Abstract
Since its introduction in the People’s Republic of China in 1992, minimally invasive esophagectomy (MIE) has shown the classical advantages of minimally invasive surgery over its open counterpart. Like all pioneers of the technique, cardiothoracic surgeons in the People’s Republic of China claim that MIE has a lower risk of pulmonary infection, faster recovery, a shorter hospital stay, and a more rapid return to daily activities than open esophagectomy, while offering the same functional and oncologic results. There has been burgeoning interest in MIE in the People’s Republic of China since 1995. The last decade has witnessed nationwide growth in the application of MIE and yielded a significant amount of scientific data in support of its clinical merits and advantages. However, no prospective randomized controlled trials have actually investigated the benefits of MIE in the People’s Republic of China. Here we review the current data and state of the art MIE treatment for esophageal cancer in the People’s Republic of China.
Introduction
The global incidence of esophageal cancer has increased by 50% in the past two decades.Citation1,Citation2 Advances in neoadjuvant and adjuvant chemotherapy and chemoradiotherapy have led to increasingly multimodal treatment for patients with esophageal cancer, which has decreased the rate of local recurrence and improved long-term survival for some patients. However, surgical resection with radical lymphadenectomy is regarded as one of the curative options for resectable esophageal cancer.Citation3–Citation6 Frequently, due consideration of surgical resection may not be given because of concerns with regard to the morbidity of open esophagectomy.
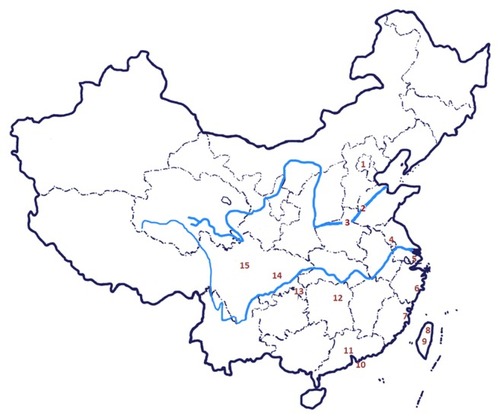
In an effort to decrease the morbidity associated with open esophagectomy, Chinese surgeons have adopted a minimally invasive approach to esophageal resection. Because of the potential advantages, including avoiding thoracotomy and laparotomy and reducing the rate of pulmonary infections (thus reducing the inpatient stay),Citation7,Citation8 minimally invasive esophagectomy (MIE) was introduced into clinical practice in TaiwanCitation9 in 1992 at the same time as in Western countries,Citation10–Citation12 was gradually implemented, and is now a commonplace procedure in the People’s Republic of China (), including in Beijing,Citation13–Citation15 Jinan in Shandong Province,Citation16 Zhengzhou in Henan Province,Citation17 Nanjing in Jiangsu Province,Citation18 Shanghai,Citation19–Citation30 Taizhou in Zhejiang Province,Citation31–Citation33 Fuzhou in Fujian Province,Citation34–Citation36 TaipeiCitation9 and TaichungCitation37 in Taiwan, Hongkong,Citation38–Citation40 Guangzhou in Guangdong Province,Citation41,Citation42 Changsha in Hunan Province,Citation43 Chongqing,Citation44,Citation45 and ChengduCitation46–Citation48 and NanchongCitation49 in Sichuan Province. There has been burgeoning interest in MIE since it was first described in Taiwan in 1995Citation9 and in the People’s Republic of China in 1999.Citation13 The last decade has witnessed nationwide growth in use of MIE, yielding a significant amount of scientific data to support its clinical merits and advantages. Here we review the current data and state of the art for MIE in the treatment of esophageal cancer in the People’s Republic of China.
Figure 1 Fifteen national areas implementing minimally invasive esophagectomy in the People’s Republic of China.
Literature on MIE in the People’s Republic of China
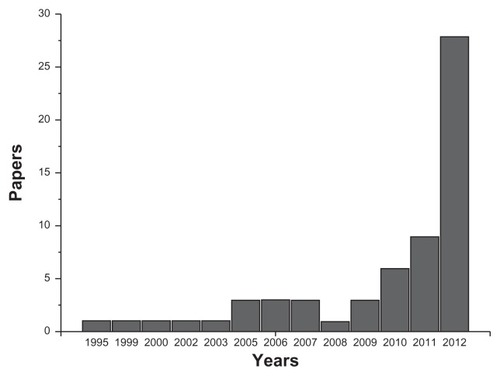
The current literature was reviewed by searching the PubMed/Medline database from January 1992 to December 2012 using keywords such as “minimally invasive oesophagectomy”, “MIE”, and “China”. Sixty-one full articles were found to be relevant to MIE (). A total of 33 publications (54.1%) were in English. However, nearly half of all relevant clinical reports (28, 45.9%) were published in Chinese, despite the fact that it has been necessary to report the current status of MIE as performed in the People’s Republic of China to cardiothoracic surgeons worldwide. A marked increase in the number of papers dedicated to MIE was observed from 2010 to 2012 (), which probably reflects increased research interest among the surgical community and wider clinical application of this patient-friendly approach.
Operative data on MIE
Key outcomes of the major studies are summarized in the and . Thirty-two relevant papers, consisting of prospective and retrospective studies, were identified. Eight papers directly compared open oesophagectomy and MIE, andCitation16,Citation17,Citation21,Citation30,Citation31,Citation39,Citation41,Citation48 five of these involved studies performed prospectively.Citation16,Citation31,Citation39,Citation41,Citation48 Common outcome measures included operative data (operative time, blood loss, conversion rate), morbidity (duration of intensive care and total hospital stay), complications (pulmonary complications, anastomotic leaks, chylothorax), mortality data, and follow-up periods. Neoadjuvant treatment numbers were included for each study.
Table 1 Survey over major reports of minimally invasive esophagectomy in the People’s Republic of China: operative data
Table 2 Survey of major reports of minimally invasive esophagectomy in the People’s Republic of China: mortality, morbidity, and postoperative complications
Surgical approaches
Surgical approaches for MIE performed by Chinese cardiothoracic surgeons are multiple and complicated. As listed in , the majority of centers use mainly total MIE (laparoscopic and thoracoscopic esophagectomy), whereas hybrid MIE (thoracoscopy and laparotomy/laparoscopy and thoracotomy) is used in routine practice in some centers. At our center, we originally used hybrid MIECitation31 but more recently transitioned to a minimally invasive modified McKeown 3-incision total MIE (laparoscopic and thoracoscopic esophagectomy) in 2010.Citation32,Citation33
Operative time and blood loss
Operative time varied significantly between the studies, reflecting the type of MIE performed as well as accumulated experience and technical skills (). Blood loss also varied significantly from center to center, comprising around 100–700 mL (). Major blood loss and need for blood transfusion in particular increased the risk of postoperative morbidity and mortality.
Conversion to open esophagectomy
The conversion rate reported in the literature is in a range of 0%–9.7% (). However, with surgical experience, the conversion rate reduces and currently does not exceed 5% in expert centers in the People’s Republic of China. The main reason for conversion was bleeding. It is not appropriate to consider conversion from MIE to open esophagectomy as a failure because patient safety and the oncologic integrity of the procedure should be of supreme importance.
Mortality, morbidity, and postoperative complications
Mortality rates following total MIE vary between 0% and 7.7% (), which compares favorably with an open transthoracic procedure mortality rate of 9.2% and an open transhiatal procedure mortality rate of 7.2%.Citation50 However, at least half of the patients who undergo open oesophagectomy, performed through a right thoracotomy and laparotomy, are at risk of developing pulmonary complications requiring a protracted stay in intensive care, with consequences for quality of life during convalescence.Citation50 Anastomotic leak is one of the most feared complications of MIE. From the operative data, the MIE leakage rate was in the range of 0%–20.8% (), which is comparable with the leakage rates reported for open oesophagectomy.Citation51 Median duration of postoperative stay in intensive care following MIE was one day in the majority of studies (). MIE is associated with a significant reduction in hospital stay, with a mean postoperative stay of 12 days ().
Outcomes
There is little survival data for MIE available in the People’s Republic of China. Only one study reported overall survival after MIE.Citation25 Feng et al reported median survival for patients in a thoracoscope-assisted transthoracic esophagectomy group and in a mediastinoscope-assisted transhiatal esophagectomy group of 34.4 months and 36.8 months, respectively.Citation25 There do not appear to be any prospective, randomized, controlled trials comparing the oncologic outcome of MIE with that of open esophagectomy. The present knowledge is based mainly on short-term, nonrandomized comparative studies or historical comparisons with outcomes of open surgery.Citation31,Citation39,Citation41,Citation48
Conclusion
In conclusion, MIE is becoming more popular in the People’s Republic of China now that Chinese cardiothoracic surgeons are receiving adequate training in major centers. Use of the technique is growing in the People’s Republic of China, as confirmed by the increasing number of recently published papers on MIE. However, no prospective, randomized, controlled trials have investigated the benefits of MIE in this country. Such trials, directly comparing MIE and open approaches, are urgently needed.
Acknowledgments
This work was supported by grants from Zhejiang Provincial Science and Technology Major Projects (2011C13039-2) and Zhejiang Provincial Science and Technology Innovation Team Projects (2011R09040-03).
Disclosure
The authors report no conflicts of interest in this work.
References
- JemalABrayFCenterMMFerlayJWardEFormanDGlobal cancer statisticsCA Cancer J Clin2011612699021296855
- ParkinDMPisaniPFerlayJGlobal cancer statisticsCA Cancer J Clin1999491336410200776
- EnzingerPCMayerRJEsophageal cancerN Engl J Med2003349232241225214657432
- SjoquistKMBurmeisterBHSmithersBMSurvival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysisLancet Oncol201112768169221684205
- CerfolioRJBryantASHawnMTTechnical aspects and early results of robotic esophagectomy with chest anastomosisJ Thorac Cardiovasc Surg20131451909622910197
- KastenmeierAGonzalesHGouldJCRobotic applications in the treatment of diseases of the esophagusSurg Laparosc Endosc Percutan Tech201222430430922874678
- PalaniveluCPrakashASenthilkumarRMinimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position – experience of 130 patientsJ Am Coll Surg2006203171616798482
- LuketichJDAlvelo-RiveraMBuenaventuraPOMinimally invasive esophagectomy: outcomes in 222 patientsAnn Surg2003238448649414530720
- LiuHPChangCHLinPJChangJPVideo-assisted endoscopic esophagectomy with stapled intrathoracic esophagogastric anastomosisWorld J Surg19951957457477571674
- SabanathanSMearnsAJRichardsonJEndoscopic oesophagectomy through a right thoracoscopic approachJ R Coll Surg Edinb19923742842851383535
- DePaulaALHashibaKFerreiraEAde PaulaRAGreccoELaparoscopic transhiatal esophagectomy with esophagogastroplastySurg Laparosc Endosc199551157735533
- ZinggUMcQuinnADiValentinoDMinimally invasive versus open esophagectomy for patients with esophageal cancerAnn Thorac Surg200987391191919231418
- WangJLiuTXingMVideo-assisted thoracic surgery in the management of chest diseasesZhonghua Yi Xue Za Zhi1999798589591 Chinese11715405
- LiHHuBYouBMiaoJBFuYLChenQRCombined laparoscopic and thoracoscopic Ivor Lewis esophagectomy for esophageal cancer: initial experience from the People’s Republic of ChinaChin Med J (Engl)201212581376138022613638
- LiHHuBYouBCompletely minimally invasive Ivor Lewis esophagectomy: the preliminary experience of circular-stapled anastomosis with the trans-oral anvilZhonghua Wai Ke Za Zhi2010482217471750 Chinese21211459
- DuJJMengLChenJHHand-assisted video-thoracoscopy for resection of esophageal cancerZhonghua Wai Ke Za Zhi2005436351353 Chinese15854336
- LiuBXLiYQinJJComparison of thoracolaparoscopic and open three-field subtotal esophagectomy for esophageal cancerZhonghua Wei Chang Wai Ke Za Zhi2012159938942 Chinese22990928
- HouYLZhaoJQGuoWZangBTangDRComparison of the short- term outcomes of patients with esophageal cancer after subtotal esophagectomy via thoracoscopy in left lateral position and in prone positionZhonghua Wei Chang Wai Ke Za Zhi2012159950953 Chinese22990931
- XueLPanTXuZMulti-factor investigation of early postoperative cardiac arrhythmia for elderly patients with esophageal or cardiac carcinomaWorld J Surg200933122615261919760310
- WuBXueLQiuMVideo-assisted mediastinoscopic transhiatal esophagectomy combined with laparoscopy for esophageal cancerJ Cardiothorac Surg2010513221194430
- MaoTFangWTGuZTYaoFGuoXFChenWHComparative study of perioperative complications and lymphadenectomy between minimally invasive esophagectomy and open procedureZhonghua Wei Chang Wai Ke Za Zhi2012159922925 Chinese22990924
- ZhouJChenHLuJJApplication of a modified McKeown procedure (thoracoscopic esophageal mobilization three-incision esophagectomy) in esophageal cancer surgery: initial experience with 30 casesDis Esophagus200922868769319392854
- TanLJWangQFengMXVideo-assisted thoracoscopic esophagectomy in esophageal carcinomaZhonghua Wei Chang Wai Ke Za Zhi20081112427 Chinese18197488
- WangHFengMTanLWangQComparison of the short-term quality of life in patients with esophageal cancer after subtotal esophagectomy via video-assisted thoracoscopic or open surgeryDis Esophagus201023540841419930404
- FengMXWangHZhangYTanLJXuZLQunWMinimally invasive esophagectomy for esophageal squamous cell carcinoma: a case-control study of thoracoscope versus mediastinoscope assistanceSurg Endosc20122661573157822179461
- WangHTanLFengMZhangYWangQComparison of the short-term health-related quality of life in patients with esophageal cancer with different routes of gastric tube reconstruction after minimally invasive esophagectomyQual Life Res201120217918920857337
- FengMXTanLJWangHComparison of thoracoscopic esophagectomy in decubitus position with prone positionZhonghua Wei Chang Wai Ke Za Zhi2011149686688 Chinese21948532
- ShenYZhangYTanLExtensive mediastinal lymphadenectomy during minimally invasive esophagectomy: optimal results from a single centerJ Gastrointest Surg201216471572122258878
- FengMShenYWangHThoracolaparoscopic esophagectomy: is the prone position a safe alternative to the decubitus position?J Am Coll Surg2012214583884422421259
- WangHTanLJLiJPEvaluation of safety of video-assisted thoracoscopic esophagectomy for esophageal carcinomaZhonghua Wei Chang Wai Ke Za Zhi2012159926929 Chinese22990925
- ZhuCCChenSLYeMHEsophagectomy combined with radical lymphadenectomy by video-thoracoscopyZhonghua Wai Ke Za Zhi20054310628630 Chinese16008927
- ChenBFZhuCCWangCGClinical comparative study of minimally invasive esophagectomy versus open esophagectomy for esophageal carcinomaZhonghua Wai Ke Za Zhi2010481612061209 Chinese21055206
- ZhuCCChenBFKongMNeoadjuvant chemoradiotherapy followed by combined thoracoscopic and laparoscopic esophagectomy in the treatment of locally advanced esophageal carcinomaZhonghua Wei Chang Wai Ke Za Zhi2012159943946 Chinese22990929
- LinJKangMChenCThoracolaparoscopy oesophagectomy and extensive two-field lymphadenectomy for oesophageal cancer: Introduction and teaching of a new technique in a high-volume centreEur J Cardiothorac Surg201343111512122518035
- LiuSYWangFZhengQFChenXFClinical application of minimally invasive esophagectomy for esophageal carcinomaZhonghua Wei Chang Wai Ke Za Zhi2012159947949 Chinese22990930
- LinJBKangMQLinRBZhenWChenCThoracolaparoscopic esophagectomy with two-field lymph node dissection for esophageal carcinoma: report of 150 casesZhonghua Wei Chang Wai Ke Za Zhi2012159930933 Chinese22990926
- LinFCRussellHFergusonMKStrangulation of the reconstructive gastric tube by the azygos archAnn Thorac Surg2006822e8e1016863732
- CenseHALawSWeiWPharyngo-laryngo-esophagectomy using the thoracoscopic approachSurg Endosc200721687968417103269
- LawSYFokMWeiWIThoracoscopic esophageal mobilization for pharyngo-laryngo-esophagectomyAnn Thorac Surg200070241842210969655
- WongSKChanACLeeDWToEWNgEKChungSCMinimal invasive approach of gastric and esophageal mobilization in total pharyngo-laryngo-esophagectomy: total laparoscopic and hand-assisted laparoscopic techniqueSurg Endosc200317579880212582757
- WangYBCaiRJHanYJWangWJYangXYLiuSEQuality of life in patients with esophageal carcinoma undergoing thoracoscopic and laparoscopic esophagectomy and circular stapled cervical esophagogastric anastomosis via retrosternal routeZhonghua Wei Chang Wai Ke Za Zhi2011146428431 Chinese21713702
- XieXFuJHWangJYAnalysis of learning process of video-assisted minimally invasive esophagectomy for thoracic esophageal carcinomaZhonghua Wei Chang Wai Ke Za Zhi2012159918921 Chinese22990923
- YuanYCXiaZKYinNYinBLHuJGModified thoracoscopic versus minimally invasive oesophagectomy in curative resection of oesophageal cancerJ Int Med Res201139390491121819723
- GuoWZouYBMaZOne surgeon’s learning curve for video-assisted thoracoscopic esophagectomy for esophageal cancer with the patient in lateral position: how many cases are needed to reach competence?Surg Endosc10242012 [Epub ahead of print.]
- GuoWZhaoYPJiangYGPrevention of postoperative chylothorax with thoracic duct ligation during video-assisted thoracoscopic esophagectomy for cancerSurg Endosc20122651332132622044984
- ZhangZMWangYGaoYSSongYMaLMinimally invasive esophagectomy for esophageal carcinoma: clinical analysis of 160 casesZhonghua Wei Chang Wai Ke Za Zhi2012159934937 Chinese22990927
- WangZQZhangYCZhangQZhuXJShuYZhouZGLaparoscopic transhiatal extended gastrectomy for type II, III esophagogastric junction cancer: a preliminary report of 55 casesZhonghua Wei Chang Wai Ke Za Zhi2010139652655 Chinese20878569
- GaoYWangYChenLZhaoYComparison of open three-field and minimally-invasive esophagectomy for esophageal cancerInteract Cardiovasc Thorac Surg201112336636921186282
- RenMYHuangBZhangJPuMDengSHLaparoscopic transhiatal proximal gastrectomy for adenocarcinoma of the esophagogastric junction: report of 98 casesZhonghua Wei Chang Wai Ke Za Zhi2012159906909 Chinese22990920
- HulscherJBvan SandickJWde BoerAGExtended transthoracic resection compared with limited transhiatal resection for adenocarcinoma of the esophagusN Engl J Med2002347211662166912444180
- HulscherJBTijssenJGObertopHvan LanschotJJTransthoracic versus transhiatal resection for carcinoma of the esophagus: a meta-analysisAnn Thorac Surg200172130631311465217