Abstract
During the last decade, there has been a huge advancement in the use of transperineal ultrasound (TPU) in the field of obstetrics and gynecology. Its main applications in obstetrics include the monitoring of fetal progression in labor and recently the assessment of maternal pelvic dimensions, whereas in gynecology, TPU is at present widely used for the evaluation of the female pelvic floor, opening new boundaries for the assessment of pelvic floor disorders. The association of volumetric three-dimensional techniques has largely contributed to the remarkable progress that has occurred in the use of TPU. The aim of this paper is to offer an overview of the advantages, challenges and future perspectives of the use of TPU for women’s imaging.
The use of transperineal ultrasound in gynecology
In the past few years, the use of transperineal ultrasound (TPU) in gynecology, especially for the evaluation of the female pelvic floor, has experienced remarkable progress with a huge potential for the improvement of women’s health.Citation1–Citation4 TPU provided an objective and reproducible method for the assessment of the female pelvic floor, and considerably increased our understanding of the link between childbirth and female pelvic floor dysfunction.
Whereas two-dimensional (2D) TPU can visualize and assess reliably the midline structure of the pelvic floorCitation5 (), the visualization of the plane of the pelvic floor muscles (levator ani muscle, LAM) is impossible without the help of three-dimensional (3D) technique. The LAM is the main support of pelvic organs, surrounding the largest hernial orifice in the female human abdomen and pelvis, which is the pelvic hiatus.Citation2,Citation6 Integrity and appropriate function of LAM are main keys for normal pelvic function. Since LAM lies in the axial plane, it cannot be visualized by using 2D ultrasound; therefore, 3D ultrasound, now widely available, permits reliable assessment of both the integrity and function of LAM.
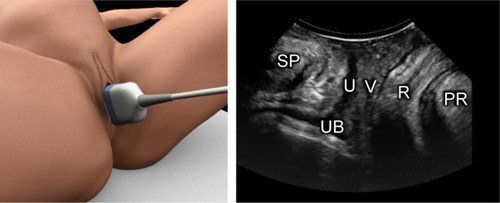
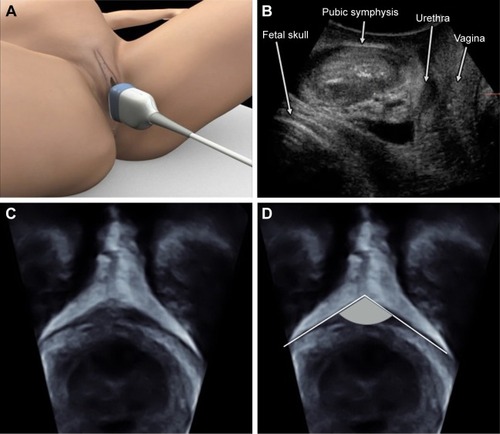
Figure 1 Two-dimensional view of the midsagittal plane of the pelvic floor.
Evaluation of pelvic organs prolapse
TPU for evaluation of the pelvic organs prolapse is performed with the patient in the lithotomy position, with hips flexed and abducted. A convex transducer (3–6 MHz) is placed transperineally on the midline (). By placing the transducer on the midsagittal plane, it is possible to visualize a section of the pubic symphysis, the urethra with the bladder, vaginal walls, perineal muscles, rectum and anal canal and anorectal angle.
The descent of the urethra, bladder, cervix and rectum during Valsalva maneuver is easily documented in the midsagittal plane with reference to a landmark defined by the inferoposterior margin of the symphysis pubis, as described by Dietz et al.Citation5 For this purpose, the 3D technology does not seem to add any relevant information. Nevertheless, in some cases, rendered volumes may allow complete 3D visualization of a cystocele or rectocele, and hence, 3D ultrasound is likely to become useful in the identification of fascial defects (eg, transverse or lateral tears of the rectovaginal septum).Citation7
In addition, the acquisition of 3D datasets allows the storage of data for further analysis. 3D TPU may also improve intra- and interobserver reproducibility in the evaluation of pelvic organs prolapse, but further studies are needed for this purpose.
Evaluation of LAM
The real advantage of 3D TPU lies in the ability of assessing the integrity of the entire LAM in particular with its attachment to the pubic rami (also referred to as “pubovisceral muscle” or “pubococcygeus/puborectalis muscle”).Citation8
Until a few years ago, magnetic resonance imaging (MRI) was the only imaging technique available for assessment of LAM anatomy. The advent of 3D/4D TPU now allows LAM evaluation in a more dynamic and economical way compared with MRI. While 3D TPU can reconstruct the 3D structure of LAM, the advantage of four-dimensional (4D) scan is its ability to assess the dynamic functional changes of the pelvic floor muscles under contraction and under Valsalva maneuver. It is important to point out that 2D, 3D and 4D TPU are a continuum, being complementary rather than comparable.
In 2005, Dietz et al established 3D TPU as a reliable and reproducible method for assessing LAM biometry and defined biometric parameters of LAM and levator hiatus.Citation9 They also found a significant correlation between levator hiatus area and pelvic organ descent, thus confirming the previously set hypothesisCitation8 of LAM anatomy and integrity playing an independent role in determining pelvic organ support.
LAM abnormalities are common in urogynecological patients, especially in parous women, and they are associated with prolapse of the anterior and central compartments.Citation10
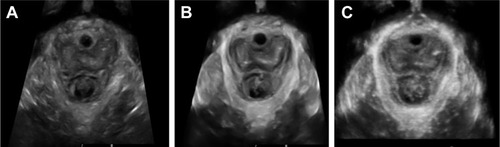
Although some authors measure the hiatal area using only the multiplanar mode, it has been demonstrated that thick-slice reconstruction (1–2 cm using render mode) correlates more strongly with symptoms of prolapse in comparison with the sectional planesCitation11 ().
Figure 2 A comparison of the images of the axial view using the three methods for the demonstration of levator ani muscle.
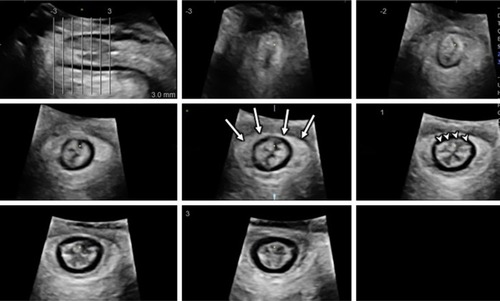
With 3D TPU, it is also possible to obtain “tomographic imaging”, through tomographic ultrasound imaging (TUI) (), a technique that reproduces pelvic floor “slices”.
Figure 3 Tomographic ultrasound imaging of the levator ani muscle obtained by three-dimensional/four-dimensional transperineal ultrasound.
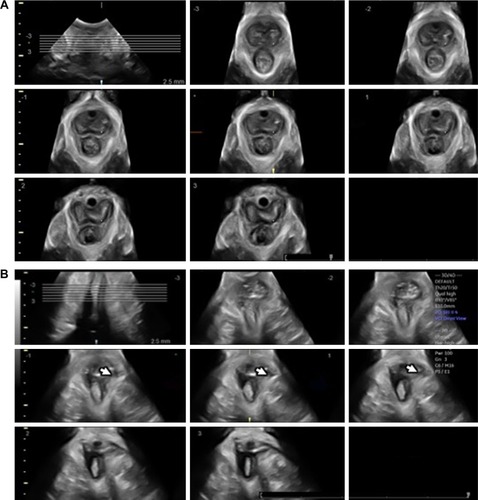
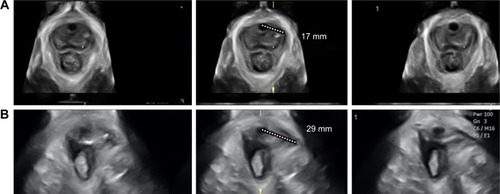
Once established that LAM defects apparently were best defined on muscular contraction, in 2007 Dietz proposed an assessment system with TUI which described the depth of the injury by counting the number of slices in which defects were identified.Citation12 Later, the author suggested an objective measurement of LAM defects (). The minimum distance between the center of the urethra and the insertion of the most medial component of the LAM on the pelvic sidewall on TUI images (the so-called levator–urethra gap, LUG) was found to be reproducible and strongly associated with levator trauma detected on palpation. The author also suggested a cut-off of 25 mm for the diagnosis of levator avulsion injury in doubtful cases.Citation13
Figure 4 Measurement of the levator–urethra gap (LUG) on tomographic ultrasound imaging (TUI).
Pelvic floor injury diagnosed by 3D/4D TPU and pregnancy/delivery
The association between vaginal childbirth, pelvic organ prolapse and pelvic floor dysfunction is nowadays more clearly established.Citation6,Citation14 It has also been demonstrated that LAM trauma and in particular a detachment or “avulsion” of the muscle from its insertion on the inferior pubic ramus and pelvic sidewall predisposes women to prolapse, especially of the anterior and central compartments.Citation12 LAM avulsions can now be reliably diagnosed by 3D/4D TPU.Citation13,Citation15–Citation18
Levator trauma seems to be the “missing link” explaining the epidemiological association between childbirth and female pelvic organ prolapse.Citation19 In fact, a 2008 study demonstrated that women examined at a urogynecological clinic presenting levator avulsion injury were approximately twice as likely to have significant pelvic organs prolapse, especially cystocele and uterine prolapse, than those with an intact levator muscle. In addition, women with significant prolapse revealed a fourfold higher prevalence of levator avulsion injury than those without.Citation20
Whereas the vast majority of the literature on 3D/4D TPU has focused on prolapse, incontinence and the correlation between pregnancy, labor and pelvic floor dysfunction, this technique may be useful in the understanding and management of other pathologies. A very recent study by Raimondo et al, showed that women with deep infiltrating endometriosis have an increased LAM tone, and less ability to dilate their pelvic hiatus on Valsalva maneuver and to contract LAM instead of relaxing with this maneuver (LAM coactivation).Citation21 These findings open the door for many other studies on the assessment and management of women with chronic pelvic pain disorders.
Ballooning of the levator hiatus
Further studies performed through MRI and TPU found LAM trauma in 15%–30% of women who delivered vaginallyCitation3,Citation19 and concluded that LAM avulsion as a result of vaginal childbirth is associated with abnormal levator biometry and function as well as with pelvic organs prolapse.Citation16,Citation22
But a LAM avulsion does not seem to be the only factor involved in pelvic floor dysfunction. An enlarged hiatus can also be related to pelvic organs prolapse: in 2008, Dietz et al performed a 3D/4D TPU retrospective study with the aim of defining “normality” for hiatal area by assessing its relationship with symptoms and clinical signs of prolapse. They demonstrated that levator hiatal area is strongly associated with symptoms and clinical signs of prolapse and introduced the idea of “ballooning” (a hiatal area of >25 cm2 on Valsalva), suggesting that this could be used as a cut-off for abnormal distensibility of the levator hiatus.Citation23 Subsequently, vaginal delivery has been associated both with levator trauma and with hiatal enlargement.Citation3
Using 3D/4D TPU, many authors tried to unveil the main risk factors for LAM injury.
Associations have been found with vaginal delivery, operative delivery (particularly forceps delivery, the association is uncertain for vacuum delivery) and a prolonged second stage of labor.Citation22,Citation24–Citation27
Epidural analgesia may exert a protective effect, but further studies are needed to confirm this finding.Citation24 Some authors found an association of levator injury with birthweight, but other authors ruled out this relationship.Citation28
Feasibility and repeatability of 3D/4D TPU
As far as repeatability is concerned, a number of studies have reported data on interobserver reliability, demonstrating moderate-to-almost perfect reproducibility for measuring levator hiatal dimensions with 3D/4D TPU, both at rest and in dynamic conditions.Citation29–Citation31
In accordance with these findings, van Veelen et alCitation32 have shown that, in nulliparous and primiparous women, the measurement of the levator hiatus and levator-urethra gap (LUG) using 3D/4D ultrasound imaging is highly reliable. They demonstrated that the technique used to measure levator hiatal distances requires limited teaching, while LUG measurement using TUI is more challenging.Citation9,Citation29–Citation35
Recently, van Delft et al have compared 3D and 4D TPU to endovaginal ultrasound and digital palpation in the evaluation of pelvic floor muscle contractility, revealing a good correlation between these three methods.Citation36,Citation37 In addition, they demonstrated that TPU had the further advantage of providing good visual biofeedback when training patients in pelvic floor muscle exercises.
Volume contrast imaging (VCI)
In the vast majority of the studies about 3D TPU, pelvic hiatal area is measured with multiplanar mode, which means using orthogonal 2D slices of a 3D volume.Citation9 However, it has been shown that using a 3D/4D render of a slice measuring 1–2 cm offers more valid measurements that correlate better with the symptoms of pelvic organ prolapse.Citation38 Nevertheless, the render technique might be more difficult than the multiplanar mode. Youssef et al recently demonstrated that a simplified technique combining linear 3D/4D reconstruction (Omniview; GE Medical Systems, Zipf, Austria) combined with contrast-enhancing tool (VCI; GE Medical Systems) could be used as a simple tool for the evaluation of the pelvic hiatal area with excellent intra- and interobserver repeatability. Furthermore, the suggested technique showed very good correlation with the 3D render techniqueCitation39 (). This was also confirmed during contraction and on Valsalva maneuver. They concluded that both rendering mode and Omniview-VCI can be used interchangeably for assessing pelvic hiatal area with 3D and 4D TPU.Citation40
Very recently, the same group has demonstrated that although there is good evidence to support that the plane of the LAM is curved (warped), the degree of warping is never greater than the usual thickness of 1–2 cm, used for the 3D reconstruction with the renderCitation6 and the Omniview-VCI.Citation39,Citation40 They confirmed that there is no need to use a curved reconstruction 3D/4D technique for the assessment of LAM.Citation41
3D imaging of synthetic implant materials
3D TPU may also be helpful in the assessment of synthetic pelvic implant materials. Most of the modern synthetic implant materials, such as tension-free vaginal tape (TVT), suprapubic arc tape (SPARC) or intravaginal slingplasty (IVS), are highly echogenic. 3D TPU allows to distinguish among these techniques and to diagnose variations in their placement. Through 3D TPU, it is also possible to identify on the axial plane most of the injectables used in anti-incontinence surgery and placed around the urethra.Citation7
A prospective randomized controlled trial assessed the effectiveness of suburethral slings and found that the three main types of suburethral sling (TVT, SPARC and IVS), investigated using 2D and 3D TPU, can be visualized by ultrasound and showed comparable outcomes.Citation42
Assessment of anal sphincter integrity
Fecal incontinence occurs in approximately 2% of the adult population, and obstetric injury of the anal sphincter (OASIS) is its most common cause.Citation43 A prompt and precise diagnosis of OASIS immediately after delivery is essential to correctly repair the anal sphincter and thus reduce the risk of fecal incontinence. Endoanal ultrasound remains the gold standard for anal sphincter assessment. MRI is a reliable technique for the evaluation of the anal sphincter complex but is expensive and not easily accessible.
With a particular attention to the obstetric context, Valsky et al, in a study on 139 patients, confirmed that 3D TPU with the multiplanar technique is an accessible and promising method for postpartum sphincter evaluationCitation44 (). The same group found that two-thirds of women, after third- or fourth-degree tears, suffered from some degree of incontinence and that normal later sonographic appearance of the anal sphincter complex was associated with an increased rate of clinical symptoms of incontinence. Since they found that the early sonographic signs of anal sphincter tears disappeared in almost half of the patients, they suggested that this examination should be postponed from the early postpartum period.Citation45
Figure 5 Three-dimensional transperineal tomographic ultrasound images of anal sphincter.
Faltin et al and Guzmán Rojas et al identified significant defects of the external anal sphincter (EAS) on 3D/4D TPU with TUI technique in 27.9% of the patients who delivered vaginally. Most women with EAS damage on ultrasound (87.0%) had not been diagnosed as having EAS tears in the delivery suite.Citation46,Citation47
Recently, Guzmán Rojas et al attempted to define normal residual anal sphincter defect at TUI. They suggested that four to six EAS slices showing a defect of ≥30° should be required for the diagnosis of significant EAS trauma.Citation48
Therefore, although endoanal ultrasound remains the gold standard for anal sphincter evaluation, there is growing evidence that 3D/4D TPU may be a valid, reliable and less invasive alternative.
3D/4D TPU in gynecology: challenges and future perspectives
3D/4D TPU is a very rapidly evolving field, with a huge potential for the improvement of women’s health, increasing our understanding of the etiology and pathophysiology of female pelvic floor dysfunction. A more widespread use of the technique, with more data on the natural history and risk factors for LAM injuries, is needed in order to plan proper prevention and rehabilitation programs for target women. Furthermore, extending pelvic floor assessment to other disorders with possible pelvic floor involvement (eg, chronic pelvic pain disorders)Citation21 may help many women to improve their lifestyles and symptoms.
Obstetrics
Introduction
To date, clinical examination remains the cornerstone of obstetrical management. Various studies demonstrated that digital assessment during the various phases of the labor has proved to be inaccurate, poorly reproducible and related to a great experience of the operator. The use of transabdominal ultrasound and TPU has been proven to be useful in many cases, as a complementary tool to clinical examination.Citation49–Citation58 The integration between obstetrical examination and intrapartum ultrasound could lead to an improvement in the clinical management of the patient, particularly for the choice of operative delivery during labor.
TPU for the assessment of fetal occiput position
There is a growing body of evidence to demonstrate the superiority of ultrasound in comparison to digital examination for the assessment of fetal head position.Citation59–Citation61 The vast majority of the published literature used the transabdominal scan. The use of TPU for the evaluation of the fetal occiput has been recently assessed with very promising results.Citation52 However, considering the relative simplicity of the transabdominal approach,Citation49 the latter remains from our point of view the preferred technique for fetal occiput position determination. Transabdominal ultrasound for this aim is traditionally 2D, although 3D suprapubic ultrasound can be helpful in diagnosing some fetal malpositions.Citation62,Citation63 Nonetheless, there is no evidence to suggest that routine use of ultrasound in labor for fetal position depiction improves outcome; therefore, this should be reserved to specific clinical conditions such as before instrumental delivery and in prolonged labor.
TPU during labor for fetal head progression assessment
TPU offers objective and reproducible measurements of various indices of fetal head progression. The acquisition of ultrasound images for this aim is performed with the patient in lithotomy position, using a convex transducer (volumetric in case of 3D), covered by a sterile glove. The useful planes needed for such assessments are mainly two:
The midsagittal plane (): In this plane, the anatomic landmarks are the pubic symphysis displayed as oval and echogenic and the fetal head bordered by the echoic bones of the skull. Using these two bony landmarks, many TPU parameters have been suggested.Citation54–Citation56,Citation64–Citation67 These parameters assess the relationship between the two landmarks.
The introduction of the use of TPU in labor has been partially hindered by the complexity of some of the suggested parameters and by the lack of substantial evidence about their usefulness.Citation68 For this reason, we chose in this review to present the most studied and simplest parameters from our point of view.Citation69
Indices for labor progression measurable in the midsagittal view include:
The angle of progression (AoP), also called the angle of fetal head descentCitation57,Citation58,Citation65 (): This is the angle formed by a line passing through the long axis of the pubic symphysis and another line running from the lowermost part of the pubic symphysis tangential to the lowermost part of the fetal skull.
The head–symphysis distance (HSD) (): This is the distance between the lowermost part of the pubic symphysis and the fetal skull on a line running perpendicular to the long axis of the pubic symphysis.Citation51,Citation67,Citation70
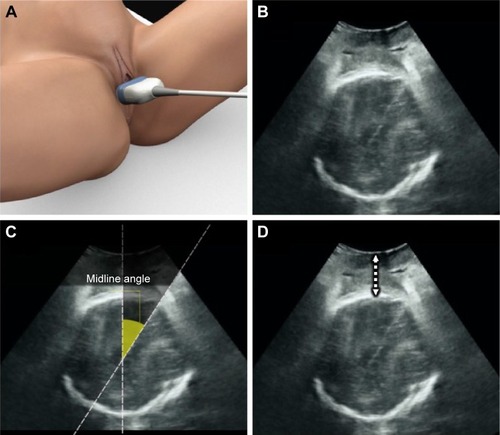
The axial plane (): This plane can be obtained by rotating the transducer 90° from the midsagittal plane. TPU indices which are measurable on this plane include:
The head–perineum distance (HPD): This is the distance between the fetal skull and the perineum.
The midline angle (MLA): This is the only TPU index on the fetal head rotation. It is measured between the midline falx of the fetal brain and the anteroposterior axis of the maternal pelvis.
Figure 6 Technique for transperineal ultrasound scan for fetal head descent assessment on the midsagittal plane.
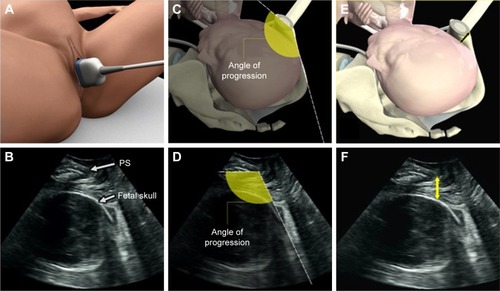
Figure 7 Technique for transperineal ultrasound scan for fetal head descent and rotation assessment on the axial plane.
Evidence on the use of the suggested parameters from 2D ultrasound
AoP is one of the most studied TPU parameters. It is highly reproducible both on 2D and 3D techniques.Citation71,Citation72 An AoP >120° in the second stage of labor seems to be a good predictor of vaginal delivery,Citation65 although there is no consensus on this cut-off. A positive correlation between the AoP measured during the second stage of labor and the time that elapses from the delivery has also been demonstrated.Citation73
The HSD, described by Youssef et al in 2013, and simple to measure, has a good reproducibility and a negative correlation with the AoP.Citation67,Citation70 The HSD measured during the second stage of labor has also been proved to be correlated with the modality of delivery.Citation51
The HPD, defined by Eggebø et al, decreases during the progression of the fetal head in the birth canal and correlates with the mode of delivery in the protracted labor.Citation55,Citation74
The MLA has the advantage of assessing the internal rotation of the fetal head. The narrower the MLA is, the lower the fetal head station is.Citation64
Another ambitious goal for TPU is the prediction of the mode of delivery before the onset of labor. A recent study by Gillor et alCitation75 evaluated the AoP in nulliparous women at term of pregnancy before the pharmacological induction of labor. They found that most women with uncomplicated vaginal delivery had a significantly wider preinduction AoP compared to those who had an emergency cesarean delivery. They also identified a cut-off at 92°: In particular, only 5.2% of women with an AoP >92° had a cesarean section due to failure of induction or dystocia.
3D TPU in labor
Most sonographic parameters assessed during labor have been widely studied using 2D ultrasound. However, some studies have questioned the reproducibility of these parameters owing to the difficulty to standardize the perfect midline and the angle of insonation.Citation76
The main advantages of the introduction of 3D ultrasound for the transperineal assessment of fetal head in labor include:
Many 3D TPU parameters should be measured on the precise midsagittal plane. Using 3D ultrasound multiplanar mode, the operator can be sure of being on the exact midline, thus improving standardization of measurements.
Since on acquired 3D datasets the three orthogonal planes can be displayed on the same volume, one can assess parameters which are measurable on various planes with only one acquisition. For example, one may be able to measure the AoP on the midsagittal plane () to assess the fetal head descent in relation to the pubic symphysis and the MLA on the axial plane () to assess fetal head rotation.
Post hoc analysis: 3D ultrasound volumes include a huge amount of data, which can be saved and then reanalyzed later, thus permitting many reassessments of the data.
Research: The saved volumes can be used later for post hoc analysis, representing an unlimited source of research.
Figure 8 A multiplanar view of three-dimensional transperineal volume performed in labor.
It should be noted however that despite the above-mentioned advantages, 3D/4D techniques are not indispensable for the assessment of the fetal head in labor, but it merely has the potential of providing more reproducible measurements.
Technique
The plane of acquisition is the midsagittal plane (). A low frequency, low depth and maximum angle on 2D is set. For the 3D/4D acquisitions, a maximum angle is used. There is no need to increase the quality of 3D acquisition. Setting a medium or low quality will increase the speed of acquisition, thus saving time.
Special software used in TPU
Many studies have acquired and elaborated the ultrasound parameters in labor using a software called Sonography-based Volume Computer Aided Display labor (SonoVCAD™ labor; GE Medical Systems). One of the most important studies was carried out by the group of Molina et alCitation77 in 2010 in a cohort of women during the second stage of labor. In this population, the authors evaluated the reproducibility of the measurements of head direction (HD), MLA, progression distance (PD) and AoP. They found some technical difficulties with the measurement of MLA especially with high head station due to inappropriate visualization of the fetal brain midline. Difficulty was also encountered with HD, as it is a dynamic subjective measurement of the direction in which the head progresses in maternal pushing, and again, it relies on visualizing the fetal intracranial structures. On the contrary, the assessment of the PD and AoP was more simple. The study demonstrated that the most reliable and reproducible parameter during labor was the AoP. The conclusions of another study, conducted by Ghi et al in 2010 on a group of nulliparous women in the second stage of labor, have led to similar results.Citation71 Various 3D ultrasound parameters resulted highly reproducible during labor, especially AoP and PD, with less reproducibility for MLA.
Torkildsen et al in 2012 studied intraoperator reproducibility and agreement between 2D and 3D ultrasound methods in assessing AoP and HPD in cases of prolonged first stage. Both intraobserver repeatability and intermethod agreement between 2D and 3D acquisitions was satisfactory, indicating that 2D and 3D ultrasound methods might be used interchangeably.Citation78 The association between AoP and HPD was acceptable for both 2D and 3D methods; however, the intraobserver repeatability was slightly better in 3D than 2D acquisitions. Therefore, the above-mentioned studies conclude that 3D ultrasound is highly reproducible especially for AoP measurements, and that it may be more standardized than 2D. On the other hand, some authors advocate that in the absence of clear benefit for 3D over 2D, and in consideration of the simplicity of 2D TPU, the latter technique should be preferred in the labor room.Citation78
Regarding the clinical applicability of 3D TPU, Ghi et al acquired datasets every 20 minutes from nulliparous women in the active second stage of labor.Citation50 They demonstrated that a narrower AoP in the first 20 minutes and a wider MLA later in the second stage were associated with operative delivery (cesarean section or vacuum delivery). Furthermore, on logistic regression analysis, both AoP and MLA were independently associated with operative delivery. They concluded that 3D ultrasonographic assessment of fetal head descent in the second stage of labor may play a role in the prediction of the mode of delivery.
The need of a simple and reproducible parameter was demonstrated by the only survey on caregivers in the literature, which showed that about two-thirds of clinicians think that the suggested parameters were too difficult to be applied in the labor ward.Citation68 Recently, in an attempt to reach a simple and reliable ultrasound parameter for the assessment of fetal head descent, Youssef et al suggested the measurement of the distance between the fetal head and the maternal pubic symphysis (fetal HSD).Citation67 They demonstrated that HSD measurement with 3D TPU has excellent intra- and interobserver reproducibility and an excellent agreement with HSD measured by 2D ultrasound.Citation49,Citation70 HSD also showed good correlation between 2D and 3D measurements performed by an expert operator, even in occiput posterior position of the fetal head.Citation70 In another recent study,Citation51 the same authors evaluated HSD during the second stage of labor at different time intervals, by analyzing 3D ultrasound datasets acquired in the context of a previous paper.Citation50 Lower HSD values at the beginning of the second stage were associated with a higher rate of spontaneous vaginal deliveries. In particular, HSD >24.3 mm in the absence of epidural analgesia and HSD >15.7 mm in the presence of analgesia were associated with a higher risk of operative deliveries.
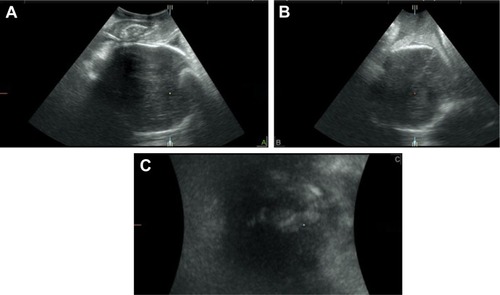
The subpubic arch angle (SPA)
Another interesting topic for the application of 3D TPU is the evaluation of maternal pelvis. The study of the maternal pelvimetry has been the subject of numerous discussions in medical literature. Digital assessment of the maternal pelvis is often imprecise and poorly reproducible.Citation79 X-ray, computed tomography and MRI were often used for this aim allowing obstetricians to measure the pelvis.Citation80,Citation81 However, due to technical complexity and the absence of valid data confirming its usefulness, pelvimetry was not widely applied in clinical practice. Recently, ultrasound pelvimetry has been suggested. The main advantage of the use of ultrasound is its availability to the clinician, and with the introduction of 3D TPU, the pubic rami can be reliably reconstructed.Citation75 The main limitation is the inaccessibility of ultrasound to the posterior and lateral parts of the maternal pelvis. TPU accessibility is limited to the evaluation of the anterior part of the pelvis, namely the pubic rami and the SPA.Citation82–Citation86 SPA is the angle formed by the two inferior branches of the pubic bone in a coronal plane. Although there is some evidence to support the use of 2D TPU for the evaluation of SPA,Citation86 we think that the plane of the pubic arches can only be adequately evaluated by 3D techniques ().Citation82–Citation85
Figure 9 The subpubic arch angle (SPA).
It has been demonstrated that SPA assessment by 3D TPU is highly reproducible.Citation82 Furthermore, a narrow SPA is associated with worse obstetrical outcomes, such as dystocia, vaginal operative delivery, cesarean section, prolonged labor and fetal head malpositions.Citation82–Citation85
Despite the strong correlation with adverse obstetrical outcome, it should be highlighted that the accuracy of SPA in the prediction of complications remains limited,Citation83,Citation84 and should not be used alone for clinical decision making.
Challenges and future perspectives of 3D TPU in obstetrics
As tackled above, 3D TPU is a reliable method for the assessment of fetal head progression in labor, and it is almost the only valid ultrasound technique to assess maternal pelvis. It has to be admitted however that 3D needs more expertise and more expensive ultrasound machines in comparison with the 2D technique. In the absence of strong evidence on its superiority, and in light of the high agreement between 2D and 3D TPU, we consider that it is reasonable to recommend the use of both techniques interchangeably in clinical practice. When the instruments and expertise are available, we think that 3D may offer some advantages over 2D such as higher reproducibility, adequacy for didactic purposes and the ability of post hoc analysis.
Another challenge both 2D and 3D TPU have yet to face is the need for more reliable evidence with clear cut-offs in order to help the clinicians to take decisions in labor ward. Despite the promising evidence on the matter, data from larger populations and different centers and prospective validation are needed in order to promote a more widespread use of TPU in labor. The combination of various parameters such as indices of fetal head descent with maternal pelvic measures may significantly increase the accuracy of prediction models, although this should be thoroughly explored.
The evaluation of TPU parameters prior to the onset of labor for the prevision of labor outcomes is a very promising field that needs to be further explored as well.
Conclusion
3D/4D TPU is a very promising technique both in gynecology and in obstetrics. In gynecology, its main advantage is the evaluation of the pelvic floor muscles. For this aim, 3D/4D TPU offer a unique opportunity for diagnosing reliably pelvic floor injuries and dysfunction with a huge potential for improving women’s health by detecting preventable risk factors for these lesions, by encouraging early pelvic floor rehabilitation for women with asymptomatic lesions and by providing a highly reproducible, quantitative technique for pelvic floor evaluation.
On the other hand, 3D/4D TPU provides a reliable method for fetal head rotation and descent in labor. This may help obstetricians in taking critical decisions on the basis of the reproducible measurable data, in addition to the subjective clinical assessment. Therefore, 3D/4D TPU can be used as a complementary tool in the labor ward.
Disclosure
The authors report no conflicts of interest in this work.
References
- DietzHPPelvic floor trauma following vaginal deliveryCurr Opin Obstet Gynecol200618552853716932048
- DeLanceyJOMorganDMFennerDEComparison of levator ani muscle defects and function in women with and without pelvic organ prolapseObstet Gynecol20071092 Pt 129530217267827
- ShekKLDietzHPThe effect of childbirth on hiatal dimensionsObstet Gynecol200911361272127819461422
- DietzHPPelvic floor ultrasound: a reviewAm J Obstet Gynecol2010202432133420350640
- DietzHPHaylenBTBroomeJUltrasound in the quantification of female pelvic organ prolapseUltrasound Obstet Gynecol200118551151411844174
- DeLanceyJOThe hidden epidemic of pelvic floor dysfunction: achievable goals for improved prevention and treatmentAm J Obstet Gynecol200519251488149515902147
- DietzHPUltrasound imaging of the pelvic floor. Part II: three-dimensional or volume imagingUltrasound Obstet Gynecol200423661562515170808
- DeLanceyJOAnatomyTextbook of Female Urology and UrogynaecologyCardozoLStaskinDIsis Medica MediaLondon, UK2001112124
- DietzHPShekCClarkeBBiometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasoundUltrasound Obstet Gynecol200525658058515883982
- DietzHPSteensmaABThe prevalence of major abnormalities of the levator ani in urogynaecological patientsBJOG2006113222523016412002
- WeemhoffMVergeldtTFNottenKSerroyenJKampschoerPHRoumenFJAvulsion of puborectalis muscle and other risk factors for cystocele recurrence: a 2-year follow-up studyInt Urogynecol J2012231657121822712
- DietzHPQuantification of major morphological abnormalities of the levator aniUltrasound Obstet Gynecol200729332933417323308
- DietzHPAbbuAShekKLThe levator-urethra gap measurement: a more objective means of determining levator avulsion?Ultrasound Obstet Gynecol200832794194519035543
- PatelDAXuXThomasonADRansomSBIvyJSDeLanceyJOChildbirth and pelvic floor dysfunction: an epidemiologic approach to the assessment of prevention opportunities at deliveryAm J Obstet Gynecol20061951232816579934
- DietzHPShekCLevator avulsion and grading of pelvic floor muscle strengthInt Urogynecol J Pelvic Floor Dysfunct200819563363617999021
- AbdoolZShekKLDietzHPThe effect of levator avulsion on hiatal dimension and functionAm J Obstet Gynecol2009201189.e189.e519426956
- DietzHPBernardoMJKirbyAShekKLMinimal criteria for the diagnosis of avulsion of the puborectalis muscle by tomographic ultrasoundInt Urogynecol J201122669970421107811
- VolloyhaugIWongVShekKLDietzHPDoes levator avulsion cause distension of the genital hiatus and perineal body?Int Urogynecol J20132471161116523184139
- van DelftKSultanAHThakarRSchwertner-TiepelmannNKluiversKThe relationship between postpartum levator ani muscle avulsion and signs and symptoms of pelvic floor dysfunctionBJOG2014121911641171 discussion 117224548759
- DietzHPSimpsonJMLevator trauma is associated with pelvic organ prolapseBJOG2008115897998418503571
- RaimondoDYoussefAMabroukMPelvic floor muscle dysfunction at 3D/4D transperineal ultrasound in patients with deep infiltrating endometriosis: a pilot studyUltrasound Obstet Gynecol Epub2016108
- DurneaCMO’ReillyBAKhashanASStatus of the pelvic floor in young primiparous womenUltrasound Obstet Gynecol201546335636225359670
- DietzHPShekCDe LeonJSteensmaABBallooning of the levator hiatusUltrasound Obstet Gynecol200831667668018470963
- ShekKLDietzHPIntrapartum risk factors for levator traumaBJOG2010117121485149220735379
- AlbrichSBLaterzaRMSkalaCSalvatoreSKoelblHNaumannGImpact of mode of delivery on levator morphology: a prospective observational study with three-dimensional ultrasound early in the postpartum periodBJOG20121191516021985531
- ChanSSCheungRYYiuAKPrevalence of levator ani muscle injury in Chinese women after first deliveryUltrasound Obstet Gynecol201239670470922045587
- Cassadó GarrigaJPessarrodona IsernAEspuña PonsMFour-dimensional sonographic evaluation of avulsion of the levator ani according to delivery modeUltrasound Obstet Gynecol201138670170621837763
- Garcia-MejidoJAGutierrez-PalominoLBorreroCValdiviesoPFernandez-PalacinASainz-BuenoJAFactors that influence the development of avulsion of the levator ani muscle in eutocic deliveries: 3-4D transperineal ultrasound studyJ Matern Fetal Neonatal Med201629193183318626634392
- YangJMYangSHHuangWCBiometry of the pubovisceral muscle and levator hiatus in nulliparous Chinese womenUltrasound Obstetrics Gynecol2006285710716
- SiafarikasFStaer-JensenJBraekkenIHBøKEnghMELearning process for performing and analyzing 3D/4D transperineal ultrasound imaging and interobserver reliability studyUltrasound Obstet Gynecol201341331231722605574
- MajidaMBraekkenIHUmekWBøKSaltyte BenthJEllstrøm EnghMInterobserver repeatability of three- and four-dimensional transperineal ultrasound assessment of pelvic floor muscle anatomy and functionUltrasound Obstet Gynecol200933556757319402120
- van VeelenGASchweitzerKJvan der VaartCHReliability of pelvic floor measurments on three- and four-dimensional ultrasound during and after first pregnancy: implications for trainingUltrasound Obstet Gynecol201342559059523729398
- BraekkenIHMajidaMEllstrøm-EnghMDietzHPUmekWBøKTest-retest and intra-observer repeatability of two-, three- and four-dimensional perineal ultrasound of pelvic floor muscle anatomy and functionInt Urogynecol J Pelvic Floor Dysfunct200819222723517599234
- ChenRSongYJiangLHongXYePThe assessment of voluntary pelvic floor muscle contraction by three-dimensional transperineal ultrasonographyArch Gynecol Obstet2011284493193621161256
- BraekkenIHMajidaMEnghMEBøKTest-retest reliability of pelvic floor muscle contraction measured by 4D ultrasoundNeurourol Urodyn2009281687318932174
- van DelftKThakarRSultanAHPelvic floor muscle contractility: digital assessment vs transperineal ultrasoundUltrasound Obstet Gynecol201545221722225044167
- van DelftKWSultanAHThakarRShobeiriSAKluiversKBAgreement between palpation and transperineal and endovaginal ultrasound in the diagnosis of levator ani avulsionInt Urogynecol J2015261333924859796
- DietzHPWongVShekKLA simplified method for determining hiatal biometryAust N Z J Obstet Gynaecol201151654054321951068
- YoussefAMontagutiESanlorenzoOA new simple technique for 3-dimensional sonographic assessment of the pelvic floor musclesJ Ultrasound Med2015341657225542941
- YoussefAMontagutiESanlorenzoOReliability of new three-dimensional ultrasound technique for pelvic hiatal area measurementUltrasound Obstet Gynecol201647562963526105710
- YoussefACavaleraMPacellaGIs a curved 3D ultrasound reconstruction needed to assess the “warped” pelvic floor plane?Ultrasound Obstet Gynecol Epub2019919
- DietzHPBarryCLimYNRaneATwo-dimensional and three-dimensional ultrasound imaging of suburethral slingsUltrasound Obstet Gynecol200526217517915988786
- HuangWCYangSHYangJMThree-dimensional transperineal sonographic characteristics of the anal sphincter complex in nulliparous womenUltrasound Obstet Gynecol200730221022017659660
- ValskyDVMessingBPetkovaRPostpartum evaluation of the anal sphincter by transperineal three-dimensional ultrasound in primiparous women after vaginal delivery and following surgical repair of third-degree tears by the overlapping techniqueUltrasound Obstet Gynecol200729219520417219371
- ValskyDVCohenSMLipschuetzMHochner-CelnikierDYagelSThree-dimensional transperineal ultrasound findings associated with anal incontinence after intrapartum sphincter tears in primiparous womenUltrasound Obstet Gynecol2012391839021845740
- FaltinDLBoulvainMIrionOBretonesSStanCWeilADiagnosis of anal sphincter tears by postpartum endosonography to predict fecal incontinenceObstet Gynecol200095564364710775721
- Guzmán RojasRAShekKLLangerSMDietzHPPrevalence of anal sphincter injury in primiparous womenUltrasound Obstet Gynecol201342446146623576493
- Guzmán RojasRAKamisan AtanIShekKLDietzHPAnal sphincter trauma and anal incontinence in urogynecological patientsUltrasound Obstet Gynecol201546336336625766889
- YoussefAGhiTPiluGHow to perform ultrasound in labor: assessment of fetal occiput positionUltrasound Obstet Gynecol201341447647823641505
- GhiTYoussefAMaroniEIntrapartum transperineal ultrasound assessment of fetal head progression in active second stage of labor and mode of deliveryUltrasound Obstet Gynecol201341443043523288706
- YoussefAMaroniECarielloLFetal head-symphysis distance and mode of delivery in the second stage of laborActa Obstet Gynecol Scand201493101011101725040777
- GhiTBellussiFEggebøTSonographic assessment of fetal occiput position during the second stage of labor: how reliable is the transperineal approach?J Matern Fetal Neonatal Med201528161985198825316562
- ShererDMMiodovnikMBradleyKSLangerOIntrapartum fetal head position II: comparison between transvaginal digital examination and transabdominal ultrasound assessment during the second stage of laborUltrasound Obstet Gynecol200219326426811896948
- DietzHPLanzaroneVMeasuring engagement of the fetal head: validity and reproducibility of a new ultrasound techniqueUltrasound Obstet Gynecol200525216516815505817
- EggebøTMGjessingLKHeienCPrediction of labor and delivery by transperineal ultrasound in pregnancies with prelabor rupture of membranes at termUltrasound Obstet Gynecol200627438739116565994
- HenrichWDudenhausenJFuchsIKämenaATutschekBIntrapartum translabial ultrasound (ITU): sonographic landmarks and correlation with successful vacuum extractionUltrasound Obstet Gynecol200628675376017063455
- BarberaAFPombarXPeruginoGLezotteDCHobbinsJCA new method to assess fetal head descent in labor with transperineal ultrasoundUltrasound Obstet Gynecol200933331331919248000
- TutschekBBraunTChantraineFHenrichWA study of progress of labour using intrapartum translabial ultrasound, assessing head station, direction, and angle of descentBJOG20111181626921083864
- RamphulMOoiPVBurkeGInstrumental delivery and ultrasound: a multicentre randomised controlled trial of ultrasound assessment of the fetal head position versus standard care as an approach to prevent morbidity at instrumental deliveryBJOG201412181029103824720273
- PopowskiTPorcherRFortJJavoiseSRozenbergPInfluence of ultrasound determination of fetal head position on mode of delivery: a pragmatic randomized trialUltrasound Obstet Gynecol201546552052525583399
- YoussefAPiluGKnowledge, understanding and fetal occiput positionUltrasound Obstet Gynecol201647452352427062977
- GhiTMaroniEYoussefAIntrapartum three-dimensional ultrasonographic imaging of face presentations: report of two casesUltrasound Obstet Gynecol201240111711822223511
- GhiTYoussefAPiluGMalvasiARagusaAIntrapartum sonographic imaging of fetal head asynclitismUltrasound Obstet Gynecol201239223824021523842
- GhiTFarinaAPedrazziARizzoNPelusiGPiluGDiagnosis of station and rotation of the fetal head in the second stage of labor with intrapartum translabial ultrasoundUltrasound Obstet Gynecol200933333133619202576
- KalacheKDDückelmannAMMichaelisSALangeJCichonGDudenhausenJWTransperineal ultrasound imaging in prolonged second stage of labor with occipitoanterior presenting fetuses: how well does the ‘angle of progression’ predict the mode of delivery?Ultrasound Obstet Gynecol200933332633019224527
- TutschekBTorkildsenEAEggebøTMComparison between ultrasound parameters and clinical examination to assess fetal head station in laborUltrasound Obstet Gynecol201341442542923371409
- YoussefAMaroniERagusaAFetal head-symphysis distance: a simple and reliable ultrasound index of fetal head station in laborUltrasound Obstet Gynecol201341441942423124698
- YoussefAGhiTAwadEEUltrasound in labor: a caregiver’s perspectiveUltrasound Obstet Gynecol201341446947022807171
- YoussefABellussiFMaroniEPiluGRizzoNGhiTUltrasound in labor: is it time for a more simplified approach?Ultrasound Obstet Gynecol201341671071123280777
- YoussefABellussiFMontagutiEAgreement between two- and three-dimensional transperineal ultrasound methods for assessment of fetal head-symphysis distance in active laborUltrasound Obstet Gynecol201443218318824006290
- GhiTControEFarinaANobileMPiluGThree-dimensional ultrasound in monitoring progression of labor: a reproducibility studyUltrasound Obstet Gynecol201036450050620652931
- DückelmannAMBambergCMichaelisSAMeasurement of fetal head descent using the ‘angle of progression’ on transperineal ultrasound imaging is reliable regardless of fetal head station or ultrasound expertiseUltrasound Obstet Gynecol201035221622220069668
- GhiTMaroniEYoussefASonographic pattern of fetal head descent: relationship with duration of active second stage of labor and occiput position at deliveryUltrasound Obstet Gynecol2014441828924496823
- EggebøTMHassanWASalvesenKÅTorkildsenEAØstborgTBLeesCCPrediction of delivery mode by ultrasound-assessed fetal position in nulliparous women with prolonged first stage of laborUltrasound Obstet Gynecol201546560661025536955
- GillorMVaisbuchEZaksSBarakOHagayZLevyRTransperineal sonographic assessment of angle of progression as a predictor of a successful vaginal delivery following induction of laborUltrasound Obstet Gynecol201749224024527062415
- PaltieliYNizardJA question of angle of viewUltrasound Obstet Gynecol2009343363364 author reply 364–36619670331
- MolinaFSTerraRCarrilloMPPuertasANicolaidesKHWhat is the most reliable ultrasound parameter for assessment of fetal head descent?Ultrasound Obstet Gynecol201036449349920533441
- TorkildsenEASalvesenKÅEggebøTMAgreement between two- and three-dimensional transperineal ultrasound methods in assessing fetal head descent in the first stage of laborUltrasound Obstet Gynecol201239331031521630362
- BöttcherBRadleySCPelvimetry: changing trends and attitudesJ Obstet Gynaecol200121545946212521797
- Huerta-EnochianGSKatzVLFoxLKHamlinJAKollathJPMagnetic resonance-based serial pelvimetry: do maternal pelvic dimensions change during pregnancy?Am J Obstet Gynecol2006194616891694 discussion 1694–169516731086
- RozenbergPIs there a role for X-ray pelvimetry in the twenty-first century?Gynecol Obstet Fertil2007351612 French [with English abstract]17188014
- GhiTYoussefAMartelliFA new method to measure the subpubic arch angle using 3-D ultrasoundFetal Diagn Ther201538319519925871360
- GhiTYoussefAMartelliFNarrow subpubic arch angle is associated with higher risk of persistent occiput posterior position at deliveryUltrasound Obstet Gynecol201648451151526565728
- YoussefAGhiTMartelliFSubpubic arch angle and mode of delivery in low-risk nulliparous womenFetal Diagn Ther201640215015526555940
- YoussefASalsiGCataneoIAgreement between two 3D ultrasound techniques for the assessment of the subpubic arch angleJ Matern Fetal Neonatal Med201638315
- GilboaYKivilevitchZSpiraMPubic arch angle in prolonged second stage of labor: clinical significanceUltrasound Obstet Gynecol201341444244623001876
- YoussefASalsiGMontagutiEAutomated measurement of the angle of progression in labor: a feasibility and reliability studyFetal Diagn Ther Epub201693
