatory signaling in cardiomyocytes entails an activation of nuclear factor-κB and increased expression of proinflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha.Citation9
The Janus kinase/signal transducer and activator of transcription (JAK/STAT) signaling pathway is an intracellular signaling pathway closely related to cardiac hypertrophy.Citation10 This pathway plays a key role in cell growth, survival, and differentiation and in regulating gene expression.Citation11 Upon phosphorylation by JAK, STAT proteins translocate into the nucleus, bind to the promoter region of target genes, and regulate their transcription.Citation12 In the heart, STATs regulate the expression of gene encoding proteins involved in angiogenesis, extracellular matrix composition, inflammation, apoptosis, and cellular signaling.Citation13,Citation14 IL-6 and its family-related proteins transduce their signals via glycoprotein 130 (gp130) mostly to STAT3 and play a key role in the development of heart failure and cardiac hypertrophy.Citation15 It has been indicated that high glucose activates the JAK/STAT signaling of vascular endothelial cells in vitro through phosphorylation of JAK2 and subsequently STAT3, leading to the proliferation of endothelial cells.Citation16 Thus, modulation of the IL-6-gp 130-JAK/STAT signaling pathway represents an important strategy for the treatment of DCM.
Dipeptidyl peptidase-4 (DPP-4) inhibitors, as sitagliptin, are a class of antidiabetic drugs that inhibit the degradation of insulinotropic incretins, mainly glucagon-like peptide-1 (GLP-1).Citation17 GLP-1 is released from intestinal L-cells and regulates circulating glucose levels by enhancing insulin secretion. Studies showed that GLP-1 confers cardioprotection after congestive heart failure, ischemia, and myocardial infarction.Citation18,Citation19 Sitagliptin has been reported to promote cardioprotection in type 2 diabetic hearts via GLP-1 stabilization and by limiting hyperglycemia and hyperlipidemia.Citation20 However, the issues of an involvement of the JAK/STAT pathway modulation in the protective effects of sitagliptin against DCM have not been previously reported. Therefore, we have investigated the cardioprotective role of sitagliptin in streptozotocin (STZ)-induced diabetic rats, focusing on its modulatory effect on the JAK/STAT pathway.
Materials and methods
STZ and sitagliptin (Januvia) were purchased from Sigma-Aldrich (St Louis, MO, USA) and Merck & Co., Inc. (Whitehouse, NJ, USA), respectively. Rabbit polyclonal anti-phospho-JAK2 and goat anti-phospho-STAT3 (pSTAT3) were supplied by Santa Cruz Biotechnology Inc. (Dallas, TX, USA). All other chemicals were of analytical grade and were obtained from standard commercial supplies.
Experimental animals
Male Wistar rats (10 weeks old) weighing between 140 and 160 g, obtained from the Experimental Animal Center, College of Pharmacy, King Saud University (Saudi Arabia), were used in this investigation. Rats were housed in special cages at controlled temperature of 20°C–22°C and humidity of 60%, fed a standard rat pellet chow with free access to tap water ad libitum and kept for 1 week before the experiment for acclimatization. All animal procedures were performed in accordance with the guidelines provided by the Experimental Animal Laboratory and approved by the Animal Care and Use Committee of the College of Pharmacy, King Saud University (Saudi Arabia).
Induction of type 1 diabetes mellitus and experimental design
Diabetes was induced in overnight fasted rats by a single intraperitoneal injection of 55 mg/kg body weight (BW) freshly prepared STZ, dissolved in 0.1 M citrate buffer (pH 4.5). Seventy-two hours later, blood glucose levels were determined using MEDISAFE MINI blood glucose reader (TERUMO Corporation, Hatagaya, Tokyo, Japan), and rats having blood glucose levels $200 mg/dL were selected for the experiment.
Thirty-two (16 normal +16 diabetic) rats were divided into four equal groups, each consisting of eight (N=8) animals as follows:
Group I: Control
Group II: Control +100 mg/kg/day sitagliptin
Group III: Diabetic
Group IV: Diabetic +100 mg/kg/day sitagliptin.
Sitagliptin was dissolved in water and supplied for 90 days via oral gavage; the dosage was balanced as indicated by any change in the BW over the entire period of study. At the end of the experiment, blood samples collected from each animal were allowed to coagulate at room temperature and then centrifuged at 3,000 rpm for 15 minutes to separate serum. Immediately after sacrifice, hearts were quickly excised, cleaned, and perfused with ice-cold saline and homogenized in phosphate-buffered saline or fixed in 10% formalin.
Determination of troponin I and creatine kinase MB
Serum levels of troponin I and activity of creatine kinase MB (CK-MB) were measured using specific rat enzyme-linked immunosorbent assay kits purchased from EIAab (Wuhan, People’s Republic of China) according to the manufacturer’s instructions. Standard curves were prepared and troponin I and CK-MB in the samples were determined from the prepared standard curves.
Determination of lipid profile and cardiovascular risk indices
Serum levels of total cholesterol, triglycerides, and high-density lipoprotein (HDL) cholesterol were assayed according to the methods of Allain et al,Citation21 Fossati and Prencipe,Citation22 and Burstein et alCitation23 using commercial diagnostic kits purchased from United Diagnostics Industry (Riyadh, Saudi Arabia). Serum low-density lipoprotein (LDL) cholesterol level was calculated from the formula:
Very low-density lipoprotein (vLDL) cholesterol concentration was calculated according to the following formula:
Cardiovascular risk indices were calculated according to RossCitation24 as follows:
Determination of oxidative stress and antioxidant defenses
Lipid peroxidation (assayed as malondialdehyde), reduced glutathione (GSH), and nitric oxide (NO) levels were determined in heart homogenate according to the methods of Preuss et al,Citation25 Beutler et al,Citation26 and Montgomery and Dymock,Citation27 respectively. Activities of the antioxidant enzymes, superoxide dismutase and catalase, were measured according to the methods of Marklund and MarklundCitation28 and Cohen et al,Citation29 respectively. Protein content was determined using Bradford reagent.
Determination of IL-6
Levels of IL-6 were determined in the cardiac homogenates using specific enzyme-linked immunosorbent assay kits (R&D Systems, Inc., Minneapolis, MN, USA) following the manufacturer’s instructions. Concentration of IL-6 in the samples was determined from standard curve constructed by using standard cytokine.
Histopathological study
Histological processing was prepared as described previously.Citation30 The excised hearts were cleaned and fixed in 10% buffered formalin for 24 hours. The fixed samples were processed to prepare 5-μm thick paraffin sections, which were then stained with hematoxylin and eosin (H&E) and Masson’s trichrome stains. High-resolution digital scans of all stained slides were created with a ScanScope scanner (Aperio Technologies, Vista, CA, USA) and were viewed and analyzed using Aperio’s viewing and image analysis tools.
Immunohistochemical examination of pJAK2 and pSTAT3
Immunostaining of the heart sections for the detection of pJAK2 and pSTAT3 was performed using streptavidin-biotinylated horseradish peroxidase (Novalink Max Polymer detection system; Novocastra Laboratories, Newcastle, UK). In brief, sections were incubated in 3% hydrogen peroxide in distilled water for 5 minutes to block endogenous peroxidase activity and then washed in Tris-buffered saline (pH 7.6) for 10 minutes. Nonspecific binding of antibodies was blocked by incubation with protein block (Novocastra) for 5 minutes. Sections were incubated with rabbit polyclonal anti-pJAK2 and goat polyclonal anti-pSTAT3 primary antibodies (Santa Cruz Biotechnology Inc.) diluted 1:100 at room temperature for 1 hour. The sections were washed in Tris-buffered saline three times and incubated with biotinylated IgG (Novocastra) for 30 minutes. After washing in Tris-buffered saline and incubation with Novolink polymer (Novocastra) for 30 minutes, peroxidase was detected with diaminobenzedine substrate (Novocastra). Sections were then washed in distilled water, stained with Mayer’s hematoxylin, and mounted in DPX. The same procedure, with the omission of incubation in primary antibodies, was followed for negative control sections.
Statistical analysis
Data were analyzed using GraphPad Prism 5 (GraphPad Software, Inc., La Jolla, CA, USA), and all statistical comparisons were made by means of the one-way analysis of variance test followed by Tukey’s test post hoc analysis. Results were expressed as mean ± standard error of the mean and a P-value <0.05 was considered significant.
Results
Sitagliptin represses hyperglycemia and BW loss and prevents cardiac hypertrophy in diabetic rats
BW of control and diabetic rats showed nonsignificant (P>0.05) differences at the start of the treatment period (). After 90 days, diabetic rats exhibited a significant (P<0.001) decrease in BW when compared with the normal control rats. Treatment with sitagliptin significantly (P<0.05) protected against diabetes-induced BW loss. On the other hand, heart-to-body weight (HW/BW) ratio showed a significant (P<0.01) increase in diabetic rats when compared with the control group. Sitagliptin administration produced a significant (P<0.01) decrease in HW/BW ratio in the diabetic rats.
Table 1 Effect of sitagliptin on BW, HW, and blood glucose in control and diabetic rats
Diabetic rats showed a significant (P<0.001) increase in blood glucose levels both before and after the treatment period. Treatment of the diabetic rats with sitagliptin for 90 days significantly (P<0.001) alleviated blood glucose levels.
Of note, sitagliptin produced a nonsignificant (P>0.05) effect on BW, HW, and blood glucose parameters when supplemented to control rats.
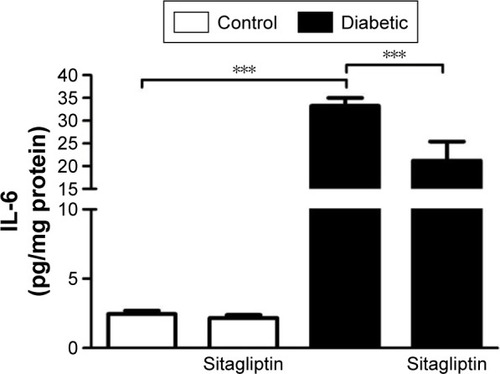
Sitagliptin reduces circulating troponin I and CK-MB in diabetic rats
Data represented in show the effects of sitagliptin on troponin I levels and CK-MB activity in serum of control and diabetic rats. STZ-induced diabetic rats exhibited significant (P<0.01) increase in serum troponin I levels when compared with the control rats. Treatment of diabetic rats with sitagliptin for 90 days produced a marked (P<0.01) decrease in serum troponin I levels ().
Figure 1 Effect of sitagliptin on (A) troponin I level and (B) CK-MB activity.
Abbreviations: CK-MB, creatine kinase MB; SEM, standard error of the mean.
Similarly, STZ administration produced a significant (P<0.05) increase in serum CK-MB activity. Oral treatment of the STZ-induced diabetic rats with sitagliptin significantly (P<0.05) ameliorated the altered CK-MB activity, as depicted in . Oral supplementation of sitagliptin to the normal rats produced a nonsignificant (P<0.05) effect on either serum troponin I levels or CK-MB activity.
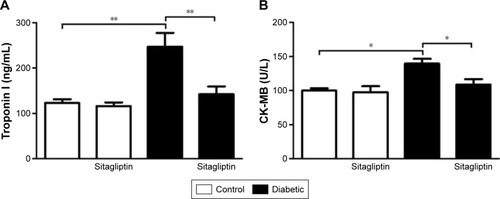
Sitagliptin alleviates lipid profile and cardiovascular risk indices in diabetic rats
Data summarized in represent the effect of sitagliptin on serum lipid profile and cardiovascular risk indices in both control and STZ-induced diabetic rats. Diabetic rats exhibited significant (P<0.001) increase in serum cholesterol (), triglycerides (), LDL cholesterol (), and vLDL cholesterol levels () when compared with the corresponding control group. HDL cholesterol showed a significant (P<0.001) decrease in serum of STZ-induced diabetic rats (). On the other hand, diabetic rats treated with sitagliptin for 90 days showed significant (P<0.001) alleviation in all parameters of the lipid profile. Control rats treated with sitagliptin showed a nonsignificant (P>0.05) change in their lipid profile when compared with the control group.
Figure 2 Effect of sitagliptin on serum lipid profile and cardiovascular indices.
Abbreviations: HDL, high-density lipoprotein; LDL, low-density lipoprotein; SEM, standard error of the mean; T cholesterol, total cholesterol; vLDL, very low-density lipoprotein.
To explore the impact of diabetes-induced hyperlipidemia and protective effect of sitagliptin on the heart, the cardiovascular risk indices, total cholesterol/HDL cholesterol (), and LDL cholesterol/HDL cholesterol () were calculated. Diabetic rats showed significant (P<0.001) increase in both total cholesterol/HDL cholesterol and LDL cholesterol/HDL cholesterol ratios when compared with the control rats. Conversely, diabetic rats supplemented with sitagliptin for 90 days exhibited marked (P<0.001) improvement in their recorded cardiovascular risk indices. As expected, sitagliptin produced a nonsignificant (P>0.05) effect on total cholesterol/HDL cholesterol and LDL cholesterol/HDL cholesterol ratios when supplemented to normal rats.
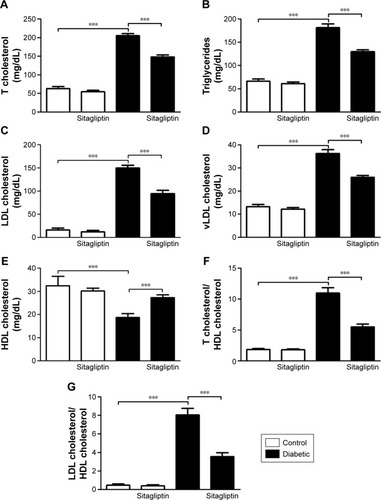
Sitagliptin attenuates oxidative stress in heart of diabetic rats
To investigate the effect of sitagliptin on the cardiac redox status, lipid peroxidation, NO, and activity of antioxidant enzymes under homeostatic and diabetic conditions were determined.
STZ-induced diabetic rats exhibited significantly (P<0.001) increased malondialdehyde and NO levels in the heart as compared with their respective normal controls. Treatment of the diabetic rats with sitagliptin for 90 days markedly (P<0.001) decreased cardiac malondialdehyde () and NO levels ().
Figure 3 Effect of sitagliptin on oxidative stress and antioxidant defense system parameters.
Abbreviations: CAT, catalase; GSH, reduced glutathione; MDA, malondialdehyde; NO, nitric oxide; SEM, standard error of the mean; SOD, superoxide dismutase.
In contrast, GSH content in the heart of diabetic rats was significantly (P<0.001) declined, as represented in . Treatment with sitagliptin produced a significant (P<0.001) alleviation of cardiac GSH content in diabetic rats. Activities of the antioxidant enzymes, superoxide dismutase () and catalase (), were investigated in control and diabetic rats, and it was found that the activities of the enzymes exhibited a significant decrease in GSH content of the heart of diabetic rats, an effect that was significantly reduced after the administration of sitagliptin. Concerning its effects on the redox status in normal rats, sitagliptin exerted a nonsignificant effect.
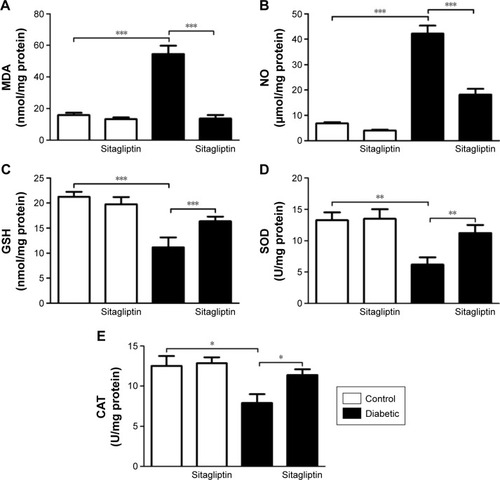
Sitagliptin decreases cardiac IL-6 levels in diabetic rats
The proinflammatory cytokine IL-6 showed a significant (P<0.001) increase in the heart of diabetic rats when compared with the control group (). Treatment of the diabetic rats with sitagliptin for 90 days significantly (P<0.001) improved cardiac levels of IL-6. In addition, sitagliptin supplementation to normal rats produced a nonsignificant (P>0.05) effect on cardiac IL-6 levels when compared with the control rats.
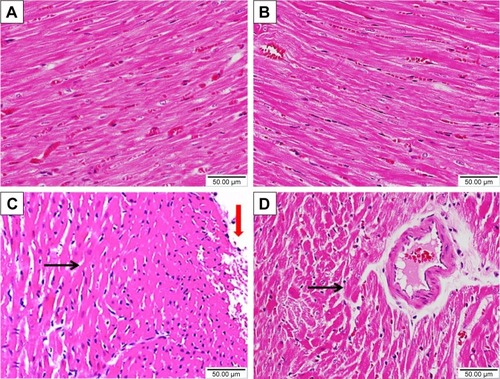
Sitagliptin improves histological architecture and decreases collagen deposition in diabetic rats
Histopathological examination of the H&E-stained heart sections of control rats showed normal heart tissue with normal features of myocardium cells, blood vessels, and endomysium (). Heart sections from sitagliptin-treated rats revealed apparently normal endocardium, myocardium, and endomysium (). On the other hand, sections in the heart of STZ-induced diabetic rats showed focal areas of myocardium degeneration and many myocardium cell degeneration (). Diabetic rats treated with sitagliptin () showed few myocardial cell degenerations.
Figure 5 Effect of sitagliptin on histological changes in the heart of control and diabetic rats.
Abbreviation: H&E, hematoxylin and eosin.
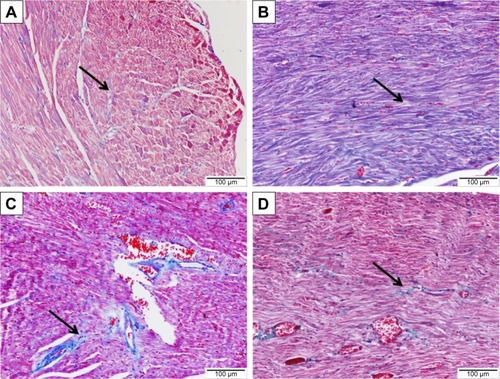
To demonstrate the effects of diabetes and treatment with sitagliptin on collagen deposition, heart sections were stained with Masson’s trichrome. Heart sections showed normal distribution and normal amount of cardiac fibrous tissue in both control and sitagliptin-treated rats, as represented in , respectively. Sections from the heart of STZ-induced diabetic rats () showed large patches of strong fibrous tissue reactivity. STZ-induced diabetic rats treated with sitagliptin showed small patches of fibrous tissue in the Masson’s trichrome-stained heart sections ().
Figure 6 Effect of sitagliptin on collagen deposition in the heart of control and diabetic rats.
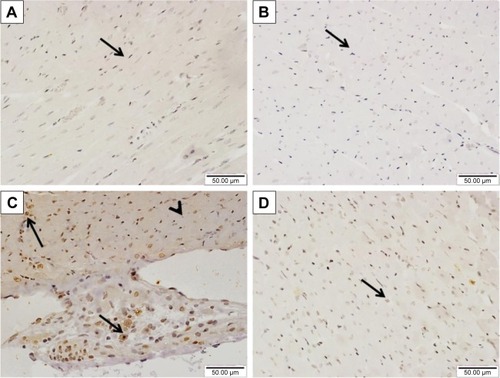
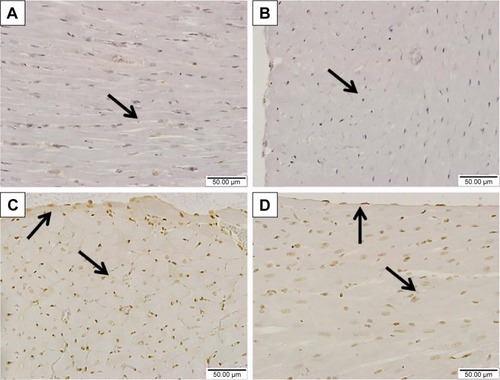
Sitagliptin reduces cardiac JAK2 and STAT3 phosphorylation in diabetic rats
The effect of sitagliptin on the expression of pJAK2 and pSTAT3 in the heart of normal and diabetic rats was determined by immunohistochemical staining. Heart sections from control and sitagliptin-treated rats, immunostained with pJAK2 primary antibody, revealed negative immune reaction of the nuclei and cytoplasm (). Heart sections of the STZ-induced diabetic rats showed strong immune reactivity of myocardium cell nuclei and moderate immune reaction of the cytoplasm (). In contrast, sitagliptin-treated diabetic rats showed few immunopositive nuclei ().
Figure 7 Effect of sitagliptin on JAK2 phosphorylation in the heart of control and diabetic rats.
Similarly, the immunohistochemical staining of the heart with pSTAT3 primary antibody revealed the absence of immune positivity especially in the nuclei of normal control () and sitagliptin-treated rats (). STZ-induced diabetic rats showed strong immune reactivity of almost all of myocardium cell nuclei and the endocardium endothelium cells (). On the other hand, diabetic rats treated with sitagliptin for 90 days showed many immunopositive nuclei of both endocardium endothelium and myocardium cells ().
Figure 8 Effect of sitagliptin on STAT3 phosphorylation in the heart of control and diabetic rats.
Discussion
The JAK/STAT signaling pathway regulates different genes involved in inflammation, fibrosis, and cell growth and differentiation.Citation11,Citation12 The present study outlines the protective effects of sitagliptin against diabetes-induced cardiomyopathy in STZ-induced diabetic rat model. Sitagliptin attenuated cardiac oxidative stress, inflammation, and collagen deposition and reduced the JAK/STAT expression, thus suggesting the potential benefit of sitagliptin to halt the progression of DCM.
As previously reported STZ-induced diabetic rats exhibited BW loss and increased blood glucose.Citation31,Citation32 Treatment of the STZ-induced diabetic rats with sitagliptin was associated with reduced blood glucose that may have contributed to the greatly alleviated BW. In contrast, we observed no difference in blood glucose levels between sitagliptin-treated and normal rats. Similar findings were reported in the study of Connelly et alCitation33 who studied the effect of DPP-4 inhibition on cardiac dysfunction in experimental diabetic rats. Although not necessarily seen in type 1 diabetic patients, these results are typical of STZ-induced diabetic animals in which high glucose provoked glucagon and insulin secretion is impaired.Citation34
Here, the STZ-induced diabetic rats showed notable increase in the HW/BW ratio, which demonstrates cardiac hypertrophy. The diabetic heart is metabolically characterized by increased fatty acid oxidation, leading to lipid accumulation in the myocardium.Citation35,Citation36 In the same context, Wang et alCitation37 reported that STZ-induced diabetic rats exhibited cardiac hypertrophy after 8 weeks of diabetes induction. Sitagliptin treatment produced a positive effect on HW/BW ratio and was thus able to prevent diabetes-associated cardiac hypertrophy. DPP-4 inhibition has been reported to reduce cardiac myocyte hypertrophy and alleviate diastolic dysfunction in diabetic rats with myocardial infarction.Citation33
This beneficial effect of sitagliptin could be directly attributable to the lowered serum lipids and increased HDL cholesterol levels. Serum total cholesterol, triglycerides, and LDL cholesterol were significantly increased, and HDL cholesterol was significantly decreased in diabetic rats, an effect that was reversed following sitagliptin treatment. In diabetes, the elevated level of serum lipids causes the risk of coronary heart diseaseCitation38 while HDL was found to be cardioprotective.Citation39 In addition, the recorded values of atherogenic indices showed the bad impact of diabetes-induced dyslipidemia on the cardiovascular system and were further confirmed by the elevated levels of CK-MB and troponin I. Increases in circulating levels of CK-MB represent a sensitive and powerful predictor of increased cardiac complications.Citation40 Furthermore, studies have demonstrated the relation between CK-MB and troponin I elevation and the onset of myofibrillar disintegration and increased permeability caused by inflammation.Citation41 Recently, we have demonstrated elevations in CK-MB and troponin I in rats with cardiac hypertrophy.Citation30 Reduction of these indices in sitagliptin-treated diabetic rats strongly supports the notion that DPP-4 inhibitors may reduce the risk of developing heart diseases.
Oxidative stress constitutes an important factor implicated in the development of DCM. Several lines of evidence indicate that hyperglycemia in diabetes is associated with increased mitochondrial production of ROS and RNS.Citation42 In addition, elevated free fatty acids in the diabetic heart modulates the mitochondrial electron chain and activates nicotinamide adenine dinucleotide phosphate oxidases to generate superoxide.Citation43 Superoxide can combine with NO forming highly reactive and damaging peroxynitrite species.Citation44 The current findings showed increased lipid peroxidation and NO levels in the heart of STZ-induced diabetic rats, demonstrating oxidative stress condition. Lipid peroxidation, produced from the reaction of ROS with membrane lipids, has been associated with altered membrane structure and enzyme inactivation.Citation45 This enhancement of lipid peroxidation might be due to hyperglycemia-induced free radical production. The elevated NO levels could be directly connected to activated inducible NO synthase. A previous study has demonstrated that inducible NO synthase is able to generate superoxide anions independent of NO production.Citation46
By comparison, STZ-induced diabetic rats exhibited significant decrease in cardiac GSH content as well as activity of antioxidant defense enzymes. GSH depletion has been linked to declined cellular defense against ROS-induced injury, leading to necrotic cell death.Citation47 Superoxide dismutase catalyzes the dismutation of superoxide radicals to oxygen and hydrogen peroxide. The latter is converted to molecular oxygen and water. Glutathione peroxidase serves a similar antioxidant role by degrading hydrogen peroxide and lipid peroxides to water and lipid alcohols.Citation48 Therefore, these antioxidants represent a vital line of defense against diabetes-induced oxidative stress.
Interestingly, diabetic rats treated with sitagliptin showed significant decrease in cardiac lipid peroxidation and NO levels, with concomitant enhancement of the antioxidant defenses. In agreement with our findings, treatment with sitagliptin for 6 weeks decreased lipid peroxidation in the heart of Zucker diabetic fatty rats.Citation49 In addition, Kelleni et alCitation50 demonstrated a protective effect of sitagliptin against doxorubicin-induced cardiotoxicity and oxidative stress in rats. Another supporting study recently conducted by Alam et alCitation51 showed that sitagliptin prevents oxidative stress of heart and kidney in two kidney and one clip rats. These data support the premise that sitagliptin can protect against DCM via suppressing oxidative stress.
Cardiac inflammation, fibrosis, and apoptosis have been recognized in DCMCitation52,Citation53 as a consequence of oxidative stress.Citation54 Therefore, diabetes induces both functional and structural disturbances in the myocardium. In the present investigation, the proinflammatory cytokine IL-6 showed a significant increase in the heart of diabetic rats. Studies demonstrated that concentrations of inflammatory cytokines including IL-6 increased in the serum of experimental animal modelsCitation55 and diabetic patients,Citation56 leading to diastolic dysfunction. The beneficial effect of sitagliptin on cardiac oxidative stress was accompanied by an improvement of IL-6 in the heart of diabetic rats. These findings point to an anti-inflammatory effect exerted by sitagliptin. In this context, Ferreira et alCitation49 and Kelleni et alCitation50 reported the anti-inflammatory effect of sitagliptin in Zucker diabetic fatty rats and doxorubicin-induced cardiotoxicity animal model, respectively.
The histological findings showed focal areas of myocardium degeneration and large patches of strong fibrous tissue reactivity in the heart sections of STZ-induced diabetic rats. These alterations could be directly connected to the hyperglycemia-induced oxidative stress and inflammation. Increased ROS are known to cause cardiac dysfunction by direct damage to DNA and proteins and by inducing apoptosis. Cardiac fibrosis occurs as a consequence of inflammation and cell injuryCitation57 as confirmed by various studiesCitation4,Citation58 where suppression of inflammation has been shown to improve DCM, enhance cardiac function, and reduce cardiac fibrosis. Furthermore, studies have demonstrated the role of oxidative stress as an important regulator of pro-fibrotic processes in the heart.Citation59 The study by Suzuki et alCitation53 showed ameliorated hyperglycemia-induced cardiac fibrosis by treatment with antioxidant. In addition, Alam et alCitation51 revealed the antifibrotic activity of sitagliptin in kidneys and heart of two kidney and one clip rats. Here, sitagliptin was able to protect the heart against diabetes-induced cellular injury and fibrosis probably through its dual ability to reduce chronic inflammation and improve the redox balance.
We hypothesized that the beneficial effects of sitagliptin in DCM might be associated with the modulation of the JAK/STAT pathway. To verify our findings, phosphorylated JAK2 and STAT3 were determined in the heart of diabetic and sitagliptin-treated rats. Diabetic rats exhibited marked increase in phosphorylation levels of JAK2 and STAT3 as seen in the immunohistochemically stained heart sections. Therefore, it is clearly apparent that diabetes induces upregulation of the JAK/STAT pathway in the heart of rats as recently reported in type 2 diabetic rats.Citation60 JAK/STAT pathway is closely related to cardiac hypertrophy caused by heart failure, pressure overload,Citation10 and isoproterenol administration.Citation30 The upregulated JAK2/STAT3 signaling in the present investigation was positively correlated with the cardiac IL-6 levels. IL-6 transduces hypertrophic signals via gp130 predominantly to STAT3Citation15 in cardiac myocytes and satellite cells.Citation61 Therefore, the IL-6-gp130-JAK/STAT signaling pathway has a key role in cardiac hypertrophy.Citation30 Compared with DCM rats, the phosphorylation levels of JAK2 and STAT3 in myocardium of rats treated with sitagliptin were declined. Because JAK/STAT signaling is induced by IL-6, the recorded down-regulation could be attributed to the anti-inflammatory effect of sitagliptin. Modulation of this pathway mediates the antifibrotic effect of sitagliptin in diabetic rat heart. Previous studies have demonstrated that inhibiting the JAK/STAT signaling pathway can decrease the synthesis of transforming growth factor-beta 1 in mesangial cells cultured in high glucoseCitation12 and type 2 diabetic rat heart.Citation60 Transforming growth factor-beta 1 is a polypeptide that regulates cell growth and differentiation, and promotes myocardial fibrosis.Citation62 These findings demonstrate that sitagliptin has a protective effect on diabetes-induced myocardial injury by down-regulating JAK/STAT signaling pathway.
Conclusion
The present study demonstrates that sitagliptin exerts protective effects against DCM. Sitagliptin has shown strong modulatory effect against hyperglycemia-induced cardiac inflammation and oxidative stress via enhancement of antioxidant defenses and suppression of ROS production. In addition, sitagliptin showed strong antihyperglycemic and antihyperlipidemic effects, attenuated collagen deposition and cardiac hypertrophy, and reduced severity of histopathological lesions in heart of diabetic rats. The study provides evidence that the cardioprotective effect of sitagliptin is related to down-regulation of the JAK/STAT signaling pathway in diabetic rats. Thus, sitagliptin could be considered as a potential candidate for the prevention/management of DCM.
Acknowledgments
This research project was supported by a grant from the Research Center of the Female Scientific and Medical Colleges, Deanship of Scientific Research, King Saud University, Saudi Arabia.
Disclosure
The authors report no conflicts of interest in this work.
References
- BautersCLamblinNMc FaddenEPVan BelleEMillaireAde GrootePInfluence of diabetes mellitus on heart failure risk and outcomeCardiovasc Diabetol20032112556246
- HuynhKMcMullenJRJuliusTLCardiac-specific IGF-1 receptor transgenic expression protects against cardiac fibrosis and diastolic dysfunction in a mouse model of diabetic cardiomyopathyDiabetes20105961512152020215428
- SolangLMalmbergKRydenLDiabetes mellitus and congestive heart failure. Further knowledge neededEur Heart J1999201178979510329075
- WestermannDWaltherTSavvatisKGene deletion of the kinin receptor B1 attenuates cardiac inflammation and fibrosis during the development of experimental diabetic cardiomyopathyDiabetes20095861373138119276445
- Falcao-PiresILeite-MoreiraAFDiabetic cardiomyopathy: understanding the molecular and cellular basis to progress in diagnosis and treatmentHeart Fail Rev201217332534421626163
- YuWWuJCaiFCurcumin alleviates diabetic cardiomyopathy in experimental diabetic ratsPLoS One2012712e5201323251674
- BrownleeMThe pathobiology of diabetic complications: a unifying mechanismDiabetes20055461615162515919781
- SchillingJDMannDLDiabetic cardiomyopathy: bench to bedsideHeart Fail Clin20128461963122999244
- AoyagiTMatsuiTThe cardiomyocyte as a source of cytokines in cardiac injuryJ Cell Sci Ther2012S5003
- KiuHNicholsonSEBiology and significance of the JAK/STAT signalling pathwaysGrowth Factors20123028810622339650
- SoebiyantoRPSreenathSNQuCKLoparoKABuntingKDComplex systems biology approach to understanding coordination of JAK-STAT signalingBiosystems200790383084217646048
- BoenglerKBuechertAHeinenYCardioprotection by ischemic postconditioning is lost in aged and STAT3-deficient miceCirc Res2008102113113517967780
- Hilfiker-KleinerDHilfikerADrexlerHMany good reasons to have STAT3 in the heartPharmacol Ther2005107113113715963355
- SnyderMHuangXYZhangJJIdentification of novel direct Stat3 target genes for control of growth and differentiationJ Biol Chem200828373791379818065416
- FischerPHilfiker-KleinerDSurvival pathways in hypertrophy and heart failure: the gp130-STAT3 axisBasic Res Cardiol2007102427929717530315
- MarreroMBSchiefferBPaxtonWGDirect stimulation of Jak/STAT pathway by the angiotensin II AT1 receptorNature199537565282472507746328
- DruckerDJDipeptidyl peptidase-4 inhibition and the treatment of type 2 diabetes: preclinical biology and mechanisms of actionDiabetes Care20073061335134317337495
- NikolaidisLAMankadSSokosGGEffects of glucagon-like peptide-1 in patients with acute myocardial infarction and left ventricular dysfunction after successful reperfusionCirculation2004109896296514981009
- SokosGGNikolaidisLAMankadSElahiDShannonRPGlucagon-like peptide-1 infusion improves left ventricular ejection fraction and functional status in patients with chronic heart failureJ Card Fail200612969469917174230
- PicatosteBRamirezECaro-VadilloASitagliptin reduces cardiac apoptosis, hypertrophy and fibrosis primarily by insulin-dependent mechanisms in experimental type-II diabetes. Potential roles of GLP-1 isoformsPLoS One2013810e7833024302978
- AllainCCPoonLSChanCSRichmondWFuPCEnzymatic determination of total serum cholesterolClin Chem19742044704754818200
- FossatiPPrencipeLSerum triglycerides determined colorimetrically with an enzyme that produces hydrogen peroxideClin Chem19822810207720806812986
- BursteinMScholnickHRMorfinRRapid method for the isolation of lipoproteins from human serum by precipitation with polyanionsJ Lipid Res19701165835954100998
- RossRThe pathogenesis of atherosclerosisBraunwaldEHeart Disease: A Textbook of Cardiovascular Medicine4th edPhiladelphia (PA)WB Saunders199211061124
- PreussHGJarrellSTScheckenbachRLiebermanSAndersonRAComparative effects of chromium, vanadium and gymnema sylvestre on sugar-induced blood pressure elevations in SHRJ Am Coll Nutr19981721161239550454
- BeutlerEDuronOKellyBMImproved method for the determination of blood glutathioneJ Lab Clin Med19636188288813967893
- MontgomeryHACDymockJFThe determination of nitrite in waterAnalyst196186414416
- MarklundSMarklundGInvolvement of the superoxide anion radical in the autoxidation of pyrogallol and a convenient assay for superoxide dismutaseEur J Biochem19744734694744215654
- CohenGDembiecDMarcusJMeasurement of catalase activity in tissue extractsAnal Biochem197034130385440916
- Al-RasheedNMAl-OteibiMMAl-ManeeRZSimvastatin prevents isoproterenol-induced cardiac hypertrophy through modulation of the JAK/STAT pathwayDrug Des Devel Ther2015932173229
- SarkhailPRahmanipourSFadyevatanSAntidiabetic effect of Phlomis anisodonta: effects on hepatic cells lipid peroxidation and antioxidant enzymes in experimental diabetesPharmacol Res200756326126617714953
- GuimaraesJFMuzioBPRosaCMRutin administration attenuates myocardial dysfunction in diabetic ratsCardiovasc Diabetol20151469026185015
- ConnellyKAZhangYAdvaniADPP-4 inhibition attenuates cardiac dysfunction and adverse remodeling following myocardial infarction in rats with experimental diabetesCardiovasc Ther201331525926722963483
- MeierJJUeberbergSKorbasSSchneiderSDiminished glucagon suppression after beta-cell reduction is due to impaired alpha-cell function rather than an expansion of alpha-cell massAm J Physiol Endocrinol Metab20113004E717E72321285404
- NishikawaTEdelsteinDDuXLNormalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damageNature2000404677978779010783895
- EvansJLGoldfineIDMadduxBAGrodskyGMAre oxidative stress-activated signaling pathways mediators of insulin resistance and beta-cell dysfunction?Diabetes20035211812502486
- WangGGLiWLuXHZhaoXXuLTaurine attenuates oxidative stress and alleviates cardiac failure in type I diabetic ratsCroat Med J201354217117923630144
- LeiteACAraujoTGCarvalhoBMSilvaNHLimaVLMaiaMBPar-kinsonia aculeata aqueous extract fraction: biochemical studies in alloxan-induced diabetic ratsJ Ethnopharmacol2007111354755217276638
- KeulPSattlerKLevkauBHDL and its sphingosine-1-phosphate content in cardioprotectionHeart Fail Rev2007123–430130617554629
- Howard-AlpeGMSearJWFoexPMethods of detecting atherosclerosis in non-cardiac surgical patients; the role of biochemical markersBr J Anaesth200697675876917074779
- AppleFSTissue specificity of cardiac troponin I, cardiac troponin T and creatine kinase-MBClin Chim Acta1999284215115910451242
- BoudinaSSenaSO’NeillBTTathireddyPYoungMEAbelEDReduced mitochondrial oxidative capacity and increased mitochondrial uncoupling impair myocardial energetics in obesityCirculation2005112172686269516246967
- SteinbergHOParadisiGHookGCrowderKCroninJBaronADFree fatty acid elevation impairs insulin-mediated vasodilation and nitric oxide productionDiabetes20004971231123810909983
- McKimSEGäbeleEIsayamaFInducible nitric oxide synthase is required in alcohol-induced liver injury: studies with knockout miceGastroenterology200312561834184414724835
- SilambarasanTRajaBDiosmin, a bioflavonoid reverses alterations in blood pressure, nitric oxide, lipid peroxides and antioxidant status in DOCA-salt induced hypertensive ratsEur J Pharmacol20126791–3818922266490
- AmaralLMPinheiroLCGuimaraesDAAntihypertensive effects of inducible nitric oxide synthase inhibition in experimental pre-eclampsiaJ Cell Mol Med201317101300130723890248
- MahmoudAMAl DeraHS18β-Glycyrrhetinic acid exerts protective effects against cyclophosphamide-induced hepatotoxicity: potential role of PPARgamma and Nrf2 upregulationGenes Nutr20151064126386843
- ArthurJRThe glutathione peroxidasesCell Mol Life Sci20005713–141825183511215509
- FerreiraLTeixeira-de-LemosEPintoFEffects of sitagliptin treatment on dysmetabolism, inflammation, and oxidative stress in an animal model of type 2 diabetes (ZDF rat)Mediators Inflamm2010201059276020652060
- KelleniMTAminEFAbdelrahmanAMEffect of metformin and sitagliptin on doxorubicin-induced cardiotoxicity in rats: impact of oxidative stress, inflammation, and apoptosisJ Toxicol2015201542481326880912
- AlamMAChowdhuryMRJainPSagorMARezaHMDPP-4 inhibitor sitagliptin prevents inflammation and oxidative stress of heart and kidney in two kidney and one clip (2K1C) ratsDiabetol Metab Syndr2015710726609328
- RajeshMMukhopadhyayPBatkaiSCannabidiol attenuates cardiac dysfunction, oxidative stress, fibrosis, and inflammatory and cell death signaling pathways in diabetic cardiomyopathyJ Am Coll Cardiol201056252115212521144973
- SuzukiHKayamaYSakamotoMArachidonate 12/15-lipoxygenase-induced inflammation and oxidative stress are involved in the development of diabetic cardiomyopathyDiabetes201564261863025187369
- SeddonMLooiYHShahAMOxidative stress and redox signalling in cardiac hypertrophy and heart failureHeart200793890390716670100
- MahmoudAMAshourMBAbdel-MoneimAAhmedOMHesperidin and naringin attenuate hyperglycemia-mediated oxidative stress and proinflammatory cytokine production in high fat fed/streptozotocin-induced type 2 diabetic ratsJ Diabetes Complications201226648349022809898
- DinhWFuthRNicklWElevated plasma levels of TNF-alpha and interleukin-6 in patients with diastolic dysfunction and glucose metabolism disordersCardiovasc Diabetol200985819909503
- DuerrschmidCCrawfordJRReinekeETNF receptor 1 signaling is critically involved in mediating angiotensin-II-induced cardiac fibrosisJ Mol Cell Cardiol201357596723337087
- WestermannDVan LinthoutSDhayatSTumor necrosis factor-alpha antagonism protects from myocardial inflammation and fibrosis in experimental diabetic cardiomyopathyBasic Res Cardiol2007102650050717909696
- ZhaoWZhaoTChenYAhokasRASunYOxidative stress mediates cardiac fibrosis by enhancing transforming growth factor-beta1 in hypertensive ratsMol Cell Biochem20083171–2435018581202
- WangLLiJLiDLosartan reduces myocardial interstitial fibrosis in diabetic cardiomyopathy rats by inhibiting JAK/STAT signaling pathwayInt J Clin Exp Pathol20158146647325755735
- SerranoALBaeza-RajaBPerdigueroEJardiMMunoz-CanovesPInterleukin-6 is an essential regulator of satellite cell-mediated skeletal muscle hypertrophyCell Metab200871334418177723
- MassagueJTGF-beta signal transductionAnnu Rev Biochem1998677537919759503