Abstract
Background
There are very limited published studies in Nigeria on the use of 24 hour Holter electrocardiogram (Holter ECG) in the arrhythmic evaluation of hypertensive and diabetic patients.
Objective
To evaluate indications, arrhythmic pattern of Holter ECG, and heart rate variability (HRV) among patients with hypertensive heart disease (HHD) with or without heart failure and type 2 diabetes mellitus (T2DM) seen in our cardiac care unit.
Methods
Seventy-nine patients (32 males and 47 females) were studied consecutively over a year using Schiller type (MT-101) Holter ECG machine.
Results
Out of the 79 patients, 17 (21.5%) had HHD without heart failure, 33 (41.8%) had HHD with hypertensive heart failure (HHF), while 29 (36.7%) were T2DM patients. The mean (standard deviation) ages of HHD without heart failure, HHF and T2DM patients were 59.65 (±14.38), 65.15 (±14.30), and 54.66 (±8.88) respectively. The commonest indication for Holter ECG was palpitation (38%), followed by syncope (20.3%). Premature ventricular contraction was the commonest arrhythmic pattern among the 79 patients, especially among HHF patients. The HRV using standard deviation of all normal-normal intervals was significantly reduced in T2DM patients (81.03±26.33, confidence interval [CI] =71.02–91.05) compared to the HHD without heart failure (119.65±29.86, CI =104.30–135.00) and HHF (107.03±62.50, CI =84.00–129.19). There was a negative correlation between the duration of T2DM and HRV (r=−0.613).
Conclusion
Palpitation was the commonest Holter ECG indication and premature ventricular contractions were the commonest arrhythmic pattern among our patients. HRV was reduced in T2DM patients compared with hypertensive patients.
Introduction
Hypertension and diabetes mellitus (DM) are common and a major public health problem in Nigeria.Citation1,Citation2 Twenty-four hour Holter electrocardiogram (Holter ECG) has been found useful in the detection of ischemic changes, cardiac arrhythmias, and heart rate variability (HRV) among hypertensive and diabetic patients.Citation3,Citation4 Type 2 diabetes mellitus (T2DM) and hypertensive left ventricular hypertrophy (LVH) are associated with increased risk of arrhythmias and mortality.Citation5,Citation6 Yet there are very limited published studies in Nigeria on the use of 24 hour Holter ECG in the arrhythmic evaluation of hypertensive and diabetic patients.Citation7–Citation9 In this study,Citation7 it was observed that LVH increased arrhythmias, and multivalvular regurgitations predispose to greater supra-ventricular tachycardia and complex ventricular arrhythmias, especially in hypertensive heart failure (HHF).
In another study, palpitation was the commonest 24 hour Holter indication and premature ventricular contraction (PVC) was the commonest arrhythmic pattern in hypertensive heart disease (HHD) and chest pain patients.Citation8 Adebola et alCitation9 also reported that the commonest indications for Holter monitoring in their patients were unexplained palpitation, dizzy spells, chest pain and syncope. Rare indications include unexplained dyspnea on exertion and pacemaker implantation. More than half of the study subjects (54%) had documented episodes of severe tachycardia (heart rate ≥120 bpm) while 18 patients had severe bradycardia (heart rate ≤40 beats per minute). Twenty-one patients were confirmed to have ventricular ectopics while three patients had non-sustained ventricular tachycardia.Citation9
We therefore evaluated the indications, arrhythmic pattern of Holter ECG, and HRV among patients with HHD without heart failure, HHF and T2DM seen in our cardiac care unit at Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC), Ile-Ife, Osun State, Nigeria. This will further help define the pattern of Holter ECG in hypertensive and diabetic subjects in our environment, and the data from this study will also add to the national and global database.
Materials and methods
This is a descriptive cross-sectional study in which consecutive diabetic and hypertensive patients referred to our cardiac care unit for 24 hour Holter ECG over a 12 month period were studied using Schiller type (MT-101) Holter ECG machine.
Inclusion criteria:
those who gave informed consent to participate in the study;
adult patients with HHD with or without heart failure;
adult patients with T2DM.
Exclusion criteria:
those who were unwilling to participate in the study;
hypertensive patients with myocardial infarction, renal failure, diabetic mellitus, or cerebrovascular diseases.
Glycated hemoglobin A1c was obtained in all T2DM patients. We separated the hypertensive patients into HHD without heart failure and HHD with heart failure. LVH and diastolic dysfunction are the early manifestations of cardiovascular target organ damage in patients with arterial hypertension and signify HHD, and can result in heart failure, arrhythmias, myocardial infarction, and sudden cardiac death.Citation10 HHD with HHF patients were recruited from patients with documented systemic hypertension or on anti-hypertensive medication who satisfy the criteria for diagnosis of heart failure based on Framingham’s criteriaCitation11 or the European Society of Cardiology criteria.Citation12 The clinical indications for Holter ECG were documented based on the recommendations of the American College of Cardiology (ACC)/American Heart Association (AHA) guidelines for ambulatory electrocardiography.Citation13 The Holter ECGs were read by an experienced cardiologist and two senior registrars in cardiology. Ethical approval was obtained from the Ethics and Research Committee of OAUTHC and all participants gave informed consent.
The HRV was analyzed in the time domain in accordance with ACC/AHA Guidelines.Citation13 The three parameters of the time domain HRV assessed were:
standard deviation of all normal-normal (NN) intervals (SDNN);
standard deviation of the averages of NN intervals in all 5 minute segments of the entire recording (SDANN); and
the square root of the mean of the sum of the squares of differences between adjacent NN intervals (RMS-SD).
The normal values of HRV used for the study were in accordance with the ACC/AHA Guidelines for Ambulatory ECG,Citation13 and are as follows: SDNN (141±39 milliseconds [ms]), SDANN (127±39 ms), and RMD-SD (37±15 ms).
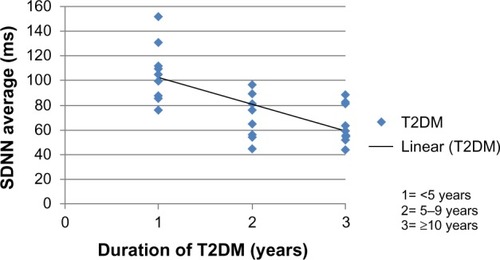
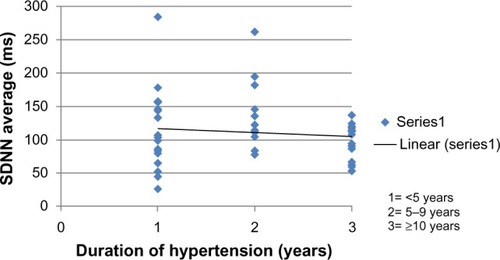
The data were analyzed using both descriptive and inferential statistics. The descriptive statistics include frequency distribution, scatter plot, mean, and standard deviation (SD). Inferential statistics that were used in the study were analysis of variance (ANOVA) and Pearson’s correlation. ANOVA was used to determine whether differences exist between HRV using SDNN average of HHD without heart failure, HHF and T2DM patients. Pearson’s correlation was used to examine the relationship between duration of T2DM or hypertension and HRV. The duration of T2DM or hypertension was grouped into less than 5 years, 5–10 years, and greater than 10 years. For the 29 T2DM patients, ten patients were grouped into less than 5 years; nine patients were grouped into 5–10 years, while ten patients were grouped into greater than 10 years. 16, 12 and 22 patients out of the 50 hypertensive patients were also grouped into less than 5 years, 5–10 years and greater than 10 years respectively.
Results
Demography and clinical indications
Demography and clinical characteristics of the studied patients were as shown in . Out of the 79 patients reviewed, 32 were males (40.5%), while 47 were females (59.5%). Seventeen (21.5%) patients had HHD without heart failure, 33 (41.8%) had HHF, while 29 (36.7%) were T2DM patients. The mean SD ages (years) of HHD without heart failure, HHF, and T2DM patients were 59.65 (±14.38), 65.15 (±14.30), and 54.66 (±8.88), respectively. The mean (SD) body mass index (BMI in kg/m2) of HHD without heart failure, HHF, and T2DM were 24.69 (±4.34), 25.18 (±4.71), and 30.63 (±11.6), respectively. The mean (SD) hemoglobin A1c (%) of T2DM patients are 7.33% (±1.18%). The mean (SD) of the duration of T2DM and hypertension (years) are 6.95±4.40 and 9.08±6.58, respectively.
Table 1 Clinical characteristics of the studied group
Clinical indications for Holter ECG are shown in and the commonest indication for Holter ECG among our study group was palpitation (38%). PVCs were the commonest type of arrhythmia accounting for 69.4% among patients with arrhythmia, followed by premature atrial contractions (8.2%) as shown in . PVCs were observed in 45.5% of HHF patients, 29.4% of HHD without heart failure and 13.7% of T2DM patients respectively. The mean total PVCs/24 hours was numerically more in HHF (5,936) as compared to HHD without failure (1,946) and T2DM (1,088). Eighteen point two percent of HHF patients had non-sustained ventricular tachycardia and one HHF patient had sustained ventricular tachycardia.
Table 2 Clinical indications
Table 3 Twenty-four hour Holter electrocardiogram rhythm distribution
Applying Lown’s grading of PVCCitation14 among patients with PVC, Lown’s grade 2 was commonest in the HHD without heart failure (35.3%) and T2DM (10.3%) patients, while Lown’s grade 4 was commonest among HHF patients (51.5%). Nine point one percent of HHF patients had fibrillation (AF). Seven patients had severe bradycardia (heart rate less than 40 beats per minute).
HRV
The mean (SD) average heart rate of HHD without heart failure, HHF, and T2DM patients were 68.47 (±10.35), 81.12 (±18.73), and 80.52 beats per minute (±12.68) respectively. The HRV using SDNN average (ms) was significantly reduced in T2DM patients (81.03±26.33, confidence interval [CI] =71.02–91.05) compared to the HHD without heart failure (119.65±29.86, CI =104.30–135.00) and HHF (107.03±62.50, CI =84.00–129.19) patients; (P<0.015). Similar findings were also noted when RMD-SD average (ms) was used to assess the HRV, with significant reduction in T2DM patients (36.48±21.10, CI =28.46–44.51) compared to HHD without heart failure (103.82±78.91, CI =63.25–144.39) and HHF (99.45±88.14, CI =60.51–94.05) patients. When SDANN average (ms) was used the HRV of HHD without heart failure, HHF and T2DM patients were variously reduced in the three studied groups, being 81.18 ms ±21.58 CI =70.08–92.27, 67.64 ms ±37.10 CI =54.48–80.79 and 65.79 ms ±18.92 CI =58.60–72.99, respectively, (P>0.078). Using SDNN, there was a statistically significant variation between day and night HRV in T2DM patients (P<0.001) and also in HHF patients (P<0.001), while the day and night HRV in HHD (without heart failure) patients was not statistically significant (P>0.051). There was a negative correlation between the duration of T2DM and HRV; (r=−0.613, P<0.001), as shown in . The duration of hypertension and HRV was also negatively correlated but was not statistically significant; (r=−0.51, P>0.731), as shown in .
Discussion
Arrhythmias, both atrial and ventricular are common co-morbidities in hypertension and DM.Citation3,Citation13 The underlying mechanisms of arrhythmogenicity in hypertension and DM include LVH, myocardial ischemia, impaired left ventricular function, and left atrial enlargement, among other factors.Citation6,Citation16
The age in the demography of our study group revealed that HHF patients were older than HHD (without heart failure) and T2DM. Obesity (grade 1) was prevalent in the T2DM patients in our study group.
The commonest indication for Holter ECG among our study group was palpitation (38%). Katibi et alCitation7 reported palpitation as the commonest indication (25%). PVC was the commonest arrhythmic pattern among our study group (69.4%). PVCs were more prevalent in HHF patients (45.5%). Katibi et alCitation7 also reported PVC as the commonest arrhythmic pattern (47.6%) in his study. The higher proportion in our study may be attributable to the fact that, our study group already has a cardiovascular disease risk factor or a cardiac disease. However, Schillaci et alCitation17 in Italy studied 126 never treated subjects with essential hypertension and reported PVCs in 71% of the subjects. The higher proportion in his study may be due to the fact that his study groups are – “never treated hypertensive patients”. Schillaci et alCitation17 also reported that complex ventricular arrhythmias (Lown’s class ≥2) were predicted by age greater than or equal to 60 years.
LVH and complex ventricular arrhythmias are significant predictors of sudden cardiac death.Citation16–Citation19 Cygankiewicz et alCitation20 reported that combining electrocardiographic stratification with assessment of myocardial substrate may provide insight into interplay between factors contributing to sudden cardiac death in heart failure. In our study, Lown’s grade 4 was found more prevalent in HHF patients compared with HHD (without heart failure) and T2DM patients. Advanced HHF irreversibly damages myocardial fibers which may serve as arrhythmogenic foci for various forms of arrhythmias.Citation21,Citation22 Ajayi et alCitation8 in a study of 24 hour Holter arrhythmic patterns of 37 HHF patients with or without valvular heart disease, reported that LVH increases arrhythmias but multivalvular regurgitation predisposes to greater supraventricular tachycardia and complex ventricular arrhythmias. Nine point one percent of HHF patients had AF. Familoni et alCitation23 in a clinical study of pattern and factors affecting outcome in Nigerian patients with advanced heart failure, reported that AF was associated with increased mortality rates among patients with advanced heart failure.
HRV is a temporal variation between sequences of consecutive heart beats.Citation24 The state of activity of the cardiac autonomic nervous system is evaluated by HRV. Diabetic autonomic neuropathy is a serious and common complication of DM and dysfunction of the autonomic nervous system is associated with increased risk of mortality in patients with diabetes.Citation25,Citation26 At the time of diagnosis, a reduced HRV is evident in T2DM patients which reflects the asymptomatic process over the years before diagnosis.Citation27,Citation28
T2DM is characterized by widespread degeneration of the small nerve fibers of sympathetic and parasympathetic branches of the autonomic nervous system, which may affect autonomic regulation of the sinus node, thereby reducing HRV.Citation29 The degree of autonomic dysfunction associated with DM is related to the severity and duration of the disease.Citation29 Diabetic patients with autonomic neuropathy also display impairment of the absolute values of the frequency domain analysis (both low-frequency component and high-frequency component). Studies in DM patients with or without chronic autonomic neuropathy indicate that both time- and frequency-domain measures of spontaneous baroreceptor-cardiac reflex sensitivity could allow early detection of chronic autonomic neuropathy in diabetic patients.Citation30,Citation31
HRV is also reduced in hypertensive patients when compared with normotensive individuals, indicating a decrease in baroreceptor reflex.Citation32 Using SDNN and RMD-SD, the HRV in T2DM patients was significantly reduced in our study. Boer-Martins et al in BrazilCitation33 reported decreased HRV in T2DM (mean age 54.7 years), and BMI (33.7±4 kg/m2) patients with resistant HTN, when compared with non-T2DM group. Nolan et alCitation34 in UK-HEART study of HRV and mortality in chronic heart failure patients (mean age 62±9.6 years), reported decreased HRV in chronic heart failure patients in some of the time domain parameters. In our study, the HRV of HHF patients using SDANN was also decreased. Our study showed a negative correlation between the duration of T2DM and HRV. Fujimoto et alCitation35 in Japan reported that all spectral variables of HRV were inversely related to the duration of DM in all diabetic patients. Khoharo et alCitation36 reported that chronic autonomic neuropathy as evidenced by decreased HRV was common in diabetic patients of greater than 5 years duration when compared with diabetic patients of less than 5 years.
The limitation of the study is the inability of the present Holter system software MT-101 to calculate the frequency domain parameters of HRV.
Conclusion
Palpitation was the commonest Holter ECG indication and PVCs were the commonest arrhythmic pattern among our patients. HRV was reduced in T2DM patients compared with hypertensive patients.
Disclosure
The authors have no conflicts of interest to disclose.
References
- Ogah OS Okpechi I Chukwunonye II Blood Pressure, Prevalence of Hypertension and Hypertension Related Complications in Nigerian Africans: A Review World J Cardiol 2012 4 12 327 340 23272273
- Akinkugbe OO Non-communicable Disease in Nigeria Final Report of National Survey Federal Ministry of Health and Social Services Lagos 1997 64 90
- Takase B Kurita A Noritake M Heart Rate Variability in Patients with Diabetes Mellitus, Ischemic Heart Disease and Congestive Heart Failure J Electrocardiol 1992 25 2 79 88 1522401
- Gasilin VS Stetsenko AE Kruglov VA Boikova OI Chernysheva GV Possibilities of Holter ECG Monitoring in Detecting Arrhythmias and Myocardial Ischemia in Persons with Ischemic Heart Disease Risk Factors Kardiologiia 1989 29 3 10 13 Russian 2733324
- Movahed MR Hashemzadeh M Jamal M Increased Prevalence of Ventricular Fibrillation in Patients with Type 2 Diabetes Mellitus Heart Vessels 2007 22 4 251 253 17653519
- Galinier M Balanescus S Fourcade J Prognostic Value of Ventricular Arrhythmia in Hypertensive Patients Arch Mal Coeur Vaiss 1997 90 8 1049 1053 French 9404407
- Katibi IA Beshir S Mudashiru Z Ambulatory 24-hour Holter Electrocardiography among Nigerians: Our Experience at a Referral Cardiac Centre in Lagos, Nigeria Nigerian Medical Journal 2006 47 2 25 27
- Ajayi OE Ajayi AA Valvular Regurgitations may Increase the Risk of Arrhythmias in Hypertensive Heart Failure in Nigerians J Cardiovasc Med (Hagerstown) 2013 14 6 453 460 23114272
- Adebola AP Daniel FA Lasisi GT Ogunleye O 24-Hour Holter Monitoring at the Lagos State University Teaching Hospital-a report of 85 cases Nigerian Journal of Clinical Medicine 2009 2 2
- Diamond JA Phillips RA Hypertensive Heart Disease Hypertens Res 2005 28 3 191 202 16097361
- McKee PA Castelli WP McNamara Kannel WB The natural history of congestive heart failure: the Framingham study N Engl J Med 1971 285 26 1441 1446 5122894
- McMurray JJ Adamopoulos S Anker SD ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC Eur Heart J 2012 33 14 1787 1847 22611136
- Crawford MH Bernstein SJ Deedwania PC ACC/AHA Guidelines for Ambulatory Electrocardiography. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the Guidelines for Ambulatory Electrocardiography). Developed in collaboration with the North American Society for Pacing and Electrophysiology J Am Coll Cardiol 1999 34 3 912 948 10483977
- Lown B Wolf M Approaches to Sudden Death from Coronary Heart Disease Circulation 1971 44 1 130 142 4104697
- Anastos K Charney P Charon RA Hypertension in Women: What is Really Known? The Women Caucus, Working Group on Women’s Health of the Society of General Internal Medicine Ann Intern Med 1991 115 4 287 293 1854113
- Powers AC Diabetes Mellitus Kasper DL Fausi AS Braunwald E Harrison’s Principles of Internal Medicine 16th ed New York McGraw-Hill 2005 2 2166 2167
- Schillaci G Verdechia P Borgioni C Association Between Persistent Pressure Overload and Ventricular Arrhythmias in Essential Hypertension Hypertension 1996 28 2 284 289 8707395
- Saadeh AM Jones JV Predictors of Sudden Cardiac Death in Never Previously Treated Patients with Essential Hypertension: Long Term Follow-up J Hum Hypertens 2001 15 10 677 680 11607796
- Dzudie A Milo O Edwards C Prognostic Significance of Electrocardiographic Abnormalities for Mortality Risk in Acute Heart Failure: Insight from sub-Saharan Africa Survey for Heart Failure (THESUS-HF) J Card Fail 2014 20 1 45 52 24269854
- Cygankiewicz I Zareba W de Luna AB Prognostic Value of Holter Monitoring in Congestive Heart Failure Cardiol J 2008 15 4 313 323 18698539
- Pohwidz SM Corr PB Biochemical and Electrophysiological Alterations Underlying Ventricular Arrhythmias in the Failing Heart Eur Heart J 1994 15 Suppl D 145 154 7713105
- Araoye MA Olowoyeye JO The Clinical Spectrum of Hypertensive Heart Failure: A Point-score System for Solving an Old Problem East Afr Med J 1984 61 4 306 315 6489234
- Familoni OB Olunuga TO Olufemi BW A Clinical Study of Pattern and Factors Affecting Outcome in Nigerian Patients with Advanced Heart Failure Cardiovasc J Afr 2007 18 5 308 311 17957325
- Karim N Hassan JA Ali SS Heart Rate Variability-A Review Journal of Basic and Applied Sciences 2011 7 1 71 77
- Vinik AI Maser RE Mitchell BD Freeman R Diabetic Autonomic Neuropathy Diabetes Care 2003 26 5 1553 1579 12716821
- Gerritsen J Dekker JM TenVoorde BJ Impaired Autonomic Function is Associated with Increased Mortality Especially in Subjects with Diabetes, Hypertension, or a History of Cardiovascular Disease Diabetes Care 2001 24 10 1793 1798 11574444
- Schonauer M Thomas A Morbach S Niebauer J Schonauer U Thiele H Cardiac Autonomic Diabetic Neuropathy Diab Vasc Dis Res 2008 5 4 336 344 18958844
- Pfeifer MA Weinberg CR Cook DL Autonomic Neural Dysfunction in Recently Diagnosed Diabetic Subjects Diabetic Care 1984 7 5 447 453
- Ahamed Seyd PT Thajudin Ahamed VI Jacob J Joseph PK Time and frequency domain analysis of HRV and their correlations in DM World Academy of Science, Engineering and Technology 2008 2 3 26
- Frattola A Parati G Gamba P Time and frequency domain estimates of spontaneous baroreflex sensitivity provide early detection of autonomic dysfunction in DM Diabetologia 1997 40 12 1470 1475 9447956
- Weston PJ Panerai RB McCullough A Assessment of baroreceptor-cardiac reflex sensitivity using time domain analysis in patients with IDDM and the relation of left ventricular mass index Diabetologia 1996 39 11 1385 1391 8933009
- Menezes Aa SJr Moreira HG Daher MT Analysis of Heart Rate Variability in Hypertensive Patients Before and After Treatment with Angiotensin II Converting Enzyme Inhibitors Arg Bras Cardiol 2004 83 2 169 172
- Boer-Martins L Figueiredo VN Demacq C Relationship of Autonomic Imbalance and Circadian Disruption with Obesity and Type 2 Diabetes in Resistant Hypertension Patients Cardiovasc Diabetol 2011 10 24 21426540
- Nolan J Batin PD Andrews R Prospective Study of Heart Rate Variability and Mortality in Chronic Heart Failure Circulation 1998 98 15 1510 1516 9769304
- Fujimoto Y Fukuki M Hoshio A Decreased Heart Rate Variability in Patients with Diabetes Mellitus and Ischemic Heart Disease Jpn Circ J 1996 60 12 925 932 8996682
- Khoharo HK Halepoto AW QTc- interval, Heart Rate Variability and Postural Hypotension as an Indicator of Cardiac Autonomic Neuropathy in Type II Diabetes Mellitus J Pak Med Assoc 2012 62 4 328 331 22755273