Abstract
Purpose
Anticancer drug delivery systems are often limited by hurdles, such as off-target distribution, slow cellular internalization, limited lysosomal escape, and drug resistance. To overcome these limitations, we have developed a stable nitric oxide (NO)-releasing nanoparticle (polystyrene-maleic acid [SMA]-tert-dodecane S-nitrosothiol [tDodSNO]) with the aim of enhancing the anticancer properties of doxorubicin (Dox) and a Dox-loaded nanoparticle (SMA-Dox) carrier.
Materials and methods
Effects of SMA-tDodSNO and/or in combination with Dox or SMA-Dox on cell viability, apoptosis, mitochondrial membrane potential, lysosomal membrane permeability, tumor tissue, and tumor growth were studied using in vitro and in vivo model of triple-negative breast cancer (TNBC). In addition, the concentrations of SMA-Dox and Dox in combination with SMA-tDodSNO were measured in cells and tumor tissues.
Results
Combination of SMA-tDodSNO and Dox synergistically decreased cell viability and induced apoptosis in 4T1 (TNBC cells). Incubation of 4T1 cells with SMA-tDodSNO (40 µM) significantly enhanced the cellular uptake of SMA-Dox and increased Dox concentration in the cells resulting in a twofold increase (P<0.001). Lysosomal membrane integrity, evaluated by acridine orange (AO) staining, was impaired by 40 µM SMA-tDodSNO (P<0.05 vs control) and when combined with SMA-Dox, this effect was significantly potentiated (P<0.001 vs SMA-Dox). Subcutaneous administration of SMA-tDodSNO (1 mg/kg) to xenografted mice bearing 4T1 cells showed that SMA-tDodSNO alone caused a twofold decrease in the tumor size compared to the control group. SMA-tDodSNO in combination with SMA-Dox resulted in a statistically significant 4.7-fold reduction in the tumor volume (P<0.001 vs control), without causing significant toxicity as monitored through body weight loss.
Conclusion
Taken together, these results suggest that SMA-tDodSNO can be used as a successful strategy to increase the efficacy of Dox and SMA-Dox in a model of TNBC.
Introduction
Targeted antitumor therapies supported by nanotechnology have emerged as attractive strategies to overcome the lack of selectivity of traditional chemotherapeutic drugs. Described as “a royal gate for targeted anticancer nanomedicines”,Citation1 the enhanced permeability and retention (EPR) effect of macromolecules is the main cause of passive targeting of various long-lasting pharmaceutical nanocarriers larger than 7 nm in solid tumors.Citation2 The EPR effect in tumors arises from the insufficient formation of tight junctions in the endothelium, leaky vasculature, slow venous return, and poor lymphatic clearance.Citation3 Animal studies have shown that nanocarriers can achieve three to ten times higher concentration of drugs at the tumor site with a concomitant reduction of off-target side effects.Citation2 However, in clinical settings, the EPR effect does not always guarantee an efficient targeting of tumor tissues due to the heterogeneity of tumor cells, microenvironment, and several barriers preventing them reaching their targets in cancer cells.Citation4,Citation5 In fact, nanoparticles (NPs) to reach the target should overcome the extracellular matrix (ECM), which is a semisolid barrier consisting of an interconnected network of collagen fibers intermingled with proteins. The higher rigidity of the ECM in most tumors compared to normal tissues hinders NP diffusion.Citation6 In addition, NPs cannot simply enter cells via diffusion; they are internalized through endocytic process, which is time and energy consuming, and this endocytic process can prevent the absorption of NPs carrying drugs acting inside the cells.Citation7 Finally, the payload efflux from the cells and multidrug resistance are major hurdles in the treatment of many cancers.Citation8 Besides the restricted uptake, the confinement of NPs in low-pH endosomal or lysosomal compartments and the reduced blood supply, leading to the presence of hypoxic areas in the central region of the tumor and in metastasis, can also negatively impact the efficacy of the treatments.Citation9 Strategies to enhance the EPR effect, aiming at increasing NPs’ selective tumor targeting, include the modulation of the tumor microenvironment. Local administration of nitric oxide (NO) donors to tumors with the aim of increasing the blood flow has been tested clinically with favorable outcome.Citation10 However, limited NO payloads, short NO half-life, and the lack of organ or tissue specificity have restricted the utilization of NO in the area of anticancer management, despite their potential antitumoral effects.Citation11
The aim of this paper is to investigate the effects of a stable NO-releasing compound loaded into styrene maleic acid nanomicelles on the anticancer properties of doxorubicin (Dox) in 4T1, a triple-negative breast cancer (TNBC) model. To this extent, we identified the NO-releasing tert-dodecane S-nitrosothiol (tDodSNO) as a stable NO-donor and encapsulated it into polystyrene-maleic acid (SMA) to formulate SMA-tDodSNO NPs. tDodSNO showed superior stability and NO release profile compared to commercially available NO donors (such as S-nitroso-N-acetylpenicillamine, S-nitrosoglutathione, and sodium nitroprusside) most probably due to its bulkiness and hydrophobicity.Citation12,Citation13 However, its hydrophobicity may limit therapeutic applications. Encapsulation of tDodSNO into SMA makes it water soluble and physically protects it from premature tDodSNO breakdown as well as trans-nitrosation reactions with proteins and thiols, thereby inhibiting unspecific NO release. In addition, as NO plays an important role in vascular tone and permeabilityCitation3 and controls the cellular trafficking process of endocytosis and exocytosis,Citation14 on this basis we hypothesized that SMA-tDodSNO can increase the efficacy of Dox in vitro and a Dox-loaded NP (SMA-Dox) formulation in vivo. Finally, therapeutic advantages of the new combination were tested in 4T1 syngeneic animal model of TNBC.
Materials and methods
Dox was purchased from Lancrix Chemicals Ltd. (Shanghai, China). Polystyrene-co-maleic anhydride terminated with cumene (SMA) as a polymeric mixture with an average molecular weight of 1,600 Da and all other chemicals were obtained from Sigma-Aldrich Co. (St Louis, MO, USA). MTT and all cell culture reagents were purchased from Thermo Fisher Scientific (Waltham, MA, USA). tDodSNO was synthesized as described before.Citation12
Synthesis of SMA-tDodSNO and SMA-Dox
SMA-tDodSNO and SMA-Dox were prepared according to the previously reported method.Citation15 Briefly, to create optimized loading of tDodSNO, or Dox in SMA NPs, escalating milligram ratios of the compounds dissolved in 2 mL DMSO were added dropwise to 10 mL of a vigorously stirring solution of SMA (10 mg/mL) at pH =5.0, followed by addition of 80 mg EDAC, and solubilized in 2 mL of deionized water. During the addition of EDAC, the pH of the solution was maintained at 5 for 10 minutes, and then it was increased by NaOH 1 M to reach pH 11. Upon the appearance of a clear solution, the pH was adjusted back to 7.4 and purified using ultrafiltration system Pellicon XL filter 10 kDa (Merck Millipore, Billerica, MA, USA). The final concentrated product was freeze-dried to get the SMA-tDodSNO and SMA-Dox powder. To measure the loading of tDodSNO or Dox in the NPs, known weights of the NPs were dissolved in methanol, and the concentrations of SMA-tDodSNO and SMA-Dox were calculated using HPLC and UV-Vis spectroscopy at 480 nm, respectively.
NPs size and zeta potential
NP size, dispersity, and zeta potential were quantified by dynamic and electrophoretic light scattering of 8 mg/mL solutions of the NPs at room temperature using a Malvern Zeta Sizer ZEN3600 (Malvern Instruments, Malvern, UK), and repeated in triplicate.
Drug release from SMA-tDodSNO and SMA-Dox
The release of the payloads from the NPs was measured using a semipermeable dialysis membrane (14 kDa molecular weight cutoff, Sigma-Aldrich Co.) as detailed before.Citation15 The concentration of tDodSNO in the solutions was measured using a BM-20Alite Prominence HPLC system (Shimadzu Corporation, Kyoto, Japan) on a reversed-phase Gemini 3 µm C18, 110A, 150×2 mm column (Phenomenex Gemini-NX, North Shore City, Auckland, New Zealand) at 25°C. The mobile phase was methanol containing 0.3% trifluoroacetic acid, and the flow rate was 0.65 mL/min. A diode array detector was set at 341 nm and linked to Chromeleon software for data analysis. tDodSNO peak was detected at 341 nm with the retention time of 4.3 minutes.
In vitro studies
Mouse 4T1 mammary carcinoma cells were used for in vitro studies. This cell line is one of the most aggressive phenotypes of cancer cells exhibiting aggressive phenotype similar to human TNBC.Citation16 Mouse 4T1 cells were purchased from ATCC, were cultured in RPMI-1640 medium supplemented with 5% heat-inactivated FBS, 100 U/mL penicillin, and 100 µg/mL streptomycin (Thermo Fisher Scientific) and maintained in a humidified atmosphere with 5% CO2 and 95% air at 37°C.
Cell viability assay and synergistic toxicity of SMA-tDodSNO and Dox
4T1 cells were seeded at 5,000 cells/well into 96-well plates and allowed to adhere overnight. Cells were then treated with various concentrations of SMA-tDodSNO (1–100 µM) and/or Dox (0.001–5 µM) and incubated for 48 hours. The medium was removed and 0.4 mg/mL MTT dissolved in media was added for 3 hours. After removing medium, the residual crystals were dissolved in 100 µL DMSO and cell viability was calculated at λ′ =550 nm.
Cell cycle analysis
Two lakh 4T1 cells/well were seeded in six-well plates and allowed to adhere overnight prior to treatment with different concentrations of Dox (0.1 µM) and SMA-tDodSNO (10 and 40 µM). Forty-eight hours post treatment, cells were harvested, washed in cold PBS, followed by fixation with 4°C chilled 70% ethanol for 30 minutes. The fixed cells were washed twice with phosphate-citrate buffer (Na2HPO4 192 mM, citric acid 4 mM), treated with 50 µL of 100 µg/mL RNase A, and finally stained with 200 µL of 50 µg/mL propidium iodide (PI) at 4°C. DNA content and percentage of cells in the different phases of the cell cycle were determined using FACScan flow cytometer (Becton Dickinson) and FlowJo software (TREE STAR, Inc., San Carlos, CA, USA). For all flow cytometry analysis, a minimum of 10,000 cells/sample were acquired and gated to remove cell debris and doublets as shown in . The main population of cells was separated from possible noises (side scatter area vs forward scatter area [FSC-A]), then single cells were selected using forward scatter height vs FSC-A plot ().
Apoptosis assay
Double fluorescence staining with Annexin V-FITC/PI was used to determine the percentage of cells actively undergoing apoptosis.Citation17 The cells were seeded and treated for 48 hours, as mentioned above. Cells were harvested, centrifuged at 2,000 rpm for 3 minutes (at 4°C), washed in cold PBS, and resuspended in 100 µL per tube of Annexin V binding buffer (HEPES: 0.1 M, NaCl 1.4 M, CaCl2 25 mM, pH 7.4). Two microliters per tube of Annexin V conjugated Alexa Fluor 488 (Alexa 488) was added to the cell solution and incubated at room temperature for 15 minutes, protected from light. Four hundred microliters of the binding buffer and 5 µL per tube of 50 µg/mL PI were then added to the solution and kept on ice. The resulting samples were analyzed by FACScan. Annexin V-positive, PI-negative cells (Annexin V+/PI−), found in the lower right quadrant of the FACS dot plot, indicated early apoptotic population; Annexin V+/PI+ cells, found in the upper right quadrant of the histogram, represented either late apoptotic or secondary necrotic populations.Citation18
Analysis of mitochondrial membrane potential
Changes in mitochondrial membrane potential were evaluated using the mitochondrial marker tetramethyl-rhodamine ethyl ester (TMRE).Citation19,Citation20 Following SMA-tDodSNO (10 and 40 µM) and/or Dox (0.1 µM) treatments, cells were harvested by trypsinization, centrifuged at 2,000 rpm for 3 minutes, and resuspended in 500 µL of media. Then, 2 µL of 10 µM TMRE was added to the suspensions of cells and incubated for 20 minutes at 37°C, protected from light, washed with PBS, and resuspended in media. The resulting samples were analyzed by FACScan cytometer.
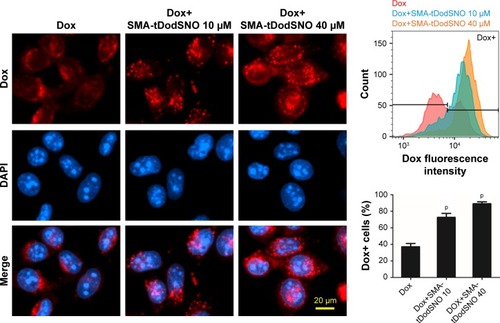
Effect of SMA-tDodSNO on the cellular uptake of SMA-Dox and Dox
To elucidate whether SMA-tDodSNO affects the cellular uptake of SMA-Dox, 4T1 cells in six-well plates (200,000 cells/well) were treated with SMA-tDodSNO (10 or 40 µM) and/or SMA-Dox (1 µM) in medium and incubated for 4 hours. The cells were then washed three times with pre-warmed fresh media and the fluorescent intensity of Dox in the cells was quantified by the Nikon Inverted Ti-E microscope (Coherent Instruments, Adelaide, Australia) and by flow cytometry. To evaluate the effect of SMA-tDodSNO on the Dox intracellular concentration, 4T1 cells were treated with SMA-tDodSNO (10 and 40 µM) and Dox (0.1 µM) and incubated for 48 hours, then the cellular concentration of Dox was quantified.
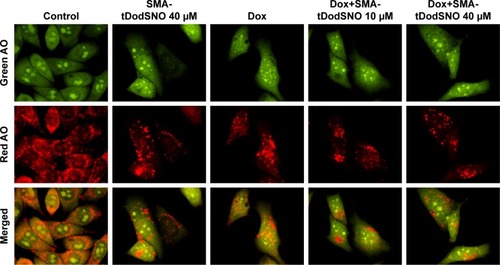
Determination of lysosomal membrane permeability
To evaluate whether the lysosomal membrane permeability was affected by SMA-tDodSNO treatment, acridine orange (AO) staining was used. 4T1 cells plated in six-well plates (200,000 cells/well) were treated in the medium for 4 hours with SMA-tDodSNO (10 and 40 µM) and/or SMA-Dox (1 µM), stained with 2 µL of solution (dissolved in double distilled water [ddW] at a concentration of 1 mg/mL) for 15 minutes at 37°C and imaged by fluorescent microscopy. For flow cytometry analysis, after incubation with AO, the cells were removed from the plate with trypsin, collected in RPMI, then resuspended in the medium and analyzed by the FACScan.
In vivo studies
All procedures involving the use of animals were conducted according to animal care policy of the Arabian Gulf University (AGU) and approved by the Research and Ethics Committee, AGU. To this end, BLAB/c female mice, 6 weeks old, weighing 22.4±2.6 g, were housed in the laboratory animal care facility of the AGU, under a standardized condition of 12 hours light and dark cycle. 4T1 cells (2×106 cell) were implanted subcutaneously in the dorsal skin (right and left sides) of 6-week-old male BALB/c mice. When tumors reached 100 mm3 in size, mice were injected with their respective test drugs. The in vivo study includes two sets of experiments. A) Evaluation of the influence of local administration of SMA-tDodSNO on SMA-Dox accumulation in tumor. To this extent, the xenografted mice were treated with either SMA-Dox or SMA-Dox+SMA-tDodSNO (four mice/group). In this experiment, SMA-Dox was injected intravenously via the tail at the dose of 5 mg/kg, and 1 mg/kg SMA-tDodSNO was injected intratumorally. Twenty four hours later, the mice were euthanized and tumors were excised and preserved in liquid nitrogen. B) Evaluation of the antitumor properties of SMA-tDodSNO alone and in combination with SMA-Dox. To this extent, the mice (5/group) were randomly distributed into four groups: 1) SMA-Dox, 2) SMA-tDodSNO, 3) SMA-Dox+SMA-tDodSNO, and 4) control group. The day of initial administration was set as day 0. At day 0 and day 8 of the study, 5 mg/kg SMA-Dox intravenous and/or SMA-tDodSNO 1 mg/kg intratumorally were injected. The tumor volume was measured by manual caliber; the volume was estimated by using the formula V (mm3) = ((transverse section)Citation2 × (longitudinal cross-section)/2). Tumor volumes were normalized by using the initial tumor volume. The body weight of mice was measured and normalized daily for 14 days as an index of acute toxicity. Tumor tissues were thawed and cut into small pieces. For each 1 g of the tissue, 10 mL of 33% HCl in ethanol was added and the suspension was heated to 70°C in an oven for 30 minutes. The mixture was homogenized followed by sonication (for five intervals), vortex, and centrifugation (for three times). Finally, the supernatant was isolated from the pellet, and using a UV-VIS spectrometer, the absorbance of Dox was measured at 480 nm.
Statistical analysis and quantification of synergism
The results were presented as the mean and SD of the mean. Half-maximal inhibitory concentrations (IC50s) for cytotoxicity were interpolated from semilogarithmic plots of concentration–response curves using OriginPro 8 software. To quantify the interaction of the combinations (synergism and antagonism), the methodology of Chou and Talay was applied using CompuSyn 1.01 software (ComboSyn, Inc., Paramus, NJ, USA).Citation21 The results were expressed as a combination index (CI), where CI <1, CI =1, and CI >1 were considered to indicate synergistic, additive, and antagonistic effects, respectively.Citation21 Statistical analysis was performed by GraphPad Prism, and all comparisons were carried out by a one-way ANOVA followed by the Bonferroni post hoc or independent sample t-test. The differences were considered significant if P-value <0.05.
Results
Synthesis and characterization of SMA-tDodSNO and SMA-Dox
A summary of the characteristics of synthesized NPs, SMA-tDodSNO, and SMA-Dox, is reported in . The loading of the correspondent active principle in SMA-tDodSNO and SMA-Dox were 21.1±1.4 and 13.1%±2.6% (w/w), respectively. SMA-tDodSNO and SMA-Dox had a mean diameter of 227±37 and 34.3±8.2 nm, respectively. Measured polydispersity index for SMA-tDodSNO and SMA-Dox was 0.211±0.024 and 0.26±0.15, respectively. The surface charge of both micellar systems in ddW was essentially neutral, with a mean zeta potential of −0.001±0.032 mV for tDodSNO and +0.15±0.14 mV for SMA-Dox (). In PBS (pH =7.4), the NPs were stable and limited release rate was detected within 6 hours (SMA-tDodSNO: 8.46%±4.12% and SMA-Dox: 3.22%±1.96%).
Table 1 Physicochemical characteristics of NPs, SMA-tDodSNO, and SMA-DoxTable Footnotea
Effect of the SMA-tDodSNO and Dox treatments on cell viability
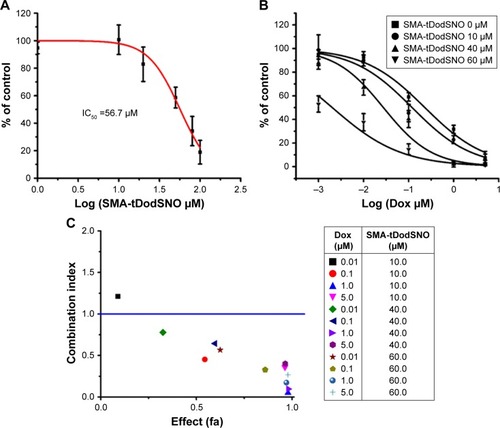
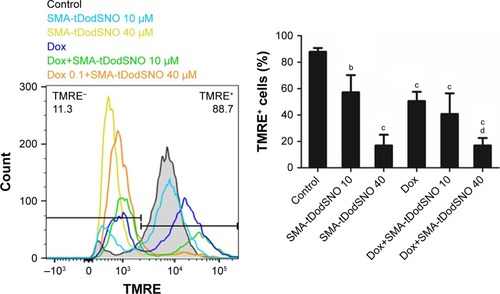
Incubation of 4T1 cells with SMA-tDodSNO for 48 hours over a range of different concentrations showed a concentration-dependent decrease in cell survival, with an IC50 calculated from the concentration–response curve of 56.7±4.9 µM (). The combination of SMA-tDodSNO and Dox potentiated the cytotoxicity of Dox with a consequent IC50 shift from 205±34 to 1.79±0.7 nM (P<0.001) when 60 µM of SMA-tDodSNO was added to the cells (). Chou-Talalay analysis of the treatments showed a CI <1, indicating a synergistic interaction between SMA-tDodSNO and Dox on 4T1 cell survival (). Apart from the lowest concentrations (Dox 0.01 µM and SMA-tDodSNO 10 µM), all other doses combination showed a synergistic effect.
Figure 1 The effect of SMA-tDodSNO and/or Dox on the 4T1 cell proliferation.
Notes: (A) SMA-tDodSNO showed cytotoxicity with an IC50 value of 56 µM. (B) Addition of SMA-tDodSNO to Dox potentiated cell toxicity of Dox and the IC50 shifted from 205±34 to 1.79±0.51 nM (P<0.001). (C) CI vs the cytotoxic effect of the treatments. The cytotoxicity of the cells treated with Dox (0.01, 0.1, 1, and 5 µM) and/or SMA-tDodSNO (10, 40, and 60 µM) was used for analysis of CI effect using Chou-Talay methodology. Apart from combination at the lowest concentrations (Dox 0.01 µM and SMA-tDodSNO 10 µM), all other doses showed a synergistic activity.
Abbreviations: CI, combination index; Dox, doxorubicin; SMA, polystyrene-maleic acid; tDodSNO, tert-dodecane S-nitrosothiol.
Effect of the SMA-tDodSNO and Dox treatments on cell cycle
To evaluate the mechanisms by which the different treatments inhibited 4T1 cell proliferation, cell cycle distribution was analyzed by flow cytometry. The identification and gating of single cells by standard biparametric dot plot are given in . Both Dox and 40 µM SMA-tDodSNO significantly increased the population of cells in the subG1 phase (P<0.05 and P<0.001, respectively) compared with untreated cells (). When a combination of SMA-tDodSNO and Dox was used, the cells population in subG1 phase was 2.8-fold more than only Dox-treated cells (P<0.001) and was significantly more than SMA-tDodSNO-treated cells (P<0.05).
Figure 2 Flow cytometric analysis of cell cycle parameters. 4T1 cells were incubated with Dox (0.1 µM) and/or SMA-tDodSNO (10 or 40 µM) for 48 h.
Notes: The treatments caused significant increase of the cell population in subG1 phase. Data are expressed as mean values ± SD (n=3). aP<0.05, bP<0.05, cP<0.001 vs control. dP<0.05, pP<0.001 vs Dox, and eP<0.05, fP<0.01, gP<0.001 vs respective SMA-tDodSNO group.
Abbreviations: Dox, doxorubicin; SMA, polystyrene-maleic acid; tDodSNO, tert-dodecane S-nitrosothiol.
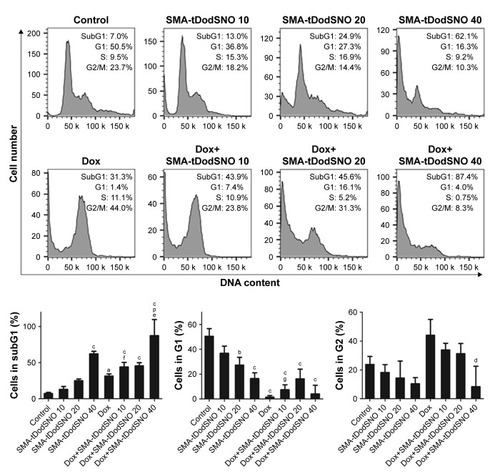
Effect of the SMA-tDodSNO and Dox treatments on apoptosis
The Annexin V and PI double labeling assay was used to determineCitation18 the extent of apoptosis following the treatments and the results are summarized in . SMA-tDodSNO at concentrations of 10 and 40 µM decreased the percentage of viable cells (Annexin V−/PI−) to approximately 48.8%±8.7% and 33.9%±3.8% (P<0.001 vs control). Upon SMA-tDodSNO treatments, cells shifted to preapoptotic (33%±8.4% and 47.1%±3.7%; 9- and 13-fold greater than that of control, respectively, P<0.001) and necrotic states (15.9%±1.6% and 14.6%±1.4%, respectively; ). Similarly, Dox (0.1 µM) caused a significant reduction of viable cells to 38%±8.7% (P<0.05) and enhancement in the population of apoptotic (8.5-fold, P<0.001 vs control) and necrotic (3.3-fold, P<0.01 vs control). When the cells were treated concurrently with Dox and SMA-tDodSNO (40 µM), the percentage of the alive cells dropped to 21.7%±3.9%, which was significantly less than control (P<0.001) and either treatment alone (P<0.05). In addition, the population of apoptotic cells was significantly greater compared to Dox-treated cells (P<0.05; ).
Figure 3 Flow cytometric analysis of apoptosis in 4T1 cells following incubation with Dox (0.1 µM) and/or SMA-tDodSNO (10 or 40 µM) for 48 hours and Annexin V/PI double staining.
Notes: The percentage of viable cells significantly decreased (P<0.001) and apoptotic cell population (Annexin V+/PI−) significantly enhanced by Dox-SMA-tDodSNO 40 µM (P<0.05). Data are expressed as mean values ± SD (n=3). aP<0.05, cP<0.001 vs control. dP<0.05 vs Dox and eP<0.05 vs respective SMA-tDodSNO group.
Abbreviations: Dox, doxorubicin; PI, propidium iodide; SMA, polystyrene-maleic acid; tDodSNO, tert-dodecane S-nitrosothiol.
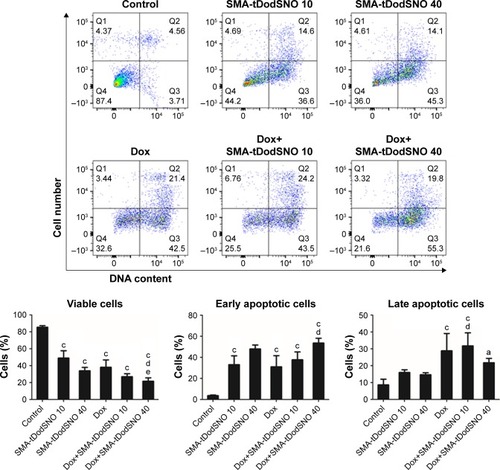
Role of mitochondria in the cytotoxicity of SMA-tDodSNO and Dox treatments
Mitochondrial dysfunction has been reported as an early indicator of Dox and NO-induced apoptosis,Citation22,Citation23 hence the effect of SMA-tDodSNO and Dox was evaluated on mitochondrial membrane potential. The TMRE histograms () show that both SMA-tDodSNO and Dox significantly shifted the fluorescence peak to the left. The percentage of TMRE+ cells in the SMA-tDodSNO (40 µM)- and Dox (0.1 µM)-treated samples were 16.9±9.5 and 35.8±3.2, respectively, which were significantly different from the control 86.5±5.6 (P<0.05) indicating a loss in mitochondrial membrane potential.Citation24 Combination treatment shifted the peak further to the left, and the population of TMRE+ cells was four times less than Dox-treated cells. However, the decrease in the fluorescent unit was not statistically significant compared to SMA-tDodSNO (40 µM)-treated cells.
Figure 4 Mitochondrial membrane depolarization was measured using TMRE staining of 4T1 cells treated with Dox (0.1 µM) and/or SMA-tDodSNO (10 and 40 µM) for 48 hours.
Notes: Data are expressed as mean values ± SD (n=3). bP<0.01, cP<0.001 vs control, dP<0.05 vs Dox.
Abbreviations: Dox, doxorubicin; SMA, polystyrene-maleic acid; tDoDSNO, tert-dodecane S-nitrosothiol; TMRE, tetramethyl-rhodamine ethyl ester.
Effect of SMA-tDodSNO on the endocytosis of SMA-Dox
Due to the size of SMA-Dox (mean diameter =34 nm), it cannot be internalized through diffusion, and their inter-nalization depends on endocytosis.Citation25 To investigate the facilitating role of SMA-tDodSNO in SMA-Dox uptake, we measured the fluorescent imaging of the cells. 4T1 cells were treated with either SMA-Dox or SMA-Dox+SMA-tDodSNO for 4 hours and, as reported in , SMA-tDodSNO enhances the cellular uptake of SMA-Dox. Quantification of the fluorescent intensity showed that the addition of 40 µM of SMA-tDodSNO to equimolar concentration of NPs was about twofold higher than in the cells treated with SMA-Dox alone (from 48.6±5.3 to 79±10.1, P<0.05) (). Higher number of cells uptaking Dox accompanied the higher intracellular concentrations after 48 hours (). The percentage of cell population with high fluorescent intensity of Dox was significantly enhanced when cotreated with SMA-tDodSNO (P<0.001) from 38.3±4.9 (Dox-treated cells) to 72.5±4.0 (Dox+SMA-tDodSNO 10 µM) and 89.1±2.3 (Dox+SMA-tDodSNO 40 µM; ).
Figure 5 Effect of SMA-tDodSNO on SMA-Dox endocytosis.
Notes: Cells were treated with SMA-Dox (1 µM) and SMA-tDodSNO (10 or 40 µM) for 4 hours. The combination resulted in a significant increase in the SMA-Dox uptake in the cells. Data are expressed as mean values ± SD (n=3). dP<0.01 and pP <0.001 vs SMA-Dox group.
Abbreviations: Dox, doxorubicin; SMA, polystyrene-maleic acid; tDoDSNO, tert-dodecane S-nitrosothiol.
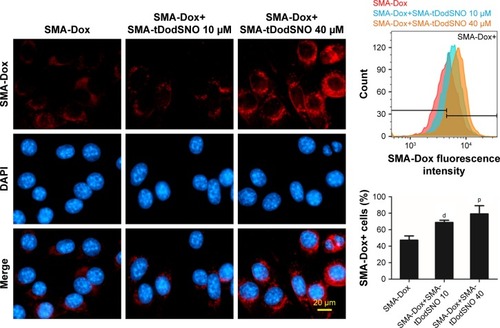
Figure 6 SMA-tDodSNO enhances Dox concentration in 4T1 cells. Cells were treated with Dox (0.1 μM) with or without SMA-tDodSNO (10 or 40 μM) for 48 hours.
Notes: Data are expressed as mean values ± SD (n=3). pP,0.001 vs Dox group.
Abbreviations: Dox, doxorubicin; SMA, polystyrene-maleic acid; tDoDSNO, tert-dodecane S-nitrosothiol.
Effect of SMA-tDodSNO on lysosome membrane permeability
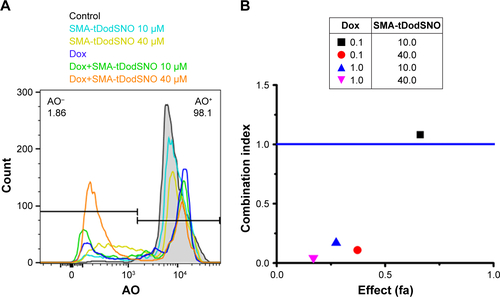
AO is a lipophilic fluorescent dye that is extensively used to stain acidic vesicular organelles including autolysosomes.Citation26 It readily diffuses into the cell compartments, and in an acidic pH of lysosomes is protonated and sequestered. The emission spectrum of protonated AO has a longer wavelength (AO is green and protonated AO is red), hence the intensity of the red fluorescence is proportional to the degree of acidity and/or the volume of the cellular acidic compartment.Citation27 Flow cytometry analysis was used to investigate the effect of SMA-tDodSNO treatment on lysosome membrane permeability. Results showed the difference in the percentage of the cell population with a high intensity of AO (AO+ cells). AO was significantly decreased when the cells were incubated with 40 µM SMA-tDodSNO for 4 hours (P<0.05 vs control; ). Four-hour incubation with SMA-Dox (1 µM) did not affect the lysosomal membrane permeability. However, the combination of SMA-tDodSNO and SMA-Dox resulted in a significant decrease in the population of AO+ cells compared to control and either treatment alone (). In addition, as reported in , Chou-Talalay analysis of combined SMA-tDodSNO (10 and 40 µM)- and Dox (1 µM)-treated cells for 48 hours showed a synergistic reduction in the population of AO+ cells (CI <1, ). The highest effect was observed at Dox 1 µM and SMA-tDodSNO 40 µM. In control cells, fluorescence is limited and evenly disbursed throughout the cell. While in the SMA-tDodSNO-treated cells, the organelles are larger in size and localized in few parts of the cells ().
Figure 7 SMA-tDodSNO treatment impaired lysosomal membrane permeability.
Notes: The cells were treated with SMA-Dox (1 µM) and/or SMA-tDodSNO (10 and 40 µM) for 4 hours, then stained by AO. The cells with high fluorescent intensity were named as AO+. Treatment of the cells with SMA-tDodSNO (40 µM) decreased significantly the percentage of AO+ cells. In addition, the combination of SMA-tDodSNO and SMA-Dox resulted in a significant decrease in the AO+ cells compared to either treatment alone. Data are expressed as mean values ± SD (N=3). bP<0.01 and cP<0.001 vs control, dP<0.05 and eP<0.05 vs SMA-Dox and SMA-tDodSNO (40 µM), respectively.
Abbreviations: AO, acridine orange; Dox, doxorubicin; SMA, polystyrene-maleic acid; tDodSNO, tert-dodecane S-nitrosothiol.
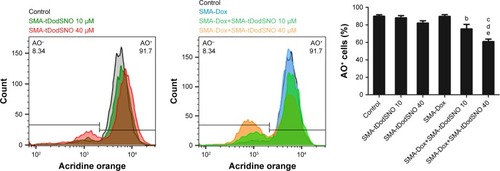
Figure 8 Effect of SMA-tDodSNO on lysosomal membrane permeability.
Notes: The cells were treated with Dox (0.1 µM) and/or SMA-tDodSNO (10 and 40 µM) for 48 hours, then stained by AO. In normal cells, the lysosomal compartments (red dots) have a small size and are evenly disbursed throughout the cell. In Dox- and SMA-tDodSNO-treated cells, the total red fluorescence of the cells decreased, and some of the fluorescence areas were larger in size and localized to few parts of the cells.
Abbreviations: AO, acridine orange; Dox, doxorubicin; SMA, polystyrene-maleic acid; tDodSNO, tert-dodecane S-nitrosothiol.
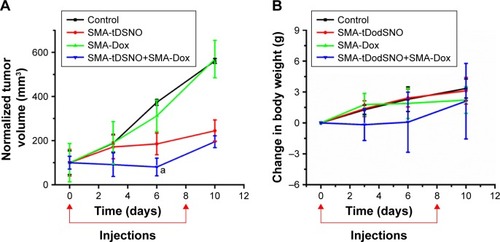
Effect of SMA-tDodSNO and SMA-Dox on concentrations in tumor tissues, tumor growth, and animals’ weight
We measured the concentration of SMA-Dox in tumor tissue upon treatment alone or in combination with SMA-tDodSNO. Local administration of SMA-tDodSNO (1 mg/kg) increased the tumor concentration of SMA-Dox 24 hours after the injections (1.65-fold of SMA-Dox alone); however, the difference did not reach statistical significance (). The effect of the treatments on tumor growth was measured in vivo in a xenograft model of TNBC. After 17 days of tumor inoculation, the control group and SMA-Dox-treated mice had equal rate of tumor progression (5.6-fold increase in the size compared to the day of drug injection D0) indicating that SMA-Dox on this tumor model at 5 mg/kg concentration was not effective (). Interestingly, SMA-tDodSNO alone resulted in a twofold reduction of the tumor size compared to the control group (244% vs 561% for control and 569% for SMA-Dox alone). Combined treatment of SMA-Dox and SMA-tDodSNO significantly arrested the tumor growth for the first 6 days of treatment (80% vs 375% for control; P<0.05) and at day 10 post injection, tumor volume was three times less than in the mice treated with SMA-Dox alone (195% vs 569% for SMA-Dox group; ); however, the difference was not statistically significant (vs either SMA-tDodSNO or SMA-Dox alone). General toxicity in mice following the SMA-tDodSNO was assessed through the experiment. The treatments did not result in any significant weight loss over the study duration indicating the safety of the combination ().
Figure 9 Effect of subcutaneous administration of SMA-tDodSNO on the concentration of SMA-Dox in tumor tissue.
Notes: To mice, intravenous SMA-Dox (5 mg/kg) or intravenous SMA-Dox (5 mg/kg)+ subcutaneous SMA-tDodSNO (1 mg/kg) were injected, and 24 hours later, the concentration of SMA-Dox in tumor tissue was evaluated. SMA-tDodSNO increased the tumor concentration of Dox; however, it was not statistically significant. Results are expressed as the mean ± SD (n=4).
Abbreviations: Dox, doxorubicin; SMA, polystyrene-maleic acid; tDodSNO, tert-dodecane S-nitrosothiol.
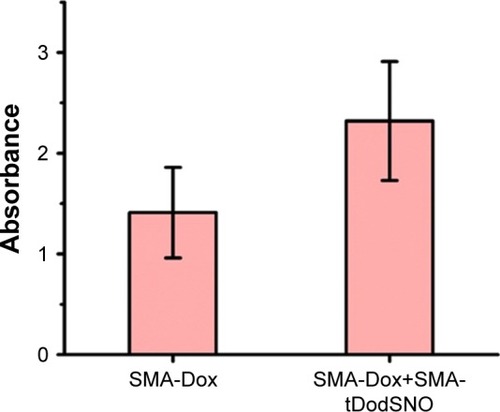
Figure 10 Effect of SMA-tDodSNO and SMA-Dox on tumor growth.
Notes: SMA-tDodSNO (1 mg/kg; subcutaneous) and SMA-Dox (5 mg/kg; intravenous) were administered alone and in combination to mice bearing mammary 4T1 tumors at days 0 and 8 of the study. The normalized tumor volume was evaluated as a function of time. The difference between the combination and either treatment alone (A) at day 6 was statistically significant (P=0.0406 for SMA-tDodSNO, and vs SMA-Dox P=0.023). (B) Body weight was evaluated as an indicator of general acute toxicity normalized. Data are expressed as mean ± SD (n=5). aP<0.001 vs control.
Abbreviations: Dox, doxorubicin; SMA, polystyrene-maleic acid; tDodSNO, tert-dodecane S-nitrosothiol.
Discussion
Targeted anticancer therapies using NP-based drug carriers have emerged as an appealing approach to overcome the limitations associated with conventional drugs such as poor pharmacokinetics resulting in dose-limiting side-effects. Few Nano-based drugs reached clinical applications as in the case of Dox, where improvements in tumor targeting and decreased cardiotoxicity resulted in the Food and Drug Administration approval of Doxil® (Doxorubicin liposomal) for the treatment of Kaposi’s sarcoma.Citation28 However, efficacious responses to Dox-loaded NPs (as well as other anticancer NPs) in tumors can be impaired by reticuloendothelial clearance, blood flow limitations, cellular internalization, escape from endosomal and lysosomal compartments, and drug efflux pumps.Citation29,Citation30
Recent experimental studies have shown that combination of NO donor drugs and Dox or Dox-loaded NPs potentiate the anticancer effects of Dox.Citation31–Citation33 However, currently available NO donors are unstable and possess limited NO payloads; therefore, they cannot be used for targeting tumors.Citation11 In addition, the mechanism by which NO donors improve the anticancer effects of Dox is not yet fully investigated.
Here, we report that SMA-tDodSNO in combination with free Dox or SMA-Dox improves their anticancer properties. Combination treatments reduce cell viability and significantly enhanced early and late apoptosis in 4T1 cancer cells when compared to control as demonstrated by cell cycle analysis. Quantification of the cell population in the subG1 phase has been known as an easy way to score apoptotic events.Citation18 Upon incubation with a combination of SMA-tDodSNO (40 µM) and Dox (0.1 µM) for 48 hours, the majority of the cell population (87%) were in the subG1 phase. Annexin V/PI assay showed that around 80% of the treated cells were not stained by PI (PI−) indicating that they were alive.Citation34 Hence, it can be concluded that combined treatment of SMA-tDodSNO and Dox arrests the cells in SubG1 phase, which then results in apoptosis. In addition, as an early indicator of apoptosis, we studied the mitochondrial dysfunction.Citation22,Citation23 Treatments with SMA-tDodSNO and/or Dox resulted in a significant depolarization of mitochondrial membrane, shown by the decrease in the TMRE fluorescence. This effect was potentiated when cells were treated with both treatments concurrently. Reactive oxygen species (ROS) and reactive nitrogen species (RNS) can significantly affect mitochondrial membrane permeability and guide cells to apoptosis and necrosis.Citation35 ROS and RNS generation plays important role in the cytotoxicity induced by Dox and NO donors.Citation36,Citation37 Dox increases mitochondrial generation of O2.−.Citation38 In addition, the reaction of NO with other free radicals such as O2.− produces highly cytotoxic free radicals such as ONOO−.Citation39 Therefore, combination of NO donor and Dox probably facilitates the production of such highly reactive species that cause damage at key intracellular sites and theoretically can reduce resistance to Dox.
Combination of SMA-Dox and SMA-tDodSNO in vitro remarkably enhanced the intracellular concentration of SMA-Dox within 4 hours compared to the SMA-Dox-treated cells. Cellular uptake of NPs occurs through endocytosis;Citation40 therefore, the enhanced SMA-Dox uptake could be due to the facilitated endocytosis. This is supported by earlier reports that showed that NO accelerates endocytosis by S-nitrosylation of dynamin, a GTPase enzyme that has a critical role in endocytic membrane fission events,Citation41 and increases its ability to hydrolyze GTP and cleave the endocytic vesicle free from the cell membrane.Citation42 Hence, in our model, NO-releasing NPs, such as SMA-tDodSNO, can be used to enhance membrane penetration of NPs. In addition, when SMA-tDodSNO was added to Dox, a twofold higher concentration of Dox in the cells was detected.Citation43 The increased intracellular concentration of Dox is in agreement with previously reported studies and seems to be responsible for the synergistic cytotoxicity of NO donor drugs and Dox when used in combination.Citation40,Citation44
One limitation related to the intracellular delivery of NPs is the escape from endosomal and lysosomal compartments, as low-pH environment and enzymes are proved to be detrimental to nanodelivery systems cargo.Citation29 Therefore, we measured AO staining as a measure of lysosomal membrane integrity. The loss of lysosomal membrane integrity can be measured as the loss of red fluorescence of AO.Citation45,Citation46 SMA-tDodSNO significantly decreased the percentage of the cell population with a high intensity of red fluorescence. In addition, when it combined with SMA-Dox or free Dox, its effect on lysosomal compartment was significantly potentiated. The effects of NO on lysosomes have been poorly investigated so far. Sarkar et al have shown that NO exhibits complex inhibitory effects on the autophagy process.Citation47,Citation48 Following the loss of lysosome membrane integrity, the lysosomal cysteine proteases, cathepsins, penetrate into the cytoplasm and activate necrosis and apoptosis.Citation49,Citation50 Our results suggest that the another possible mechanism for the synergistic anticancer activity of Dox and SMA-tDodSNO might be their synergistic destabilization of lysosomal compartments. This is in agreement with a recent study that has shown that supplementation of Dox with lysosome inhibitors such as bafilomycin A1 and chloroquine provided a more efficient anticancer effect in hepatic cancer cells by increasing lysosomal membrane permeability.Citation51
Subcutaneous administration of SMA-tDodSNO (1 mg/mL) did not induce any sign of toxicity in mice and when administered with SMA-Dox, it increased the concentration of Dox in tumor tissue, even though the difference was not statistically significant. This is in agreement with earlier reports that showed that NO donorsCitation52–Citation55 and other vasodilators like sildenafilCitation56 enhance EPR effects in tumor tissues. In addition, our findings are in agreement with earlier reports showing that the NO donors inhibited drug resistance by decreasing the expression of P-glycoproteins in CT26 cell line.Citation31
Treatments with SMA-tDodSNO in vivo resulted in a twofold decrease in tumor size, which supports the in vitro apoptotic and anticancer properties of the NPs. Herein, we hypothesize that the antitumor effects of SMA-tDodSNO could be due to the generation of nitrosative and oxidative stress in the cancer cells.Citation57,Citation58 As expected, the highest antitumor effects were observed when SMA-tDodSNO and SMA-Dox were injected concurrently. It has been shown that NO sensitizes cancer cells to subtoxic chemo-immunocytotoxic agents by its direct inhibition of nuclear factor kappa B (NF-κB) and Snail (the NF-κB target gene).Citation59 Previous studies in 4T1 TNBC model using the free Dox at the same dose equivalence of SMA-Dox in this study failed to show any significant anticancer activity.Citation56,Citation60
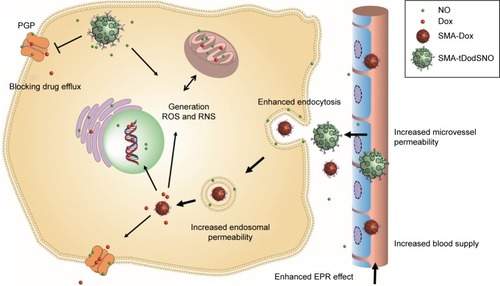
Finally, in , we schematically showed our hypothesis explaining the potential beneficial effects of SMA-tDodSNO on the antitumor properties of Dox and SMA-Dox. SMA-tDodSNO could enhance blood supply and vessel permeability in tumor tissues, which results in the accumulation of SMA-Dox. In addition, SMA-tDodSNO can help to overcome some of the biologic barriers that hinder the delivery of SMA-Dox. Uptake studies showed that SMA-tDodSNO that increases the intracellular concentration of SMA-Dox may be favoring their endosomal escape. Attenuating the drug efflux from the cells or increasing its intracellular concentration with consequent generation of RNS and ROS would help to prevent drug resistance and improve the efficacy of anticancer drugs.
Figure 11 Possible mechanisms by which SMA-tDodSNO potentiates the anticancer efficacy of SMA-Dox and Dox.
Notes: Due to sustained NO release, the vessels can be dilated and blood supply to the tumor can be enhanced, rendering vessels permeable to SMA-Dox. Endocytosis of SMA-Dox could also be enhanced when combined with SMA-tDodSNO. Endosomal escape of SMA-Dox could be facilitated, given the higher endosomal membrane permeability caused by SMA-tDodSNO treatment. In addition, SMA-tDodSNO as an NO-releasing agent can sensitize cancer cells to chemotherapeutic drugs such as Dox.
Abbreviations: Dox, doxorubicin; EPR, enhanced permeability and retention; NO, nitric oxide; RNS, reactive nitrogen species; ROS, reactive nitrogen species; SMA, polystyrene-maleic acid; tDodSNO, tert-dodecane S-nitrosothiol.
Conclusion
In this work, we demonstrated that SMA-tDodSNO as a novel NO-releasing NP synergistically increased anticancer properties of Dox-loaded NPs through enhanced EPR effect, compromising endosomal membrane integrity, enhancing intracellular concentrations, and augmenting the overall drug concentrations in tumor tissues. Our work suggests that stable NO donor NPs such as SMA-tDodSNO can be used to overcome the biologic barriers, which hinder the efficacy of anticancer NPs.
Author contributions
HA designed and conducted in vitro experiments, analyzed the data, and wrote the draft of the manuscript; KG conceived the idea, acquired the fund, supervised the work, designed and conducted the in vivo work, and contributed to writing the manuscript; AB-F conducted the flow cytometry work and analyzed its data; LA contributed to in vivo work; VP contributed to in vivo work and to writing and revising the manuscript. All authors contributed toward data analysis, drafting and revising the paper, gave approval for the final version to be published and agree to be accountable for all aspects of the work.
Acknowledgments
The authors would like to thank Dr Greg Giles (Otago University) for all the generous support he provided throughout this work and Prof Sarah Hook (Otago University) for the use of FACScan flow cytometer.
Supplementary materials
Figure S1 Identification and gating of single cells by standard biparametric dot plot.
Notes: (1) The main population of cells was separated from possible noises (SSC-A vs FSC-A), then (2) single cells were selected using FSC-H vs FSC-A plot. Plotting cell count vs DNA content (the PI intensity) showed atypical cell cycle in control group. The population of the cells colored in blue are in G1 phase, green is showing cells in synthesis phase, and red represents cells in G2 phase.
Abbreviations: FSC-A, forward scatter area; FSC-H, forward scatter height; PI, propidium iodide; SSC-A, side scatter area.
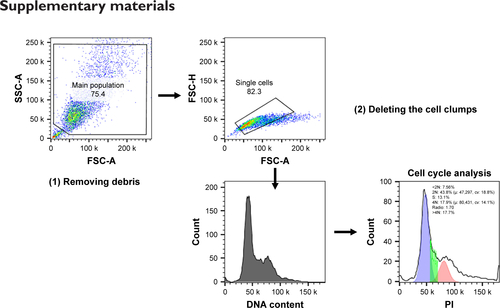
Figure S2 (A) Flow cytometry spectrum of AO-stained cells and treated with free Dox (0.1 µM) and/or SMA-tDodSNO (10 and 40 µM). The percentage of the cell population with high fluorescent intensity (AO+) decreased following the treatments. (B) Chou-Talalay analysis showed a synergistic increase in the lysosomal permeability (decrease in the population of AO+) when the cells were treated with Dox (0.1 and 1 µM) and SMA-tDodSNO (10 and 40 µM) concurrently. The highest effect was observed at Dox 1 µM and SMA-tDodSNO 40 µM.
Abbreviations: AO, acridine orange; Dox, doxorubicin; SMA, polystyrene-maleic acid; tDoDSNO, tert-dodecane S-nitrosothiol.
Disclosure
The authors report no conflicts of interest in this work.
References
- GreishKEnhanced permeability and retention of macromolecular drugs in solid tumors: a royal gate for targeted anticancer nanomedicinesJ Drug Target2007157–845746417671892
- MaedaHNakamuraHFangJThe EPR effect for macromolecular drug delivery to solid tumors: improvement of tumor uptake, lowering of systemic toxicity, and distinct tumor imaging in vivoAdv Drug Deliv Rev2013651717923088862
- MaedaHWuJSawaTMatsumuraYHoriKTumor vascular permeability and the EPR effect in macromolecular therapeutics: a reviewJ Control Release2000651–227128410699287
- AlimoradiHMatikondaSSGambleABGilesGIGreishKHypoxia responsive drug delivery systems in tumor therapyCurr Pharm Des201622192808282026898739
- BaruaSMitragotriSChallenges associated with penetration of nanoparticles across cell and tissue barriers: a review of current status and future prospectsNano Today20149222324325132862
- NettiPABerkDASwartzMAGrodzinskyAJJainRKRole of extracellular matrix assembly in interstitial transport in solid tumorsCancer Res20006092497250310811131
- BarefordLMSwaanPWEndocytic mechanisms for targeted drug deliveryAdv Drug Deliv Rev200759874875817659804
- YinQShenJZhangZYuHLiYReversal of multidrug resistance by stimuli-responsive drug delivery systems for therapy of tumorAdv Drug Deliv Rev20136513–141699171523611952
- SelbyLICortez-JugoCMSuchGKJohnstonAPRNanoescapology: progress toward understanding the endosomal escape of polymeric nanoparticlesWiley Interdiscip Rev Nanomed Nanobiotechnol201795e1452
- KumarVHongSYMaciagAEStabilization of the nitric oxide (NO) prodrugs and anticancer leads, PABA/NO and double JS-K, through incorporation into PEG-protected nanoparticlesMol Pharm20107129129820000791
- MillerMRMegsonILRecent developments in nitric oxide donor drugsBr J Pharmacol2007151330532117401442
- GilesNMKumariSGangBPYuenCWBillaudEMGilesGIThe molecular design of S-nitrosothiols as photodynamic agents for controlled nitric oxide releaseChem Biol Drug Des201280347147822642531
- KumariSSammutIAGilesGIThe design of nitric oxide donor drugs: s-nitrosothiol tDodSNO is a superior photoactivated donor in comparison to GSNO and SNAPEur J Pharmacol201473716817624858367
- LowensteinCJNitric oxide regulation of protein trafficking in the cardiovascular systemCardiovasc Res200775224024617490627
- GreishKSawaTFangJAkaikeTMaedaHSMA-doxorubicin, a new polymeric micellar drug for effective targeting to solid tumoursJ Control Release200497221923015196749
- KaurPNagarajaGMZhengHA mouse model for triple-negative breast cancer tumor-initiating cells (TNBC-TICs) exhibits similar aggressive phenotype to the human diseaseBMC Cancer20121212022452810
- VermesIHaanenCSteffens-NakkenHReutelingspergerCA novel assay for apoptosis. Flow cytometric detection of phosphatidylserine expression on early apoptotic cells using fluorescein labelled Annexin VJ Immunol Methods1995184139517622868
- Rello-VaronaSHerrero-MartínDLópez-AlemanyRMuñoz-PinedoCTiradoOM“(Not) all (dead) things share the same breath”: identification of cell death mechanisms in anticancer therapyCancer Res201575691391725724677
- LoewLMCarringtonWTuftRAFayFSPhysiological cytosolic Ca2+ transients evoke concurrent mitochondrial depolarizationsProc Natl Acad Sci U S A1994912612579125837809081
- FarkasDLWeiMDFebbrorielloPCarsonJHLoewLMSimultaneous imaging of cell and mitochondrial membrane potentialsBiophys J1989566105310692611324
- ChouTCDrug combination studies and their synergy quantification using the Chou-Talalay methodCancer Res201070244044620068163
- GreenPSLeeuwenburghCMitochondrial dysfunction is an early indicator of doxorubicin-induced apoptosisBiochim Biophys Acta2002158819410112379319
- DoutheilJAlthausenSTreimanMPaschenWEffect of nitric oxide on endoplasmic reticulum calcium homeostasis, protein synthesis and energy metabolismCell Calcium200027210711510756977
- BossOSamecSKühneFUncoupling protein-3 expression in rodent skeletal muscle is modulated by food intake but not by changes in environmental temperatureJ Biol Chem19982731589417036
- ZhangSLiJLykotrafitisGBaoGSureshSSize-dependent endocytosis of nanoparticlesAdv Mater20092141942419606281
- Pierzyńska-MachAJanowskiPADobruckiJWEvaluation of acridine orange, LysoTracker Red, and quinacrine as fluorescent probes for long-term tracking of acidic vesiclesCytometry A201485872973724953340
- TraganosFDarzynkiewiczZLysosomal proton pump activity: supravital cell staining with acridine orange differentiates leukocyte subpopulationsMethods Cell Biol1994411851947532261
- BarenholzYDoxil® – the first FDA-approved nano-drug: lessons learnedJ Control Release2012160211713422484195
- BlancoEShenHFerrariMPrinciples of nanoparticle design for overcoming biological barriers to drug deliveryNat Biotechnol201533994195126348965
- RigantiCMiragliaEViarisioDNitric oxide reverts the resistance to doxorubicin in human colon cancer cells by inhibiting the drug effluxCancer Res200565251652515695394
- TanLHuangRLiXLiuSShenYMControllable release of nitric oxide and doxorubicin from engineered nanospheres for synergistic tumor therapyActa Biomater20175749851028499633
- SongQTanSZhuangXNitric oxide releasing d-α-tocopheryl polyethylene glycol succinate for enhancing antitumor activity of doxorubicinMol Pharm201411114118412925222114
- KashfiKRigasBMolecular targets of nitric-oxide-donating aspirin in cancerBiochem Soc Trans200533Pt 470170416042578
- RiegerAMNelsonKLKonowalchukJDBarredaDRModified annexin V/propidium iodide apoptosis assay for accurate assessment of cell deathJ Vis Exp2011502597
- WinkDAMitchellJBChemical biology of nitric oxide: insights into regulatory, cytotoxic, and cytoprotective mechanisms of nitric oxideFree Radic Biol Med1998254–54344569741580
- SenSKawaharaBChaudhuriGMitochondrial-associated nitric oxide synthase activity inhibits cytochrome c oxidase: implications for breast cancerFree Radic Biol Med20135721022023089229
- MimnaughEGTrushMABhatnagarMGramTEEnhancement of reactive oxygen-dependent mitochondrial membrane lipid peroxidation by the anticancer drug adriamycinBiochem Pharmacol19853468478563977958
- GoormaghtighEPollakisGRuysschaertJMMitochondrial membrane modifications induced by adriamycin-mediated electron transportBiochem Pharmacol19833258898936838634
- BrownGCNitric oxide and mitochondrial respirationBiochim Biophys Acta199914112–335136910320668
- RigantiCMiragliaEViarisioDNitric oxide reverts the resistance to doxorubicin in human colon cancer cells by inhibiting the drug effluxCancer Res200565251652515695394
- FergusonSMDe CamilliPDynamin, a membrane-remodelling GTPaseNat Rev Mol Cell Biol2012132758822233676
- WangGMoniriNHOzawaKStamlerJSDaakaYNitric oxide regulates endocytosis by S-nitrosylation of dynaminProc Natl Acad Sci U S A200610351295130016432212
- EvansCJPhillipsRMJonesPFA mathematical model of doxorubicin penetration through multicellular layersJ Theor Biol2009257459860819183560
- KimJYungBCKimWJChenXCombination of nitric oxide and drug delivery systems: tools for overcoming drug resistance in chemotherapyJ Control Release201726322323028034787
- PetersenNHOlsenODGroth-PedersenLTransformation-associated changes in sphingolipid metabolism sensitize cells to lysosomal cell death induced by inhibitors of acid sphingomyelinaseCancer Cell201324337939324029234
- KirkegaardTRothAGPetersenNHHsp70 stabilizes lysosomes and reverts Niemann-Pick disease-associated lysosomal pathologyNature2010463728054955320111001
- SarkarSKorolchukVIRennaMComplex inhibitory effects of nitric oxide on autophagyMol Cell2011431193221726807
- YuHXiaoYJinLA lysosome-targetable and two-photon fluorescent probe for monitoring endogenous and exogenous nitric oxide in living cellsJ Am Chem Soc201213442174861748923043509
- RepnikUStokaVTurkVTurkBLysosomes and lysosomal cathepsins in cell deathBiochim Biophys Acta201218241223321914490
- KroemerGJäätteläMLysosomes and autophagy in cell death controlNat Rev Cancer200551188689716239905
- LiYSunYJingLLysosome inhibitors enhance the chemotherapeutic activity of doxorubicin in HepG2 cellsChemotherapy2017622859327764836
- KinoshitaRIshimaYChuangVTGImproved anticancer effects of albumin-bound paclitaxel nanoparticle via augmentation of EPR effect and albumin-protein interactions using S-nitrosated human serum albumin dimerBiomaterials201714016216928651144
- MaedaHMacromolecular therapeutics in cancer treatment: the EPR effect and beyondJ Control Release2012164213814422595146
- IshimaYInoueAFangJPoly-S-nitrosated human albumin enhances the antitumor and antimetastasis effect of bevacizumab, partly by inhibiting autophagy through the generation of nitric oxideCancer Sci2015106219420025457681
- IshimaYAlbumin-based nitric oxide traffic system for the treatment of intractable cancersBiol Pharm Bull201740212813428154250
- GreishKFateelMAbdelghanySRachelNAlimoradiHBakhietMSildenafil citrate improves the delivery and anticancer activity of doxorubicin formulations in a mouse model of breast cancerJ Drug Target201826761061529148852
- ChoudhariSKChaudharyMBagdeSGadbailARJoshiVNitric oxide and cancer: a reviewWorld J Surg Oncol20131111823718886
- MorikawaSBalukPKaidohTHaskellAJainRKMcDonaldDMAbnormalities in pericytes on blood vessels and endothelial sprouts in tumorsAm J Pathol20021603985100011891196
- BonavidaBGarbanHNitric oxide-mediated sensitization of resistant tumor cells to apoptosis by chemo-immunotherapeuticsRedox Biol2015648649426432660
- GreishKTaurinSMorsyMAThe effect of adjuvant therapy with TNF-α on animal model of triple-negative breast cancerTher Deliv20189533334229681232
